pathology everything
1/498
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
499 Terms
what is pathology?
the study of disease by scientific means, elucidating its causes and effects
branch of medical science that investigates the causes, nature and effects of diseases - plays a crucial role in advancing our understanding of diseases, improving diagnostic accuracy, and facilitating personalised patient care
pathos = disease
logos = discourse
what does pathology involve?
study of abnormal changes in cells, tissues, organs and bodily fluids, aiming to understand the underlying mechanisms of disease processes
analysis of specimens collected through biopsies, surgeries or autopsies to diagnose diseases, determine their progression, and guide treatment decisions
use of various techniques, including micropsy, molecular testing and imaging, to identify cellular, molecular and gross abnormalities and provide insights into disease development and management.
what is the definition of diagnosis?
determination of the exact nature of disease
what is a biopsy?
sample of body tissue during life to aid in diagnosis
what is an autopsy?
aka necropsy, examination of body/organs after death to aid in determination of the cause of death
what is anatomical pathology and the two disciplines of anatomical pathology?
detecting structural abnormalities in tissues and cells
naked eye/microscopic examination of biopsy/autopsy material
excision/surgical specimens → histopathology
exfoliative/needle specimens → cytology
what is the pathology discipline histopathology/histology?
excision/surgical specimens → histopathology
cutting a piece of tissue out
ie. suspicious mole
assessing microscopic anatomy of tissue - what is one cell doing to the other tissue?
is the abnormal tissue doing to the normal tissue?
what is the pathology discipline cytology/cytopathology?
exfoliative/needle specimens → cytology
scrapings of tissue cells
ie. cervix
looking at cells
what is exfoliative biopsy as an example of cytology?
examination of secretions, tissue scraping for detection of cancerous cells
ie. cervix, lung, stomach, bladder cancers
what is fine needle aspiration as an example of cytology?
extracting cells from a suspected mass
ie. breast, lymph node, thyroid
what is the pathology discipline haematology?
detection of blood and bone marrow abnormalities
red blood cell, white blood cell, platelet disorders
anomalies in blood cell profile: number, size, shape, structure
clotting diseases and effects of other diseases on the blood
cross matching blood for compatible transfusions
what is the pathology discipline biochemistry?
detection of abnormalities in body chemistry
metabolism analysed for disease (ie. levels of glucose, urea, electrolytes, enzymes, hormones)
analysis of blood, urine, CSF other bodily fluids
protein (albumin → oedema), lipid (cholesterol → heart disease, atherosclerosis), carbohydrate (glucose → diabetes) levels
blood or urine testing, cerebrospinal fluid
what is the pathology discipline microbiology?
detection of infectious disease
analysis of blood, urine, faeces, secretions (vaginal, genital)
respiratory swabs for diagnosis of COVID
bacteria, virus, fungi, parasites, sample of normal flora or exogenous acquired infections from environment, animal sources
HIV → AIDS
SARS COV 2 → COVID 19
virus causes illness
what is the pathology discipline immunoserology?
can be considered subdivision of microbiology
detection of immune disease/status and infectious disease
detecting HIV positive
analysis of blood and other bodily fluids for antigen/antibody reactions
ELISA test
what is the pathology discipline molecular pathology?
can be under biochemistry, microbiology, cytopathology (HPV)
detection of abnormalities at molecular level (gene and gene products)
analysis of very small amounts of tissues and bodily fluids
PCR (polymerase chain reaction) machine, amplifying genetic material/DNA/nucleic acids
checking for viral DNA sequences
infection unable to detect via blood/urine/culture → chlamydia, gonorrhoea
what is the pathology discipline medical genetics?
detection of inherited disease
prenatal diagnosis
amniocentesis (amniotic fluid containing foetal cells), chorionic villus sampling (placenta)
chromosome spread karyotype
what is the discipline medical radiations (radiography, nuclear medicine, radiation therapy)?
not considered a pathology discipline
aids in diagnosis and/or treatment of disease
x radiation
computed tomography
magnetic resonance imaging
ultrasound
SPECT, PET, nuclear medicine scans
provides details in abnormalities regarding structures of the body
detecting changes in function of body
what are symptoms?
