Male Reproductive System
1/88
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
89 Terms
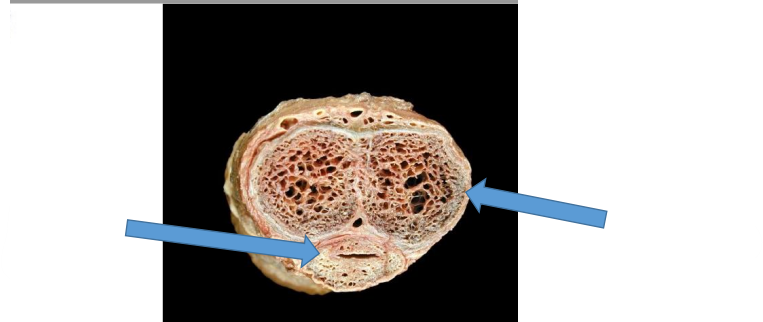
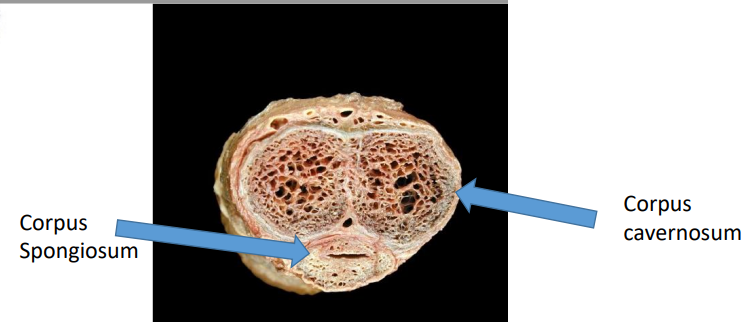
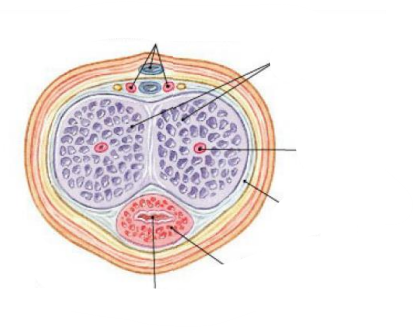
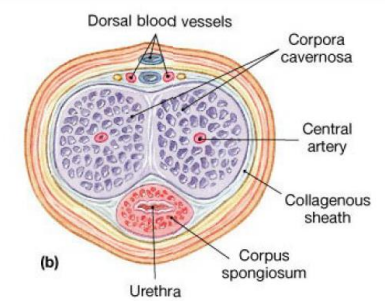
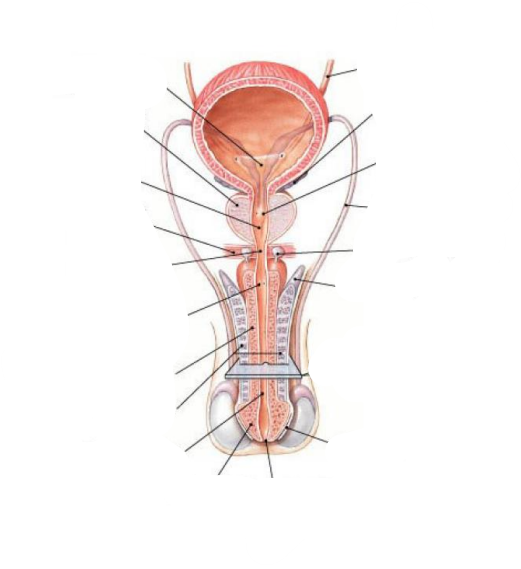
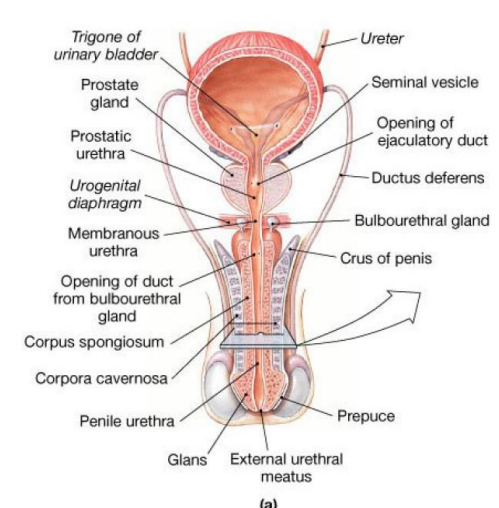
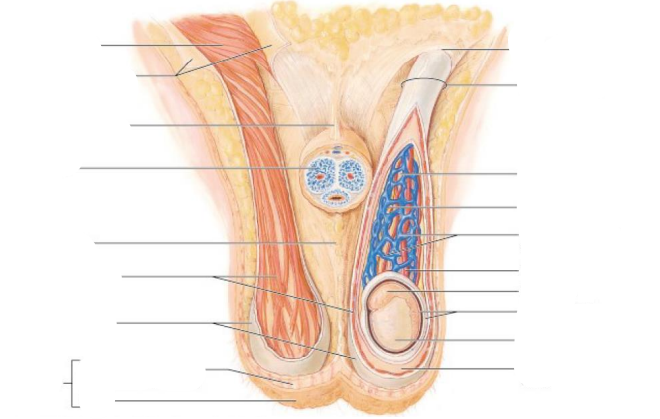
There are 3 columns of erectile tissue in the penis. What are they
Corpus Spongiosum (urethra)
2 Corpra Cavernosa
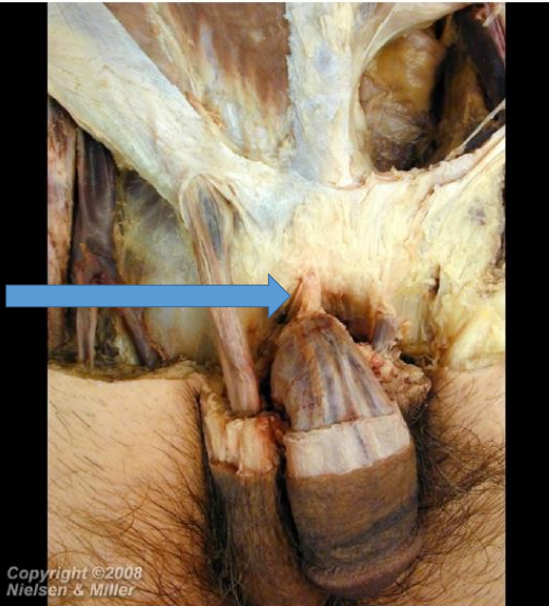
What’s that & what does it do
The penile suspensory ligament (PSL) supports and maintains the erect penis in an upright position during sexual intercourse
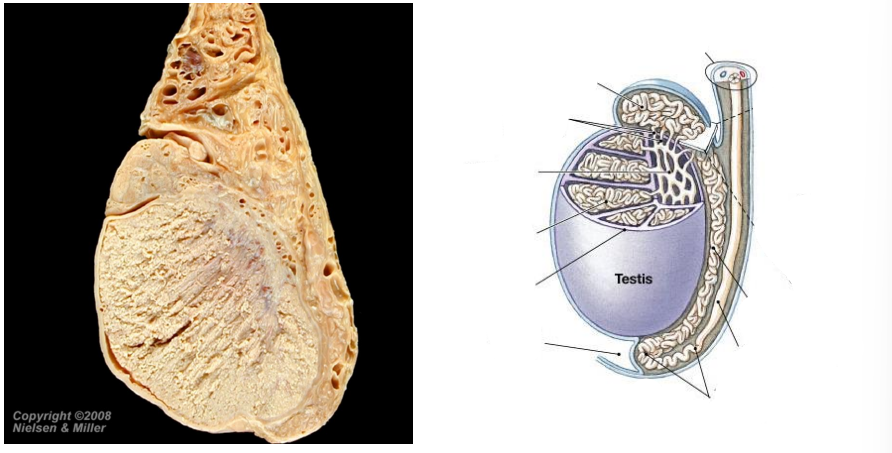
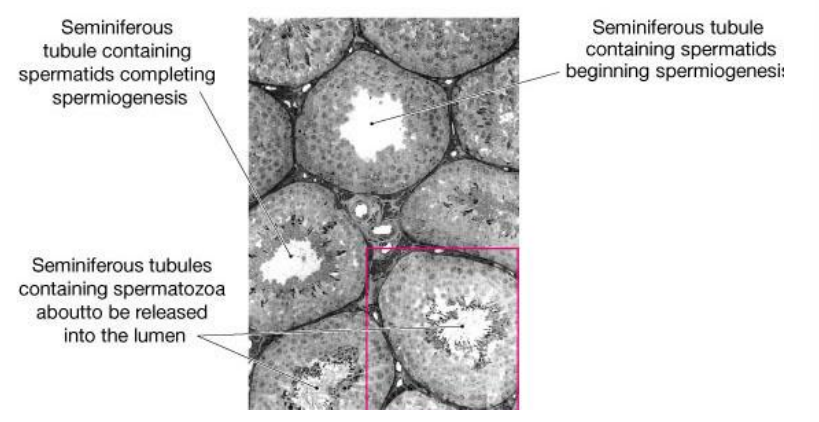
Seminiferous tubules are the site of what process
Germ Cell Production
Leydig cells function
