thyroid hormones - lecture 28 FIRST LECTURE FOR EXAM 5
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
38 Terms
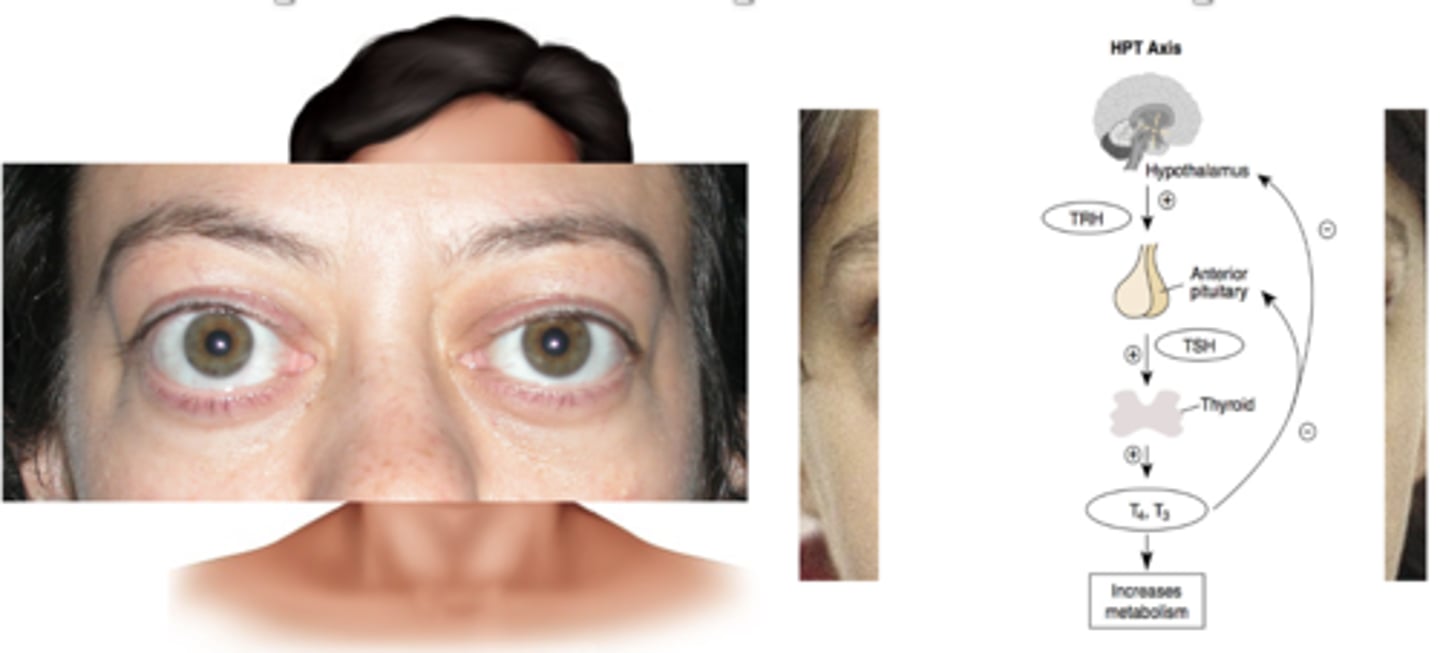
hypothalamus and pituitary
control the normal secretion of thyroid hormones, which in turn control metabolism
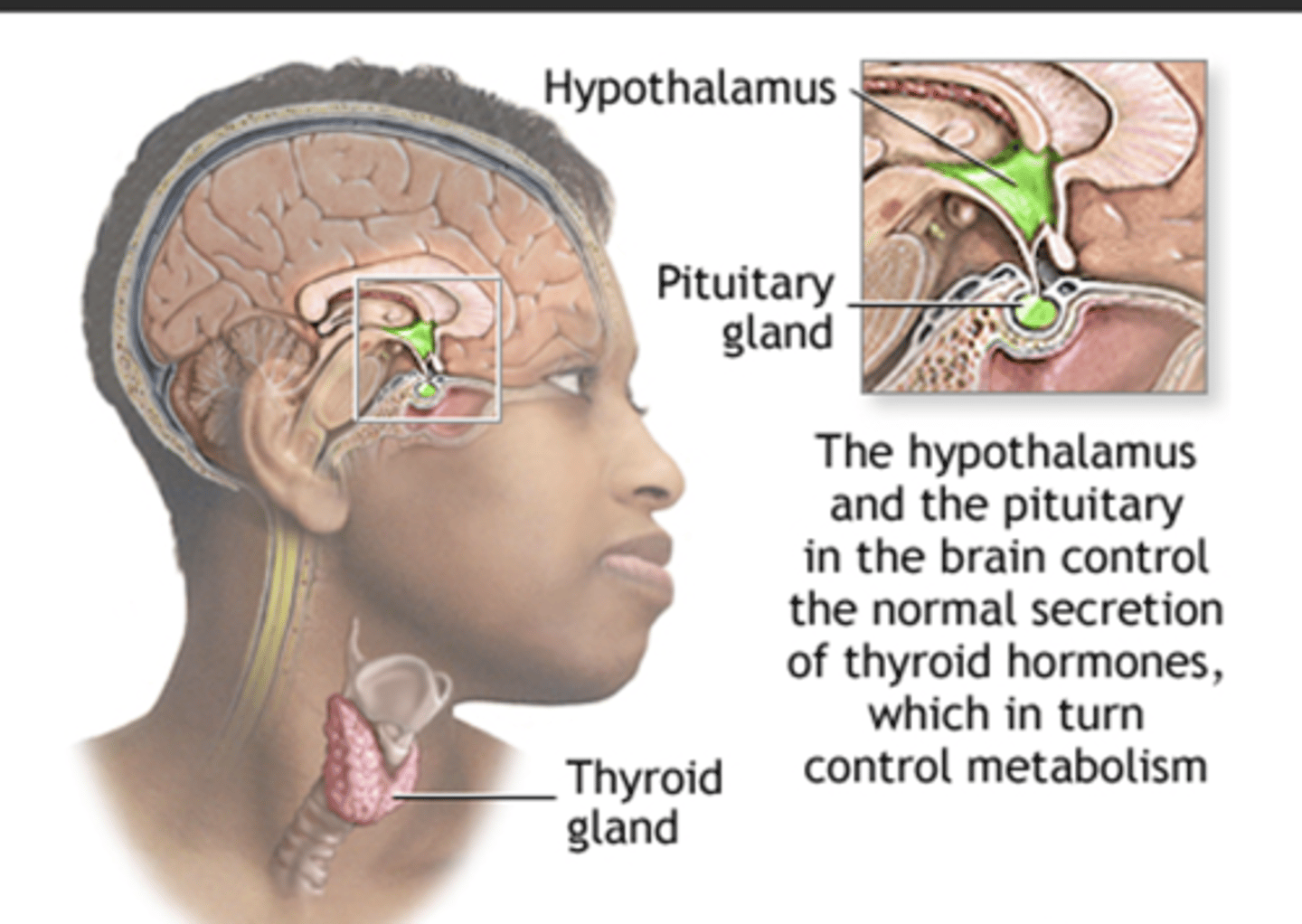
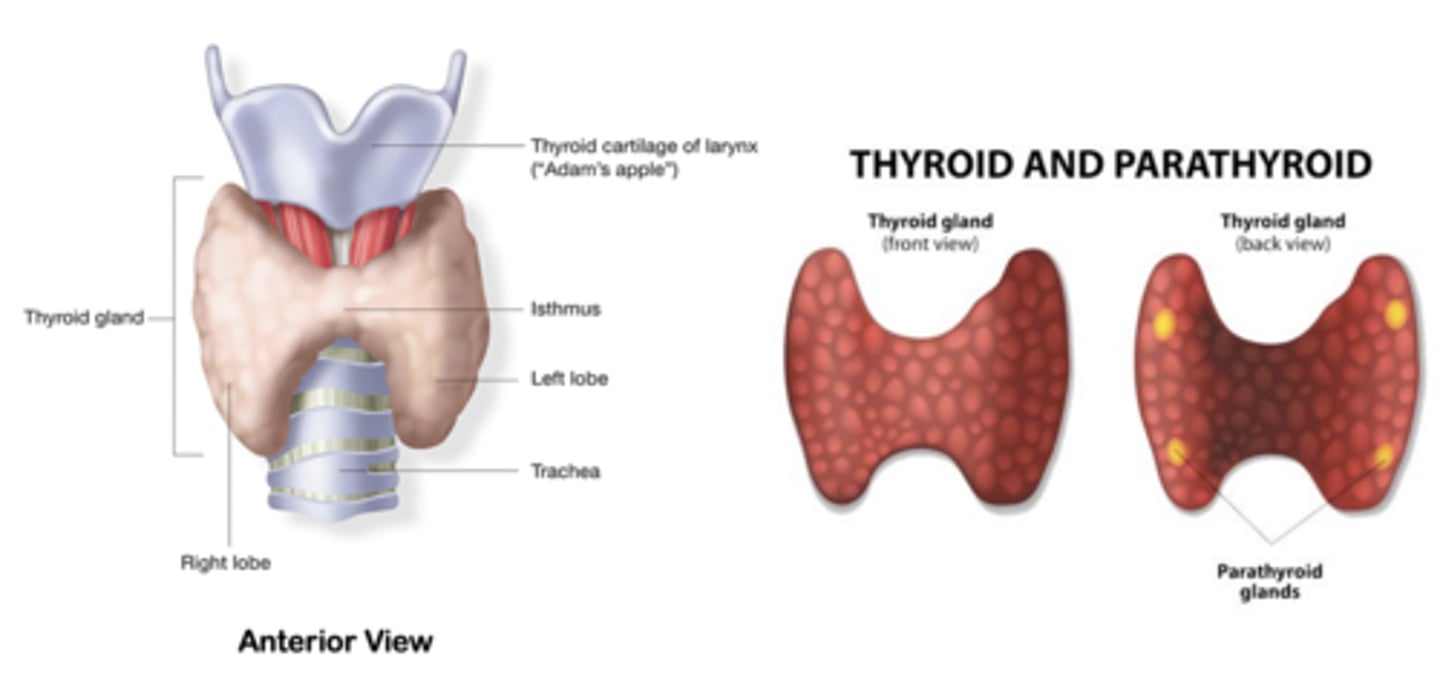
thyroid gland
is a butterfly-shaped organ located in the base of your neck
main function is the synthesis and storage of thyroid hormone
Thyroid hormones
circulate throughout the body bound to proteins- thyroid-binding globulin (TBG)
bind to their receptors, expressed in virtually all tissues and affect multiple cellular events
Genomic effects
Effects mediated primarily by the transcriptional regulation of target gene
Nongenomic effects
stimulations of activity of Ca2+ ATPase at the plasma membrane increasing oxygen uptake of the cells and the sarcoplasmic reticulum needed for cellular metabolism
THYROID HORMONE TRANSPORT AND CLEARANCE IN BLOOD
Circulating T4 - 90-95% - t1/2 = 6-8 d
