Bloodstream Infections Clinical Microbiology II
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
What are serious consequences of bloodstream infections?
Shock, multiple organ failure, disseminated intravascular coagulation (DIC), and death.
How many cases of bloodstream infections occur annually?
Approximately 200,000 cases.
What is the mortality rate for bloodstream infections?
20% to 50%.
What are some common bacteria isolated from bloodstream infections?
E. coli, CNS (coagulase-negative staphylococci), Klebsiella, S. aureus, Pseudomonas, Streptococcus viridans, Enterobacter, Enterococcus, Proteus, Bacteroides, beta-hemolytic streptococcus, Clostridium, S. pneumoniae.
What are the three types of bacteremia?
Transient, continuous, and intermittent.
What is transient bacteremia?
Bacteremia that occurs spontaneously or incidentally, such as from brushing teeth or chewing food, and surgery of non-sterile sites.
What is continuous bacteremia?
Bacteremia associated with septic shock or bacterial endocarditis, where organisms are released into the blood at a constant rate.
What is intermittent bacteremia?
Bacteremia seen in patients with un-drained abscesses.
What factors contribute to blood infections?
Immunosuppressive agents, widespread antibiotic use that suppresses normal flora, emergence of resistant strains of bacteria, invasive procedures bringing bacteria into the host, extensive surgeries, and seriously ill individuals.
What are the two types of blood infections?
Intravascular and extravascular.
What are intravascular infections?
Infections that originate within the cardiovascular system and cause continuous bacteremia.
What are extravascular infections?
Result from bacteria entering blood through
lymphatic system
What are some serious conditions caused by intravascular infections?
Infective endocarditis, mycotic aneurysm, suppurative thrombophlebitis, IV catheter-associated bacteremia.
What agents are commonly associated with IV catheter-associated bacteremia?
S. epidermidis, other CNS, S. aureus, Enterobacteriaceae, Pseudomonas aeruginosa, Candida spp., Corynebacterium spp., other Gram-negative rods.
What is infective endocarditis?
An infection of the endocardium where bacteria stick to damaged surfaces (Cardiac abnormalities damage cardiac endothelium), primarily caused by viridans Streptococci - S. anginosus, S. sanguis, S. mutans (normal inhabitants of oral cavity). Can also be caused by IV catheters, lines, prostheses with skin inhabitants S. epidermidis and S. aureus.
What are common portals of entry for extravascular infections?
Genitourinary tract (25%), respiratory tract (20%), abscesses (10%), surgical wound infections (5%), biliary tract (5%).
What organisms are associated with extravascular blood infections?
Haemophilus influenzae type b, Streptococcus pneumoniae, Neisseria meningitidis, Brucella spp., Salmonella typhi, Listeria.
What is septicemia?
When bacteria or bacterial products are causing harm
What are the clinical manifestations of septicemia?
Fever, hypothermia, chills, hyperventilation, respiratory alkalosis, skin lesions, change in mental status, diarrhea, hypotension, shock, DIC, and major organ failure.
What is septic shock?
A severe condition characterized by fever, acute respiratory distress, shock, renal failure, intravascular coagulation, and tissue destruction, often associated with endotoxin release from Gram-negative rods.
What does blood culture media do?
It is an enrichment broth, so it encourages the growth of one organism.
What blood culture systems are commonly used in medical laboratories?
BACTEC and BACT-Alert
What is the recommended blood culture volume for adults?
10 to 20 ml per culture.
How does specimen volume affect detection of bacteria in blood cultures?
Yield increases by 3.2% for each additional ml of blood.
What is the specimen volume requirement for blood culture in children?
Only 1-5 ml can be drawn. There are special pediatric blood culture bottles.
What is the age-volume protocol for blood cultures in children?
1 mL of blood for each year of life for those younger than 10 years; 20 mL for those 10 years and older; less than 10 mL (preferably between 10-20 mL) for those 10 years or older WITH poor veins.
How many blood cultures are sufficient to achieve optimum sensitivity?
Usually 2 to 3. In treated patients, three blood collections and an additional one on the second day detects most. 80% bacteremias are detected in the first set of blood cultures, 90% detected if two sets are taken, and 99% diagnosed if a third set is taken
What percent of blood cultures are positive in untreated patients with endocarditis?
90-95%
What percent of the first blood culture in bacteremic patients without endocarditis is positive?
80-92%
What anticoagulant is recommended for blood cultures?
Sodium polyethanol sulfonate (SPS) is preferred, as it is anti-complementary and antiphagocytic. SPS may inhibit some organisms, such as Neisseria, Gardnerella, Streptobacillus, and Peptostreptococcus, but the addition of 1.2% gelatin counteracts the inhibitory action
What anticoagulants are NOT recommended for blood cultures?
