endocrine system
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
70 Terms
local communication methods ( 3 types )
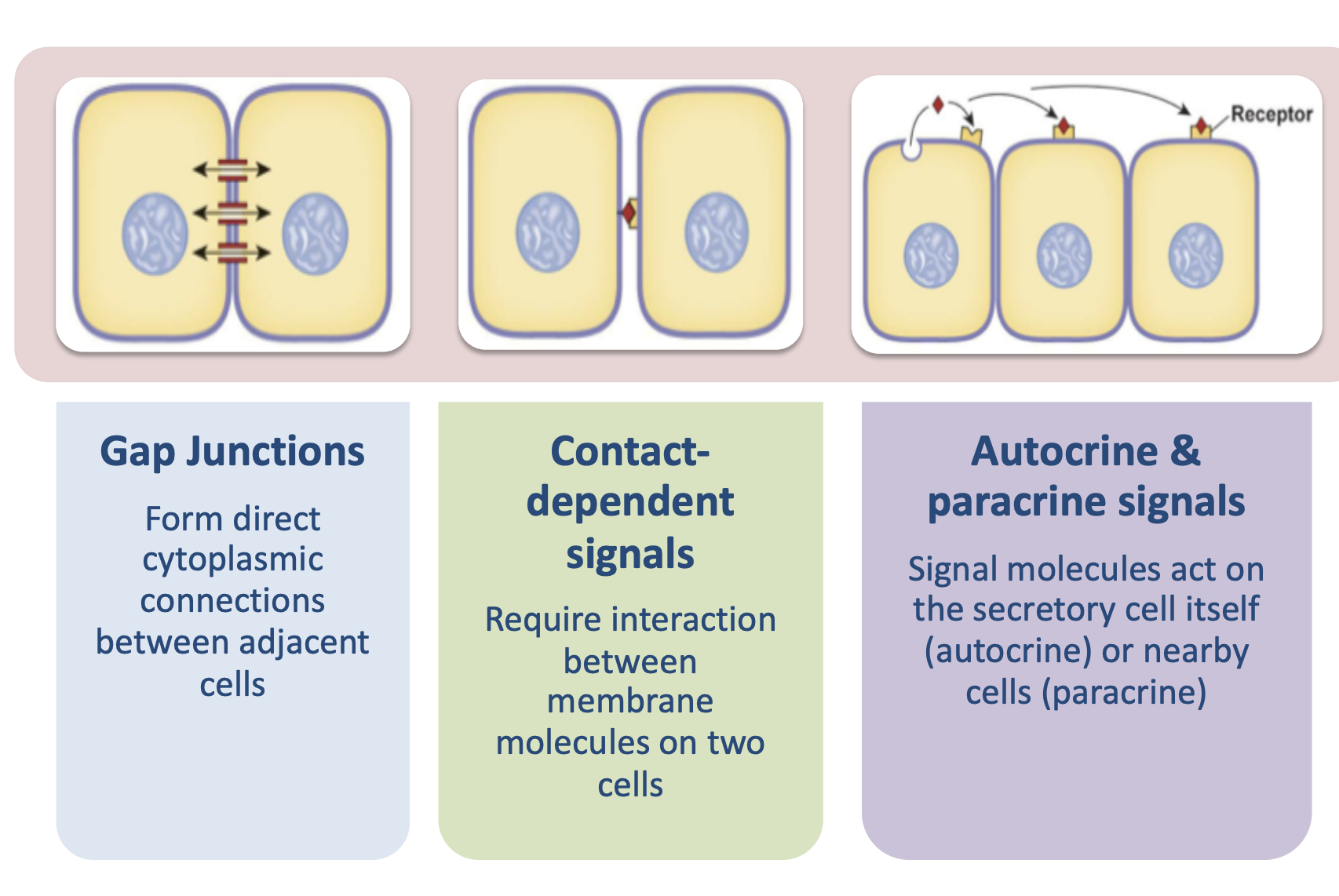
Proteins called connexions form pore like structures in gap junctions
Also provide electrical pathway for heart and other things
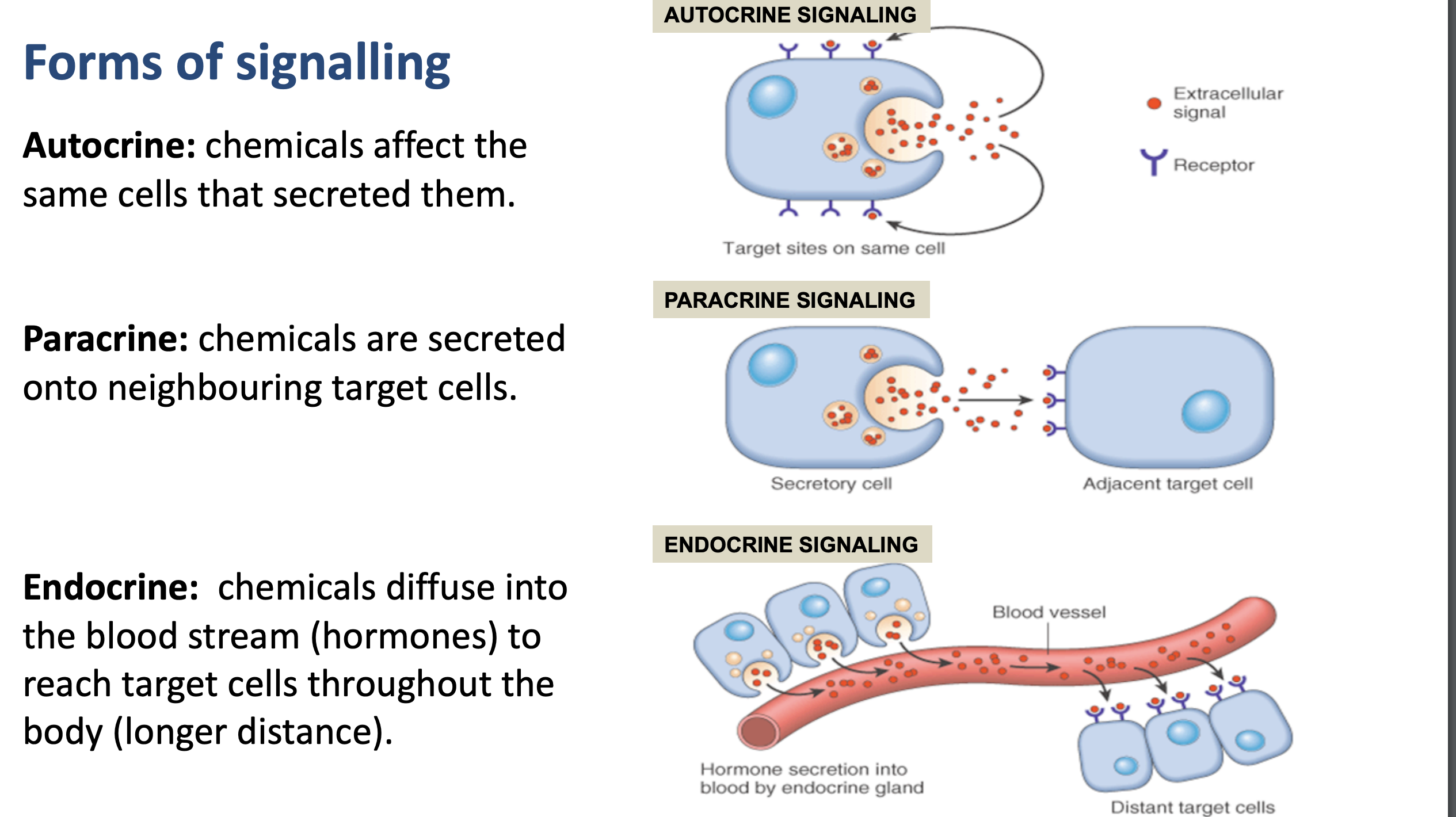
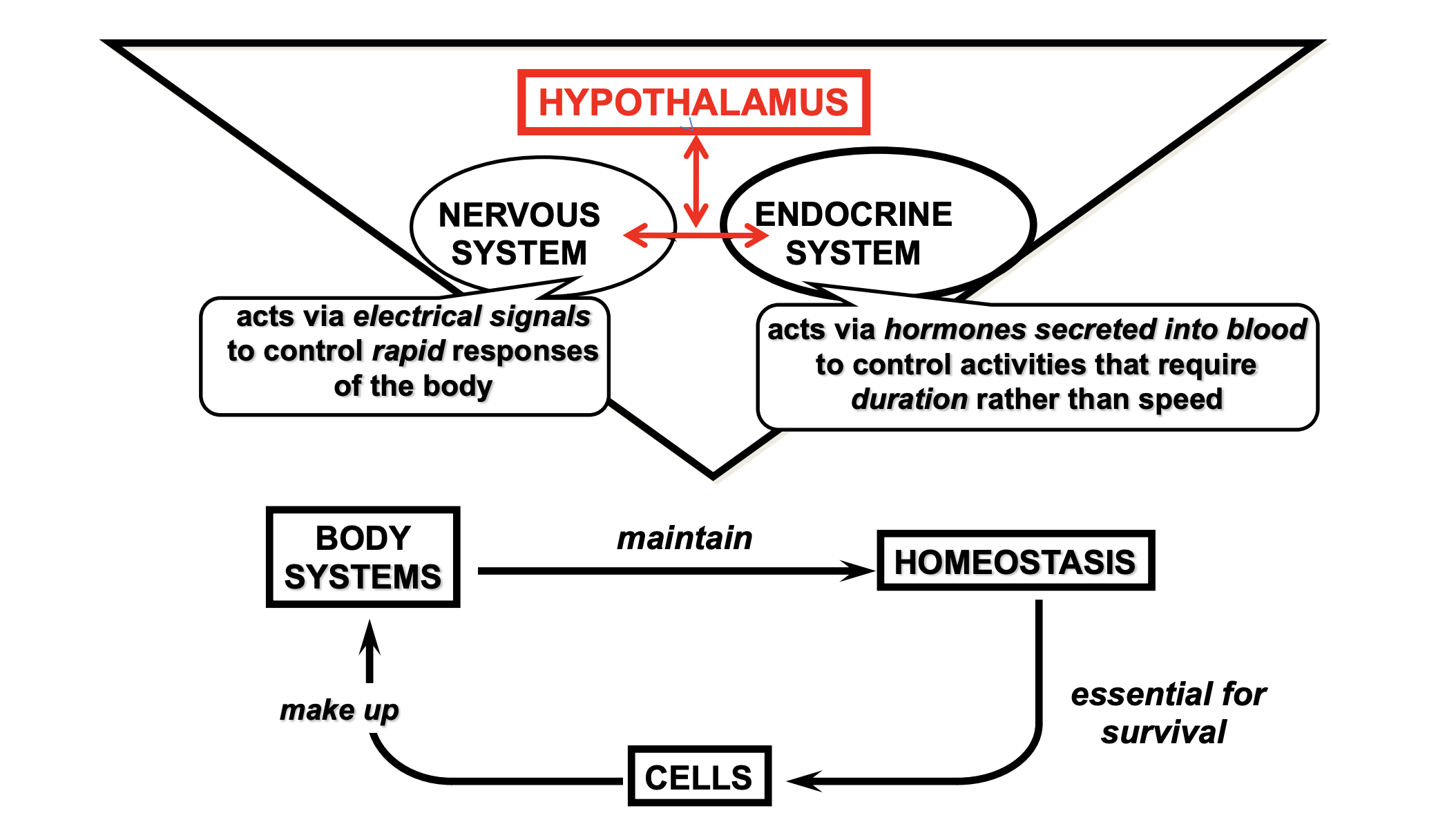
types of signalling
endocrine versus exocrine glands
some organs have both functions, like the stomach and pancreas
major structures in the endocrine system
hypothalamus
pituatiary gland
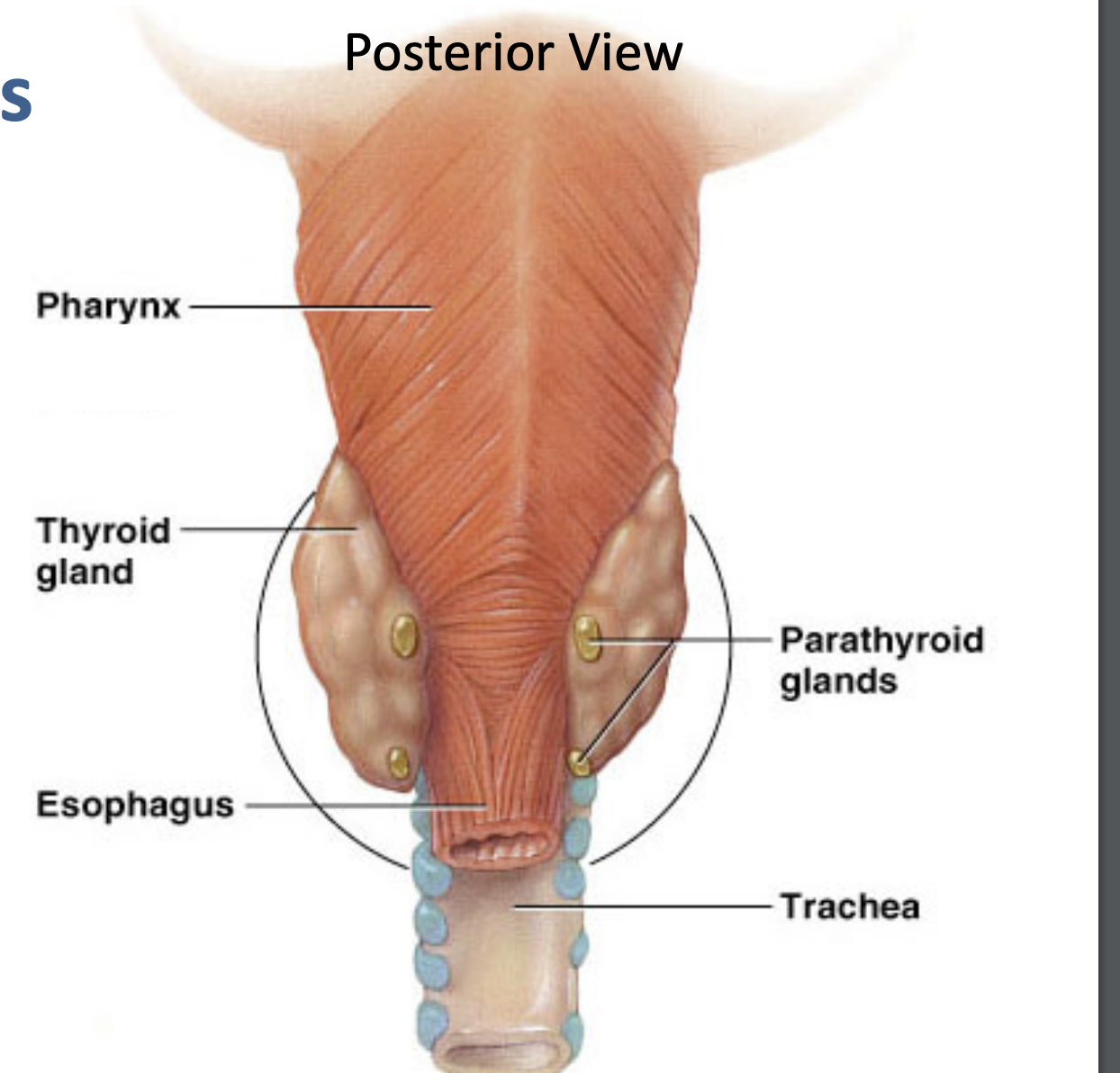
thyroid gland
parathyroid gland
thymus
adrenal glands
pancreas
pineal gland
3 main types of hormones
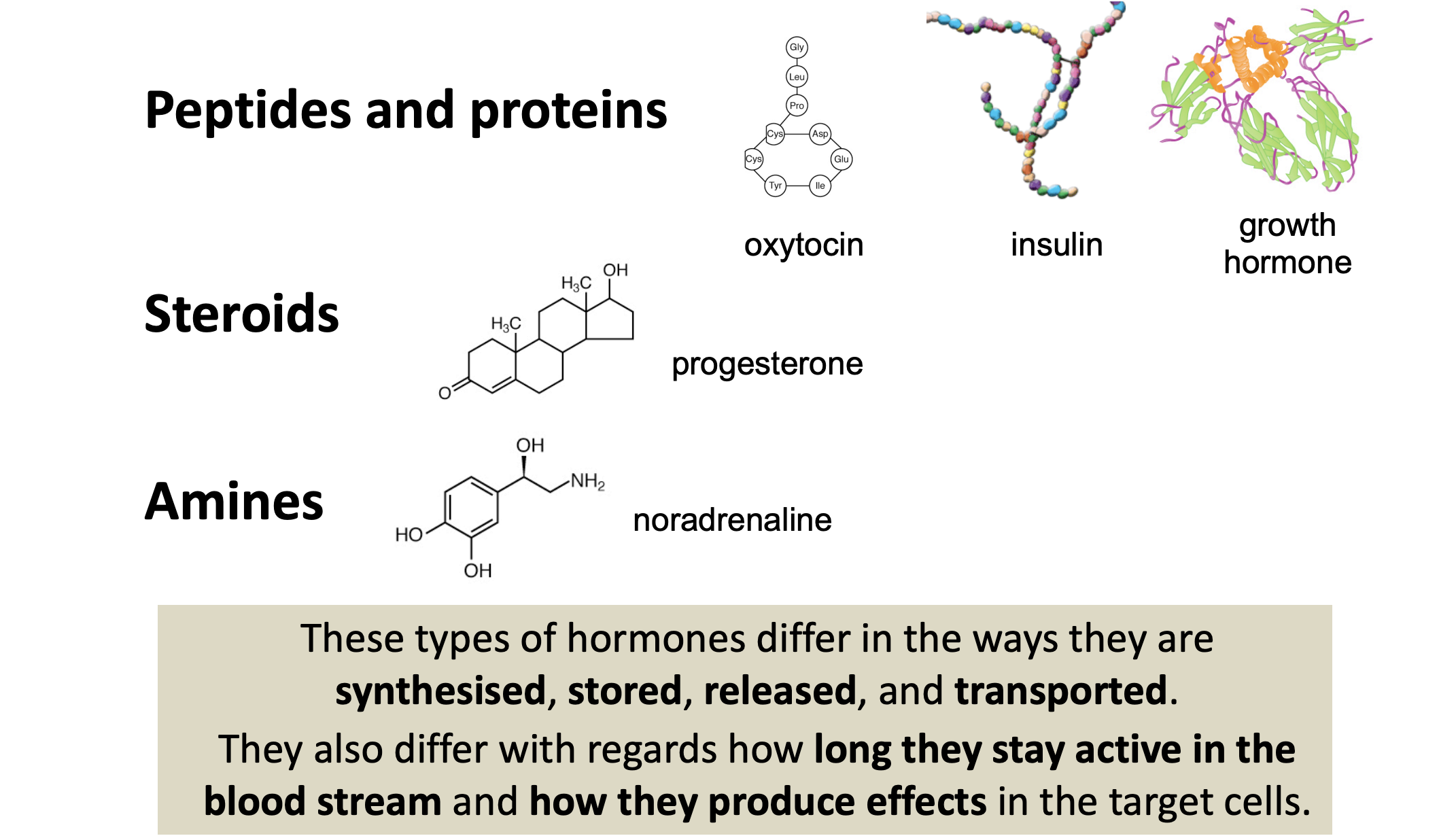
Steroids formed in smooth ER
Amines from amino acids
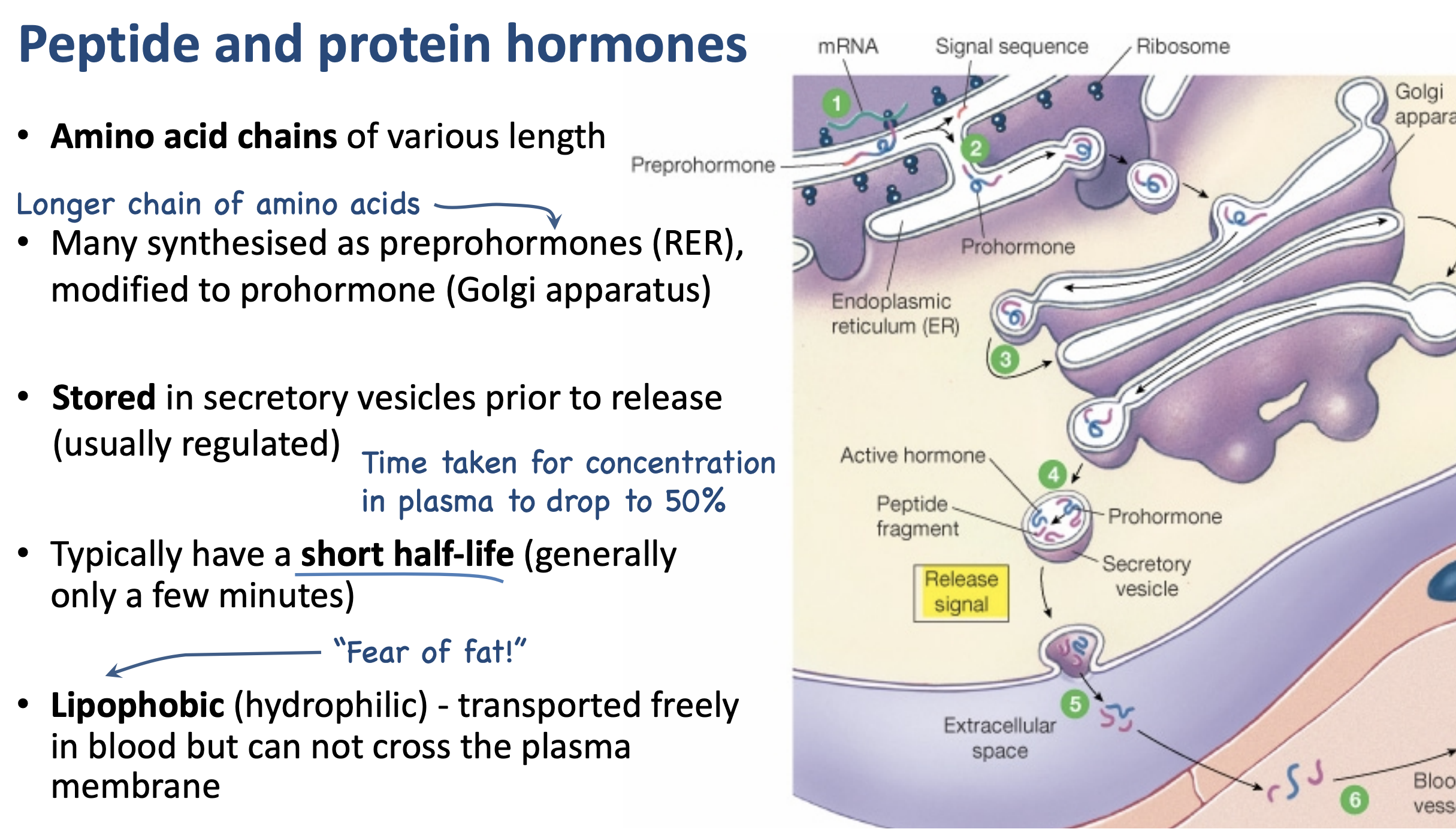
peptide and protein hormones
steroid hormones
All are derived from cholesterol
• Synthesised as needed in the smooth endoplasmic reticulum of gonads, adrenal glands and placenta.
