primary wound closure - skinner
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
50 Terms
what is primary wound closure?
surgical closure of a wound that has edges apposed and will heal by 1st intention healing
what are the main goals of wound closure?
closure
no complications
cosmesis
what are required to achieve the goals of wound closure?
planning and proper technique
primary wound closure
close a site right after it is damaged
delayed primary closure
delaying when to close a wound but closing before any granulation tissue forms
secondary closure
manage a wound open until it is clean and healthy with granulation tissue to then close
second intention healing
leaving a wound to close overtime on its own
what are Halsted’s 7 principles of surgery?
1) strict aseptic technique
2) gentle tissue handling
3) meticulous hemostasis
4) preservation of blood supply
5) obliteraction of dead space
6) accurate anatomic apposition
7) minimisation of tension
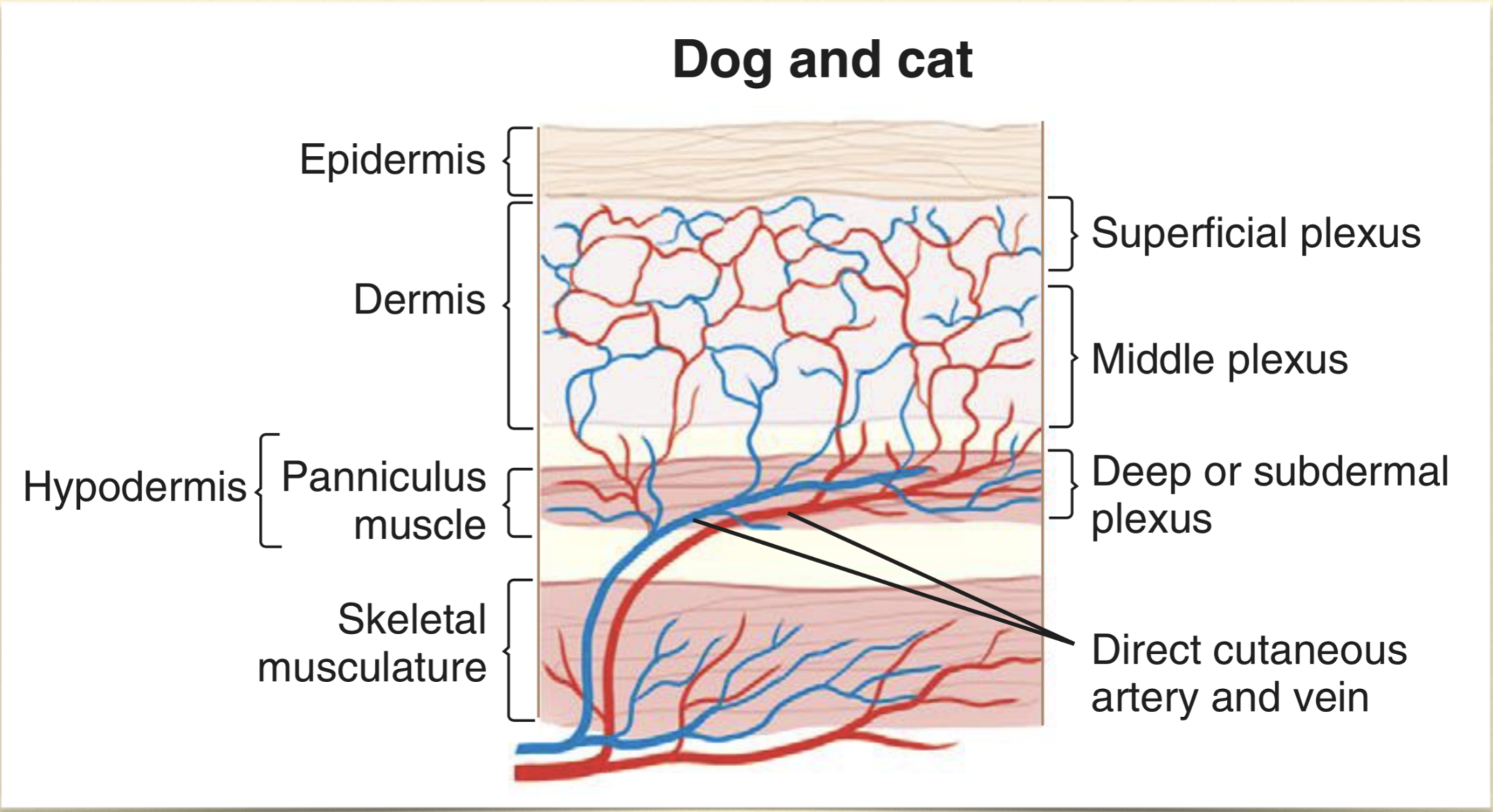
what area of tissue that supply blood to skin and SQ tissues?
deep or subdermal plexus
why to use primary closure?
simple
rapid wound healing
reduce pain
minimise scarring
protect underlying tissues
cosmesis?
cost? → may be less than second intention healing with visits and bandage changes
what are the patient characteristics that you must consider when deciding on how to close a wound?
systemic condition
immunosuppression → reduced wound healing, more prone to infection
metabolic disease → reduced wound healing = diabetes or cushings
cancer
radiation → causes delayed healing
temperament
species?
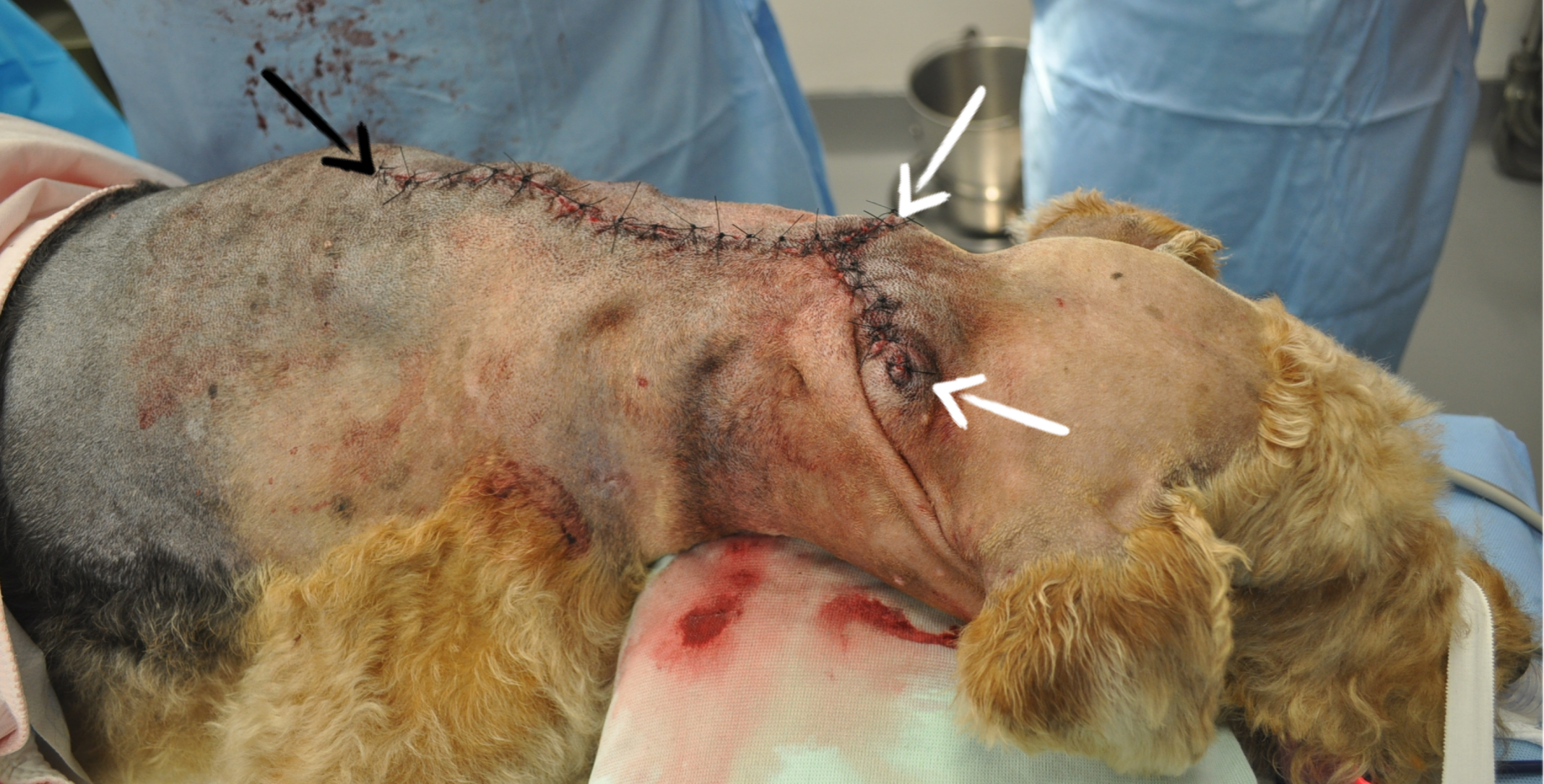
what are the wound factors that must be considered when deciding on how to close a wound?
