Bio 2 - Urinary: Lectures 1 -
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
Roles of the kidney (8):
Regulate blood volume
Regulate BP
Modify plasma composition & volume
Maintain long-term blood pH
Regulate erythropoiesis
Involved in gluconeogenesis
Detoxify blood & excretes wastes
Converts vitamin D into its active form
Urethral sphincters (2)
Internal
Involuntary control of urine flowing from the bladder into the urethra
Smooth muscle
External
Voluntary control over the initiation and cessation of urination
Skeletal muscle
What muscles contract during urination to expel urine from the bladder?
Detrusor muscles
Anatomy of the kidney - VISUAL
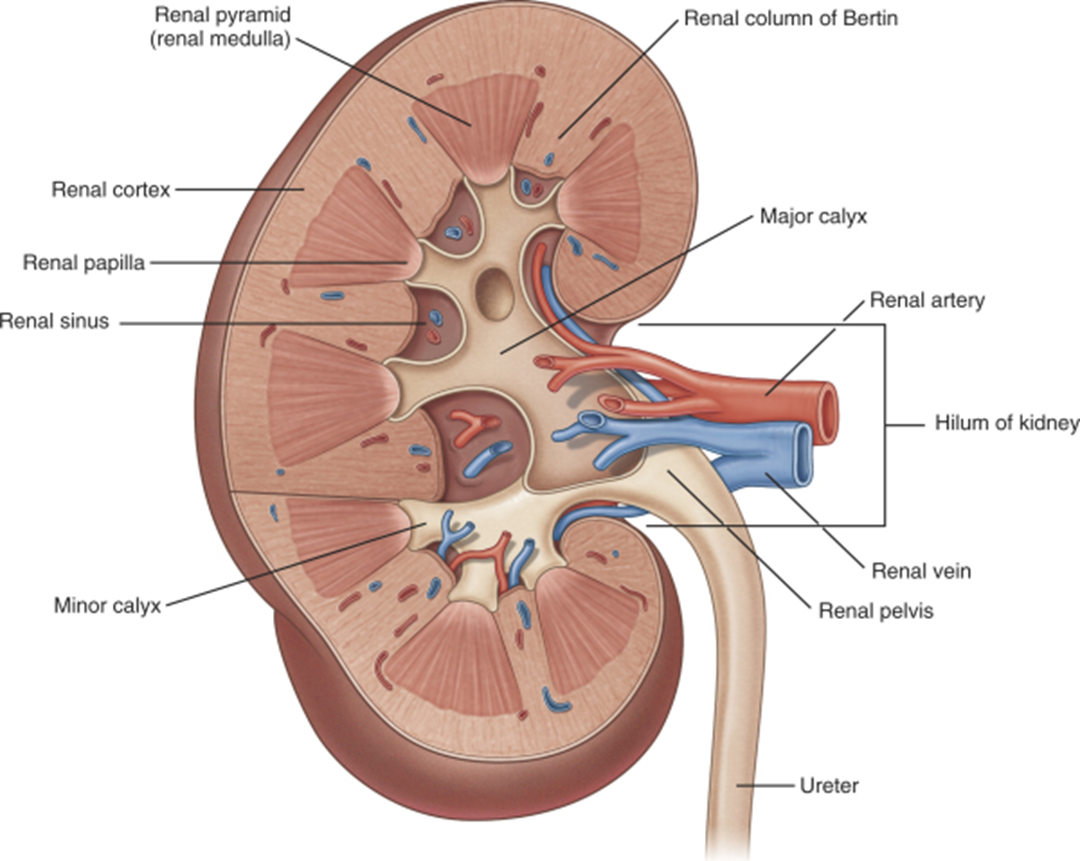
Blood flow to and from kidneys
Aorta
Renal artery
Afferent arteriole
Glomerulus (capillaries)
Efferent arteriole
Peritubular capillaries and vasa recta
Renal vein
Inferior vena cava
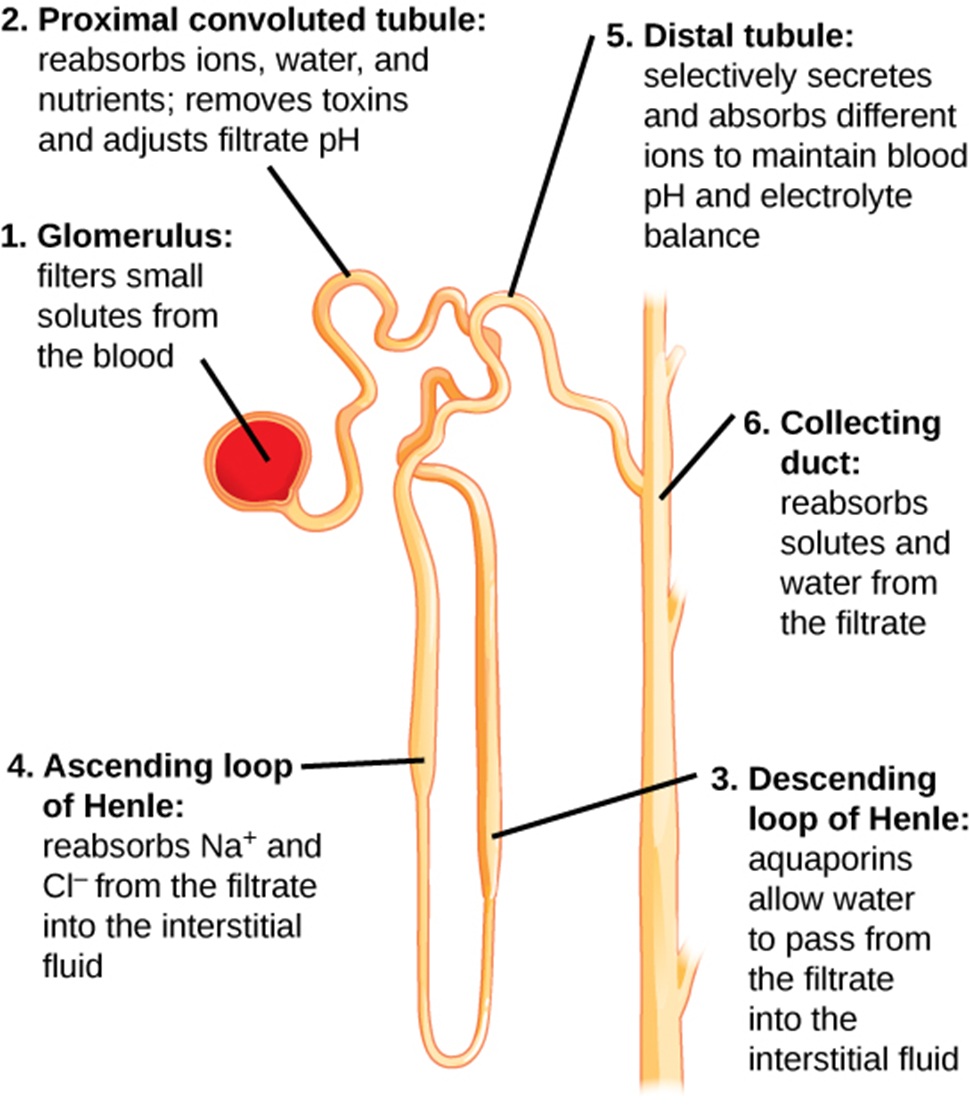
Nephrons
Functional and structural units of the kidney responsible for forming urine
> 1 million nephrons/kidney
Consists of: renal corpuscle & renal tubule
Renal corpuscle
It’s where blood plasma is filtered
Composed of glomerulus (fenestrated capillary network) & glomerular capsule
Renal tubule
The glomerular filtrate, filtered fluid, passes through here from which: 1. tubular reabsorption (lots of water & solutes are reabsorbed into the blood) and/or 2. tubular secretion (some water & solutes are added to the filtrate) occurs
Composed of: proximal convoluted tubule (PCT), loop of Henle, distal convoluted tubule (DCT)
Process of nephron - VISUAL
3 steps of urine formation:
Filtration
Reabsorption
Secretion
Glomerular Filtration - step 1
G Filtration is a passive process from which blood plasma fluids — water, glucose, amino acids, ions, nitrogenous wastes, etc. —- (NOT proteins!) are forced out of the glomerular capillaries into the Bowman’s capsule due to the hydrostatic pressure. Fluid captured by the glomerular capsule is called filtrate.
