NSG 501 Exam 3: Informatics & Documentation expert curated questions and answers 2025
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
37 Terms
informatics
processing of data
-the use of technology to chart data
-using tech for pt care
before-paper charting used to be used but now it is more digital
pros and cons of systems like EPIC
pros:
-can access from anywhere
-can track changes
-follows the pt
-do not have to read bad writing
cons:
-can be complex and one needs to learn how to use it
-less personalized care, bc professionals are looking at the computer screen more than at the patients
healthcare informatics (definition from lecture)
•Health care Informatics is the "application of computer and information science in all basic and biomedical sciences to facilitate the acquisition, processing, interpretation, optimal use, and communication of health-related data.
The focus is the patient and the process of care and the goal is to enhance the quality and efficiency of care provided."
in short: use of technology to improve patient care
documentation
•Electronic Medical Record (EMR)
- Legal record that provides a vehicle for sharing information with members of the health care team - includes Personal Health Information (PHI)
what can/is included in documentation?
•Admission data and physical assessment
•Ongoing assessments (flow sheets and progress/DAR notes)
•Medications, laboratory, procedures, and treatment
•Standardized care plans
•Acuity ratings
•Education
•Discharge summaries/teaching
the EMR is:
a legal document!
-you must chart accurate and good information
where do you document
epic
what are the purposes of documentation? (6)
•Communication
>can communicate among other teams, and anyone working with the patient
•Legal record of patient care
•Health care reimbursement
>insurance companies access these records to pay
•Quality Improvement
>example: reassessment of pain
•Research
•Nursing Education
>reading a patient charge helps students learn
>Epic Read-only
what are guidelines for documenting/charting
-always document everything
-there can be audits and all we do is monitored so we need to be purposeful
-the information helps to inform the continuity of care
-need to document in a timely manner
-need to be able to read the things and understand abbreviations etc.
-document appropriately and CURRENT and ACCURATE data
-as close to real time as possible
#1 documentation basic principle
if it was NOT documented...it was NOT done!
>>you need to chart for it to have been done
>>if it is not, it is as if you did not do it
guidelines for effective documentation (5 guidelines)
-factual
-accurate
-current
-organized
-complete
factual
objective data, real
example: vitals
accurate
actually the pt data
and also using the appropriate abbreviations and other words while typing out notes etc.
current
want to chart on time
-do not ever get stuck doing charting all at the end of a shift for all multiple patients
organized
-do not put info in the incorrect place
-know where to document what
-get familiar with EPIC
complete
fully thorough charting
what do you do if you forget to chart something?
chart it as soon as you remember that you have forgotten
>better late than never but best on time
again--avoid this by charting on time, asap
what organizations and associations provide guidelines and standards for documentation?
•American Nurses Association (ANA)
>Principles for Nursing Documentation
>Code of Ethics
•National Committee for Quality Assurance (NCQA)
•The Joint Commission (TJC)
•Specialty organizations
•Policies and Procedures
•RUMC P&Ps (policies and procedures)
>own in house policies for ways to chart things
the 5 W's guidelines for the EMR
WHO
-right person
WHAT
-requirements
-e.g. acceptable abbreviations
-provider or pt conversations
WHEN
-timely or follow up with correction ASAP
>can go back to pt chart for documentation purposes! (30 days after discharge)
WHERE
-correct location for info
WHY
if it was not documented, it was not done
documentation consideration: Confidentiality
•Nurses are legally and ethically obligated to keep client information confidential.
>CANNOT share any pt info
•Clients must give permission for info to be given to family, significant others
>always ask patient if their guests, family, etc. could get/listen to info about them
>if a family member calls--again you cannot give info!
->sometimes pt family and pt will agree to allow info over the phone and they will set up a passcode to say to "release" the information
-->very general info over the phone--not the whole patient life story and details!
•Clients have the right to obtain their medical record. They must complete the HIPPA Privacy Rights Request Form.
>pt fills out a request form to get these items/access
>records are destroyed after (x) years-(3-5)-so they should be in the know of that
>>MyChart is a great place for pt's to get info about their health and record
>>requesting a medical record for no actual medical reason is an additional charge!
•To have records sent to anyone who is not providing treatment, payment, or health care operations, client must sign an Authorization for Release of Patient Health Information Form.