location → higher area or contamination or highly mobile area?
configuration → is it even possible to close this?
tension
blood supply → a traumatic wound can have degloving that doesn’t declare itself for a number of days
what contamination levels are okay to close?
clean and clean-contaminated
what type of contamination is questionable to close?
contaminated wound → your judgement call/ on a case by case basis
how long does it roughly take for bacteria to grow enough in a wound to produce infeciton?
6 hours
what is the level of growth in bacteria that can occur in 6 hours?
105 bacteria per g tissue
what other wound factors can cause you to question whether to close or not?
extent of tissue trauma
tissue loss
crushing/shearing/burn
lag time
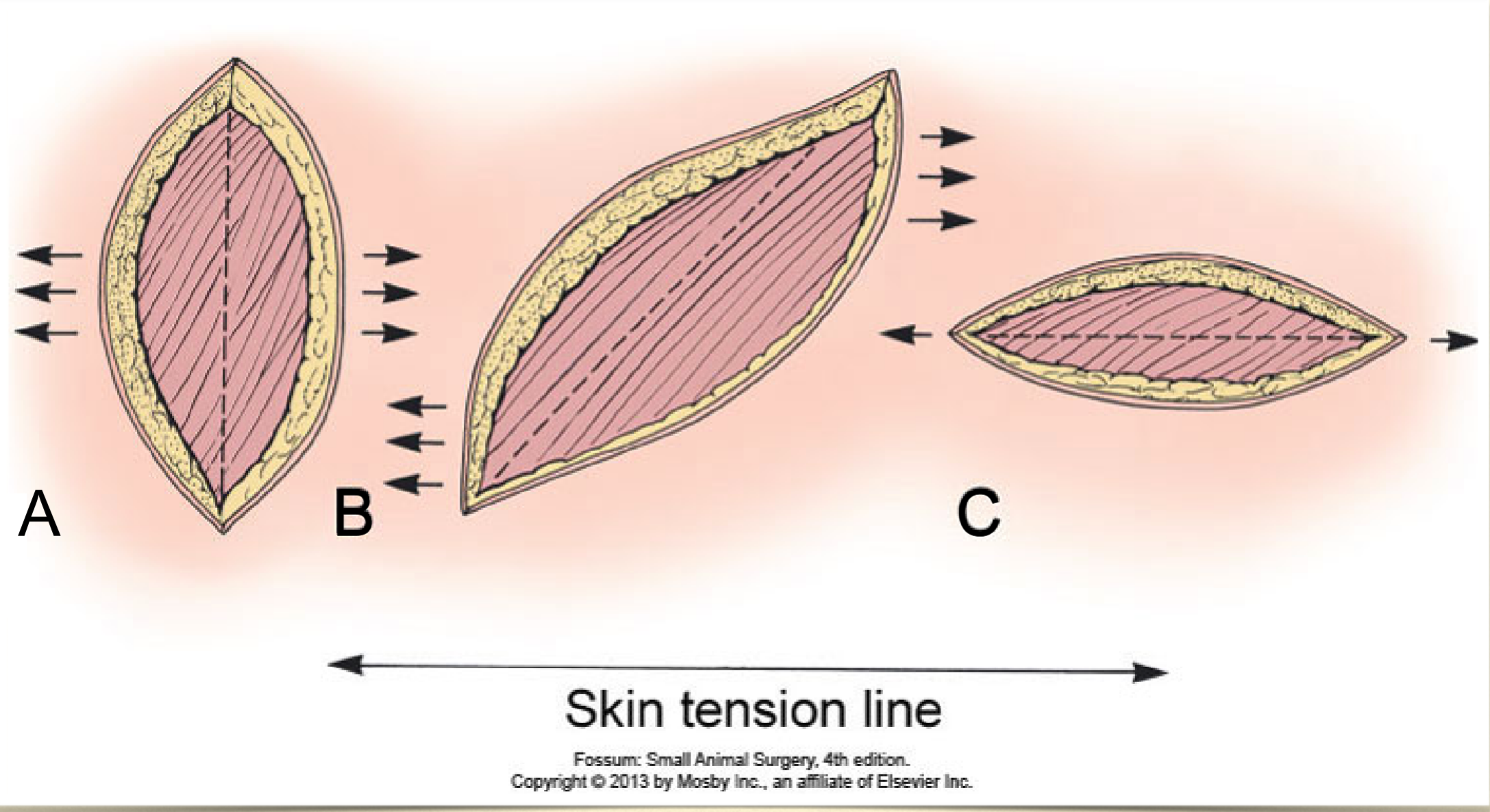
what is the general guidelines of skin tension lines?
on trunk = tension runs parallel
on limbs = perpendicular
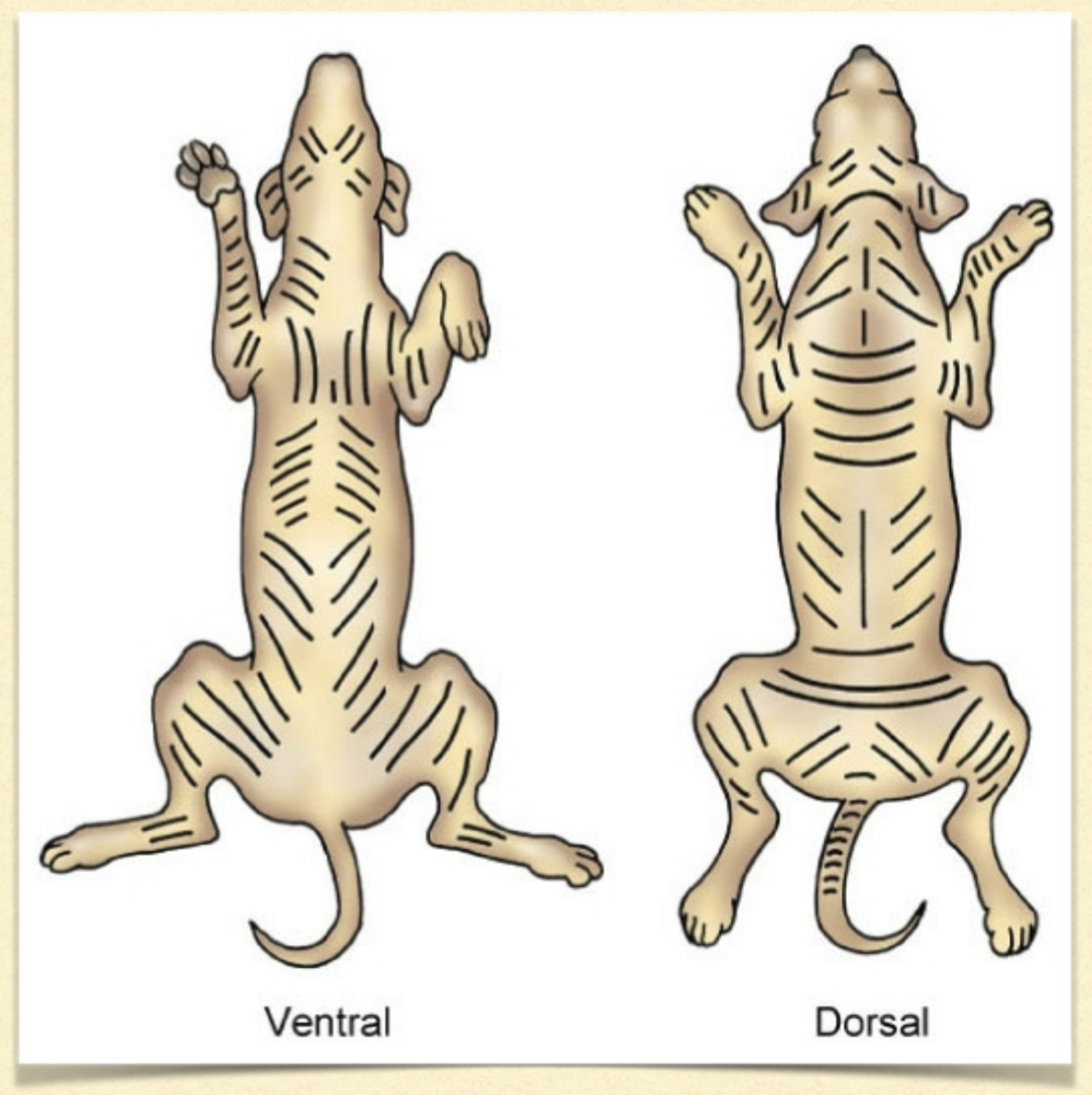
in what oriention to the tension lines do you want to close a wound?