• Largely bound to carrier proteins in the blood in order to TRAVEL (extends half-life)
• Lipophilic (FAT LOVING) - can cross the plasma membrane - receptors are in the cytoplasm or nucleus (mostly).
• Activate transcription of target genes - alters protein synthesis
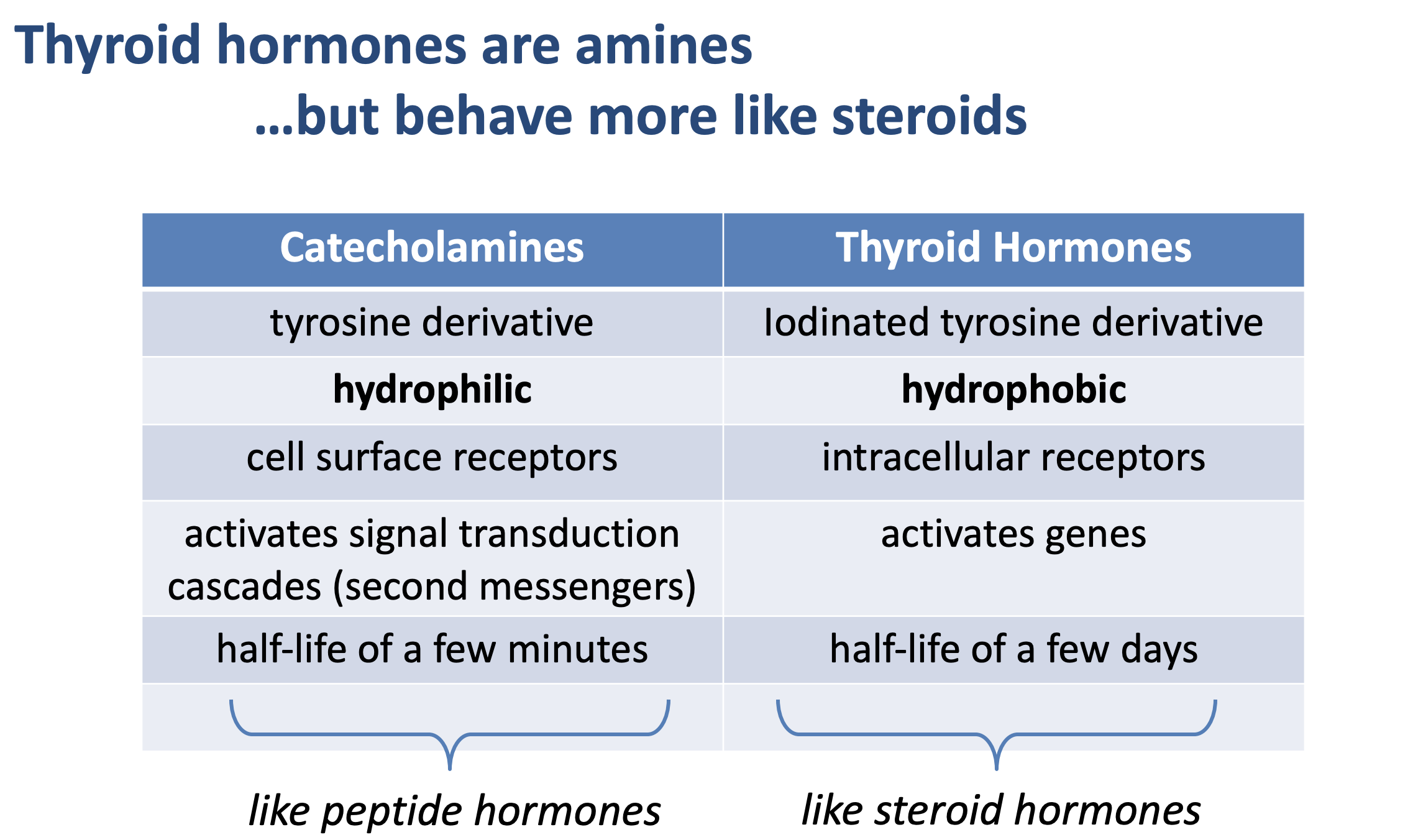
amine hormones
Amino acids with modified groups
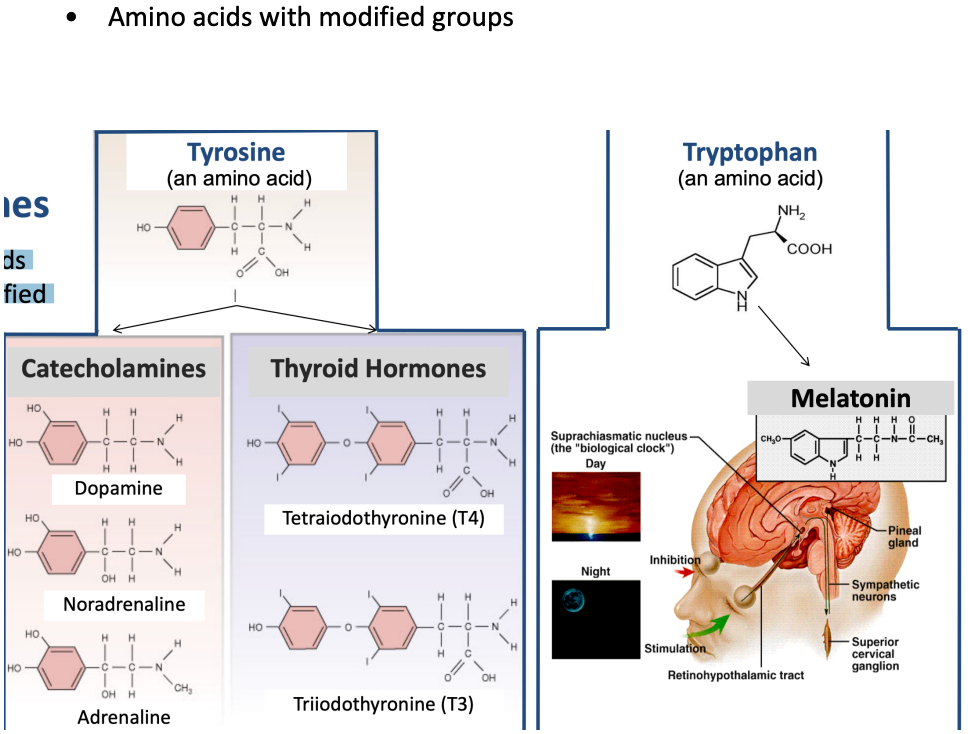
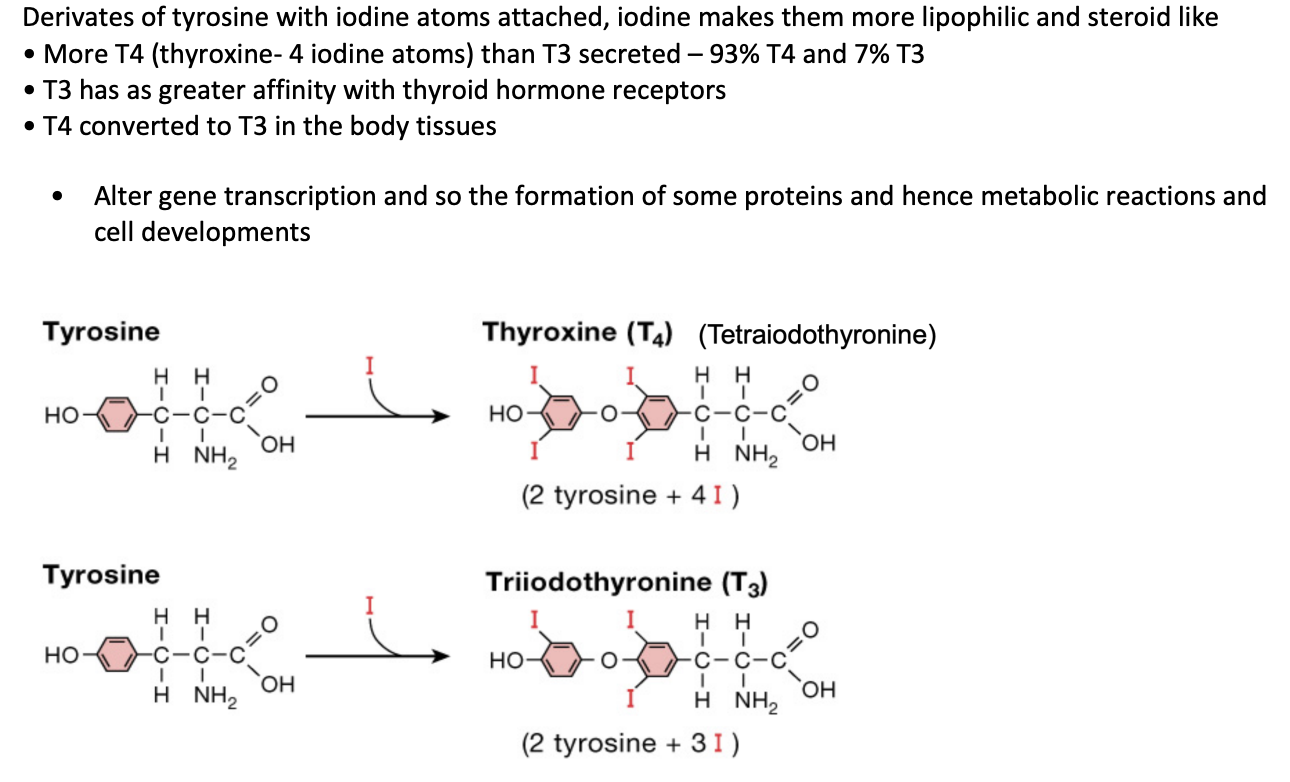
thyroid hormones properties
absoprtion times of hormones
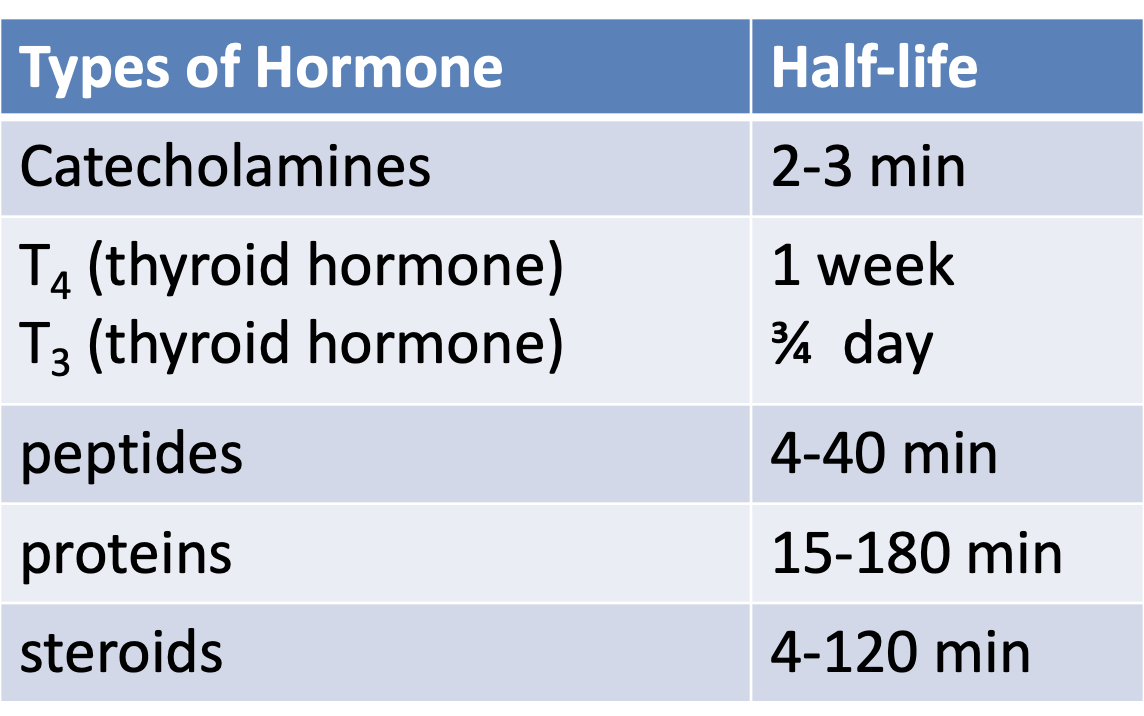
Onset can range from seconds to hours depending on pathways activated
Duration of the response can range from minutes to days.
Clearance is the removal of hormone from plasma (bulk cleared by liver and kidneys with only a small fraction actually removed by target tissue).
Half-life is the length of time it takes for the hormone concentration to drop by half. This can range from seconds to days.
