Neuroanatomy 4 -- development of nervous system 3
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
43 Terms
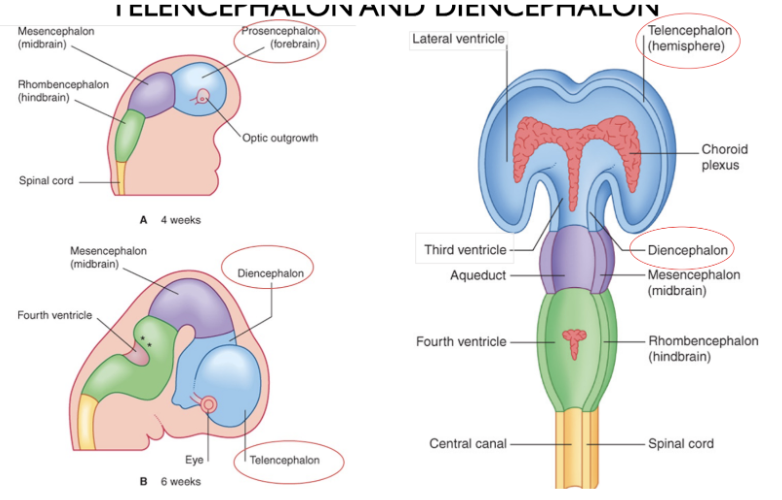
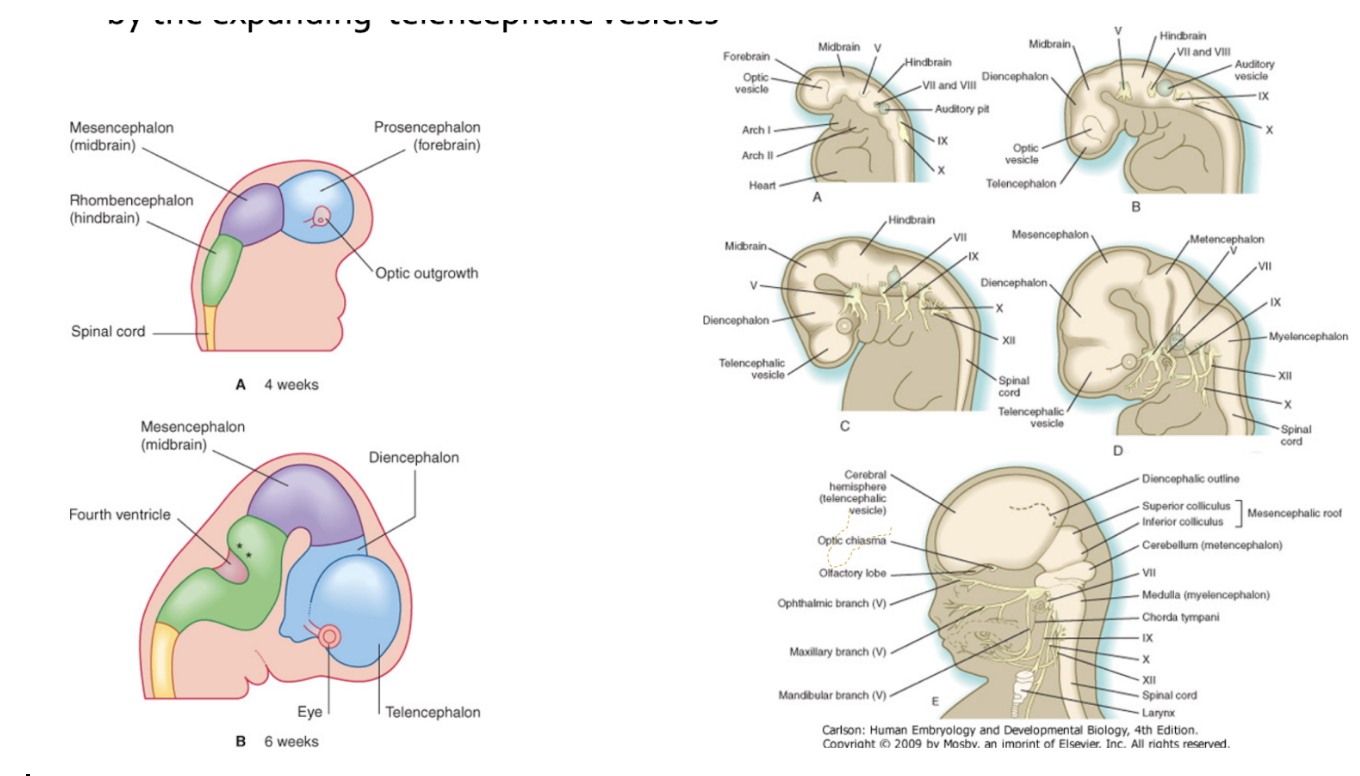
Three part & 5 part human brain –
First subdivision
Forebrain (prosencephalon)
Midbrain (mesenchephalon)
Hindbrain (rhombencephalon)
Second subdivision
Prosencephalon →
Telencephalon & diencephalon
Rhombencephalon →
Metencephalon & myelencephalon
Midbrain (mesencephalon)
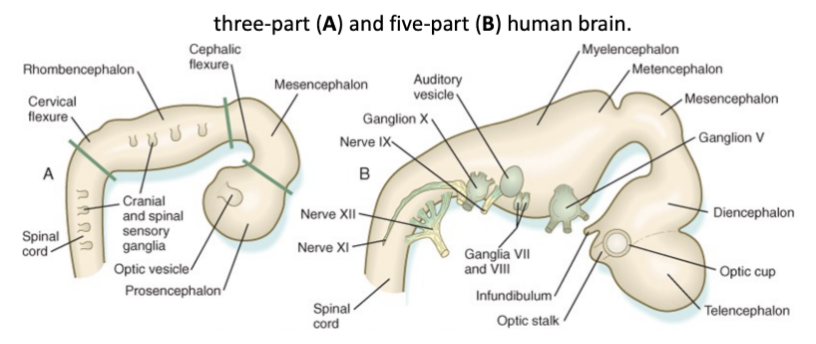
Cranial nerves in relation to different divisions of brain
3.5 mm swellings in the rhombencephalon, marking how it is divided into 2 sub territories which will originate from the 5th to 12th cranial nerve
Motor & sensory nerves from the 5th to 12th cranial nerve are placed in rhombencephalon
Each of these subsegments of the rhombencephalon harbor the nuclei of the cranial nerves of 5th → 12th cranial nerve
4th & 3rd are related to mesencephalon
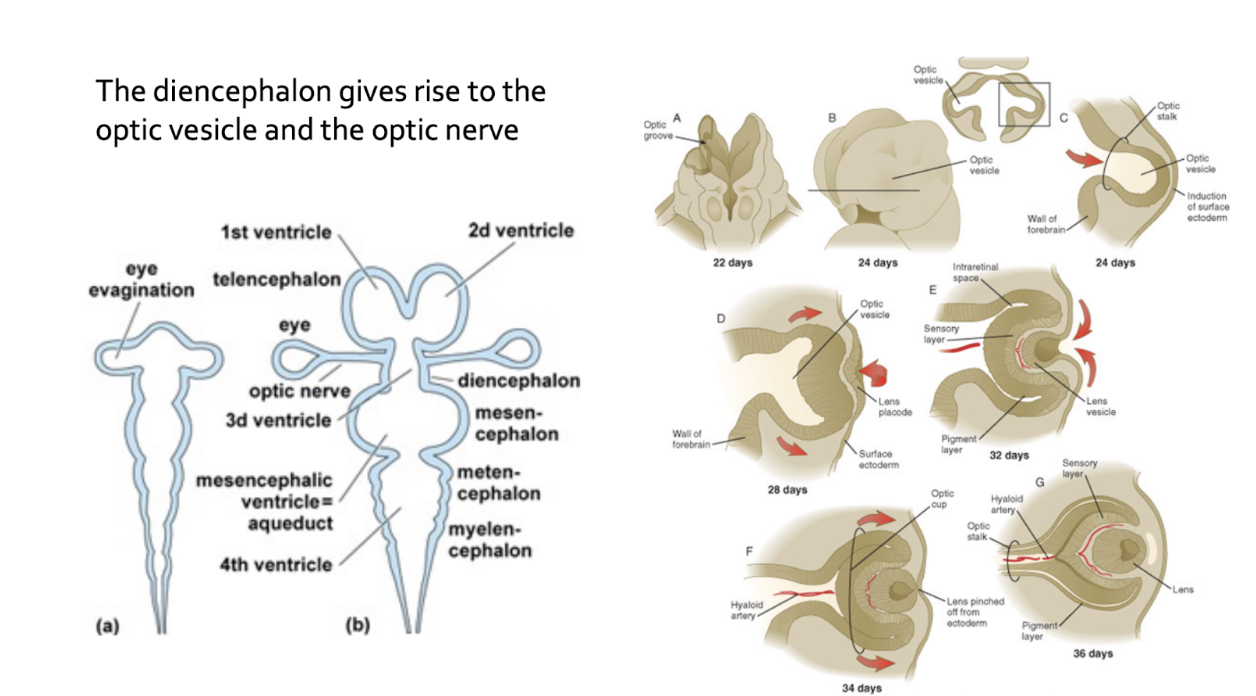
First 2 cranial nerves (olfactory from prosencephalon, while optic nerve originates from the diencephalic portion of the prosencephalon)
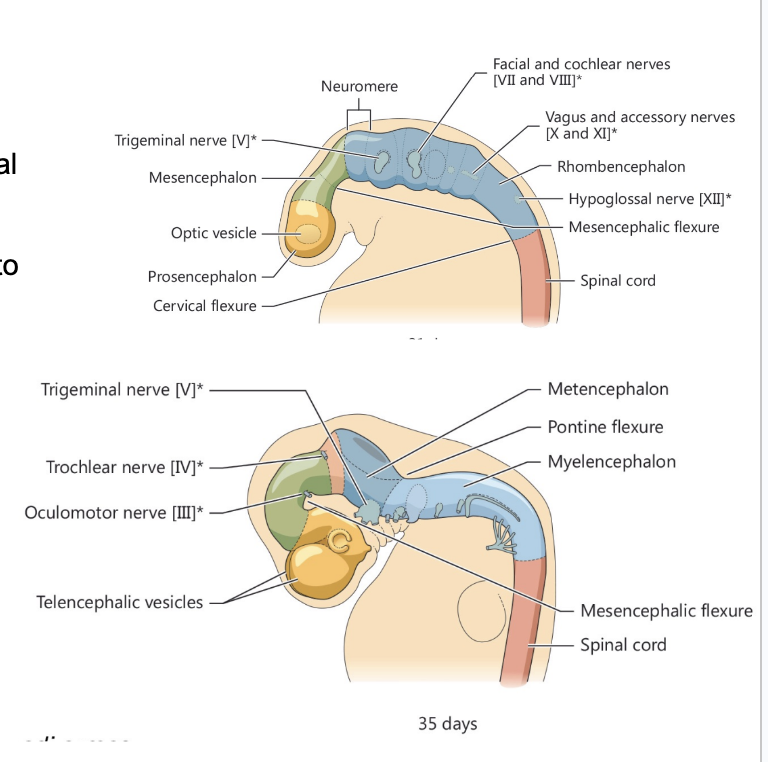
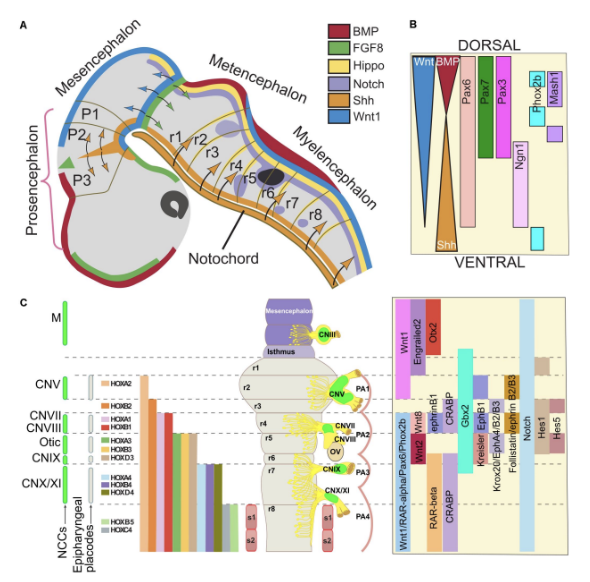
Patterning of the rostral portion of the neural tube –
Rhombomeres and prosomeres
Formation of cranial nerves
Some more concentrated ventrally, some more concentrated dorsally
Ex. HOX genes, FGF, Shh, etc.
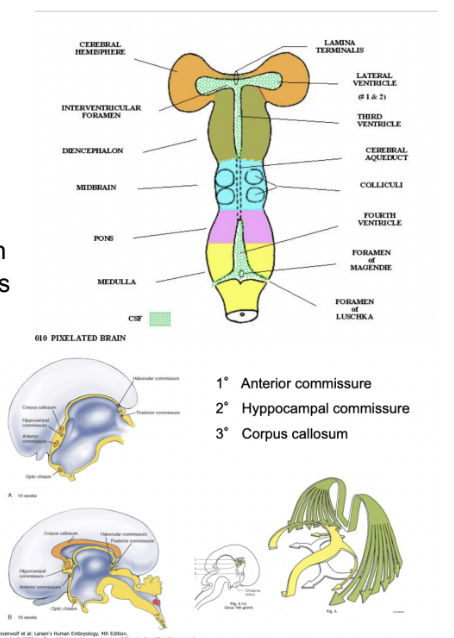
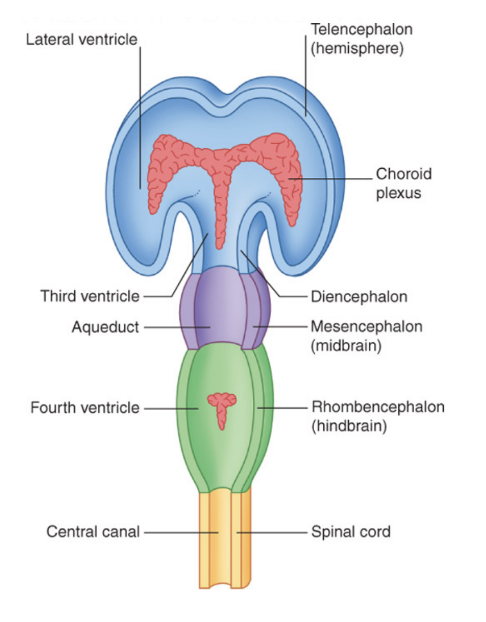
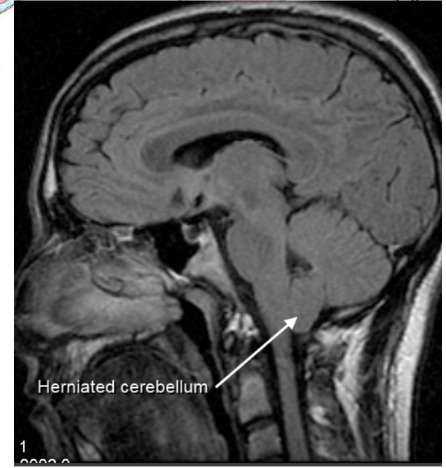
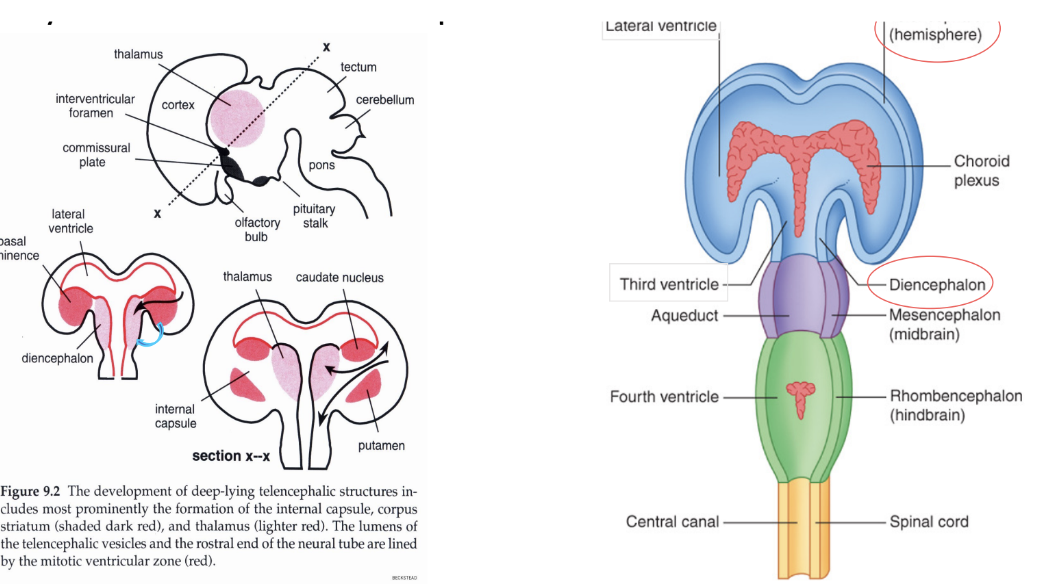
Ventricular system – lumenal shape changes
The shape of the lumen of the tube changes
Spinal cord very tubular & simple, but because of proliferation of neural tube wall, cavity becomes narrower & narrower at end of spinal cord (central/spinal/ependymal canal)