parallel to tension lines
how to help to promote apposition with deep lesions?
multiple layer closures
muscle movement can be used to decrease space superficially
what do we want to use to create good apposition of the SQ?
distribute tension
decrease dead space
cruciate or mattress sutures
can also take wider bites that and into the fascial plane
can then add an additional suture in the skin to fully close - intradermal
continuous horizontal intradermal pattern
~50% overlap of bites
small bites
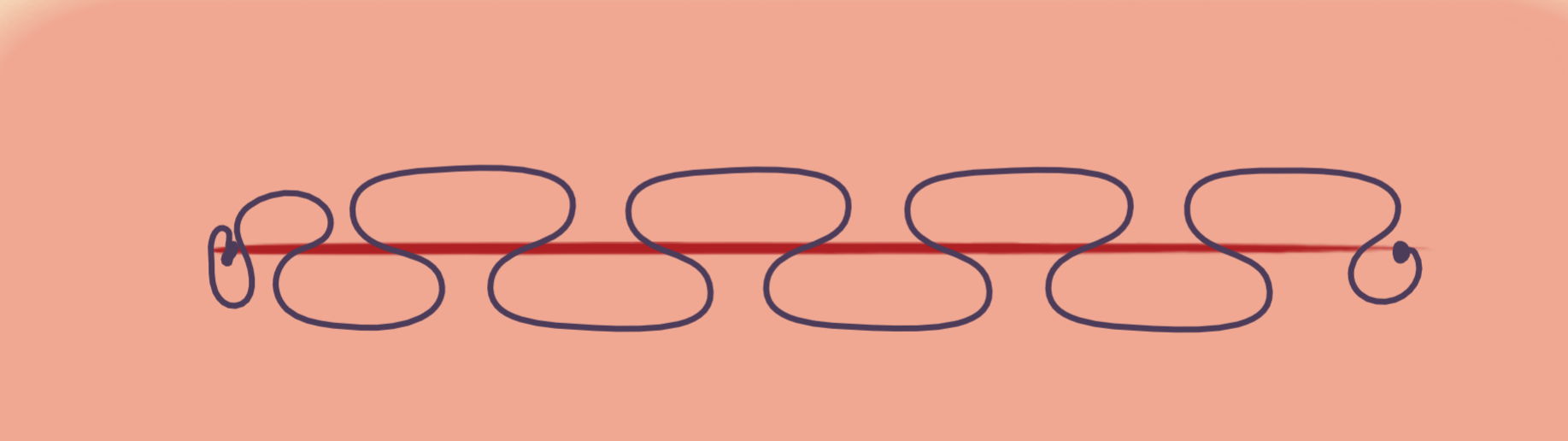
what happens with an intradermal pattern that has no overlap or larger bites?
gapping of the incision
simple interrupted
poor tension relief
slow to do
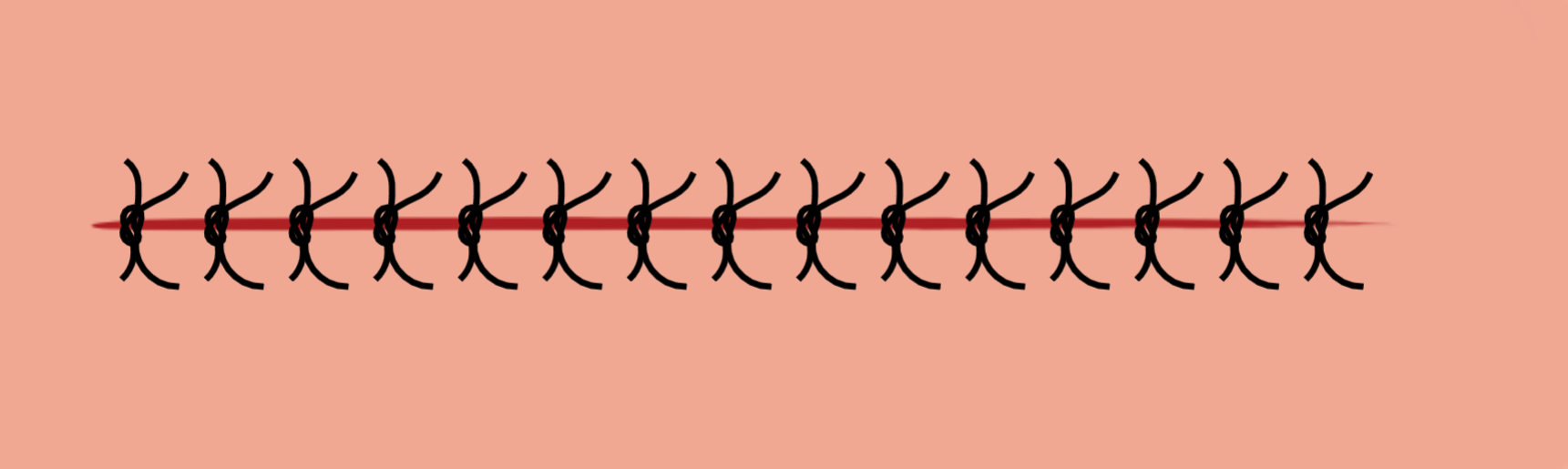
cruciate mattress
some tension relief
faster to put in
simple continuous
