Lecture 24 and 25: Bacterial diseases
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
Most common locations for bacterial infections
Skin, Urinary, respiratory, GI tract
Diagnostics for bacterial infections
CBC/Chem/UA, cytology, culture and sensitivity
Acute hemorrhagic diarrhea syndrome. Diagnosed by ELISA, PCR, or fecal culture
C. perfringens
Treatment for C. perfringens
Metro, ampicillin, NO tetracycline
Toxin A and Toxin B. Diagnosed with fecal culture, antigen test, ELISA. Treated with metronidazole
C. difficile
Watery diarrhea. Diagnosed with fecal exam and culture. Treated Erythromycin and fluoroquinilones.
Campylobacter
Diagnosed by PCR, serology, culture. Treated with fluorquinolones, chloraphenicol, TMS, amoxicillin
Salmonella
Granulomatous colitis (boxer colitis)
E. coli
How do you diagnose bartonella?
Serum antibodies, PCR, in clinically ill animals w/ no other explanation for illness
Treatment of bartonella
Doxycycline, azitrhomycin, fluroqunilones for 4-6 weeks
Flea and tick control
Check serum antibodies after treatment 🤷🏼♀️
What is main reservoir host for B. henselae and B. clarridgiae
Cats
How is C. felis transmitted?
Survives in flea feces → cat claws → scratch, open wounds
CS of bartonella in cats
Fever and cardiac issues (most common) , lethargy, lymphadenopathy, uveitis, gingivitis, endocarditis, myocarditis, hyperglobulinemia, vasculitis, neuro
Diagnosis of bartonella in cats
Blood culture, PCR assay, serology
Test casts with clinical signs
Treatment of bartonella in cats
Doxycycline
Fluroquinolones
Zoonotic control of bartonella
Flea control year round
Claws should be trimmed regularly
Bites and scratches should be avoided
Wash any cat related wounds promptly
Keep cats indoors
Avoid need sticks contaminated with blood from potentially infected animals
How is brucellosis transmitted?
Mucus membrane → Macrophages → LN → bacteria → repro organs
CS of brucella
Abortion and infertility
Lethargy, exercise intolerance, WL, back pain, lympadenopathy, poor hair coat
Epididymitis, scrotal pain and swelling, sperm abnormalities, testicular atrophy
Abortion, vulvar discharge, puppy death or bacteremia
How do we diagnose brucellosis?
No single reliable test
Serology
Blood culture or PCR (definitive diagnosis)
Treatment of brucella
Enrofloxacin
Euthanasia
prevention, quarantine/isolate, screen
Characteristics of clostridium
Ubiquitous in the environment
Neurotoxins produced by bacteria
Dogs/cats are more resistant
Transmission of tetanus
High resilient spores introduced via wound/penetrating injury (affects inhibitory interneurons GABA)
How is botulism transmitted?
Ingestion of preformed toxin in bad food
CS of tetanus
Localized or generalized muscle rigidity of facet and eyes, limbs, stiff gait/sawhorse stance
CS of botulism
Flaccid paralysis w/ autonomic nervous system. 12 hours after ingestion
Diagnosis of tetanus
History and CS, serology for antibodies to tetanospasmin
Diagnosis of botulism
History and CS
Treatment of tetanus
Remove source of infection (metronidazole combo w/ clindmycin/doxy)
Control symptoms with supportive care (phenobarbital, phenothiazines, benzodiazepines)
Treatment of botulism
Antitoxin (Type C botulism)
Prognosis actually fair if can support for 2-3 weeks though muscle weakness can be prolonged
Inhabits mucosal surface of respiratory, digestive and urogenital tract (M. felis, M. cynos)
Non-hemotropic
Candidates mycoplasma haeomomitum, M. haemocelis, M. haemocanis
Hemotrophic
Do cats with bartonella get IMHA?
No
Diagnosis of non-hemotropic mycoplasma
Cytology, culture, PCR (can be normal flora)
Diagnosis of hemotropic mycoplasma
Culture or PCR
Treatment of non-hemotropic
Doxycycline, clindamycin, azitrhomycin, fluorrqinolone
Treatment of hemotropic mycoplasma
Doxycycline, marbofloxacin, pradoflaxcin
Most common Lepto classifications
L. autumnalis
L. bratislava
L. canicola
L. grioppotyphosa
L. hardjo
L. icterohaeomorrhagiae
L. pomona
How is lepto transmitted?