In the vesicular portion, form a system of ventricles (in brain) – at level of rhombencephalon, we have formation of 4th ventricle
Canal of spinal cord communicates with 4th ventricle
At level of mesencephalon (midbrain), lumen becomes very small and opens into mesencephalic/sylvian aqueduct
Sylvian aqueduct communicates with 3rd ventricle at level of diencephalic vesicle, which then communicates with the lateral ventricle – what remains of original cavity at level of 2 cerebral hemispheres
Highly vascularized regions, production of CSF – Choroid plexuses
At level of roof of 4th, 3rd ventricle & medial wall of lateral ventricles, wall of neural tube becomes very very thin, and we have formation of choroid plexuses
Regions where from blood there is formation of fluid (cerebrospinal fluid, CSF) found inside ventricular cavities & spaces surrounding the brain
Brainstem
Spinal cord communicates with brainstem, which is made of 3 regions (caudal → rostral –) (originate from rhombencephalic vesicle (separates into myelencephalon & metencephalon) & mesencephalon)
Medulla oblongata
Originates from Myelencephalon
Pons
Originates from Metencephalon
Midbrain – Mesencephalon
Originates from mesencephalon
In adult, brainstem doesn’t look segmented like spinal cord — why?
Spinal cord has clear segmental organization, and also the spinal nerves (originating from roots) have nicely organized segmental organization – on right & left on each segment we have a nerve – on the other hand, brain doesn’t have macroscopic segmental organization – from the brain stem we have the origin & exit of 10 cranial nerves – from the 3rd to the 12th
No segmental organization in their exit –
Due to cranial nerves having an heterogeneous composition (unlike spinal)
The internal organization of the brainstem cannot be the same of the spinal cord — why
Inside the spinal cord, you can find
An Alar plate & an Baal plate
