2153 IC7
1/16
Earn XP
Description and Tags
cardiac output and heart failure
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
17 Terms
Define cardiac failure (2 def)
Failure of the heart to pump at a sufficient rate to service the metabolic requirements of the tissue OR the ability to only do so at elevated filling pressure (through compensation. Elevated filling pressure is still heart failure)
Define HFrEF, common causes, and treatment
Heart failure with REDUCED ejection fraction (EF <40%)
left ventricle fills with blood but is only able to pump out <40% of what it was originally filled with (HFrEF) during systole
DECREASED CONTRACTILITY > decreased time in systole > decrease in CO
also if there is INCREASED AFTERLOAD (higher pressure > LV hypertrophied > increased oxygen demand but lower oxygen supply because blood cannot pass through as easily)common causes: MI, HT, arrythmia, abnormalities of the ventricular muscle itself
treatment: reduce blood vol. load using DIURETICS and ACE-i to counteract the effects of RAAS
Define HFpEF
heart failure with PRESERVED ejection fraction (EF >50%)
thicke, stiffer, hypertrophied left ventricle > incomplete filling during diastole when blood is supposed to enter ventricle from atria because inadequate relaxation of LV, cannot suck blood in > need higher pressure to fill left ventricle > increases left atrial pressure > increase in pulmonary venous pressure > pulmonary edema and heart failure (back pressure effecT)
also reduced stroke volume due to lower end diastolic volume. but CO is usually not compromised AT REST
causes: many
treatment: diuretics
List major causes of cardiac failure (aka reduction of cardiac failure) related to preload, contractility and afterload
preload (venous return and filling of the heart)
e.g. haemorrhage = excessive blood loss from circulation > decrease in venous return to the heart/ decreased blood pressure so reduced ventricular filling > decrease in preload.
e.g. increased HR > less filling time = decrease in preload
heart
e.g. myocardial infarction >> lack of blood supply to the heart due to blockage of coronary artery > heart muscle dies > cannot pump out with enough strength > cardiac output compromised
bradycardia = slow heart rate > low increase in diastolic volume > cardiac output compromised
afterload
e.g. hypertension (increase in blood pressure) > increase in worload on the heart because of increased blood volume > heart works against resistance > hypertrophies overtime > remodelling > less effective pump
Outline how the body compensates for cardiac failure acutely and what are the patient presentations
via the ACTIVATION of sympathetic and SUPPRESSION of parasympathetic nervous system
increases the heart rate and increases the contractility of the heart >> increases cardiac output as a compensation
increase heart rate, increase strength of cardiac contractions, sweating
Outline how the body compensates for cardiac failure on the longer term and what are the patient presentations
RAAS activated
kidneys sense a drop in blood pressure > increase retention of salt and water volume > increase blood volume > increase cardiac output
less urine (oliguria), increased fluid accumulation > edema and breathlesness, remodelling of the heart and blood vessels = worsens heart failure
will become maladaptive overtime
define cardiac output (which ventricle?)
cardiac output is the volume of blood pumped out by the right and left ventricle into the aorta per minute
does not eject all the blood that it is filled with (ejection fraction)
ex. ejected = 60ml, filled = 100ml = EDV (60% EF), remaining = 40ml (ESV)
how many litres of blood does the heart pump out per min in a healthy adult?
around 5L/min for each ventricle
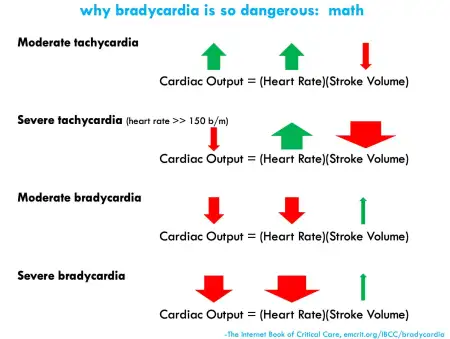
what is the equation for cardiac output?
