AT 505 ch.8 pt1
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
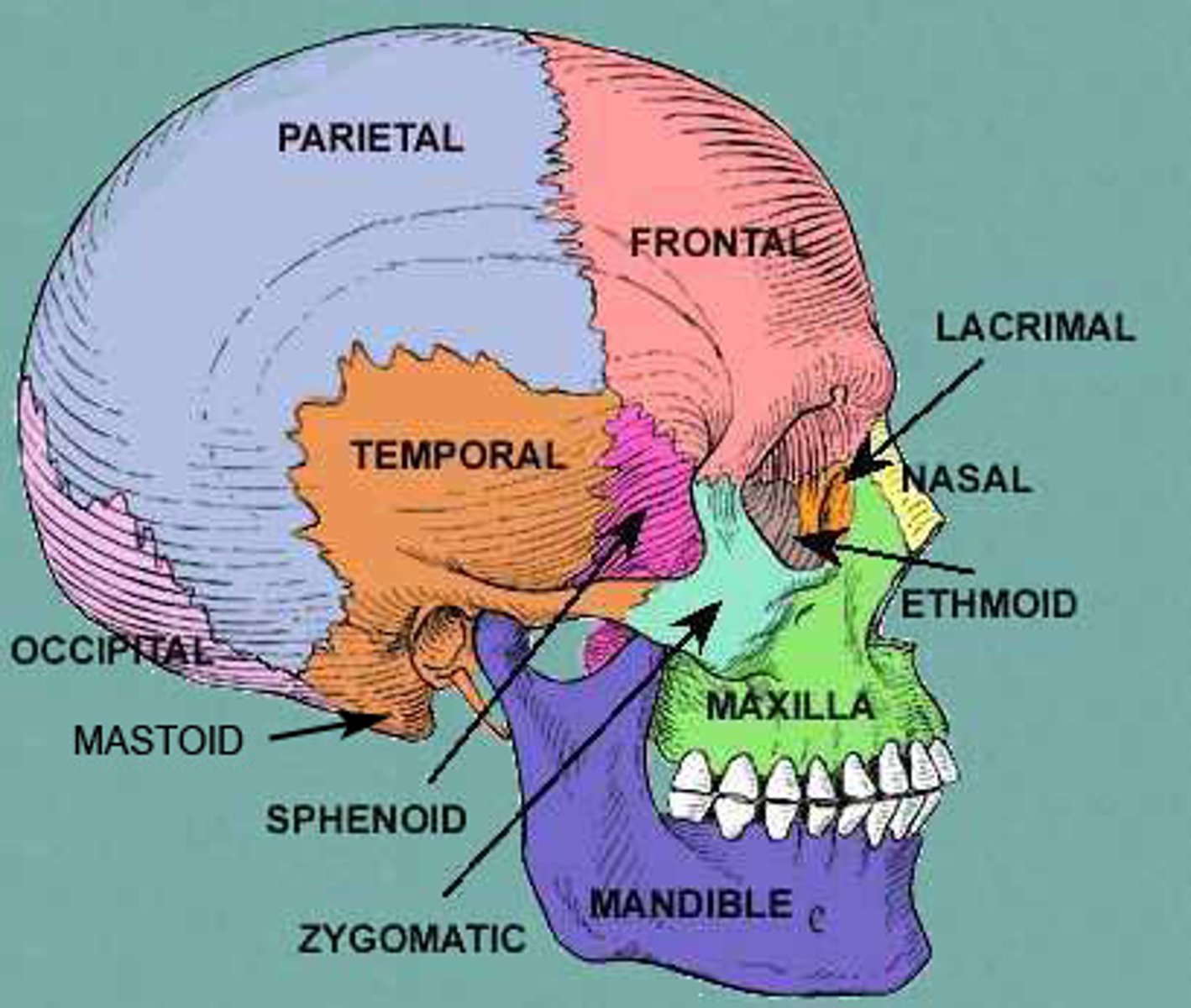
skull
Cranium and facial skeleton
• Ethmoid, frontal, occipital, parietal, sphenoid, and temporal bones• Lacrimal, mandible, maxilla, and nasal bones
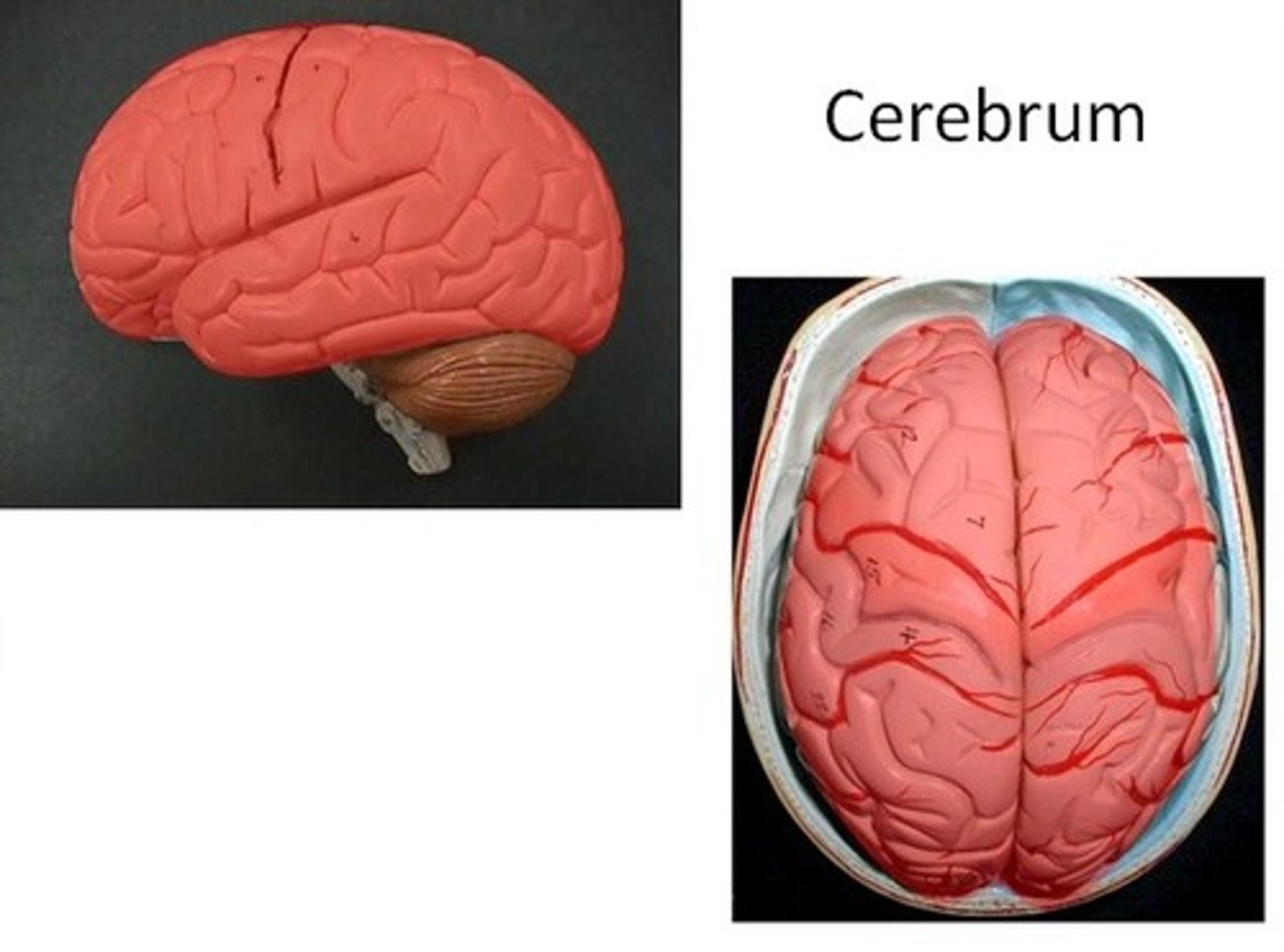
Cerebrum
Compromises about 75% of the total brain volume
• Control voluntary muscle activities, sensation, and higher-level brain functions such as emotion,hearing, learning, memory, personality, and vision.