Cats subbclincial but will shed the organism
Pass in urine → enter through abraded skin or through mucous membranes (ingestion, contaminated soil or water)
Hepatic, renal, or pulmonary disease secondary to inflammation toxin production
CS of lepto
Fever, uveitis, vomiting, diarrhea, renomegaly, hepatomegaly, PU/PD, icterus
Diagnosis of lepto
Globulin abnormalities
Hypocalcemia and renal issues
Microscopic agglutination test (MAT)- antibody titer
Darkfield microscopy, PCR
Treatment of lepto
Fluids for renal treatment
Ampicillin/amoxicillin for acute phase
Doxycycline for carrier phase
Enrofloxacin
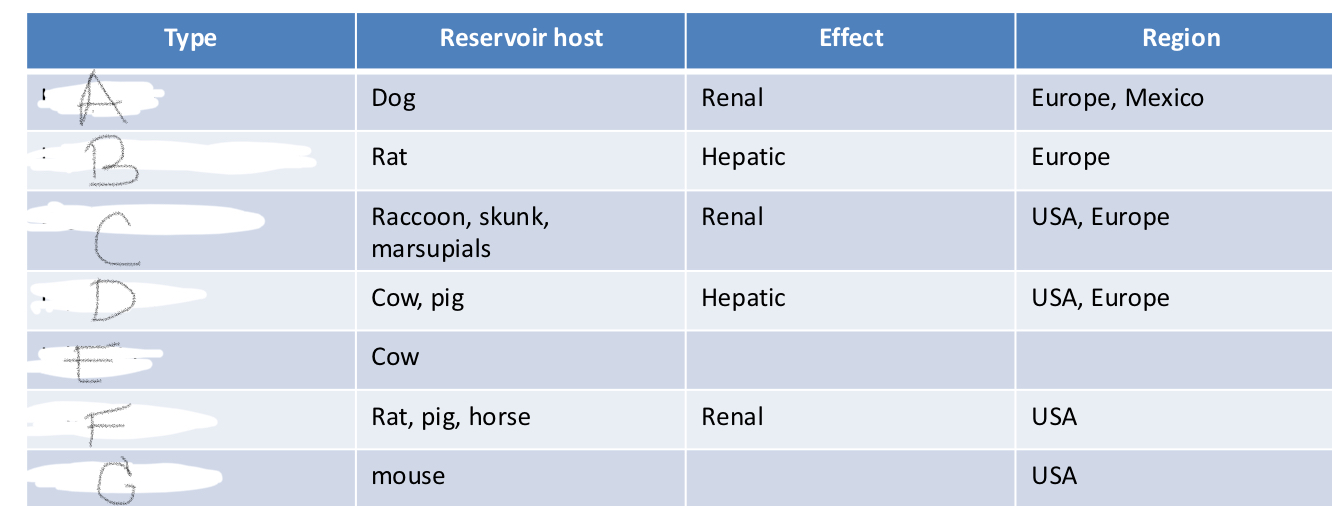
A- L. canicola
B- L. Icterohaemorrhagiae
C- L. grippotyphosa
D- L. pomona
E- L. hardjo
F- L. bratislava
H- L. autumnalis
LC of Yersinia
Rodent flea → rodent/squirrles/prarie dogs
C. felis is the vector
Cats and dogs are suspceptible
How do you transmit Yersinia?
Flea bite, ingestion of infected rodent, inhalation of organism
CS of Yersinia
Fever, anorexia, depression, cervical swelling, dyspnea/respiratory, cough
Diagnosis of Yersinia pestis
NSF CBC, chemistry, rads
Culture, cytology, PCR, fluorescent antidbody of affected tissue
Bipolar rods
Treatment of Yersinia
Supportive care
Drain abscesses
Unclear which antibiotics
Streptomycin, gentamicin, chloraphenicol, tetracycline
A 3-year-old Labrador Retriever presents with symmetrical, ascending weakness starting in the pelvic limbs. On neurological examination, hyporeflexia and hypotonia are noted. The owner reports that the dog ate some raw chicken a few days ago. Which of the following is the most likely diagnosis? (a) Canine Leptospirosis (b) Canine Tetanus (c) Canine Botulism (d) Canine Plague
(c) Canine Botulism
Which of the following statements about the etiology of canine botulism is correct? (a) It is caused by a gram-negative, aerobic bacterium. (b) The bacterium produces toxin in anaerobic, acidic environments. (c) The most common toxin subtype in canine cases is type B. (d) Toxin is actively secreted by the bacterial cells.
