Fractures & Ultrasound
1/68
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
69 Terms
What is the standard across healthcare for fracture evaluation?
The 7 Elements of Fracture Evaluation
What are the "7 Elements of Fracture Evaluation"?
1. Site and extent of fracture
2. Complete or incomplete
3. Relationship of fragments
4. Direction of fracture line
5. Special feature (impaction, avulsion)
6. Associated abnormalities (joint dislocations)
7. Special types (stress/pathological fractures)
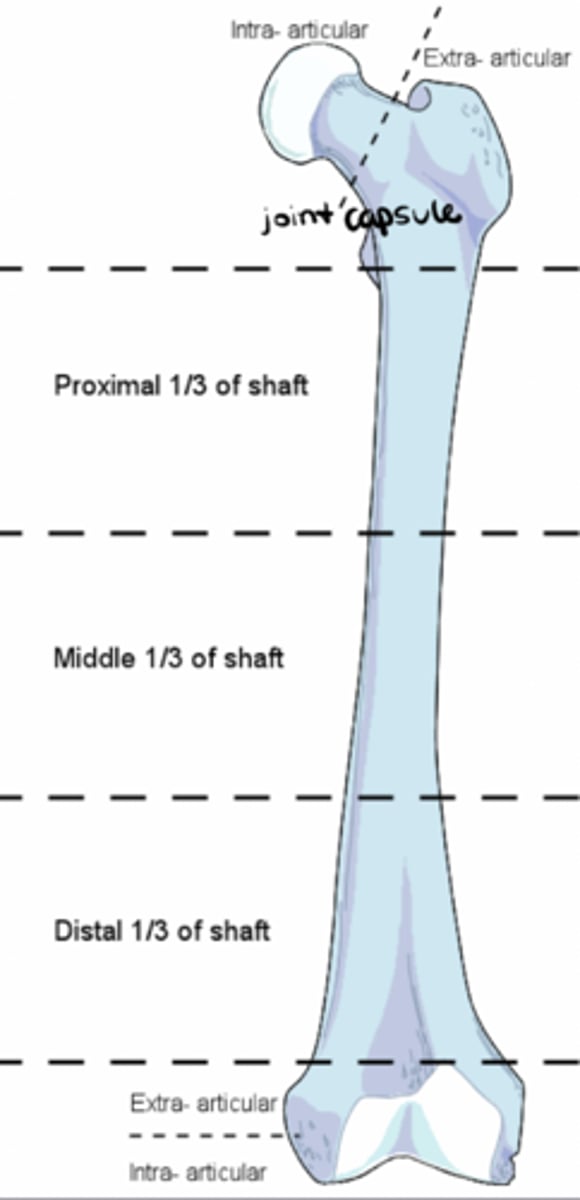
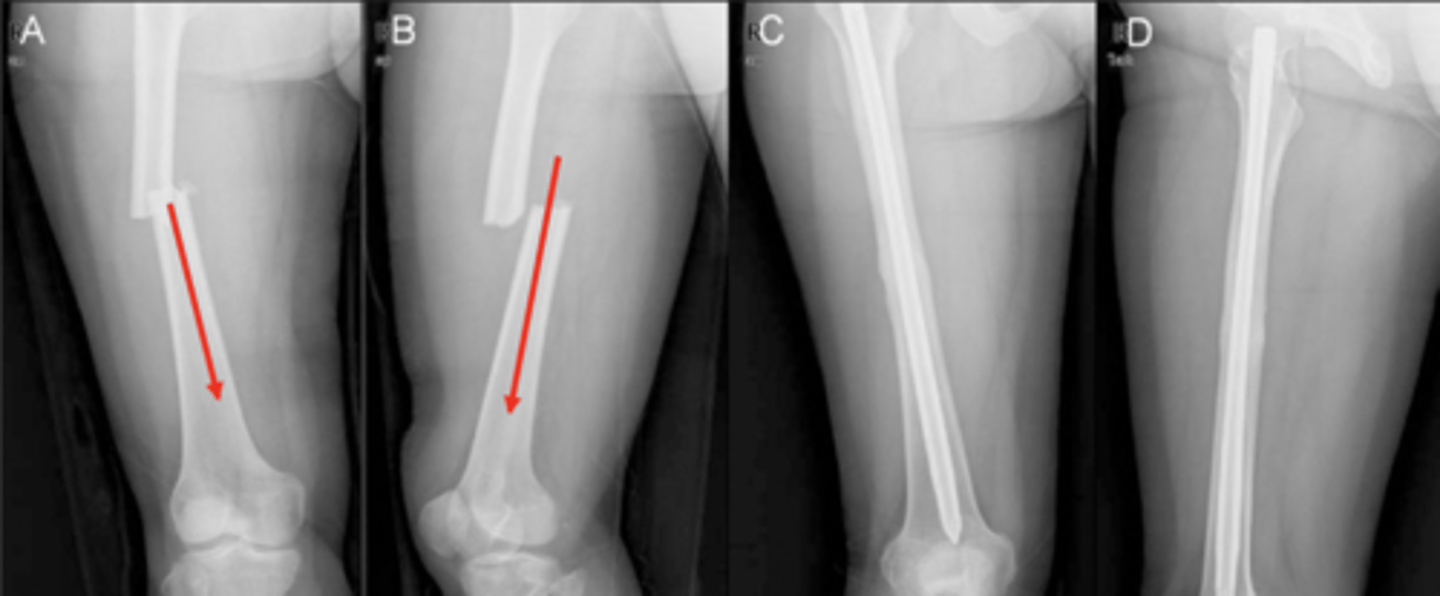
What is the site of fracture?
Thirds of bone (middle, proximal, distal); intra- vs. extra-articular
What is the extent of fracture?
Open vs. closed

What is a "complete" fracture?
