02 - Illness, disease, pain, and suffering
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
58 Terms
Asymmetry of information
• The recipient of care cannot judge the effectiveness of care
articulate body
the ability of providers to FEEL their patient's experience and acknowledge the vulnerability and difference in bodies, including their own
Imagination
• Details of a patient’s world are revealed through the stories they tell
• Act of telling and listening to stories depends on imagination
When clinicians talk about purpose and meaning in the life of an individual
no longer science but imaginative work of arts and humanities
Storytelling for patients
• For patients, storytelling is a matter of life and death
• Illness stories must be at the centre of clinical encounters
medical decision making
the decisions made in a medical setting pertaining to a patient's care and health, often affected by the person's abiliity to imagine and engage in an embodied process
embodied, relational process
give a tangible or visible form to care, relating it back to the patient and the provider, rather than seeing it as transactional or idealized. Care should be rooted in daily practices that respond to and attune to the changing needs of an unpredictable body-mind
Sociological imagination in health
• Acknowledges the ways an individual’s biography and health emerge from historical processes that occur within larger social and economic contexts
• This imaginative reach allows our perceptions to move past narrow focus on individual biological function into multidimensional lived experiences of human beings
• How clinicians imagine human worth and dignity has great consequences!
Fractured self
• Patients struggle for language to articulate their lives
• Difficult to give an account of one’s self amidst the disorienting experience of illness and disability
• This may “fracture the self” (p. 113)
• Ordinary language may be insufficient to describe this suffering
• Need a voice beyond words, a new language
suffering
the state of undergoing distress, pain, or hardship
Imagination in Clinical Practice
• Imaginations of clinicians need to be trained to recognize metaphor
• Begin to hear in patients’ stories “the main points of metaphor: the
achievement of intimacy”
• Exchange: maker of metaphor offers a concealed invitation that the
listening interprets and accepts → constitutive of community
Imagination and Awareness
• Imagination allows the mind to be aware of reality that exists at the
margin of the mind’s current experience
• Expands what is available to rational thought and language we use to
express thought and feeling
• Reality will always be larger than our language
Imagination and Discovery
• Need imagination for leaps of discovery
• Language of all kinds (words, painting, music, drama, dance, etc.) help
the imagination
• Francis Bacon:
• The excellent question is half of wisdom
• (The source of the excellent question is imagination)
• Imagination is the origin of any hypothesis that leads to discovery
• Apprehends invisible pieces that make a whole from pieces à
meaningful connections we haven’t seen before
Imagination and Rationality
• Imagination and power of rationality are always working together
• All great discovery works in this way
• “Art renders the familiar world strange” (p. 115)
Strangeness of disembodied medicine
• Contemporary medicine is disembodied
• Primary articulations (accounts) of the body are lab values, images, reports
• Medicine’s articulations of the body are held to be true, objective, and primary
• But multiple articulations of lived body by patients are seen as secondary and “subjective”
• Rather than rejecting the hierarchies of medicine, we can supplement it
Fractures
• Body is the ground of our history, memory, trauma, desire
• Illness fractures this body
• Fractures can be reintegrated, even if physical condition does not
leave (and vice versa!)
• “This is why a cure may not necessarily heal, and healing does not
depend on a cure” (p. 116)
articulations
explanations, presentations, accounts (of the body)
disembodied
the disconnect from the body due to being overly objectified
Embodiment
• Requires the integration of all these dimensions in the human being
• Ancient wisdom: we are not born fully human, but become so as we
cultivate ourselves and our relations with others
• Recognize that the physical and metaphysical are interwoven and
inseparable
• Goes against biomedical materiality
• Excludes poetic materiality:
poetic materiality:
way of accounting for how imagination wraps around and shapes our experience across personal, social, historic dimensions
Enactivism
• Active, interchanging relationship between observer and observed
• Human cognition emerges dynamic interaction and co-creation
between perceiver and environment
• “Enactivism” holds that observers actively shape the worlds they
perceived à the world is enacted in this relation
Care as a relational embodied process
• Medical education needs to cultivate an understanding of care as
something neither idealized nor transactional
• Instead, “care is a process rooted in daily practices that attempt to respond and attune to the changing needs of unpredictable bodyminds” (pp. 116-117)
• This is deeply imaginative!
