Adult Health Integumentary
1/8
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
9 Terms
What are the stages of Burn Care
Resuscitative/Emergent Phase
Emergency-lightsThe emergent (resuscitative) phase of burn management begins at the time of burn injury. The focus of this phase is to address the immediate and potentially fatal problems caused by the burn injury. Assessing the patient's burns will determine the plan of treatment (refer to the Picmonic "Burns Assessment"). The main concerns include hypovolemic shock and edema formation.
Injury to Return of Capillary Permeability
Injured Returning to CaterpillarAs quickly as 20 minutes after the burn occurs, injury to the capillaries can cause major fluid and electrolyte shifts from the vasculature into the interstitial tissues. The primary concern is hypovolemic shock, as the vascular fluids move into interstitial spaces (second-spacing) and areas that normally have no fluid (third-spacing), leading to vascular volume loss. Examples of third-spacing include blisters and edema. Capillary permeability is restored by adequate fluid replacement. As interstitial fluid gradually returns to the vascular space, edema disappears and diuresis begins.
48-72 hours
(40) Oz and (8) Ball to (70) Guy and (2) TutuThe emergent phase usually lasts 48-72 hours from the time the burn occurred. The beginning of diuresis marks the end of the emergent phase.
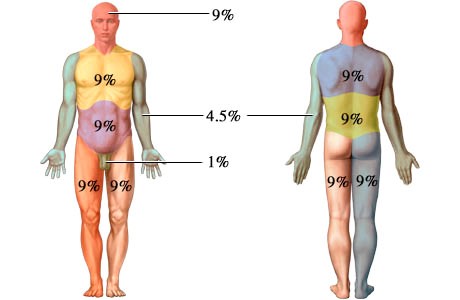
IV Fluid Replacement
Fluids being Replaced by IVPatients with 15% TBSA or more will need at least two large bore IV access sites for infusing large volumes of fluid (refer to the Picmonic on "Rules of 9s"). After calculating the patient's fluid needs using the Parkland (Braxton) formula, crystalloid solutions (Lactated Ringer's) or colloidal solutions (albumin) are infused as scheduled. Colloidal solutions are recommended after the first 12-24 hours postburn when capillary permeability returns to normal and the fluid stays in the vasculature for circulation. The rate of fluid administration is titrated hourly based on patient response such as urine output or vital signs.
Acute Phase
Acute-angleDuring the acute phase of burn management, wound care is the primary focus. This phase, which may last for weeks or months, starts with diuresis and ends with wound healing or skin grafting. Bowel sounds return and the patient may need psychosocial support as reality sets in. The patient's laboratory values, especially sodium, potassium, and glucose, should be closely monitored as capillary permeability restores to normal. As the burn wounds begin to heal, encourage the patient to stretch and move as much as possible to prevent painful contractures.
Diuresis to Near Wound Closure
Die-rocket Near Wound ClosureFluid mobilization results in diuresis and the patient becomes less edematous. Necrotic tissue surrounding the wound sloughs off as fibroblasts begin the process of forming granulation tissue. Partial-thickness burn wounds will heal within 10-21 days as long as kept moist and free of infection. However, full-thickness burn wounds require the surgical excision of burn eschar and application of skin grafts for healing
Wound Closure to Return of Optimal Level
Wound Closure Returned to FameDuring the final stage of burn care management, wounds have healed and the patient begins to engage in self-care. The patient works toward rehabilitation and reintegration into society. Teaching and psychosocial support will help the patient manage changes in body image. Since newly-healed areas of skin may be hypersensitive to sun, teach the patient to avoid direct sunlight for the next 3 months to prevent hyperpigmentation and sunburns. Teach the patient how to complete dressing changes and wound care. If necessary, refer the patient to home care nursing services for follow-up care after discharge.
Skin anatomy
Epidermis (Outer Layer)
Structure: This is the thin, top layer of the skin that you see and touch.
Function: It acts as a protective barrier, preventing germs and water from entering the body. It also produces new skin cells, contains melanin for skin color, and includes immune cells to fight off infections.
Dermis (Middle Layer)
Structure:
Located beneath the epidermis, the dermis is a thicker layer. It contains connective tissue, hair follicles, sweat glands, and blood vessels.