All cortices of the bone have been broken

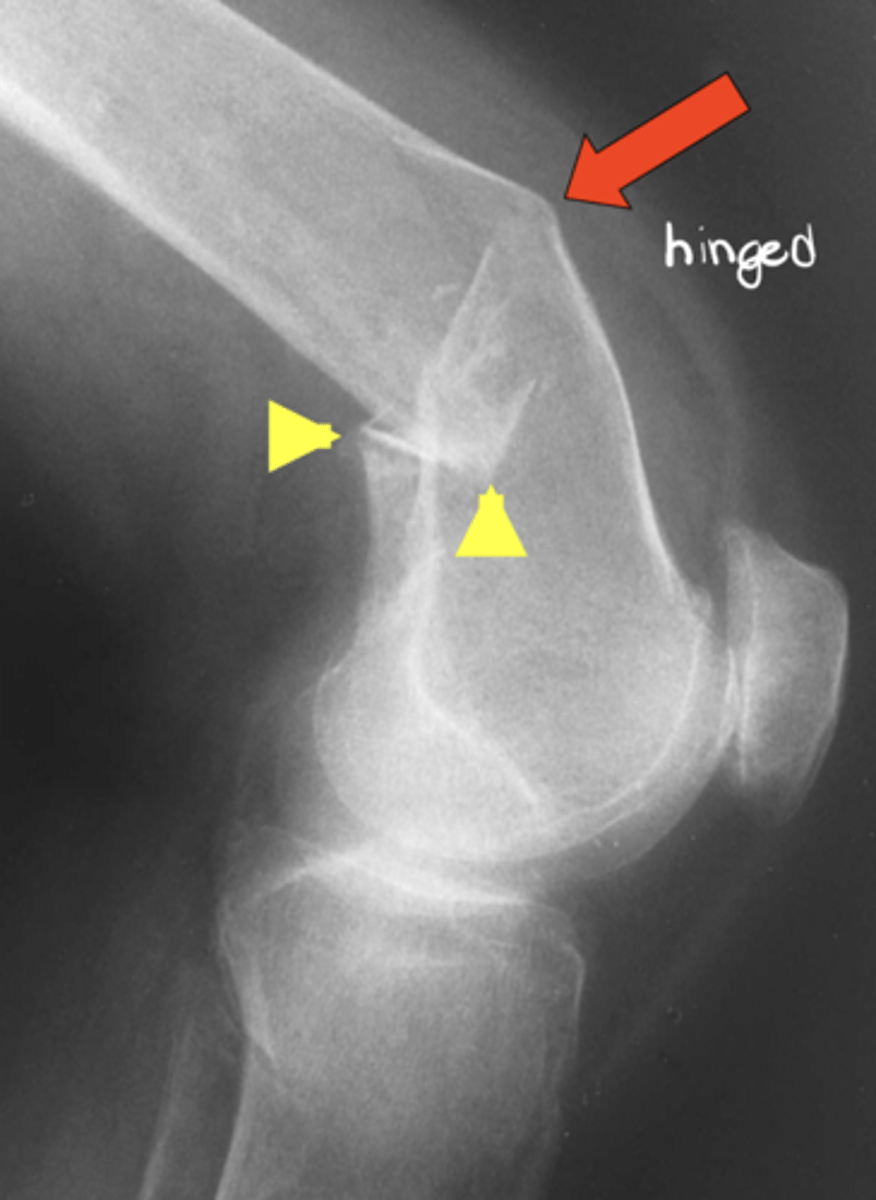
What is an "incomplete" fracture?
Fracture "hinges" on an unbroken cortex (e.g., "greenstick fracture" in immature bone)
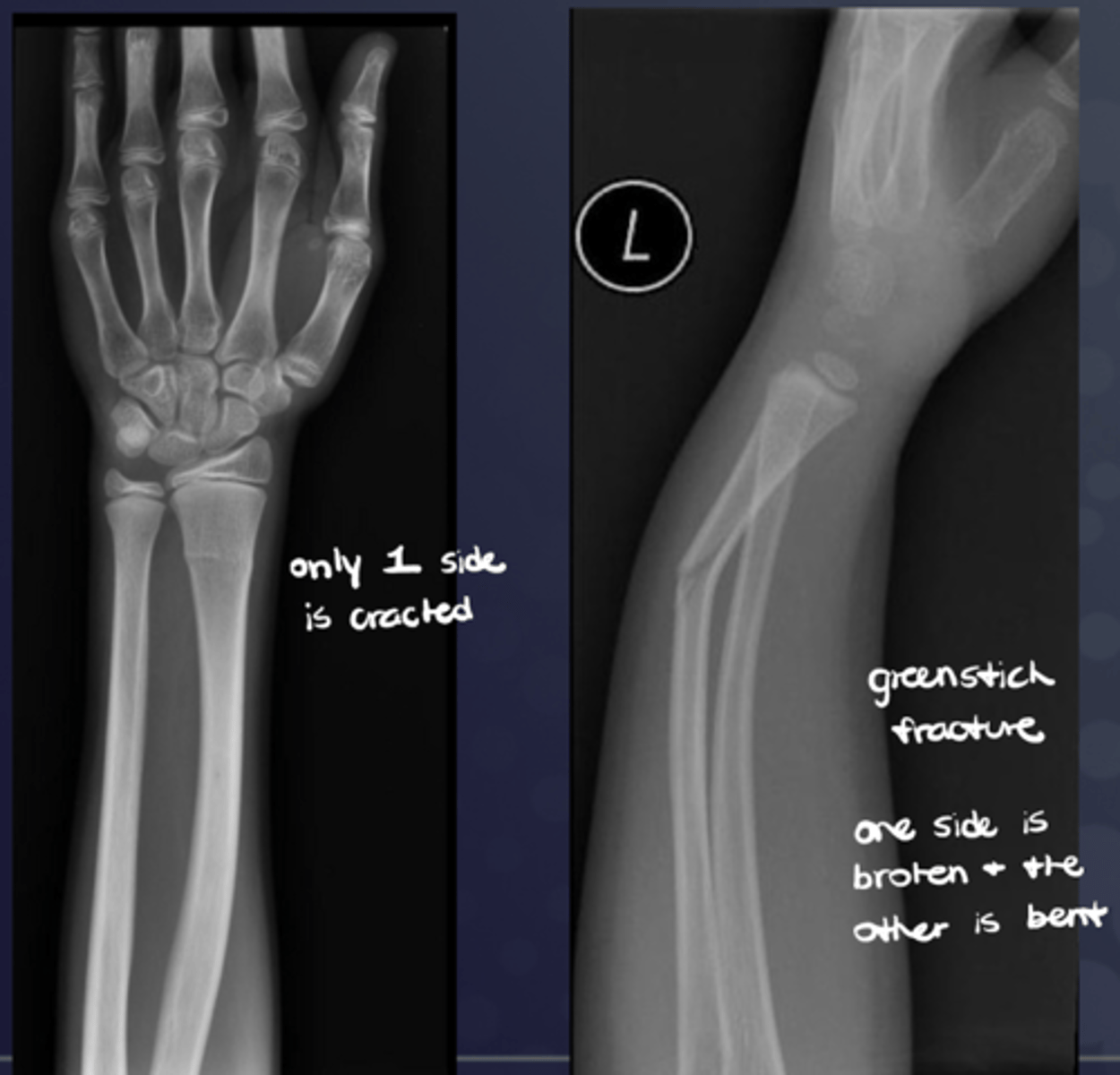
What is a "buckle" fracture?