• Medical education must incorporate practices from arts and
humanities à deeper view of what the body is, what illness is, what a
person is
• Artistic inquiry is a practice that asks questions and makes discoveries
through making à giving form to imagination
• Embodied artistic inquiry helps clinicians gain “articulated bodies” à
bodies that have learned to be affective
• Gives form and voice to questions whose answers can never be
complete
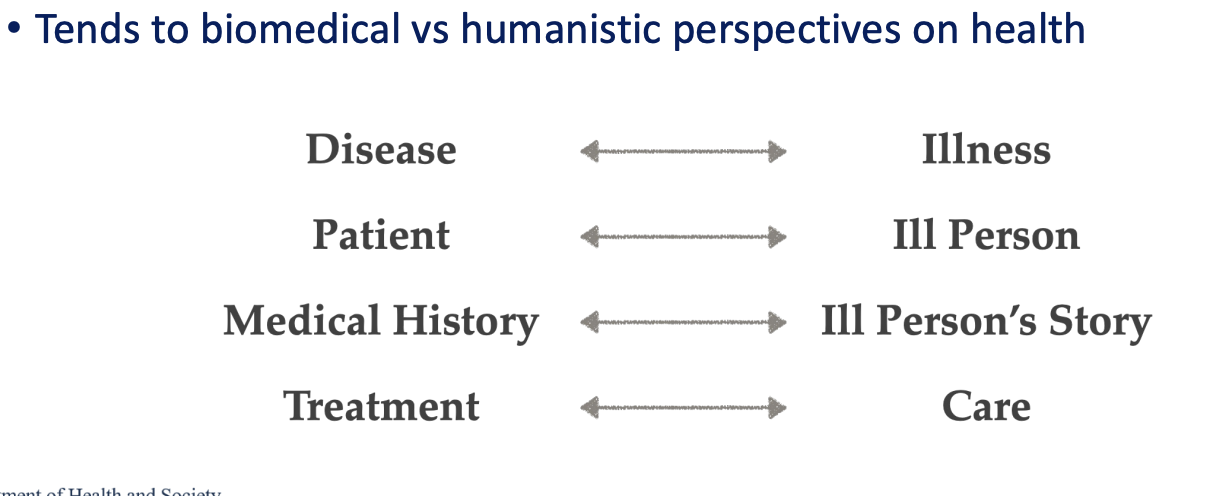
• Art Frank: Four key distinctions
• Disease vs illness
• Patient vs ill person
• Medical history vs ill person’s story
• Treatment vs care
Disease vs illness
• Disease: Condition of the body reducible to biochemistry (“bare disease”)
• Illness: An experience that “involves a biography, a reflective consciousness, multiple relationships, and institutions”
Patient vs ill person
• Patient: Identity imposed upon a person by medical/ health institutions
• Ill person: “a patient only some of the time and…remains many other things as well” means that illness does not erase the rest of who they are.
Medical history vs ill person’s story
• Medical history: An understanding of the patient in terms of the nature of disease. “Set parameters” of relevant information that create “illusion” of knowing the ill person
• Ill person’s story: The medical patient becomes delimited by his or her history. If the storytelling is truly a relationship, the [ill person] storyteller is invited to reinvent his or her own character… what the storyteller needs the listener to know about him or herself, to appreciate that self.
Treatment vs care
Treatment
• “Service” with monetary value
• Instrumental; requires technical expertise
• Defined boundaries between bodies giving and
receiving treatment
• “Untroubled by its use of power as a resource”
Care
• “Gift”
• Involves emotion as well as cognition
• Relational nature of giver and receiver
• “Sensitive to asymmetries of power”
difference between treatment provider and care giver
The treatment provider acts through precision and control — their body is a tool for technical work (steady hands, medical procedures).
The caregiver engages with feeling — their body is present and responsive, sensing the other’s pain while maintaining enough emotional distance to stay effective.
→ This balance is key: too detached = cold; too emotionally involved = overwhelmed (“engulfed”).
“fundamental asymmetry”
Tensions
fundamental asymmetry, conflict/strain between ideas
Instrumental value
a means to an end, doing it to achieve another goal
Intrinsic Value
something inherently valuable, there's value in in of itself
Difficulty in representing depression?
internality
Depression is internal, invisible, and deeply personal.