complaints that the patient is aware of
weakness, pain, fever, headache, SOB
what are signs?
abnormalities associated with a disease that the patient is not usually aware of
retinal bleeding caused by high blood pressure
crackling lung sounds, heart sounds0
what is a differential diagnosis?
clinician lists possible diseases that may cause the symptoms and signs
what is a presumptive diagnosis?
an initial diagnosis is made
assumed most likely diagnosis for the patient
the most likely diagnosis
tests still required to rule out other differential diagnoses
what is a definitive diagnosis?
following test results, a final diagnosis is made
after ruling out all other differential diagnoses
what is a prognosis?
a forecast is made on the probable course and outcome of the disease
what is remission?
state of absence of disease activity in patients with a chronic illness, with the possibility of return
after cancer has been removed they are in remission
what is relapse?
state of renewed disease activity following the end of a remission
if cancer returns after remission, they have relapsed
how can disease can be classified and what do they mean? (2)
by an eponymous term
giving the disease the name of the discoverer
ie. Bright’s disease
by a descriptive term
ie. glomerulonephritis
related to the kidney at the glomerular level
provides more information to the name
what is the definition of aetiology?
the cause of a disease
ie. Staph. aureus causing bronchopneumonia
what is the definition of pathogenesis?
how the aetiology brings about the disease
the ‘course’ of the disease
how can diseases be grouped? (2)
genetically determined
acquired
what is a genetically determined disease?
due to gene defects/DNA anomalies
may be influenced by environment
present at birth
may be brought about by abnormal genes that are inherited, or by abnormal expression of normal genes
what are the types of genetically determined diseases? (4)
cytogenic disorders
Mendelian disorders
multifactorial inheritance disorders
congenital malformations
what is a cytogenic disorder of genetically determined disease?
chromosomal defects (structure/number)
down’s syndrome
47 chromosomes/cell
47, XY+21
Klinefelter’s syndrome
47, XXY - male but with feminised features
what is a Mendelian disorder of genetically determined disease?
due to gene defects
ie. Phenylketonuria (PKU)
enzyme gene defect leads to abnormal metabolism of phenylalanine
what is a multi factorial inheritance disorder of genetically determined disease?
often involve many genes (polygenic)
may have an environmental influence
ie. hypertension
a set of genes predisposes one to hypertension
environmental factors (salt, stress) can contribute
what is a congenital malformation of genetically determined disease?
DNA expression errors ie. heart defects
may have an environmental cause
ie. thalidomide phocomelia - morning sickness drug interfering with development of limbs
ie. rubella virus infection of mother - causing deafness and blindness of baby
gross anatomical defects
what is acquired disease?
due to environmental factors
due to environmental agents interacting with the tissues of the body and causing cell
injury.
more common than genetic diseases
what are the environmental factors that can contribute to acquired disease? (3)
aetiology
causative agent
predisposing factors
these make one more likely to develop the disease
ie. cigarette smoking
contributing factors
make one develop the disease more severely
ie. malnutrition
what are the pathological stimuli that can cause acquired disease? (8)
physical agents
chemical agents
biological/infective agents
immune factors
deficiency or excess factors
psychogenic factors
iatrogenic factors
idiopathic factors
what are physical agents as a pathological stimuli that can cause acquired disease?
trauma, heat, cold, radiation (X rays, UV rays)
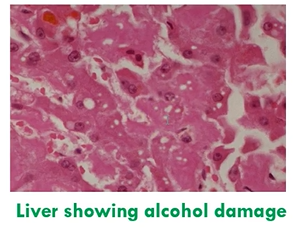
what are chemical agents as a pathological stimuli that can cause acquired disease?