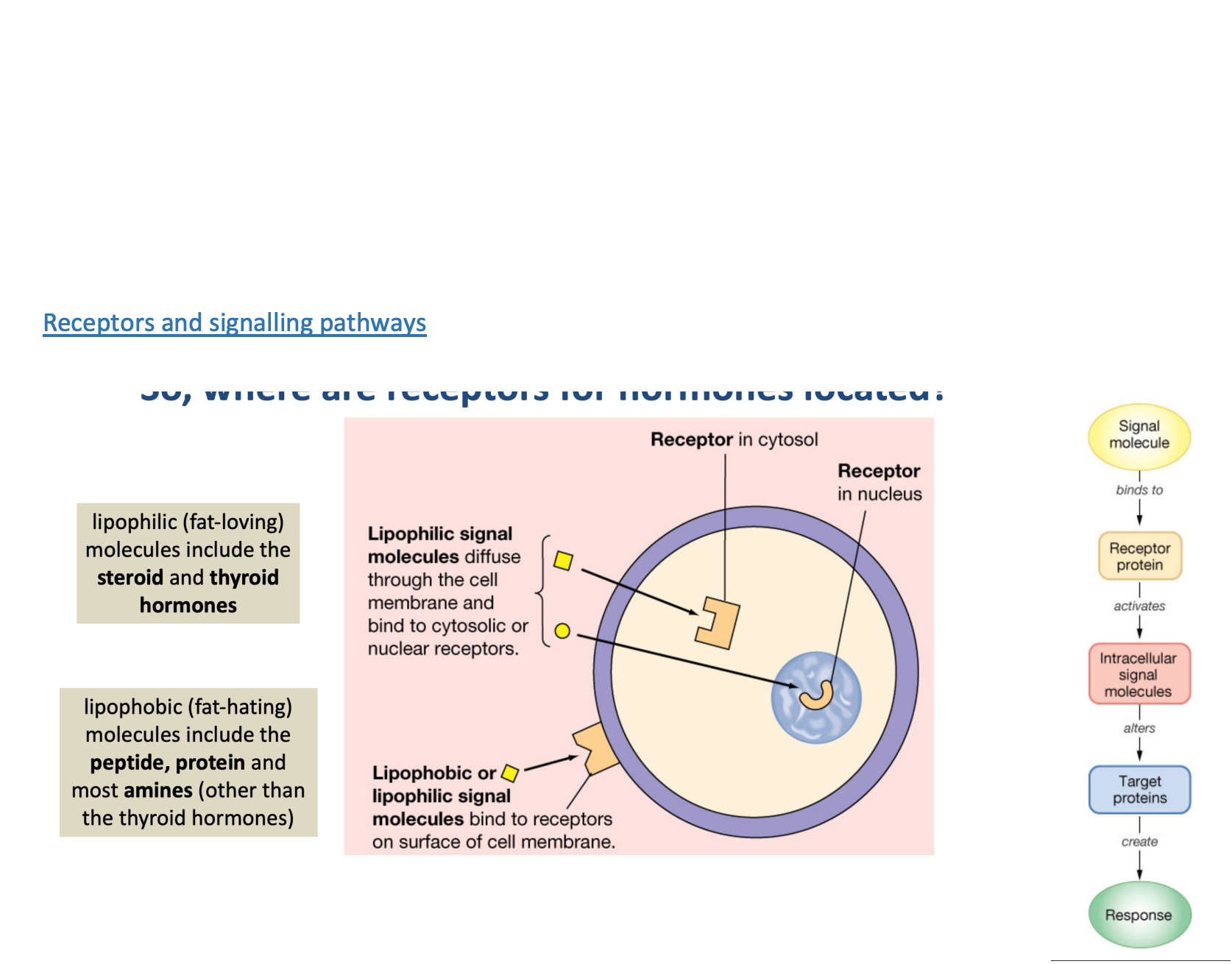
receptors and signalling pathways
different for lipophilic and lipophobic
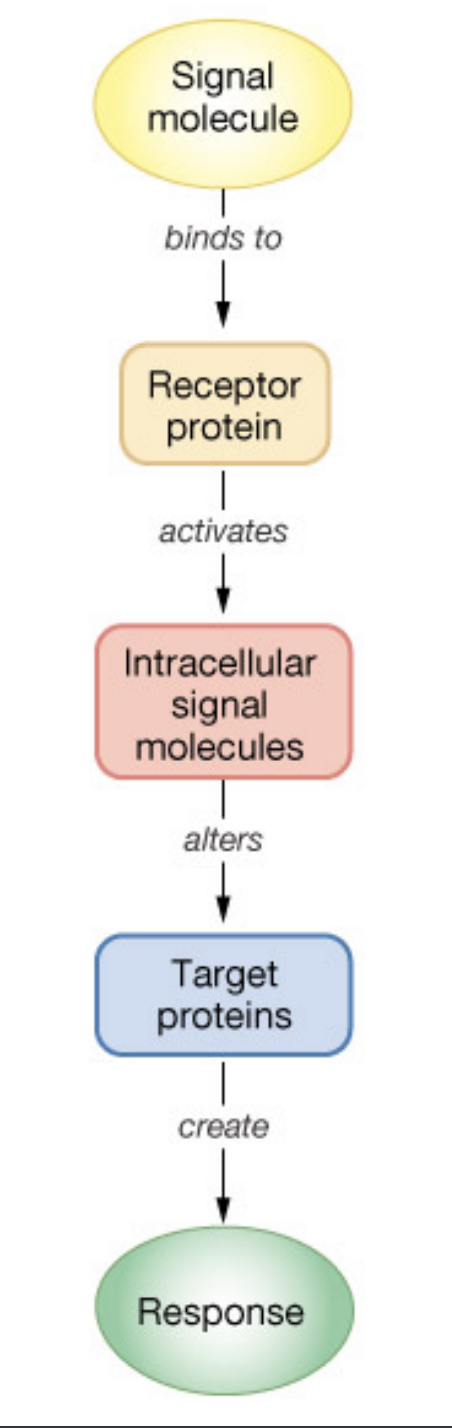
types of cell surface receptors
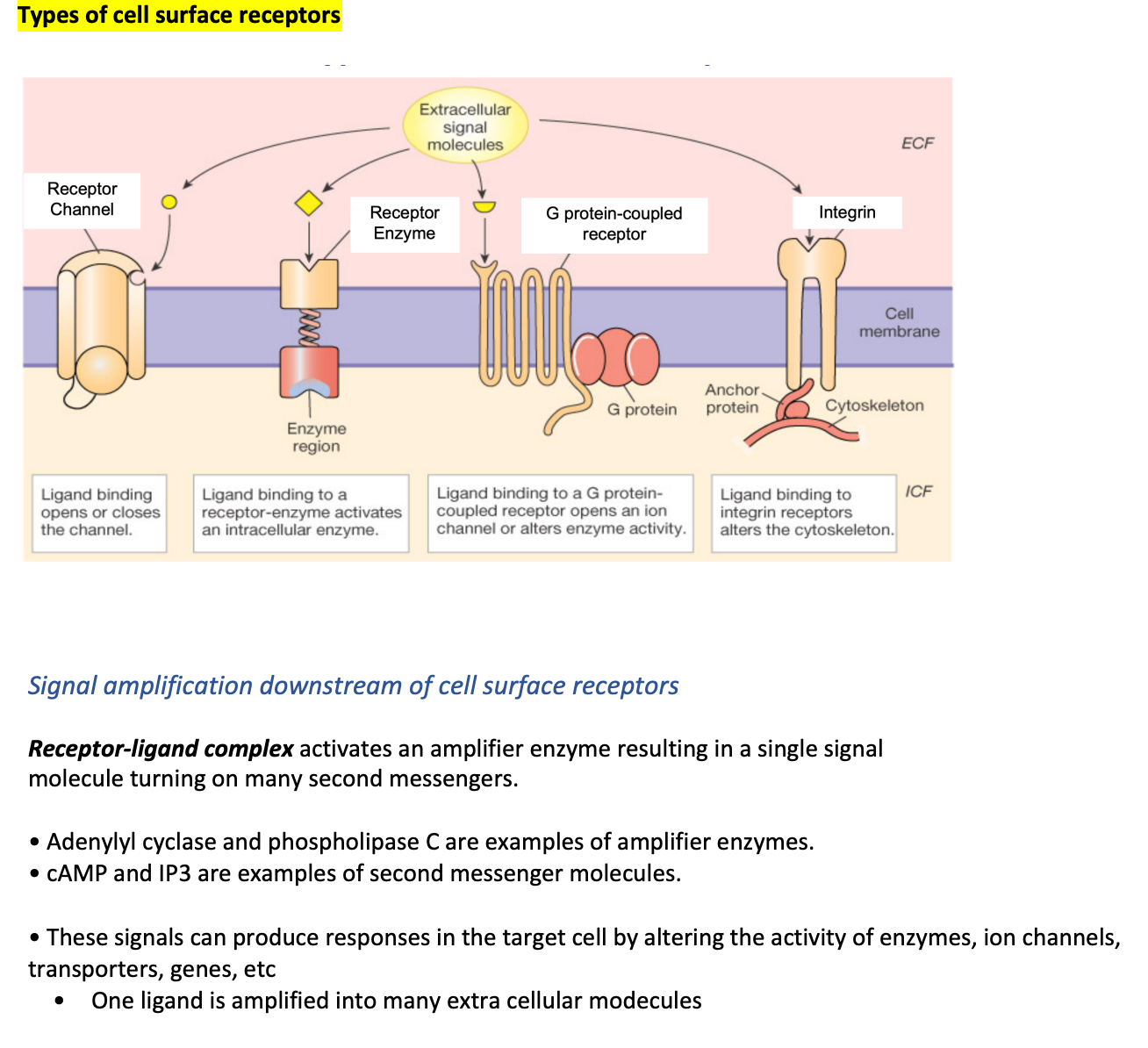
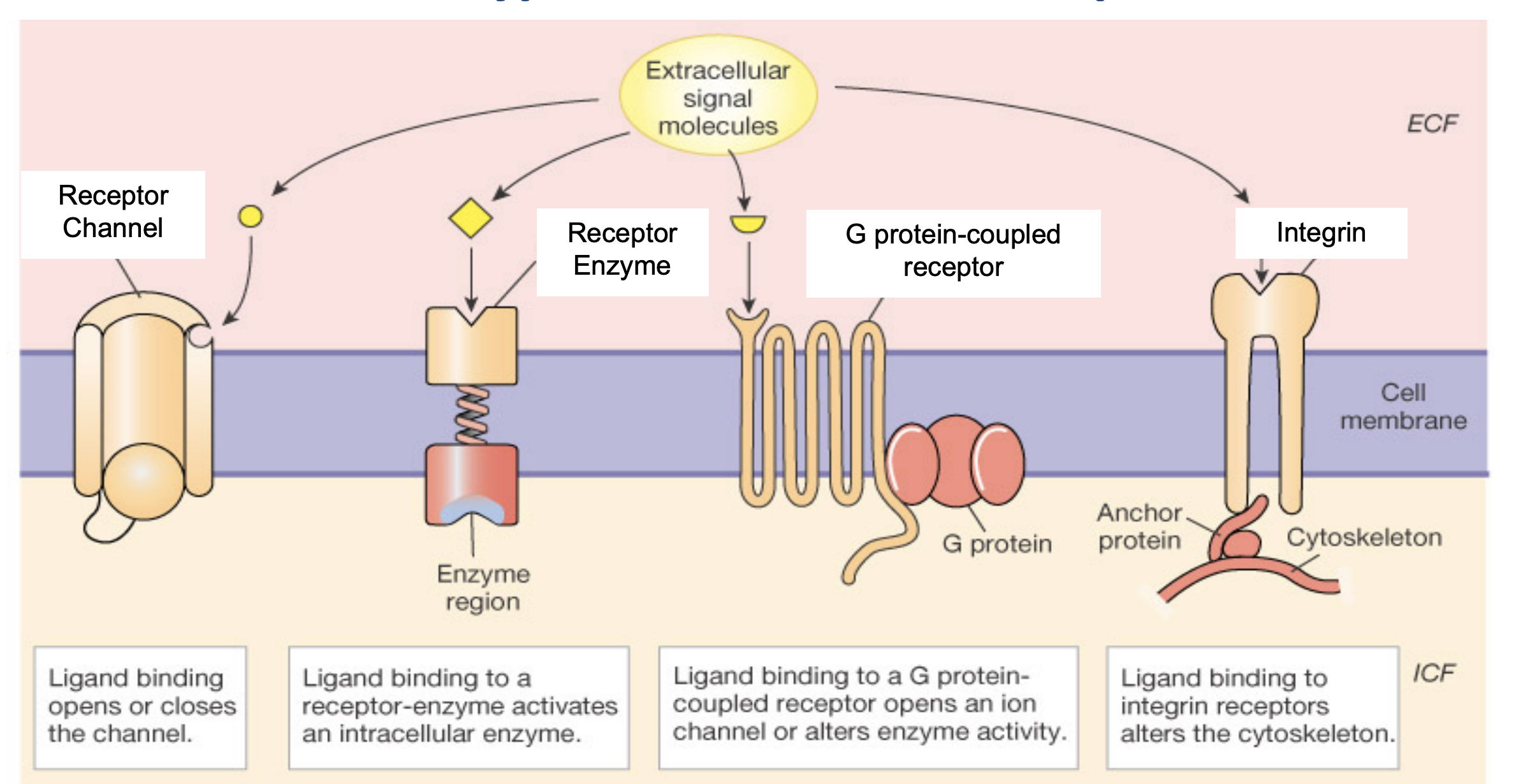
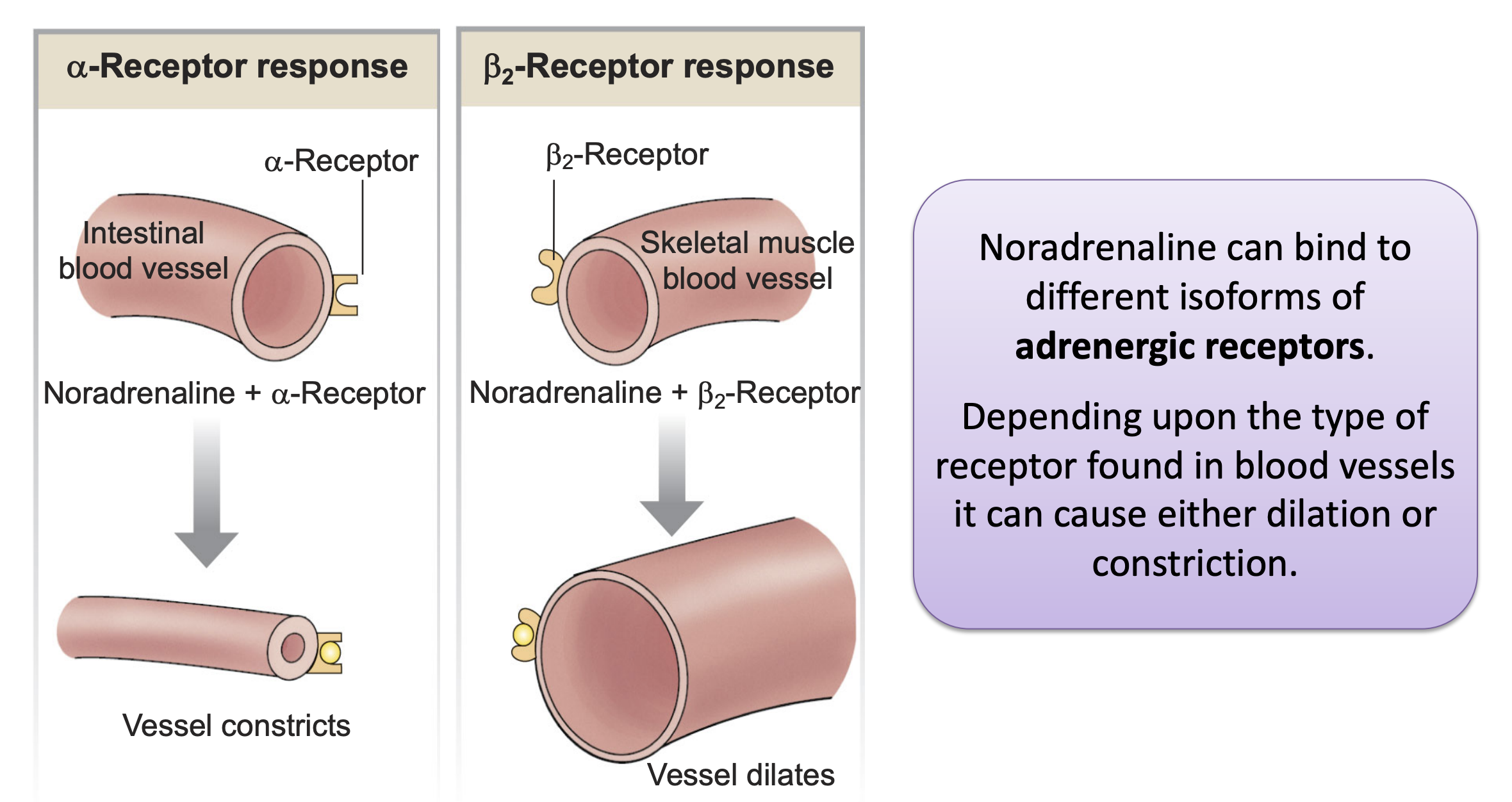
response based on receptor type
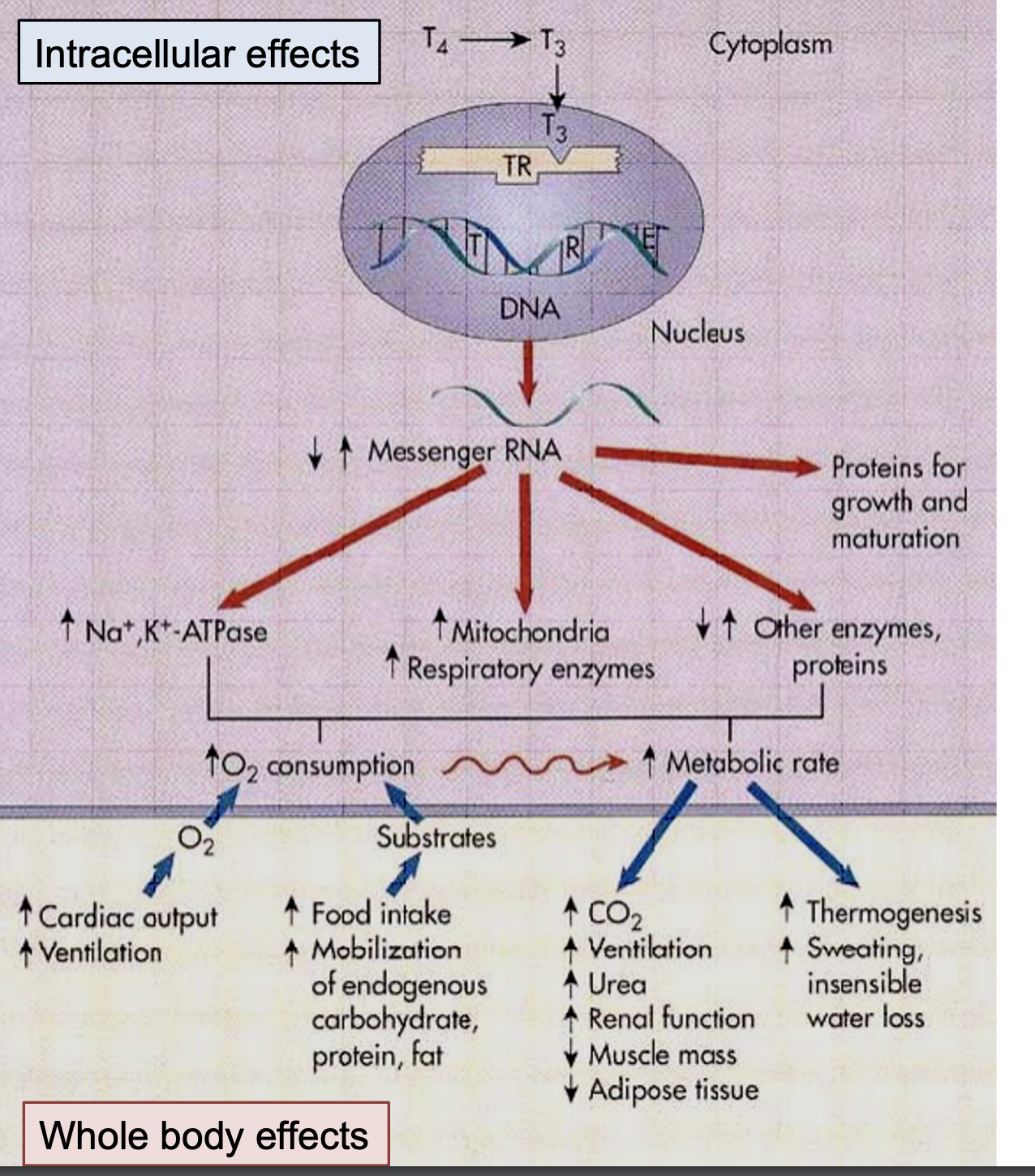
Lipophilic hormones (steroid and thyroid hormones) act primarily on intracellular receptors
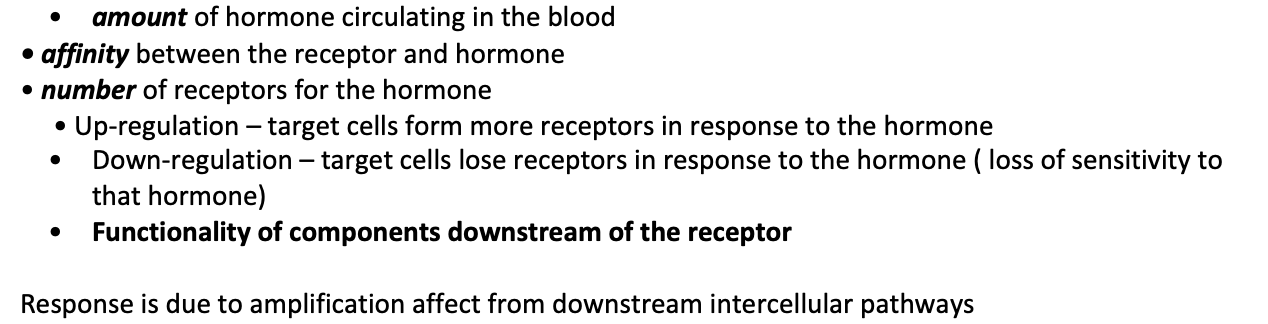
What determines how big the response elicited by the hormone will be?