fast
not for high tension/motion
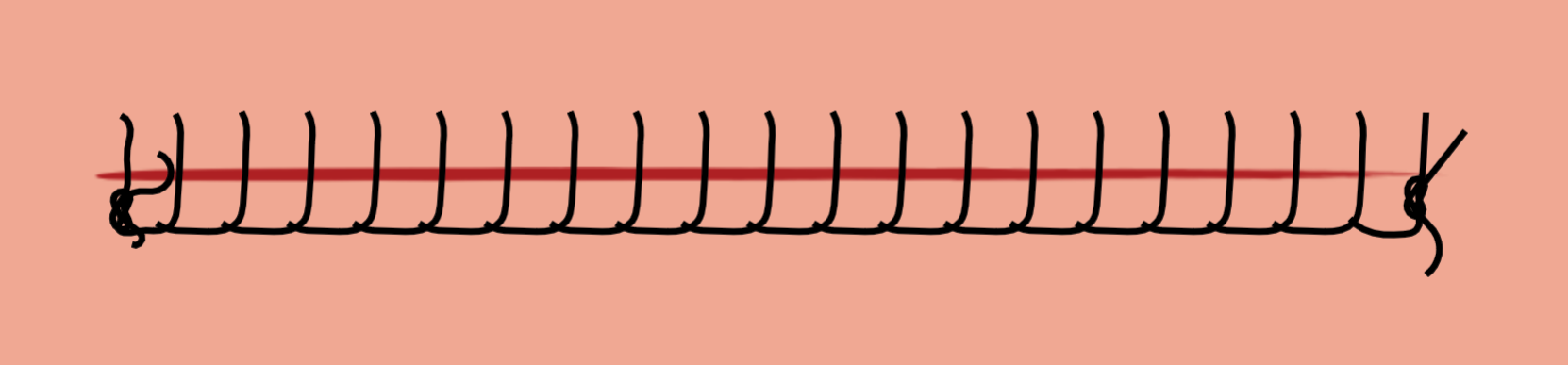
ford interlocking
fast
more secure if broken compared to simple continuous as it grabs onto itself
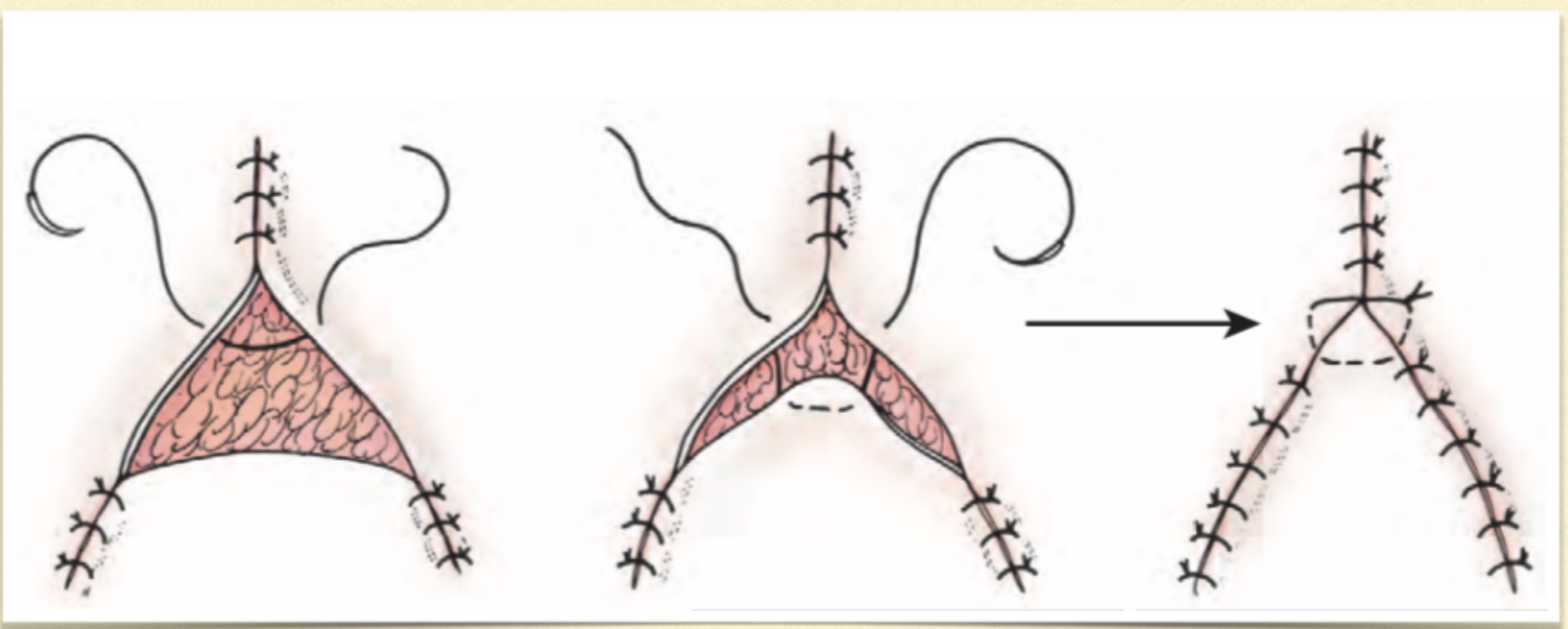
what are dog ears created by suturing a wound close?
folding up of skin after suturing an awkward wound
what are the reasons for dog ear formation?
unequal suture spacing
non-linear wound
are dog ears really a problem?
no more a cosmetic problem and will diminish with time
what is a technique you can use to close a very large wound?
halving to help guide your suturing placement
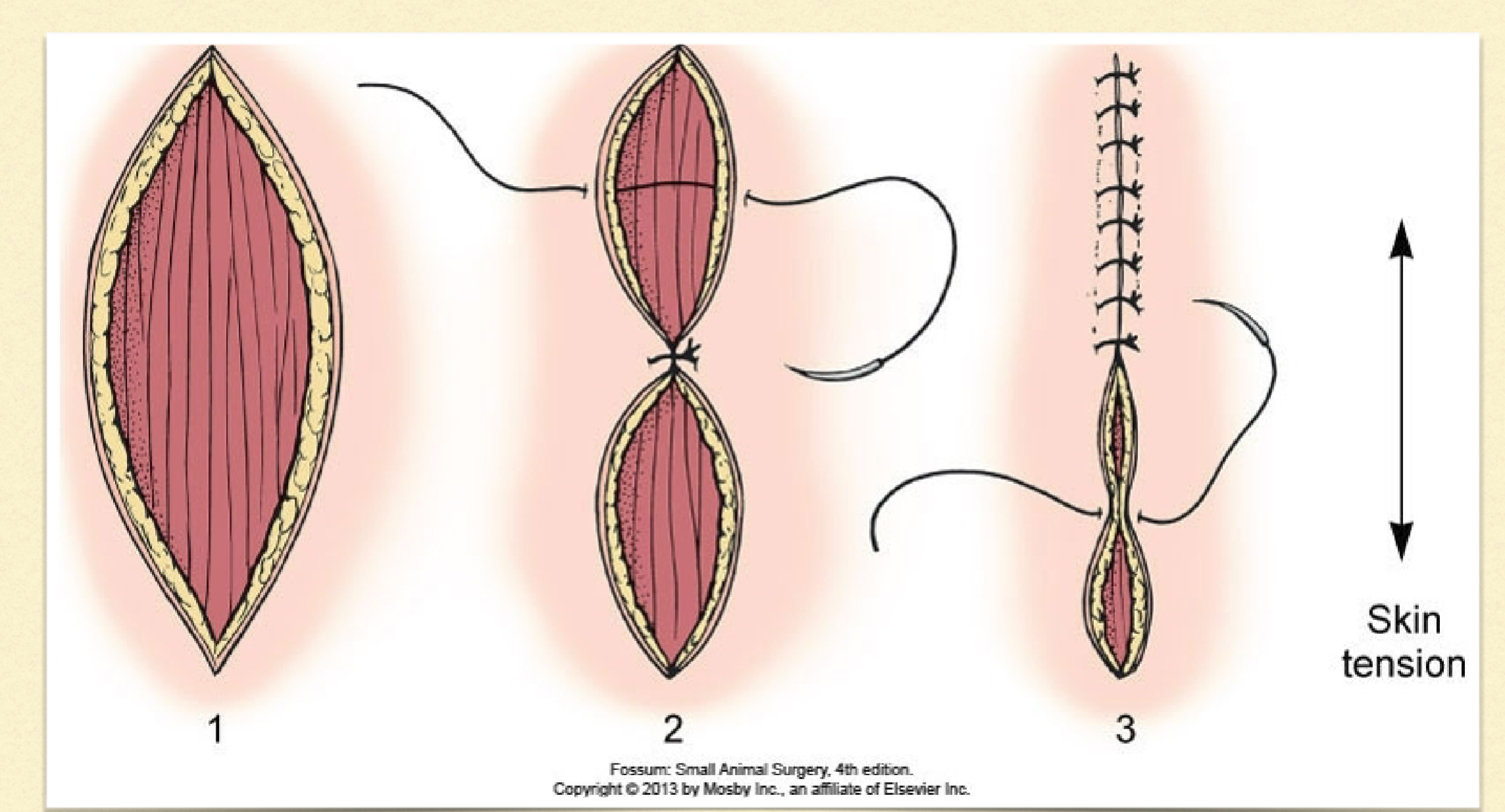
can halving work on a curved wound?
yes! suture bits need to be placed at different lengths across the curve so halving can help guide
how can you close a rectangular lesion?
