Pediatrics
1/144
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
145 Terms
what is sudden infant death syndrome (SIDS)?
sudden death of an infant younger than one year of age (<1 y/o), which remains unexplained
- after thorough case investigation, including the performance of a complete autopsy, exam of death scene, & review of clinical history
what is the leading cause of infant mortality between 1 month & 1 yr of age in the US?
SIDS
in the US, the incidence of SIDS has declined by >50% since the 80s, & the greatest reduction occurred after 1992. what caused this?
American Academy of Pediatrics (AAP) issued a recommendation to reduce the risk of SIDS by placing infants in a supine position for sleep
maternal risk factors for SIDS
- young age
- smoking during pregnancy
- late or no prenatal care
- drug use (including alcohol use)
- pregnancy complications (placenta previa, abruptio placenta [placental abruption], premature rupture of membranes)
- elevated maternal alpha fetoprotein (neural tube defect, down syndrome, more than 1 fetus)
infant & environmental risk factors for SIDS
- preterm birth &/or low birth weight
- prone sleep position
- sleeping on soft surface &/or w/ bedding accessories (loose blankets & pillows)
- bed sharing (sleeping in parents' bed)
- overheating
- sibling of SIDS victim
- twins
- exposure to cigarette smoke
what is the biggest protective factor against SIDS?
modifiable risk factors
factors that are somewhat protective against SIDS:
- room sharing w/o bed sharing
- breastfeeding
- pacifier use
- fan use
what is the pathogenesis of SIDS?
unknown
- most compelling hypothesis involves brainstem abnormality or maturational delay related to neuroregulation or cardiorespiratory control, combined w/ a trigger event (such as, airflow obstruction)
what can be done to prevent SIDS?
- infants should be placed supine (on their backs) for every sleep
- sleep on a firm surface designed specifically for infants w/o pillows, stuffed toys, crib bumper pads, blankets, loose bedding, excessive clothing, or sleep positioners
- NO bed sharing (although ROOM sharing is encouraged)
- mothers should avoid smoking, alcohol, illicit drug use & should obtain proper prenatal care
what is respiratory distress syndrome (RDS) (formerly known as hyaline membrane disease [HMD])?
caused primarily by a deficiency of pulmonary surfactant in an immature lung (premature infant)
in preparation for air-breathing, surfactant is expressed in the lung starting around the _______ week of gestation
20th
what does surfactant do?
reduces alveolar surface tension
- thereby facilitating alveolar expansion & reducing the likelihood of alveolar collapse from atelectasis (complete/partial collapse of the lung)
what is the most common cause of surfactant deficiency?
preterm delivery
- there are also genetic causes
incidence of RDS increases w/ ______________ GA
decreasing
1 multiple choice option
which infants are at the greatest risk for RDS, with an incidence of of 90%?
extremely preterm infants (GA
clinical manifestations of RDS:
present w/i the 1st mins to hrs after birth
- signs of respiratory distress
*tachypnea
*nasal flaring
*use accessory respiratory muscles
*expiratory grunting
*intercostal/subxiphoid/subcostal retractions
*cyanosis
- hypoxemia
what may a CXR show w/ RDS?
- air bronchograms (tubular outline of an airway made visible by filling of the surrounding alveoli by fluid or inflammatory process)
- diffuse bilateral atelectasis (causing ground glass appearance)
- doming of the diaphragm (causing low lung volumes)
what should be administered to all pregnant women at 22-34 wks gestation who are at increased risk of preterm delivery w/i the next 7 days?
antenatal corticosteroid (ACS) therapy
- betamethasone & dexamethasone (most widely used)
what does antenatal corticosteroid (ACS) therapy do?
it enhances maturational changes in the fetal lung w/ increased synthesis & release of surfactant
- resulting in improved neonatal lung function
what is recommended after delivery for tx of preterm infants w/ RDS?
NIPPV (CPAP)
- may require intubation/mechanical ventilation
_______________________ is recommended for pre-term infants in respiratory distress which should be given w/i 30-60 mins after delivery for optimal effect
exogenous surfactant
exogenous surfactant is recommended for pre-term infants in respiratory distress which should be given w/i _________________ after delivery for optimal effect
30-60 mins
how is the exogenous surfactant given to the infant (route)?
directly into lungs
what is foreign body aspiration (FBA)?
unintentional inhalation of foreign body into the airway
- most often in children < 3 y/o (but can occur in all ages, esp. older adults)
- aspiration may be gastric contents, inert material, toxic material or food
when should FBA be suspected?
