PTE 753: exam 1
1/106
Earn XP
Description and Tags
myelsodysplasia, brain tumor
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
107 Terms
what is myelodysplasia
a birth defect in which there is abnormal development of the back bones, spinal cord, surrounding nerves, and the fluid-filled sac that surrounds the spinal cord
aka spina bifida
list the 6 types of myelodysplasia.
myelomeningocele (spina bifida cystia)
meningoceles
lipomas of the spinal cord
myelocytoceles
diastematomyelia
spina bifida occulta (spina bifida aberta)
myelomeningocele (spina bifida cystia)
spinal cord (nerves too) and meninges protrude through an opening in the spine usually resulting in some form of paralysis
what is another way to describe myelomeningocele lesions?
failure of the ectoderm of the notochord to form a tube during neuorulation
meningoceles
sac-like protrusion of the meninges due to a defect in the spinal column in which a cyst may form that is usually not associated with paralysis
lipomas of the spinal cord
subcutaneous fat masses of the spinal cord which may lead to paralysis depending on the location of the mass
myelocyctoceles
spinal cord’s central canal expands into a cyst and protrudes through a gap in the spine ultimately compressing nerves
may or may not lead to nerve impairment tho
diastematomyelia
bony bands that split the spinal cord into 2 hemicords
spina bifida occulta (spina bifida aberta)
incomplete closure of the vertebra and failure of the dura mater to form around the spinal column, leaving a gap
usually not associated with paralysis
what are the 2 etiology possibilities that result in spina bifida?
failure of the ectoderm of the notochord to form a tube during neurulation (within the first 28 days of pregnancy)
failure below the S2 vertebra of groups of nerve cells to clump together and form canals during canalization
what are some other possibilites that may result in a baby developing spina bifida?
genetic abnormalities (multifactorial)
nutritional deficiencies of folic acid
increase alcohol consumption of mom and increase in valpaouric acid
teratogens and chromosomal defects
describe the meaning behind the “lemon” and “banana” signs found in an ultrasound taken of a baby with spina bifida.
lemon sign: flattening or indentation of the frontal bones
banana sign: the cerebellum appears curved due to a small posterior fossa and the downward displacement of the cerebellum (arnold-chiari malformation)
T or F: early surgical intervention may reduce UMN symptoms and cognitive consequences of spina bifida and decrease level of SCI by 2 levels.
T
what are some examples of early surgical interventions for a baby with spina bifida?
prelabor C-section
cover and close spine (post-natal)
ventriculoperitoneal (VP) shunt
in-utero closure
what is Arnold-Chaiari Malformation?
a structural defect where the lower part of the brain, including the cerebellum and brainstem, extends into the spinal canal due to the the base of the skull being too small or misshapen
what are the signs of hydrocephalus?
enlarged head
separation of skull sutures
bulging fontanelle
sunset sign
why might a patient present with UE involvement if she is suffering from hydrocephalus?
the expanding ventricles compress the motor pathways, primarily the UE ones due to location/orientation, leading to UMN signs and symptoms
weakness, poor coordination, spasticity
T or F: spasticity of the UE is likely a complication of hydrocephalus.
T
what are some other complications that result from hydrocephalus?
visupoerceptual deficits → vestibular issues
cognitive function
awareness in space
seizures
crainal nerve palsy/ bulbar symptoms
what are some examples of the signs and symptoms associated with shunt dysfunction?
