HSCI 366L FINAL
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
73 Terms
What is an echocardiogram?
Measures the heart’s movement, which helps to evaluate the heart’s pumping/mechanical
function
What is an echo usually used with?
A Doppler ultrasound and color Doppler techniques are used to evaluate blood flow across heart valves
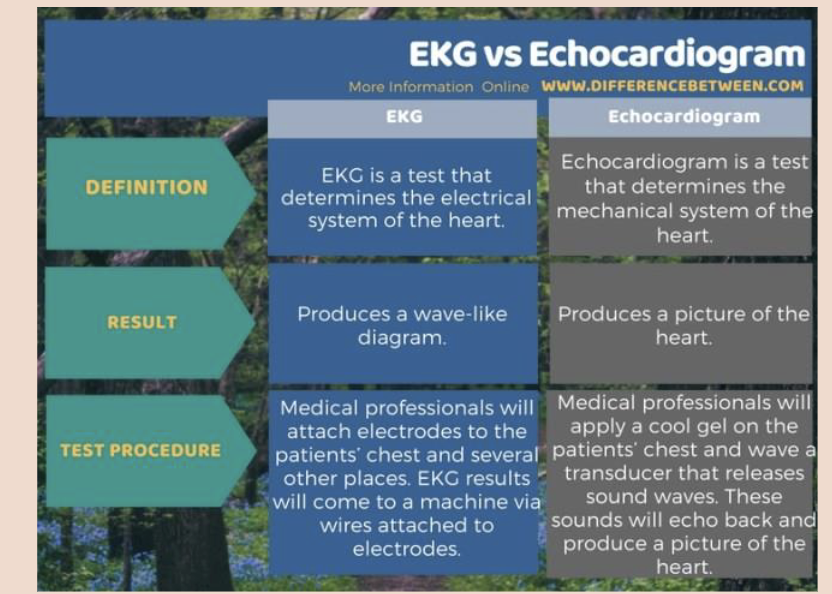
What is the difference between EKG and echo?
What is a TTE? What is it used for? What can it diagnose?
Transthoracic Echocardiogram: most common type that is noninvasive or minimally invasive
TTE is used to check the health of heart valves, determine how well the heart is pumping blood, measure blood pressure, and measure the size/shape of the heart chambers
It can diagnose aortic aneurysm/dissection, blood clots, ECG results, congenital heart diseases, heart failure, heart valve diseases, hypertrophic cardiomyopathy, cardiac tumors
What is a TEE? When is it used? What can it diagnose?
Transesophageal Echocardiogram: invasive because provider slides down an endoscope down the patient’s esophagus; TEE takes pictures of the heart from within the body, may take up to 90 minutes
May be used as a follow-up for TTE, emergency and critical care, check for blood clots before a medical procedure like cardioversion, confirms surgery success, real-time imaging for catheter-based procedures
Can be used to diagnose aortic aneurysms, blood clots, cardiac tumors, CHD, heart valve disease, infective endocardititis, pericaridal disease
What is a stress echo? When is it used? What can it diagnose?
It assesses the heart’s function when it is beating fast (usually performed on treadmill or stationary bike)
It can diagnose CAD, cardiomyopathy, CHD, heart failure, heart valve disease, pulmonary hypertension, aortic dissection, endocarditis, myocarditis, pericarditis, persistent chest pain, recent heart attack, severe aortic stenosis, uncontrolled arrhythmia
2D vs 3D echo techniques
Two-dimensional (2D) ultrasound: This
approach is used most often. It produces
2D images that appear as “slices” on the
computer screen. These slices could be
“stacked” to build a 3D structure.
• Three-dimensional (3D) ultrasound:
Advances in technology have made 3D
imaging more efficient and useful. New 3D
techniques show how well the heart pumps
blood. This technique also allows the
sonographer to view the heart from
different angles.
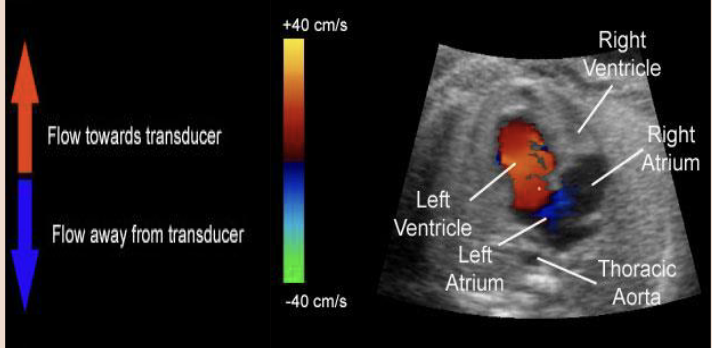
Doppler Ultrasound vs Color Doppler Ultrasound
Doppler ultrasound: This technique shows how fast blood flows and in what direction.
• Color Doppler ultrasound: This technique also shows blood flow, but it uses different colors to highlight the different directions of flow.