in patients who have a sudden onset of lower respiratory sx (including asphyxia)
____________ may result from the aspiration of obstructing material
asphyxia
clinical manifestations of FBA:
- sudden onset of lower respiratory sx (including asphyxia)
- cyanosis
- loss of consciousness
- inability to cry or make much sound
- weak, ineffective cough
- soft or high pitched sounds while inhaling
- pneumonia, secondary to aspiration
what is one of the most common causes of acute respiratory distress syndrome (ARDS)?
acute gastric aspiration
how is FBA diagnosed?
clinically (based on sx/choking)
1. obtain plain CXR
- neck XR can also be obtained
- usually proceed to bronchoscopy
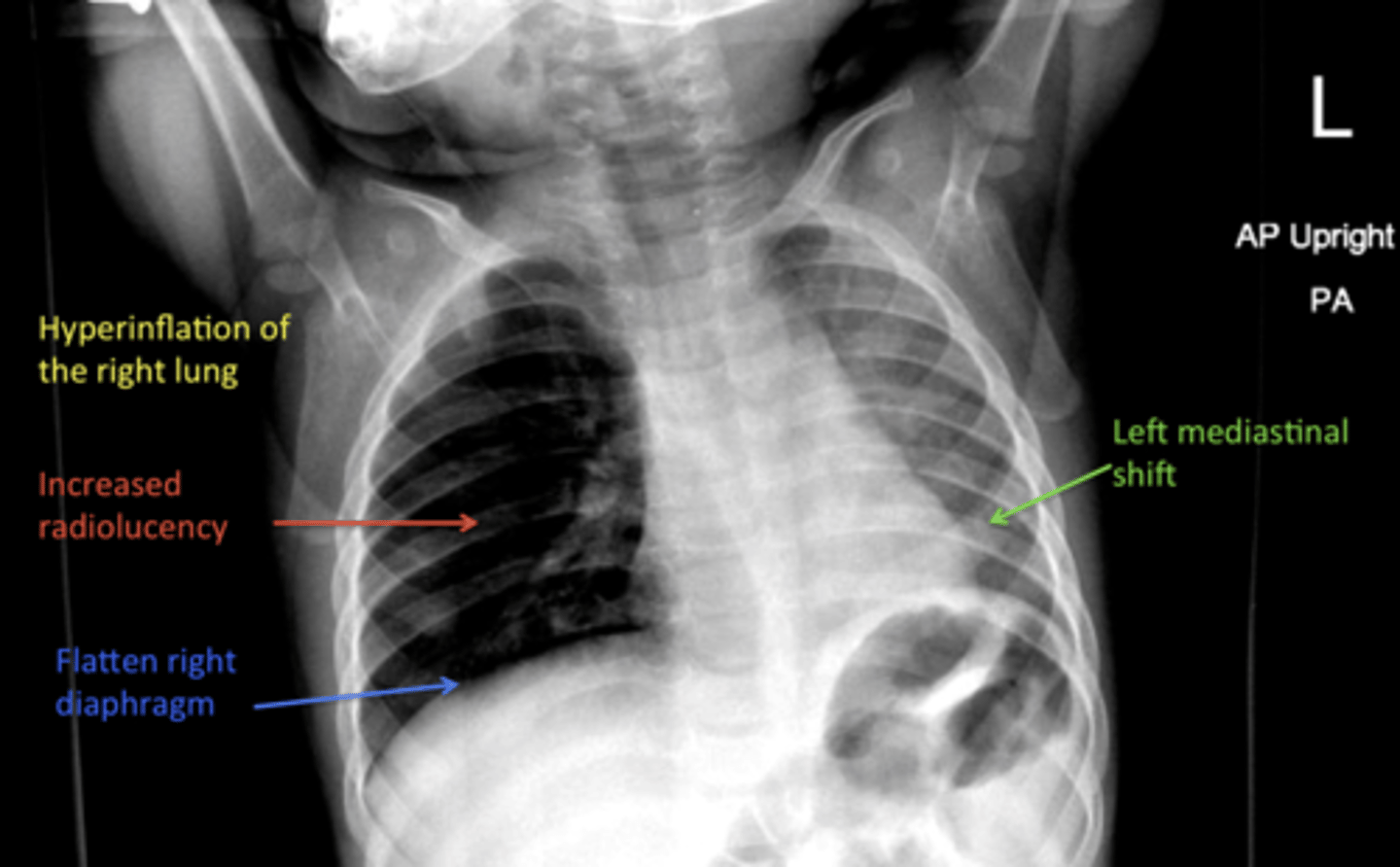
what are the most common radiographic findings on CXR w/ FBA?