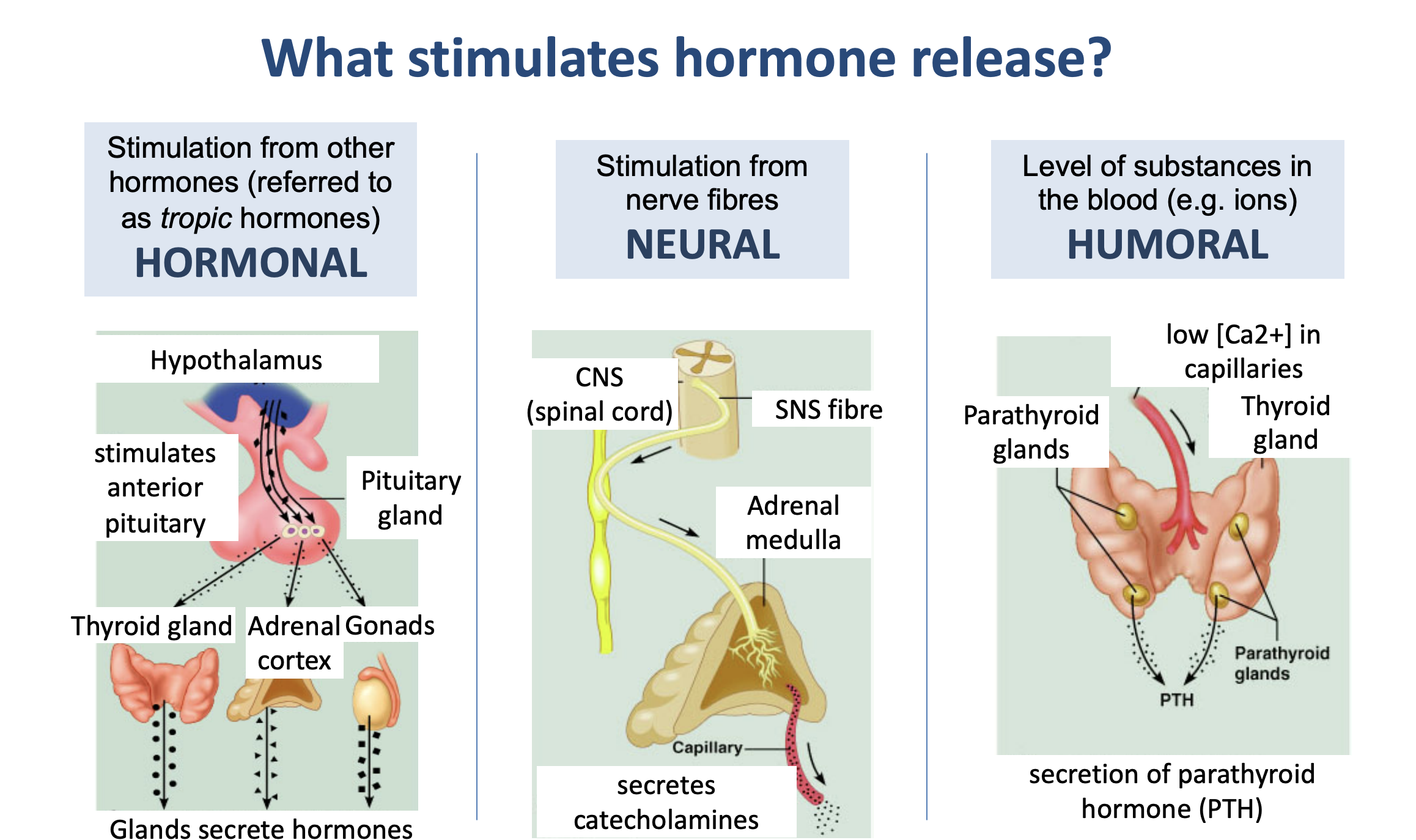
what stimulates hormone release
hormonal
neural
humoral
different patters of hormone secretion
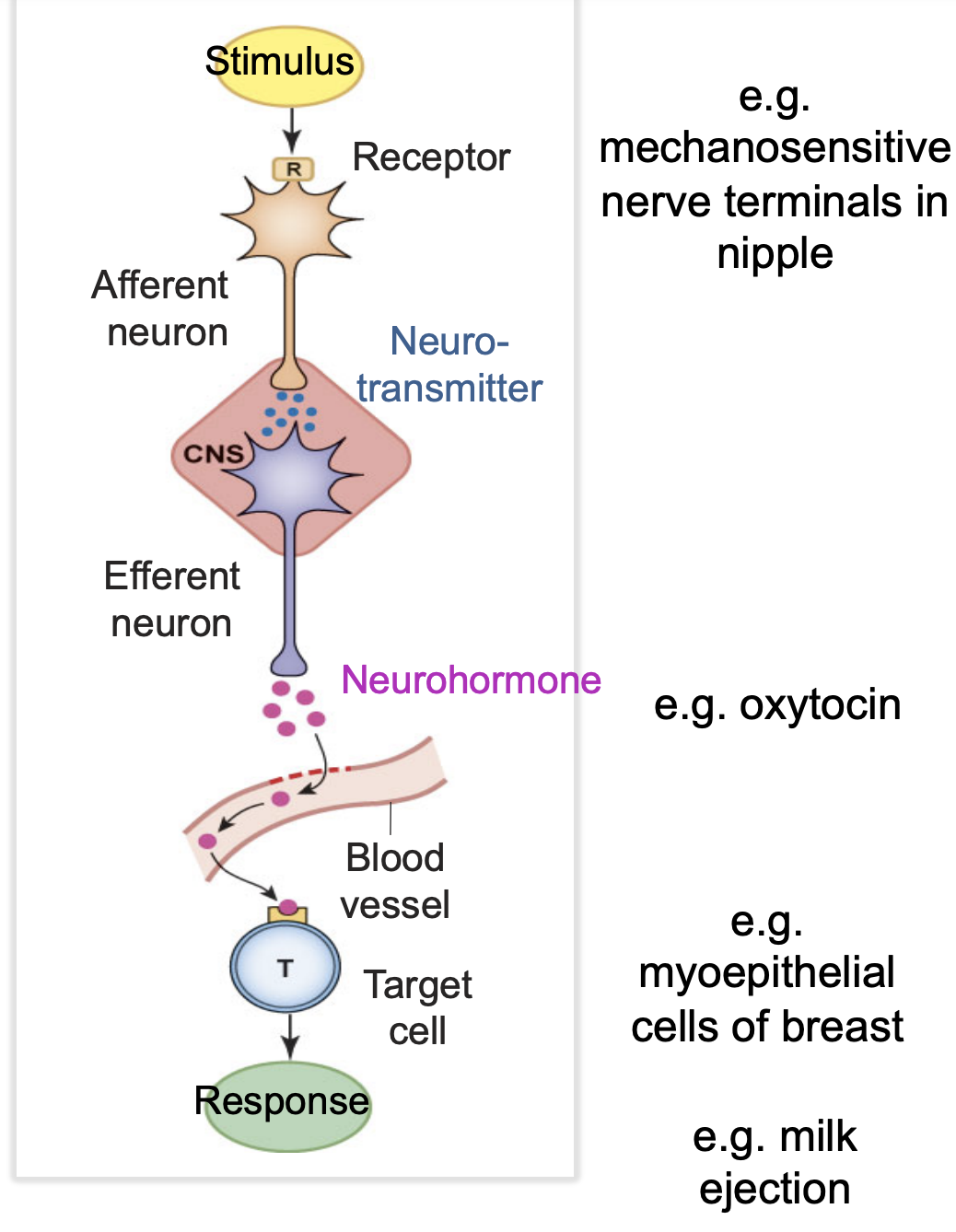
example of a neuroendocrine pathway
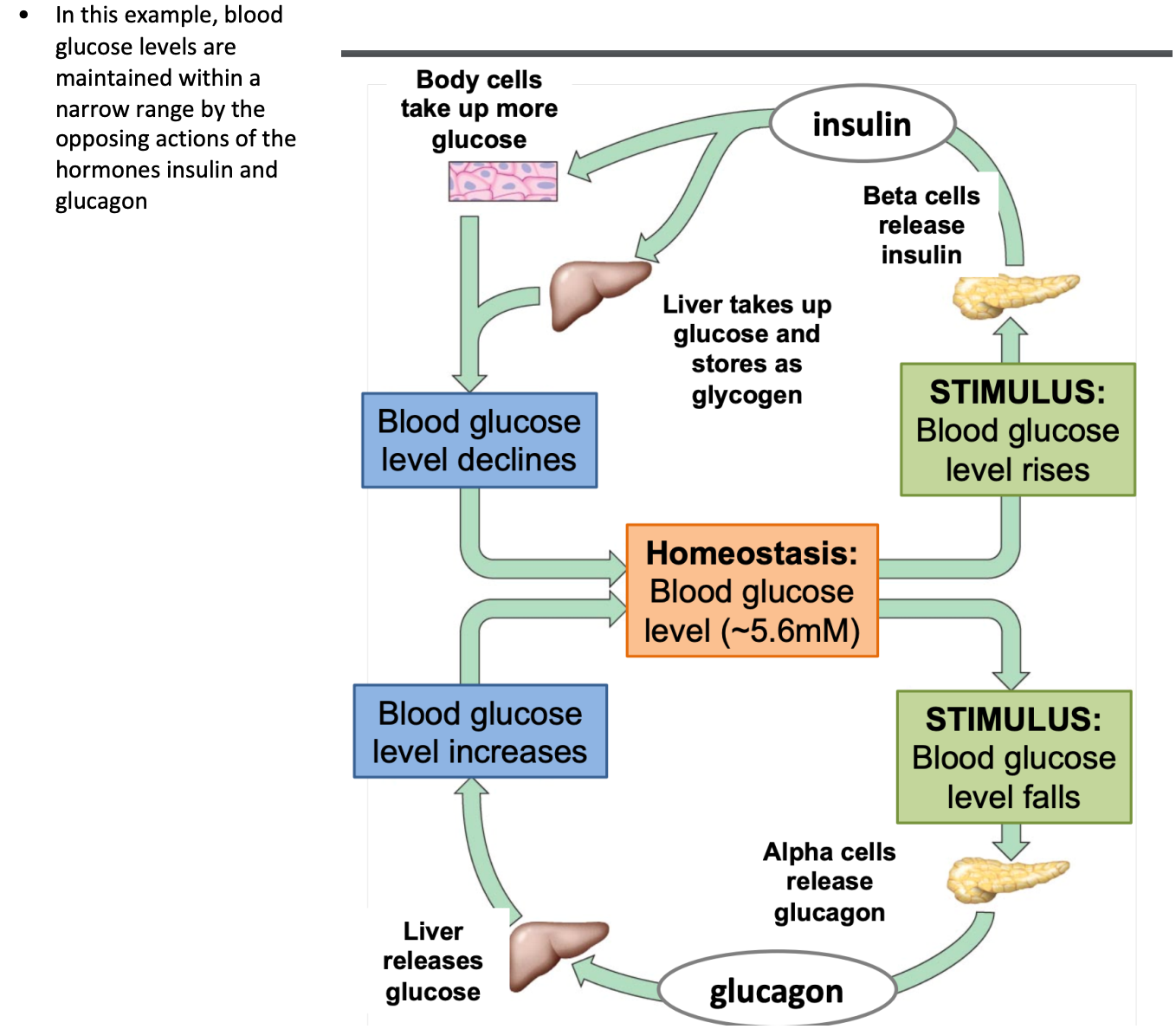
regulating hormone secretion with feedback
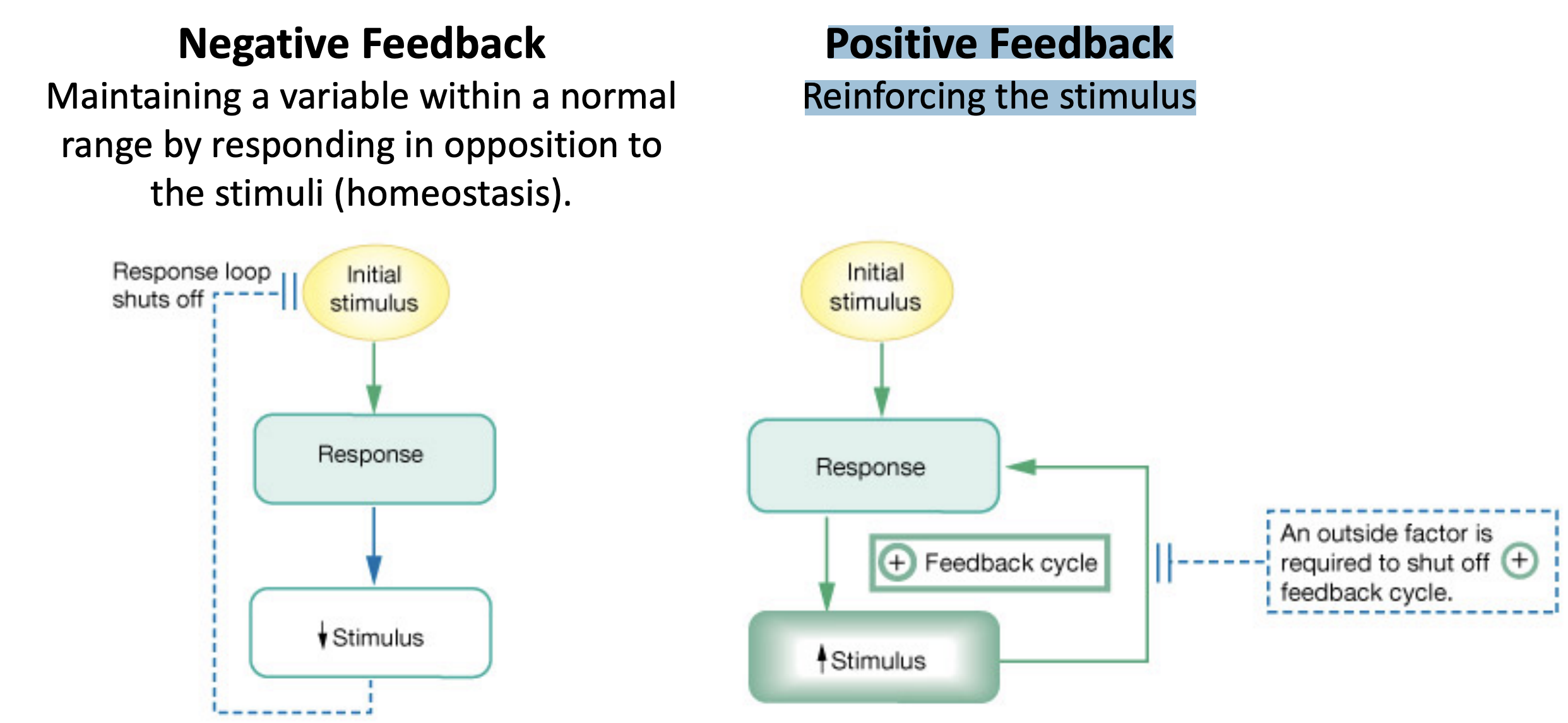
how negative feedback works
factors that influence levels of hormones in plasma
Rate of secretion (regulated - most important)
Rate of binding to carrier proteins
Rate of metabolism (activation/degradation)


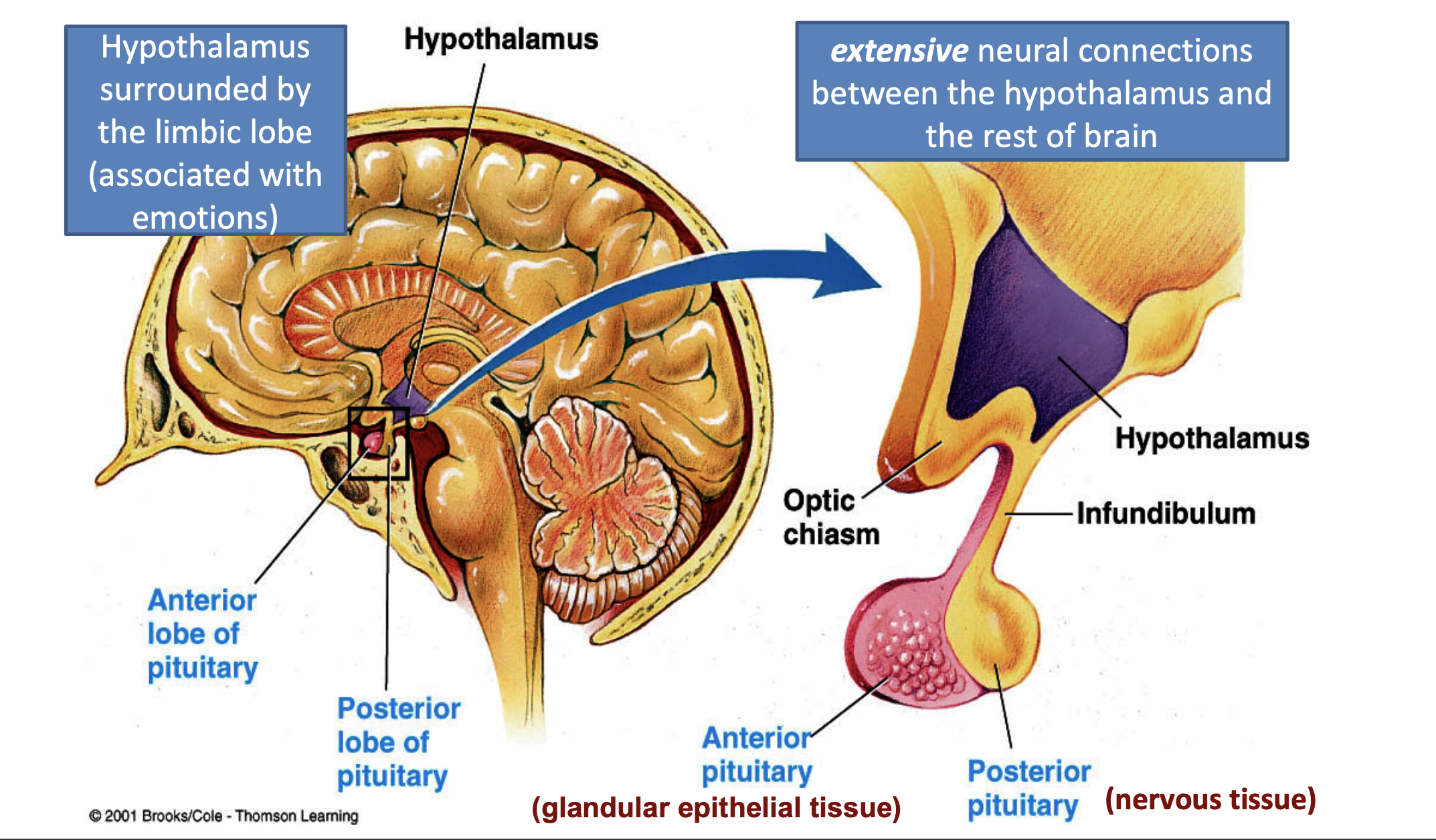
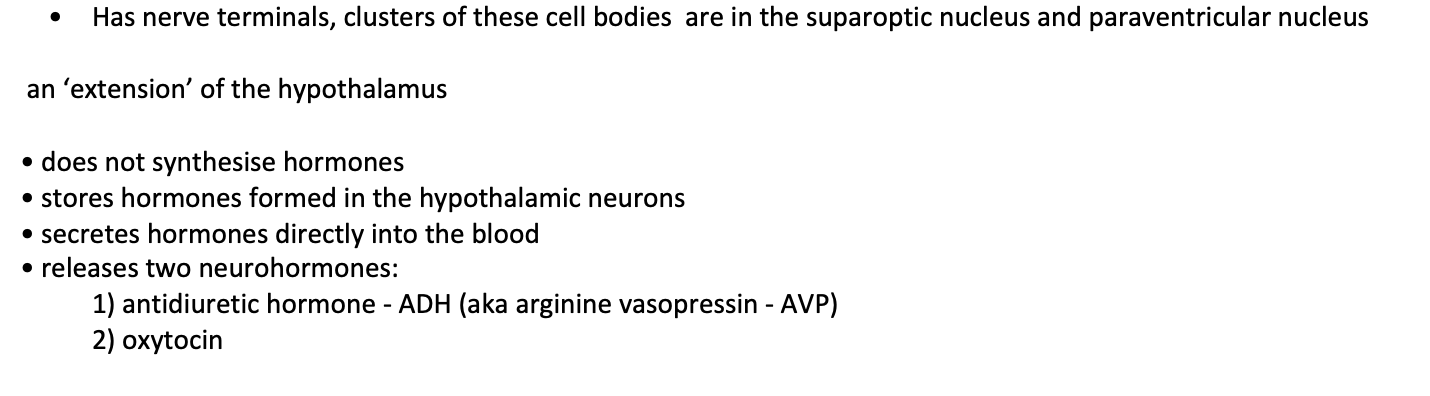
Posterior Pituitary (Neurohypophysis)
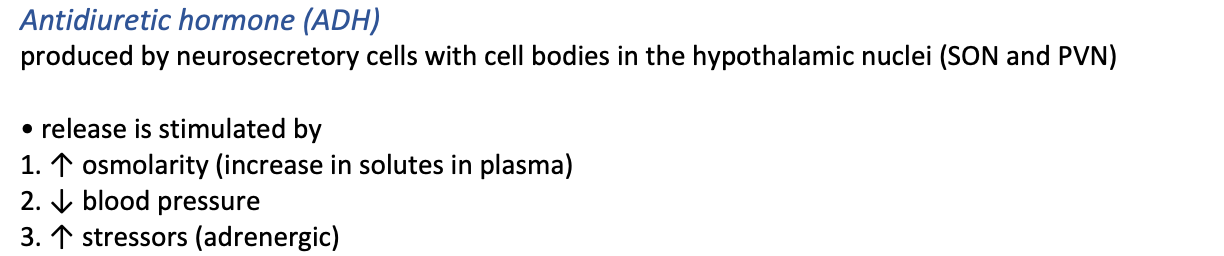
how the posterior pituitary works
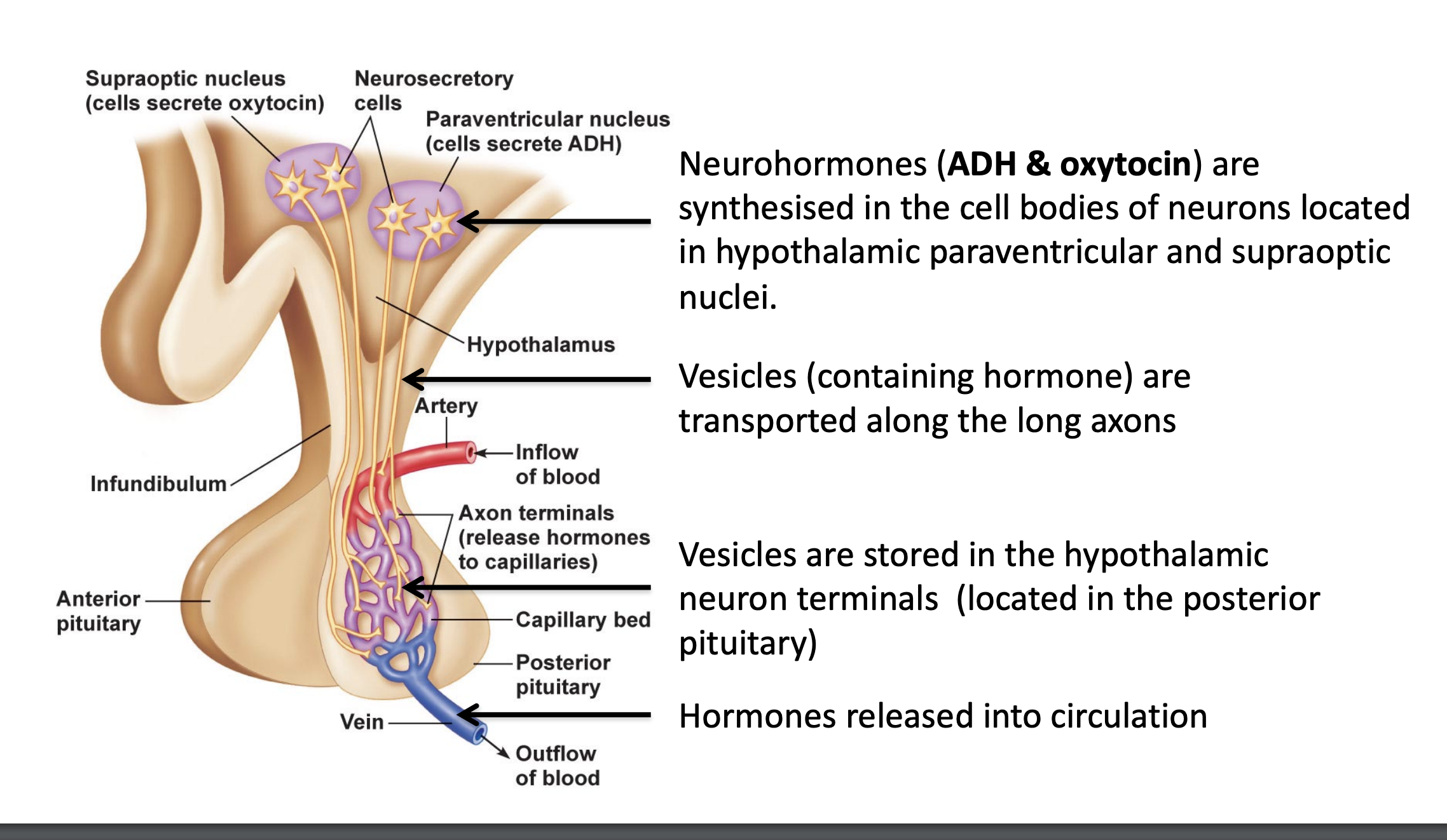

Made up of glandular epithelial cells
Short axon neurons synthesise hypophysiotropic hormones and release them into capillaries of the hypothalamic-hypophyseal portal system.