synthetic, naturally occurring chemicals
elements, compounds, toxins, poisons, free radicals
acid burn: chemical damage to tissue
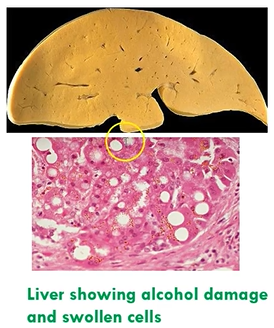
alcohol damaging liver, cirrhosis, stomach lining, ulcers, fatty change
what are biological/infective agents as a pathological stimuli that can cause acquired disease?
worms, protozoa, fungi, bacteria, viruses leading to variety of lesions
respiratory, gastrointestinal, urinary, skin, genital infections
facial herpes (viral infection)
what are immune factors as a pathological stimuli that can cause acquired disease?
allergies/hypersensitivities, autoimmunity, immunodeficiency (ie. AIDS)
exaggerated immune responses
attacking self cells
allergy (hypersensitivity reaction) to mosquito bite
what are deficiency or excess factors as a pathological stimuli that can cause acquired disease?
deficiency or excess of vitamins, minerals, hormones, oxygen
Kwashiorkor - severe dietary protein deficiency - changes in skin, hair
excess oestrogen can lead to breast/uterine cancer
excess testosterone can lead to prostate cancer
decreased growth hormone - dwarfism
what are psychogenic factors as a pathological stimuli that can cause acquired disease?
caused by or greatly contributed to by patient’s psychological state
psychological factors acting as pathological stimuli
chronic peptic ulcer
stress contributes to its pathogenesis
chest pain, heart palpitations, high blood pressure
what are iatrogenic factors as a pathological stimuli that can cause acquired disease?
caused by medical/paramedical intervention (maltreatment, wrong dosage)
aspirin overdose → leads to haemorrhage
penicillin when patient is allergic → anaphylaxis
what are idiopathic factors as a pathological stimuli that can cause acquired disease?
of unknown cause
may have multifactorial aetiology
ie. sarcoidosis
some brain tumours
what is injury, and how can it be categorised? (4)
injury is any stress upon tissue or a cell that disrupts its normal structure and function
sublethal or lethal, mild or severe
this results in a pathological process in tissue, causing disease
any stress that acts on the body and causes disruption to the normal physiological processes that
are active in tissues. This results in an abnormal, pathological process that may disrupt normal anatomy
and brings about disease
what is trauma?
trauma is an injury due to mechanical/physical agent
not biological or chemical
trauma: physical disruption to tissue
what are parenchymal cells?
parenchymal cells (specialised cells of the organ)
parenchymal cells gives organ specific function
the heart, cardiocytes
the brain, neurons
what occurs to parenchymal cells during sublethal (mild) injury? (5)
sublethal (reactive changes)
hydropic change
fatty change
glycogen depletion
decreased protein synthesis
autophagy
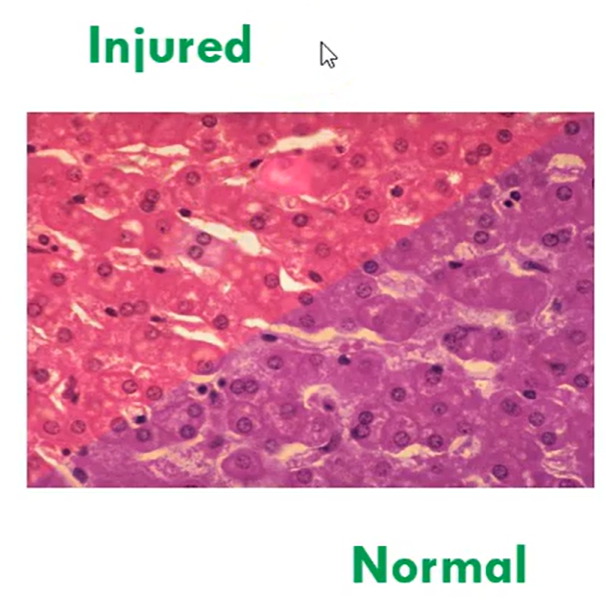
what is hydropic change occurring to parenchymal cells during sublethal (mild) injury?