- hyperinflated lung (caused by airway obstruction)
- atelectasis
- pneumonia (consolidated infiltrates)
- mediastinal shift
- the object & its location
w/ FBA, what is the hyperinflation of the lung caused by?
a check valve effect
- airways dilate during inhalation, permitting air to pass by a partial obstruction; however, airways constrict tightly around the obstruction during exhalation resulting in trapped air/hyperinflation
CXR is ________ in atleast 30% of FBA cases
normal
in FBA, why would you do a neck radiograph (PA/lateral view)?
to evaluate for a foreign body or signs of a foreign body (subglottic density or swelling)
in stable pts w/ a high clinical suspicion of FBA if the plain radiographs are inconclusive or normal, what should they proceed to?
bronchoscopy
- an endoscopic procedure that passes a probe w/ a camera into the trachea & proximal airways
are bronchoscopies diagnostic, therapeutic or both for FBA?
both
3 multiple choice options
what is the treatment for unstable patients w/ suspected FBA?
immediate BLS measures to relieve the obstruction
- including: heimlich maneuver or for an infant, back blows (between scapula) w/ chest thrusts
what is the treatment for stable patients w/ suspected FBA?
removal of the object ASAP w/ bronchoscopy
in a patient w/ FBA, what should be given for further tx if there's suspicion of bacterial pneumonia caused by aspiration?
antibiotics
in comparison to adults, where is the position of the larynx in infants & children?
higher & more anterior
as a result of the higher & more anterior larynx in infants & children, what may happen?
w/ resuscitation, hyperextension of the neck may worsen obstruction in the upper airway
why are the airways of children more susceptible to obstruction from edema, mucous plugs or foreign body?
bc their airways are smaller
what contributes to a tendency for the posterior pharynx to buckle during resuscitation in infants/children?
the larger occiput causes passive flexion of the cervical spine in the supine position
what is the occiput?
back of head or skull
what is a common cause of airway obstruction in the unresponsive child?
the tongue (which is relatively larger compared to the oral cavity in a child)
- it can fall back against the hypopharynx w/ a decreased level of consciousness
what is croup?
a respiratory illness characterized by inspiratory stridor, cough, & hoarseness which result from inflammation in the larynx & subglottic airway
- most commonly occurs in children 6 mo to 3 y/o
what is the hallmark symptom of croup among infants & young chilren?
barking cough
- hoarseness predominates in older children & adults
what is the anatomic hallmark of croup?
narrowing of the subglottic airway (the portion of the larynx immediately below the vocal folds)
- this is what causes the "barking cough"
other terms used to describe croup:
- laryngotracheitis
- laryngotracheobronchitis
what is the most common cause of croup (esp. in the fall & winter)?
parainfluenza virus type 1
parainfluenza type 2 sometimes causes croup outbreaks, usually with ________ disease than type 1
milder
1 multiple choice option
parainfluenza type 3 also causes sporadic cases of croup that often are _____ severe than those due to types 1 or 2.
more
1 multiple choice option
other viruses that can cause croup:
- RSV
- adenoviruses
- coronavirus
- measles
- influenza
- measles
- rhinoviruses
- enteroviruses
- metapneumoviruses
is croup always viral?
no, it can be bacterial
- mycoplasma pneumoniae has been associated w/ mild cases
- croup caused by viruses can also lead to a secondary bacterial infection
which bacteria has been associated w/ mild cases of croup?