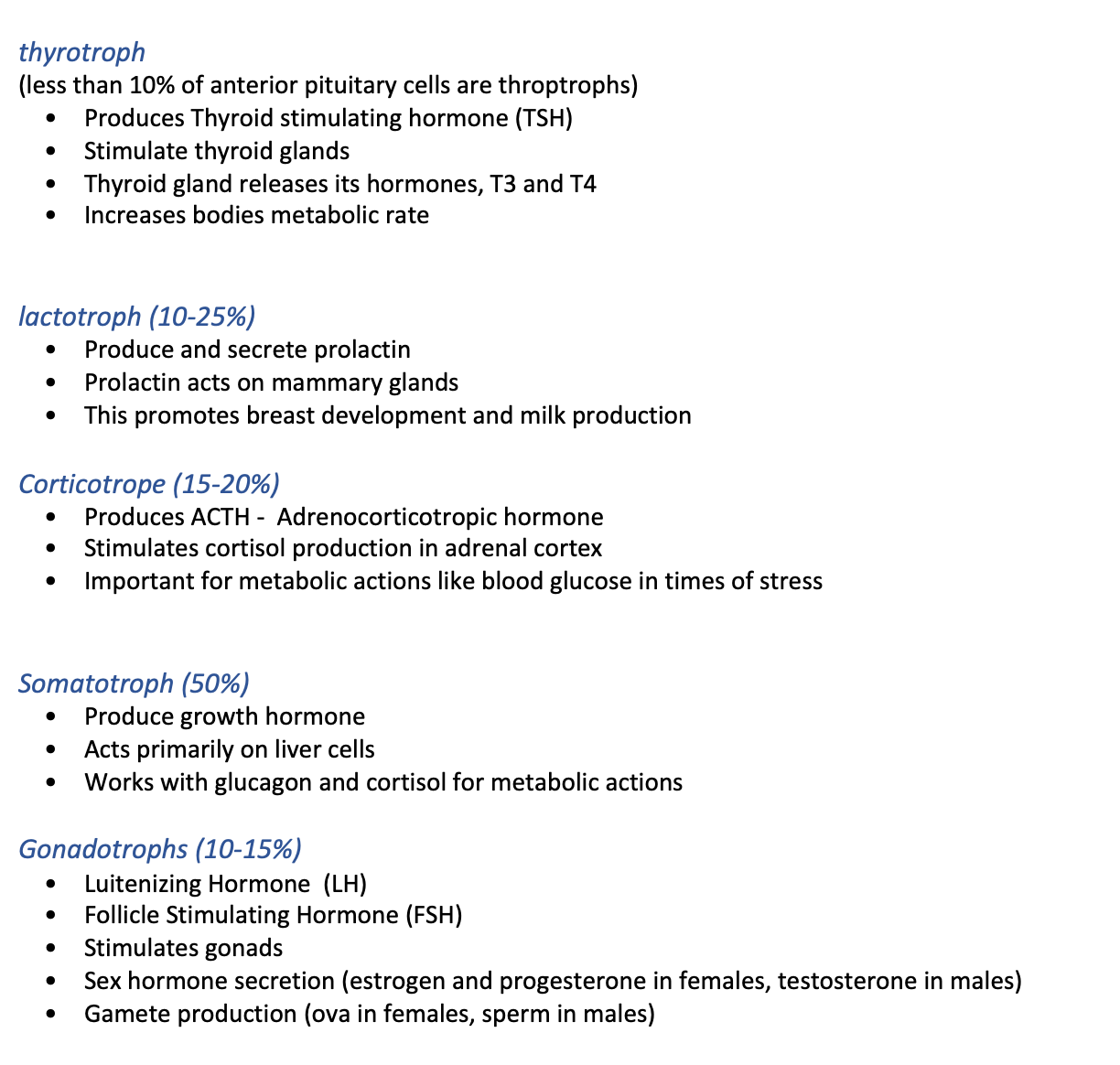
Hypothalamic – pituitary – adrenal axis (HPA axis)
Stressors (internal/external) trigger the release of cortisol.
This involves the release of intermediary hormones from the hypothalamus (CRH:
corticotropin releasing hormone) and the
anterior pituitary (ACTH: adrenocorticotropic hormone).
Release is regulated via negative feedback.
thyroid gland
Endocrine gland regulated by the hypothalamus and anterior pituatiary
Located immediately below the larynx on each side of and anterior to the trachea (BOWTIE)
The two lobes are joined by the Isthmus
• Normally weighs 15-20g in adults
thyroid gland hormones
intracellular and whole body affects of thyroid hormones
thyroid follicles
the functional unit of the thyroid
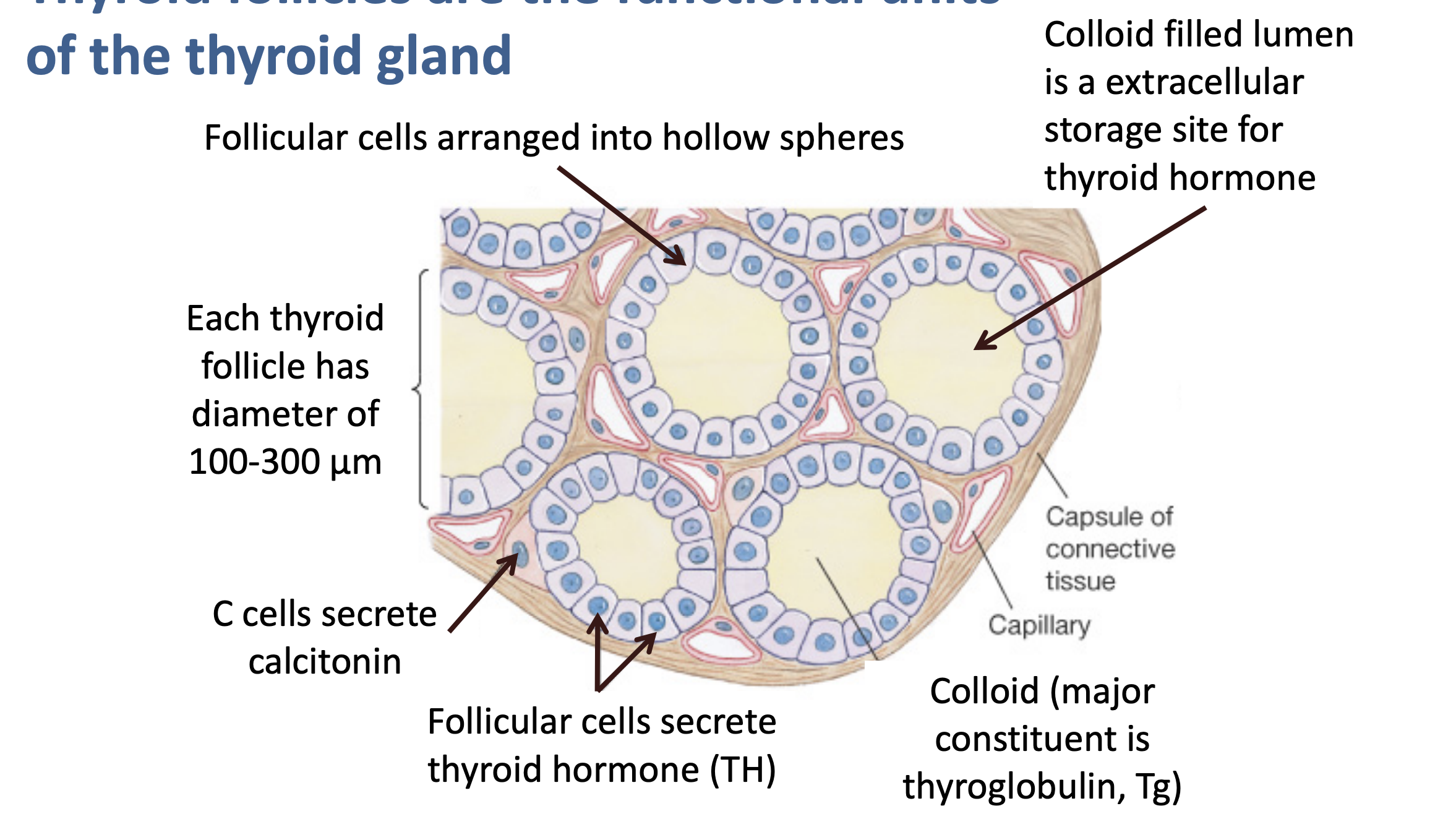
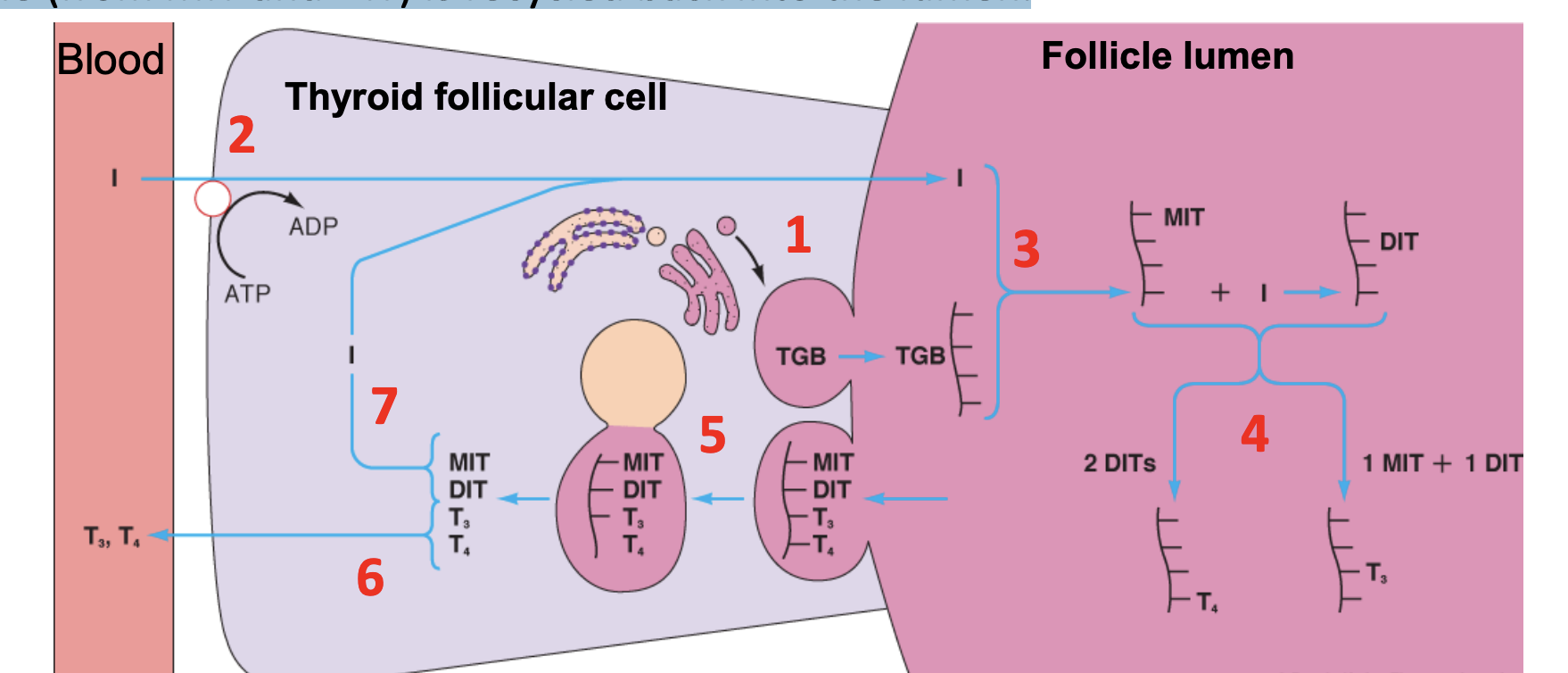
thyroid hormone synthesis = T3 and T4
Thyroglobulin (large protein) synthesised in follicular cell and exocytosed into the lumen ( as the vesicles in colloid are released)
2. Iodide pump actively pumps iodine into follicular cell
3. Iodine is attached to tyrosine residues on thyroglobulin molecules in follicle lumen
4. Iodinated residues couple to form T3 and T4
5. Thyrogobulin is endocytosed and vesicles fuse with lysosomes
6. Enzymes cleave T3 and T4 which then diffuse into the bloodstream.
7. Iodine (from MIT and DIT) is recycled back into the lumen.
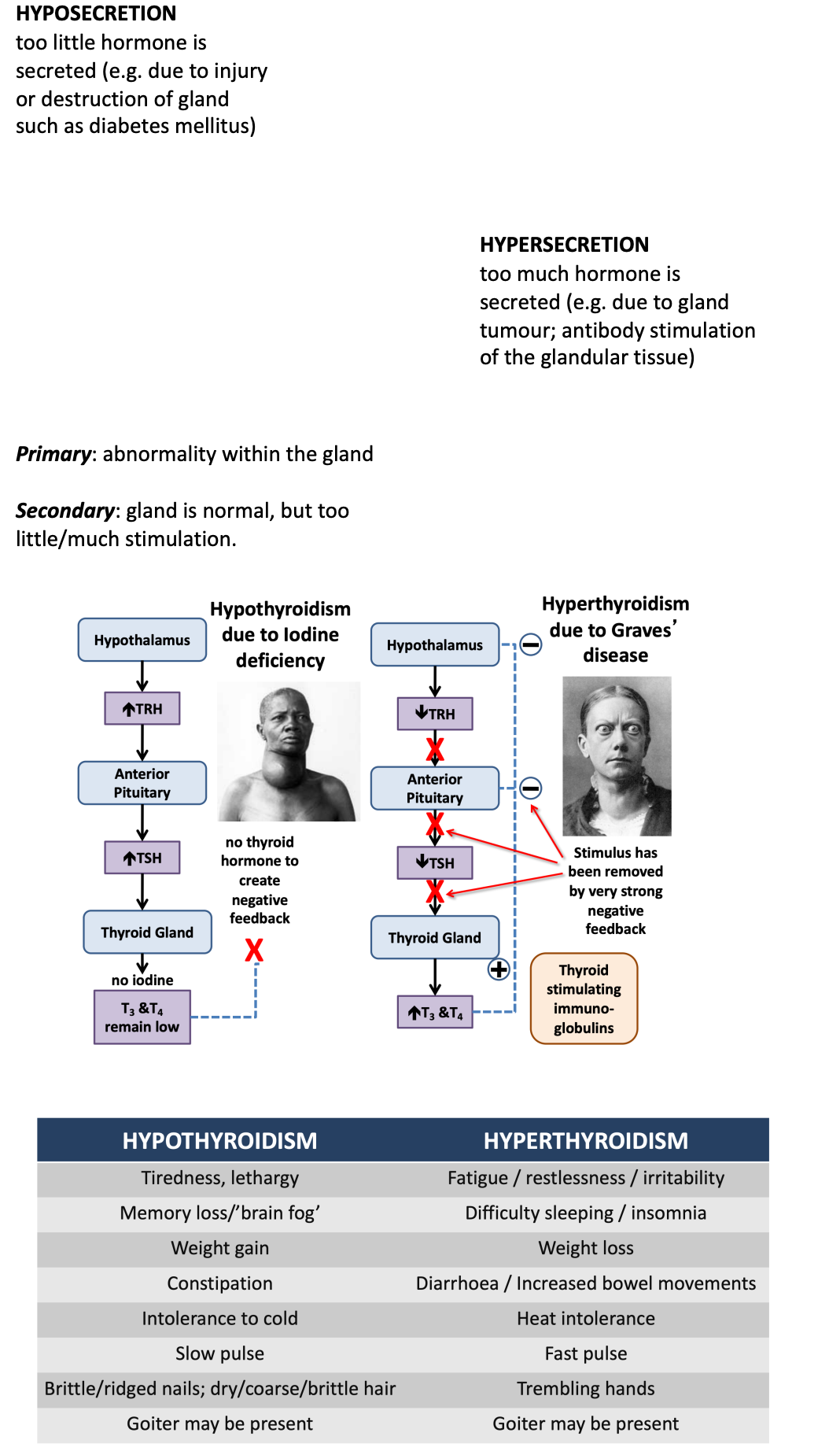
regulation of thyroid hormone secretion
thyrotropin-releasing hormone (TRH) stimulates release of thyroidstimulating hormone (TSH)
• Negative feedback maintains relatively constant supply of thyroid hormones
In tissues T4 may be converted to T3 as it is more bio-available
T3 and T4 both act on thyroid hormone receptors but T3 has more reactivity
endocrine dysfunction
3 main functions of male reproductive system
Production of sperm cells in the testes: Sperm cells in males and oocytes (eggs) in females are referred to as gametes.
Sustaining and transfer of sperm cells to the female: The ducts and glands in the male reproductive system provide nutrients for the sperm cells produced in the testes, and transport the sperm from the testes through the penis, which is a specialised organ that deposits sperm into the female reproductive system.
Production of male sex hormones: Hormones produced by the male reproductive system control the development of the reproductive system itself and of the male body form. These hormones (including testosterone) are essential for the normal function of the reproductive system and reproductive behaviour.