CO = SV x HR
SV = stroke volume (volume of blood ejected by left ventricle in one stroke/heartbeat)(avg ~ 70-80ml/beat)
HR = heart rate
*change in HR not necessarily proportionate to change in CO. if HR is too fast, compromises SV —> decrease in CO
if HR is reduced but SV increased, might maintain CO
why is cardiac output important?
affects the perfusion rate (rate of blood flow through capillaries) is sufficient to meet the metabolic requirements of the tissues
CO drops = perfusion drops = insufficient supply of nutrients to the tissues
what are the factors that affect CO?
preload (related to EDV, vol. of blood heart is filled with, dependent on venous return (venous constriction would increase preload.)
contractility (force of contraction of the heart muscle. Greater the force, greater the degree of contraction)
afterload (resistance that the ventricle overcomes to eject blood. dependent on vascular pressure (pressure of LV > pressure of aorta) and valve damages)
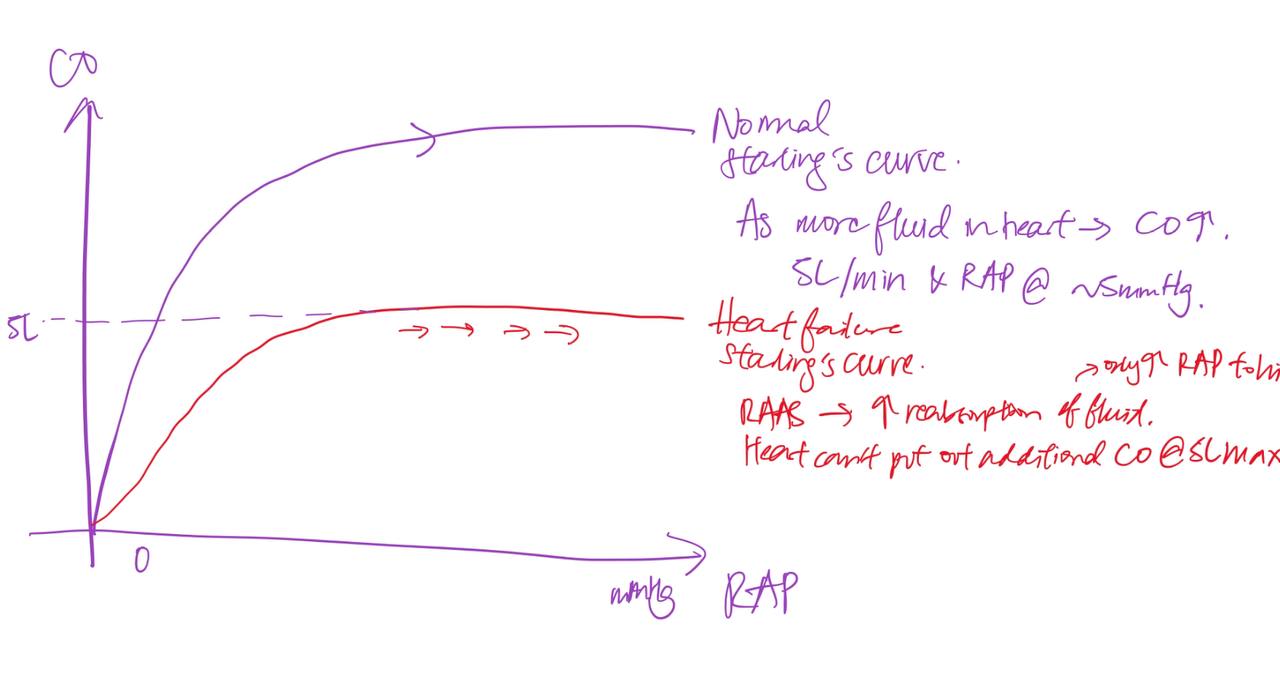
how can fluid reabsorption by the kidneys become maladaptive
RAAS > increase reabsorption of fluid > increase right atrial pressure to higher levels > venous pressure increases > fluid cannot be reabsorbed back in the body so comes out to interstitial spaces > edema
excessive fluid reabsorption cannot increase cardiac output beyond a certain limit
excessive venous pressure > edema > breathlessness
frank starling’s curve:
how is chronically elevated levels of angiotensin II maladaptive
increased levels of Ang2 and its effects > remodelling of the heart caused by inflammation, fibrosis and hypertrohy makes it less effective as a pump over time
increased levels also increases the heart’s workload > Ang2 decreases the conc. of NO of the blood which is an important vasodilator > vasoconstriction > resistance increases
what plays a role in increasing cardiac output during exercise? decreased contractility, increase peripheral resistance, decreased venous pooling or decreased preload?