Circulating T3 - 5% (1/100 of T4), t1/2 = 3-4 d
T4 and T3 are bound tightly to TBG - T4 also binds albumin and transthyretin
0.03% T4 free and bioactive compared to 0.3% T3
decrease levels of free hormone/drug
Drugs that increase thyroid binding globulin (TBG) binding: e.g., estrogens and opiates are going to ....
increase levels of free hormone/drug
Drugs that decrease TBG binding: e.g., glucocorticoids, androgens, aspirin and anti-seizure medications are going to ...
Steps in hormone synthesis and secretion
1. Iodide trapping (Iodide is the ion state of iodine)
2. Organification reaction(Iodination of thyroglobulin (Tg))
3. Coupling reaction (conjugation of monoiodotyrosine (MIT) and diiodotyrosine (DIT))
4. Hormone release (T4 and T3)

symptoms of hypothyroidism
Enlarged thyroid - goiter
Fatigue
Weight gain, inability to lose weight
A puffy-looking face
Primary Hypothyroidism
Low free T4, low or sometimes normal T3
High TSH
In utero - severe mental retardation or cretinism
In adults: -
-- Hashimoto disease – autoimmune
-- Causes might also include radioactive iodine therapy or surgery for an overactive thyroid
Secondary Hypothyroidism
Low T4 and T3 and TSH
-- Pituitary failure Thyroid gland functions well, but the pituitary gland doesn't stimulate the thyroid to produce more hormones.
-- The hypothalamus causing secondary hypothyroidism - The brain does not stimulate the gland for more hormone production.
Treatment: levothyroxine (T4)
Myxedema Coma
Rare life-threatening clinical condition in patients with longstanding severe untreated hypothyroidism. Early diagnosis, rapid administration, IV administration of levothyroxine and adequate supportive measures are essential for a successful outcome (e.g., IV hydrocortisone to address adrenal insufficiency, O2 therapy, fluid management to correct dehydration, warm blanket). The prognosis, however, remains poor.
-- Medical emergency - Extreme prolonged hypothyroidism
-- Elderly in winter, Infection, congestive heart failure can precipitate emergency
-- Mortality up to 60%.