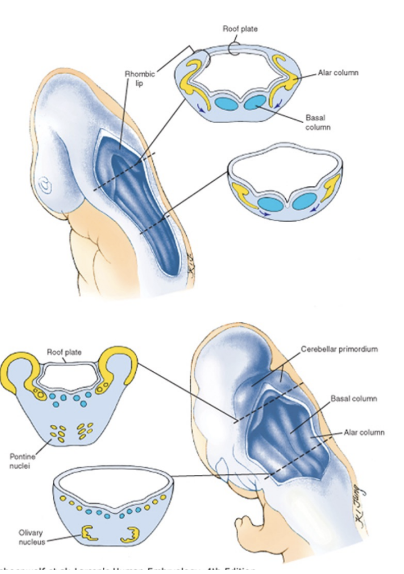
But in the brainstem, especially in rhombencephalon derivatives, things change very much – In the rhombencephalon, we have 2 things occurring
A “booklike” opening, leading to formation of the 4th ventricle
Fragmentation of the plates – no ventral & dorsal horn but clusters of neurons into nuclei
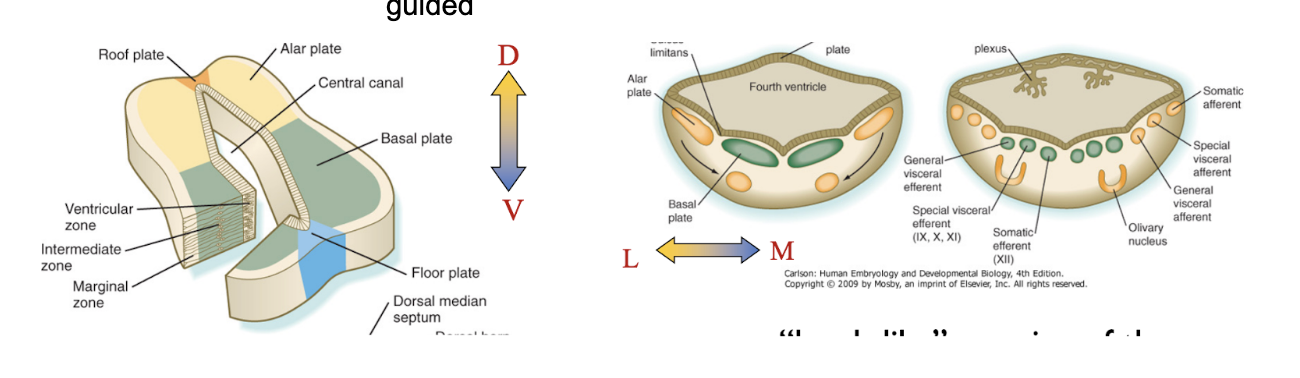
“Booklike” opening leading to formation of the 4th ventricle
Roof plate becomes quite stretched, alar plate moves laterally, basal plate located medially
Rostral part of myelencephalon booklike opens, caudal doesn’t but rather grows into 4th ventricle –
Original roof of this ventricle is the stretched roof plate
Metencephalon fully opens, myencephalon only rostrally opens — why adult medulla oblongata has both open & closed part
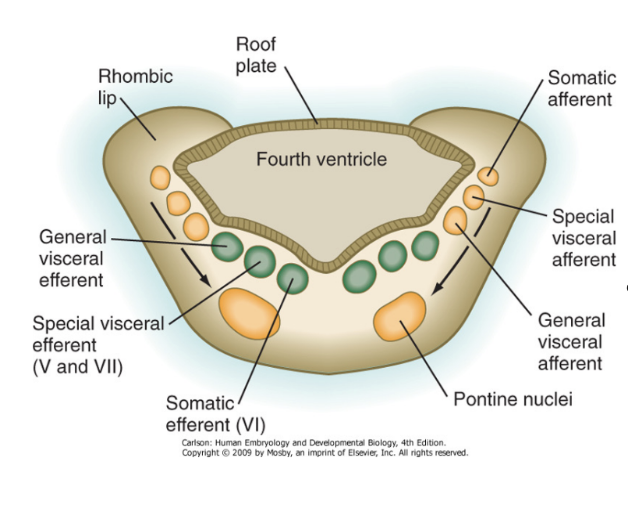
Fragmentation of the plates – no ventral & dorsal horn but clusters of neurons into nuclei
Neurons of basal & alar plate migrate to form clusters – becoming specific nuclei of the cranial nerves (motor & sensory)
Organize themselves in a pattern to form nuclei, with this being guided
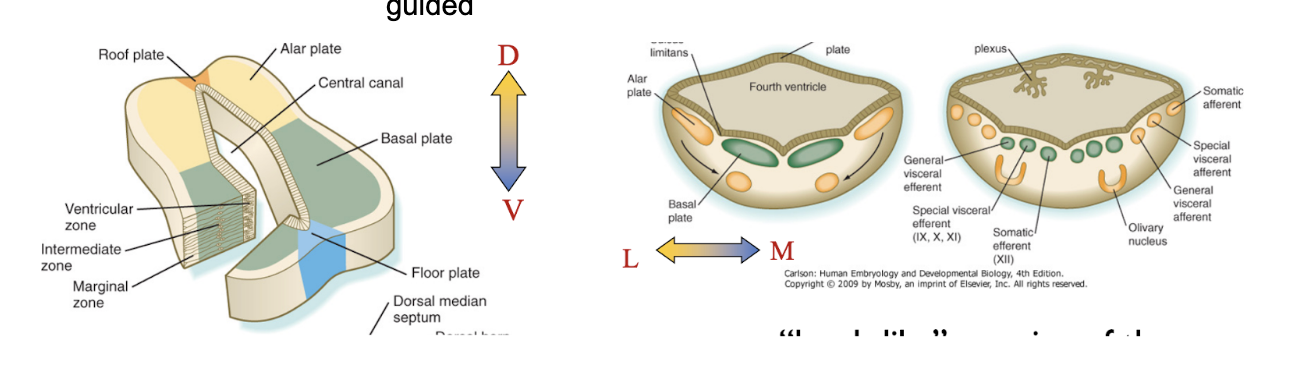
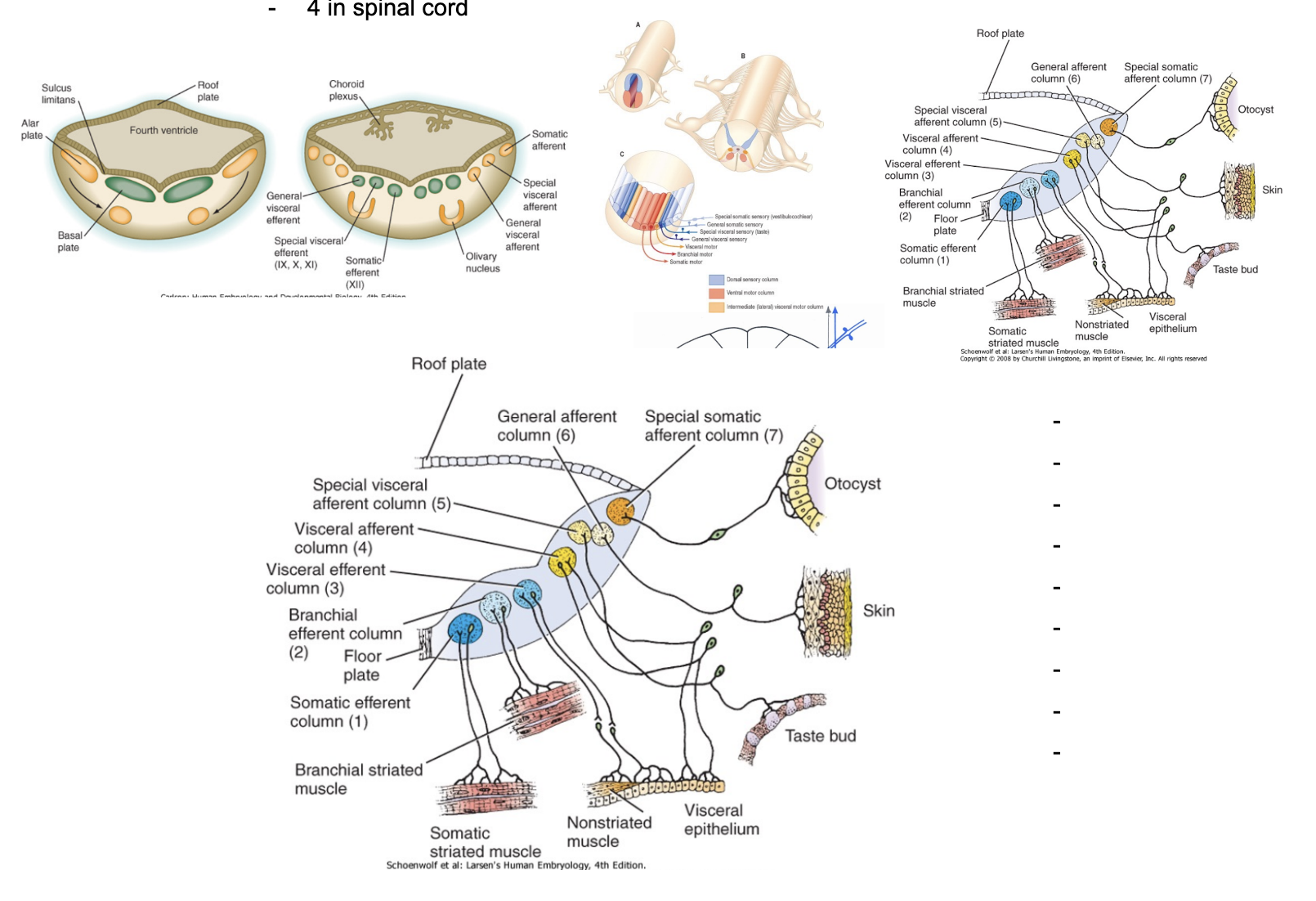
Territories (of brainstem & spinal cord)
4 in spinal cord
7 in brainstem
Each of the 7 territories is not always present along the longitudinal axis of the brainstem
Cranial nerves differ in composition
Specific nuclei not related to cranial nerves belong to pathways forming control centers
Control vital functions – ex. Motor circuits, communicate with cerebellum, etc.
Most of the specific nuclei originate from the alar plate
Explains homogenous vs heterogenous —
Each segment of spinal cord has all 4 territories, but not each cranial nerve has all 7 territories (ex. XII only somatic efferent)
Changes occuring to mesencephalic vesicle –