Heparin, EDTA, and citrate are not recommended because they inhibit some organisms.
What two types of culture bottles are used?
1 for aerobic recovery and 1 for anaerobic recovery
After how many hours of incubation are most organisms present in large enough numbers to recover?
After 6-18 hours. Then subculture can be performed.
How long are culture-negative bottles incubated for?
5-7 days
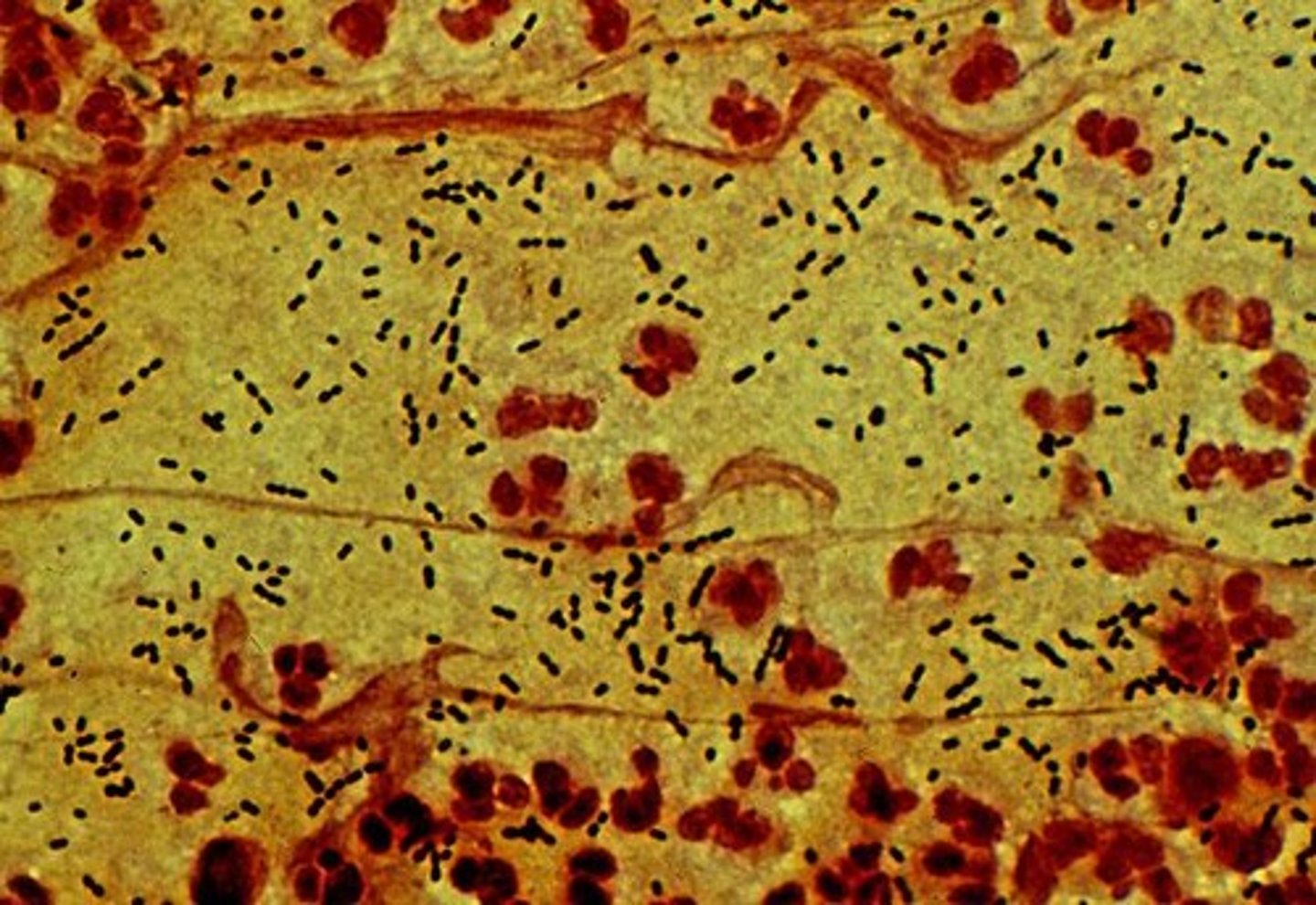
What is acridine orange staining?
A fluorochrome dye that stains gram-positive
and gram-negative bacteria, either alive or dead. It binds to nucleic acid of the cell and fluoresces
a bright orange.
What is acridine orange staining used for?
To locate bacteria in blood cultures and other specimens where finding bacteria is difficult.
What indicates a positive blood culture?
Growth indicated by hemolysis of RBCs, gas bubbles in medium, turbidity, or appearance of small aggregates.