•Features: hypothermia, respiratory depression, coma -Test plasma T4/TSH
-- Therapy: supportive care, ventilation, warming, intravenous steroids for
coexisting decreased adrenal reserve, thyroxine therapy with loading dose
Usually, a precipitating event disrupts homeostasis which is maintained in hypothyroid patients by a number of neurovascular adaptations:
-- chronic peripheral vasoconstriction
-- diastolic hypertension
-- diminished blood volume, to preserve a normal body core temperature.
ACT IMMEDIATELY
Hypothyroidism in Pregnancy
1. Pregnancy may exacerbate or unmask disease in patients with
preexisting autoimmune disease or living with iodine deficiency
due to increased estrogens increasing serum Thyroxine- binding globulin (TBG).
2. May increase miscarriage, preterm delivery, produce developmental delay.
Treatment : levothyroxine with regular monitoring with blood tests to ensure dosage is correct.
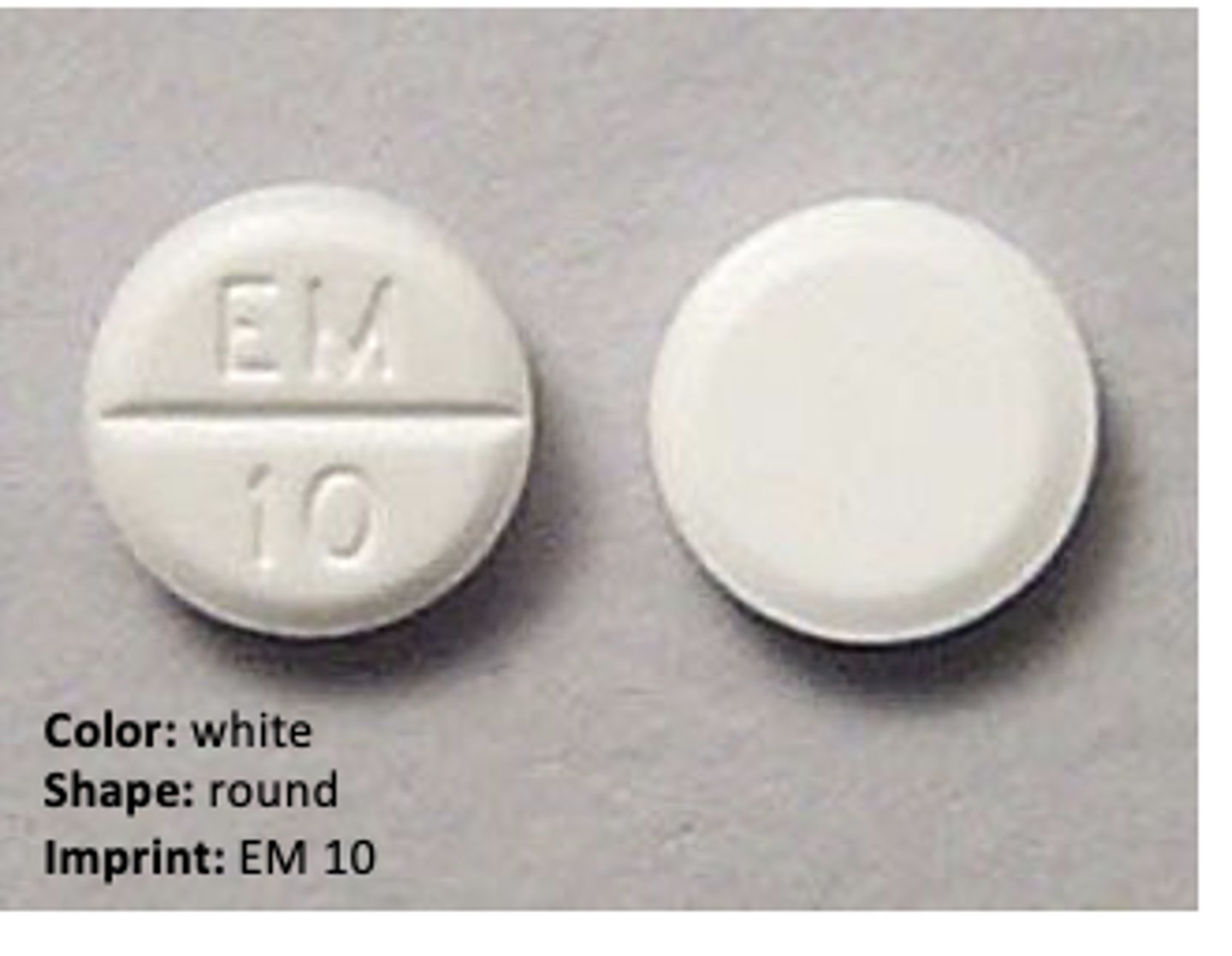
Levothyroxine (Synthroid)
Thyroid Replacement Therapy
is used to treat an underactive thyroid gland (hypothyroidism).