Cerebellum
Responsible for coordinated body movement

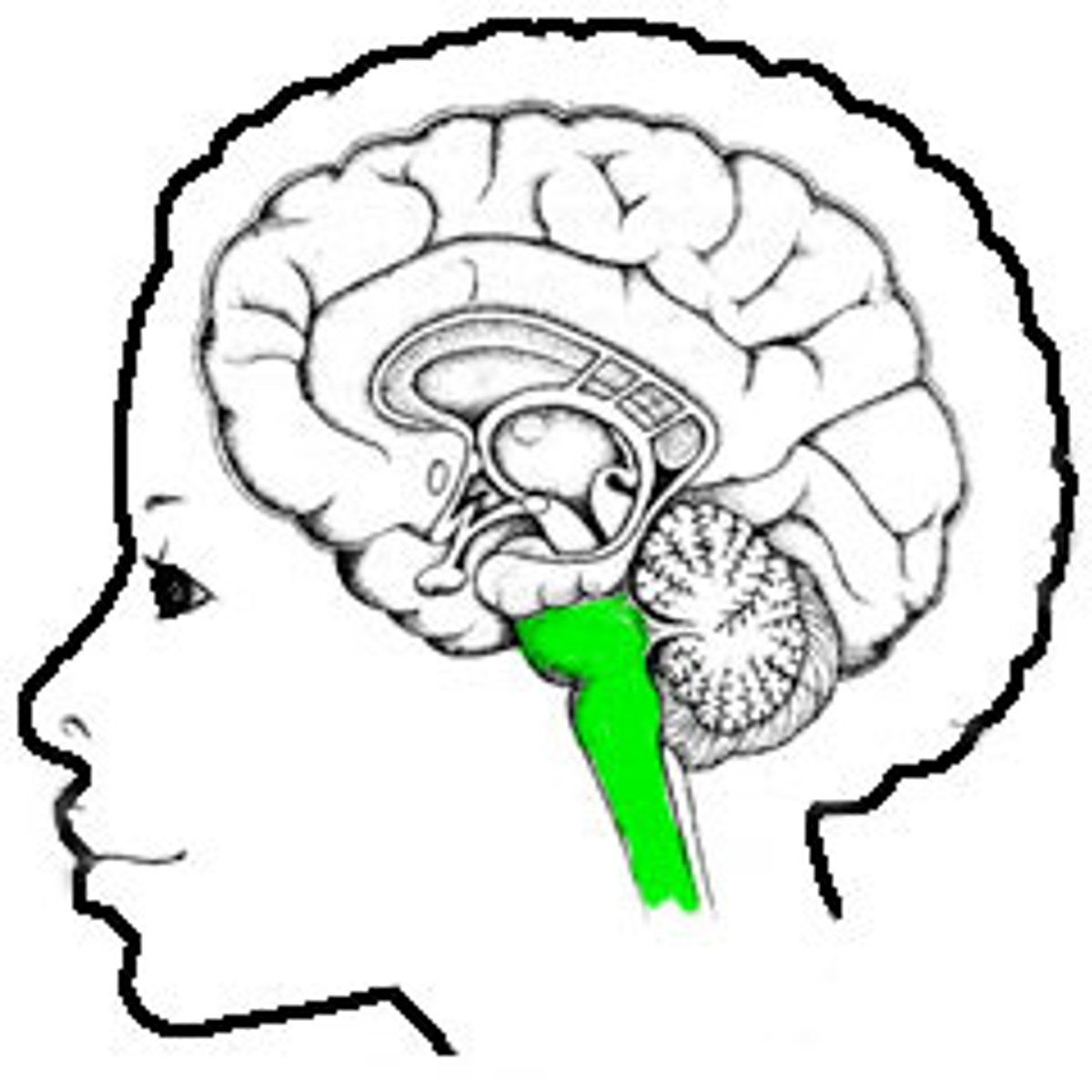
brain stem
controls basic life functions
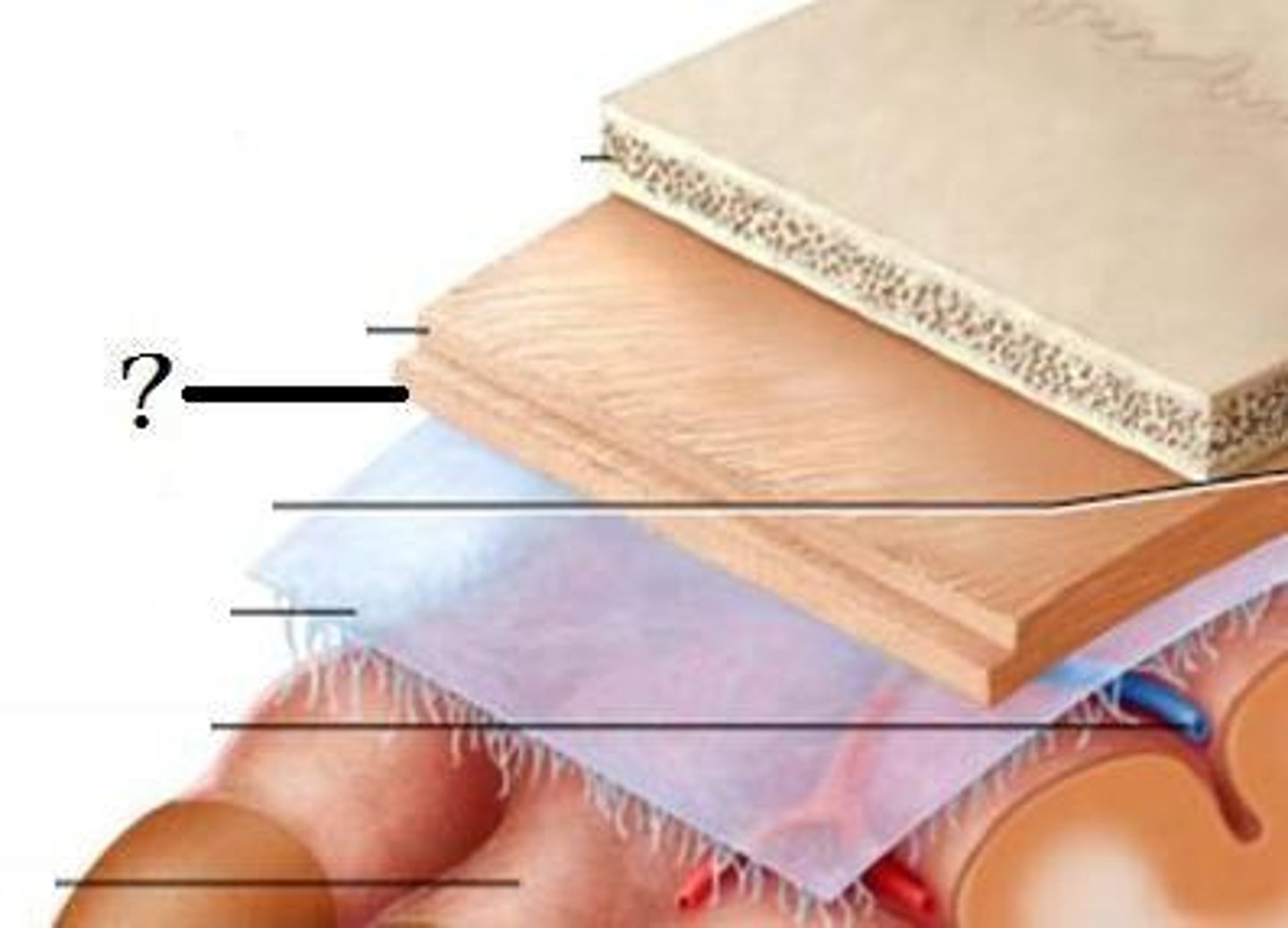
Meninges
- 3 layers surrounding the brain and spinal cord
• Dura mater (outer layer)
• Arachnoid (middle layer)
• Pia mater (inner layer)