close corners to bring middle closer together then
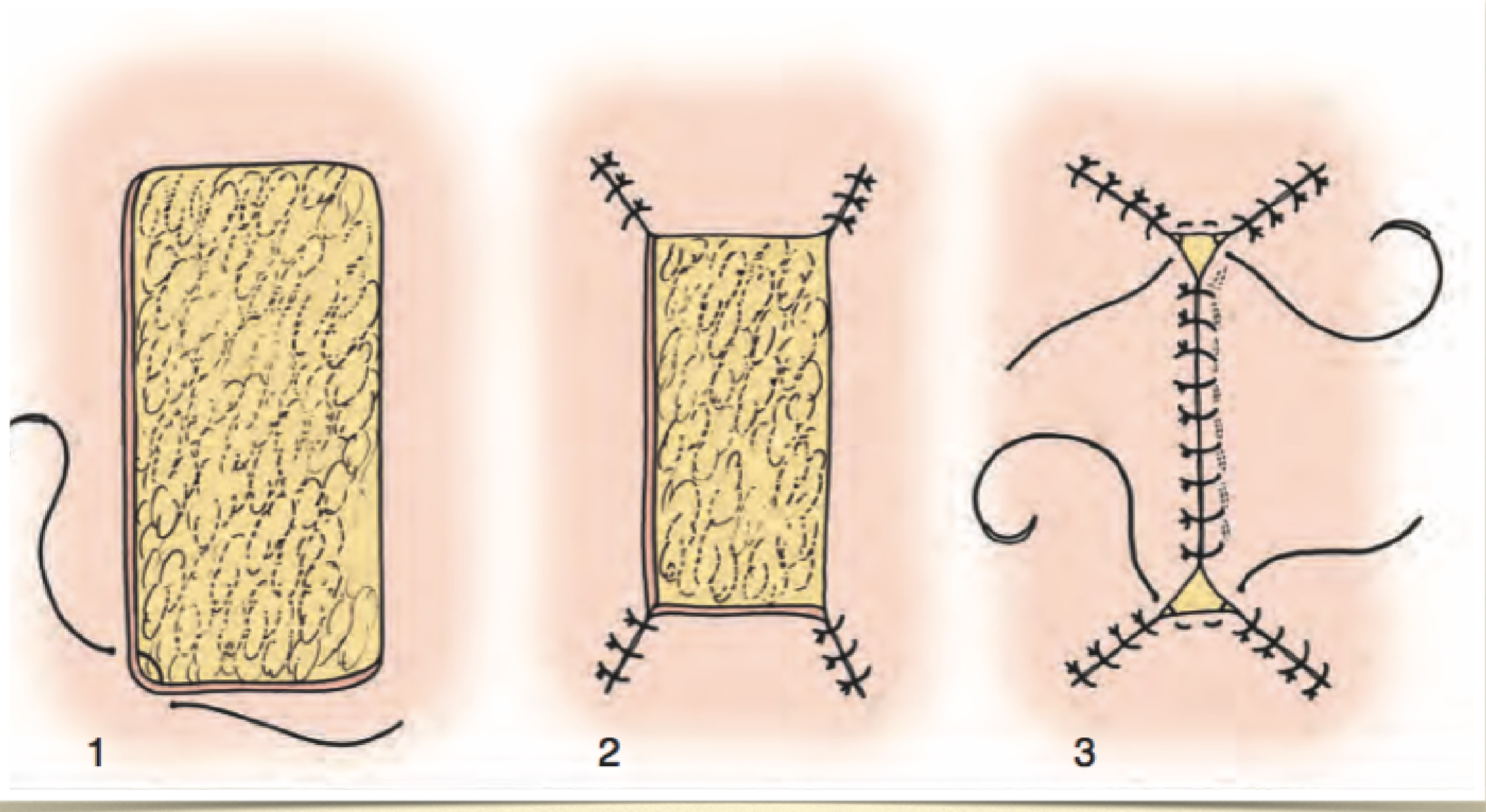
triangular closure
close up each side of triangle until meet in middle
what component of a primarily closed skin incision is most likely to fail with excess tension?
tissue
excessive tension of skin can lead to what?
dehiscence and tissue necrosis
what is another aspect that can cause dehiscence?
excessive activity that puts too much motion and tension on healing wound