No book-like opening but fragmentation of the plates into nuclei
Mesencephalic aqueduct (of Sylvius)
Lamina quadrigemina (Tectum)
Book-like opening of rhombencephalon causes (& 4th ventricle importance)
The formation of an enlarged cavity – the 4th ventricle –
Floor & roof communicate with subarachnoid spaces
4th ventricle is very important – arachnoid forms a space called the subarachnoid space (space between trabeculae of arachnoid), and in this space we find CSF
CSF is produced at level of plexuses & released in ventricular cavities, but is also in subarachnoid spaces surrounding CNS – must be a connection between them
This communication is only at the level of the 4th ventricle – important bc REALLY bad if some sort of obstruction
CSF flow — from lateral ventricle choroid plexuses to those of 3rd ventricle, then at level of 4th ventricle continues below to fill spinal canal & at the same time exits into subarachnoid space, where there mostly absorbed by venous sinuses
Roof of the 4th ventricle
tela choroidea — gives rise to choroid plexuses
Flow of cerebrospinal fluid
Cerebellum –
Above roof of 4th ventricle in the posterior cranial fossa
Connected to brainstem through 3 pairs of cerebellar peduncles —
Superior peduncles — connect to midbrain
Middle peduncles — largest & connect to pons
Inferior peduncles — connect to medulla oblongata
Derives mostly from proliferation of alar plate of the metencephalic vesicle (pons), forming a region called the rhombic lip (thickening on lateral sides of pons), and these lateral thickenings grow until they reach each other medially to cover the roof of the 4th ventricle
Cells keep on growing to finally give rise to vermis, with a cerebellar hemisphere on each lateral side
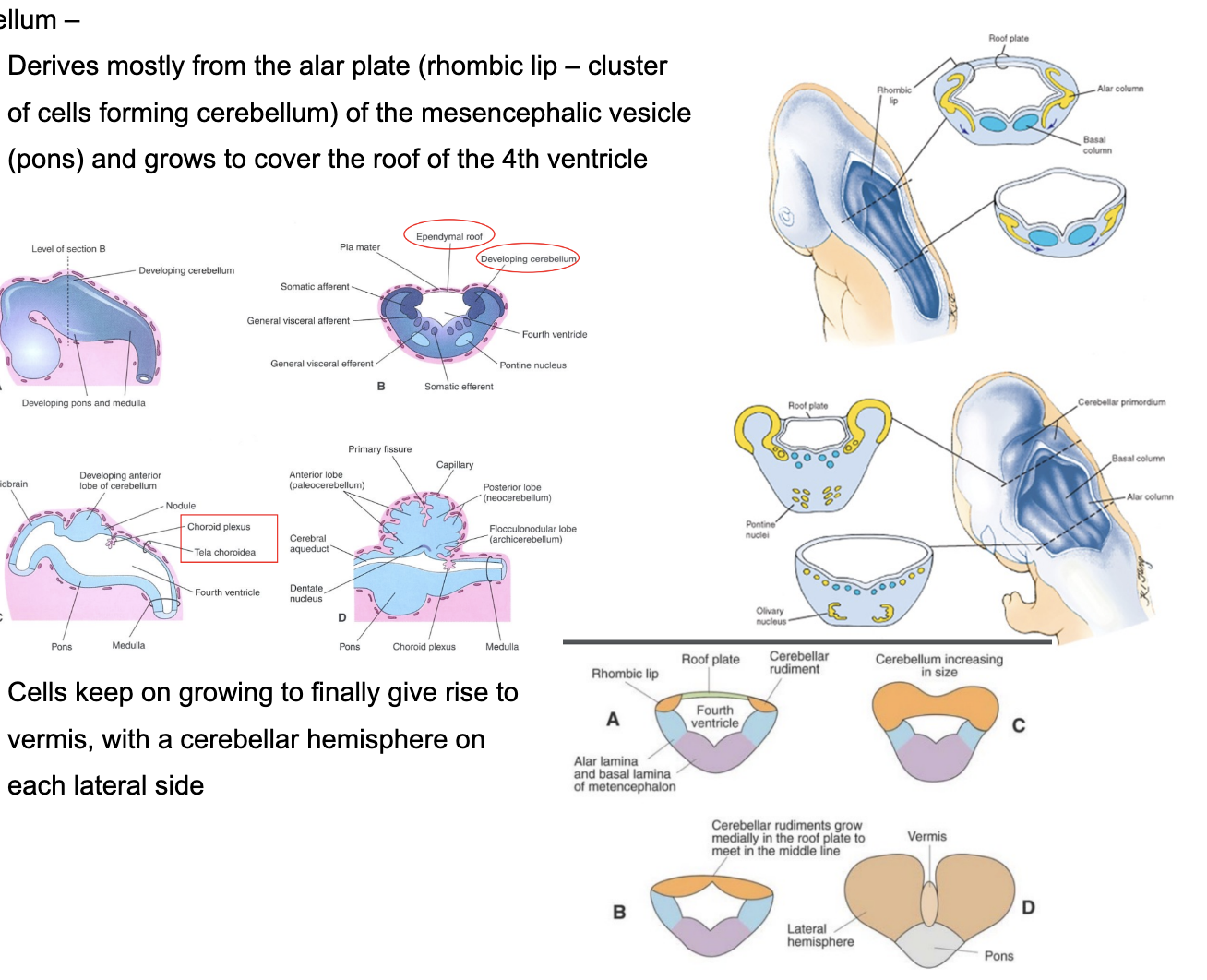
Vermis and Hemispheres –
Cerebellum is divided into lobes –
Anterior lobe, posterior lobe, & Flocculonodular lobe (oldest phylogenetically)