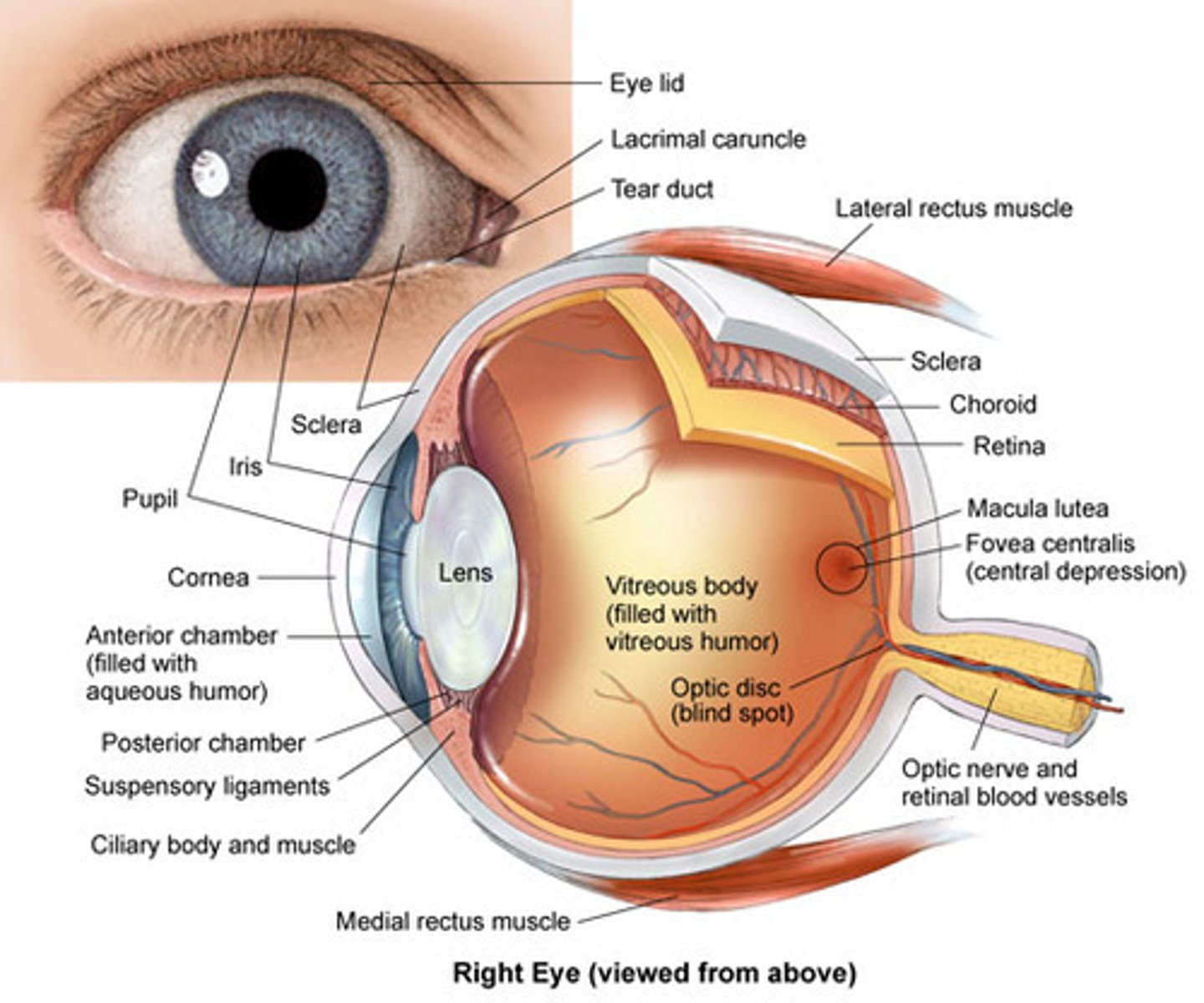
anatomy of the eye
Light waves enter eye & pass through cornea, pupil, & lens, then received by the retina
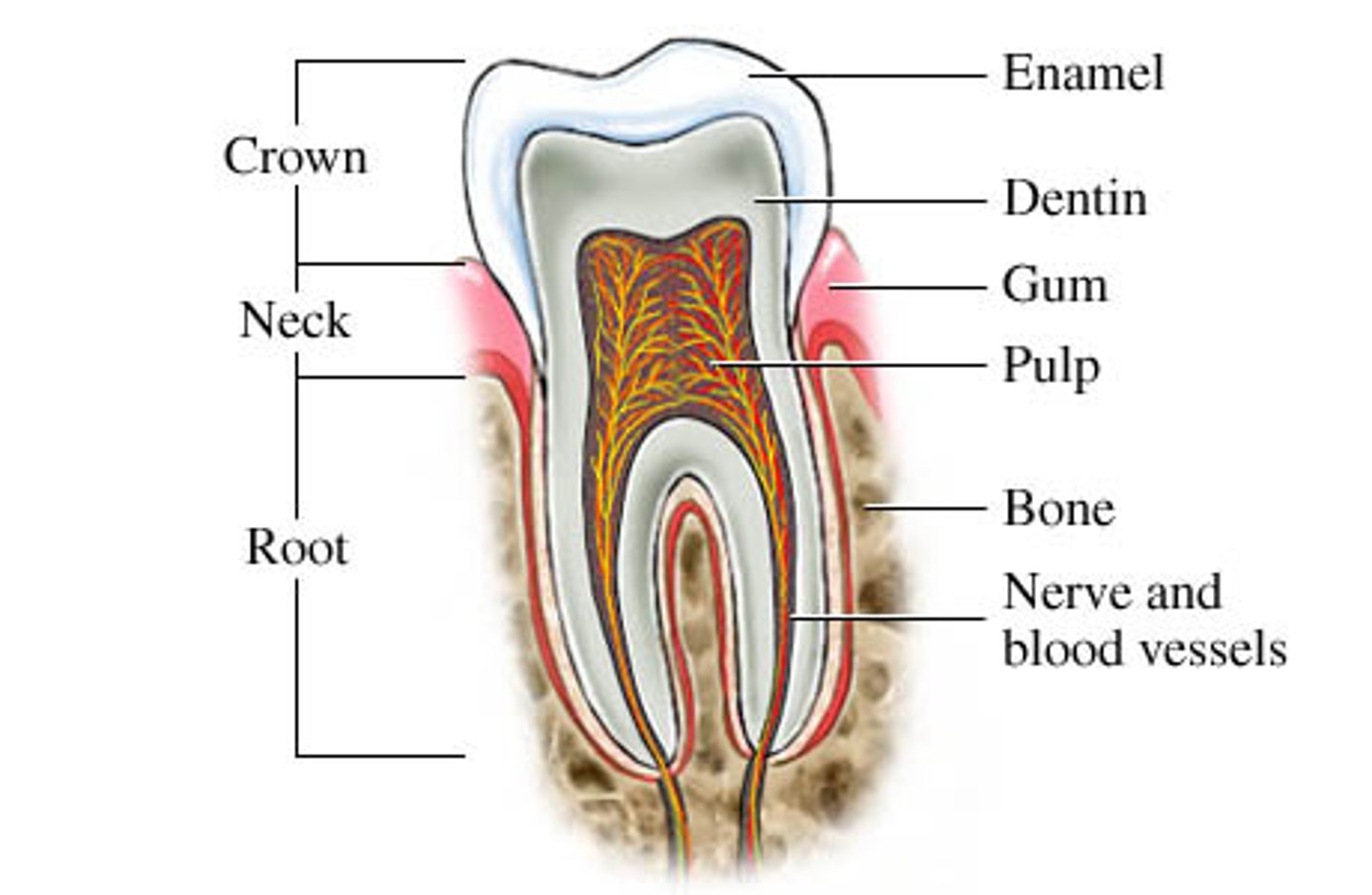
anatomy of the tooth
crown, neck, root
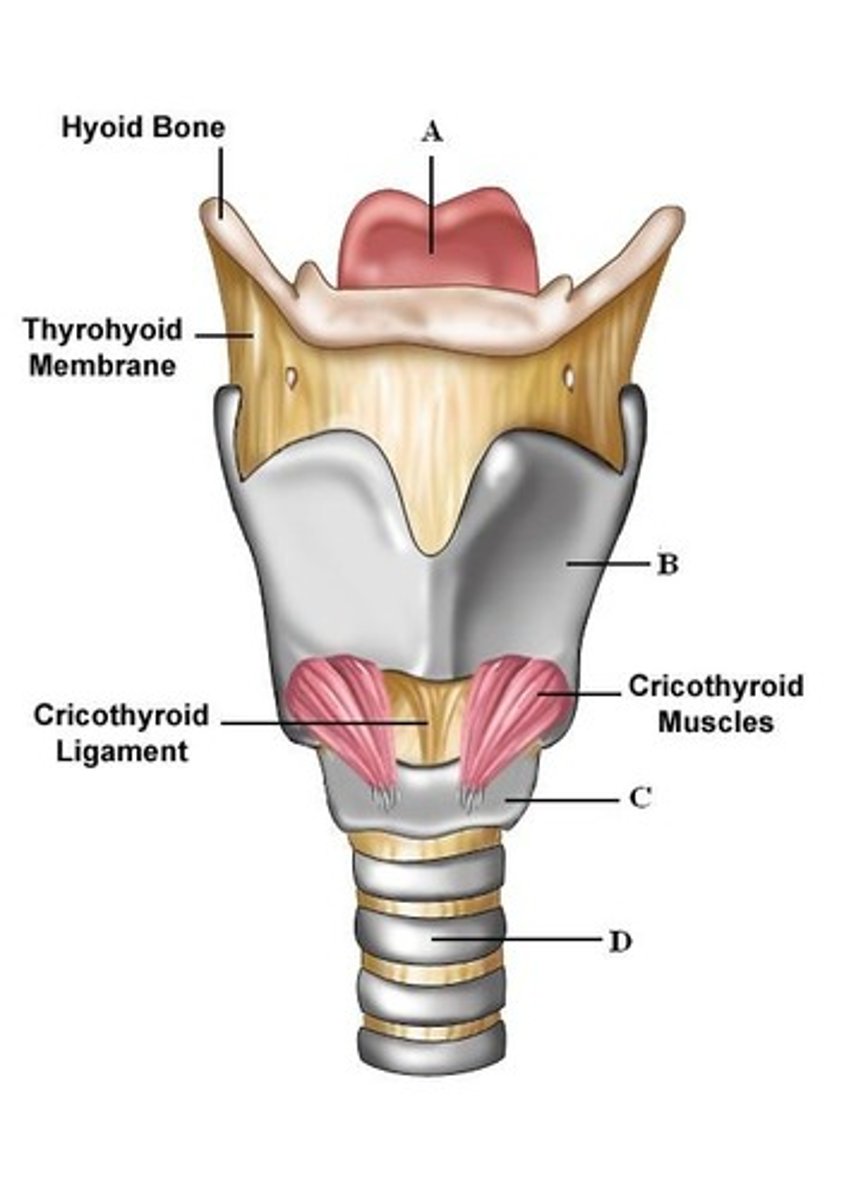
anatomy of larynx
articulated cartilages, vocal cords, muscle and ligaments, which keep the airways open during breathing and closed during swallowing
coup
damage where injury occur
coontrecoup
damage opposite where injury occurred
Traumatic brain injuries (TBI) are typically categorized along a severity spectrum as mild, moderate, or severe.