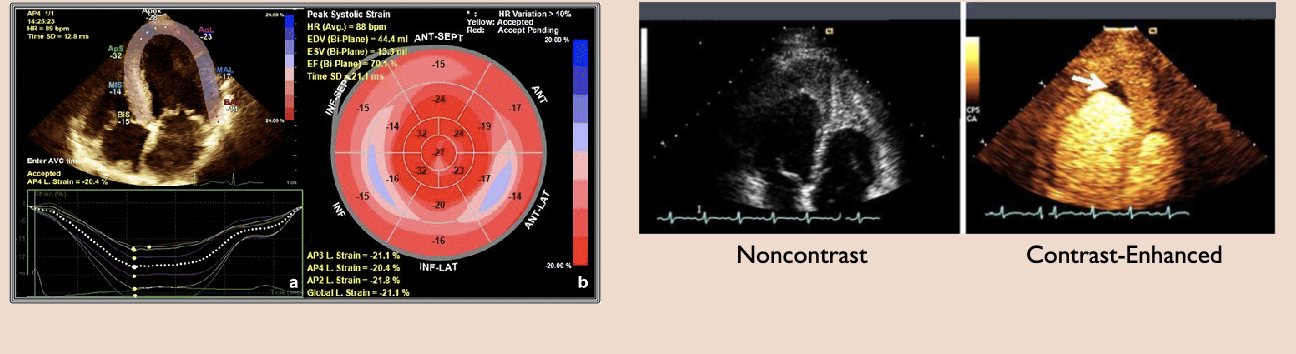
Strain imaging vs contrast imaging
Strain imaging: shows changes in how the heart muscle moves. It can catch early signs of heart disease
Contrast imaging: A contrast agent is injected into a vein. The contrast agent is visible in the images and can show details of the heart
What is a transducer?
A transducer is a device that produces
sound waves that bounce off body tissues
and make echoes.
The transducer also receives the echoes
and sends them to a computer that uses
them to create a picture called a
sonogram
What type of transducer is used in echo?
Phased Array transducer (Cardiac Sonography)
Different planes that can be shown in relation to transducer
Sagittal Plane: When the transducer is placed over the chest and the indicator
on the transducer is pointing up toward the patient’s head, the ultrasound beam
“slices” the patient’s heart in the sagittal plane.
• Transverse Plane: When the transducer is placed subcostally (below the rib
cage) and the indicator on the transducer is pointing toward the right side of
the patient’s body, the ultrasound beam “slices” the patient’s heart in the
transverse plane.
• Coronal Plane: When the transducer is placed along the mid-axillary line and
the indicator on the transducer is pointing toward the patient’s axillary region,
the ultrasound beam “slices” the patient’s heart in the coronal plane.
• Long Axis and Short Axis: Sometimes structures do not lie in the classic
planes. In that case, the long axis or short axis of the heart is used to perform
the Echo.
How does the transducer work?
The ultrasound beam shines from the near field (narrow tip of the triangular screen image) to the far field (wide base of the triangular screen image).
• Therefore, if you place the transducer over the chest the near field is anterior and the far field is posterior.
• If you place the transducer on the left side of the body in the midaxillary region, near field is left and far field is right.
• If the transducer indicator is pointing toward the patient’s head, and the screen indicator is on the top left, the left side of the Echo screen is showing superior structures and the right side of the screen is showing inferior structures.
• If the transducer indicator is aligned laterally over the chest pointing to the patient’s right and the screen indicator is on the top left, the left side of the Echo screen is showing heart structures on the right side and the right side of the screen is showing heart structures on the left side.
Basic Views in Echo
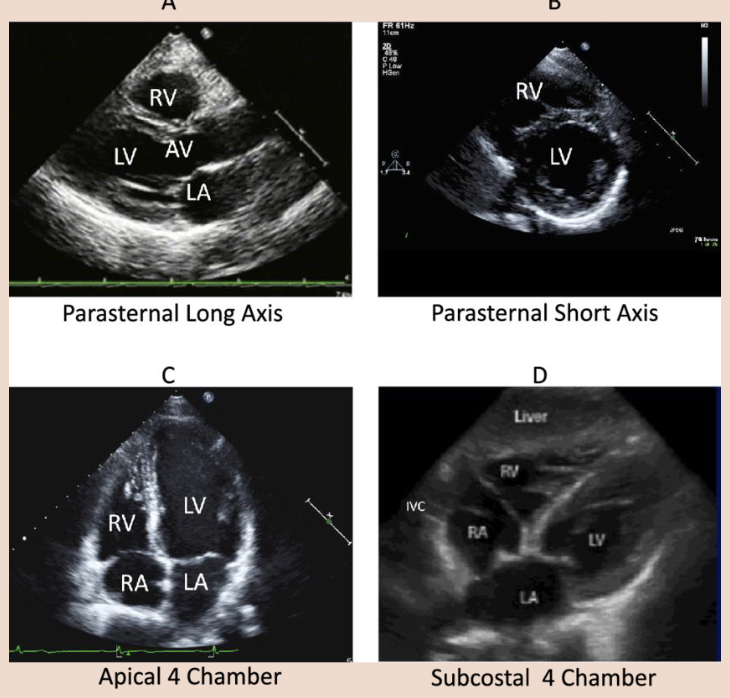
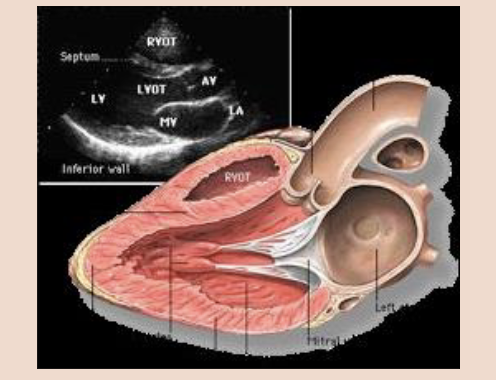
What is the parasternal long axis view?
The aim in this view is to orientate the beam with the long axis of the left ventricle (LV).
• The transducer is placed to left of the sternum in the 3rd, 4th, or 5th intercostal space with the
transducer indicator orientated towards the right clavicle (approximately 11 o’clock).
• PLAX allows for excellent images of the right ventricle (RV), left atrium, left ventricle, mitral valve, aortic valve, aortic root, aortic outflow tract, and the surrounding pericardium.