mycoplasma pneumoniae
3 multiple choice options
s/s of croup:
usually begin w/ nasal discharge & congestion & progress over 12-48 hrs to include:
- fever (low grade)
- hoarseness
- barking cough (seal like)
- inspiratory stridor
- tachypnea w/ a prolonged inspiratory phase
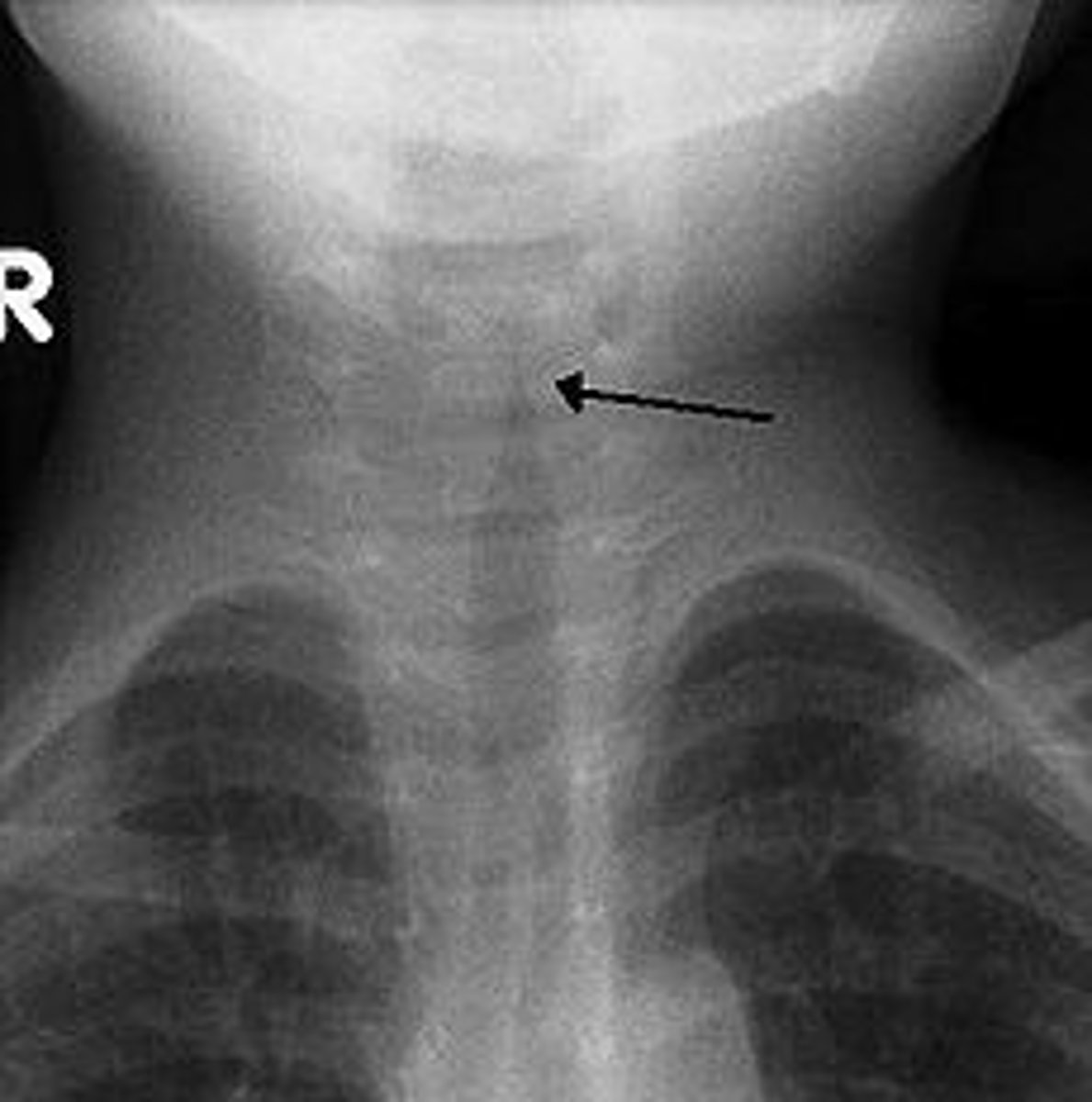
how is croup diagnosed?
clinically
- imaging not required but XR can show subglottic narrowing, commonly called the "steeple sign"
what radiographic finding is diagnostic for croup?
"steeple sign"
- subglottic airway narrowing at the cricoid cartilage
how is mild croup treated?
can be managed at home w/ the option of giving a single dose of glucocorticoids (dexamethasone or prednisolone)
moderate/severe croup =
stridor at rest &/or other signs of respiratory distress, such as:
- retractions
- tachypnea
- accessory muscle use
mild croup =
no stridor at rest & no respiratory distress
how is moderate/severe croup treated?
nebulized epinephrine (racemic epinephrine)
+ a single dose of glucocorticoid (dexamethasone)
patients w/ croup should also be given supportive care. what can this include?
- humidified air
- antipyretics
- encouragement of fluid intake
what is pertussis?
"whooping cough"
- very contagious
- spread by respiratory droplets
which bacteria causes pertussis?
bordatella pertussis
- gram negative (-) coccobacillus
which vaccines given in the US help prevent pertussis?
- DTaP (children < 7 y/o)
- Tdap (> 7 y/o)
can pertussis still occur in fully vaccinated people?
YES
- but the infection is usually less serious
what are the 3 stages of classic pertussis?