true
Glasgow Coma Scale
• Eyes opening
• Verbal response
• Motor response
scalp lacerations
The most minor type of head trauma
Scalp is highly vascular → profuse bleeding
Major complication is infection
immediate management for scalp lacerations
Debride wound
• Direct pressure (10-15 min)
• Approximate wound
• Approximation may be accomplished up to 24 hours post-injury
skull fracture categories
depressed, linear, basilar, diastatic
Depressed fracture
may cause indentations and bony fragments to enter the brain cavity

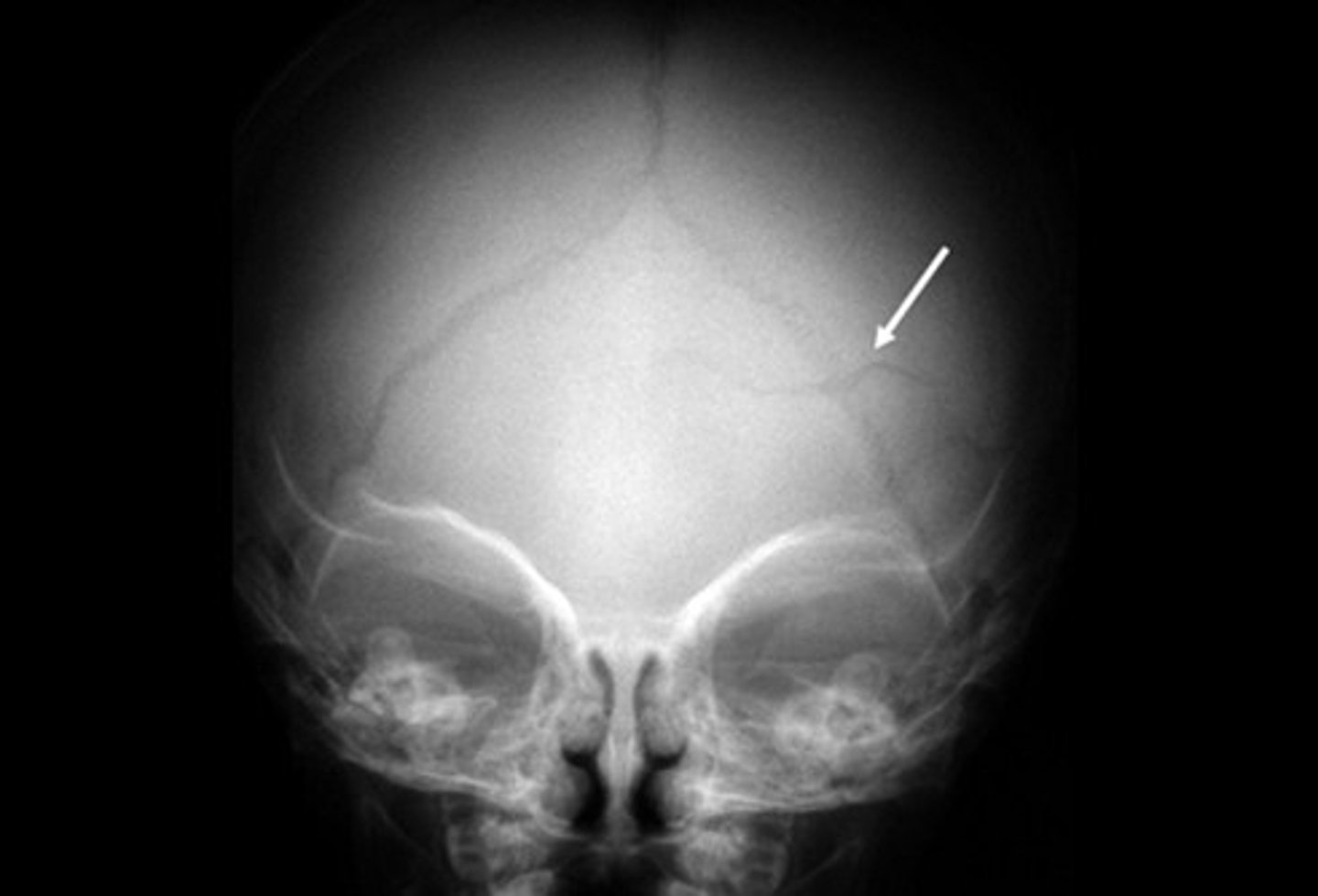
Linear fracture
most common, result of minor blunt trauma

Diastatic fracture
occur at the suture lines (usually affect young children)
Skull fractures require surgery when other brain injuries exist.
true
immediate management for skull fractures
• Avoid direct pressure
• Control bleeding (if necessary)
• Transport
Basilar skull fractures signs and symptoms
• Raccoon eyes
• Battle's sign
• Blood pooling behind the eardrum
• Leakage of cerebrospinal fluid

Given the individualized __________ presentation and treatment, it is important for HCPs to develop a systematic and comprehensive sideline evaluation technique.
nature of concussion
About 2/3 of ED visits are related to concussions (age <19)
true
Recurrence of concussions is likely to occur within the first 10 days of initial injury.
true
concussion
a bruise like injury of the brain
concussion signs and symptoms
-usually transient and can be identified through witnesses or self-reported by the patient
-Loss of consciousness may or may not be associated with concussions.
-Headache, fatigue, blurred vision, irritability, inappropriate emotions or behaviors, nausea, vomiting, poor concentration and memory, and drowsiness
Post-Concussive Syndrome
Complex disorder characterized by continuation of concussion symptoms for weeks and even months after the initial injury
Post -concussive syndrome symptoms persist for greater than _____ months and It is estimated that ______ of patients will develop this
3, 10-15%
Second impact syndrome
Condition in which a second concussion occurs prior to a first concussion completely resolving, causing rapid and severe decompensation of the patient.
Concussion assessments
• Life-threatening injuries assessed first
• Remove patient from participation and assess in quiet space/environment
No definitive test exists; use combination of assessments through screening tools with traditional or computerized neurocognitive testing, postural stability, self-report symptom instruments, and [hysical and neurological examination components.• SCAT-5• SAC• CARE• King Devick• BESS• VOMS
concussion return to participation
1. Symptom limited activity: Activities of daily living
2. Light aerobic conditioning
3. Sport-specific activity: Earliest attempt at resistance training
4. Noncontact sport training
5. Full-contact practice
6. Return to competition
Chronic Traumatic Encephalopathy
form of dementia caused by repeated head trauma such as concussions
Degenerative brain disease associated with populations exposed to repetitive head trauma.
true
Brain degeneration is caused by
a protein known as tau, which forms clumps in the brain tissue that spread over time
Patients who are ultimately diagnosed with CTE typically began participating in their sport as____________and played for at least 5 years
children and adolescents
It is thought that ________of athletic individuals who develop CTE are symptomatic at retirement, and the condition advances over time.