testosterone production
What sits between the seminiferous tubules
Interstitial cells of Leydig
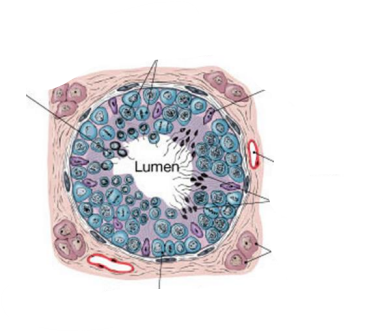
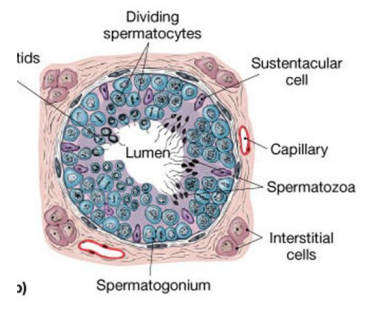
Name the 2 main types of cells in seminiferous tubules & give their function
Spermatogonia: Stem cells involved in spermatogenesis
Sustentacular cells (Sertoli): Sustain and promote development of sperm
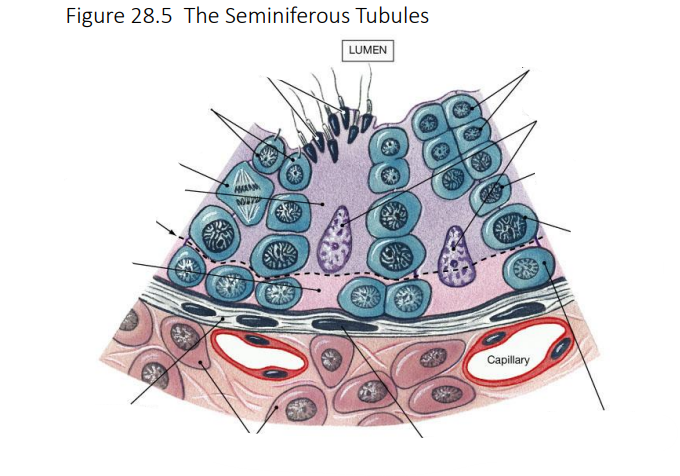
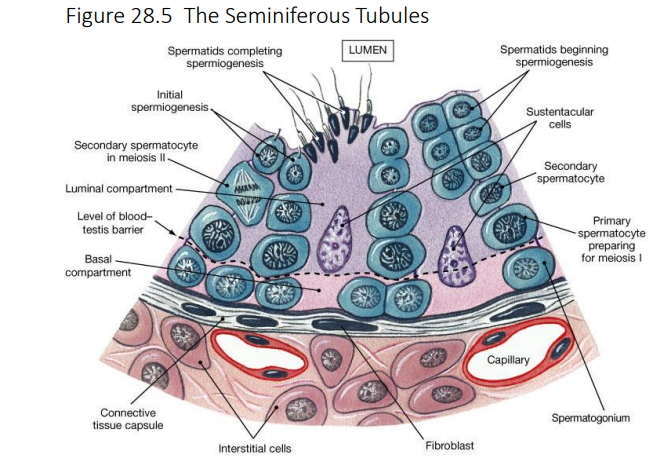
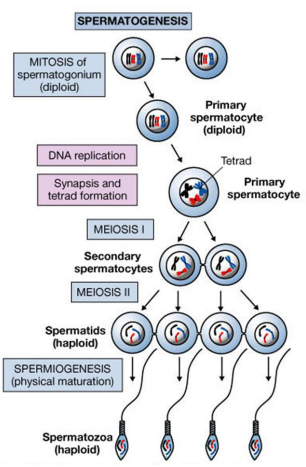
Spermatogenesis involves three processes. What are they
Mitosis
Meiosis
Spermiogenesis
Structure of a spermatozoon (fully mature male gamete)
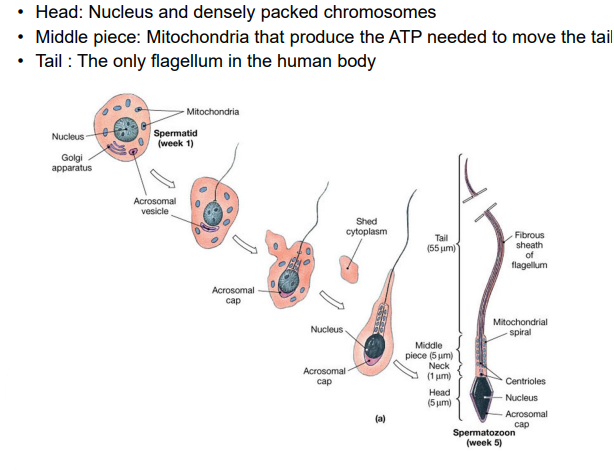
The acrosomal cap on the spermatozoon is derived from what
Golgi
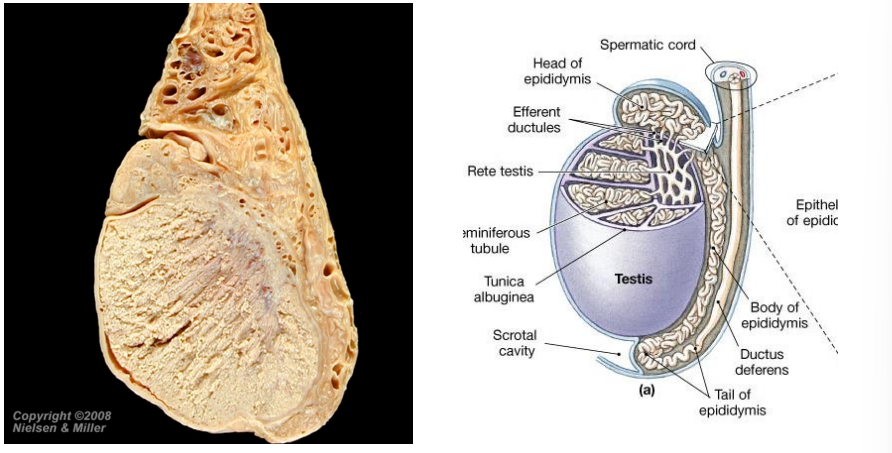
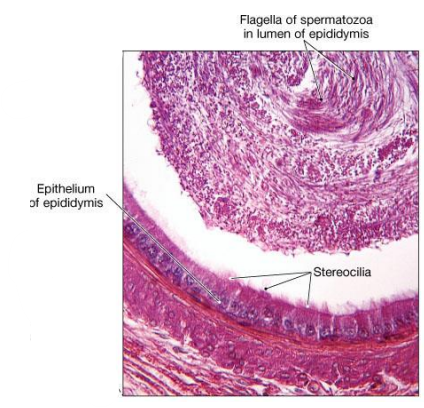
epididymis role