Used to treat pituitary failures, Hashimoto disease
Adverse effects rare unless excessive doses are taken
Thyroid Hormone Receptor
Nuclear receptor
Function as molecular switches in response to hormone binding
Can activate or repress gene transcription thereby effecting protein expression
Unoccupied thyroid hormone receptors are bound to DNA thyroid hormone response element (TRE)
Binding of the hormone to its receptor leads a confirmational change and modulates transcriptional regulation of target gene

Levothyroxine
Drug-Drug Interactions
Estrogen: Increase thyroxine-binding globulin (TBg) thereby decreasing free T4/T3
Barbiturates: Increases hepatic metabolism of levothyroxine
T4/T3: Increase receptor responsive of anticoagulants and tricyclic antidepressants
Increases receptor expression of vasopressors and sympathomimetics
Contraindications:
Patients with heart disease, diabetes, adrenal insufficiency and treatment for obesity
Hyperthyroidism
excessive thyroid function

Symptoms of Hyperthyroidism
Goiter
Anxiety
Weight loss
Larger eyes
secondary hyperthyroidism
High TSH
High T4 and t3
Increased thyroid hormone release by the thyroid gland in response to elevated TSH levels TSH-secreting pituitary adenomas
Treatment: methimazole, propylthiouracil
Graves disease autoimmune
TSH receptor stimulation by immunoglobulin G
Excessive T3 and T4 production
Protruding eyeballs exophthalmos
Thyroid storm
uncommon but is a crisis or life-threatening condition characterized by an exaggeration of the usual physiologic response seen in hyperthyroidism.
* High fever
* Tachycardia
* Nausea/vomiting
* Irregular heartbeat
* Acute heart failure
* Confusion/disorientation
Usually precipitated by concurrent medical problems (infections, stress, surgery, trauma, heart disease, diabetic ketoacidosis).
Treatment:
- antipyretics,
- large dose (200-400 mg) propylthiouracil (PTU) because of additional action of blocking peripheral T4 conversion
- b-blockers (propranalol) to counteract effects on SNS and heart
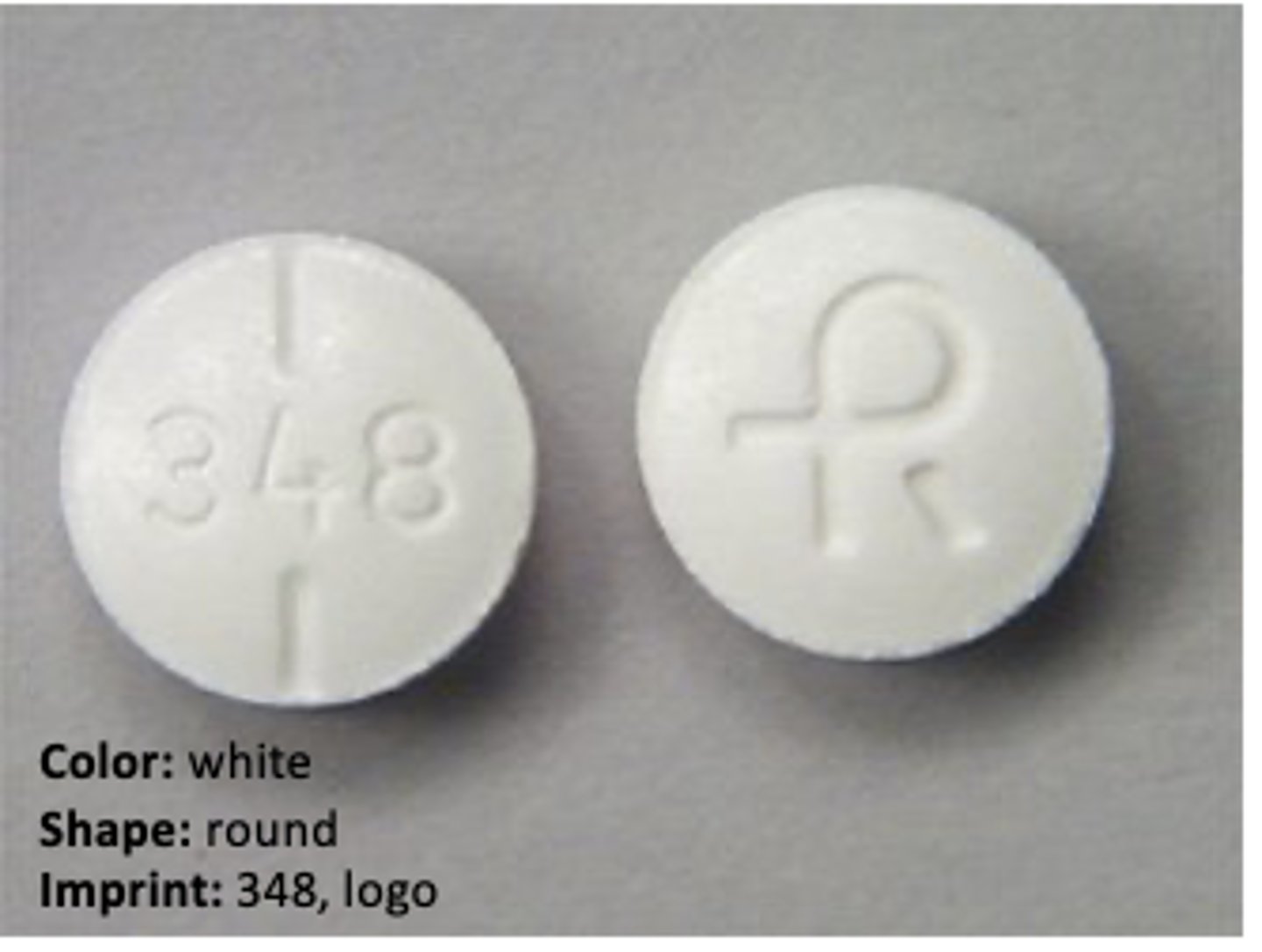
methimazole, (Tapazole) - antithyroid drug
Used to treat hyperthyroidism (overactive thyroid) and it is also used before thyroid surgery or radioactive iodine treatment
Prevents the thyroid gland from producing too much thyroid hormone. Inhibits the actions of thyroid peroxidase inhibiting organfication.
Using ____________ during pregnancy could harm the unborn baby. Methimazole can pass into breast milk and may harm a nursing baby. You should not breast-feed while using this medicine
propylthiouracil (PTU), (Propacil) - antithyroid drugs
Drug of choice in the treatment of thyroid storm;
Inhibits actions of thyroid peroxidase thereby inhibiting iodine organification and partially inhibits the peripheral deiodination of T4 to T3
There is positive evidence of human fetal risk during pregnancy.
perchlorate - Ionic Inhibitor - antithyroid drugs
2nd line treatment, used in wwii
limited use, low dose may be considered as a second-line treatment
Inhibits the sodium-iodide symporter (NIS). Blocks the entrance of iodide into the thyroid and inhibits the organification of iodine
Iodine - SSKI (potassium iodide saturated solution) - antithyroid drugs
Reduces the synthesis and secretion of thyroid hormones
Autoregulatory phenomenon inhibits organification (Wollf-Chaikoff effect)
Protects the thyroid from radioactive iodine fallout
131 I radioactive Iodine - antithyroid drugs
Destroys hyper-functioning thyroid tissue
Effective for permanent treatment of Graves disease and toxic goiter
Permanent cure to hyperthyroidism, results in permanent hypothyroidism and lifelong requirement for levothyroxine replacement