HIPAA (Health Insurance Portability and Accountability Act)
we must follow HIPAA rules and laws to keep pt information confidential
•1996 - purpose to make health insurance info "portable"
•2003 - updates clarified and expanded privacy and security regulations
•Governs all areas of health care management
•Laws that guide the treatment of personal health care information.

security tips when documenting and handling patient information (lessons learned as a student)
list of things to follow to make sure we are maintaining HIPAA law and confidentiality!
•Sign out
>we do not want others to access our accounts and do things under our admin
•Only view the chart of YOUR patient
>Not appropriate to be curious
>only should be interested in who we are actively caring for
•Never print pages from the EMR
•Do not discuss patients off the unit
>Post Conference is a protected space
>b/c education
•Do not view the medical record off the unit
>example: at lunch
•Shred all paper documents with identifying info
>Only use initials
>makes pt less identifiable
•No social media posts about your patient
>NEVER
•Get permission to "Break the Glass!"
>some pt's will have a break the glass warning and you must receive permission to gain access to that chart
>it is never an accident to end up in this chart--bc you found yourself with the warning
can we access pt charts that we are curious about?
NO. you cannot go snooping into medical charts
>can only see charts for the pt's we are actively taking care of
can we talk about pt's to other nurses or members of the team?
when doing it for pt care, yes you need to communicate
>but to gossip about patients ABSOLUTELY not
>>you never know who is listening and they may know who you are talking about even without the use of names etc.
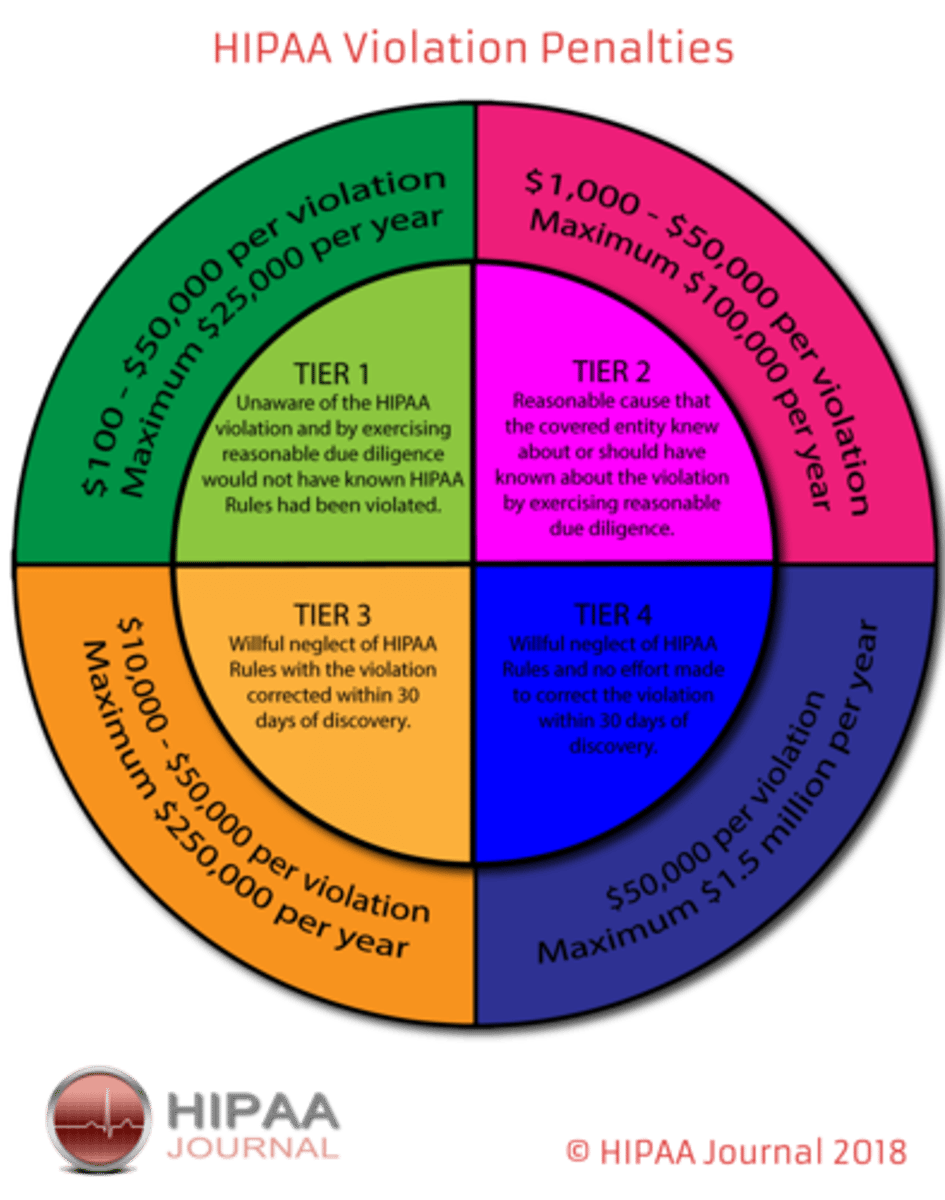
HIPAA violation penalties
4 tiers
fines $
you can be fined and you can also be fired and lose your job for violating HIPAA violation
what are the methods of documentation?