*The afferent arteriole is larger in diameter than the efferent arteriole
Glomerular filtration pressures (3):
Outward force:
Glomerular Capillary Hydrostatic Pressure (HPgc) = the BP in the glomerulus and promotes filtration
Apposing (inward) forces:
Blood Colloid Osmotic Pressure (OPgc)
Capsular Hydrostatic Pressure (HPc)
Net filtration pressure formula
NFP = HPgc – (HPcs + OPgc)
Outward forces - Inward forces
approx. 10 mm Hg
Glomerular Filtration Rate (GFR)
The volume of filtrate produced by the combined activity of all glomeruli in the kidneys each minute.
Directly proportional to:
NFP - Main controlling factor & is modified by altering the diameter of the afferent arterioles leading into glomeruli
Total surface area available for filtration
Filtration membrane permeability
Must be tightly regulated as it is essential for the kidneys to produce urine and also for the body to maintain BP
+ GFR —> + Urine output —> - Blood volume —> - BP and vice versa
Factors affecting GFR (3):
Changes in:
HPgc (e.g. hyper- or hypotension)
HPc from blockages in the nephron tubules or excretory system (i.e. renal pelvis, ureter, etc.) (e.g. a tumour or kidney stone)
OPgc from +/- plasma protein content in the blood (e.g. liver disease)
Which body system is very closely linked to the urinary system?
The cardiovascular system
Being that the kidneys and the CV system are so interlinked, many renal pathologies will tend to affect the CV system (e.g. hypo/hypertension), and vice-versa
Hyperfiltration (GFR too high)
Chronic hypertension can damage the filtration membrane and eventually lead to kidney failure
Homeostasis = 60-120mL/min (normal range)
Hypofiltration (GFR too low)
Plasma waste solutes accumulate over time and create a toxic environment for the body, as is the case during kidney disease/failure
Homeostasis = 60-120mL/min (normal range)
Tubular Reabsorption - step 2
T Reabsorption is a reclamation process where many of the useful substances that are present in the filtrate is reclaimed by the body (water, glucose, amino acids, needed ions), back into the blood within the peritubular capillaries. This process occurs throughout the renal tubule but the cells in the proximal convoluted tubule (first section) are the most active reabsorbers.
If no tubular reabsorption?
All of body’s plasma would be drained away as urine within 1hr
Tubular Reabsorption methods/pathways:
Transcellular route:
Osmosis - water reabsorption through open aquaporins channels
Simple diffusion - lipid soluble solutes
Primary/secondary active transport - glucose, amino acids, some ions and vitamins (water soluble solutes)
Paracellular route: Some other molecules pass between the cells lining the tubule (urea, various ions)
Transport Maximum
It refers to the solute’s rate of reabsorption is dependent on the number of protein carriers in the membrane.
Low solute concentration = ALL is reabsorbed
But
Solute concent. exceeding the number of available carriers = Transporters become saturated and excess is secreted in urine
Desirable substances i.e. glucose have more protein carriers, not desirable = few to none
*This applies to solutes that are reabsorbed by secondary active transport. Lipid soluble solutes and those entering via para-cellular route are less restricted in their reabsorption
What does it mean when glucose is present in the urine (2)?
It’s abnormal and MAY indicate diabetes mellitus
Diabetic —> High concen. glucose in blood —> Saturated protein carriers in renal tubules = Incapable of reabsorbing all = Excreted in urine
It’s normal if the person consumed a lot of sugar
*Accurate urinalysis for diabetes will be from pt fasting before test
Reabsorption of Na+
What is the role of aldosterone in reabsorption and secretion?
Aldosterone is a hormone that stimulates the production of Na+/K+ ATPase pumps in the cells lining the distal tubules and collecting ducts of the kidney
Pumps —> transport Na+ ions out of the tubular fluid —> into the blood
Simultaneous
Pumps —> transport K+ ions from the blood —> into the tubular fluid
= Na+ in the blood increases from reabsorption, while K+ decreases for secretion