Procedures Proficiency Exam
1/792
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
793 Terms
What is venipuncture?
the puncture of a vein for withdrawal of blood or injection of a solution
What is the parenteral route?
drug administration by route other than the GI tract, typically intravenous, intradermal, intramuscular, subcutaneous
What precautions are used in venipunture?
strict aseptic technique with standard precautions (because we are penetrating the protective layer of the skin, and all patients are considered potentially infectious)
Explain standard precautions
adhere to aseptic technique
one needle, one syringe, one patient
dispose after use
use single dose vials when possible
What are the most common types of needle used for parenteral drugs?
plastic/angiocath
steel shaft/butterfly
How should the bevel be before inserting into the vein?
facing up
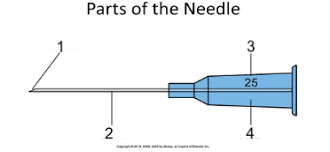
Label the parts of the needle
bevel
shaft
gauge number
hub
What are some things that determine which needle you use?
what you need it for
blood draw
procedure
medication
which veins are available
how long the IV will be in
How are needles sized?
gauge (G): the thickness or diameter of the needle
commonly 18-22 G
higher number = smaller diameter
length: measurement in inches of the shaft portion
.25-5”
1-1.5” used for IV injections
What are short and long bevels used for?
short: IV injections
long: subcutaneous and intramuscular
Explain angiocath/intravenous catheter needles
over-the-needle cannula
flexible catheter over a stylet
even gauge numbers (18, 20, 22, etc.)
primarily used for prolonged infusion
safer device in venipuncture (because needle is drawn back up into the protective sheath)
greater tendency for staying in veins (reduces risk of extravasation)
Explain butterfly/scalp vein needles
has wings
flexible tubing from shaft to hub
gauge numbers 18, 20, 22, 23
.25-1.25 inches
What must be done before inserting an IV?
verify patient
What are some indications of IVs?
IV fluid
medications
contrast
lab draws
emergency access
What are some contraindications of IVs?
edema to extremities
breast or lymph surgeries
fistula, shunt, vascular graft in arm
scar, wound, rash, hematoma at site
extravasation on the side
vein is thrombosed
What are some complications that can occur with venipuncture?
pain
bleeding
hematoma
infection
infiltration
phlebitis (inflammation)
Explain the 3 layers of the vein
outer layer of fibrous connective tissue called adventitia
middle layer of smooth muscle called tunica media
inner layer of epithelial tissue called intima
What are the most common sites for venipuncture?
antecubital area of the arm
cephalic vein (lateral side of forearm), median cubital (midline of forearm), basilic (medial side forearm, elbow, arm
What are the best sites for venipuncture?
cephalic and basilic veins
Why is the back of the hand a less common site?
painful
veins tend to move around
must use smaller catheter = slower injection rates
How do you select which vein to use?
non-dominant arm when possible
look for long, straight vein
listen to the patients suggestions
How do you assess vein quality?
palpate to determine size, angle, and depth
How can you “bring up” a vein?
have patient “pump” their hand
hang arm down
warm compress
slap briskly
How do you know you have a vein and not an artery?
arteries pulse
What is a bolus?
entire dose is injected into the venous system at one time
What is a drip infusion?
dose is delivered more slowly over time
What is extravasation?
discharge or escape of fluid from a vessel into surrounding tissue
What is infiltration?
diffusion of a fluid into tissue
What supplies are needed for IV insertion?
gloves
tourniquet
skin prep
needles
IV tubing
prepared contrast
gauze/cotton and tape or band aid
sharps container
emergency cart (for possible reactions)
What steps must be taken before IV insertion?
identify patient
explain procedure
ask about allergies
List the steps for IV insertion
wash hands and put on gloves
select site, apply tourniquet 3-4 inches above site, clean the site
initiate puncture
stabilize needle and advance catheter
prepare for contrast insertion
remove needle and apply gauze
How should you use the IR on a hypersthenic patient?
always use IR crosswise
How should you use the IR on a sthenic patient?
generally use IR crosswise
How should you use the IR on a hyposthenic patient?
generally use IR lengthwise
How should you use the IR on an asthenic patient?
always use IR lengthwise
What vertebrae does the vertebral prominence correspond with?