Incomplete bone break where one side of the bone bulges or "buckles" under pressure, without the bone completely snapping in two, usually occurring in children due to their softer bones that bend more easily than adults' when force is applied
What is the position of fragments (under #3 "relationship of fragments")? What is an abnormality known as?
Degree of apposition at osseous ends; abnormality = displacement
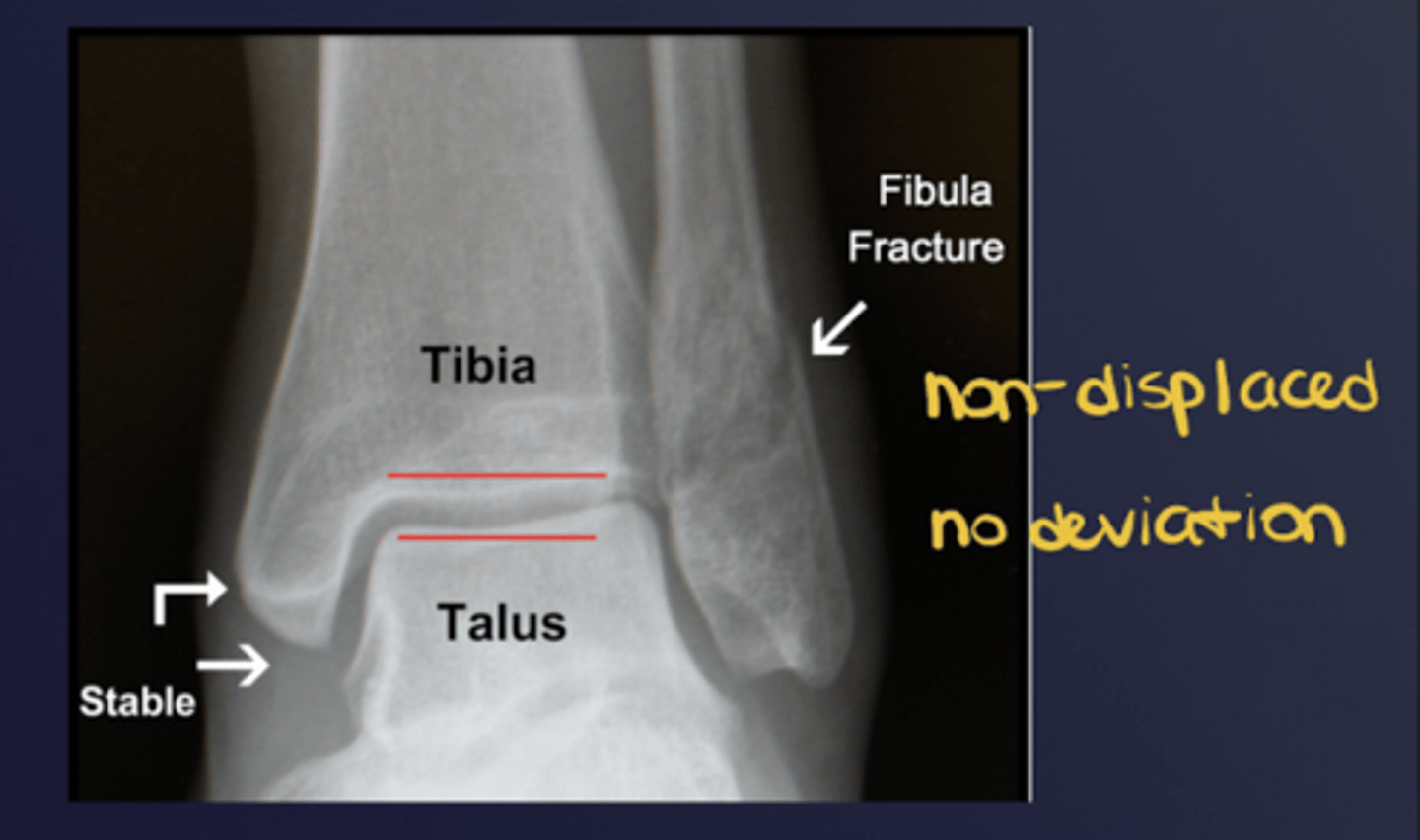
What is the alignment of fragments (under #3 "relationship of fragments)? What is an abnormality known as?