Cerebellum has 3 layers —
Outer grey matter — cortex
Medial white matter
Inner grey matter
Organized into 4 nuclei called deep nuclei
Folding of the cortex – folia
Due to huge number of neurons, cortex begins folding on itself, forming parallel folia or lamellae
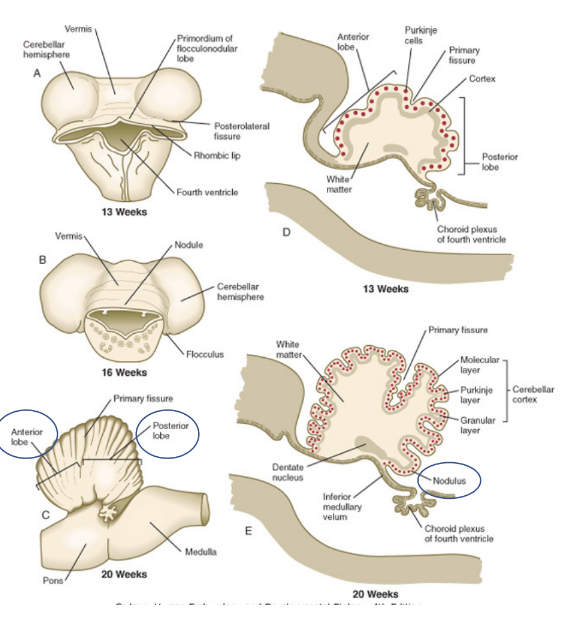
The cerebellar cortex –
Organized into 3 layers
Molecular layer
Purkinje cell layer
Granule cell layer —
External granular layer
Form due to progressive migration of cell/neurons from the ventricular region/zone – some of them organize themself very superficially, forming external germinal layer,
Small amount of neurons – largest population of neurons in CNS, biggest layer of cerebellum WHEN MATURE – ORIGINALLY most neurons are very superficial
Inner small granular layer
From here neurons will migrate deep to form internal granular layer of the cerebellum
Most neurons of cerebellum originate from the ventricles — specifically, external germinal layer present on rhombic lip — give rise to small granule cells (present from 8th week of gestation to 2nd year of life) — if issues with this mechanism (or migration?) —
If migration doesn’t occur correctly, cerebellar cortex doesn’t form correctly, leading to problems — ex. ?
Medulloblastoma
Medulloblastoma –
Most common malignant brain tumor in children
10-20% of primary CNS neoplasms & approximately 40% of all posterior fossa tumors
Highly invasive embryonal neuroepithelial tumor – arises in cerebellum
Mostly vermis but also hemispheres
Has a tendency to disseminate throughout the CNS early in its course
Causes compression of the 4th ventricle – hydrocephalus
Leads to –
Headache, lethargy, vomiting
Due to increased intracranial pressure – intermittent & subtle signs
Different types
Different types of medulloblastoma –
30-35% due to problem of external germanitive layer, can be many other reasons, but..