C7
What vertebrae does the jugular notch correspond with?
T2/T3
What vertebrae does the inferior angle of the scapula correspond with?
T7
What are the breathing instructions for a chest x-ray?
double breath (for greater inspiration and more depressed diaphragm)
What is the difference between personal/controllable artifacts and medical/uncontrollable artifacts?
personal artifacts (jewelry, clothing, hair, bra, etc.) can be removed from the area of the body being imaged
medical artifacts (pacemakers, feeding tubes, stents, etc.) can not be moved
What are some reasons for ordering a CXR?
pathology
fluid levels
foreign body (aspiration)
movement of diaphragm
rib detail
How far below the vertebral prominens should you center a PA chest projection?
7 inches lower in females
8 inches lower in males
What do you need to make sure is included in a chest x-ray?
apices, costophrenic angles, 10 ribs above diaphragm, and medial scapula borders lateral to lungs
Why are chest laterals done as left laterals?
reduces the heart magnification
What is considered acceptable rotation for a chest x-ray?
½ an inch or less
What does RIPA stand for? (Hint: it is used for critiquing PA/AP chest x-rays)
R-Rotation
I-Inspiration
P-Penetration
A-Angulation
How can you make sure that the rotation is acceptable in a PA/AP chest x-ray?
medial ends of clavicles should be equidistant from spine
How can you make sure that the inspiration is acceptable in a PA/AP chest x-ray?
minimum of 10 ribs above the diaphragm
How can you make sure that the penetration is acceptable in a PA/AP chest x-ray?
thoracic vertebrae are seen through the heart and mediastinum, lung markings are clearly demonstrated, penetration through costophrenic angles
How can you make sure that the angulation is acceptable in a PA/AP chest x-ray?
medial ends of clavicles should be at level of T3/T4 and 1in of apical lung tissue above clavicles should be demonstrated
What is lordotic position?
patient in AP position, one foot away from the bucky, hands on hips with palms up, patient leaning backward so shoulders and neck are against bucky
What is the purpose of a lateral decubitus CXR?
demonstrate air/fluid levels
How long should you (ideally) let patient lay on their side before taking a lateral decub?
5 minutes
If you are looking for air in the lungs, which side should patient lay on?
the side you are looking at should be up
If you are looking for fluid in the lungs, which side should patient lay on?
the side you are looking at should be down
On a decub, which side should the marker be on?
the side down
How should your technique change for emphysema?
reduce technique
How should your technique change for pleural effusion?
increase technique
How should your technique change for pneumothorax?
take an image on inspiration and on expiration
What is the purpose of a Swan Ganz catheter?
monitoring the heart’s function and blood flow, as well as pressures in and around the heart
What is a picc line?
peripherally inserted central catheter inserted into a vein in the arm that goes to the heart
What is a balloon pump?
mechanical device that allows the heart to pump more blood by inflating when heart relaxes
What is the purpose of an endotracheal tube (ETT)?
establishing and maintaining a patient airway to ensure the adequate exchange of oxygen and carbon dioxide
The tip of the ETT should be ___ to the carina
5 cm superior
What is the purpose of a nasogastric (NG) tube?
provide nutrition to patients who cannot obtain nutrition by mouth (or are unable to swallow safely)
What is the purpose of chest tubes?
removing something (air/fluid) frum intrathoracic space
tube remains in the chest until all/most of the fluid has drained
CXRs to check chest tube progress should be taken ___
upright (to show air/fluid levels)
What is the purpose of pacemakers?
steady electrical impulses to regulate the beating of the heart (treats bradycardia)
What is the purpose of implantable cardioverter-defibrillators(ICD)?
treating heart rhythm disturbances by means of electric shock (treats tachycardia)
What is the purpose of a heart valve replacement?
to repair or replace diseased heart valves (can be mechanical or biological)
What is a clavicle series?