Function:
The dermis provides the skin with strength and elasticity due to its collagen and elastin fibers. It also houses sensory nerve fibers, which allow us to feel.
Hypodermis (Deepest Layer)
Structure: Also known as subcutaneous tissue, this is the deepest layer of the skin.
Function: The hypodermis is made of fat and connective tissue that anchors the skin to the underlying muscle. It stores fat for insulation, protects the body, and provides padding.
What are the hormones secreted in burn patients
Epinephrine - causes vasoconstriction, rises blood pressure, perfuses the vital organs
Antidiuretic hormones (ADH) - retain water and increase blood volume (causes increased BP that helps in perfusion)
Aldosterone - retain sodium and water leading to an increase in blood volume (causes increased BP that helps in perfusion)
Rule of nine in burn patient
Stages of Pressure Ulcer
Stage I: Intact skin with a localized area of non-blanchable redness
Stage II: Partial-thickness skin loss involving the epidermis and dermis.
Stage III: Full-thickness skin loss extending into the subcutaneous tissue but not through the fascia.
Stage IV: Full-thickness tissue loss involving deep tissue damage to muscle, bone, tendons, or ligaments
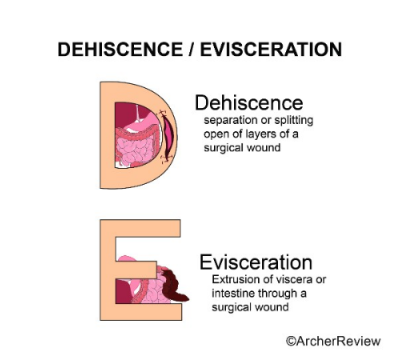
Dehiscence vs Evisceration
Dehiscence - separation or splitting open of layers of a surgical wound
Evisceration - extrusion of viscera or intestine through a surgical wound
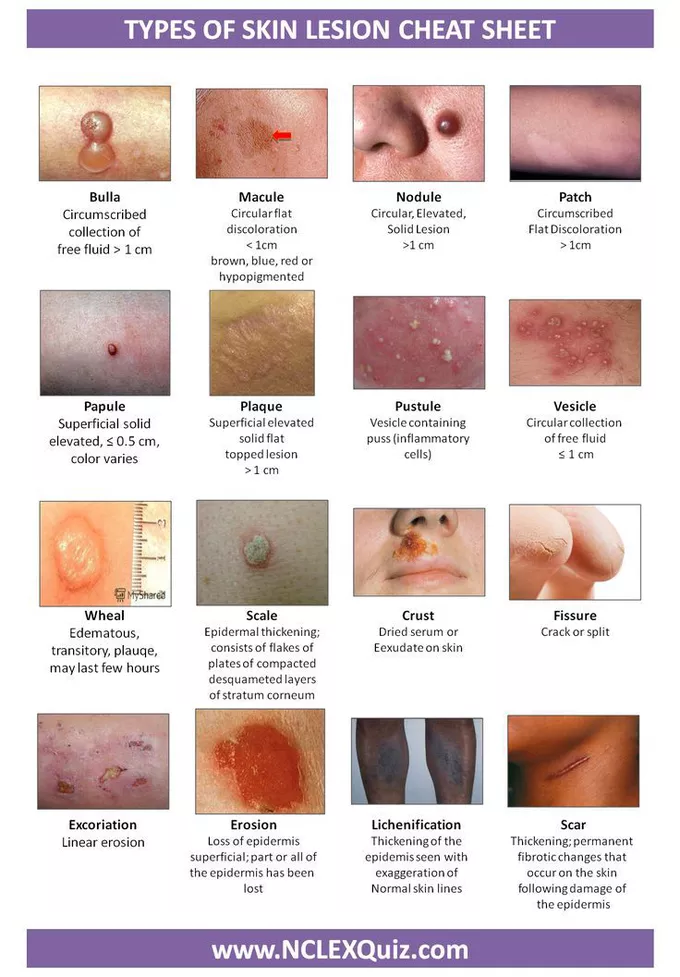
Types of Skin Lesions
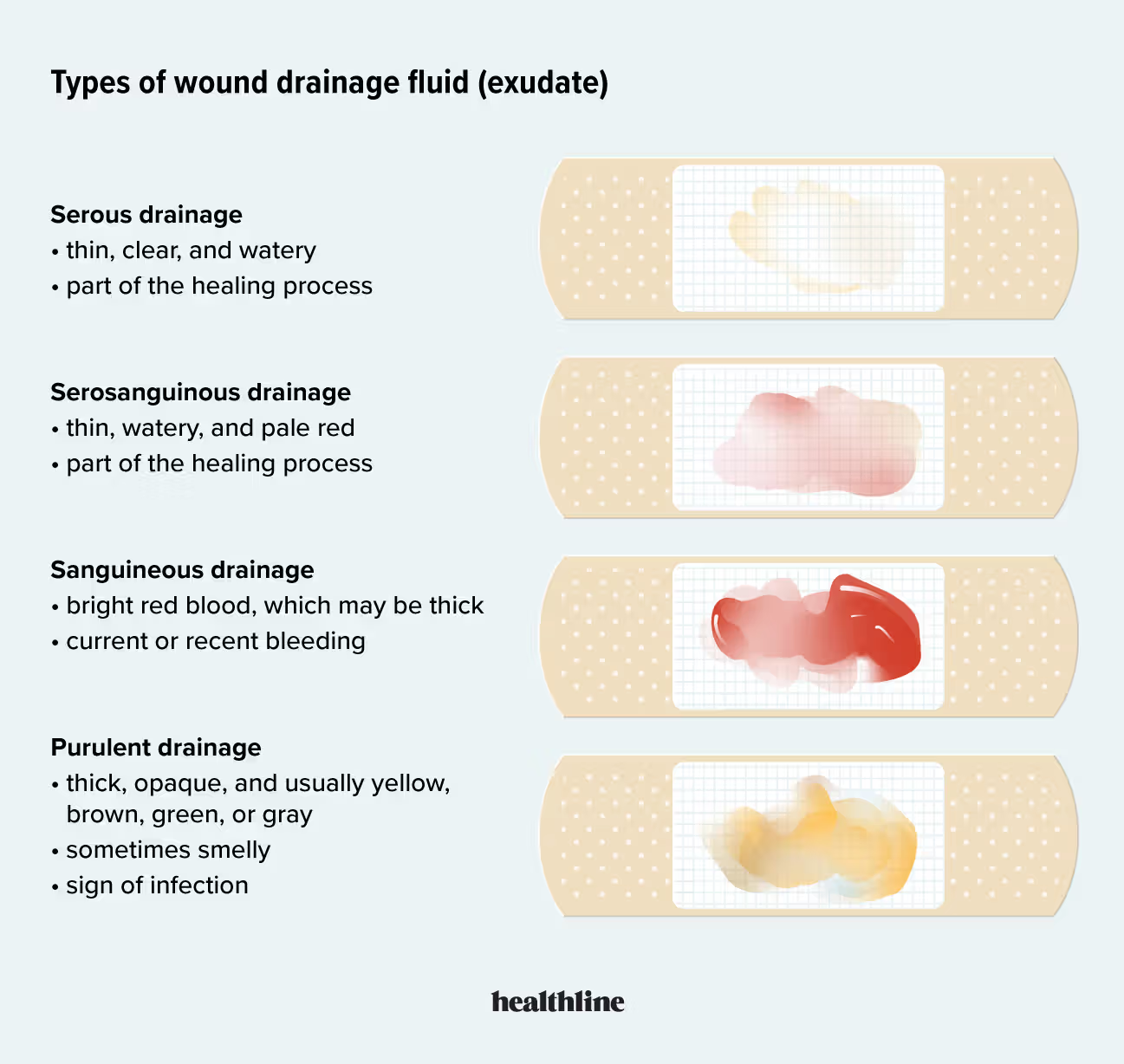
Types of Wound Drainage
Serous drainage
thin, clear, watery
part of healing process
Serosanguinous drainage
thin, watery, and pale red
part of the healing process
Sanguineous drainage
bright red blood, which may be thick
current or recent bleeding
Purulent drainage
think, opaque and usually yellow, brown, green, or gray
sometimes smelly
sign of infection