33%
Intracranial pressure
the amount of pressure inside the skull
stage 1 (Chronic Traumatic Encephalopathy)
Headaches and attention and concentration issues
stage 2 (Chronic Traumatic Encephalopathy)
Depression, short-term memory loss, and explosivity
stage 3 (Chronic Traumatic Encephalopathy)
Cognitive impairment and executive function shortfalls in planning, organization,multitasking, and judgement
stage 4 (Chronic Traumatic Encephalopathy)
Full-blown dementia (memory and cognitive impairment significant enough to impede daily living)
Resting Intracranial pressure (ICP)
7-15 mm Hg
Potential causes of ICP include
Blow to the head, infection, tumor, stroke, aneurysm, epilepsy, hypoxemia,and meningitis
signs and symptoms of ICP
• Headache
• Double vision
• Nausea/vomiting
• Unequal pupil size
• Confusion
• Seizures
immediate management for ICP
Immediate transport to hospital
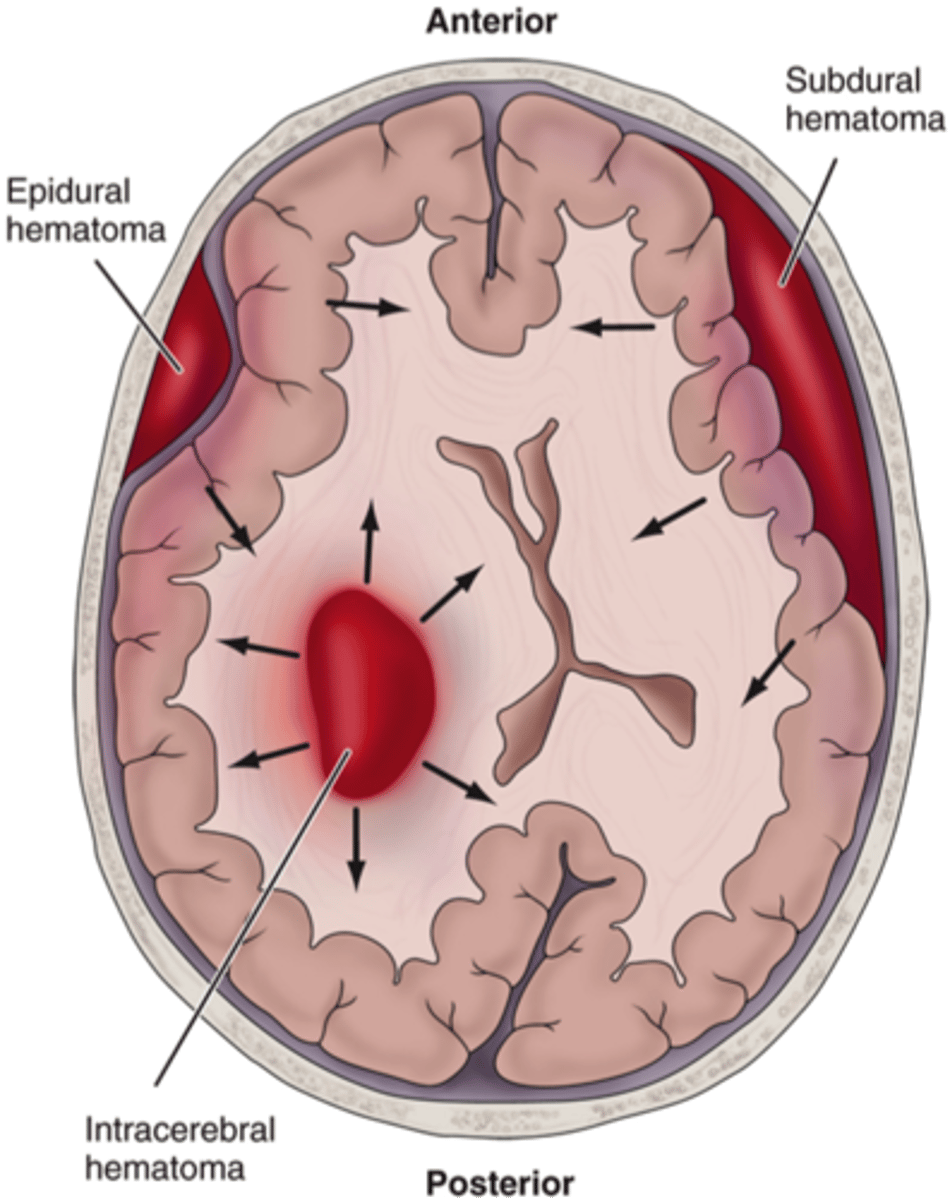
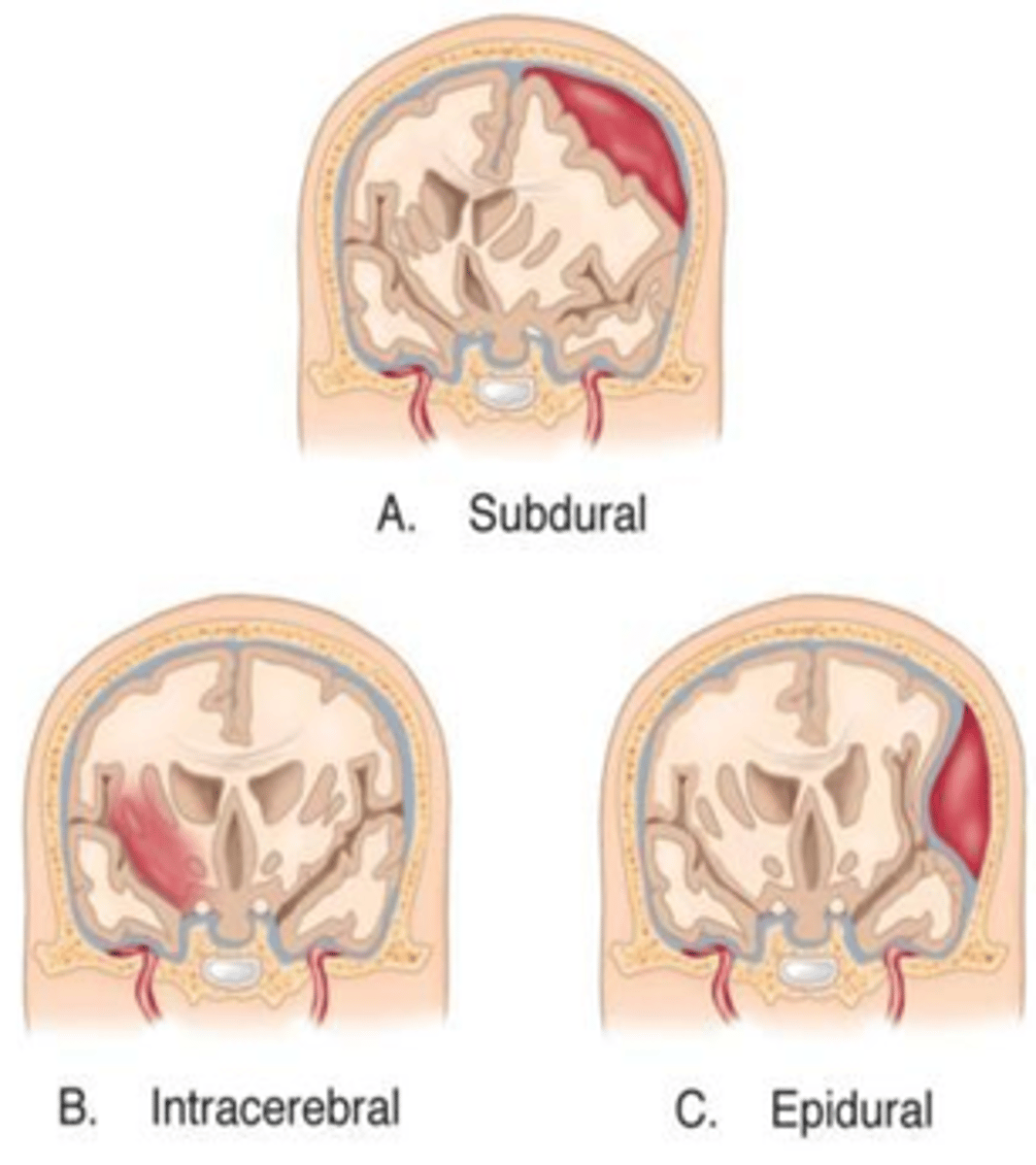
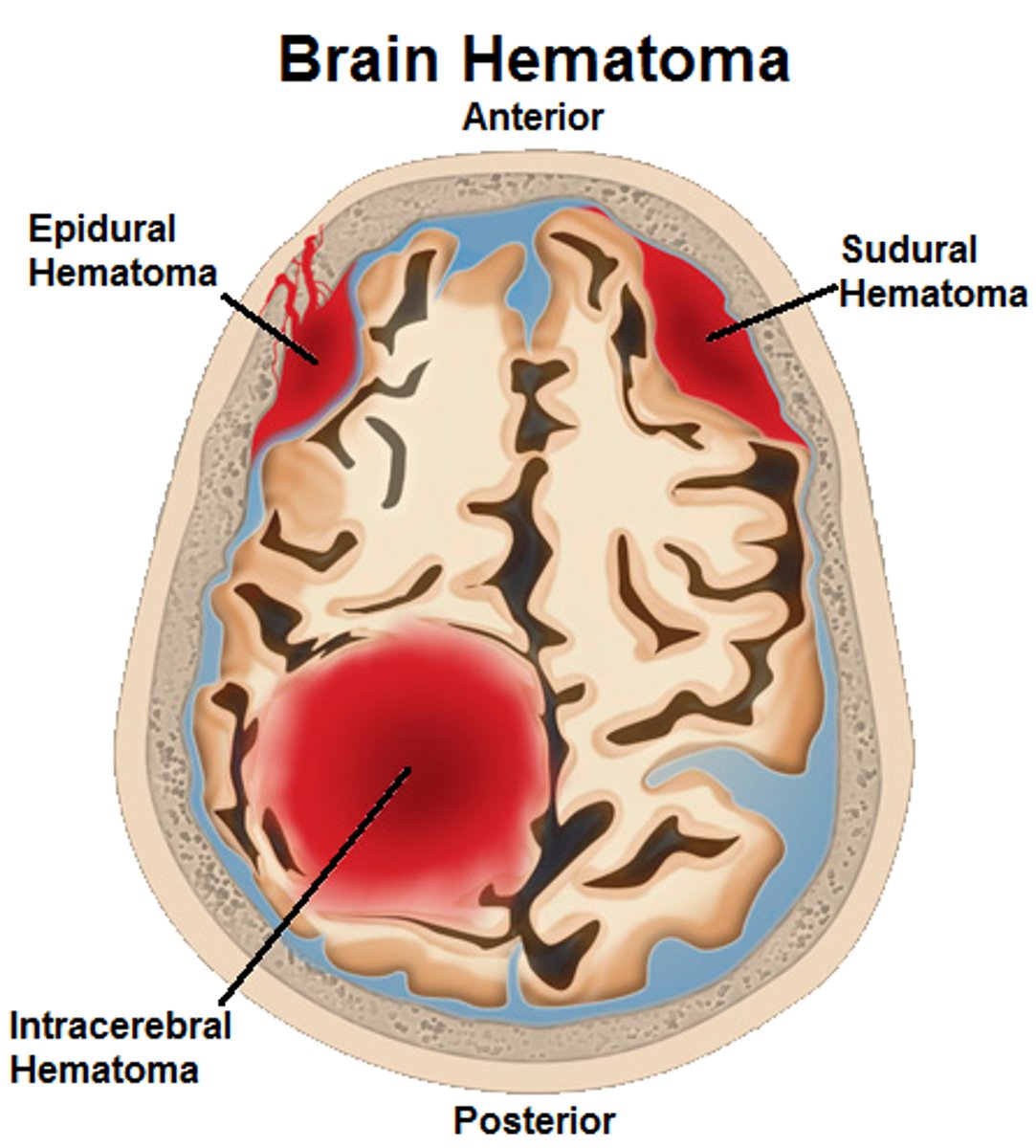