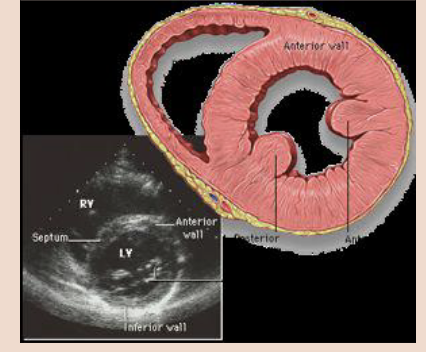
What is the parasternal short axis view?
In the PSAX view, the transducer remains in the intercostal space used to obtain the parasternal long axis view and is rotated clockwise 90 degrees so that it is perpendicular to the long axis of the LV (probe marker to left shoulder). It is then tilted to sweep through from base to apex of the heart,
obtaining a number of different views.
• PSAX examine the shapes and sizes of the ventricles. The LV should be bigger than the RV. The LV should be round, and the RV crescent shaped like a reverse letter ‘D’.
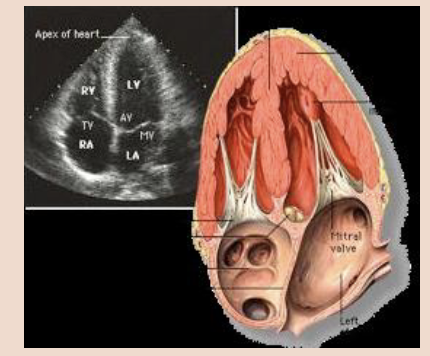
What is the Apical 4-Chamber view?
In this view, the transducer is placed at the point of maximum impulse if the patient has a palpable apical beat. Otherwise, it is placed in the fifth intercostal space near the anterior axillary line.
• The beam is directed up towards the patient’s head, and the transducer is rotated so the marker is at around 3 o’clock.
• This view is helpful for the identification of pericardial effusion (fluid between the heart and
pericardium) which indicates cardiac tamponade, as well as RV dilation in pulmonary embolism.
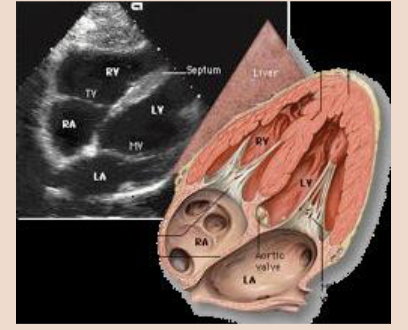
What is a subcostal 4-Chamber view?
This window may provide the only achievable view in technically difficult patients such as those with chronic obstructive pulmonary disease or who are receiving mechanical ventilation.
• The patient is supine and if possible, the knees are slightly bent to reduce abdominal wall tension.
• The transducer is placed below and slightly to the right of the xiphisternum.
• The side marker is in the 3 o’clock position and the transducer is tilted anteriorly. It may be necessary to push slightly downwards into the abdomen in order to achieve this scan plane.
• The subcostal view shows the Inferior Vena Cava (IVC) in a long axis.
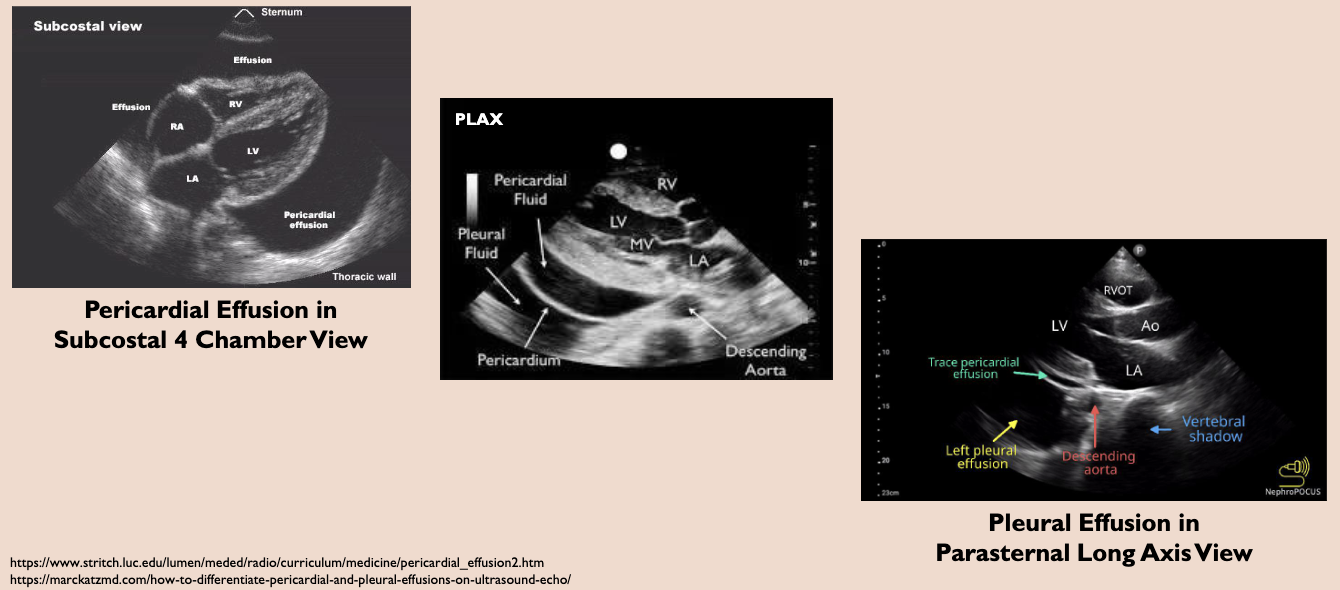
What is pleural effusion?t
The buildup of fluid between the lungs and the pleural membranes. Can occur due to inflammation or congestive heart failure (CHF)
What is pericardial effusion?
the buildup of fluid between the heart and the pericardial membranes. Can occur due to Pericarditis (inflammation of pericardium).