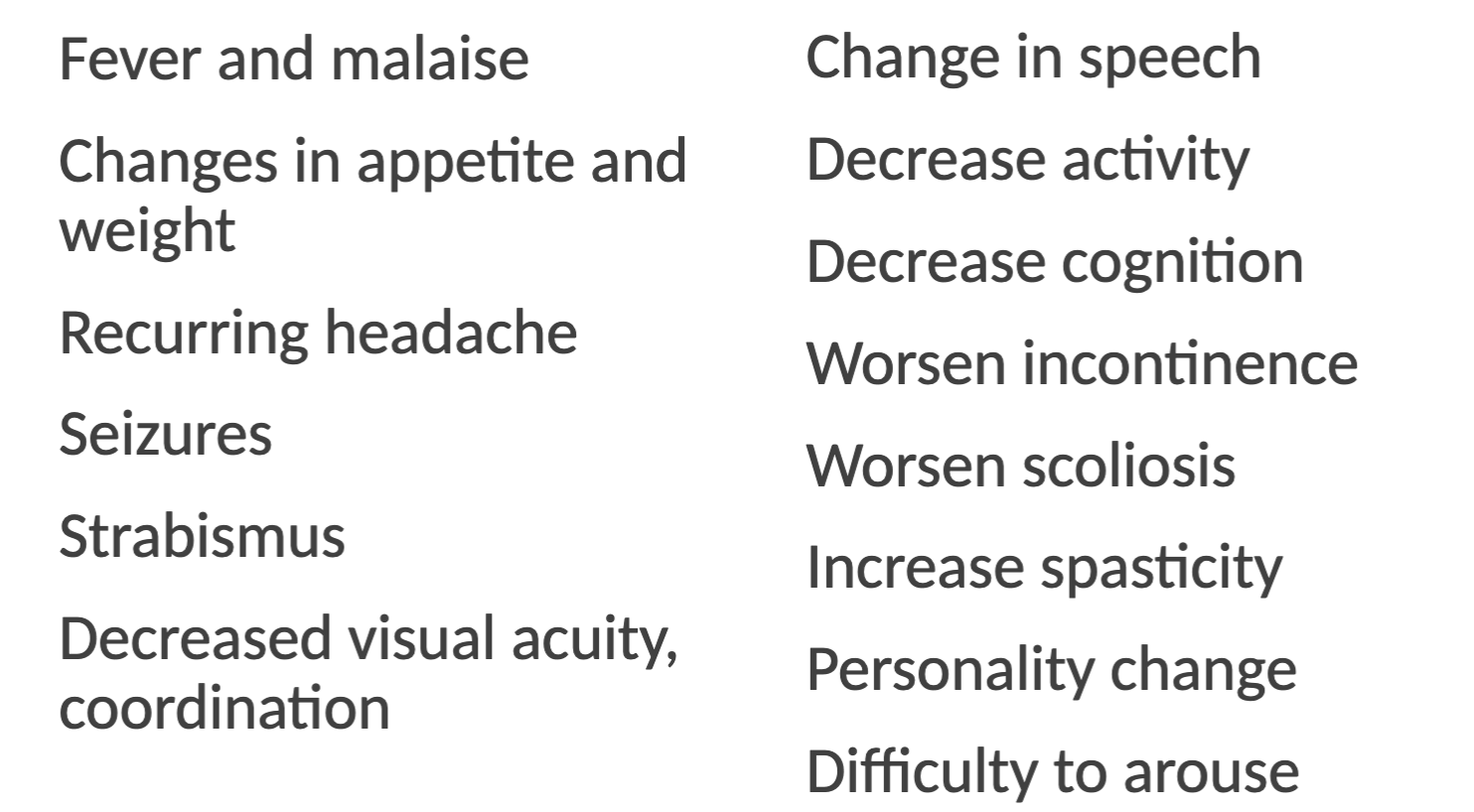
your patient is a regular and was diagnosed with spina bifida during infancy. one day, she complains of recurring headaches, a decrease in energy levels, and you note an increase in spasticity. you also notice she presents with a decrease in cognition levels compared to normal but she waves it off as “just being too tired to think”. why should you be concerned?
she is suffering from a shunt dysfunction and needs to go to the hospital ASAP rocky
what are the two key signs and symptoms of shunt dysfunction?
decrease cognition
personality change
syringomyelia
cyst forms in spinal cord proper resulting in changes in sensation, numbness, complaints of being too hot or too cold, weakness, spasticity, and increased scoliotic changes
tethered cord syndrome (TCS)
life threatening stretching of the spinal cord as the child grows but the spinal cord does not.
leads to weakness, gait deformities, pain, scoliosis, urological changes, and deceased UE coordination
why do children who suffered a SCI experience more significant dysfunctions?
they are still growing and changing!
what are some possible dysfunctions a child suffering from a SCI might experience as he grows?