- catarrhal
- paroxysmal
- convalescent
catarrhal stage of pertussis
appears similar to viral URI w/ mild cough & coryza
- fever is uncommon but may be low grade
- cough gradually increases (instead of improving like it would in a typical viral URI)
the cararrhal stage generally lasts ____________
1-2 wks
which stage of pertussis is the most infectious?
catarrhal
paroxysmal stage of pertussis
coughing spells increase in severity
- during episodes, child may gag, develop cyanosis, & appear to be struggling to breathe
- "whoop" is noise made by forced inspiratory effort that follows coughing attack
- posttussive vomiting
_______________________ is moderately sensitive & specific for pertussis in children
posttussive vomiting
the paroxysmal stage may last ____________
2-8 wks
convalescent stage of pertussis
cough subsides over several weeks to months
- episodic coughing may recur or worsen w/ interval URI
older children/adults w/ pertussis generally present w/ _______ disease
milder
1 multiple choice option
any cough persisting for __________ w/ no other cause should be questioned for pertussis
> 2 wks
how is pertussis diagnosed?
clinically
- nonspecific lab finding of leukocytosis resulting from lymphocytosis (although WBC count can be normal)
- CXR not helpful (can be normal or show peribronchial cuffing, perihilar infiltrates, or atelectasis)
according to the CDC case definition, probable pertussis can be diagnosed w/o lab testing in pts w/o a more likely diagnosis who have either of the following:
- acute cough illness >/= 2 wks & atleast 1 of the following perussis-associated sx: paroxysms of coughing, inspiratory whoop, posttussive vomiting, apnea w/ or w/o cyanosis
- acute cough illness of any duration w/ atleast 1 of the above pertussis associated sx & contact w/ a lab confirmed case
although lab testing is not necessary to make the diagnosis of pertussis, why do we often perform it?
to confirm the diagnosis
- particularly when there is a need for contact prophylaxis
for confirmation of pertussis in pts w/ sx for < 4 months, what can be done?
PCR & culture (if available) of nasopharyngeal specimens
for confirmation of pertussis in pts w/ sx for > 4 months, what can be done?
PCR & culture (if available) of nasopharyngeal specimens
+ consider serology antibodies to pertussis toxin
recommend ____________________ for all pts w/ a clinical or microbiologic diagnosis of pertussis ASAP - do NOT wait for lab findings to confirm
antibiotic therapy
which abx can be used to treat pertussis?
macrolides (erythromycin, azithromycin, & clarithromycin)
- Bactrim is an alternative option for children > 2 mo who have a contraindication or cannot tolerate macrolides
**these same agents are used for postexposure prophylaxis
who should you recommend post-pertussis exposure prophylaxis to?
- all household & close contacts of the index case
- exposed individuals at high risk for severe or complicated infection (even if they're fully immunized)
what is antiobiotic treatment of pertussis focused on?
a. decreasing symptoms
b. decreasing transmission
b. decreasing transmission
1 multiple choice option
supportive care is essential in treating pertussis. what does this include?
- fluids
- nutrition
- mgmt of cough
- avoiding triggers that may worsen cough
what is diphtheria?
infectious disease caused by corynebacterium diphtheriae
how can corynebacterium diphtheriae cause myocarditis & neuropathy?
it has a propensity for mucous membranes, especially the respiratory tract & produces an endotoxin
diphtheria infection may lead to:
- respiratory disease
- cutaneous disease
- asymptomatic carrier state
what are the primary modes of spread of diphtheria?
close contact w/ infectious material from:
- respiratory secretions (direct or via airborne droplet)
or
- skin lesions
what is the most common form of diphtheria infection?
pharyngeal infection
clinical findings in diphtheria:
- tenacious gray membrane covering the tonsils & pharynx which bleeds w/ scraping
- sore throat
- fever
- malaise
- cervical lymphadenopathy
- low grade fever

what is cutaneous diphtheria characterized by?
chronic, nonhealing sores or shallow ulcers w/ a dirty gray membrane

how is diphtheria diagnosed?
clinically
- requires culture from respiratory tract secretions or cutaneous lesions & a positive toxin assay to confirm
what does treatment of respiratory diphtheria consist of?
antibiotic therapy & diphtheria antitoxin
abx of choice for diphtheria =
erythromycin or PCN
- alt: azithromycin or clarithromycin
_______________________ due to airway compromise is a major complication of diphtheria & is an important cause of mortality
respiratory failure
diphtheria contacts should be treated w/ ______________ to eradicate carries states
erythromycin
what is epiglottitis?
inflammation of the epiglottis & adjacent supraglottic structures
- w/o tx, can progress to life threatening airway obstruction
infectious epiglottitis is a ____________ of the epiglottis & other adjacent tissues
cellulitis