APPP Flashcards - Kidneys
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
62 Terms
What categories is body fluid divided into?
Extracellular fluid
Interstitial fluid
Blood plasma
Intracellular fluid
How is the size of the extracellular compartment determined? Why?
It is determined by the body’s total sodium content.
Sodium is the predominant ion of the extracellular fluid and as a result is available in large enough quantities to influence osmotic distribution or redistribution of large amounts of water.
Where are the kidneys located?
On the posterior wall of the abdomen.
How much do kidneys filter in a day? How much urine does this result in?
Filter 125 mL/min (180 L/day)
Make 1 mL/min urine
What is the man unit that makes up the kidneys? How many of these units are there?
Nephron
1 million
What are the main components of the nephron?
Glomerulus and long tubule
What is the glomerulus?
The place in the nephron where large amounts of fluid are filtered from the blood. It consists of glomerular capillaries surrounded by the Bowman’s capsule.
How does blood enter and exit the glomerulus? What is significant about this?
Blood enters through the afferent arteriole (thick) and leaves through the efferent arteriole (thin). More fluid enters the glomerular capillaries than can leave. This causes a pressure buildup that allows for filtration.
How much of the plasma entering the glomerulus is filtered? What happens to the plasma that is not filtered?
20% is filtered, 80% is not filtered and just leaves through the efferent arteriole.
What is the long tubule?
The site of reabsorption and secretion in the nephron where filtered fluid is converted into urine. It consists of the proximal tubule, loop of Henle, distal tubule, and collecting duct.
What are the two capillary beds in the nephron?
Glomerular capillaries and peritubular capillaries
What are the glomerular capillaries?
Location where the afferent arteriole ends and splits into capillaries. The high pressure here causes filtration.
What are the peritubular capillaries?
Location where the efferent arteriole ends and splits into capillaries. Low pressure here permits absorption.
What are the 5 steps of urine formation?
1) Blood enters the glomerulus from the afferent arteriole.
2) Blood is filtered from the glomerular capillaries into the Bowman’s capsule. Cells and proteins remain in the blood.
3) Filtered fluid leaves the Bowman’s capsule and passes through the tubules. Remaining blood leaves the glomerulus through the efferent arteriole.
4) Fluid in tubules is modified by reabsorption of water and specific solutes back into the blood, or secretion of substances from the peritubular capillaries into the tubules.
5) Urine travels through the ureter into the urinary bladder and exits the body through the urethra.
What is the filtration pressure in the glomerulus? How is this calculated?
Filtration pressure is 10 mmHg
Glomerular hydrostatic pressure (55 mmHg) – [Osmotic pressure (30 mmHg) + [capsular hydrostatic pressure (15 mmHg)] = Net outward pressure (10 mmHg)
What allows the glomerular capillary membrane to act as a filter?
It has a three-layer membrane:
Endothelium: perforated by thousands of fenestrae, and also has tight junctions
Basement membrane: a meshwork of collagen and proteoglycan, the main filtration barrier
Epithelial cells: have long foot-like processes (podocytes) that wrap around the capillaries, leaving gaps called slit pores
What can get through the slit-pores between epithelial cells on the outer layer of the glomerular capillaries?
Albumin and other low molecular weight proteins can get through and need to be absorbed later.
How do glomerular filtration and tubular reabsorption differ in selectivity?
Glomerular filtration is nonselective, tubular reabsorption is highly selective.
How much creatine is reabsorbed in the long tubule?
None of it. It all remains in the urine.
How much glucose is reabsorbed in the long tubule?
All of it. No glucose remains in the urine.
How much sodium is reabsorbed in the long tubule?
Almost all of it. 0.6% remains in the urine (99.4% reabsorbed).
What substances are secreted into the tubular fluid from the peritubular capillaries for removal?
Potassium ions, hydrogen ions, urea, and thiazide drugs.
What ions have a higher extracellular concentration that intracellular concentration?
Sodium, bicarbonate (HCO3-), and chloride.
What ions have a higher intracellular concentration that extracellular concentration?