high risk of TCS
worsening contractures
increase risk of UMN s/s and cognition issues
hydrocephalus
increase musculoskeletal issues
what musculoskeletal deformities might you see on a child with spina bifida?
scoliosis
hip issues
genu valgus or varus
equinovarus
calcanea valgus
torsional deformities
contractures
why are children suffering from spina bifida more prevalent to hip dislocations, dysplasia, and/or subluxations?
their hip ADductors are stronger than their hip ABductors and the hips lack loading forces from ambulating, leading to an imbalance in musculature
what are some other medical problems associated with spina bifida?
neurogenic bladder and bowel
chronic kidney disease
skin breakdown
latex allergy
cranial nerve palsy
seizures
obesity
T or F: fetal meylomeningocele repair often results in improved urological outcomes.
F; this was a quiz question
list the cognitive and psychosocial problems associated with spina bifida.
anxiety and depression
ADD
perceptual, visuomotor difficulties
attention and executive function
social cognition
T or F: a systems review should be completed at every physical therapy visit when working with neurological patients.
T
what consists of a systems review for neurological patients?
changes in behavior, activity level, and/or functional capabilities
bladder and bowel control
spinal alignment
skin breakdown or swelling
your older spina bifida patient suddenly has increased swelling in his LEs since his last visit one week ago. why are you concerned?
this is one indication of chronic kidney disease
when testing and analyzing ROM in patients with spinda bifida, joints are often _____, meaning they are not well developed.
arthrogrypotic
often born with severe deformities
when testing sensory in patients with spina bifida, what is the progression of tests as the baby ages?
newborns: sharp
2-7 year olds: light touch and positioning (proprioception)
7+ year olds: temperature and two-point discrimination
instead of Thomas test, we use _____ ____ for children with spina bifida.
Staheli test
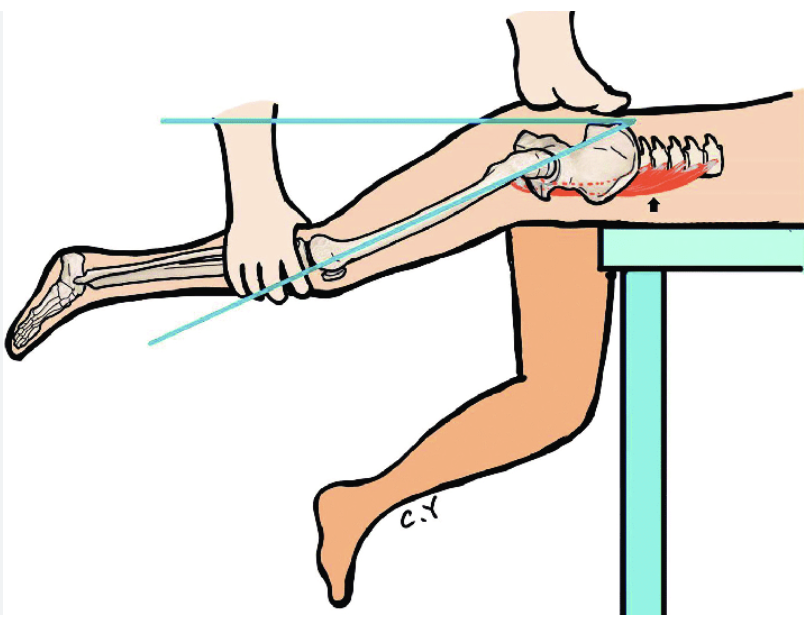
why is the Staheli test favored over the Thomas test for this population?
it allows for hip and pelvis stabilization to account for their “extreme” lordosis and/or kyphosis through spine
what are the two tools needed when assessing MMT on patients with spina bifida?
use a 5-point scale even with neonates
use a dynamometer if possible
T or F: when grading MMT with a 5 point scale, a therapist never notes his confidence because the scale is used for standardization.
F; always note confidence of MMT rating for scoring reliability with this population
what patient diagnosis should a therapist be very exact with when measuring MMT?