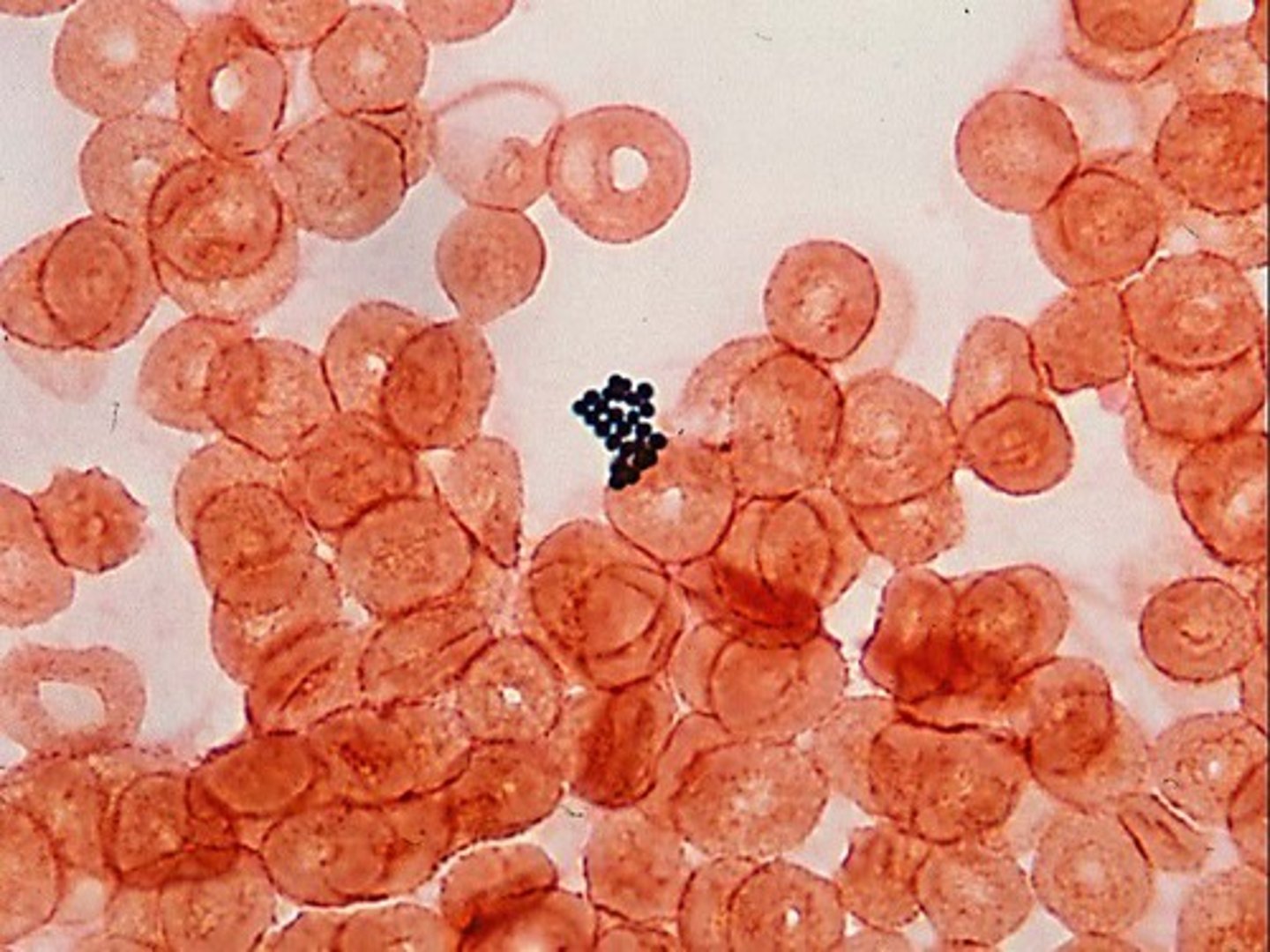
After a positive blood culture is indicated, what should be done?
Gram-stain an air-dried drop of medium, physician contacted when the morphologic description can be given. Subcultures are performed even if the organisms are not visualized microscopically
What are probable contaminants in blood cultures?
Growth of Bacillus spp., Corynebacterium spp., Propionibacterium acnes, or CNS in one of several cultures; Growth of multiple organisms from one of several cultures; Clinical presentation or course not consistent with sepsis; Organism causing infection at primary site not the same
What are probable pathogens in blood cultures?
Growth of the same organism in repeated cultures; Growth of certain organisms commonly seen in sepsis
What is the significance of immunocompromised patients in bloodstream infections?
They are at greatest risk for bacteremia and systemic complications.
What is a common cause of pneumonia in a patient who fell ill after eating unpasteurized goat cheese?
The most likely organism is Listeria.