(b) The bacterium produces toxin in anaerobic, acidic environments.
A dog presents with dysuria, pollakiuria, and hematuria. Urinalysis reveals proteinuria, hematuria, and pyuria. Routine aerobic urine culture is negative. Which of the following pathogens should be suspected? (a) Clostridium botulinum (b) Yersinia pestis (c) Leptospira spp. (d) Mycoplasma spp.
(d) Mycoplasma spp.
Which of the following diagnostic findings is most indicative of canine mycoplasmal cystitis? (a) Observation of motile bacteria on urine sediment. (b) Persistent pyuria with negative routine aerobic urine culture. (c) Detection of Mycoplasma spp. in urine collected by voiding. (d) Elevated blood urea nitrogen and creatinine.
(b) Persistent pyuria with negative routine aerobic urine culture.
A dog from New Mexico presents with fever, lethargy, and a swollen, painful lymph node in the submandibular region. The owner mentions the dog frequently chases prairie dogs. Which of the following is the most likely causative agent? (a) Clostridium tetani (b) Leptospira spp. (c) Yersinia pestis (d) Mycoplasma canis
(c) Yersinia pestis
What is the primary mode of transmission for Yersinia pestis in endemic areas? (a) Direct contact with infected animals. (b) Ingestion of contaminated food or water. (c) Flea bites from infected rodents. (d) Aerosol transmission from infected dogs.
(c) Flea bites from infected rodents.
A dog with a wound on its paw exhibits muscle rigidity, a stiff gait, and a characteristic "risus sardonicus" facial expression. Which of the following neurotoxins is responsible for these clinical signs? (a) Botulinum toxin (b) Tetanospasmin (c) Tetanolysin (d) Mycoplasma cytotoxin
(b) Tetanospasmin
Tetanospasmin exerts its effects by inhibiting the release of which neurotransmitters? (a) Acetylcholine and norepinephrine (b) Dopamine and serotonin (c) Glycine and γ-aminobutyric acid (GABA) (d) Glutamate and aspartate
(c) Glycine and γ-aminobutyric acid (GABA)
Which of the following antibiotics is generally considered the drug of choice for treating canine plague? (a) Amoxicillin (b) Doxycycline (for less severe cases) (c) Enrofloxacin (d) Gentamicin
(d) Gentamicin
A dog presents with fever, vomiting, diarrhea, and icterus. Urinalysis reveals proteinuria and hematuria. The dog's owner lives in a rural area and the dog often drinks from puddles. Which of the following diagnostic tests would be most useful in initially screening for leptospirosis? (a) Aerobic urine culture (b) Point-of-care test for Leptospira antibodies (e.g., SNAP® Lepto) (c) Electromyography (d) Fecal cytology
(b) Point-of-care test for Leptospira antibodies (e.g., SNAP® Lepto)
Which of the following statements regarding the Microscopic Agglutination Test (MAT) for leptospirosis is correct? (a) A single negative MAT test rules out leptospirosis. (b) It can definitively identify the infecting serovar. (c) Obtaining paired titers at a 7-14 day interval is recommended to identify seroconversion. (d) Post-vaccinal titers are typically very low and never exceed 1:800.
(c) Obtaining paired titers at a 7-14 day interval is recommended to identify seroconversion.
A dog diagnosed with leptospirosis is being treated with penicillin. However, the veterinarian is concerned about the potential for the dog to become a carrier. Which of the following antibiotics is effective against the carrier state of leptospirosis by eliminating the organism from the kidneys? (a) Penicillin (b) Ampicillin (c) Doxycycline (d) Amoxicillin-clavulanate
(c) Doxycycline
A cat presents with unilateral conjunctivitis characterized by conjunctival hyperemia, edema, and a thick, white exudate. Corneal involvement is not noted. Cytology of the exudate reveals pleomorphic bacteria. Which of the following is a likely causative agent? (a) Chlamydia felis (b) Feline Herpesvirus-1 (c) Nonhemotropic Mycoplasma spp. (d) Bordetella bronchiseptica
(c) Nonhemotropic Mycoplasma spp.
Which class of antibiotics should generally be avoided in dogs with botulism due to their potential to block neuromuscular function? (a) Penicillins (b) Cephalosporins (c) Fluoroquinolones (d) Aminoglycosides
(d) Aminoglycosides