Potassium, magnesium, phosphate (PO4-)
What do diuretics do?
Inhibit the tubular reabsorption of sodium ions.
How much water is absorbed in the proximal tubule, loop of Henle, and distal tubule + collecting duct? How much is excreted in the urine?
Proximal: 70%
Loop of Henle: 15%
Distal + collecting duct: 14%
Excreted: 1%
How much sodium is absorbed in the proximal tubule, loop of Henle, and distal tubule + collecting duct? How much is excreted in the urine?
Proximal: 70%
Loop of Henle: 25%
Distal + collecting duct: 4.5%
Excreted: 0.5%
What are the mechanisms of tubular transport in the kidneys?
Simple diffusion
Channel-mediated diffusion
Carrier-mediated diffusion
Facilitated diffusion (down electrochemical gradient)
Co-transport (two or more solutes in the same direction)
Counter transport (two or more solutes in different directions)
ATP mediated transport (against electrochemical gradient using ATP hydrolysis)
What is the sodium-potassium ATPase pump? Where does in function?
Present on the basolateral side of the tubular epithelial cell throughout most parts of the long tubule.
Hydrolyzes ATP and uses that energy to transport 3 Na+ out of the cell, and 2 K+ in.
Helps to maintain low intracellular sodium, and create a net negative charge in the cell. This favors movement of Na+ across the luminal membrane into epithelial cells.
As sodium diffuses back into the cell down its concentration gradient, the resulting energy release is used to co-transport or counter-transport other substances.
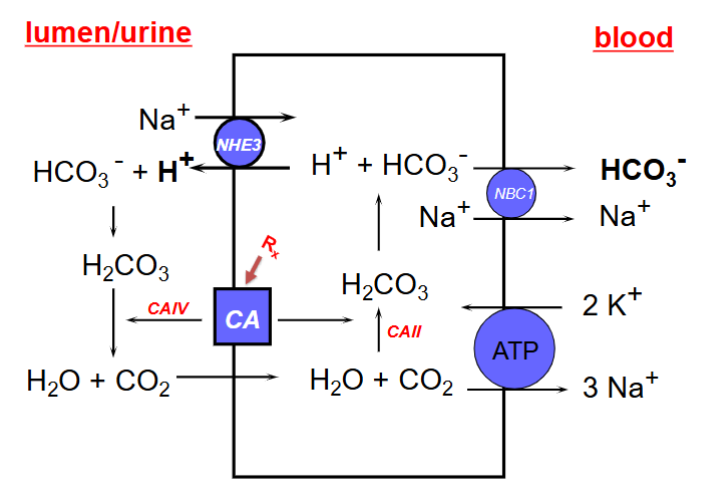
How does transport in the proximal tubule work (7 steps)? Draw the diagram.
1) Sodium-hydrogen exchanger (NHE3) on the apical side of the luminal membrane brings 1 Na+ into the cell and 1 H+ out.
2) H+ reacts with extracellular HCO3- to form carbonic acid.
3) Carbonic anhydrase IV (CAIV) on the apical side of the luminal membrane catalyzes the cleavage of carbonic acid to H2O and CO2
4) CO2 diffuses into the cytoplasm.
5) CAII rehydrates CO2 to carbonic acid.
6) Carbonic acid dissociates into HCO3- and H+.
7) HCO3- is cotransported with Na+ across the basolateral membrane of the epithelial cell into the blood by the NBC1 transporter.
The sodium-potassium ATPase is also continuously working to help power this transport system.
What is unique about cells in the proximal tubule?
They are highly metabolic, have a lot of mitochondria, and have an extensive brush border to increase surface area.
How does the amount of Na+ and the concentration of Na+ in the tubular fluid change through the proximal tubule?
Amount of Na+ decreases, but concentration stays the same because water reabsorption keeps pace with sodium reabsorption.
How does the majority of calcium reabsorption in the proximal tubule occur?
80% occurs by passive diffusion and solvent drag.
How are uric acid and diuretics secreted from the blood into the luminal fluid in the proximal tubule?
Organic acid secretory systems.