(a child with) tethered cord syndrome
what’s the difference between muscle tone with a neural tube defect and hydrocephalus?
neural tube defect → LMN so hypotonicity
hydrocephalus → UMN so hypertonicity
why does pain and ligamental instability arrive early in a patient with spina bifida?
movement patterns change as child grows
what is the best tool to monitor physical ability across a spina bifida patient’s lifetime?
funcitonal assessment
what are three factors that are important when educating parents?
repetition with reassurance
illustrations with minimal verbiage
focus on successes rather than failures
list some examples of physical therapy practices to teach parents.
positioning: extensor patterns and tummy time are best
stretching/ soft tissue mobilization
handling techniques
skin care
when should a parent facilitate vertical activities for a baby with spina bifida?
at 6 months
a child experienced spina bifida around her thoracic spine level but had early surgery intervention to help. what are likely outcomes that she may face in her lifetime?
using a wheelchair for mobility
needing a parapodium for exercise at T12
possibly having cognitive defects
may require supervised living
what are the most common orthoses for patients who experienced spina bifida at the thoracic-L2 region?
THKAFOs (thoracic-hip-knee-ankle orthoses
parapodium
what is a parapodium and what are the indications for needing one?
parapodium: upright positioning “brace” for high level lesions during exercise walking
indications: limited mobility, upright positioning, and walking
what are the likely outcomes for patients with spina bifida around the L1-L2 region?
hip dislocation due to unopposed hip flexion and adduction
may live independently
can work in a “sheltered” environment (non-competitive)
with spina bifida ranging from L1-L3, what are the differences in the assisted devices required between children and adults?
child: household ambulator with KAFOS with a walker or crutches
adult: wheelchair for community environment
what are the most common orthoses for patients who experienced spina bifida at the L1-L3 region?
HKAFOs (hip-knee-ankle-foot orthoses)
RGOs (reciprocating gait orthoses)
T or F: weak hip flexors are required for the use of RGOs because they are indicated to facilitate hip extension and swing phase.
T
what is the most common orthosis used for patients who experienced spina bifida at the L4 region?
KAFOs (knee-ankle-foot orthoses)
what are the indications for needing a KAFO?
unable to maintain upright posture due to contracture or weakness of knee
knee joints are unstable → medial and lateral instability
weak quadriceps 4/5 MMT or less
with spina bifida occurring at the L4 region, the anterior tibialis muscle remains “unopposed.” what deformity stems from this?
calcaneal foot
what are the assisted devices required for a patient suffering from spina bifida at the L5 region throughout his lifetime?
child: unaided ambulation in household environment and crutches for the community
adult: crutches with an inefficient gait and a wheelchair for long distances
with spina bifida occurring at the L5 region, what is a possible deformity occurring at the ankle/foot?
hindfoot valgus or calcaneous
what are the most common orthoses for patients who experienced spina bifida at the L4-S1 region?
standard AFOs
ground-reaction force AFOs
what are the indications for using the various AFOs for patients who had spina bifida at the L4-S1 region?
weak or absent ankle musculature
knee extensors 4/5 MMT or greater
medial and lateral instability of knee and ankle
inefficient-no push off and/or inadequate foot clearance
“crouch” gait pattern
at which level will a therapist note decreased push off force and clearance (during gait) from a patient with spina bifida?
S2-S3
what are the most common orthoses for patients who experienced spina bifida at S1-no loss?
FOs (foot orthoses)
SMO (supramalleolar orthoses)
what are the indications for using FOs or SMOs?
must clear foot and have adequate push off
unequal weight distribution of foot
medial and lateral ankle instability
poor alignment of subtalar joint, forefoot, or rearfoot
who are the most common populations to suffer from brain tumors?
children aged 0-15
adults aged 40-60
white Americans
males
what are the three most common pathogenesis for the development of brain tumors?
abnormal stem cell differentiation
abnormal cell proliferation
environmental factors
tumors likely arise from the abnormal proliferation of which structures?
neurons or glial cells, meninges, blood vessels, cranial/spinal nerves, and the pituitary or pineal glands
what are the three factors that make up a brain tumor’s classification?
origin
cell differentiation
border
what’s the difference between primary and secondary brain tumors?
primary: originate in CNS
secondary: spread to the CNS from areas outside the brain (mostly spreads from lung or breast cancers)
T or F: a tumor with well differentiated cells leads to a worse diagnosis and prognosis.