AP and AP axial
Where do clavicle fractures usually take place?
80% in the middle, 15% on the lateral end
Explain the positioning for an AP clavicle
10×12 CW
AP upright or supine with table bucky
shoulders flat, arms at sides, chin raised, look forward
on inspiration
What is a benefit of doing a clavicle PA?
shorter OID, increases the detail
Where should you center for an AP clavicle?
mid-clavicle
What SID is used for most clavicle and scapula images?
40”
What needs to be demonstrated on an AP clavicle image (film eval)?
full body of the clavicle
AC and SC joints in view
half of clavicle unsuperimposed from thorax
clavicle at level of 3rd/4th rib
superior scapular angle should be superimposed on mid-clavicle
marker lateral
How are clavicle and scapula images sent?
as if someone is standing in front of you in anatomic position
Explain the positioning for an AP axial clavicle image
10×12 CW
AP upright or supine
shoulders flat, arms at sides, chin raised, look forward
on inspiration
Explain the centering/angulation for an AP axial clavicle image
15-30o angle
if AP: cephalic
if PA: caudal
patient may be in a lordotic position to decrease the angle
asthenic patients use more angle
What needs to be demonstrated on an AP axial clavicle image (film eval)?
inferior surface of clavicle (tubercles visible)
lateral 2/3 of clavicle unsuperimposed
clavicle above superior angle of scapula
AC and SC joints visible
medial aspect of clavicle at level of 1st/2nd rib
marker lateral
What is a scapula series?
AP and Lateral (Y-View)
Explain the positioning for an AP scapula image
10×12 LW
upright or supine
abduct affected arm 90o
moves scapula off of thorax
places scapula lateral to IR
supinate the hand
suspend breathing or breathing technique
Explain the centering for an AP scapula image
perpendicular 2 inches inferior to coracoid (with 2 in of IR above shoulder)
What needs to be demonstrated on an AP scapula image (film eval)?
true AP
lateral border free of superimposition of ribs
arm abducted
includes inferior angle of scapula
marker lateral
How is the arm placed for a lateral scapula that the scapular body is of primary focus?
arm (of affected side) brought across the chest
How is the arm placed for a lateral scapula that the acromion and coracoid are of primary focus?
arm tucked behind the back
Explain the positioning for a lateral scapula image
upright (AP or PA)
oblique body 45-60o to place scapula perpendicular to IR
arm placement (determined by whether you are looking at the body or the acromion and coracoid)
Where do you center for a lateral scapula image?
perpendicular to mid-vertebral border of scapula
What needs to be demonstrated on a lateral scapula image (film eval)?
superimposed lateral and medial borders
no superimposition of scapula on ribs
marked lateral
acromion and coracoid processes
What are AC and SC joint x-rays done for?
r/o separation or dislocation
What SID is used for AC joints?
72”
Explain the positioning and centering for AC joints
14×17 CW
centered 1 inch above jugular notch
upright (standing or sitting) with back against bucky
arms at sides (neutral rotation)
Explain the breathing recommendations for clavicle, scapula, AC, and SC images
clavicle: on inspiration
scapula: breathing technique
AC: suspend breathing
SC: on expiration
What is the AC joint routine?
without weights first, then with weights
Why do you put the weights around a patient’s wrists for AC images?
so they don’t try to hold their arms up
If the without weights image shows a clavicle fracture, can you still do the with weights image for AC joints?
NO
If the without weights image shows a clavicle dislocation, can you still do the with weights image for AC joints?
YES
What needs to be demonstrated on an AC joints image (film eval)?
both AC joints, both SC joints, and full clavicle in view
markers on both sides of patient
annotate whether it was with or without weights
If a patient has broad shoulders that don’t fit on the IR together for AC joints, how can you alter the procedure?
two separate images for each joint
do both shoulders without weights before doing with weights
center 1 in below AC joint
cone in more