How is glucose reabsorbed into the blood in the proximal tubule?
Sodium-glucose co-transporters (SGLTs) that couple glucose reabsorption with sodium reabsorption.
What is SGLT-2?
A sodium-glucose co-transporter in the S1 and S2 convoluted section of the proximal tubule.
Transports 1 sodium ion and 1 glucose into the blood
Responsible for reabsorption of 90% of glucose filtered out
What is SGLT-1?
A sodium-glucose co-transporter in the S3 straight section of the proximal tubule
Transports 2 sodium ions and 1 glucose into the blood
Responsible for reabsorption of 10% of glucose filtered out
How do SGLTs and GLUTs facilitate insulin independent reabsorption of filtered glucose?
At normal glucose levels the amount of glucose filtered by the glomerulus increases with glycaemia and is entirely reabsorbed from the proximal tubule (no glucosuria). Beyond a given glycaemia (renal threshold for glucose), the reabsorption method becomes saturated and glucose appears in the urine. This is a natural defence mechanism against hyperglycemia.
How are small proteins reabsorbed in the proximal tubule?
Cross the apical membrane by endocytosis, are degraded in lysosomes, and the remaining amino acids are transported across the basolateral membrane by amino acid transporters.
99% are reabsorbed this way, 1% is lost in the urine.
What are the segments of the loop of Henle? What are their key features (if any)?
Descending thin segment
Freely permeable to water
Few mitochondria
Ascending thin segment
Thick ascending segment
20-25% of filtered Na+, Cl-, and K+ are reabsorbed here
Impermeable to water
High metabolic activity
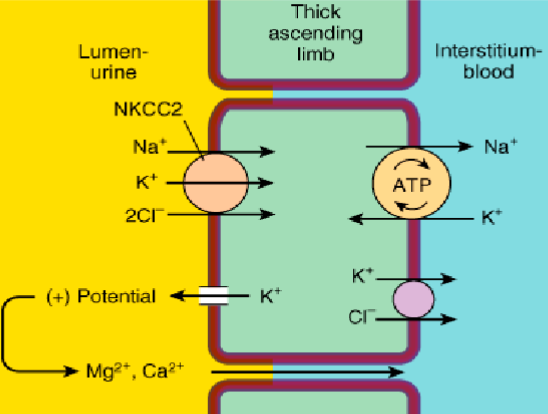
How does transport in the loop of Henle work (3 main mechanisms)? Draw the diagram.
1-sodium, 1-potassium, 2-chloride co-transporter (NKCC2) in the thick ascending loop moves 1 Na+, 1 K+, and 2 Cl- into the cell from the urine. Movement of sodium across the luminal membrane is primarily mediated by this pump.
Sodium-potassium ATPase also functions here to bring 3 Na+ from the cell to the blood, and 2 K+ from the blood to the cell.
Backflow of K+ into the lumen through K+ channels creates a trans-epithelial voltage along the thick ascending limb, such that the lumen is positive relative to the interstitial fluid. This drives paracellular reabsorption of luminal divalent cations like Mg2+ and Ca2+ into the blood through tight junctions.
What does the first portion of the distal tubule do?
Forms part of the juxtaglomerular complex, where the distal convoluted tubule comes in contact with the afferent arteriole. Here distal tubular cells become highly specialized and are referred to as the macula densa. They respond to changes in Na+.
Activation of the macula densa triggers highly specialized cells lining the afferent arterioles (granular juxtaglomerular cells) to release renin into the blood stream.
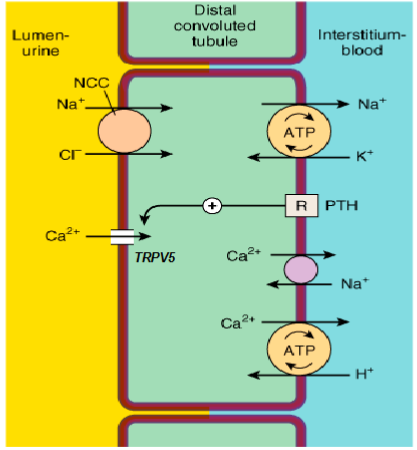
How does transport in the second portion of the distal tubule work? Draw the diagram.