•DAR (Data, Action, Response)
>nurse note
>focused charting used by nursing at RUMC
•Narrative
>tell pt stories
>these are notes typically done by the provider
•Charting by Exception
>only the abnormals
•SOAP(IE)
>subjective, objective, asessment, plan, implemetation, and evaluation
>typically also done by providers
•Critical/clinical pathways
>steps on care
A DAR note address what?
a sign or symptom, condition, nursing diagnosis, behavior, significant event or change in patients condition. Follows the nursing process
data: what the pt is experiencing and showing
action: what we did for that or are going to do for that
response: how did the pt respond to that intervention
>>try to focus on the priority for the pt in that moment
DAR note example
D(data)
States pain in right leg (4/10). Denies injury
during the night. Right leg swollen and warm;
non-pitting; temperature 99.7 orally, other VSS. (vital signs stable)
Right post-tibial and dorsalis pedis pulses +2.
A(action
Instructed to remain on bed rest; right foot
elevated on 2 pillows. HCP notified and orders
for heating pad and analgesic received and
implemented.
R(response)
Pain has reduced to 1/10; swelling is slightly less,
verbalizes understanding the need for bed rest.
charing do's and dont's: wording! (amount of details)
there is good wording and bad wording
>typically related to the amount of detail provided in the documentation
examples:
POOR
>eats poorly
>pt confused
>uncooperative
>pt complains of pain
>good day
>diuresing well
>walking ad lib
GOOD
>ate 1/2 meal and drank 80mL
>pt cannot recognize family
>refuses to help in AM care
>complains of constant sharp RUQ pain
>pt states being pain free w/o meds, and can complete ADLs
>lasix 10 mg in IV at 14:30 resulted in 1000mL of clear, yellow urine
>walks around unit and up to the elevator and back to room w/o any discomfort
>>you need to DESCRIBE
>>all who read this should be able to understand the pt's condition and details
safety event
an event, incident, or condition that could have resulted in direct harm to a patient
>unusual occurrence (UO)
>concern for safety
>must fill it within 24 hours
>incident report
purpose of a safety event
•Quality Improvement
•Risk management
>we want to learn from our mistakes
examples of safety events
•Unexpected death or outcome
•Injury to patient or visitors or staff
•Device failure
•Specimen labeling error
>never label something you did not collect
•HAPUs
>hospital acquired pressure ulcer
•Burns
a safety event SHOULD:
•Should Include objective info
>info of things that we did
a safety event SHOULD NOT:
•Should not be used to assign blame - "Just Culture"
>we want to learn how to be more safe and we should not be putting blame b/c then people will not want to speak up when they make a mistake
is a safety event a part of the EMR?
•Not a part of the legal EMR
>we do not put "we wrote a safety event" on the patient's chart
>can chart what occurred but just not chart that we filled this "incident report"
is a safety event only when something bad actually occurs?
no--also for "near-miss"
>something that was a risk for something bad occurring that could have reached the pt but did not
example: a wrong medication
if we are asked about what occurred or need to recall what occurred from some time ago--do we make things up if we do not remember?
NO. if you do not remember you stay honest and say that you do not remember what occurred. never make stuff up.