membrane ion pumps failing
cells accumulate water and electrolytes - cloudy swelling
there is still nuclei present - cells have not died
reversible if stimulus is removed

what is fatty change occurring to parenchymal cells during sublethal (mild) injury?
smooth endoplasmic reticulum damaged
fat metabolism stops, cytoplasm accumulates fat droplets - signet ring
nucleus pushed to the side - peripheral
reversible
what is glycogen depletion occurring to parenchymal cells during sublethal (mild) injury?
mitochondria damaged
cells begin to produce more ATP anaerobically and demonstrate loss of glycogen - using glycogen stores
periodic acid Schiff PAS staining method used to detect glycogen
reversible

what is decreased protein synthesis occurring to parenchymal cells during sublethal (mild) injury?
ribosomes, granular/rough endoplasmic reticulum damaged
protein synthesis stops
cytoplasm stains more eosinophilic (ie. more pink)
reversible
what is autophagy occurring to parenchymal cells during sublethal (mild) injury?
lysosomes damaged
lytic enzymes released in pockets of cytoplasm
vacuolation seen as a result of limited digestion of cytoplasm
bubbles in cytoplasm
reversible
what are connective tissue cells and what occurs to them during sublethal (mild) injury?
connective tissue cells (supporting cells of the organ) → acute or chronic inflammation
macrophages, fat cells, adipose, nerve cells
what occurs to parenchymal and connective tissue cells during lethal (severe) injury?
necrosis
what is necrosis?
death of cells while still part of living body
what is hypoxia?
mild injury, deficiency in the amount of oxygen reaching the tissues, partial occlusion
can cause angina pectoris in myocardium
what is anoxia?
severe injury, an absence of oxygen, complete occlusion
can cause myocardial infarction (heart attack)
what is the aetiology of myocardial infarction?
ischaemia (interrupted blood supply) due to blockage of end artery to myocardium
what is the pathogenesis of myocardial infarction?
acute anoxia to tissue
oxidative phosphorylation stops
anaerobic glycolysis generates ATP
membrane ion pumps start to fail, influx of H2O and electrolytes, cell swells
biochemical necrosis (point of irreversibility)
intracellular membrane rupture
.
a. autolysis: cytoplasm dissolves
b. coagulation: cytoplasm solidifieshistological necrosis ~= 8 hours
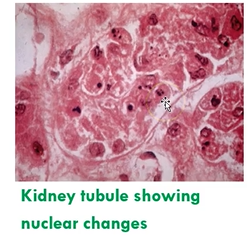
what are the nuclear changes seen in the process of necrosis, and what happens? (3)
pyknosis: nucleus shrinks and condenses
karyorrhexis: nucleus fragments
karyolysis: nuclear fragments dissolve away
how can a patient react to necrotic tissue? (4)
in vital organs such as heart (myocardial infarct), brain (stroke) → death may occur
if patient survives
inflammation seen around necrotic region and necrotic tissue removed by phagocytic cells
necrotic tissue replaced by scar tissue (ie. fibrosis, except in the brain where gliosis occurs)
calcium may deposit in necrotic tissues
dystrophic calcification, necrotic tissues only, normal blood calcium levels
metastatic calcification, both living and necrotic tissues, hypercalcaemia
what are the types of necrosis?
coagulative necrosis
colliquative (liquefactive) necrosis
a. occurs in the brain
b. occurs in suppuration (pus formation)caseous necrosis
haemorrhagic necrosis
gummatous necrosis
fat necrosis
a. enzymatic type
b. traumatic typefibrinoid necrosis
gangrenous necrosis
what is coagulative necrosis?
most common, occurs in solid organs
ie. heart, kidney, spleen, liver
due to ischaemia → coagulation of proteins (myocardial infarction)
what are the two types of colliquative (liquefactive) necrosis?
i. Occurs in the brain
due to autolysis progressing almost to completion with little coagulation
ischaemia → autolysis of cells (cerebral infarct - stroke)
ii. Occurs in suppuration (pus formation)
due to neutrophils lysing pyogenic bacteria and tissue, ie. heterolysis (not autolysis, not self-lysis of cells)
heterolysis of cells (abscess)
neutrophils lyse bacteria

what is caseous necrosis?