Difficulty in representing pain?
• Physical and psychic
Pain can be both physical (bodily suffering) and psychic (emotional or mental anguish).
→ These two forms often overlap — emotional trauma can manifest physically, and vice versa.
Why are medical images “never simply unmediated”?
Because they don’t show the body directly — they’re shaped by technology, interpretation, and perspective. Every image is a constructed view of the body, not pure reality.
Mediation
having something in between. In interpretation, it is mediated by the knowledge and experience of the provider who is looking at the image
How do cultural influences shape medical images?
Cultural assumptions affect what is imaged, how it’s labeled, and what meanings are attached.
What is the “imaginative leap” in medical imaging?
Clinicians must imagine the patient’s experience of pain or illness — because the image alone can’t show suffering.
→ Understanding requires empathy and imagination, not just data.
What is ‘representation’?
• Literary critic WJT Mitchell describes representation as the use of
signs that stand in for or take the place of something else
• Representation refers to the use of (X) to:
• Look like or resemble something or someone
• Stand in for something or someone
• Present a second time; to re-present
The means of literary representation is
language
The means of visual representation is the
image or icon
Medical images generally assumed to be ___ RATHER THAB __
Mimetic (content directly represented/ shown; fixed meaning)
Diagetic (told, recounted, interpreted)
Medical sciences claim to represent the body objectively
Medical sciences claim to represent the body objectively through brain imaging and the neurosciences or evolutionary biology or psychology, approaches that offer a single, unambiguous pathway without much attention to who sees and what is claimed to be seen”
Medical images claim to mirror aspects of the body
Medical images claim to mirror aspects of the body, whether imaged externally by photographs or internally by x-rays or fMRIs, and thus they claim to represent bodies as they actually are
key to understanding communication of pain
• Imaging – and imagining – human body as something to be seen, turned insight out, revealed to sight is key to understanding communication of pain
Pain
• Pain is inherently subjective
• There is no way to comprehensively measure or ‘see’ objective reality of pain
communicating pain relies
communicating pain relies on patient’s account (narrative)
On the other hand, the listener (clinician) will be similarly molded or influenced to receive a story of pain
gerunds
“nouny” verbs ending with –ing
The McGill Pain Index
Clinical tool developed at McGill University (1971) to evaluate a
person experiencing significant pain
• What does your pain feel like?
• How does your pain change with time?
• How strong is your pain?
Provides a list of gerunds as a way of articulating pain
After completing the questionnaire, users will have selected seven words that best describe their pain
Facing pain
Pain scales attempt to capture the ‘face of pain’ as objective reality
“whatever the motivation of the sufferer and, perhaps, whatever his or her cultural location” (p. 175)
Drive to universality is important
Certain groups of people throughout history have been understood to have different thresholds of pain
Women, people of colour, people with intellectual disabilities, animals
Photographing pain (late 19th c.)
• Charles Darwin’s Expression of Emotion in Man and Animals (1872)
• Darwin argued that emotions are mimetic (unmediated) physical expressions of experience
• Use of photographs to prove continuity of pain expression across species
Existential suffering
• Deep psychological and emotional distress when confronting
meaning, purpose and value of life in face of mortality
• Fears of the unknown, loss of identity, perceived pointlessness of life
• NOT = pain
• We can suffer even if there is no pain (e.g., grief) and vice versa
• Nociception =
detection of a painful stimulus, physical phenomenon
Suffering
the specific distress that occurs when persons feel their intactness and integrity as persons are threatened or disintegrating, and continues until the threat is gone or intactness or integrity are restored… Bodies do no suffer; only persons suffer.
Subjective knowledge and suffering
• Objective knowledge is needed in the
practice of medicine
• But good clinicians need subjective
information to address suffering, specifically
• “to hear, feel, see, and smell everything
Suffering occurs because the
integrity of the person is threatened
Loss of purpose and meaning
• All suffering involves loss of or profound change in
meaning and purpose of one’s life
• Purpose of being “me”
• Every moment, every movement, thought, action are
expression of purpose
• “My purpose creates me and creates my world”
• Loss of purpose is a breakdown of the self
Integrity of the person
the sense of self - if broken or damaged, by illness or trauma alike, can threaten the person's well being