Angular relationship; one fragment to another; abnormality = deviation

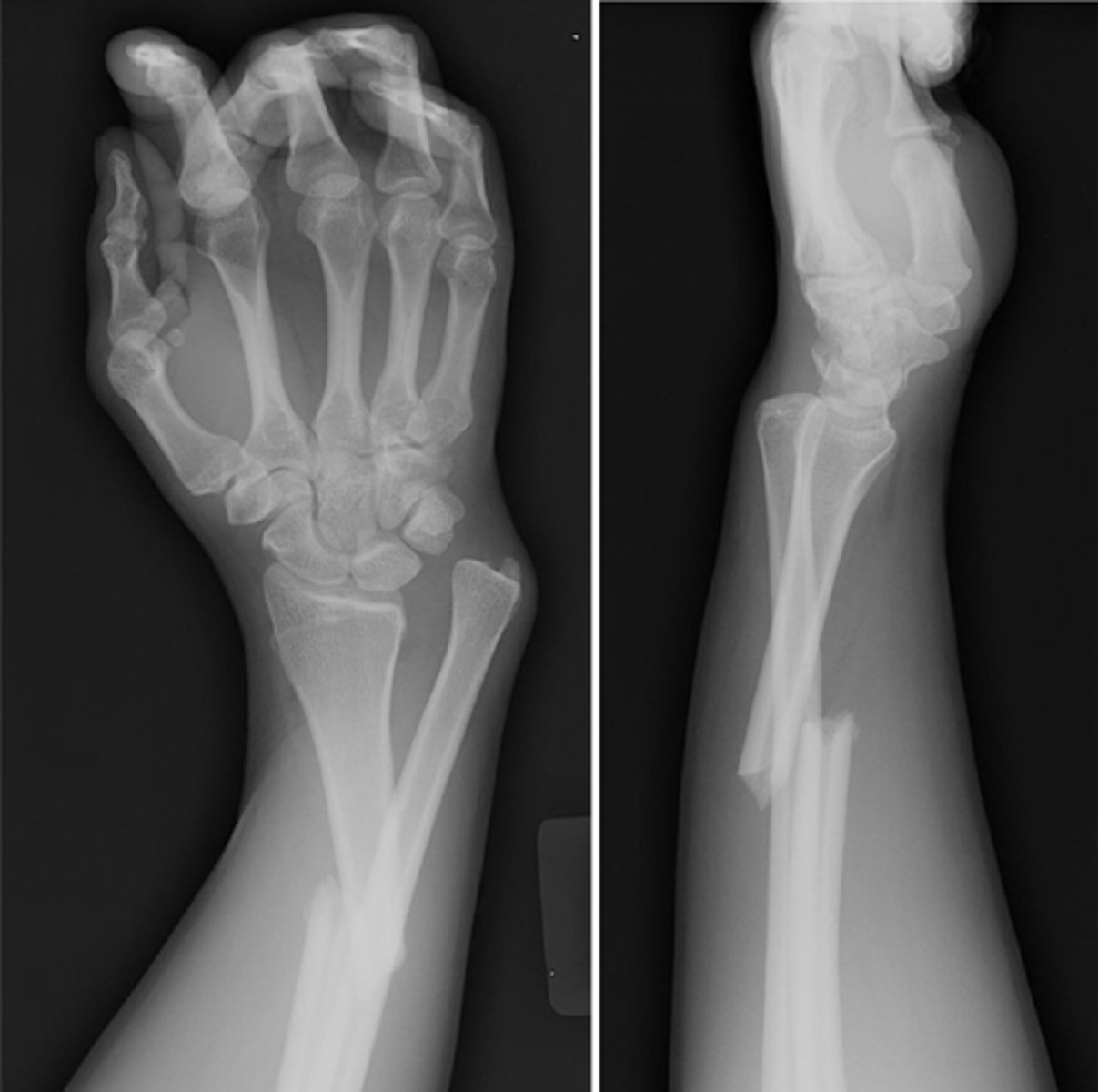
What does good position, good alignment look like vs. displaced with deviated alignment?
See image.
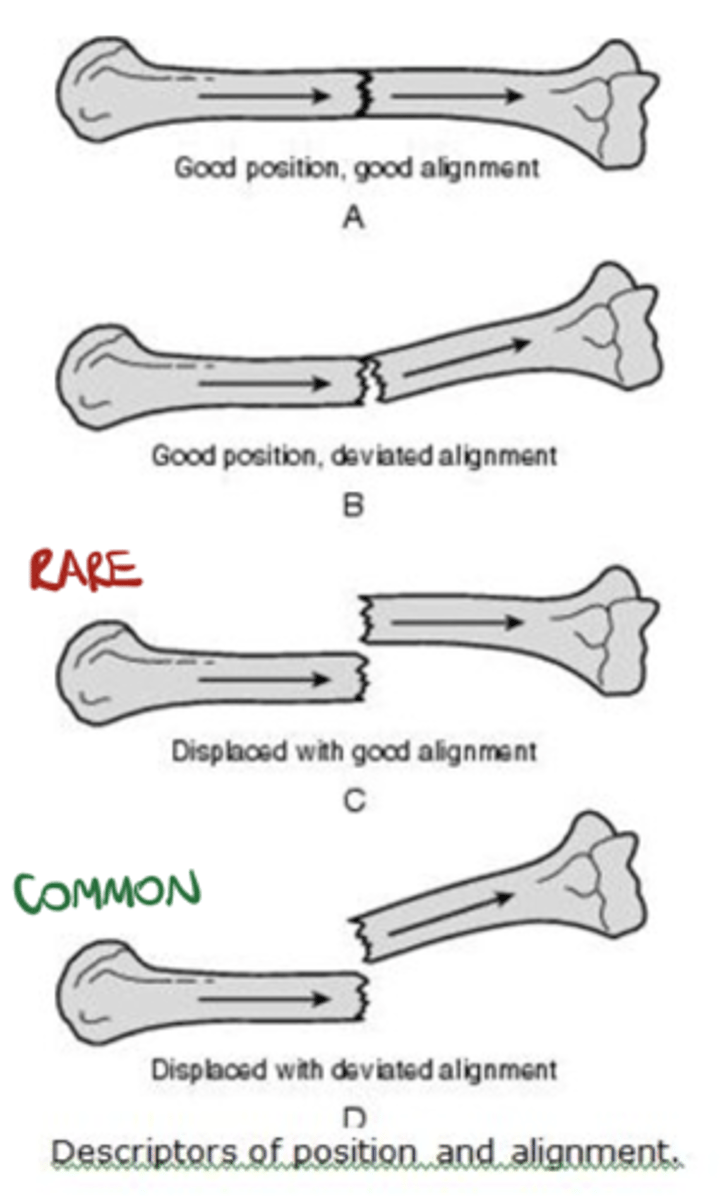
Name displacement based on the ________ fracture end in anatomical position
DISTAL!! -- i.e., "displaced medial, posterior, and overriding"
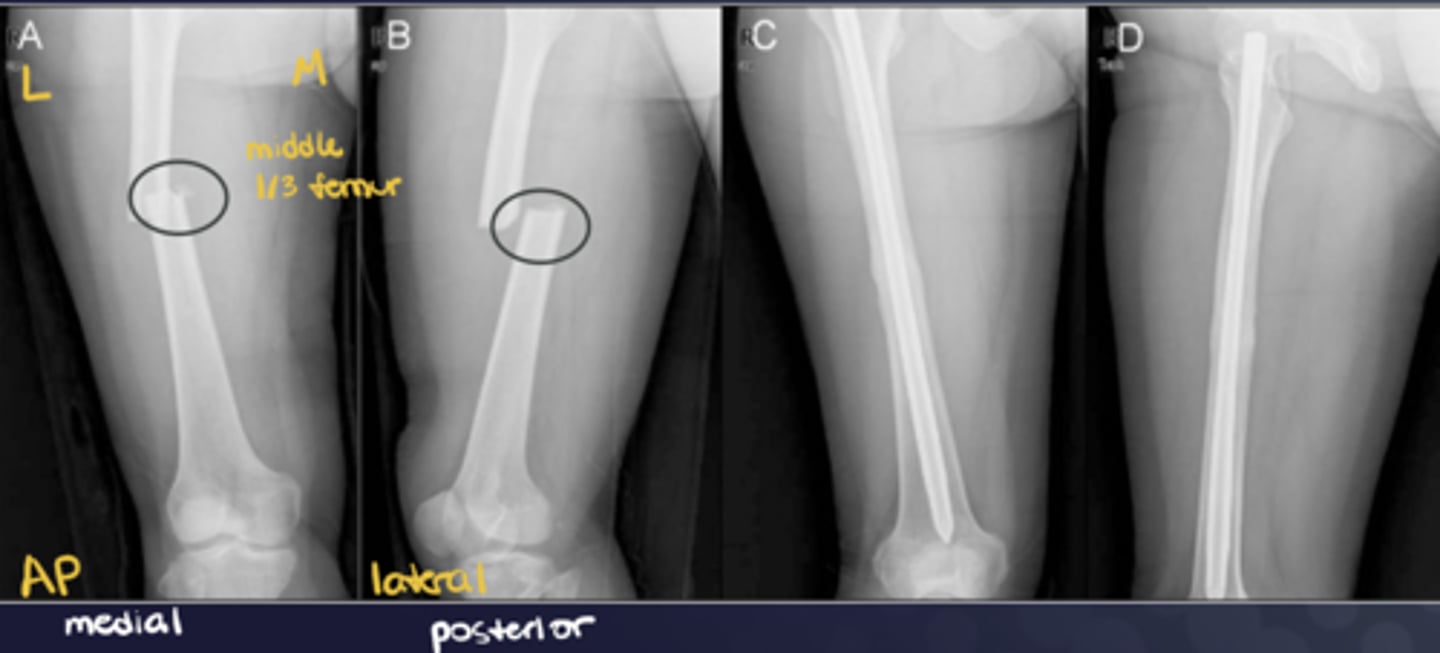