Euthyroid Sick Syndrome
Levels of T3 and/or T4 are abnormal, but the thyroid gland does not appear to be dysfunctional
A state of adaptation or dysregulation of thyrotropic feedback control
Caused by increased circulating cytokines and other inflammation mediators
Starvation, sepsis, surgery, myocardial infarction, bone marrow transplantation
Mediators Inhibit the thyroid axis at multiple levels, including the pituitary, the thyroid , transport proteins, peripheral tissues
Treatment: Primary goal is to treat underlying medical condition (e.g., infection or malnutrition. Use of thyroid hormone is controversial will depend on attending physician
KNOW THIS
KNOW THIS

Secondary Hypothyroidism
Pituitary Failure
what does low T4 and low TSH mean
Primary hypothyroidism
Hashimoto's thyroiditis
what does low T4 and high TSH mean
Primary Hyperthyroidism
Grave's disease (autonomous secretion of target gland hormone)
what does high T4 and low TSH mean
Secondary Hyperthyroidism
Pituitary tumor
what does high T4 and high TSH mean
Goiter
Excessive Thyroid Function or Lack of Iodine
Treatment: depends on the underlying cause
levothyroxine if caused by underactive thyroid
methimazole or propylthiouracil (PTU) if overactive thyroid
Corticosteroid medication if goiter is caused by inflammation

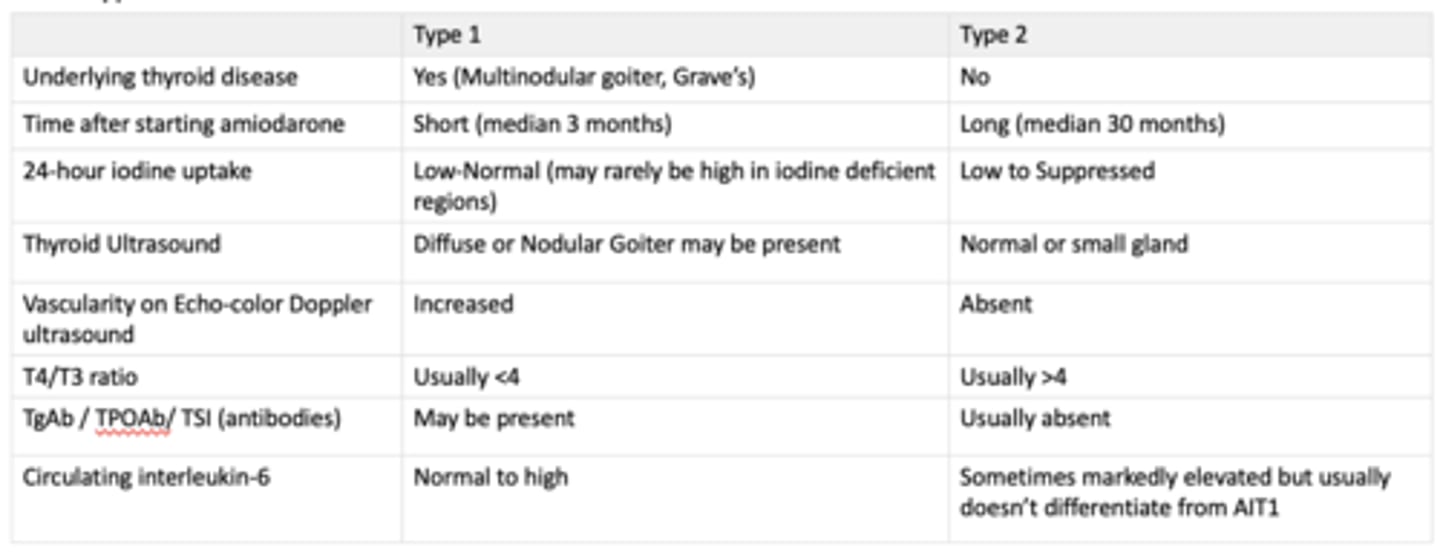
Amiodarone
is a class III antiarrhythmic agent commonly used to treat Afib
Amiodarone-induced hypothyroidism (AIH)
Amiodarone-induced Thyrotoxicosis (AIT)
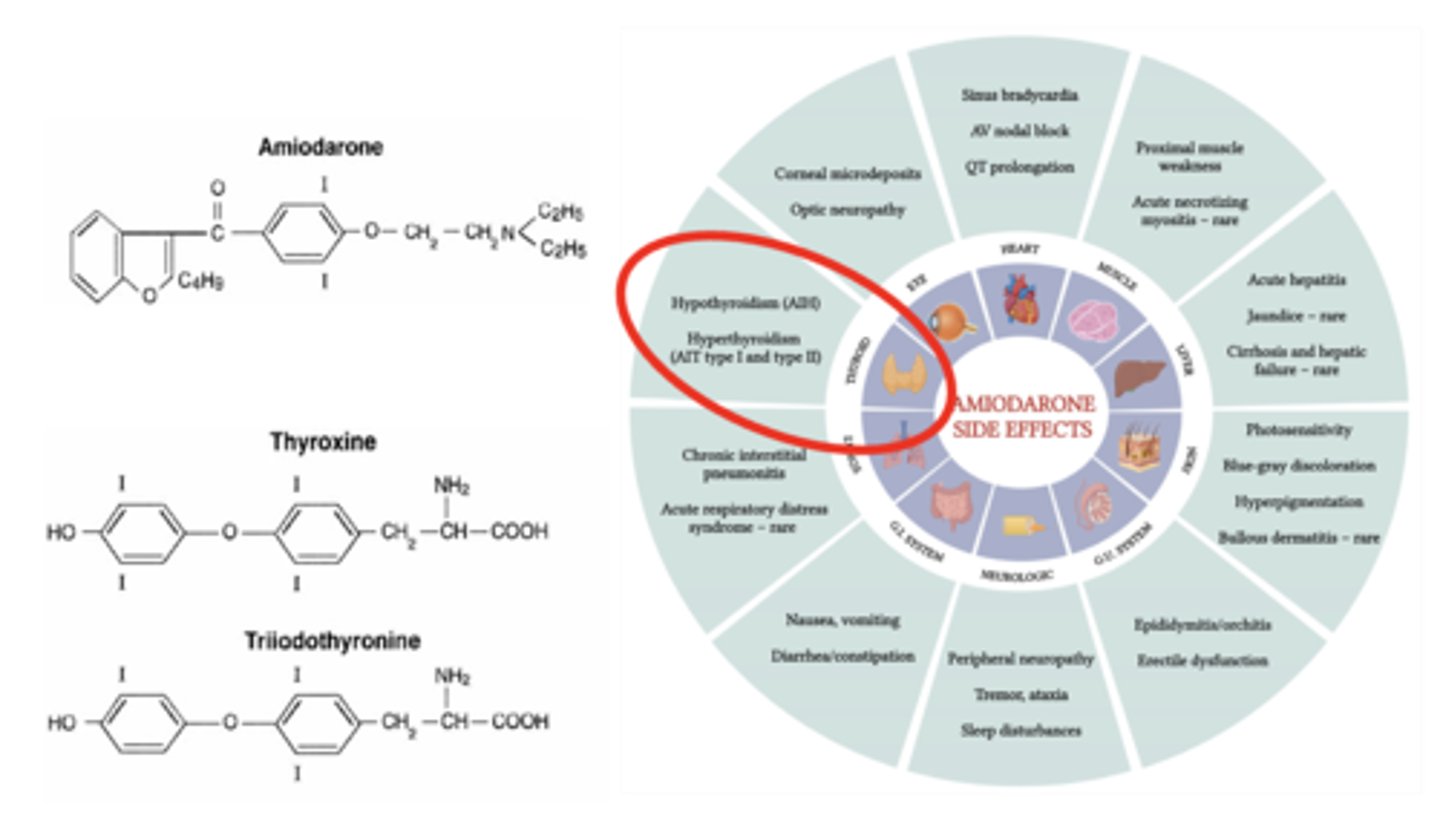
Intrinsic drug effects of amiodarone
Amiodarone-induced hypothyroidism (AIH)
- inhibits thyroxine (T4) conversion to T3 and rT3 thus decreasing triiodothyronine (T3) production
- (and particularly the metabolite desethylamiodarone) blocks T3-receptor binding to nuclear receptors and decreases expression of some thyroid hormone-related genes