Elongated tubule with head, body and tail regions
Monitors and adjusts fluid in seminiferous tubules
Stores and protects spermatozoa
Facilitates functional maturation of spermatozoa
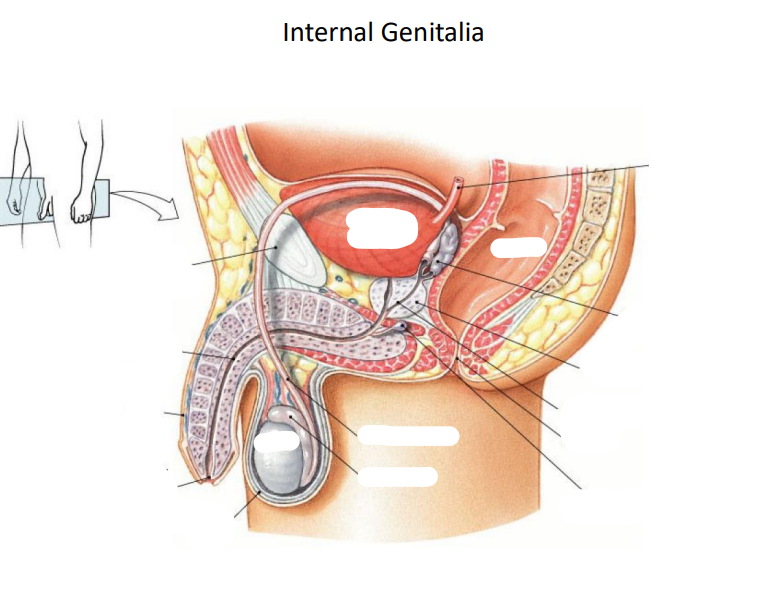
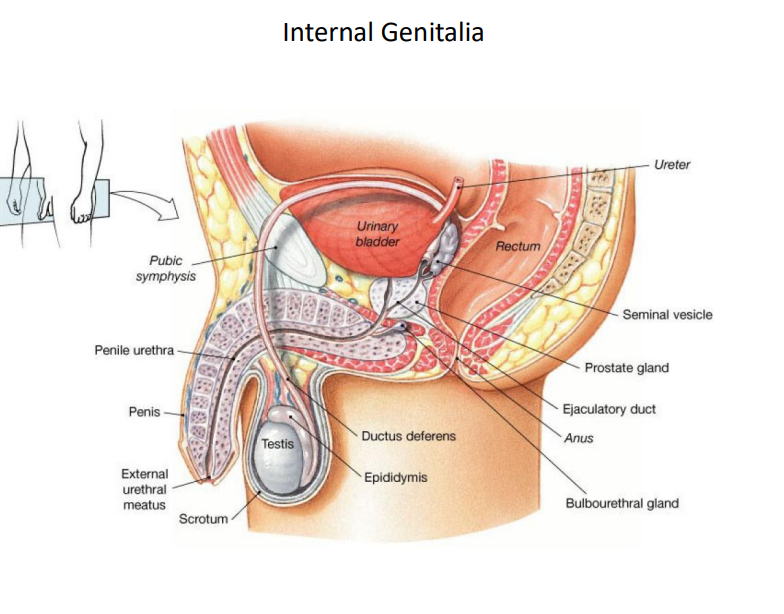
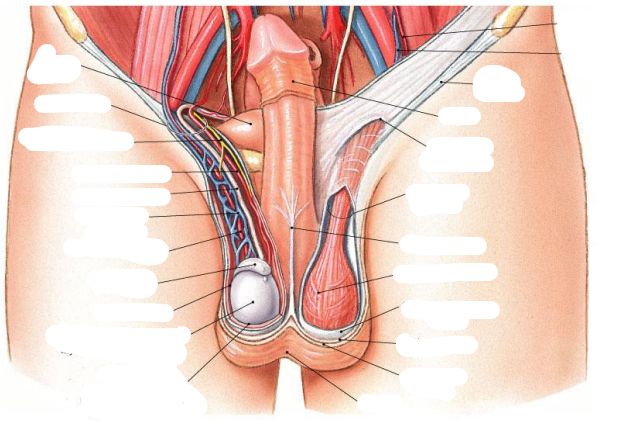
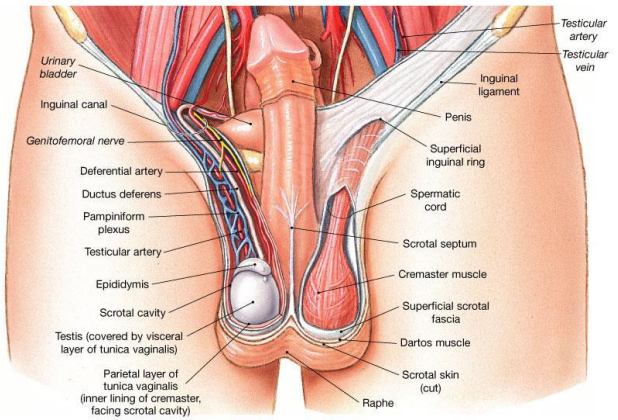
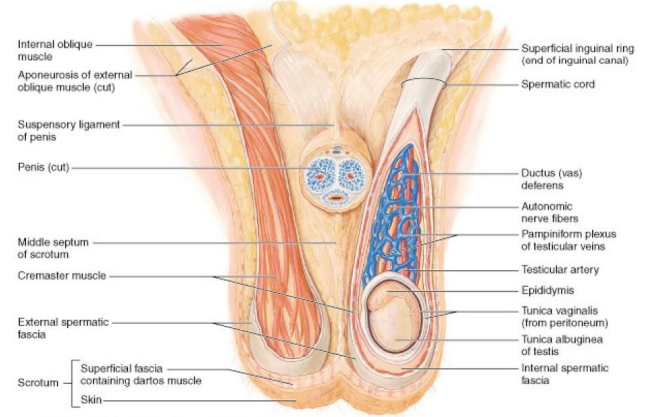
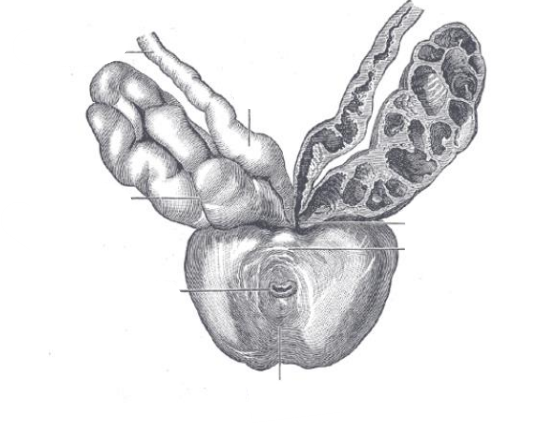
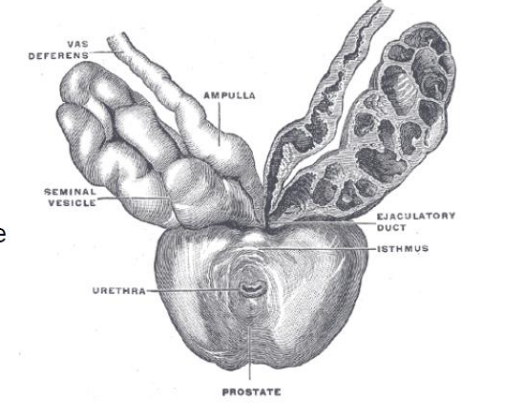
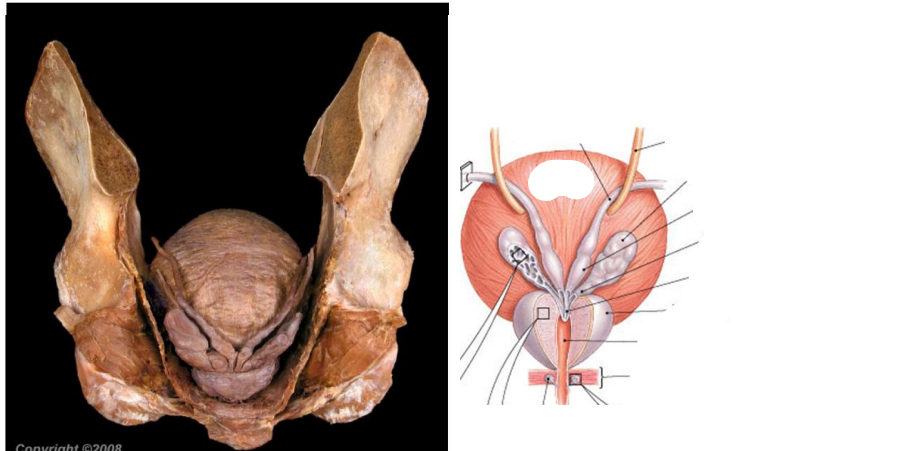
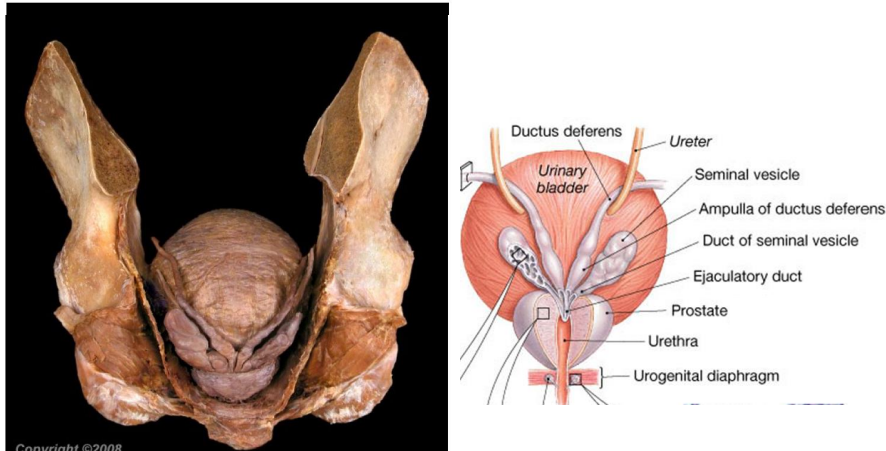
Ductus (vas) deferens path & structure
Begins at epididymis
Passes through inguinal canal
Enlarges to form ampulla
Ejaculatory duct at base of seminal vesicle and ampulla
Empties into urethra
Urethra path & region names
Urinary bladder → tip of penis
3 regions
Prostatic (most distensible)
Membranous
Penile
Typical ejaculate is how many ml of fluid
2-5ml
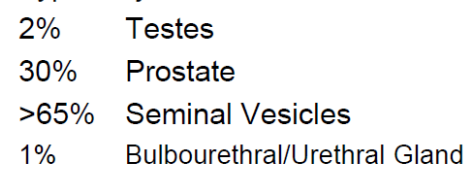
What percentage of semen comes from where
What do the seminal vesicles contribute to semen
Secretions contain fructose, prostaglandins & fibrinogen
What does the prostate contribute to semen
Proteolytic enzymes
Prostatic acid phosphatase
Prostate specific antigen
What do the bulbourethral glands contribute to semen
Secrete alkaline mucus with lubricating properties
What do the right & left gonadal veins generally drain into & how often does this actually occur (%)
Right gonadal vein drains directly into the IVC (seen in 78%).
Left gonadal vein drains into the left renal vein (seen in 79%).
About ___% of right and ___% of left gonadal veins show different drainage patterns than the classic RHS → IVC, LHS → L renal
About 22% of right and 21% of left gonadal veins show different drainage patterns.