What is cardiac/pericardial tamonade?
Pericardial effusion puts pressure on the heart which prevents it from filling properly (diastolic collapse of right ventricle, with symptoms of hypoperfusion) causing Cardiac Tamponade. This will cause blood pressure to drastically drop; and can be fatal.
What is ejection fraction?
EF is the measurement of the percent of
blood leaving the heart each time it pumps.
EF (%) = (SV/EDV) x 100
Where, SV =Stroke Volume, EDV = End Diastolic Volume
EF > 50% is normal, EF of 30-50% is moderately depressed, EF < 30% is severely depressed.
What is congestive heart failure?
can occur if the heart cannot pump (systolic) or fill (diastolic) adequately. Left-sided CHF will occur due to left ventricle dysfunction and result in decreased EF
What can Decreased EF be caused by?
also be caused by aortic regurgitation (backflow of blood from Aorta which
prevents the mitral valve from opening fully), and mitral valve stenosis.
Pericardial Effusion vs Pleural Effusion
What is Patent Foramen Ovale?
a hole in the interatrial septum separating the right atrium from the left atrium.This opening exists during fetal development, but should close shortly after birth.
However, in some individuals the opening fails to close. Often this condition is asymptomatic.
What is atherosclerosis?
Deposition of plaque in the intimal layer of arteries (tunica intima/endothelial layer of
artery wall). Risk factors for atherosclerosis include hyperlipidemia, hypertension, and smoking.
Atherosclerotic plaques can be detected in a Carotid (artery) scan.
Bicuspid Valve Conditions
• Patent Foramen Ovale (PFO) – is a hole in the interatrial septum separating the right atrium from the left atrium.This opening exists during fetal development, but should close shortly after birth. However, in some individuals the opening fails to close. Often this condition is asymptomatic.
• Atherosclerosis – deposition of plaque in the intimal layer of arteries (tunica intima/endothelial layer of artery wall). Risk factors for atherosclerosis include hyperlipidemia, hypertension, and smoking.
Atherosclerotic plaques can be detected in a Carotid (artery) scan.
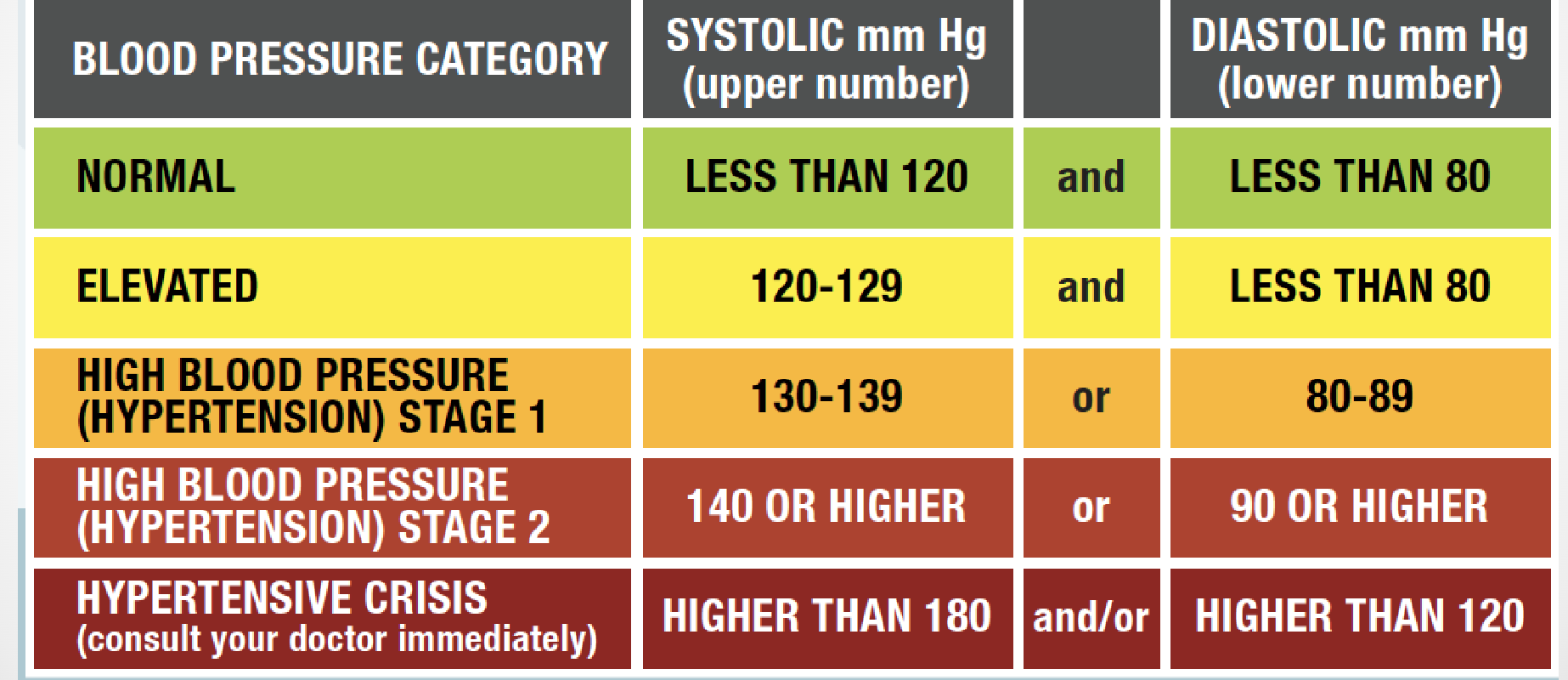
What is blood pressure?
Blood pressure is defined as the amount of force/pressure exerted against the walls of an artery and recorded as two
numbers, the systolic pressure and the diastolic pressure.