Most cases is a genetic problem –
damage to chromosomes, factors (ex. Shh) not working correctly – give rise to different types of medulloblastoma
Different types are divided into 4 groups that can affect a person at different ages with different localizations, anatomophysiological characteristics & symptoms
Large cell anaplastic medulloblastoma – more severe version
Highly aggressive variant – 25% of medulloblastomas – seen in young patients (1-4 yr), with a male predominence
Arnold-Chiari or Chiari spectrum of malformations –
4 syndromes — Type 1 (out of 4) is most common
Herniation of cerebellar tonsils, caudal vermis, and medulla through the foramen magnum — frequently associated with syringomyelia
Posterior cranial fossa problems
Example of (could lead to) non-communicating hydrocephalus
Obstructed CSF flow within the ventricular system
Communication at 4th ventricle is compressed
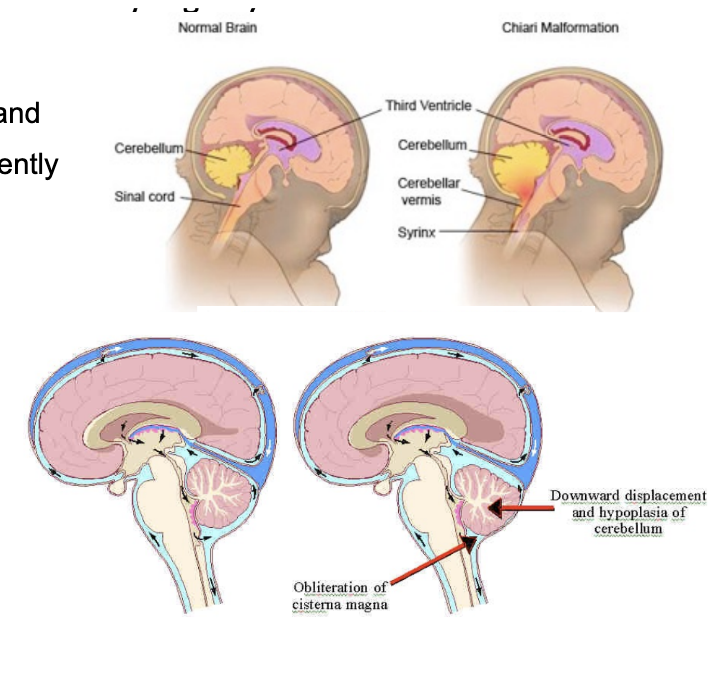
Symptoms of herniated cerebellum –
Cerebellar signs –
Ex. ataxia (lack of coordination), vertigo (spinning), nystagmus (eye fuckery)
Brainstem signs
Ex. respiratory & cardiac arrest, or signs relating to them
Cranial nerves stretching (CN IX, X, XII) – dysphonia, difficulty in swallowing, vocal cord paralysis, diminished gag reflex
Hydrocephalus
(abnormal buildup of CSF in ventricles)
Dandy-walker malformation or syndrome –
Most common malformation of the posterior cranial fossa
Agenesis or hypoplasia of the vermis and cystic enlargement of the fourth ventricle, occipital meningocele
Appears to be associated with atresia of the foramen of Magendie and foramen of Luschka
Causes —
Clinical history/genetics —
May appear sporadically, or may show autosomal-recessive or X-linked inheritence
Risk of chromosomal anomalies —
High, with up to 35% of cases being associated with aneiploidy — mainly trisomies 18 & 13
Teratogens —
Congenital infections
Embryology —
Develops in the 5th to 6th week after conception
Congenital Aqueductal Stenosis
X-linked traits or autosomic
Infective causes:
cytomegalovirus or toxoplasmosis
Dilated lateral and third ventricles
Other CNS malformations
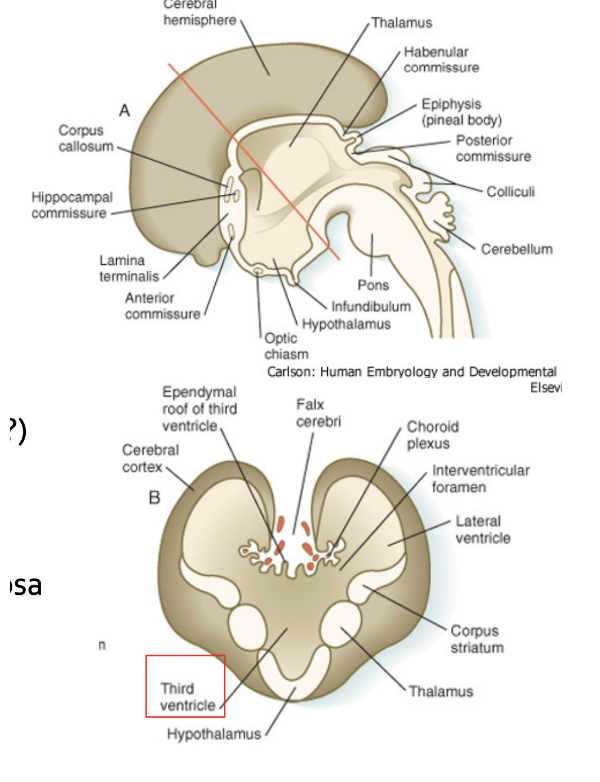
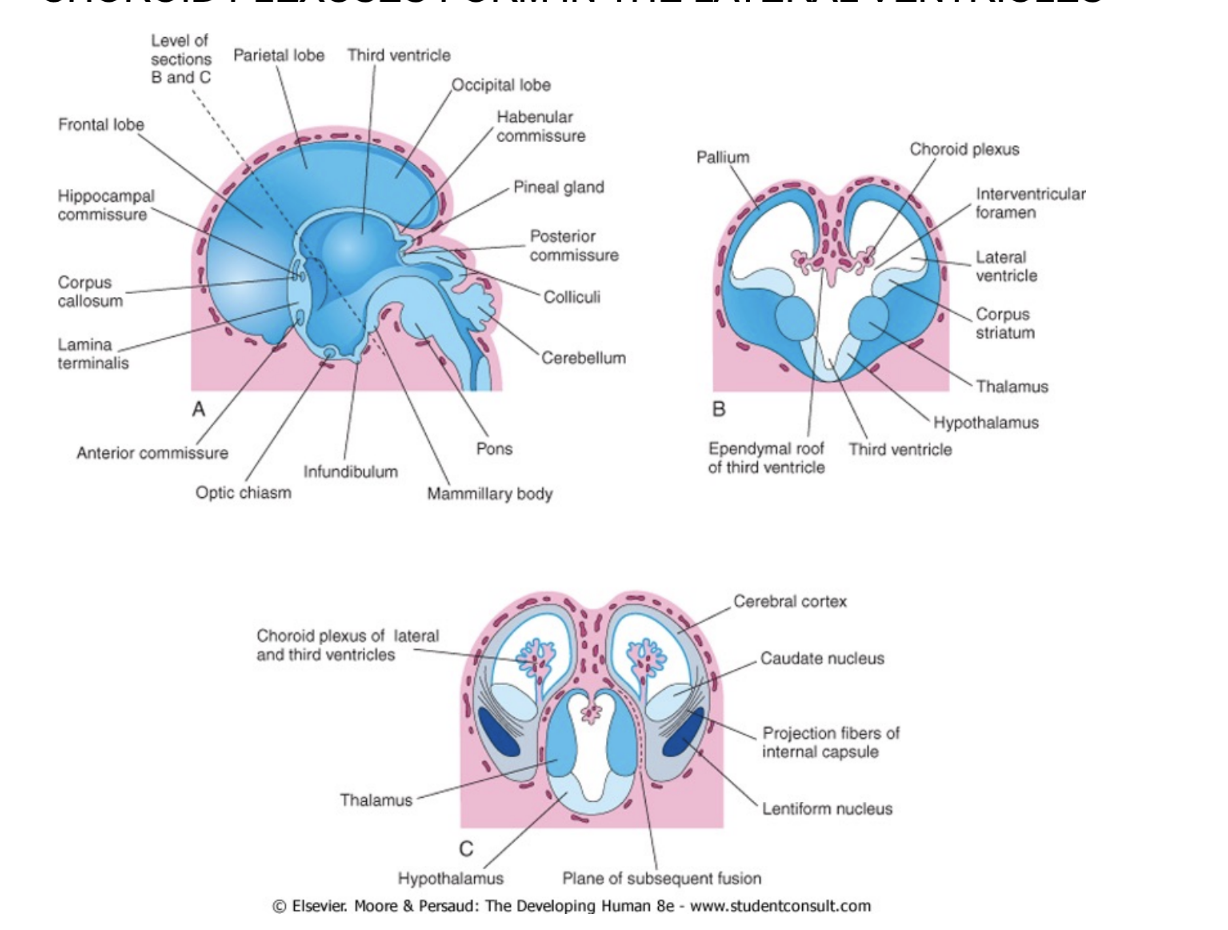
Forebrain or Prosencephalon division
Telencephalon
Gets divided into 2 telencephalic vesicles
Diencephalon
Telencephalon & Diencephalon were in series, but then in the adult, must look at ventral surface to find diencephalon – so what happens?
The telencephalic vesicles grow very much due to the process of cephalization, with the development of the neocortex. At some point, these 2 vesicles grow & grow & try to grow anteriorly, but find the skull developing, so they grow dorsally, and curve more & more (more bones blocking), and try to grow posteriorly, but there there is squama of temporal bone – grow but bend and acquire a C shaped appearance
The diencephalon is embraced/enveloped between the two telencephalic vesicles
At development completed, we see only the ventral portion of the diencephalon — image
Because the diencephalon is surrounded b y the telencephalon..