Contains sodium-chloride co-transporter (NCC) that bring 1 Na+ and 1 Cl- from the lumen into the cell.
Contains sodium-potassium ATPase.
Mediates reabsorption of luminal Ca2+ via ion-specific Ca2+ channels (TRPV5). They can then cross the distal tubule basolateral membrane via specific Na+/Ca2+ exchangers and Ca2+ ATP-ases that exchange Ca2+ for H+.
How does transport in the collecting duct work? Draw the diagram.
Have Na+ specific ion channels that let Na+ into the cell from the lumen. No co/counter-transport so Cl- and HCO3- are left in the lumen, making it negative. This draws K+ out of the cell into the lumen through K+ ion channels. Can also move Cl- from the lumen into the blood through paracellular transport.
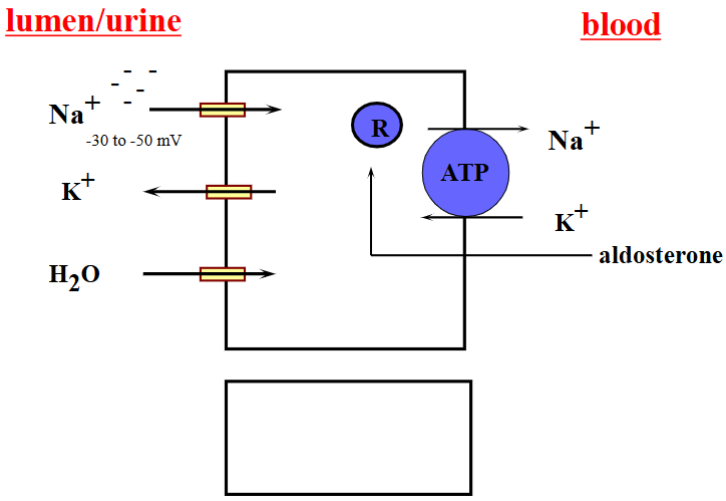
How is transport in the collecting duct regulated?
Reabsorption of Na+ and secretion of K+ are regulated by aldosterone. It increases synthesis of proteins including Na+ channels and Na+/K+-ATPase. It also causes mitochondria to be produced.
How is permeability of the collecting duct controlled?
By antidiuretic hormone (vasopressin). It increases the permeability of the collecting duct to water, concentrating the urine. It does this by stimulating a G-protein coupled receptor in the basolateral membrane, which cases cAMP to be produced, promoting the insertion of aquaporin-2 into the apical membrane.
What is diabetes insipidus?
A deficiency of antidiuretic hormone (vasopressin), resulting in a large volume of urine being excreted because it is not being concentrated.
What are the functions of the kidneys?
Remove waste products from your body (urine)
Control composition, volume, and pH of body fluids
Help maintain healthy bones
Control blood pressure
Help the body produce red blood cells
How do the kidneys control blood pressure?
1) The juxtaglomerular cells (JGCs), lining sections of the afferent and efferent arterioles by the macula densa, secrete renin.
2) Renin cleaves the circulating angiotensinogen, formed by the liver, to the decapeptide angiotensin I (ATI).
3) Angiotensin converting enzyme (ACE) cleaves ATI to the active octapeptide ATII.
4) Angiotensin II performs four main functions that all work to increase intravascular volume and raise blood pressure.
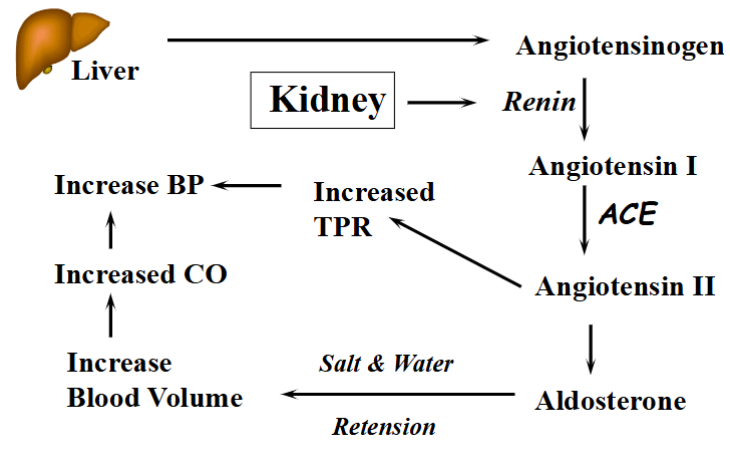
How does angiotensin II raise blood pressure?