Name deviation based on the ________ bone angle in the ________ direction
DISTAL!! -- i.e., "deviated medial and anterior"
Direction of fracture lines is described relative to the ________ of the bone
Long axis
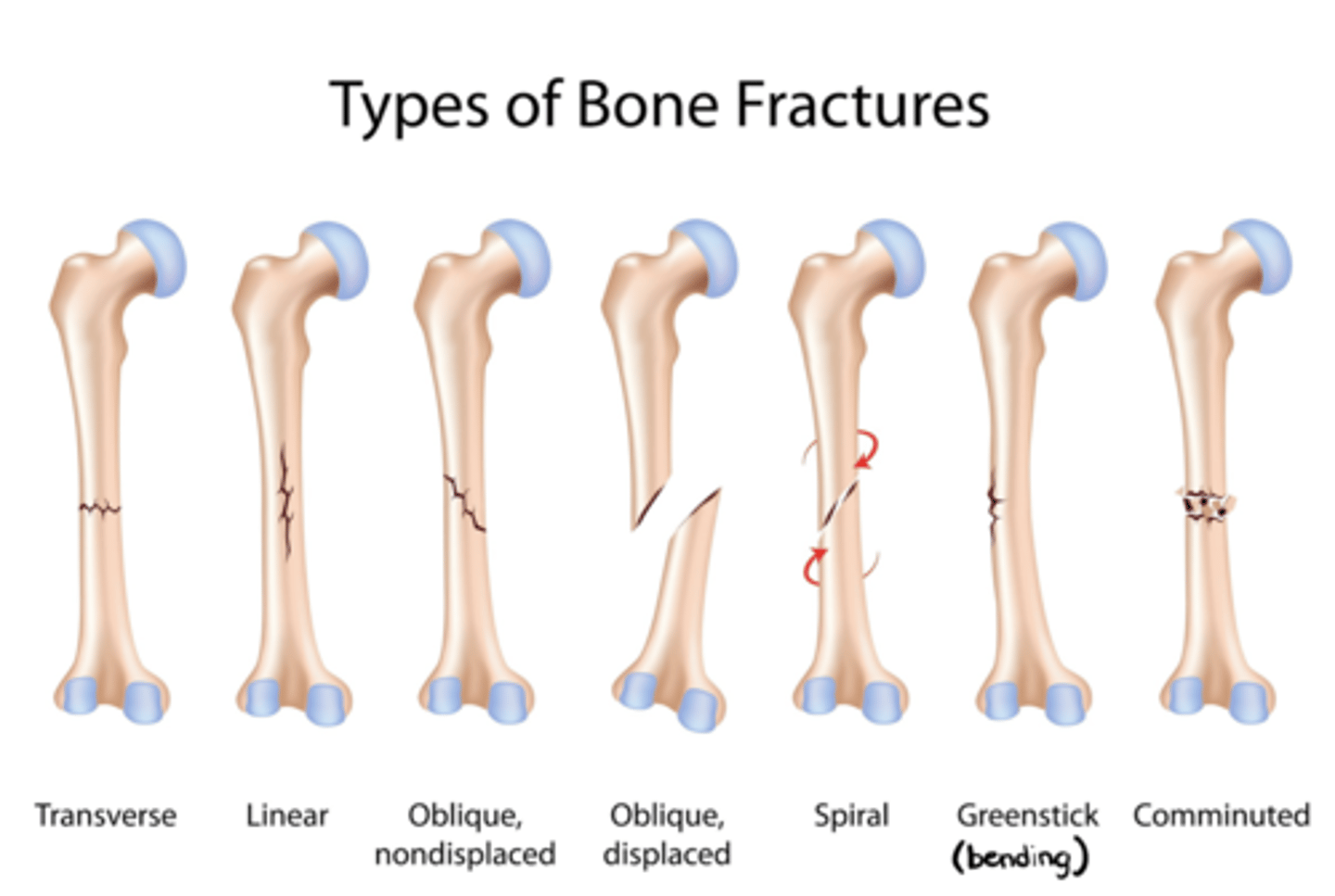
________ fractures = multi-fragment (3+ pieces)
Comminuted

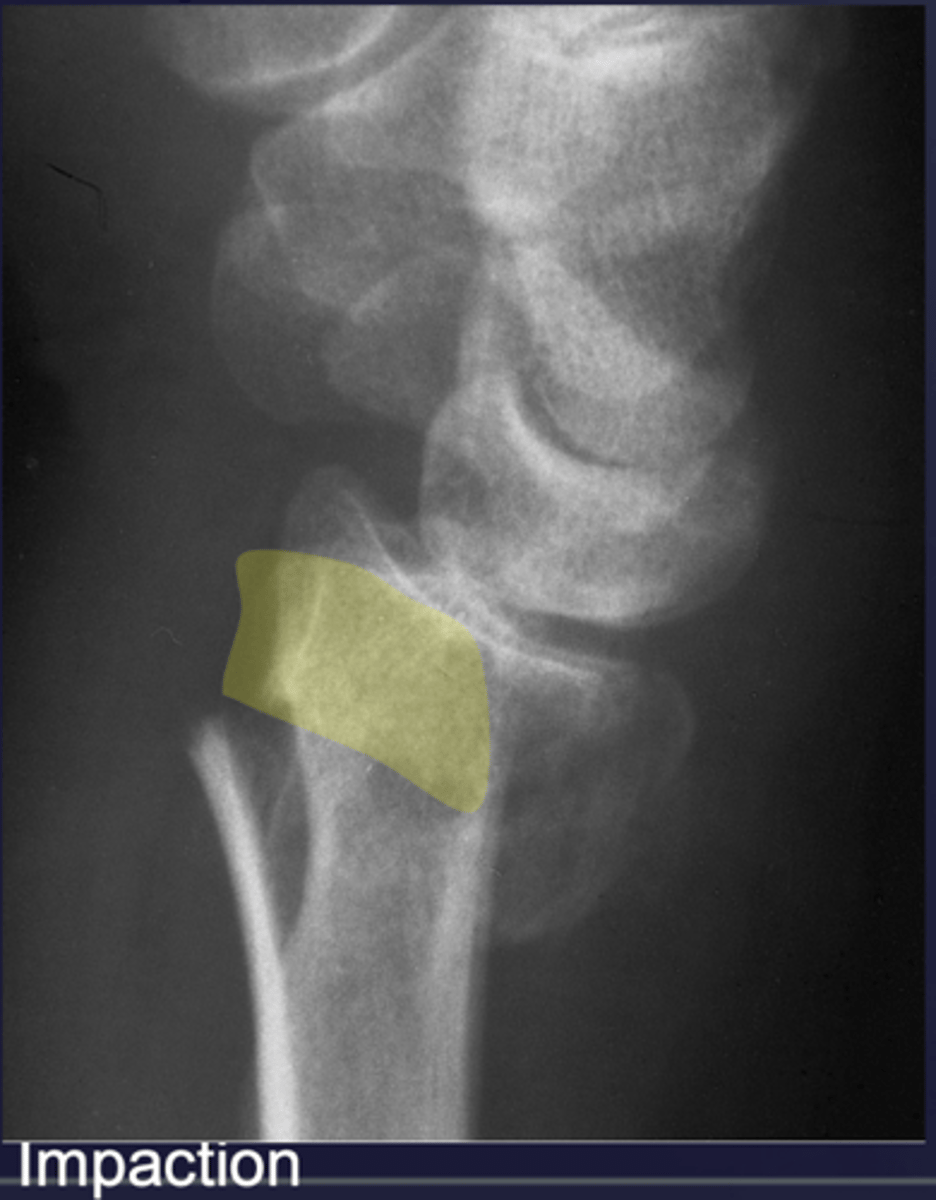
________: one fragment forced into another
Impaction (ex: compression fractures, endplate impacted; CT can help define location and the extent)