The unit of blood pressure is millimeters (mm) of Mercury (Hg).
What do you need to measure blood pressure?
Stethoscope and sphygmomanometer
What is the sphygmomanometer?
There are two types of sphygmomanometers;
aneroid and mercury filled.
• Given the units of BP, the mercury filled
sphygmomanometer rarely needs to be
calibrated.
• In contrast, the aneroid sphygmomanometer
may (in time) require calibration since its
operation depends upon a vacuum seal and
the seal can eventually wear out
What are the Krotkoff sounds to listen to?
① Phase 1 – appearance of a faint tapping sound “systolic pressure”
② Phase 2 – sound becomes louder and usually characterized by a
“swishing” sound
③ Phase 3 – sound is very distinct and loud
④ Phase 4 – sound becomes muffled and softer “diastolic pressure”
⑤ Phase 5 – sound disappears
How to measure BP at rest?
Wrap the cuff around the arm and secure
• Using the bulb, inflate the cuff about 30-40 mm Hg above where you anticipate the systolic pressure to occur. Typical systolic pressures for women ~110 whereas typical systolic pressure for men ~120
• Place the diaphragm over the brachial artery and deflate the cuff at a rate of 3-4 mm Hg per second
• Recall when you heard the first heart sound (i.e. Phase 1 tapping) →estimation for systolic pressure
• Continue deflating the cuff.
• Recall when the sound disappeared (i.e. Phase 5) →estimation for diastolic pressure
How do you measure BP at exercise?
It should be noted that the better estimation for diastolic pressure would be Phase 4 (muffling)
• At rest, however, Phase 4 and Phase 5 occur close together and it is easier to identify the disappearance rather than the
muffling.
• However, during hard exercise, it is possible that the heart sound never disappears. In this case, the estimation for diastolic pressure is Phase 4 (muffling) that will now be easier
to identify.
What is the auscultatory method?
The Auscultatory Method of taking blood pressure is considered the “gold standard” if performed by a
trained healthcare provider.
• However, there are other factors that can affect the accuracy using this method. Two of these factors are found below:
1. Cuff Size
Cuff Tension
What happens if cuff is too loose? Too tight?
However, the use of cuff that is too big or too loose for the arm, results in erroneously low blood pressure measures.
• Studies have shown that using too small or too tight blood pressure cuff can cause a patient's systolic blood pressure measurement to increase.
• Too wide a cuff will underestimate BP
• Too narrow a cuff will overestimate BP
What are the four major categories for HTN?
Treatment for HTN
Healthy diet and exercise
Diuretics
Ace Inhibitors
Beta blockers
Vasodilators
Normal BP Response to Exercise
Systolic pressure elevates with each increase in
workload due to stretch in the left ventricular wall and increased force to pump more blood.
• Diastolic pressure either remains the same or may decrease with each increase in workload due to the vasodilation of the arteries from the exercise bout
Abnormal BP Response to Exercise
Systolic pressure fails to elevate or declines after an increase in workload due to heart diseases that affect the heart’s ability to contract.
• Diastolic pressure elevates after an increase in
workload due to high pressure in the blood vessels while the heart is in diastole.
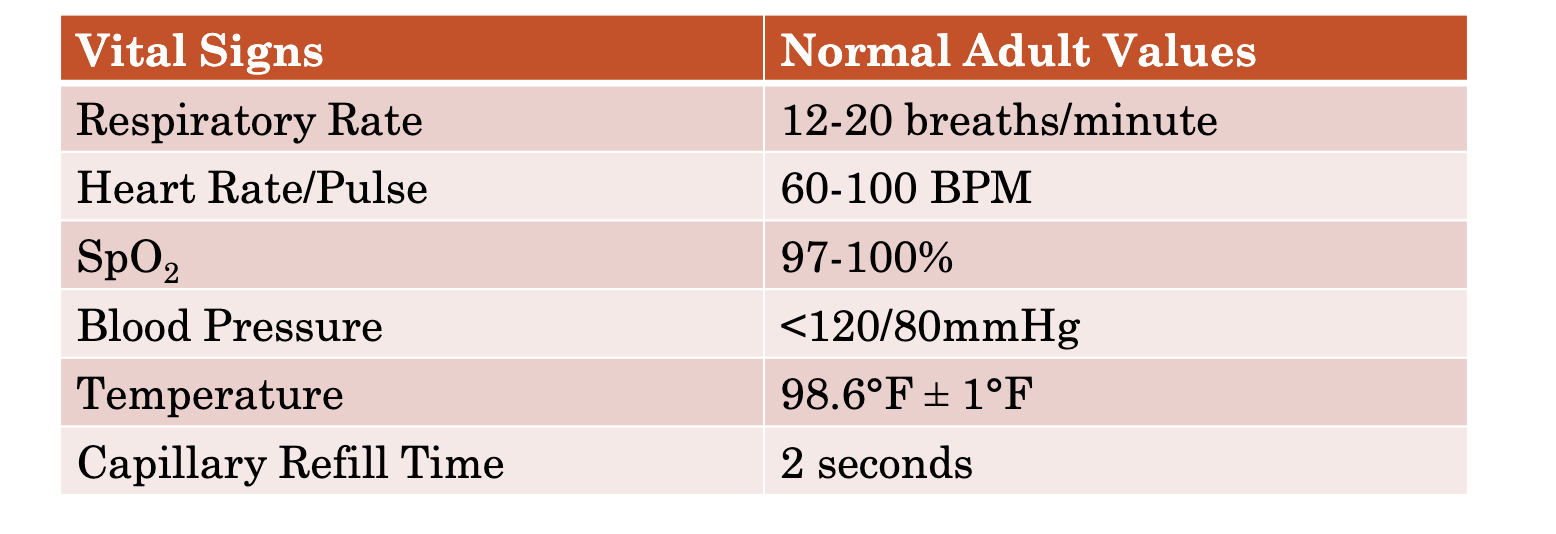
What do you measure for vital signs?