Stimulates aldosterone secretion from the adrenal cortex, promoting reabsorption of NaCl into the blood.
Causes arteriolar vasocontriction.
Stimulates thirst.
Stimulates antidiuretic hormone secretion (ADH / vasopressin)
How does the secretion of antidiuretic hormone raise blood pressure (2 ways)?
Acts on V1 receptors on vascular smooth muscle, causing the muscles to contract, causing increased resistance in the blood vessels.
Acts on V2 receptors in the collecting duct of the kidney, causing AQ2 to be translocated to the plasma membrane, increasing the absorption of water into the blood.
What three mechanisms control the release of renin by the juxtaglomerular cells?
1) Direct pressure sensing with the afferent arteriole. Decreased blood pressure increases renin release.
2) Sympathetic innervation of the juxtaglomerular cells. Promotes renin release via B1-adrenoreceptor signaling. When B1 cells are stimulated, renin release is increased.
3) Specialized cells in the distal tubule (macula densa) that are sensitive to NaCl concentration. Decreased luminal NaCl delivery increases renin release.
How do the kidneys help to maintain healthy bones?
Respond to parathyroid hormone to increase the reabsorption of calcium in the second portion of the distal tubule and the proximal tubule.
When and how is parathyroid hormone release?
In the presence of decreased extracellular Ca2+ levels, reduced activation of the calcium-sensing receptor (CaSR) in the parathyroid glands results in a rapid increase in parathyroid hormone (PTH) secretion.
What receptors does parathyroid hormone act on? What does this result in?
PTH1R in the kidneys. This increases calcium reabsorption by activating TRPV5 in the second portion of the distal tubule.
CYP27B1 in the proximal tubule. This promotes the conversion of inactive vitamin D to active vitamin D (calcitriol). Calcitriol acts on the intestine to increase the absorption of dietary calcium via the vitamin D receptor (VDR).
PTH1 receptor in the bone. Increases osteoclast activity, resulting in a transfer of calcium from bone tissue to the blood.
How do the kidneys help to make more red blood cells?
The kidneys contain non-endothelial renal interstitial cells called erythropoietin-producing cells (EPCs) or fibroblasts. Under hypoxic conditions, hypoxia-inducible factor (HIF-2) is activated and signals for erythropoietin (EPO) to be produced by these cells.
Erythropoietin stimulates the proliferation and differentiation of erythroid progenitors into reticulocytes, and prevents their apoptosis. More reticulocytes enter the circulating blood and differentiate into erythrocytes. This increases the RBC pool.
How does chronic kidney disease affect erythropoietin-producing cells?
It causes they to transdifferentiate into myofibroblasts, which synthesize collagen and lose their ability to produce erythropoietin.
How does erythropoietin play a role in iron metabolism?
When erythropoietin secretion is decreased, the reduction in erythropoiesis means that the erythroblast decreases erythroferrone production. This increases levels of hepcidin, which negatively effects iron absorption and mobilization.
How is iron taken up from the intestine?
Using divalent metal transporter 1 (DMT1).
How are iron levels controlled?
Ferritin stores some iron in cells and releases it in a controlled fashion.
Ferroportin binds some iron and transfers it to transferrins (iron-binding blood plasma proteins) to be brought out of the cell. This controls the levels of free iron in biological fluids.
How does hepcidin decrease the amount of iron absorbed into the body?
Bind to ferroportin, causing it to be internalized and degraded. As a result, more iron stays in the intestinal cells and gets bound to ferritin because it is not being transported.