what are the two methods of tension relief?
redistribution
creep
what are the two forms of creep?
mechanical
biological
what is mechanical creep?
stretching/breaking collagen and elastin
takes hours to days
common to use with larger defects
what is biological creep?
allowing new skin to grow
takes weeks
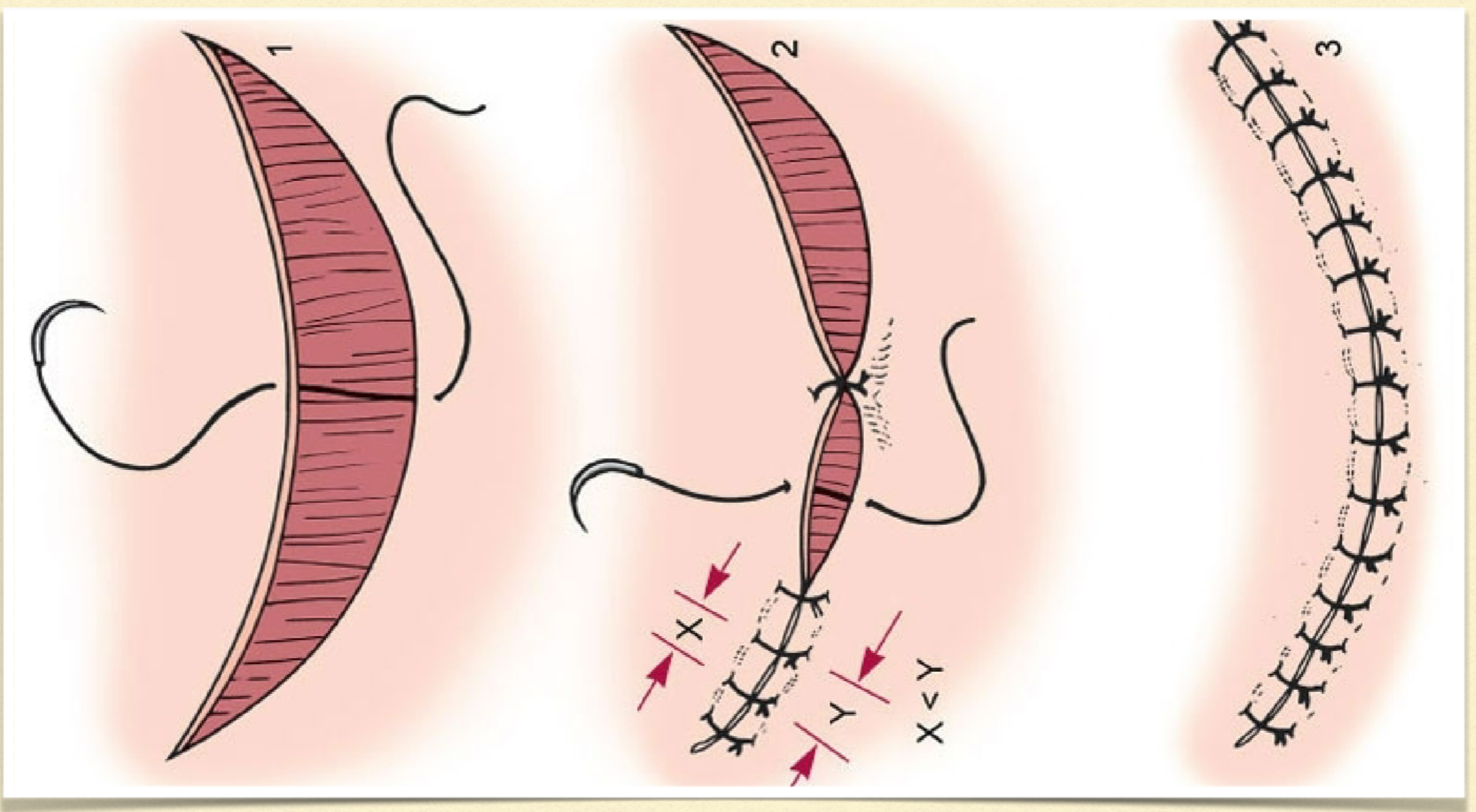
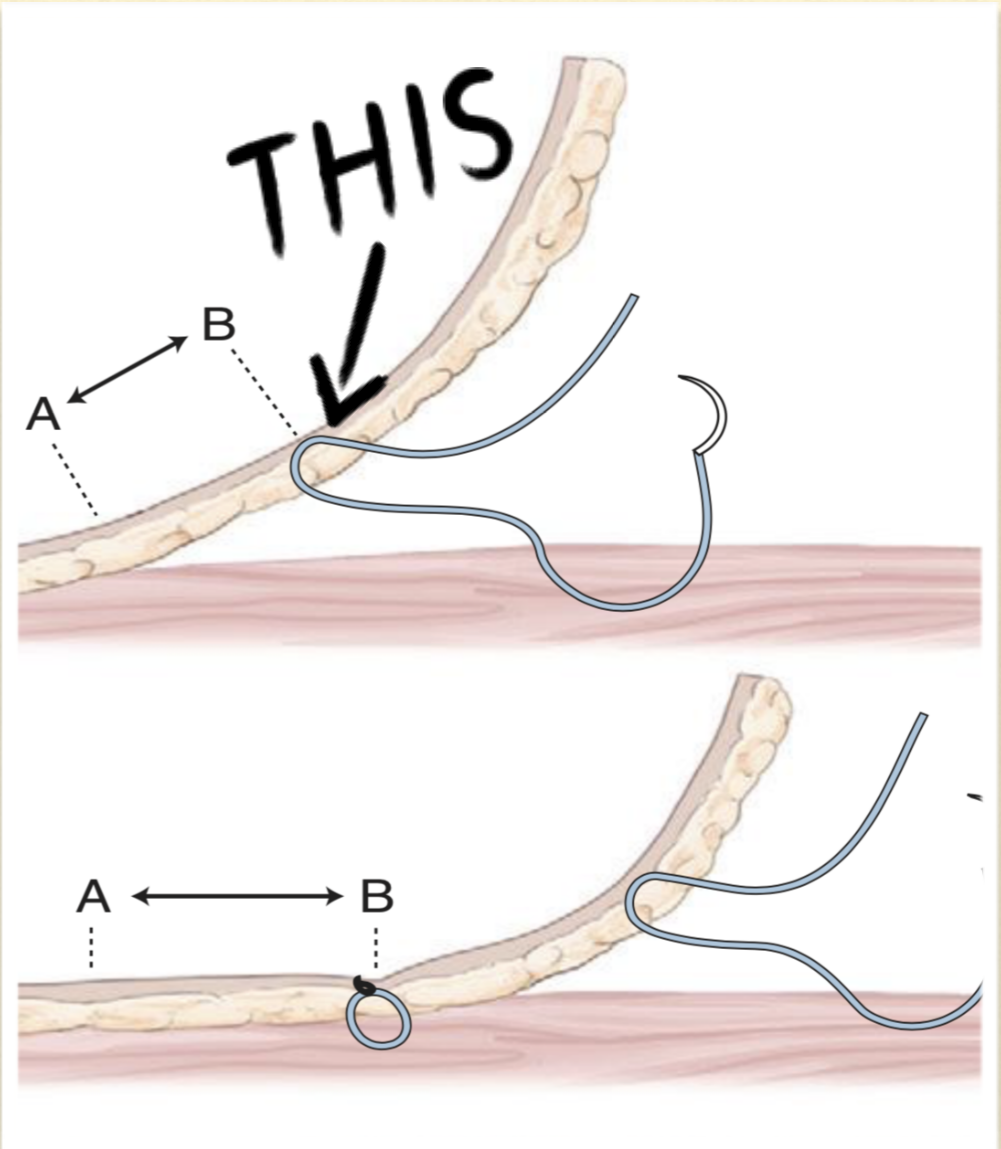
what is undermining?
mobilizing skin by separating it from deeper levels but going deep to the cutaneous trunci