RR and quality, Pulse/heart rate and quality, skin assessment, pulse oximetry, blood pressure
What do you measure for primary survey?
Level of consciousness (LOC), level of distress (LOD), orientation, airway, breathing, circulation (ABC)
What do you measure for physical exam?
Head to toe exam, Pupils (PERRLA)
What do you measure for patient history?
complaints, diet and exercise, medical history, pain assessment
How do you measure respiratory rate?
Observe Rise and fall of chest
Do this WITHOUT patient’s knowledge
One breath= inhalation + exhalation
Respiratory rate= count in 30 seconds and multiply by 2
What are the different types of respiration quality?
▪ Normal respiration – involves average chest wall motion with at least 1 inch expansion in the outward direction. The person does not use accessory muscles of the chest, neck or abdomen. Exhalation is typically twice as long as inhalation. Normal breathing is quiet and does not produce noise.
▪ Shallow respiration – involves only slight chest or abdominal wall expansion during
inhalation.
▪ Labored respiration – patient is working hard to breathe, which can be indicated by
abnormal breathing sounds; nasal flaring; use of accessory muscles of the chest, neck or abdomen; and sometimes gasping. The use of accessory muscles requires more energy to be expended during breathing, which can lead to respiratory muscle
fatigue and subsequently respiratory failure.
▪ Noisy respiration – involves abnormal breathing sounds such as snoring and
stridor which can be heard without a stethoscope; or wheezing, rales, and rhonchi
which can be heard with a stethoscope. All noisy breathing is obstructed breathing, but not all obstructed breathing is noisy.
How to measure pulse/heart rate?
Pulse is the pressure wave generated by the contraction of the left ventricle; and it
can be felt at any point where an artery crosses over a bone near the surface of the
skin. The pulse provides an indirect measure of heart rate.
▪ The patient should be sitting or lying down when you measure their pulse.
▪ Use your index and middle fingers to measure pulse. Never use your thumb, as it
has a pulse of its own.
▪ Count the number of beats in a 30-second period and then multiple it by 2 if the
patient has a regular pulse. If the pulse is irregular, count for a full minute.
▪ Normal heart rate for an adult at rest is 60-100 beats per minute.
▪ A heart rate above 100 bpm is termed Tachycardia, and a heart rate below 60bpm
is termed Bradycardia.
▪ A heart rate above 130 bpm or below 45 bpm typically indicates a serious illness or
injury.
▪ Before coming to a diagnosis, ask the patient what their heart rate is typically like
at rest.
Where can pulses be found?
Pulse/Heart Rate can be located either
centrally or peripherally.
▪ Central pulses include Carotid and
Femoral.
▪ Peripheral pulses includes Radial,
Brachial, Popliteal, Posterior Tibial, and
Dorsalis Pedis.
▪ Today, we will assess the Radial Pulse,
which can be found proximal to the thumb
on the palmar surface of the wrist.
▪ The radial pulse is assessed in all patients
1 year or older. For infants younger than 1
year, the brachial pulse is assessed.
▪ When a peripheral pulse cannot be
obtained in a person 1 year or older, the
carotid pulse is assessed.
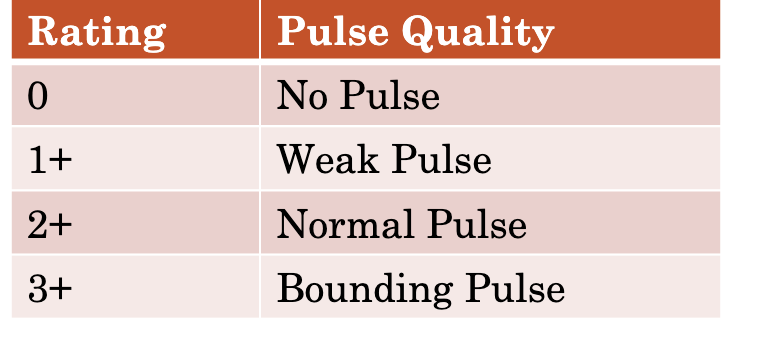
How to determine pulse quality?
▪ Strong pulse – is a pulse that is both full and normally strong. A “bounding” pulse is abnormally strong.
▪ Weak pulse – is a pulse that does not feel full or is difficult to find or palpate. A weak pulse might also be rapid. The term used for a weak, rapid pulse is “thready”.
▪ Regular pulse – is a usual, normal pulse that occurs at regular intervals.
▪ Irregular pulse – is a pulse that occurs at irregular intervals and might indicate cardiac disease. An irregular pulse can be regularly irregular or irregularly irregular
Where should you look for skin assessment?
▪ In all patients, check the color of the nail beds, oral mucosa, and conjunctiva. In dark-
skinned people and children, check the palms of the hand and soles of the feet. All these
areas should be pink.
▪ Abnormal skin colors include:
✓ Paleness/Pallor (white) – might indicate vasoconstriction, blood loss, shock
(hypoperfusion), heart attack, fright, anemia, fainting, or emotional distress. Pale, cool,
and clammy (moist) skin might be an early sign of inadequate oxygenation, hypoxia and
hypoxemia.
✓ Blue-gray color/Cyanosis – indicates inadequate oxygenation or perfusion, inadequate
respiration, suffocation, hypoxia, hypoxemia, heart attack, or poisoning. Cyanosis
always indicates a serious problem but is often observed very late.
✓ Red color/Flushing – might indicate heat exposure, peripheral vasodilation, or a very
late sign of carbon monoxide poisoning.