DECREASED VENOUS POOLING
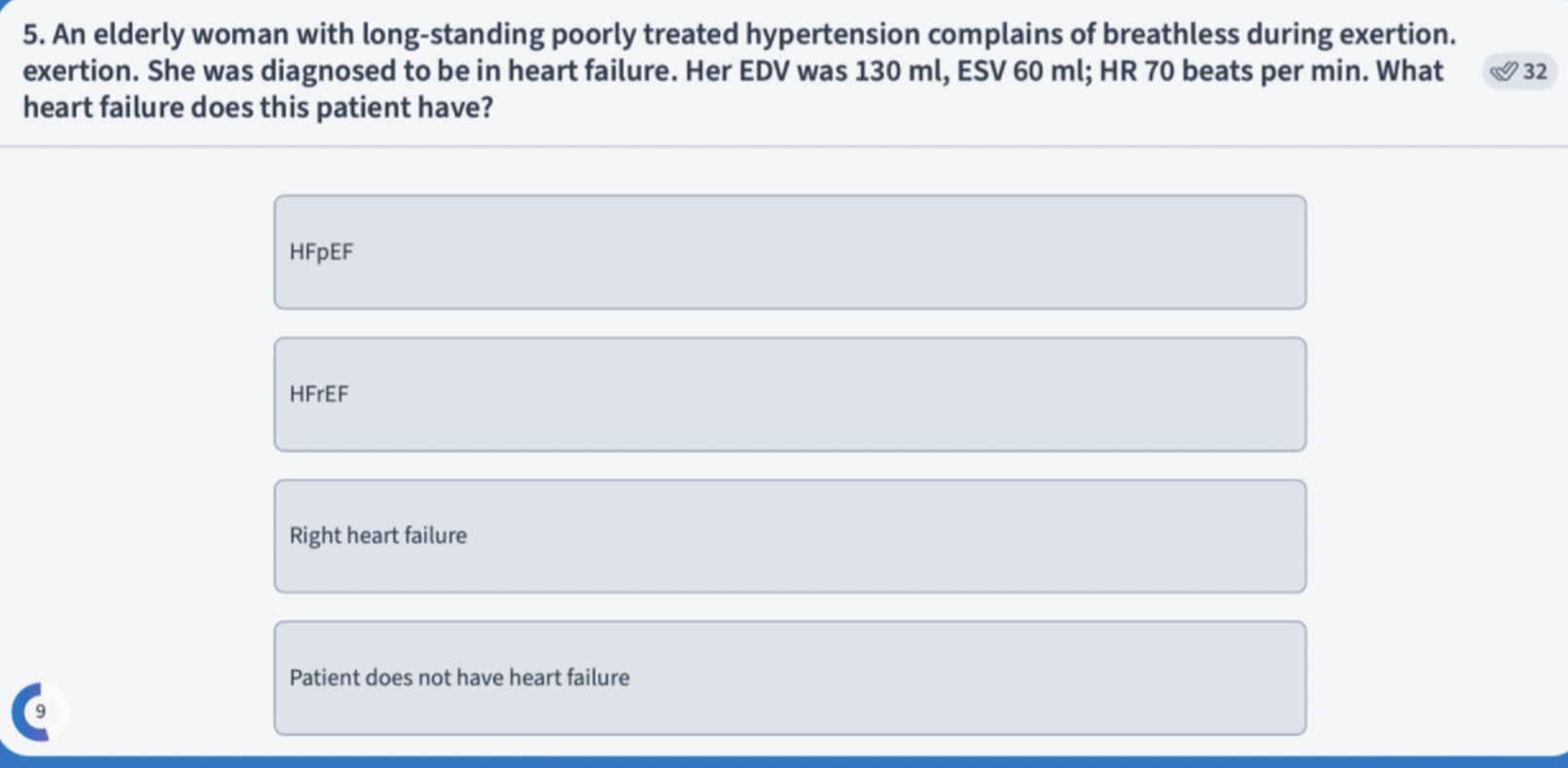
HFPEF
70 × 70 = 4900 or 4.9L/min
ejection fraction = SV / how much the ventricle is filled (EDV)
can you describe the natriuretic peptide system in heart failure
increase in heart failure > increase in atrial stretch > increase in natriuretic peptides to counteract RAAS > vasodilation and diuresis and natriuresis
why do you use ARBs with neprilysin inhibitor? (ARNIs)
neprilysin inhibitors increases the availability of natriuretic peptides by inhibiting the breakdown of the peptides so that it continues to exert its effect. used in combination with ARNIs to inhibit the ang2 from exerting its effects