why do keeping the cutaneous trunci with the tissue in undermining important?
preserves subdermal plexus
preserve vessel
all this keeps the skin viable
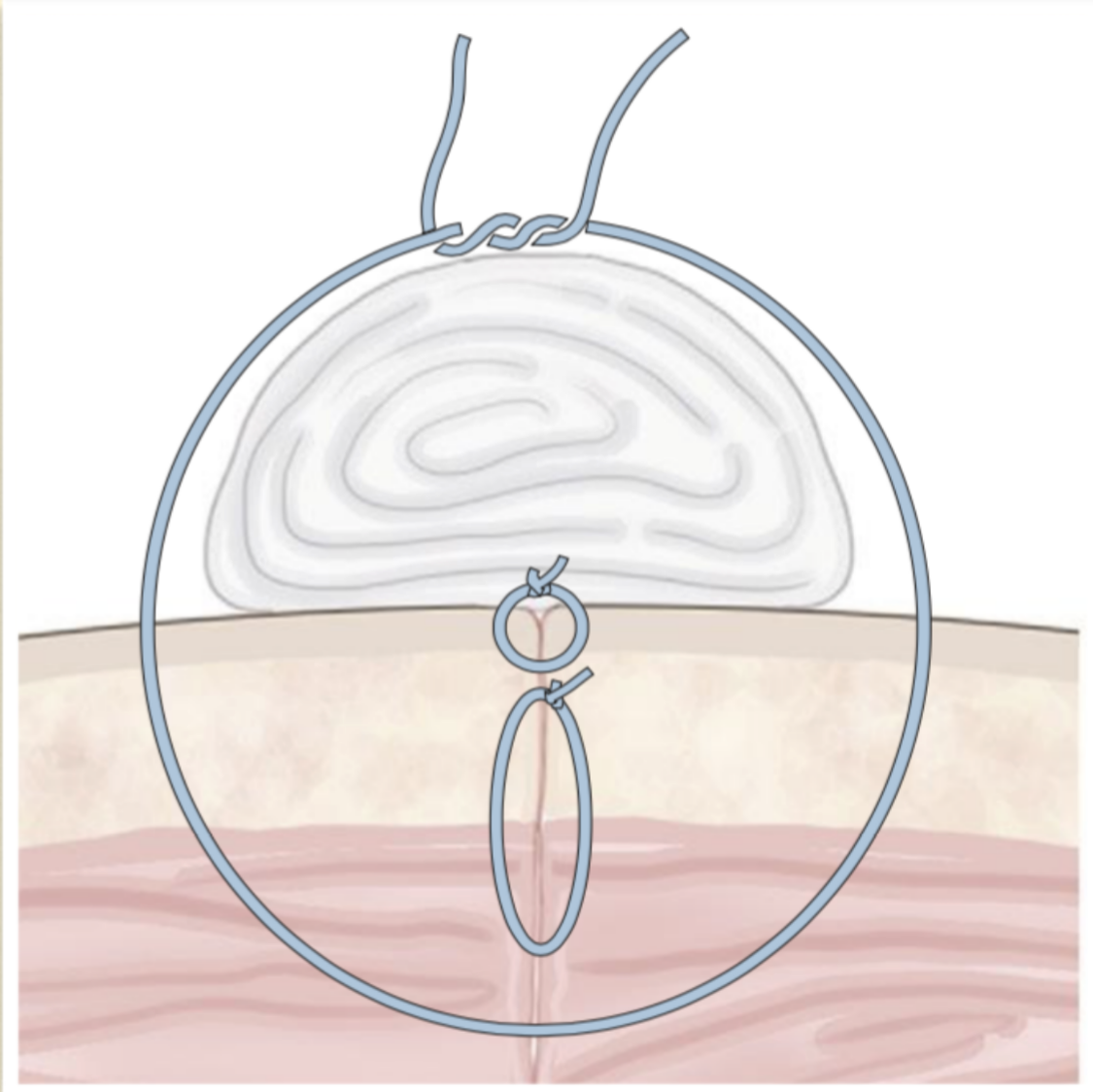
walking sutures
tension relieving
move skin across a defect → offset deep and superficial bites
stretching skin out
close dead space
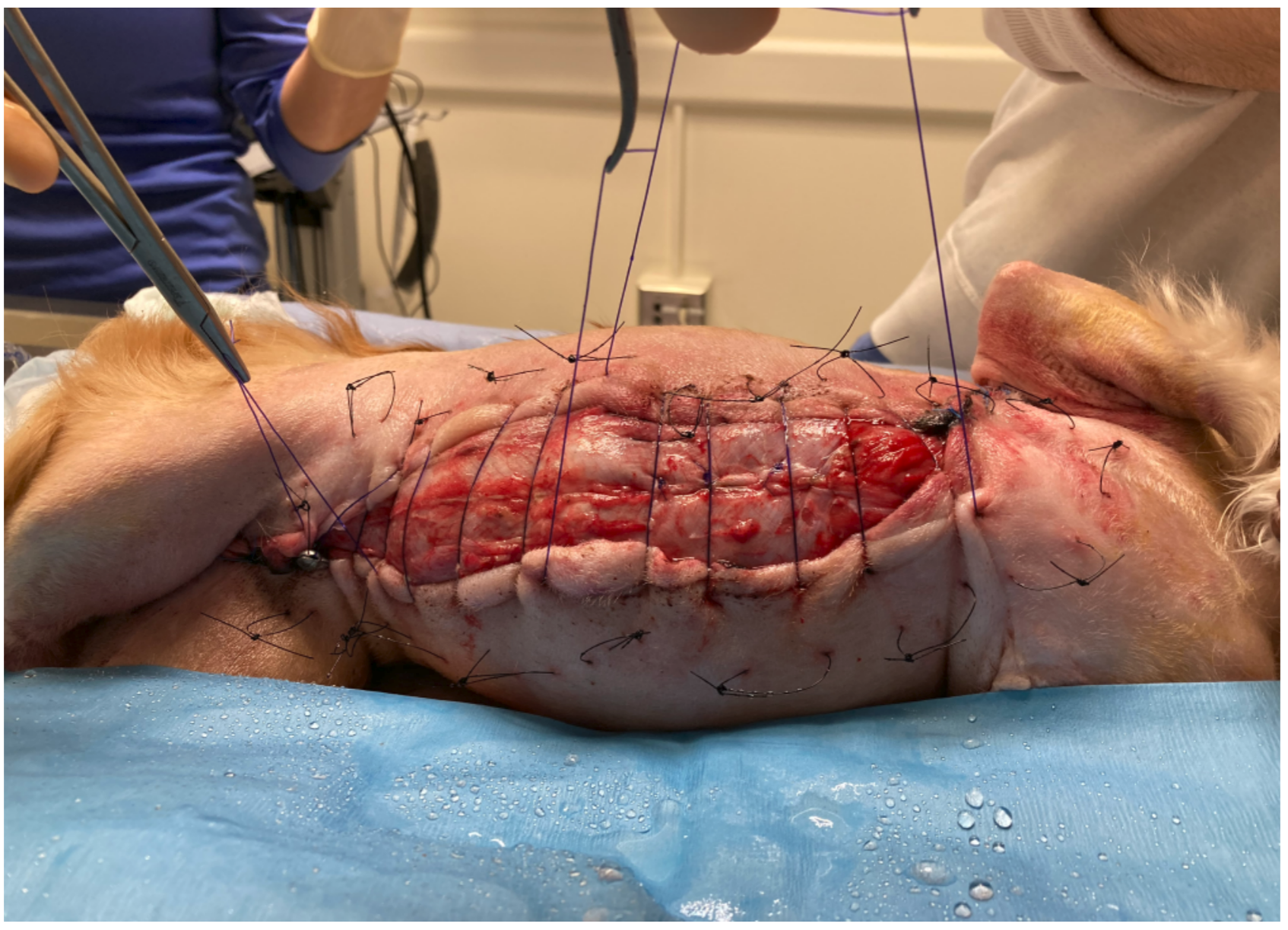
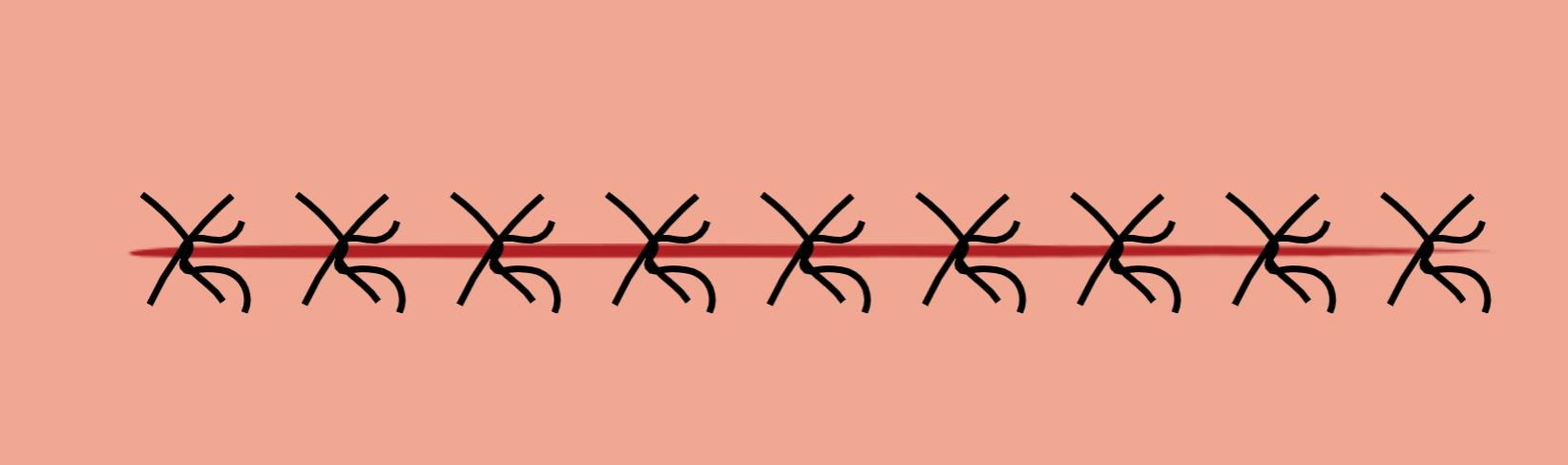
what are the types of external sutures that help to relieve tension?