- may have a direct toxic effect on thyroid follicular cells, which results in a destructive thyroiditis
Effects due to iodine of amiodarone
Amiodarone-induced hypothyroidism (AIH)
- contains a large proportion of iodine: When intrathyroidal iodine concentrations reach a critical high level, iodine transport and thyroid hormone synthesis are transiently inhibited until intrathyroidal iodine stores return to normal levels (the Wolff-Chaikoff effect).
- contains two iodine atoms. It is estimated that amiodarone metabolism in the liver releases approximately 3 mg of inorganic iodine into the systemic circulation per 100 mg of amiodarone ingested. The average iodine content in a typical American diet is approximately 0.3 mg/day. Thus, 6 mg of iodine associated with a 200 mg dose of amiodarone markedly increases the daily iodine load
Treatment: Levothyroxine
Amiodarone-induced Thyrotoxicosis (AIT)
manifests with clinical signs indistinguishable from spontaneous hyperthyroidism
Treatment:
Mild AIT may spontaneously resolve in about 20% of the cases.
Type 1 AIT should be treated with high doses of methimazole (20-60 mg/day) or propylthiouracil (400-600 mg/day) to block the synthesis of thyroid hormones. The response to methimazole or propylthiouracil is often modest due to the high iodine levels in patients taking amiodarone. In selected patients, potassium perchlorate can also be used to increase sensitivity of the gland to methimazole or propylthiouracil by blocking iodine uptake in the thyroid.
Type 2 AIT can be treated with prednisone, starting with an initial dose of 0.5-0.7 mg/kg body weight per day and the treatment is generally continued for three months. Methimazole and propylthiouracil are generally not useful in Type 2 AIT.