F; well differentiated = good prognosis
why might a patient’s prognosis be bad even if his brain tumor is removed?
tumor could’ve lead to brain damage and/or still present with neurological issues
what are the two types of borders a brain tumor may present with?
localized: encapsulated and grow where originated
infiltrating: invade and become entangled in surrounding neural tissue
what are the characteristics of a benign tumor?
slow growing
capsulated
non-invasive
no metastasizing
well differentiated
suffix = “oma”
what are the characteristics of a malignant tumor?
fast growing
non capsulated
invasive and infiltrate
metastasizing
poorly differentiated
suffix = “carcinoma” or “sarcoma”
T or F: glial cells (microglia, astrocytes, oligodendrocytes, and ependymal cells) are the “unsung” heroes of the CNS.
T
tumor signs and symptoms (clinical manifestation) depends on the ___ and ___ of tumor.
location
type
list some examples of s/s associated with brain tumors (in adults).
headaches, nausea, vomiting, blurred vision, drowsiness, seizures
list some examples of s/s associated with brain tumors (in infants).
irritability, sleep issues, protruding fontanelles, and poor feeding
people get headaches all the time. how do we know if it’s a symptom related to a brain tumor?
if the headache interrupts sleep, worsens/changes with postural positioning, coughing, or exercising, and results in nausea and vomiting
which s/s is typically the first one noted by patients with a brain tumor?
seizures
papilledema
swelling of the optic nerve resulting in transient visual loss, especially with positional changes
s/s of a brain tumor too
frontal lobe
motor functioning, initiation of action (decision-making), interpretation of emotion, thinking/judgments, movement, and personality
a brain tumor within the frontal lobe results in?
hemiparesis
aphasia
gait difficulties
parietal lobe
processes sensation, perception and movement coordination through sensorimotor integration
a brain tumor within the parietal lobe results in?
contralateral sensory loss
homonymous visual deficits or neglect
agnosias (difficulty recognizing objects)
apraxias (difficulty planning movements)
aphasia (difficulty processing language)
visual-spatial disorders
temporal lobe
hearing, especially language, memory, and object identification
a brain tumor within the temporal lobe results in?
auditory and perceptual changes
cognitive integration
long-term memory deficits
learning and emotional changes
occipital lobe
vision processing- color, motion, shape, and background/ foreground distinction
a brain tumor within the occipital lobe results in?
disorders of eye movements
homonymous hemianopsia
visual agnosia
agraphia (impairment or loss of ability to write)
cerebellum
responsible for coordination and equilibrium
a brain tumor within the cerebellum results in?
ataxia (poor muscle control)
dysmetria (impaired coordination)
dysdiadochokineasia (inability to perform rapid, alternating movements)
intention tremor
dizziness
brain stem
controls basic life functions, communication between cortex and nervous system
a brain tumor within the brain stem results in?
focal weakness or sensory loss
cranial nerve loss
autonomic dysfunction
a brain tumor within the pituitary gland results in?
loss of hormone secretion specific to type of hormone involved
hypothyroidism, diabetes, addison’s disease, etc.
which cranial nerves will be affected with an enlargement of a tumor in the pituitary gland?
CN 3,4, and 5
the pituitary gland sits superiorly/posteriorly to the ___ _____ which can cause bitemporal hemianopia (tunnel vision) if enlarged via tumor.
optic chiasm
an acoustic neuroma is a type of tumor that compresses which cranial nerve?
CN 8: vestibulocochlear
according to our notes, what is chemotherapy?
a toxic drug that acts on the DNA of the tumor cells and limits their ability to replicate
what are the two types of chemotherapy?
cytostatic: drugs that prevent cells from reproducing
cytotoxic: drugs that cause cellular death
describe the characteristics of radiation therapy.
delivers high-powered energy directly to tumor site
typical course is 1-5mins 5 days/week for ~6 weeks
has a life-time dosage that can be tolerated