Prevalence of variances in drainage pattern of the right gonadal vein
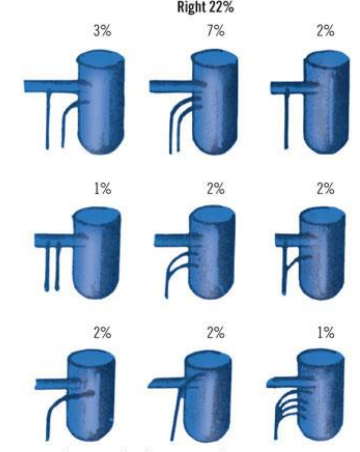
Prevalence of variances in drainage pattern of the left gonadal vein
What type of innervation does the pudendal nerve (in the lumbosacral plexus) provide?
Somatic innervation (motor and sensory)
Which spinal cord levels give rise to sympathetic innervation of the epididymis, vas deferens, seminal vesicles, and prostate gland
T12–L2
Pathway of T12-L2 nerves to the hypogastric plexus
The axons pass through the sympathetic chain, exit in the lumbar splanchnic nerves, and synapse on the neurons in the inferior mesenteric ganglion.
The postganglionic axons reach target tissues in the male reproductive system via hypogastric plexuses
Some preganglionic fibres from L1-L2 spinal segments descend in the sympathetic chain and synapse on postganglionic neurons in the hypogastric plexus.
The postganglionic fibres from these neurons then innervate the male erectile tissue
What is the effect of sympathetic activation on male reproductive organs
Ejaculation of spermatozoa and secretions from the prostate and seminal vesicles
Which spinal cord levels provide parasympathetic innervation to male erectile tissue?
S2–S4
Pathway of parasympathetic fibres to erectile tissue
The parasympathetic preganglionic fibres exit from the ventral roots, travel in the pelvic nerves, pass through the hypogastric plexus, and are distributed to the erectile tissue.
Activation of the parasympathetic nervous system results in what
the dilation of the arteries and increased blood flow in the corpora cavernosa causing erection of the male sexual organ
At what stage of development are the testes usually in the scrotum
8 lunar months (8th month of pregnancy)
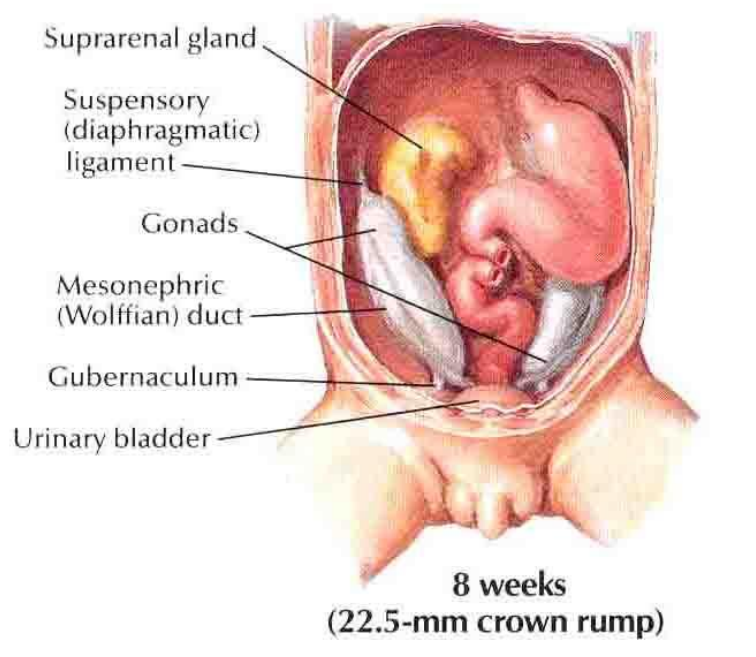
Explain the level of Testicular Descent at 8 weeks
8 weeks (22.5 mm crown-rump)
Testes (gonads) develop high on the posterior abdominal wall.
Positioned near the suprarenal gland and kidney.
Connected to the future scrotal region by the gubernaculum.
Suspensory (diaphragmatic) ligament present, later atrophies.
Mesonephric (Wolffian) duct present.
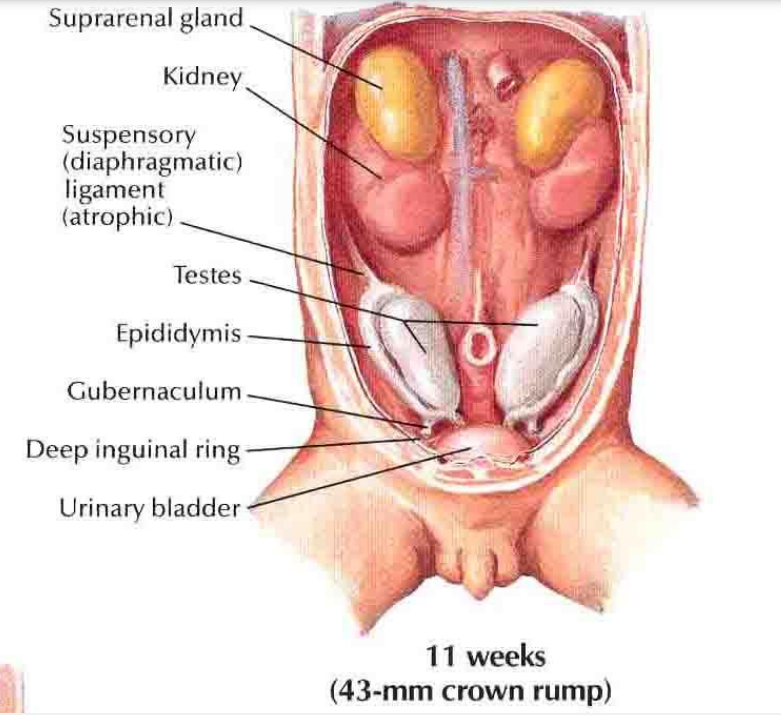
Explain the level of Testicular Descent at 11 weeks
11 weeks (43 mm crown-rump)
Testes descend slightly, now closer to the deep inguinal ring.
Epididymis begins to form along testis.
Gubernaculum persists, guiding testis downward.
Urinary bladder descends relative to the gonads.
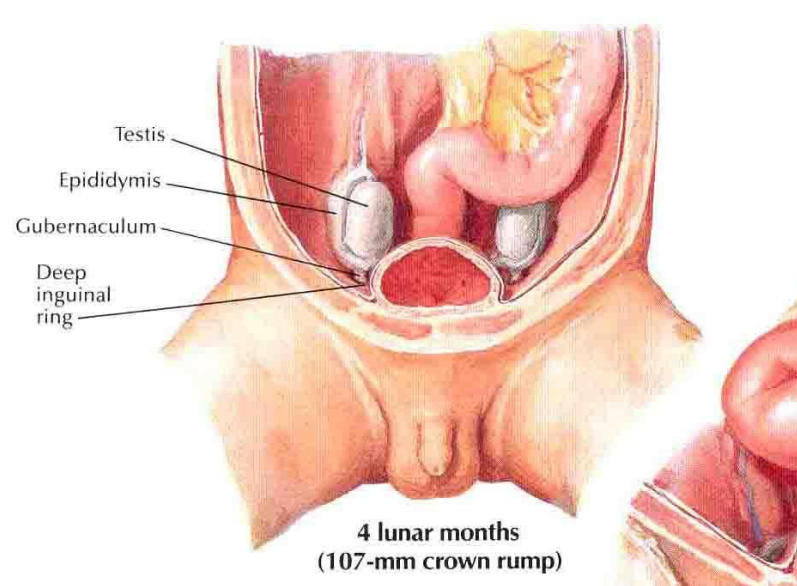
Explain the level of Testicular Descent at 4 lunar months
4 lunar months (107 mm crown-rump)
Testes approach the deep inguinal ring.