mattress sutures (horizontal, vertical, cruciate)
far-far-near-near/far-near-near-far
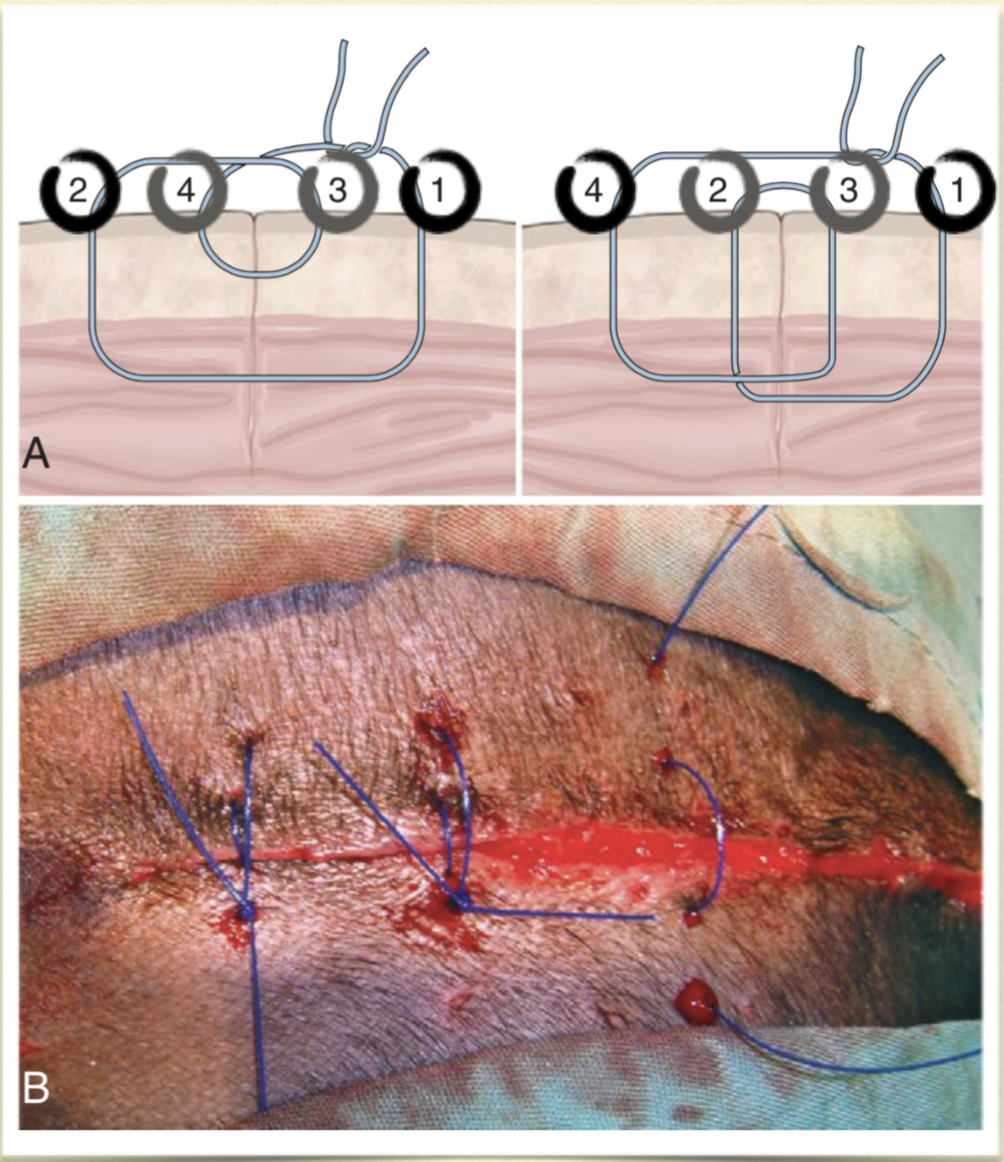
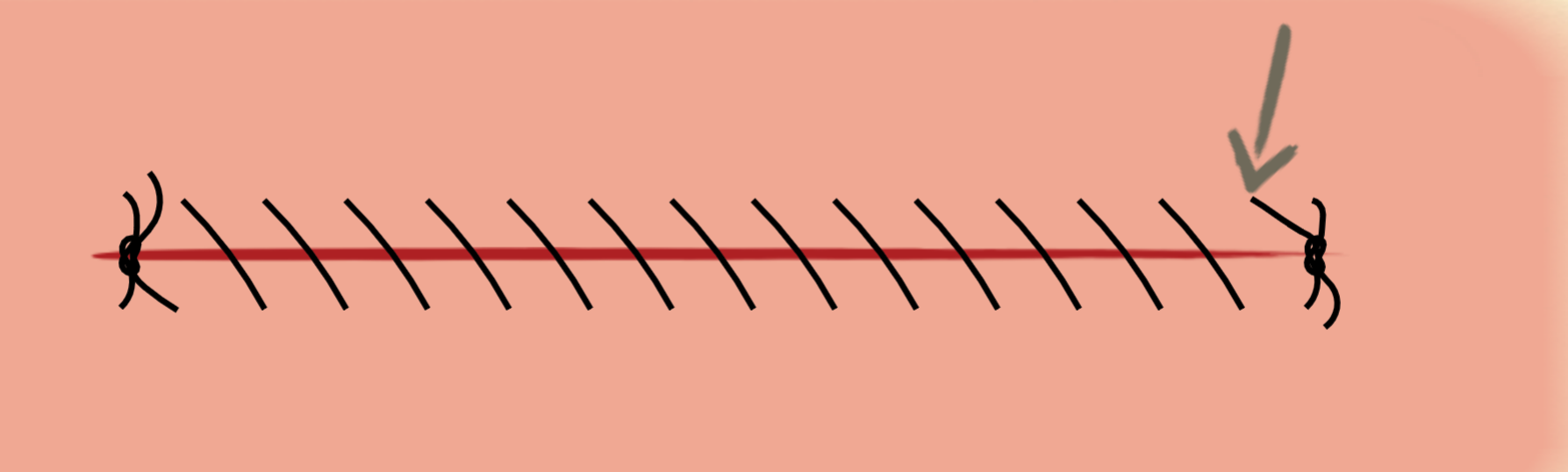
bolster/stent sutures
pre-place with wide bites
padding to distribute tension
what are releasing incisions?
incisions in healthy skin
heal by second intention
distal limbs is an optimal area to use this technique
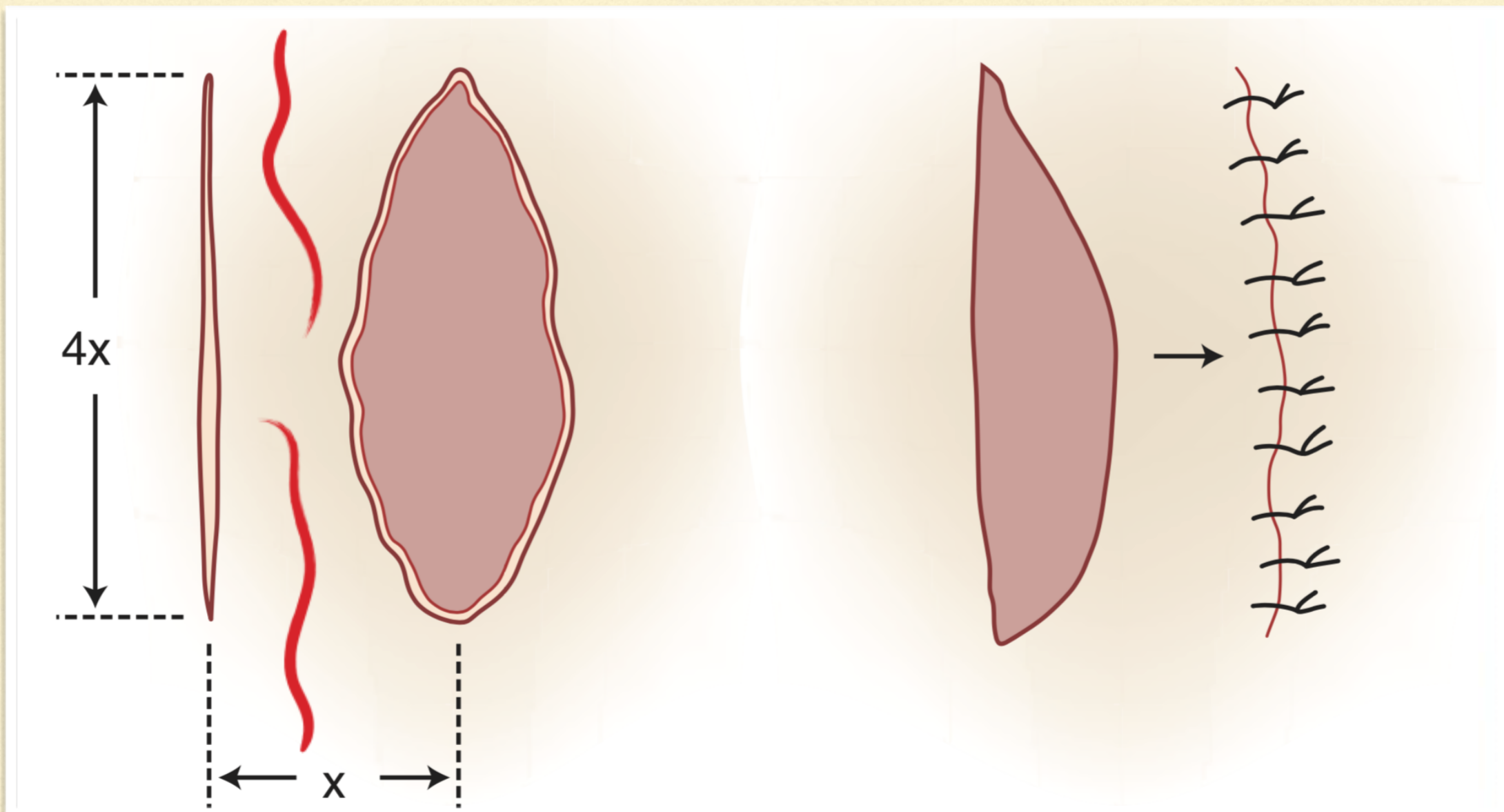
mesh releasing incisions
~ 1 cm or less incisions parallel to the closure and staggered

what is another way to close a large defect?
skin stretching
what are the options of skin stretching?
commerical/homemade
velcro/suture
adjusting the tension over time