In the same plane of section we find diencephalic and telencephalic structures
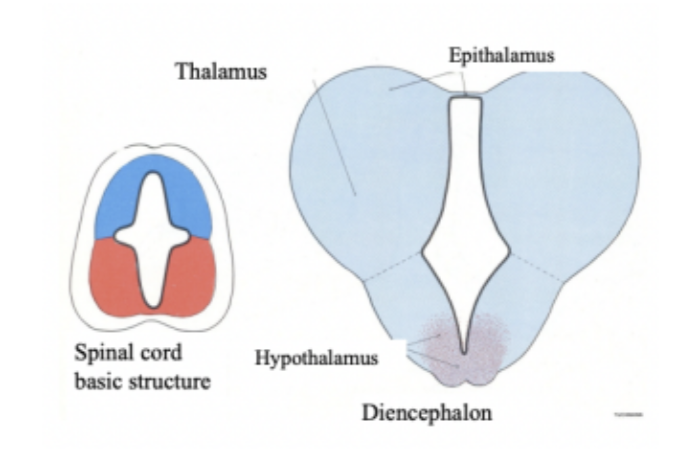
Development of diencephalic vesicle –
Has a roof with alar plates & a base with basal plate — territories separated by sulcus limitans — thus divided into roof, lateral walls, & floor, each giving rise to different things —
Thinning of the roof –
So thin that most of it becomes a Tela choroidea (preformation for choroid plexus), with the formation of a Choroid plexus at that level – 3rd ventricle.
Posteriorly, there is an area that develops as nervous tissue – called Epithalamus – (in posterior portion) can find the pineal gland (melatonin)
Thickening of the lateral walls
Above the sulcus limitans —
The body develops in what will be called the thalamus
Very important region of CNS – door to the cortex – most information reaching cortex stops in thalamus first
And the metathalamus
Very specific – involved in the nuclei of the thalamus that project the acoustic & optic information to the cortex
Where medial & lateral geniculate bodies will form
(acoustic & optic paths)
Below the sulcus limitans —
Subthalamus
Below thalamus & caudally & laterally to hypothalamus
Hypothalamus
(diencephalic vesicle & 3rd ventricle shaped like a funnel – narrower and narrower)
Outpocketings of the floor
Will give rise to the optic vesicles
These forms 2 extroflections that grow to periphery & form the retina & eye structures while remaining connected to diencephalon via the optic nerve
The narrowest portion will become the infundibular process/eminence – will give rise to the neurohypophysis
Infundibular process, pars nervosa (neurohypophysis)
The optic nerve
In the territory of the prosencephalon that will become the diencephalon (priorly), we have the formation of 2 optic vesicles that will elongate and enter the orbital cavity, and there undergo changes to form the retina, etc. But they will remain connected to the diencephalon via a system of axons called the optic nerve
Hypophysis –
Rathke’s pouch, ectodermal diverticulum of the stomodeum + hypothalamus
Its development is very complex — requires contribution of 2 components —
The adenohypophysis — develops from the Rathke’s pouch
A diverticulum of the stomodeum (primitive mouth)
The neurohypophysis from the infundibulum (hypothalamus?? — why was it written before)** (i think bc hypothalamus stimulates/inhibits hypophysis)
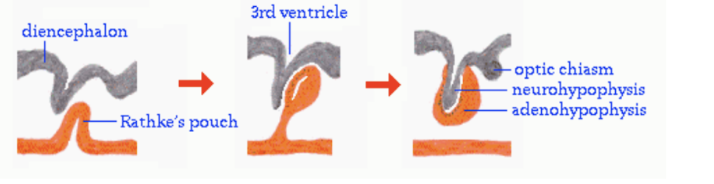
Craniopharyngioma
Congenital cystic tumor from Rathke’s pouch
Leads to problem in the visual field, Hypothalmic problems (ex. obesity), Endocrine problems, and Increased intracranial pressure
Most common in children but also men & women in their 50s & 60s
Diencephalon giving rise to the optic vesicle & nerve — image
The telencephalic vesicles — expansion & proliferation
The telencephalic vesicles are sort of vaults, with a roof & floor — they undergo a process of expansion & proliferation
The floor of the vesicle —
Heavy proliferation with limited/modest expansion (neurons remaining clustered) —
Causes a thickening of the wall, with adhesion to the lateral wall of the diencephalon (blue arrow) and the formation of the basal (or ganglionic) eminence, which will give rise to the deep nuclei of the telencephalon
The vault of the vesicle —
Proliferates and undergoes a large expansion, causing the 2 telencephalic vesicle to bend on themselves and envelop the diencephalon. This proliferation will form the cerebral cortex -
Divided into — archicortex & paleocortex, allocortex, neocortex (most proliferated in humans), isocortex
Median walls of the vault —
Thin, with the formation of the tela choroidea & choroid plexuses of the lateral ventricles
Olfactory bulbs —
Form from the 2 telencephalic vesicles & connect to the olfactory (I) nerve
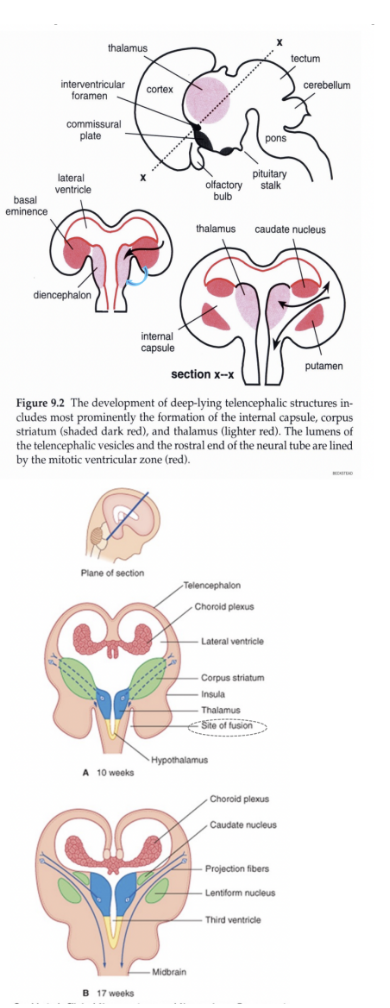
What occurs due to telencephalic vesicle proliferation & expansion
The medial wall of the telecephalic vesicles adhere with the lateral wall of the diencephalic vesicles —
Meaning that in the same section there will be presence of both dien & telencephalon
At the same time, the neurons of the forming cerebral cortex begins to produce axons, which will extend towards the thalamus, spinal cord, etc.. On this side,, the neurons forming in the thalamus begin to project into the cerebral cortex
These 2 processes reaching each other will cause a division of the basal eminence or ganglionic eminence into 2 compartments —
1 will remain medial to the bundle of axons (internal capsule) and the other one remains lateral to them
The bundle of axons (extending from the cerebral cortex) will form a very important system of white matter called the internal capsule
The internal capsule
A very important system of white matter formed from the bundle of axons extending from the cerebral cortex.