Epididymis more distinct.
Gubernaculum continues to shorten, pulling testes downward.
Testes preparing to enter the inguinal canal.
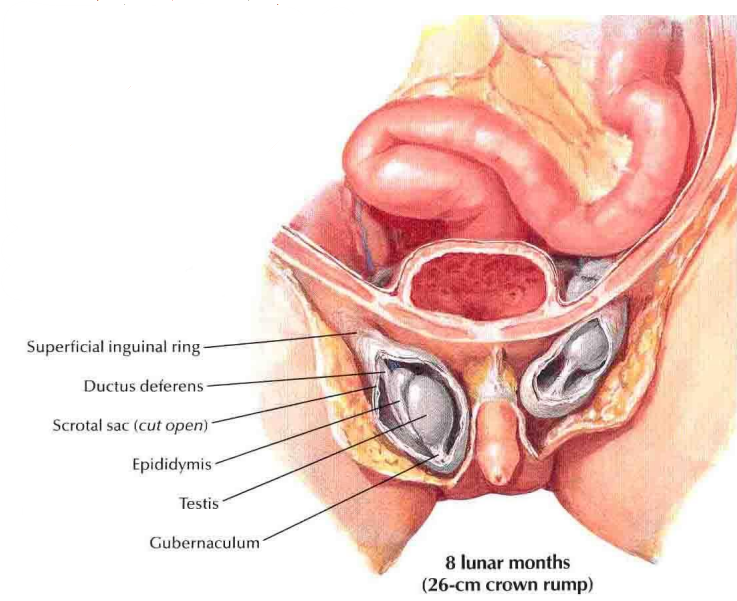
Explain the level of Testicular Descent at 8 lunar months
8 lunar months (26 cm crown-rump)
Testes have passed through the inguinal canal.
Located in the scrotal sac.
Superficial inguinal ring now behind them.
Ductus deferens visible.
Gubernaculum attaches testes to scrotal sac.
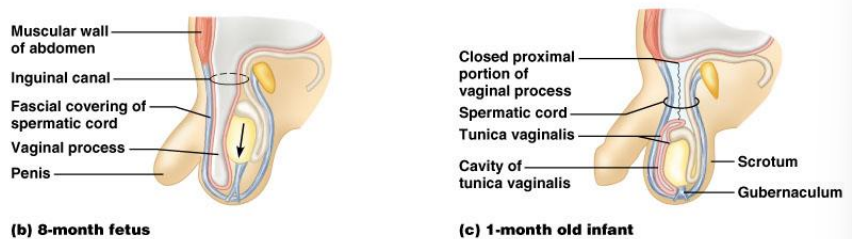
Compare level of Testicular Descent in an 8 lunar month fetus & a 1 month old infant
Cryptorchidism
absence of one or both testes from the scrotum.
(Most common birth defect of the male genital tract)
% incidence of cryptorchidism
3% of full-term and 30% of premature infant boys are born with at least one undescended testis. However, about 80% descend by the first year
True incidence of cryptorchidism around 1% overall.
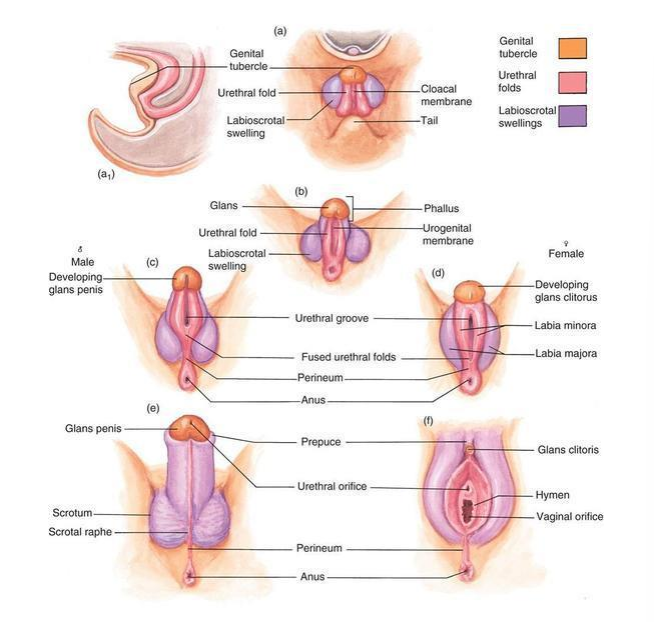
How is development of male genitalia similar to the development of female genitalia
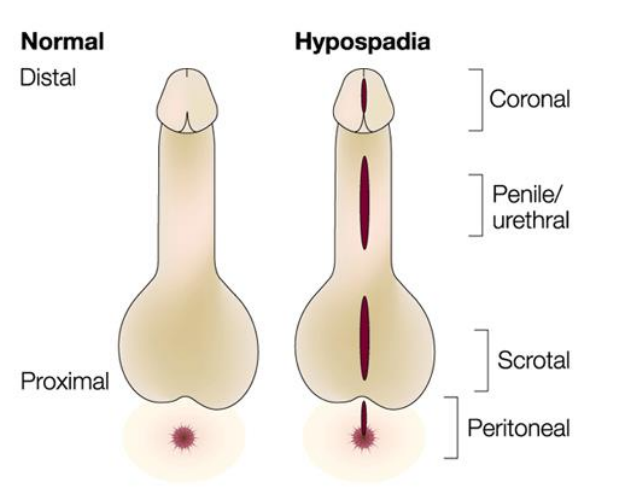
Hypospadias
A common variation in fetal development of the penis in which the urethra does not open from its usual location in the head of the penis.
2nd most common birth abnormality of the male reproductive system, affecting about one of every 250 males at birth.