Intracerebral Contusion
Associated with a direct blow or acceleration-deceleration injury and can vary in size
.• Differs from a laceration - the pia mater remains intact
• Differs from a hematoma - blood is intermixed with brain tissue
Intracerebral contusions an be present in any area of the brain but are more common in the frontal and temporal regions
true
signs and symptoms of Intracerebral contusions
-Sleepiness
• Coordination difficulties
• Dizziness
• Seizures
• Confusion
• Tinnitus
• Nausea/vomiting
• Loss of consciousness
MOI of epidural hematoma
• Focal injuries often caused by a linear and direct impact force (e.g., hit with baseball or bat)
• Associated with skull fractures and lacerations
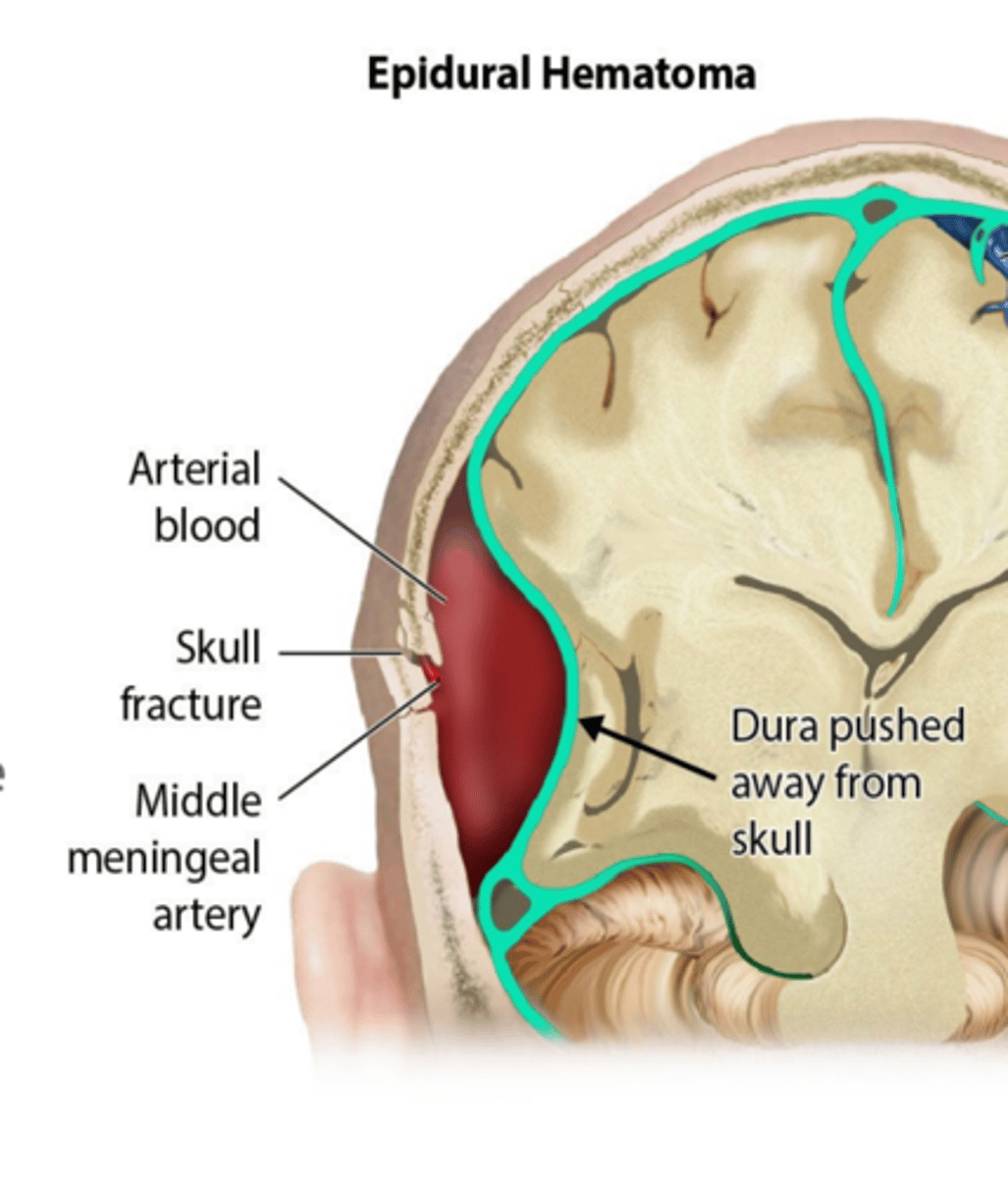
Signs and symptoms of epidural hematoma
• Headache
• Nausea/vomiting
• Seizures
• Focal neurologic deficits (e.g., aphasia, weakness, numbness, visual field disturbances)
• Keep in mind that an epidural hematoma can cause death within minutes