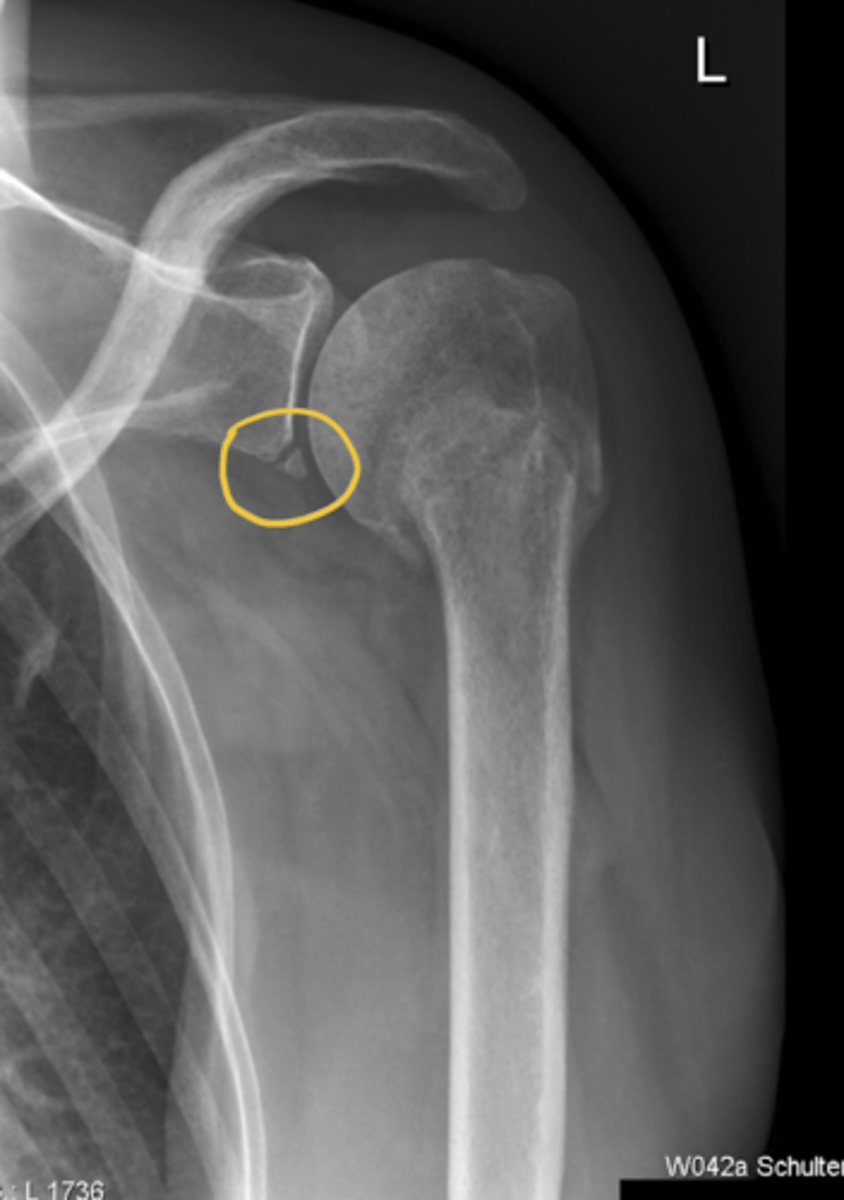
________: type of bone fracture that occurs when a ligament or tendon forcefully pulls a small piece of bone away from the main bone mass
Avulsion (occurs at the site of musculotendinous and ligamentous attachments)

________: can occur when dislocated humeral head compresses border of glenoid (ex: from an anterior/inferior dislocation)
Bony Bankart lesion (i.e., an avulsion of the capsulolabral tissue from the anteroinferior glenoid rim)