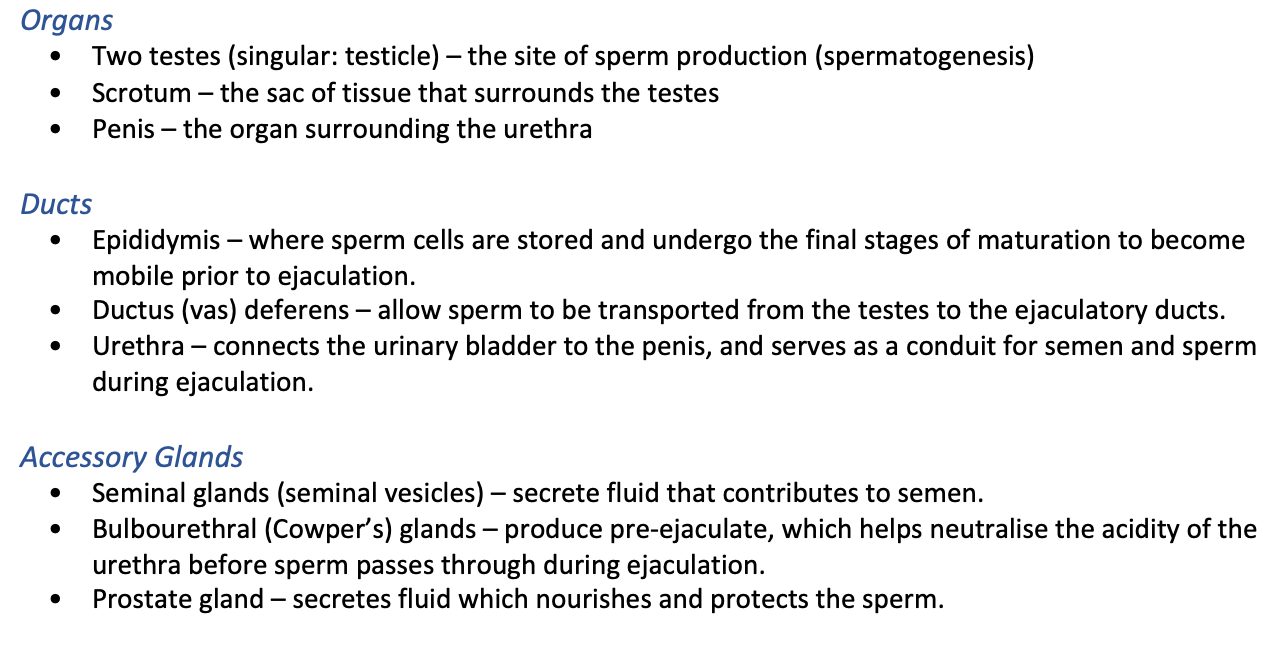
Functional categories of MALE reproductive structures
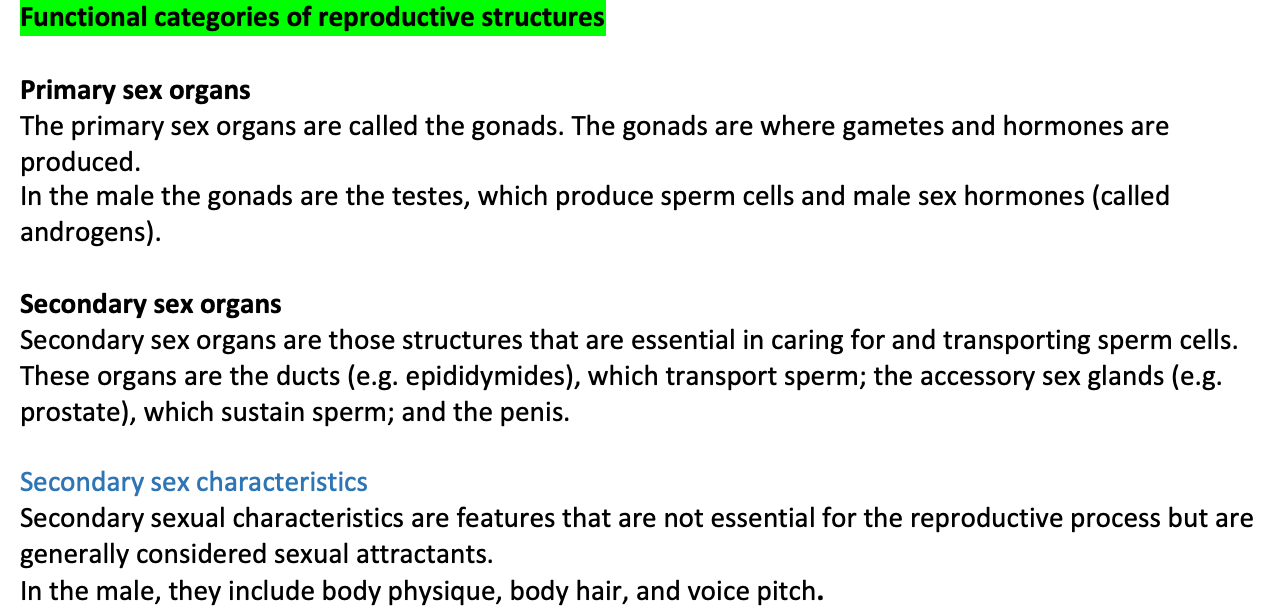
Secondary sexual characteristics are features that are not essential for the reproductive process but are generally considered sexual attractants. In the male, they include body physique, body hair, and voice pitch.
parts of male reproductive system
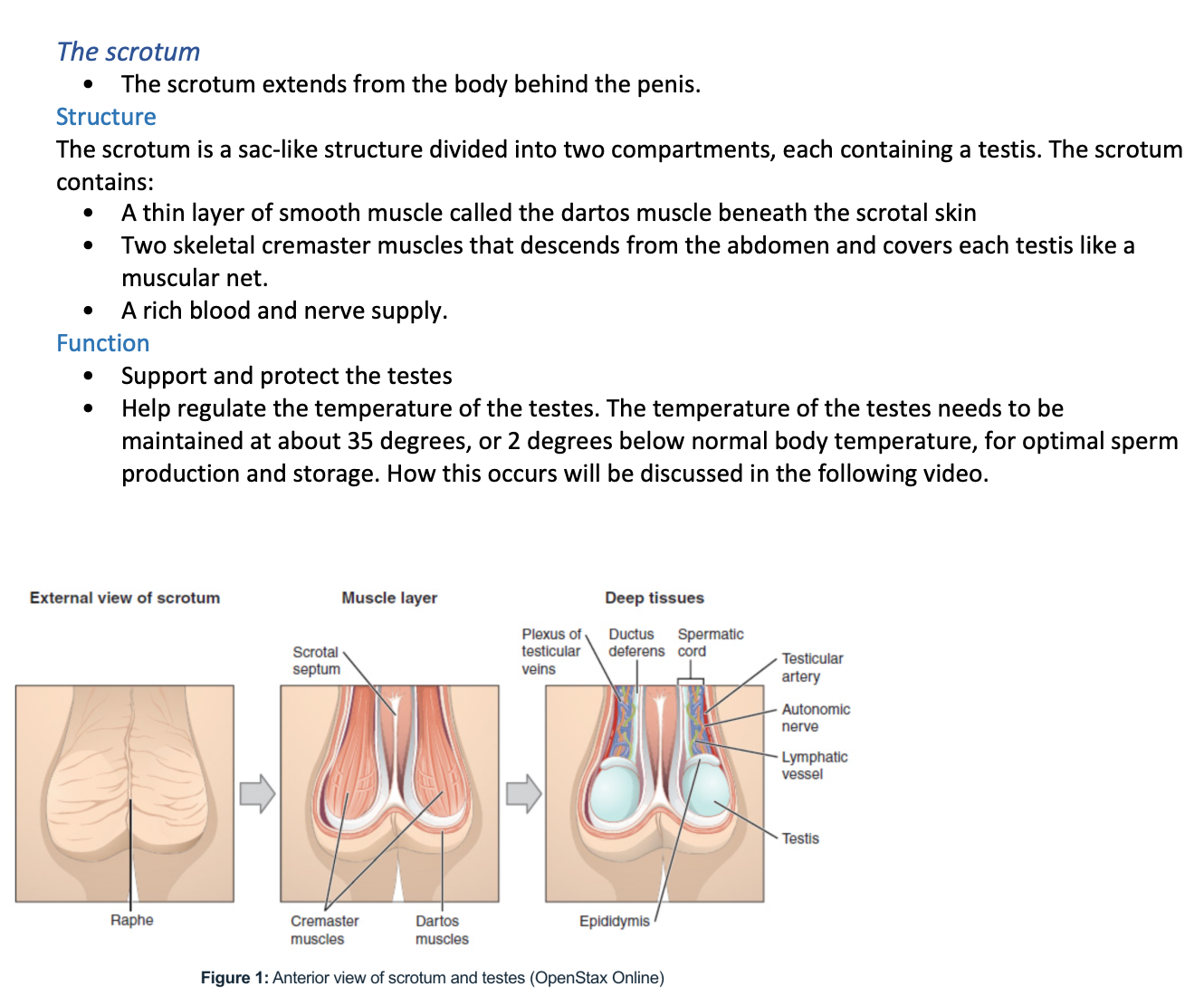
the scrotum
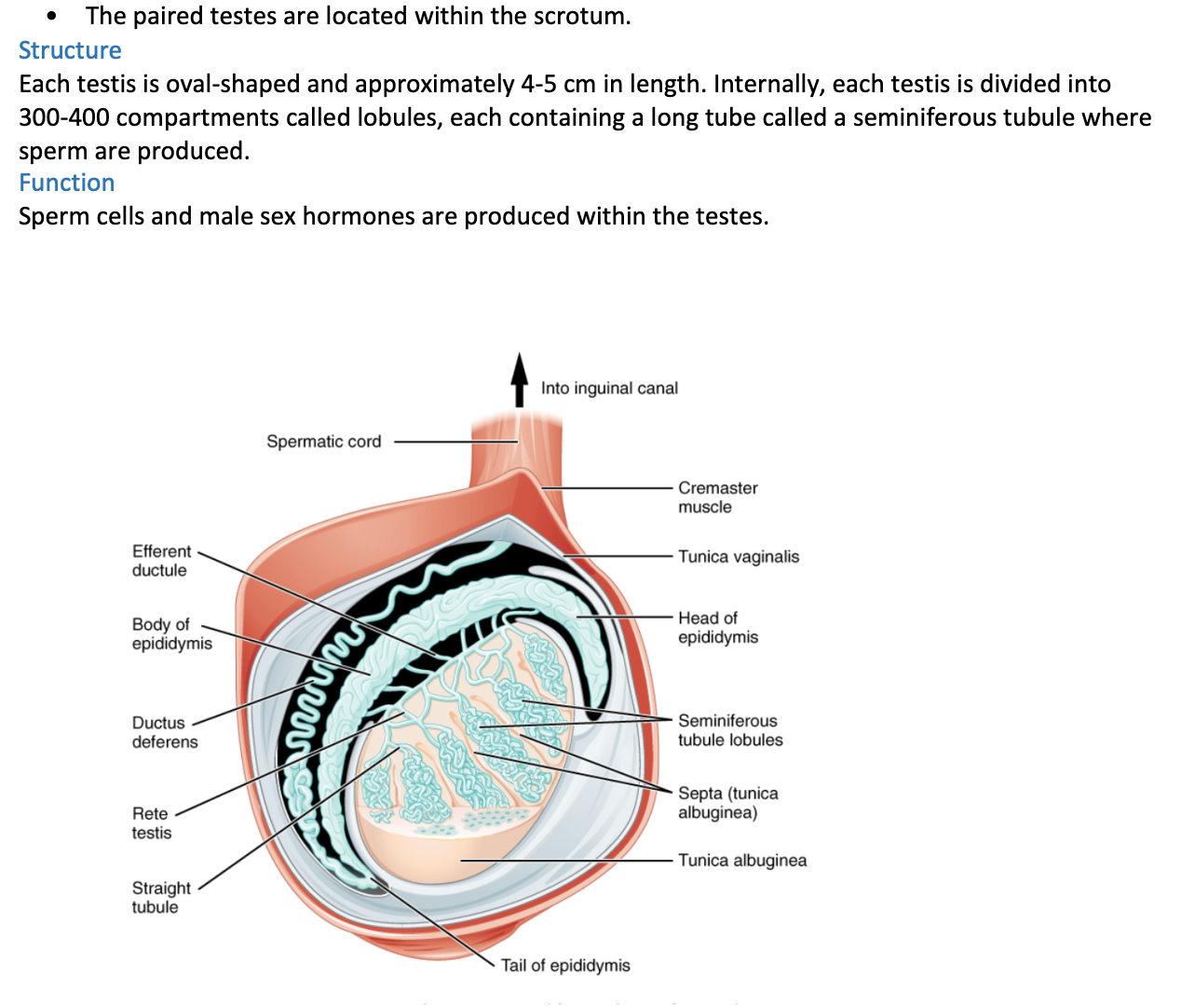
the testes
importance of thermoregulation of the testes
how thermoregulation is maintaned
How Testes Temperature is maintained
Located outside body within scrotum
Copious temperature receptors and sweat glands in scrotal skin
Cremaster muscle
Skeletal muscle that is under the dermis, Descends from abdomen through spermatid cord
Cold: contract to lift testes closer to warm pelvis
Hot: relax to drop testes away from warm pelvis
3. Dartos muscle
Smooth muscle
Within dermis
Resting muscle tone of dartos causes characteristic wrinkling of scrotal surface
Cold: contracts (increased wrinkling) to reduce surface area for heat loss
Hot: expands (reduced wrinkling) to increase surface area and promote heat loss
Counter-Current Heat Exchange
Network of testicular veins (pampiniform plexus) wrap around around testicular artery
Exchange of heat from artery to vein - material blood cooled; venous blood warmed

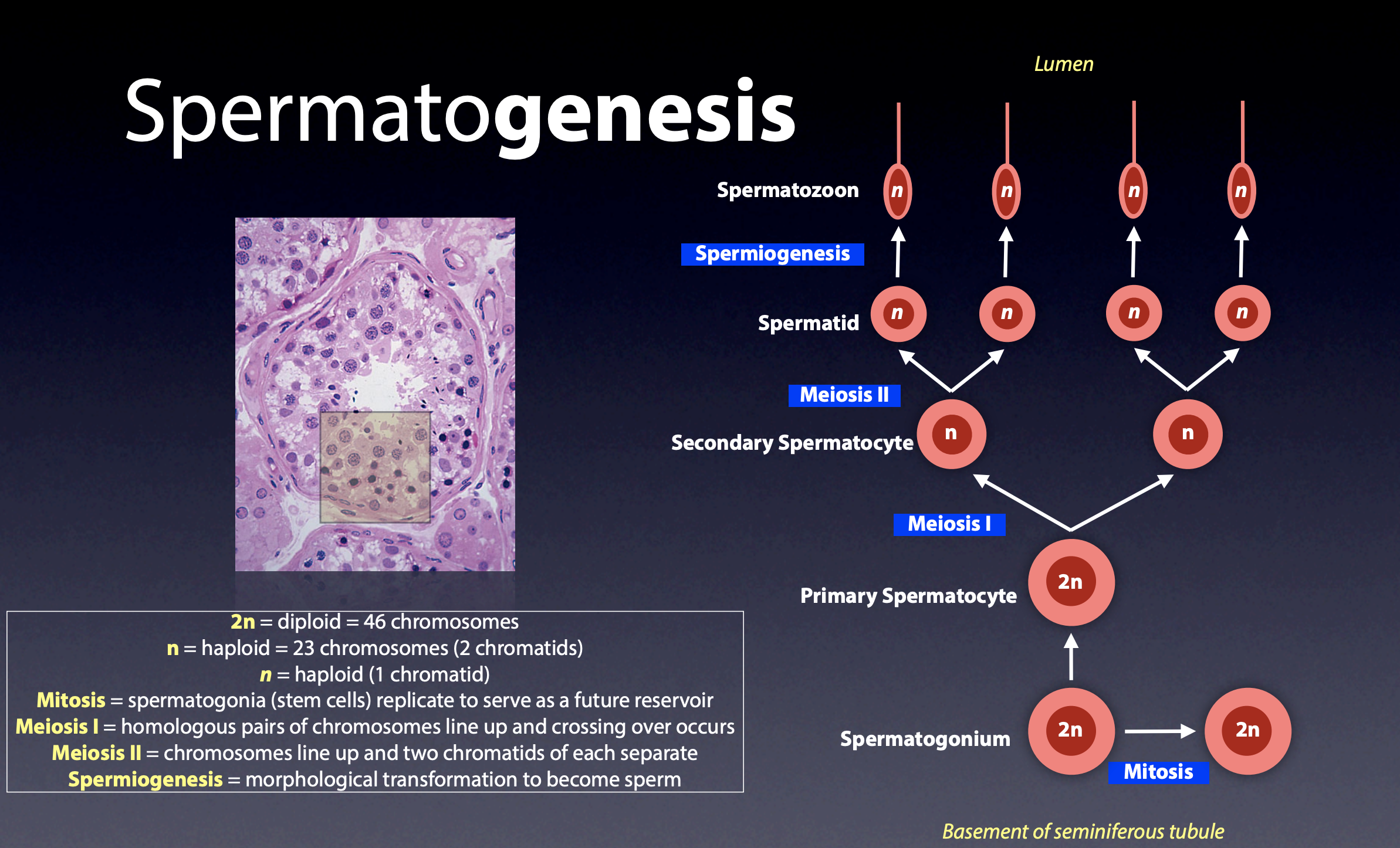
spermatogenesis
process of production of sperm
Simple, round cell becomes an elaborate, highly specialised cell
Most immature form of cell found in the basement membrane, most mature towards the lumen
Begins in outermost layer of seminiferous tubules and proceeds toward the lumen.