✓ Yellow color/Jaundice – might indicate liver disease.
✓ Gray/blue color/Mottling – discoloration is similar to cyanosis, but it occurs as a blotchy
pattern. Mottled skin can be seen in some shock patients, or patients with blood pooling
in the extremities.
Temperature analysis for skin assessment
▪ Average normal body temperature in adults at rest is 98.6°F (37°C).
▪ The normal temperature can vary due to factors such as: age, differences among
individuals, time of day (often highest in the evening), and which type of
measurement was taken (oral, rectal, armpit, or forehead).
▪ Today, we will measure temperature using a forehead thermometer.
▪ A forehead scanner is most often 0.5°F (0.3°C) to 1°F (0.6°C) lower than an oral
temperature.
▪ A temperature of more than 99.6°F (37.5°C) in an adult; or a temperature more
than 1°F – 1.5°F above the person’s normal temperature is considered a fever.
Skin condition analysis for skin assessment
Skin is normally dry.
▪ Wet or moist skin might indicate shock; poisoning; or a heat-related, cardiac or
diabetic emergency.
▪ Skin that is both cool and moist is often termed clammy skin.
▪ Profuse sweating is termed Diaphoresis.
▪ Extremely dry skin might be a sign of spinal injury or severe dehydration.
What is the capillary refill time?
▪ The time it takes for compressed capillaries to fill with blood again is called capillary refill time. It is a more reliable sign in infants and younger children compared to older children or adults.
▪ A cold environment, preexisting circulatory conditions and certain medications can
influence capillary refill time. It can also be difficult to assess in dark-skinned
people.
▪ To measure capillary refill time, press firmly on the skin or nail bed. When you remove your finger, the nail bed will be white. Count the time it takes for the return of the original pink color.
▪ At room temperature, the upper limits of capillary refill time are 2 seconds for
infants, children and male adults; 3 seconds for female adults; and 4 seconds for the
elderly.
▪ A longer capillary refill time might indicate shock
What is blood oxygen saturation?
Pulse oximetry is a method of measuring oxygen saturation levels in the hemoglobin of blood.
▪ The probe of the pulse oximeter is typically placed around the patient’s finger where infrared
light from the probe can shine through tissue and arterial blood flow to a photo sensor on the
opposite side of the probe. The light detects the amount of hemoglobin in the blood that is
saturated with oxygen. This is recorded at % SpO2.
▪ Connect the probe to the pulse oximeter and attach the probe to the patient’s fingertip.
▪ Turn on the device and wait a few seconds for the SpO2 reading to appear.
▪ Reassess SpO2 every 5mins in an unstable patient, and every 15mins in a stable patient.
▪ A pulse oximeter reading for a person breathing room air is typically between 97-100%.
▪ An SpO2 reading of <90% is a definite indication of hypoxia.
▪ One limitation of the device is that it will also measure other gases containing oxygen that
may be attached to hemoglobin in the blood, such as carbon monoxide.
What are “normal” vital signs?
How to determine LOC?
The patient’s LOC can be quickly assessed by using the mnemonic AVPU, which stands for
Alert, responds to Verbal stimulus, responds to Painful stimulus, or Unresponsive.
▪ A patient who responds to a verbal stimulus has a higher level of consciousness compared to
one who only responds to a painful stimulus, who has a higher level of consciousness
compared to one who is unresponsive.
▪ With response to verbal stimulus, if the patient obeys a command such as “wiggle your toes”,
they have a higher level of responsiveness than a patient who stares off or mumbles
incomprehensibly.
▪ If there is no response when you speak, use a painful stimulus to determine if they respond.
▪ To apply a central painful stimulus, you can use the Trapezius Pinch, or the Sternal Rub.
▪ To apply a peripheral painful stimulus, pinch the web between the thumb and index finger.
Trapezius Pinch Sternal Rub Thumb-Index Finger Pinch
How do you determine the level of LOC?
If the patient reaches up and grabs your hand
following a painful stimulus, they have a
higher level of consciousness compared to
someone who just moves their arm towards
the pain.
▪ Patients with head injury or spinal cord injury
might respond to pain abnormally. A patient
with spinal cord injury might respond only to
pain applied above the site of injury or to one
side of the body.
▪ Two non-purposeful movements that are not
related to pain response are flexion posturing/
decorticate posturing where the patient
arches the back and flexes the arms inward
toward the chest, and extension posturing/
decerebrate posturing where the patient
arches the back and extends the arms straight
out parallel to the body. Both postures are
signs of serious head injury.
Questions to ask for orientation
Person, place, time, situation
What do you look for in pupil exams?
Normal pupils are about the same size (equal). But, for about one in five people, one is
bigger than the other. This condition is called Anisocoria and may be harmless. In normal,
or “physiologic anisocoria,” pupils will react to changes in light the way they should. A
number of serious health conditions can also cause unequal pupils.
▪ Normally pupils should be perfectly round circles. Abnormal pupils may look like a keyhole
or a cat’s eye.
▪ The iris muscles open and close the pupil in response to light. Normal pupils get smaller in
brighter light and larger in the dark.
▪ To observe the patient’s pupil response to light, perform the “swinging light test.” Using a
penlight (small light with a narrow beam), shine it first into one eye for about 3 seconds and
then into the other for 3 seconds. Normal pupils shrink in reaction to bright light. Both the
pupils should get smaller together, even when you shine direct light into only one eye at a
time. Both pupils should get bigger once it’s dark again.
▪ The pupils should also constrict when they are focusing on an object very close to the eye and
dilate when focusing on an object far away. This is termed accommodation.
▪ To assess pupils for accommodation, turn off the penlight and hold it close to the patient’s
eyes a few inches in front of the bridge of their nose and ask them to focus on the penlight.