occurs in tuberculosis (infection with Mycobacterium tuberculosis)
due to type 4 hypersensitivity reaction and nature of bacterium
caseous necrosis of lung
appears like cottage cheese, very crumbly
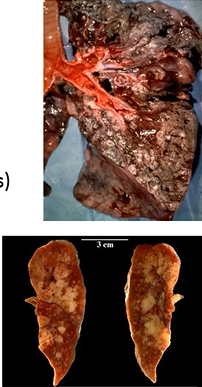
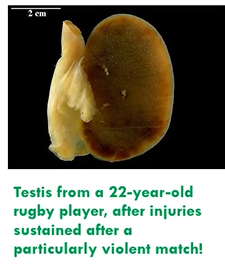
what is haemorrhagic necrosis?
result of ischaemia leading to necrotic tissue infiltrated with extravasated red blood cells
ie. lung infarct with blood supply still present or torsion of the testis
trickle of blood into infarcted area
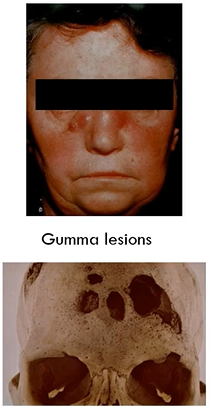
what is gummatous necrosis?
due to infection with Treponema pallidum
occurs in tertiary syphilis
especially in cardiovascular system and central nervous system
causes gumma lesions
variation of coagulative necrosis
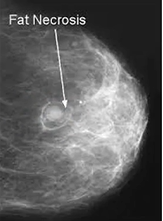
what are the two types of fat necrosis?
i. Enzymatic type
only occurs around pancreas
associated with adipose tissue injury and release of pancreatic lipases (ie. in alcoholics)
ii. Traumatic type
occurs when adipose tissue in any site is injured by trauma
ie. injury to breast tissue following surgery
what is fibrinoid necrosis?
occurs in connective tissue, blood vessel walls in hypertension and autoimmune disease
collagen degenerates, resembles fibrin but not true fibrin
fibrinoid nodule seen in rheumatoid arthritis

what is gangrenous necrosis?
dark, discoloured, foul smelling tissue
result of ischaemia (coagulative necrosis) and infection of necrotic tissue with anaerobic bacteria, especially Clostridium spp

what is apoptosis?
shrinkage necrosis (no inflammation/other degenerative changes)
a controlled process of cell death, programmed into cells to occur at a certain stage in their life cycle
death inducing signals are more dominant than cell surviving signals

when can apoptosis occur? (5)
embryogenesis ie. in separating digits
withdrawal of a hormonal growth stimulus ie. uterus following childbirth
removal of cells with high turnover ie. gastric mucosal epithelial cells
removal of cells with acquired DNA damage ie. viral infection, irradiation, cytotoxic drugs
removal of neoplastic cells in tumours
what is disease?
any departure from the normal physiology and anatomy evident in a healthy body. Diseased
tissue will show abnormalities in its morphology (structure)
what is ischaemia?
lack of blood in a tissue (interrupted blood supply)
what is inflammation?
response of connective tissue to mild/sublethal injury, and may also be seen following necrosis
what are the potential processes of inflammation, and how long do they take? (3)
process may be
acute
short lasting, hours to days
subacute
days to weeks
or chronic
long lasting, weeks, months, years
how are inflamed tissues named?
inflamed tissues are named accordingly
prefix = tissue name in Latin or Greek
suffix = itis
tonsilitis, appendicitis, hepatitis
exceptions pneumonia, pleurisy (aka pleuritis)
what are the examples of respiratory inflammations? (8)
rhinitis - nose
bronchiolitis
sinusitis
tracheo-bronchitis
tracheitis - trachea
pneumonia - inflammation at alveolar level
laryngitis - larynx
pleurisy/pleuritis - pleura
what are the 5 cardinal signs of acute inflammation?