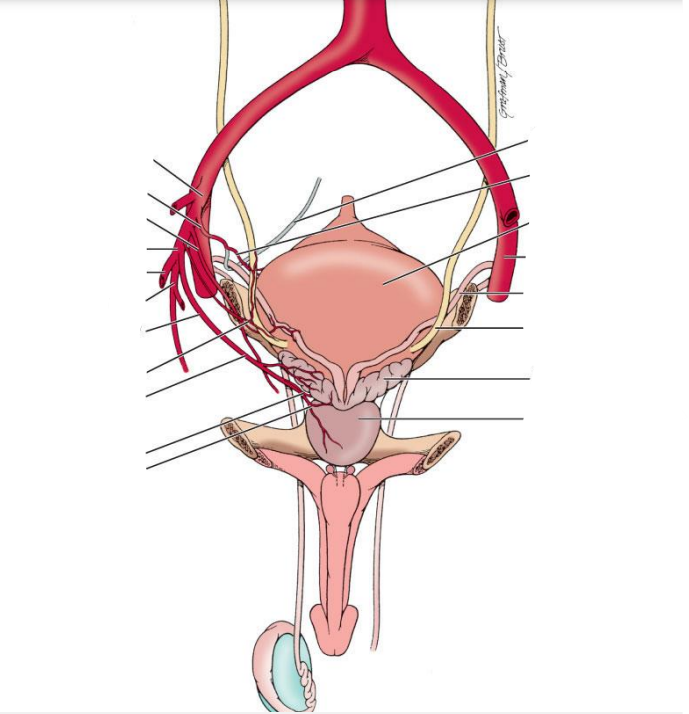
Benign prostatic hyperplasia (BPH)
Prostate enlargement - noncancerous increase in size of the prostate gland
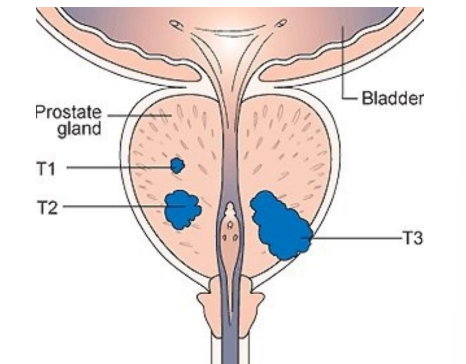
what does this diagram show
T1-3 stages of prostate cancer
(The most common cancer in males in 84 countries)
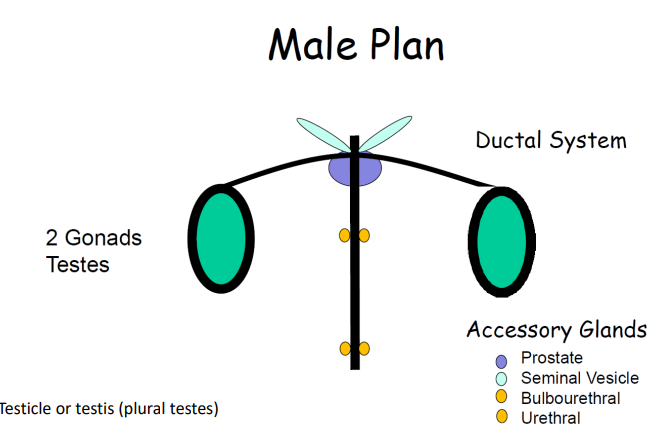
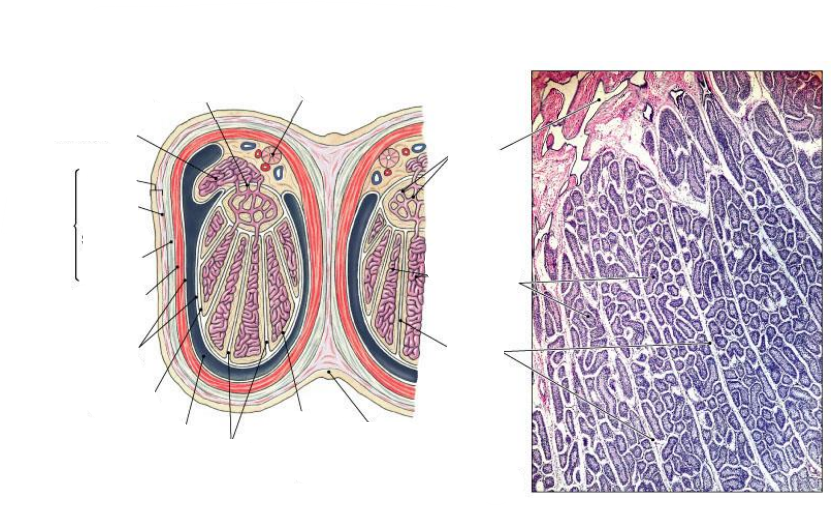
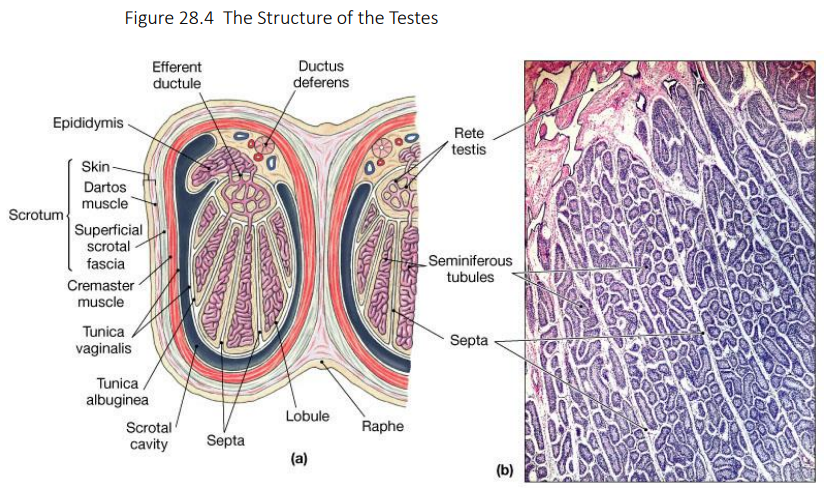
Scrotum contains the ________
Gonads
Sebaceous glands on the genitalia secrete what for what purpose
Sebaceous glands secrete an oily/waxy secretion called sebum. Sebum lubricates skin and hair, prevents water loss, and provides some antimicrobial defense.