It is formed by the axons descending from the cortex & ascending from the thalamus
During embryological development, this capsule splits the ganglionic eminence into a medial & lateral division —
The medial division will give rise to one of the neuclei of the brain, called caudate nucleus
The lateral division will give rise to the putamen
Chorioid plexuses forming in the lateral ventricles (image)
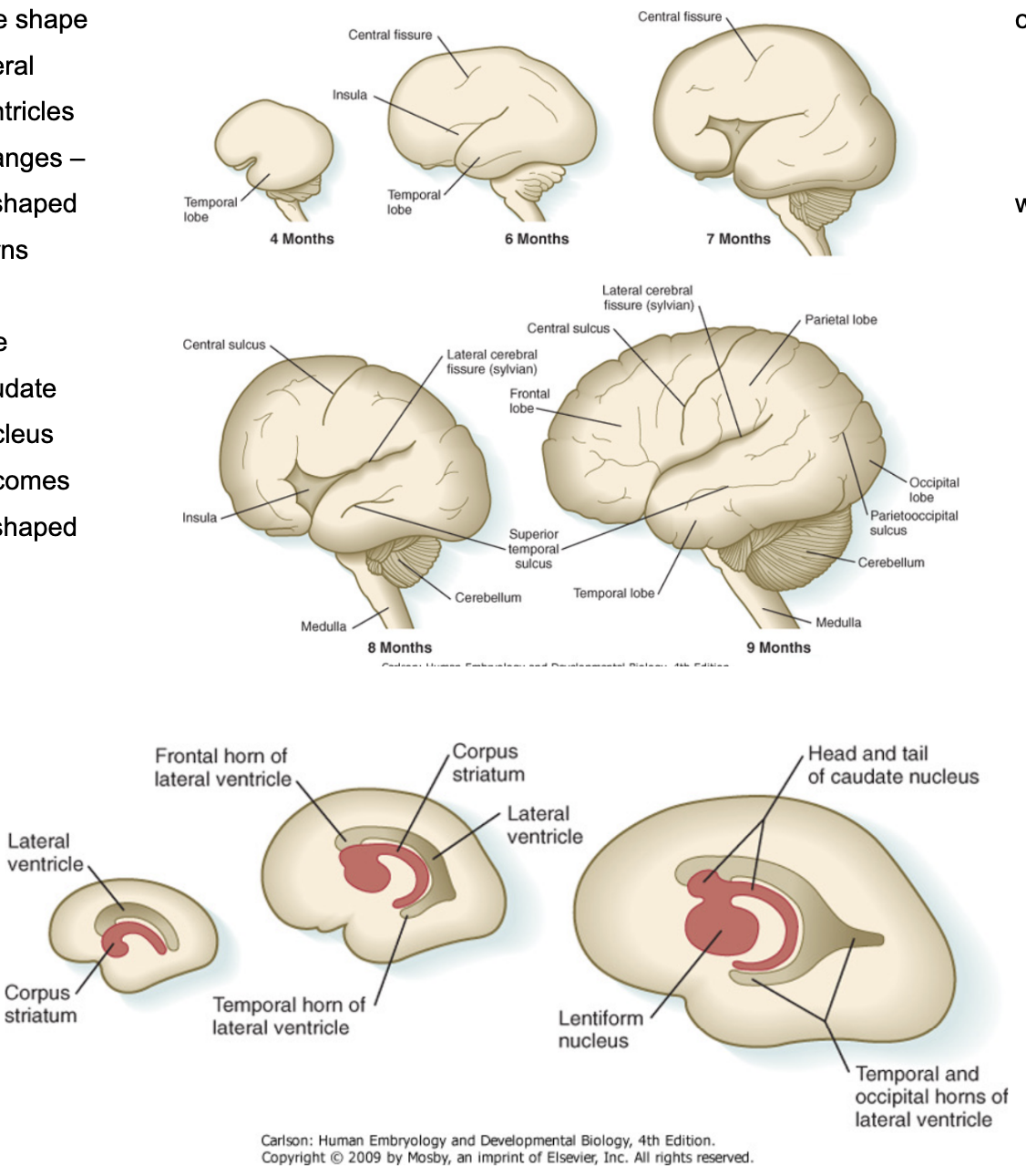
Cerebral lobes — expansion of the vesicles
At 6th month, the cortex begins to bend on itself, and sulci (grooves, fissures) and gyri (convolutions) begin to appear
Sulci separate the brain into lobes —
First fissure — central fissure of Rolando (6th month, separates frontal & parietal)
Then, lateral fissure of Silvius (separates temporal, frontal & parietal)
Cerebral lobes —
Parietal lobe (below parietal bone), the occipital lobe (relation with squamous portion of occipital bone), and temporal lobe (below temporal bone)
Insula/hidden lobe —
Lobe covered by portions of parietal, frontal & temporal lobes — to find in adult brain we must divaricate the lateral fissure
Forms because that portion of the telecephalic vesicle doesn’t expand much due to its proximity to the feveloping ganglionic eminence, thus stuck in that position as the cortex of the other lobes grows over it.
Portions of other lobes covering insula are called — operculum
The telencephalic vesicles acquire a C-shape appearance, along with their lumens and part of the ganglionic eminence that will give rise to the caudate nucleus (so also that will be C-shaped)
This change in shape of the lateral ventricles forms 3 horns —
Frontal, temporal, and occipital horns
And the caudate nucleus is divided into —
Head, body, and tail
Hydranencephaly –
Congenital absence of cerebral hemispheres replaced by hugely dilated ventricles
Causes –
Infarction (stroke) due to occlusion of internal carotid arteries in uterus
Severe necrotizing encephalitis in uterus from Toxoplasma, Rubella, Cytomegalovirus, or Herpesvirus (TORCH)
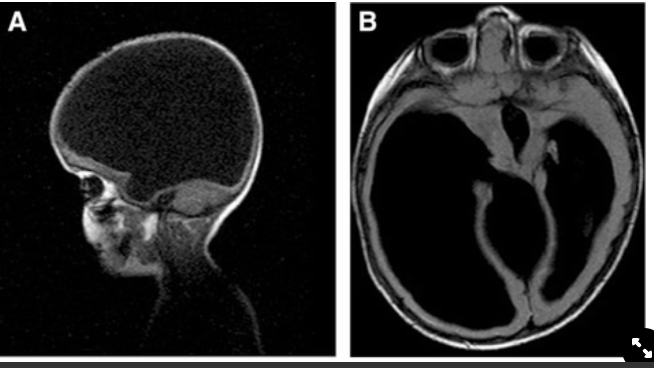
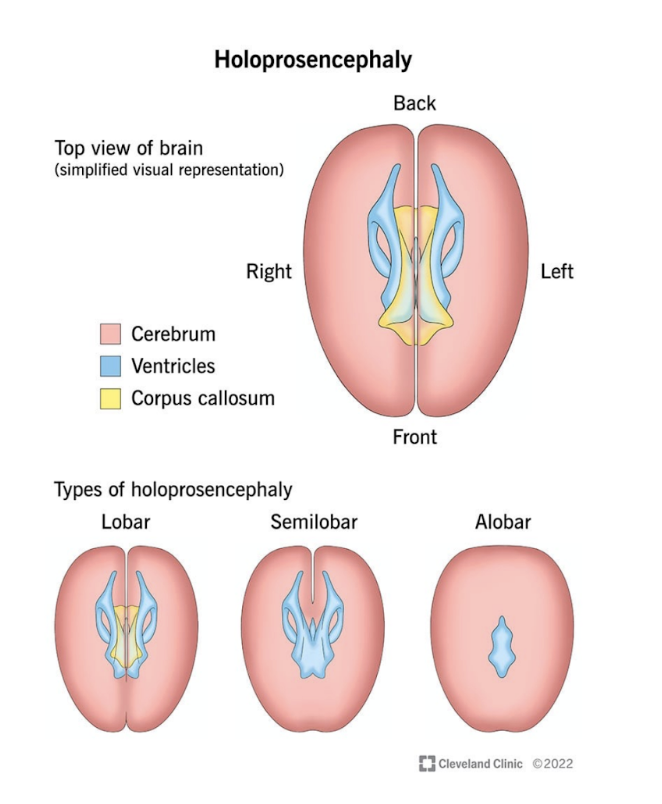
Holoprosencephaly
A disorder caused by the failure of the prosencephalon (embronic forebrain) to sufficiently divide into double lobes of the cerebral hemisphere — leading to a single-lobed braine structure with severe skull & facial defects
3 types —
Alobar
Where 2 hemispheres are completely fused
Semilobar —
Where there is frontal & parietal fusion
Lobal
Where there is only frontal fusion
Commissures
During CNS development, so do commissures — axonal connections between the left & right sides of the brain, which are crucial for bilateral integragion of lateralized sensory, motor, & associative functions
Throughout vertebrate species, forebrain commissures share a conserved development plan, a similar position relative to each other within the brain, and similar patterns of connectivity — thus due to this communication there is an evolution/phylogenesis
Commissures origination
Mostly originate from lamina terminalis
Situated at end of the neural tube in the region where we have the closure of the anterior neuropore (anterior territory)
From the lamina termminalis, we have the origin of —
Corpus callosum
Anterior commissure
Hippocampal commissure