calor - heat
rubor - redness
dolor - pain
tumor - swelling
functio laesa - loss of function
what is the series of reactions in acute inflammation causing the cardinal signs?
transient vasoconstriction of arterioles → blanching of area (not always seen)
scratching a line into skin with nail produces white line
sustained vasodilation of arterioles/venules and hyperaemia (increased blood flow to area) → redness, heat
histamine released
increased vascular permeability
histamine helps cause vessels to be leaky
increased leakiness of vessels to fluid and protein, leading to formation of inflammatory exudate
→ swelling, pain, loss of function
stasis (blood flow slows or stops)
margination and diapedesis
escape of leukocytes from circulation to tissue
adhere to white blood cell wall and then pass through into tissue space
chemotaxis
movement of leukocytes to site of injury
increased tissue pressure
→ pain, loss of function
phagocytosis
ingestion of necrotic debris, toxins
what is histamine release in acute inflammation illustrated by? (3)
pallor - vasoconstriction
flare (redness) - vasodilation
weal (swelling) - exudate
what are the types of escape of fluid from vessels? (3)
continuous
fenestrated
sinusoidal
what is continuous escape of fluid from vessels, and where is it seen?
skin, muscle, CNS
endothelium have to open up for fluid to flow
what is fenestrated escape of fluid from vessels, and where is it seen?
glands, kidneys, gastrointestinal system
areas that are thinner and thicker
fluid could seep through
what is sinusoidal escape of fluid from vessels, and where is it seen?
seen in liver, spleen, bone marrow
easy to produce exudate
what are Starling forces, and what does it help form?
physical forces acting across capillary walls (Starling forces) causes fluid to move from within vessels to extravascular space, and vice versa
these forces determine how much fluid is lost to extravascular space
transudate (tissue fluid) forms in normal tissue via Starling forces while lymphatics return fluid to circulation
what are the types of exudate? (4)
the composition of exudate depends on nature of injury
serous inflammatory exudate
fibrinous exudate
suppurative exudate
haemorrhagic exudate
between transudate, plasma and exudate, which has the highest concentration of protein?
normal plasma > exudate > transudate
plasma has the highest concentration
what is serous inflammatory exudate?
low protein levels and very little leukocytic emigration
very watery
very few white blood cells move into tissue
ie. skin blister
touching a very hot plate
what is fibrinous exudate?
kidney disease
high urea in blood
high protein levels ie. fibrinous pericarditis or pleurisy
high fibrinogen (soluble in circulation)
high fibrin (insoluble and sticky in tissue)
ie. pleural “friction rub”
when clinician listens to lungs, they will hear friction rub
what is suppurative exudate?
much leukocytic emigration due to infection
infection and leukocytes form pus
ie. meningitis
what is haemorrhagic exudate?
injury directly damages vessels and all blood components (fluid, proteins, RBC, WBC) leak out
bacterial infection (Helicobacter pylori) → thrive in high acid → stomach
ie. bleeding peptic ulcer
looks red (RBC)
what are the factors controlling exudate formation? (5)
endogenous mediators will wear off
histamine
arterioles gradually constrict
platelets plug up leaking vessel
distensibility of tissue is limited
increased lymphatic drainage
what is the purpose of exudate in acute inflammation?
i. fluid
water, electrolytes, dilutes toxins
ii. proteins
antibodies important in immunity, inactivate microbes
fibrin forms, acts as tissue glue
fibrin pretends spread of bacteria in tissue
complement helps acute inflammation and phagocytosis, enhances inflammation and kills bacteria
what is the purpose of infiltrate in acute inflammation?
i. neutrophils
phagocytosis
destroy debris
ii. macrophages
phagocytosis and immune function
iii. few lymphocytes
immune function
what is sequela?
a sequela is any possible result, complication or conclusion of pathological process
possible outcome
what are the sequela of acute inflammation?
resolution
formation of an abscess (pus filled cavity)
repair (healing)
regeneration
organisation
chronic inflammation