Their pupils should constrict in response. Then move the penlight (still turned off) several
more inches away from the bridge of their nose and ask them to focus on the penlight which
is now farther away. Their pupils should dilate in response.
Potential pupil problems
Dilated pupils – might indicate cardiac arrest (in which case pupils will also be fixed), or use
of drugs such as LSD, amphetamines or cocaine.
▪ Constricted pupils – might indicate a central nervous system disorder, or use of narcotics.
▪ Unequal pupils – might indicate stroke, head injury, or eye trauma.
▪ Nonreactive pupils – might indicate cardiac arrest, brain injury, or drug overdose.
What is the markle test?
Use the Markle test, also called the heel drop test to assess abdominal pain. If the
patient can stand, ask them to stand on the balls of their feet and then suddenly
drop down onto their heels. If they grimace or complain of pain, abdominal pain is
present. This is a positive Markle sign
Lower Extremity Physical Exam
Circulatory, Motor, & Sensory (CMS)
▪ Range of Motion (ROM)
▪ Does the patient have pedal edema?
▪ Check Babinski Reflex by firmly stroking the plantar surface of the feet. A normal
negative response in adults is when the toes flex. If the big toe moves upward and the
other toes fan out, the person has a positive Babinski Reflex. This reflex is normal in
infants <2 years. In adults it is a sign of CNS disorders.
Upper Extremities Physical Exam
Circulatory, Motor, & Sensory (CMS)
▪ Range of Motion (ROM)
▪ Check if patient has pronator (arm) drift. This is an indication of Stroke.
▪ Does the patient have an AV Fistula? This indicates that they are a Dialysis patient
What is minute ventilation?
The volume of air a person inhales and exhales
in one minute.
Calculating Minute Ventilation:
Calculate the person’s tidal volume (volume of air expired and inspired
during quiet breathing).
Count the number of times the person breathes in 1min (inhalation +
exhalation).
Multiply the tidal volume by the number of breaths per minute to get the
minute ventilation.
Minute Ventilation = Tidal Volume x Breaths in 1min.
Minute Ventilation for average-sized adult = 500ml x 12/min = 6000ml/min
What is alveolar ventilation?
Alveolar Ventilation is the amount of air moved in and out of the alveoli in one
minute.
Both tidal volume and the frequency of breaths per minute have to be within the
normal range to ensure the person has adequate alveolar ventilation
How do you calculate alveolar ventilation?
Calculate the volume of air in the dead air space, the areas in the respiratory tract
where air collects during inhalation but no gas exchange occurs.
Subtract the dead air space from the tidal volume, and multiply that number by
the number of breaths per minute to get the alveolar ventilation.
Alveolar Ventilation = (Tidal Volume – Dead Air Space) x Breaths in 1min.
Alveolar Ventilation for average-sized adult = (500ml – 150ml) x 12/min = 4200ml/min
What impacts alveolar ventilation?
Decreased tidal volume has a greater impact on respiration, and increased breathing rate does not compensate for decreased tidal volume.
What is the Borg Rating of Perceived Exertion (RPE) Scale?
The Borg Rating of Perceived Exertion (RPE) scale is a subjective method of quantitatively measuring the intensity of physical activity.
In this test, the subject rates how hard they feel like their body is working during an exercise test.
It is based on the physical sensations that the subject experiences during physical activity, including increased heart rate, increased
respiration or breathing rate, increased sweating, and muscle fatigue.
Scientific evidence indicates that the subject’s self-perceived exertion rating provides a fairly good estimate of their actual heart
rate during physical activity.
The Borg RPE Scale is a numerical scale that ranges from 6-20
Healthy Individual’s Response to Exercise
Respiration: Rate and depth of breathing increase.
Heart Rate: Increases with exercise.
Blood Pressure: Systolic pressure increases, while diastolic pressure either stays
the same or decreases.
Perceived Exertion Rating: Light to Somewhat hard based on exercise intensity.
How would Ischemic Heart Disease react to Exercise?
Respiration: Shortness of breath. Breathing deeper (tidal volume) during exercise is
better than breathing faster (frequency) to ensure adequate alveolar ventilation.
Heart Rate: Rapid heart rate.
Blood Pressure: Systolic pressure fails to increase or decreases, whereas diastolic
pressure increases.
Perceived Exertion Rating: Extreme exertion even with light intensity exercise.
Signs and symptoms of Ischemia observed during or after exercise:
Moderate to severe chest pain (Angina)
Severe shortness of breath
Abnormally high or low blood pressure
ST Segment changes in the ECG
An abnormal heart rhythm
Dizziness
Fatigue
How would Obstructive Pulmonary Disease alter response to Exercise?
Respiration: Extreme shortness of breath, rapid breathing, cough, chest tightness.
Heart Rate: Normal sinus rhythm.
Blood Pressure: Systolic pressure increases, while diastolic pressure either stays the
same or decreases.
Perceived Exertion Rating: Extreme exertion with heavy intensity exercise.
Signs and symptoms of Asthma observed during or after exercise:
Severe shortness of breath
Abnormally rapid breathing
Dry or persistent cough
Wheezing (typically expiratory) upon auscultation
Rapid heart rate
Use of accessory respiratory muscles
Excessive sweating
Chest tightness
How do you determine work?
Work = Force x Distance
Distance on the Monarch: Flywheel is 2 meters (circumference) and spins
3 times per pedal revolution. Thus, at 50 RPM, the distance is (2 meters x 3
flywheel revolutions) 6 meters x 50 RPM = 300 m/min
Force on the Monarch: The amount of resistance applied to the flywheel
expressed in kg.
If you apply 2 kg of force while pedaling at 50 RPM, the work would be: 2kg x 300 m/min = 600kgm/min
How do you calculate Power?
Watts = work/6 watts/kgm/min