4 sperm produced for every spermatogonium, begins at puberty
Takes approx 65-75 days
3 elements:
Mitotic proliferation - produces large number of cells
Meiotic division - generates genetic diversity and halves number of chromosomes in daughter cells
Spermiogenesis - morphological change in shape of the cell from round to sperm shape
spermatogenesis flow chart
spermiogenesis
Round spermatid into elongated spermatozoa = 60 µm long
Adapted for reaching and penetrating an oocyte
300 million sperm produced per day
4 key events:
Development of acrosome
Over anterior nucleus, vesicle of digestive enzymes
Help sperm penetrate oocyte by dissolving surrounding structures of oocyte
2. Development of tail (flagellum)
Sperm motility, as it allows sperm to swim to the oocyte
Help sperm penetrate oocyte through force from the tail
Condensation of nucleus
DNA undergoes packaging, becoming highly condensed, as the wider the nucleus the more risk of the DNA being damaged
This Protects DNA
Shedding of excess cytoplasm
Taken up by Sertoli cells
Streamlined sperm; better motility
male reproductive tract (duct system)
Duct system =
Testes produce physically mature sperm that are incapable of fertilising an oocyte
Tract (ducts) are responsible for functional maturation, nourishment, storage and transport of sperm
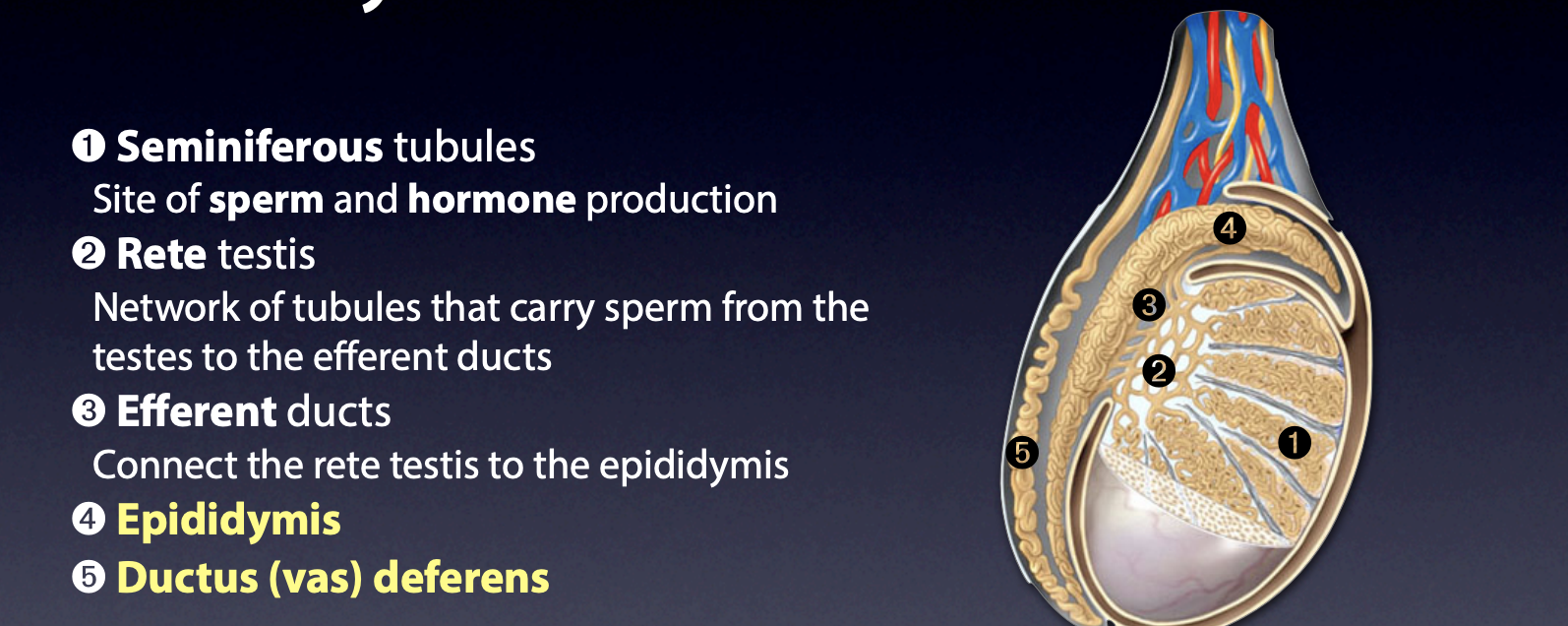
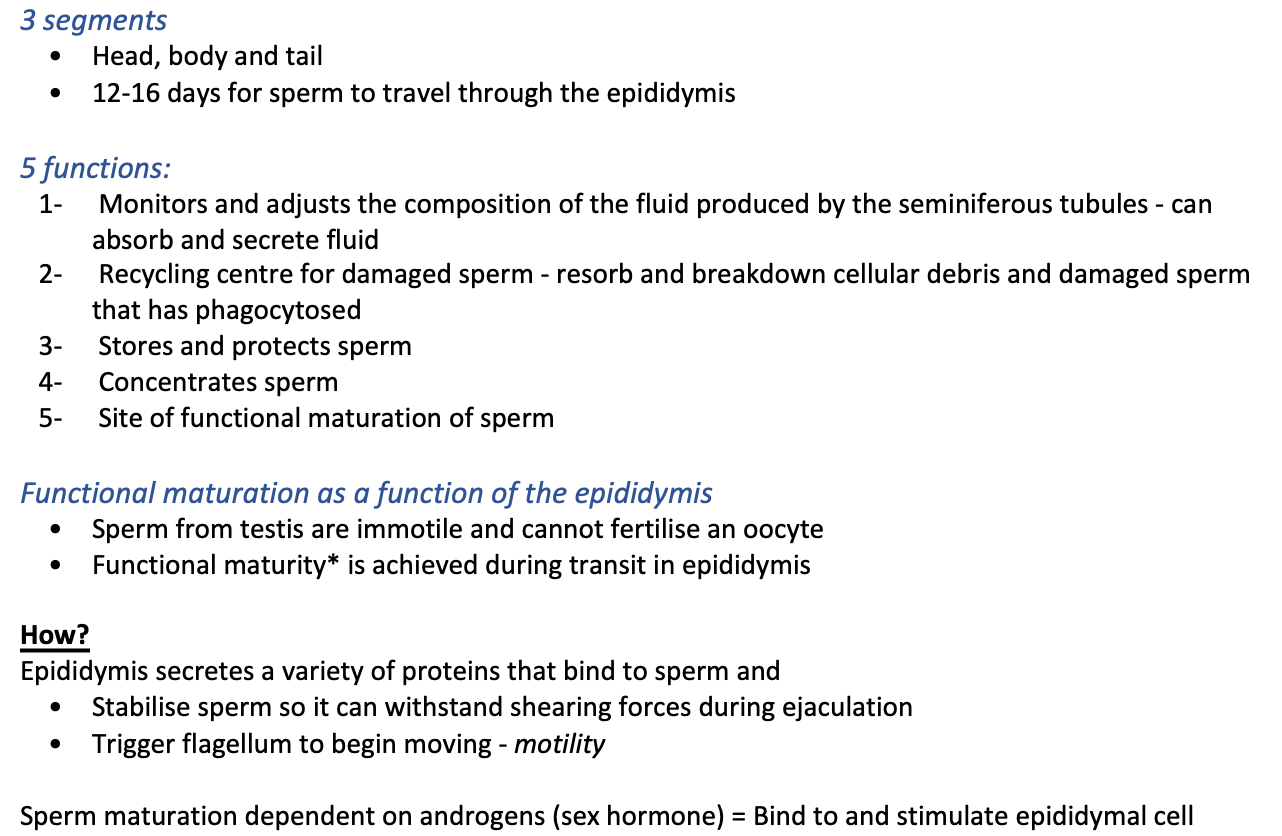
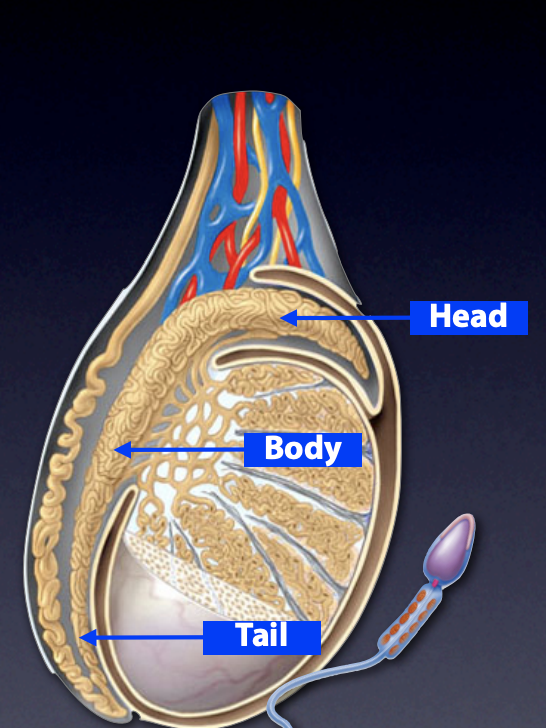
epididymis
Posterior side of testis, can be felt through skin of scrotum
7m long tubule
Coiled and twisted so that it takes up very little space
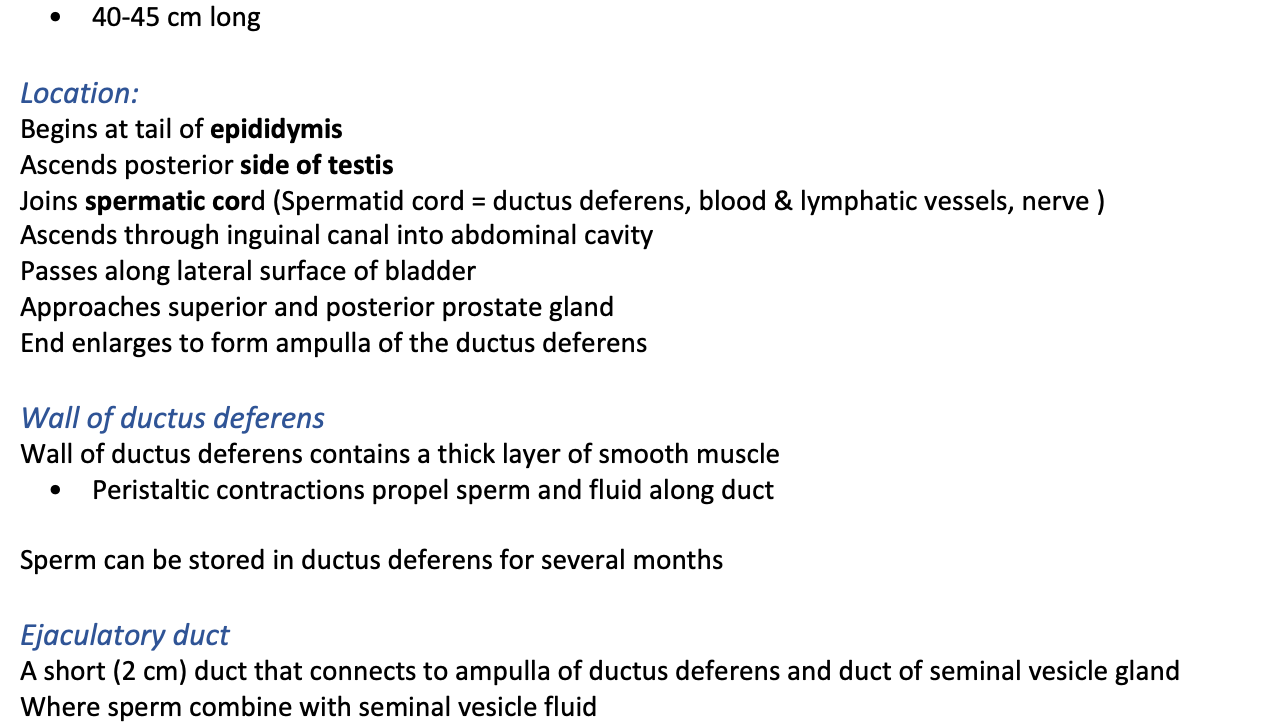
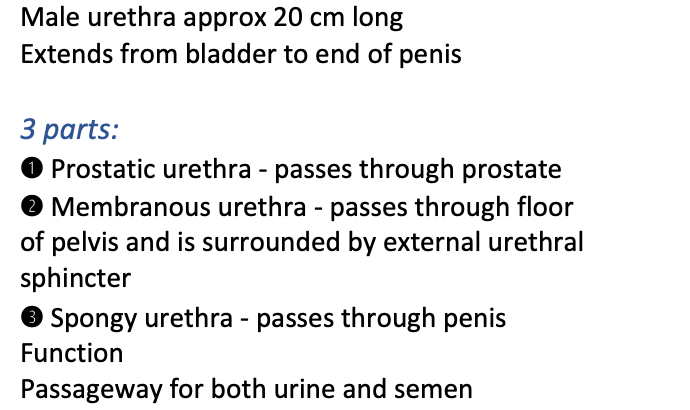
ductus/ vas deferens
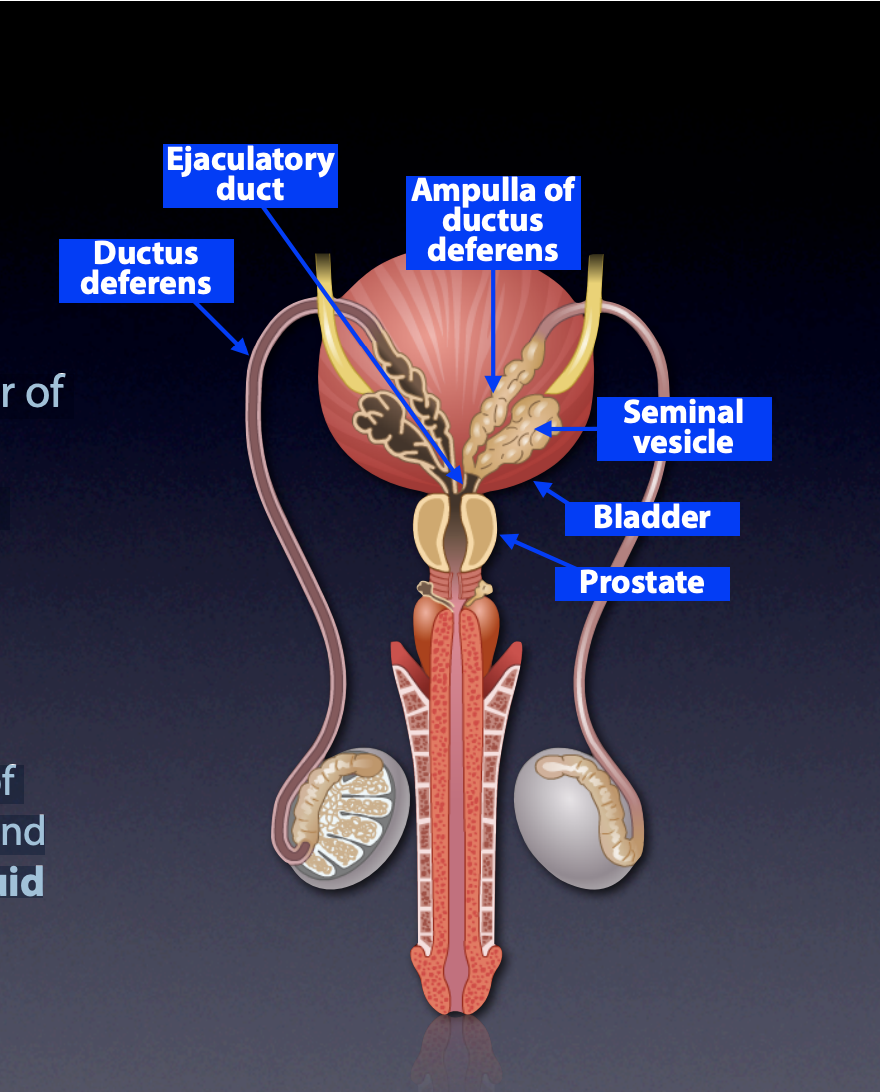
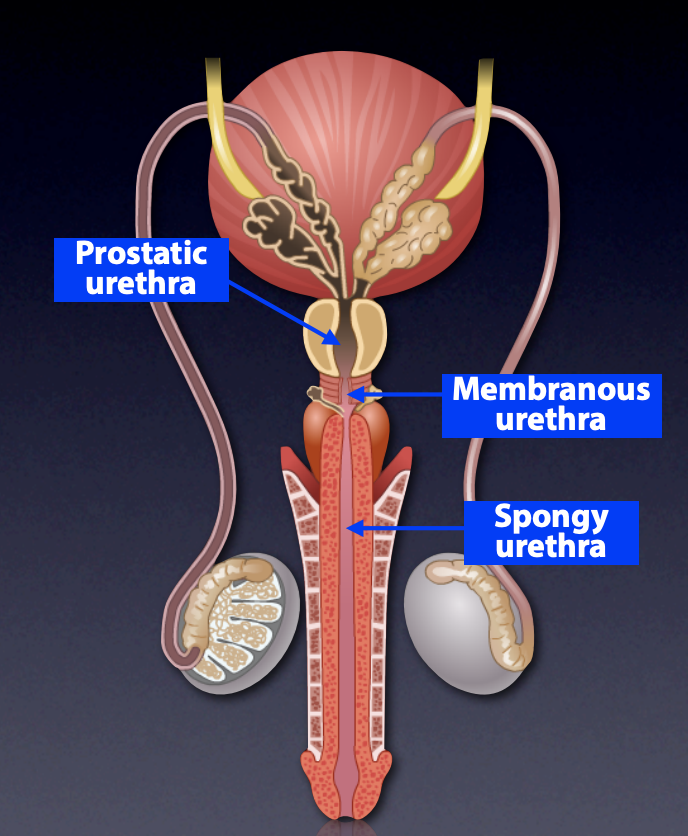
urethra
male accessory glands
seminal vesicles
prostate gland
bulbourethral glands
Small (1 cm) paired glands at the Base of penis
Ducts empty into penile urethra
Secrete thick alkaline mucus prior to ejaculation
Neutralises urethra (acidic from urine) to protect the sperm
Lubricates glans penis
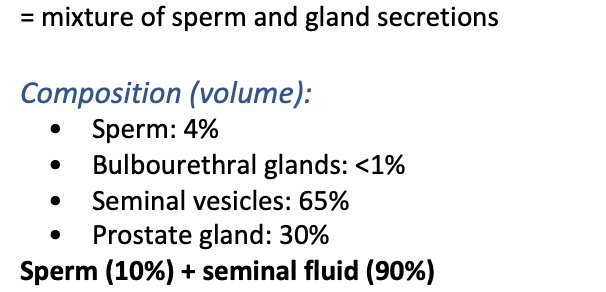
semen composition
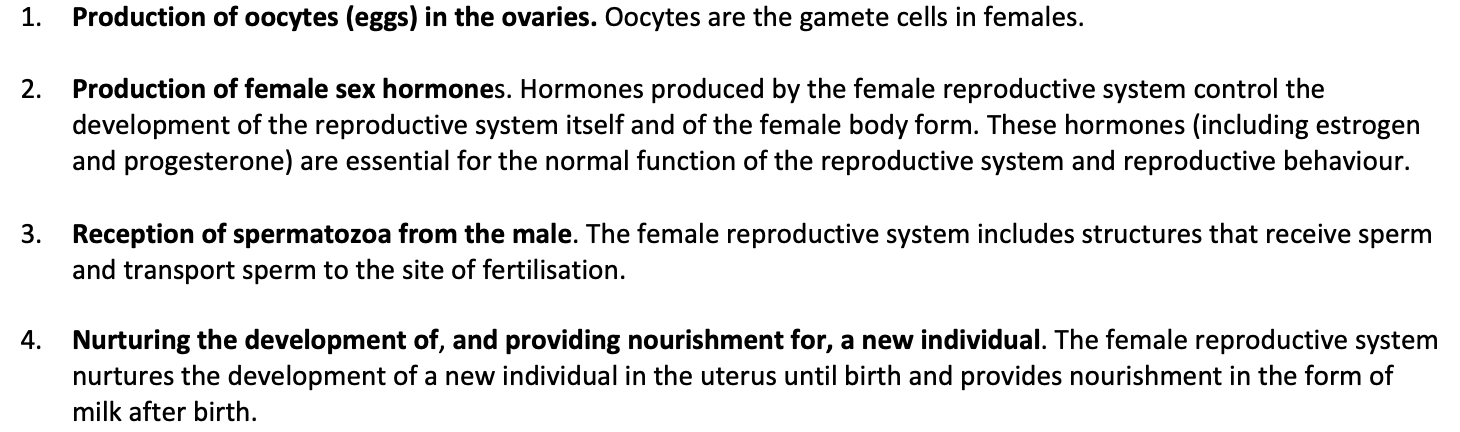
four main functions of female reproductive system
catagories of female reproductive system
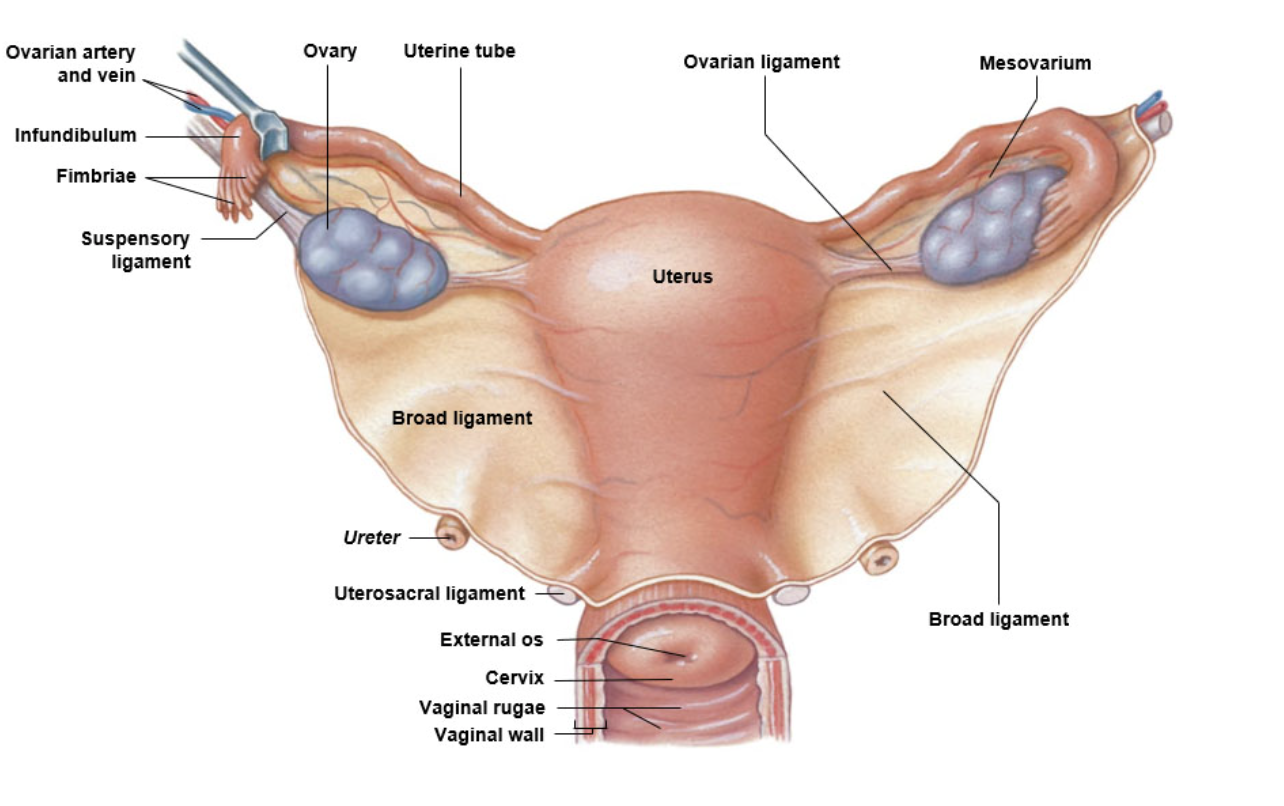
uterine tubes
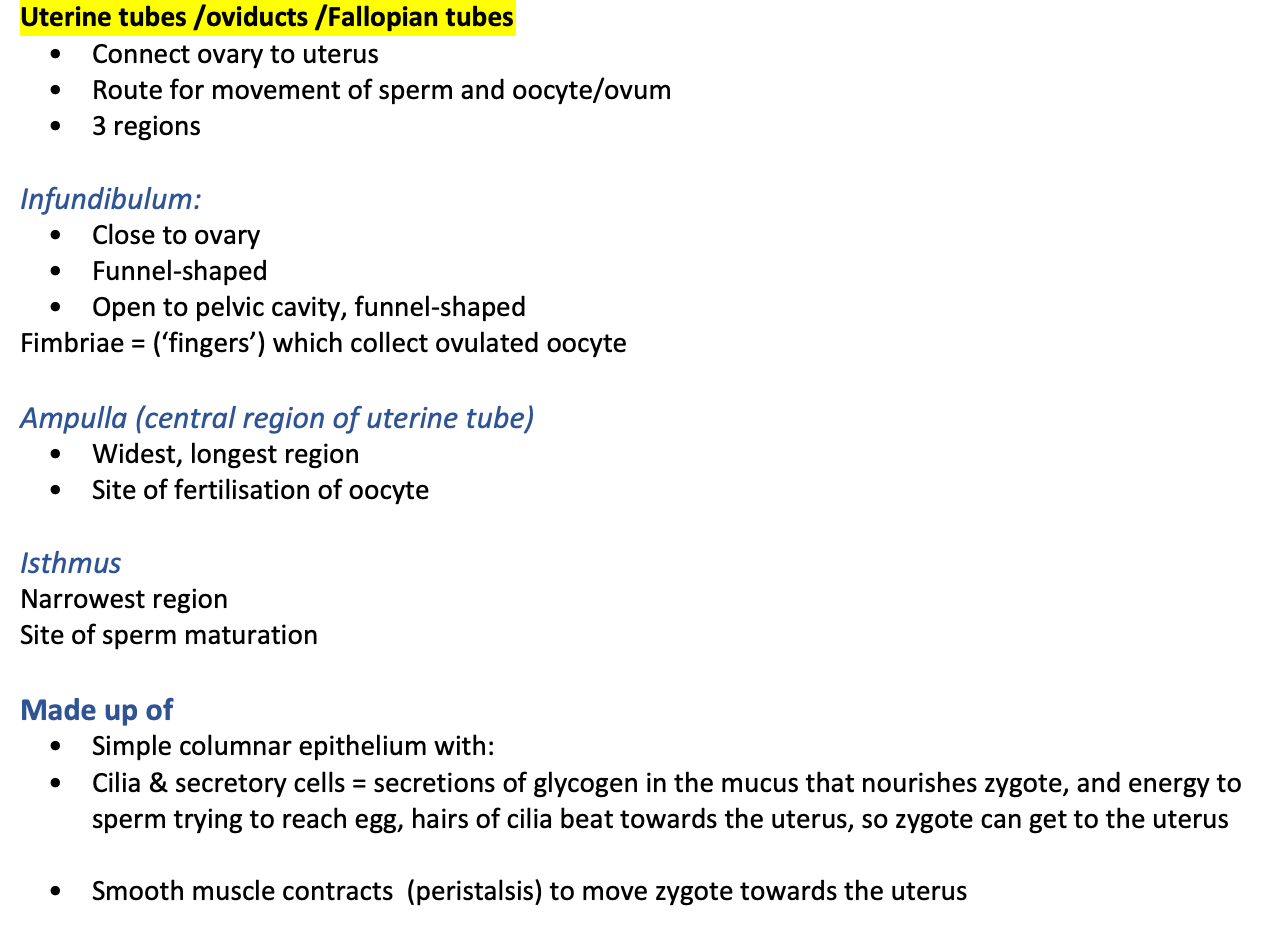
uterus
cervix and vagina
Cervix
Contain mucous glands
Water, proteins; lipid, salts etc. Consistency varies during cycle Near/at ovulation: Less viscous (watery) to allow sperm passage Other times: More viscous (thicker) to impede sperm penetration Vagina Passageway for birth and menstrual flow 10cm fibromuscular canal Stratified squamous non-keratinised epithelium Glands producing glycogen Decomposition produces organic acids Acidic environment retards microbial growth, but … Harmful to sperm
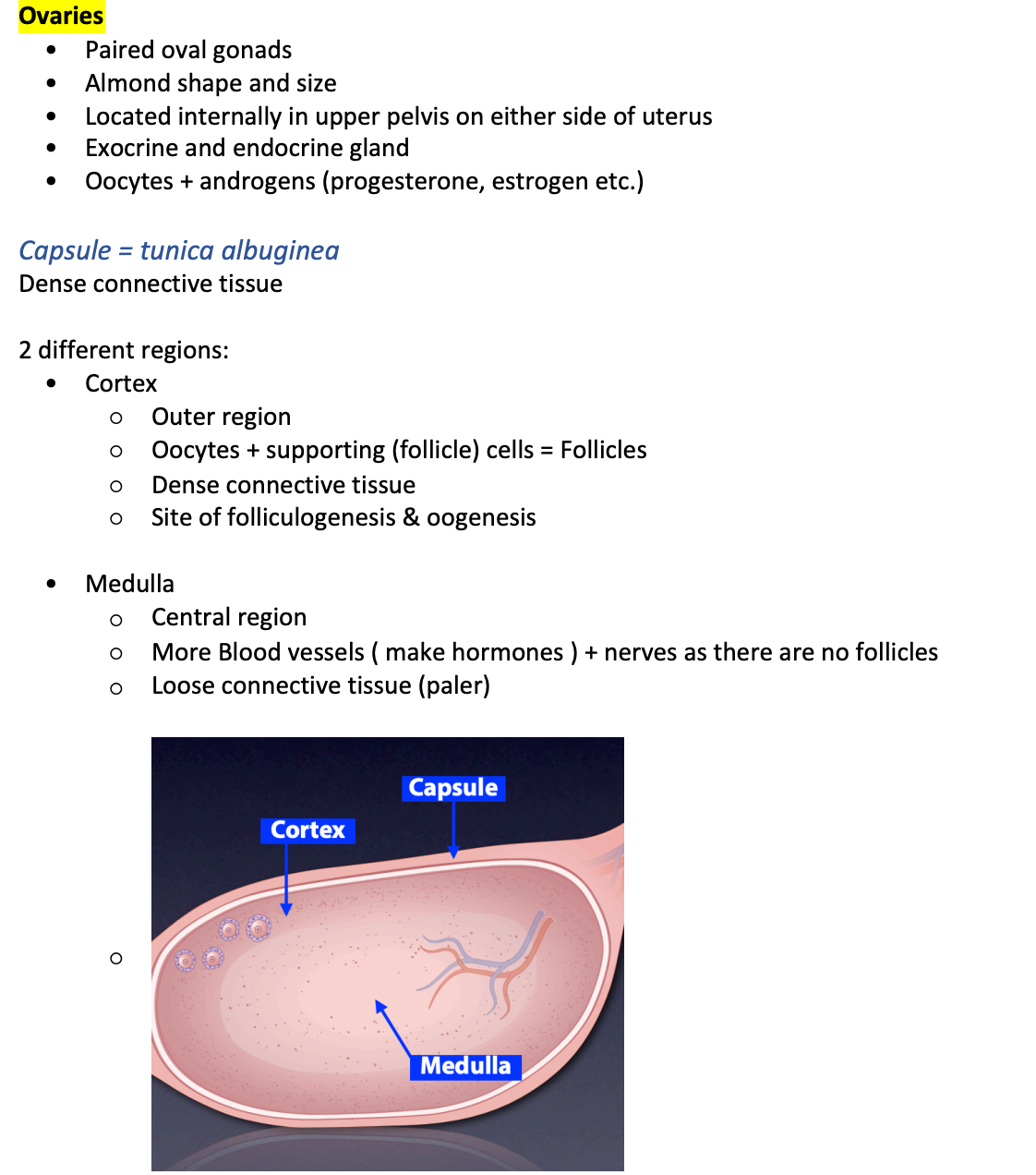
ovaries
folliculogenesis
= development of the follicle
Follicle: oocyte + support (follicle) cells
Begins before birth
Maturation of oocyte + increased number of follicle cells
Primordial follicle
Primary oocyte + single layer of flat follicle cells
Primary follicle
Primary oocyte + 1-2 layers of cuboidal follicle cells
Follicle cells secrete estrogen
Secondary follicle
Enlarged oocyte
Additional layers of follicle cells
Multiple, small fluid-filled spaces develop between follicle cells
Tertiary follicle
= mature or Graafian) follicle
Single, large fluid-filled space (antrum)
Oocyte surrounded by specialised follicular cells called granulosa cells
Ovulation = release of oocyte from ovary
Oocyte and granulosa cells rupture and exit the ovary, most of the follicle and the follicular cells stay behind, it becomes the corpus luteum
Corpus Luteum
= Glandular structure left behind in ovary after ovulation
Empty tertiary follicle collapses
Remaining follicular cells proliferate to fill space
Secrete estrogen and progesterone ( follicular cells made estrogen only before ovulation then after they make BOTH)
Lifespan of 10 days, unless pregnancy occurs
Then after 10 days it becomes the corpus albicans
oogenesis

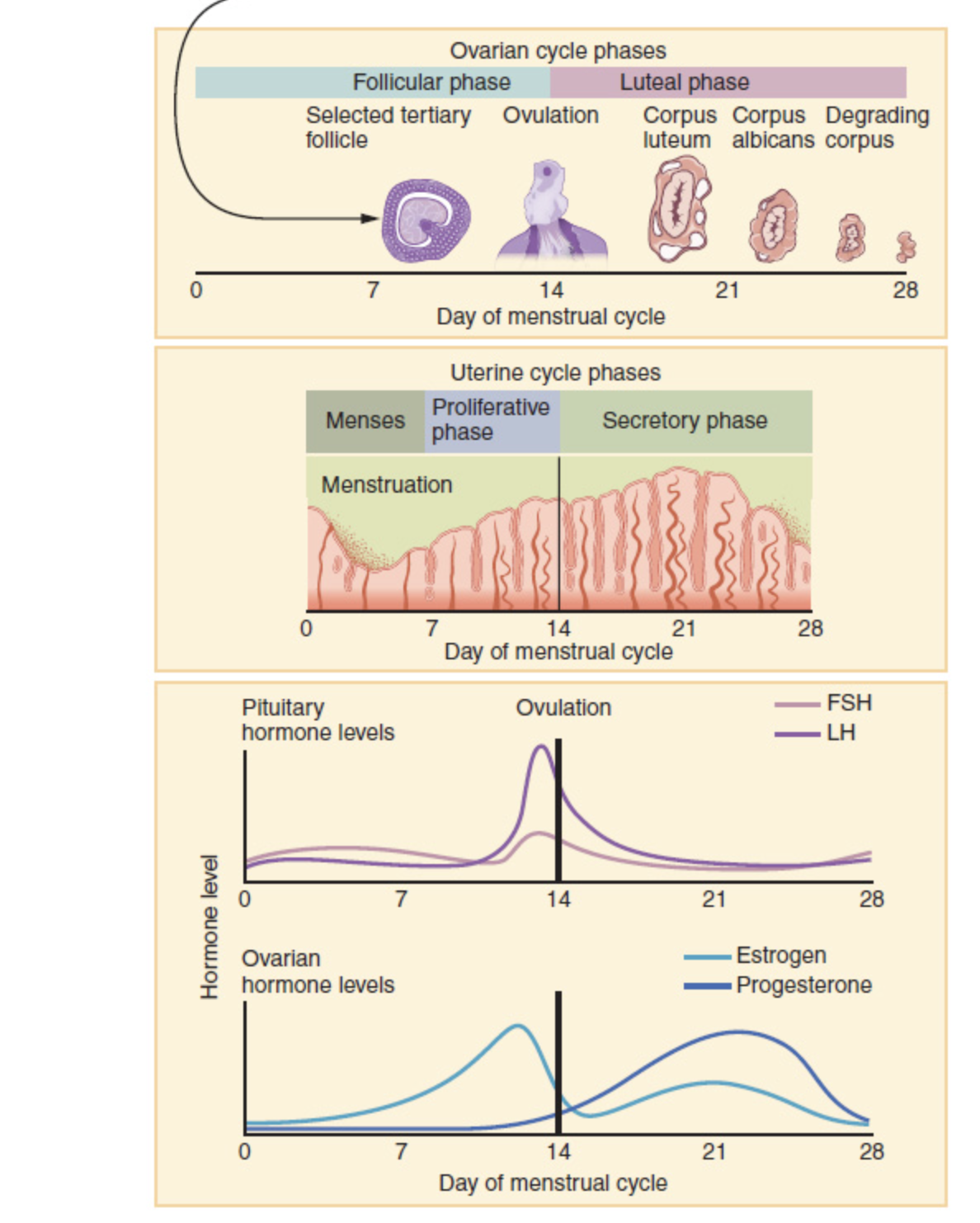
ovarian cycle
Primary oocytes are eggs that are suspended in meiosis I just after a female’s birth. The oocytes remain dormant, surrounded by protective follicular cells, until the menstrual cycle begins at puberty. At puberty, the initiation of the ovarian cycle causes the oocyte to mature within a protective structure called a follicle.