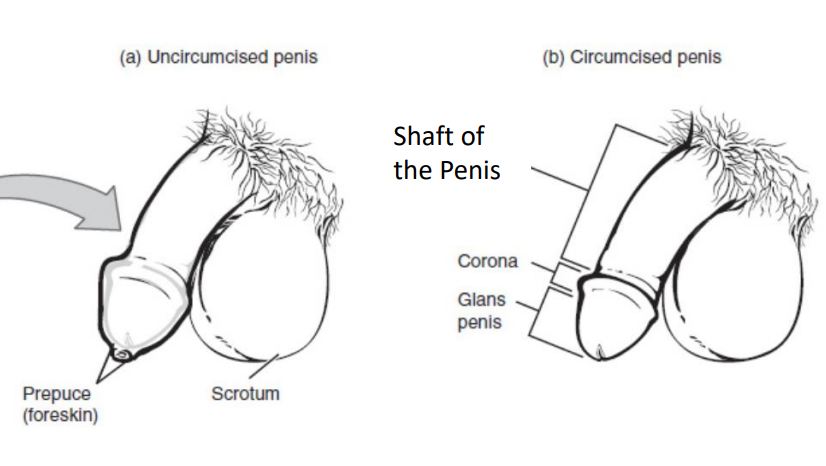
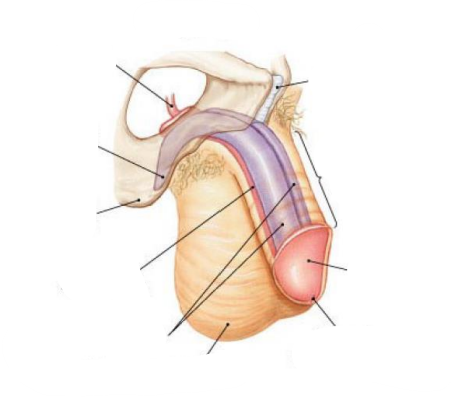
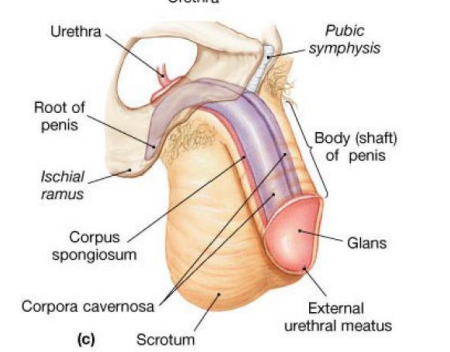
Of the 3 erectile columns of tissue that the penis is made up of, which one has the swollen end - the glans penis
The ventral one - corpus spongiosum
The proximal end of the penis is attached to what membrane
Perineal membrane
(The perineal membrane is a tough, fibrous sheet that spans the urogenital triangle of the perineum. The root of the penis is anchored to it: Bulb of penis (corpus spongiosum) attaches in the midline of the perineal membrane. Crura (corpora cavernosa) attach laterally to the ischiopubic rami, with their medial parts anchored at the membrane. After that, the penile shaft extends forward (anteriorly) and is free of the membrane)
What is the roughening along the ischiopubic rami for
The roughening along the ischiopubic rami is where the ischiocavernosus muscle (a thin sheet of skeletal muscle) attaches. It runs from the ischiopubic ramus → to the crus of the penis (the proximal part of the corpus cavernosum).
Which penile erectile column contains the penile urethra
Corpus spongiosum
What lie inferior to the prostatic urethra
the urogenital diaphragm (deep perineal pouch)
Towards the end of the prostatic urethra, two tubes open into it. What are the 2 tubes?
the ejaculatory ducts, formed by the union of the ductus deferens and seminal vesicles
Surgery to lengthen penis
make a small incision into the penile suspensory ligament, it can lengthen the penis by a small bit
What is the effect of contraction of the dartos & cremaster muscle on the scrotum & when would they contract
Dartos muscle = smooth muscle: From thinking about entering cold water, skin around the scrotum with shrivel up - contraction of dartos muscle
If you stay in cold water - testes will move up towards the body - cremaster muscle
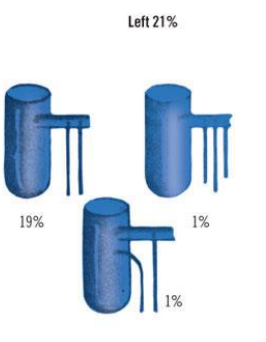
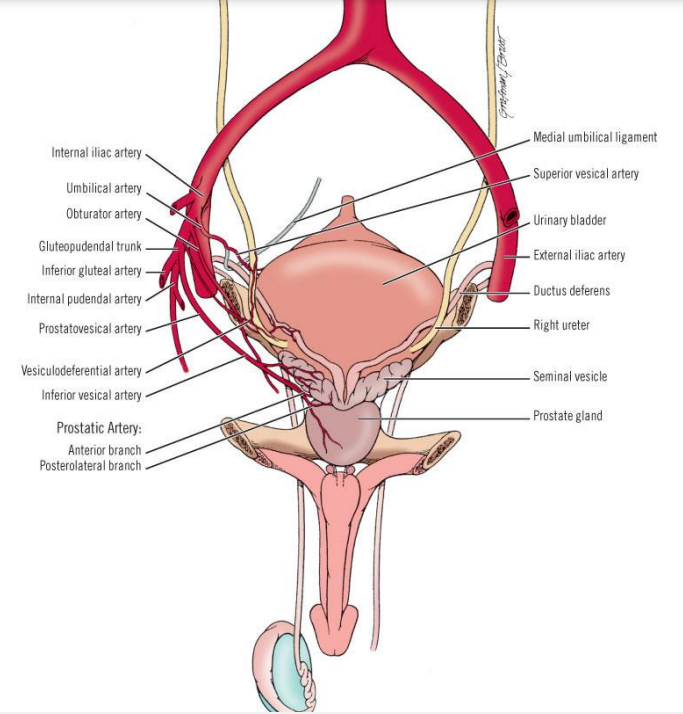
Blood supply to the gonads comes from where
Directly from the aorta - the testicular artery
Why are the testes located outside the abdominal cavity
temperature important in proper maturation of sex cells
intricate venous network around the testes =
pampiniform plexus
Role of bulbourethral glands
During sexual arousal / erection, they secrete a clear, mucus-like fluid into the spongy urethra.
Roles of this fluid:
Lubrication → reduces friction during intercourse.
Neutralizing acidity → helps flush out residual urine and neutralize acidic urine in the urethra, making a safer environment for sperm.
100s of seminiferous tubules combine to form what
Epididymis → a single, long, highly coiled tube where sperm mature and are stored

what is each part of this for (seminiferous tubule cross-section)
Epithelial cells (green in your image)
These are the Sertoli cells, which are tall, columnar cells lining the tubule.
Function: Support and nourish developing sperm cells (spermatogenic cells) and help move them toward the lumen.
Smooth muscle-like cells (yellow outer layer)
These are myoid cells, which are contractile cells surrounding the tubule.
Function: Perform peristaltic-like contractions to push sperm and fluid from the developing germ cells toward the lumen of the seminiferous tubule.
Lumen (center of tubule, brownish area)
This is where mature sperm are released before entering the rete testis → efferent ductules → epididymis.
Importance of the blood-testes barrier
keeps new genetic information in sperm from the immune system in the body
Major disruption to this barrier can be very dangerous
What are the first cells that go through reduction division in the formation of sperm
primary spermatocytes
Role of the acrosome
Enzymatic - help sperm penetrate the egg
The epididymis is where sperm mature and gain motility but what else happens here
A lot of the fluid in which sperm are suspended is reabsorbed.
This resorption of water concentrates the sperm and allows them to mature properly.
What % of semen is sex cells
1%
After ejaculation, what happens the semen
First that happens ejaculation is the semen coagulates - sticky substance left in vagina for a while until enzymes liquify it so that sperm can move freely
Match:
Parasympathetic / Sympathetic
Erection / Ejaculation
Parasympathetic - Erection
Sympathetic - Ejaculation
(Mnemonic: “Point and Shoot”)
The testes are pulled town into the pelvis by the what
gubernaculum (fibrous cord)
Most common form of hypospadias
Coronal
If you have hypospadias what are you more prone to
UTIs
Is prostate cancer or benign prostatic hyperplasia more common
Benign prostatic hyperplasia
What does Benign prostatic hyperplasia present as
Difficulty urinating
A man being grumpy could be a sign of what
Prostate cancer - their testosterone is too high