Immediate management of epidural hematoma
• Stabilize ABCs
• Immobilize
• Transport immediately to the nearest level 1 trauma center
Leading cause of sports-related fatalities
Subdural Hematoma
Subdural hematoma bleeding collects ______ the inner layer of the dura mater but external to the brain and arachnoid membrane
under
Subdural hematoma may occur when
• May present either acutely or chronically:
• Acute occurs within 72 hours after injury
• Chronic may take as long as 3 weeks
risk factor for Subdural hematoma
• Head trauma
• Post-surgical complications
• Anticoagulation drug therapy
• Nontraumatic cerebral aneurysm
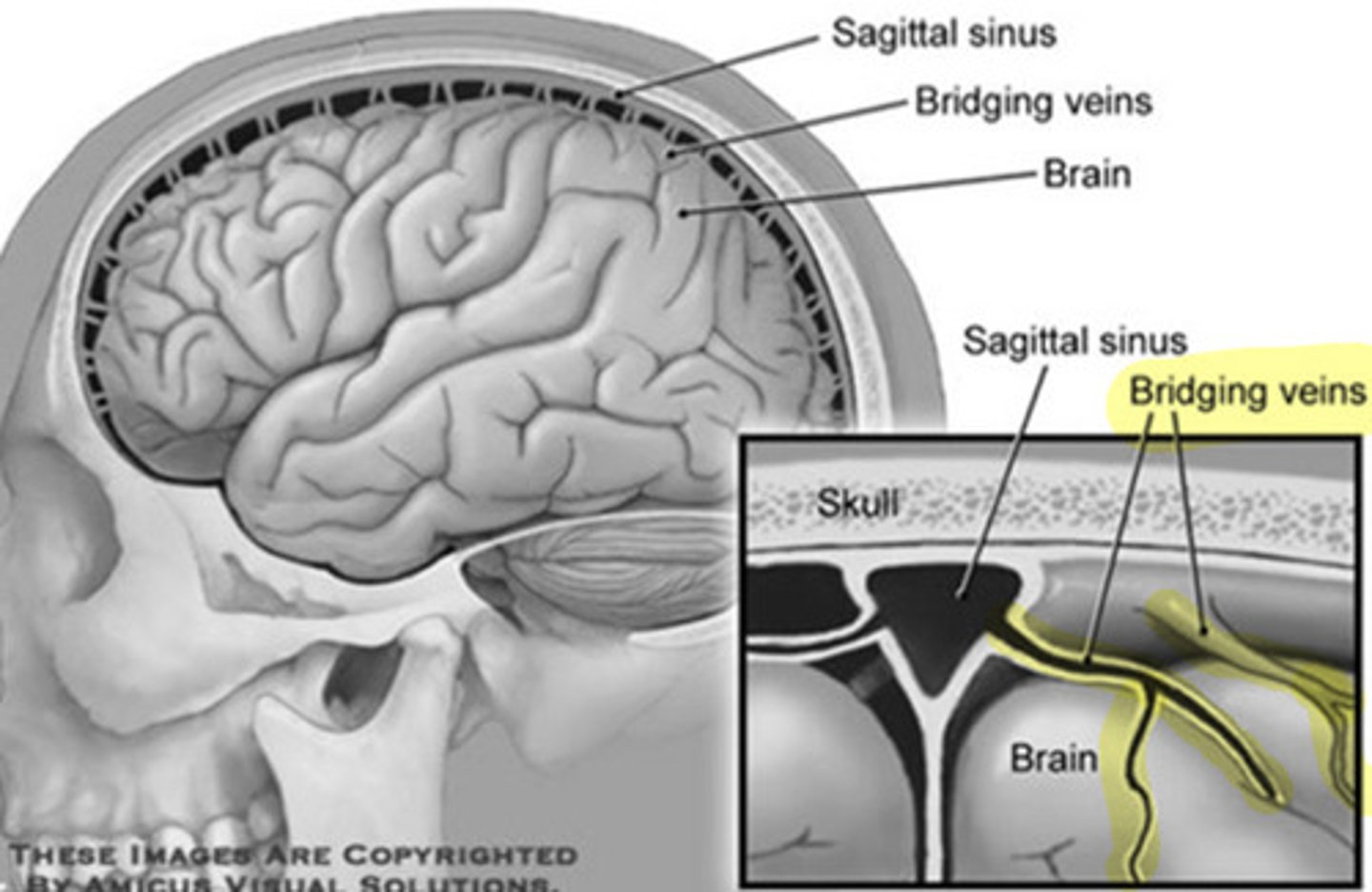
signs and symptoms of subdural hematoma
• Deteriorating neurologic function
• Decreasing LOC
• Decreasing or irregular respiration
• Decreasing or irregular heart rate
• Unequal, dilated, or unreactive pupils
immediate management for subdural hematoma
-Assess ABCs and LOC
• Head injuries can escalate quickly; be prepared to transport