Follicular phase (day 0-13)
The ovarian cycle is regulated by hormones produced in the hypothalamus (GnRH) and anterior pituitary gland (FSH and LH). The ovary contains many follicles with oocytes in various stages of development, however typically only one primary oocyte is released during ovulation approximately every 28 days. The ovarian follicle goes through a series of growth phases until it becomes a fluid-filled vesicular (Graffian) follicle.
Ovulation (day 14)
During ovulation, the vesicular (Graffian) follicle ruptures to release the oocyte into the abdominal cavity, to be picked up by the fimbriae and guided into the uterine tube.
Luteal phase (day 15-28)
The ovulated (empty) follicle transforms into the corpus luteum. The corpus luteum acts as a temporary endocrine gland, secreting large amounts of progesterone (and also moderate levels of other hormones such as estradiol and inhibin A). After pregnancy or menstruation, the corpus luteum deteriorates into a scar of dense connective tissue called the corpus albicans.
what is the female reproductive cycle
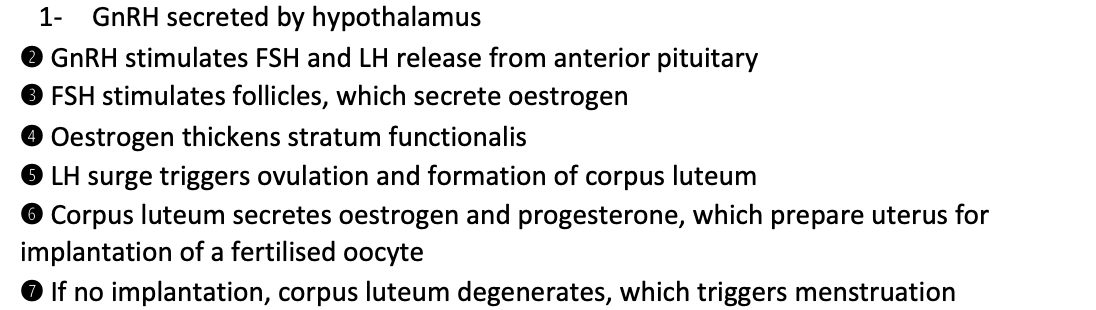
steps in the female reproductive cycle
Gonadotropin hormone-releasing hormone
phases of female reproductive cycle
Pre-ovulation / Proliferative Phase
GnRH secreted by the hypothalamus, travels to the anterior pituatiary
This makes FSH (follicle stimulating hormone) binds to follicular cells casing follicles to grow and develop
Follicle with most FSH receptors becomes the tertiary follicle
Estrogen from the follicles then tells stratum functionalis to regrow in uterus
Ovulation
Then estrogen levels are high there is a positive feedback with more GnRH secreted, triggering a luteinizing hormone (LH) surge, which triggers the follicule rupturing and so OVULATION, at around day 14
Post-ovulatory /Secretory Phase
Ruptured follicle collapses in on itself and becomes the corpus luteum, LH keeps this structure ALIVE and instructs it to make estrogen and progesterone
Progesterone switches endometrial glands on and tells them to make mucus
Negative feedback on GnRH is suppressed for ~10 days whilst oestrogen and progesterone levels are high ( to allow time for egg fertilization)
Menstrual phase
Hypothalamus then picks up on high levels of oestrogen and progesterone in the body
This means there is no GnRH secreted and so no LH, so corpus luteum becomes the corpus albicans
Because there is no oestrogen and progesterone being made (with no corpus luteum) the spiral arteries in the stratum basalis layer in the endometrium the blood flow stops in the stratum functionalis layer, KILLING it, the shedding of this layer is menstruation
This leaves the stratum basalis layer behind and oestrogen and progesterone levels have dropped so negative feedback on GnRH ends and these hormones are made again
how the pill works
Combination of oestrogen and progesterone (or synthetic versions)
21 hormone pills + 7 placebo pills
Suppresses GnRH and thus FSH and LH (i.e., hold cycle at secretory phase)
The high levels of oestrogen and progesterone have a negative feedback and supress the GnRH, so no FSH, and no follicle developing and so nothing to ovulat
fertilizations steps
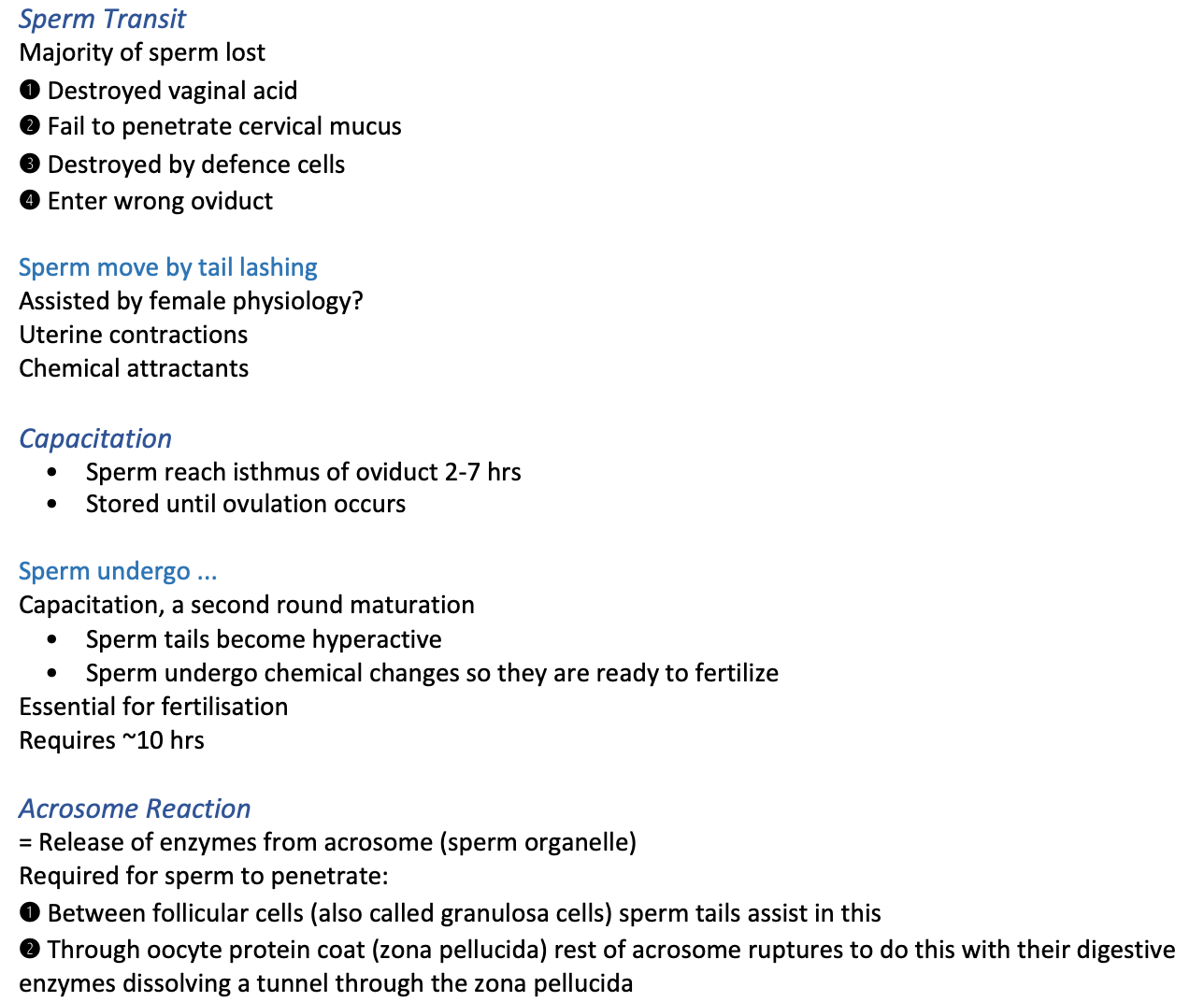
how polyspermy is blocked
Polyspermy blocked
Depolarisation (Na+ influx) when one sperm has entered the oocyte, changing the electrical charge of it, electrically repelling further sperm
Cortical granule reaction (Ca2+ influx) hardens zona pellucida = seen below as the green granules
pre- implantation process
= the First week of development
Characterised by:
Fertilisation
Cleavage of zygote
Blastocyst formation
Followed by implantation
Cleavage of zygote
Once sperm enters oocyte:
Single cell now called a zygote
This is called cleavage
'
Morula
Day 4
Solid ball of cells
Enters uterus day 5
Zona pellucida disintegrates to release…
Blastocyst
Cavity appears
Outer cells (trophoblast) become foetal part of the placenta
Inner cell mass (embryoblast) become the embryo
Occurs in the isthmus and the oviduct
Morula appears at day 4 when the oocyte has entered the uterus
At day 5 the zona pellucida is dissolved away
Structure can then implant into the wall, as a blastocyst, centre is fluid surrounded by cells