What falls under the category "associated abnormalities"?
Dislocations (i.e., at proximal/distal joint + accompanying fractures)
What is a "Monteggia fracture"?
Ulnar fracture --> dislocation of radio-humeral joint

What is a "Galeazzi fracture"?
Fracture of the radius and the dislocation or subluxation of the DRUJ
What falls under the category "special types"?
Stress fractures and pathological fractures (i.e., if bone breaks w/o trauma)
What are some ways pathology weakens bone?
Tumor, osteoporosis, infection, Paget's disease
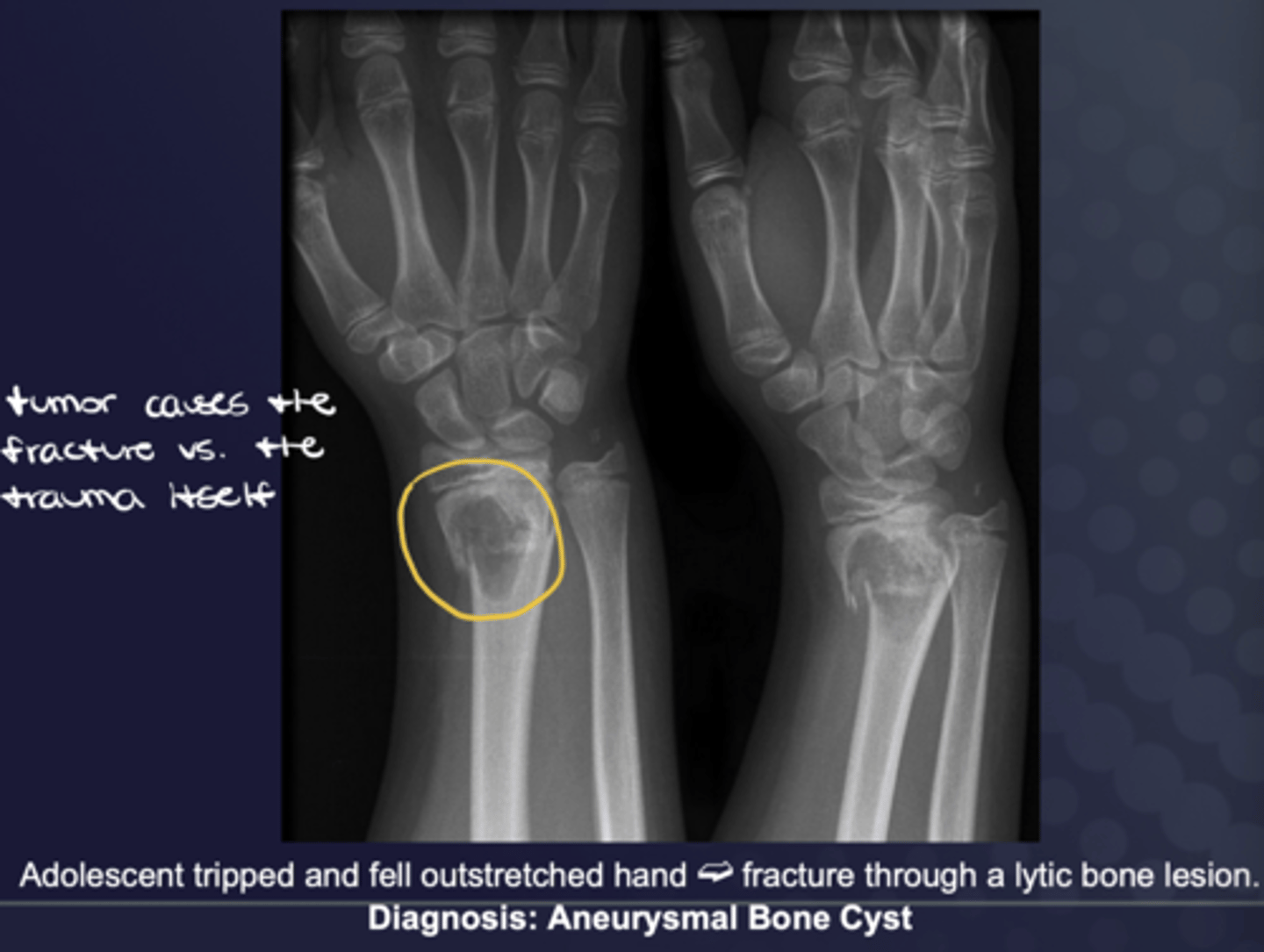
If the bone is normal and the bone breaks WITHOUT trauma, what is this known as?
Stress fracture
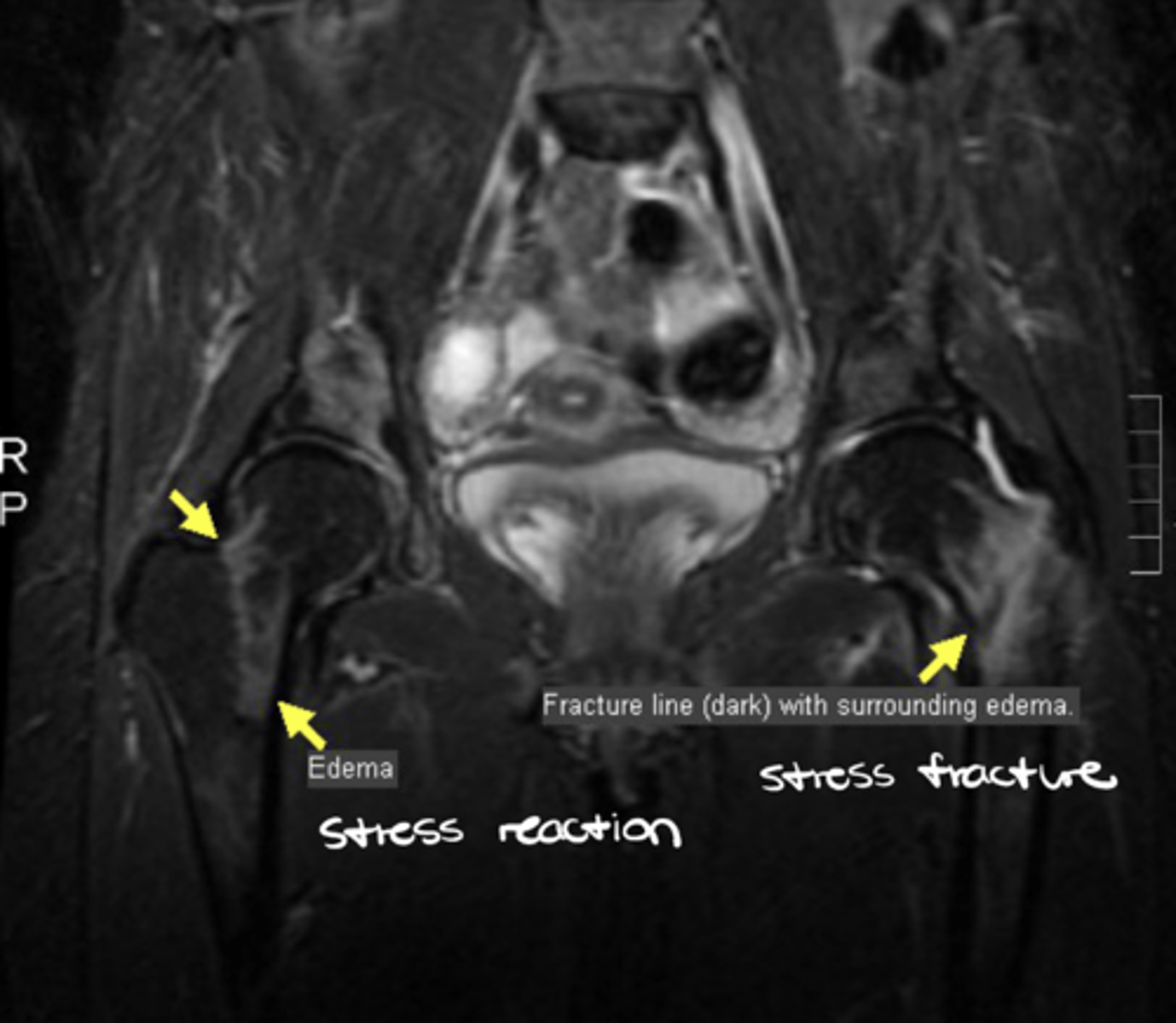
How do you ID a stress fracture?
1. History of activity induced symptoms
2. Standard radiograph initially normal
3. MRI shows abnormality much earlier (a band low signal on T1 and T2 + a zone of low (T1) and high (T2) signal)
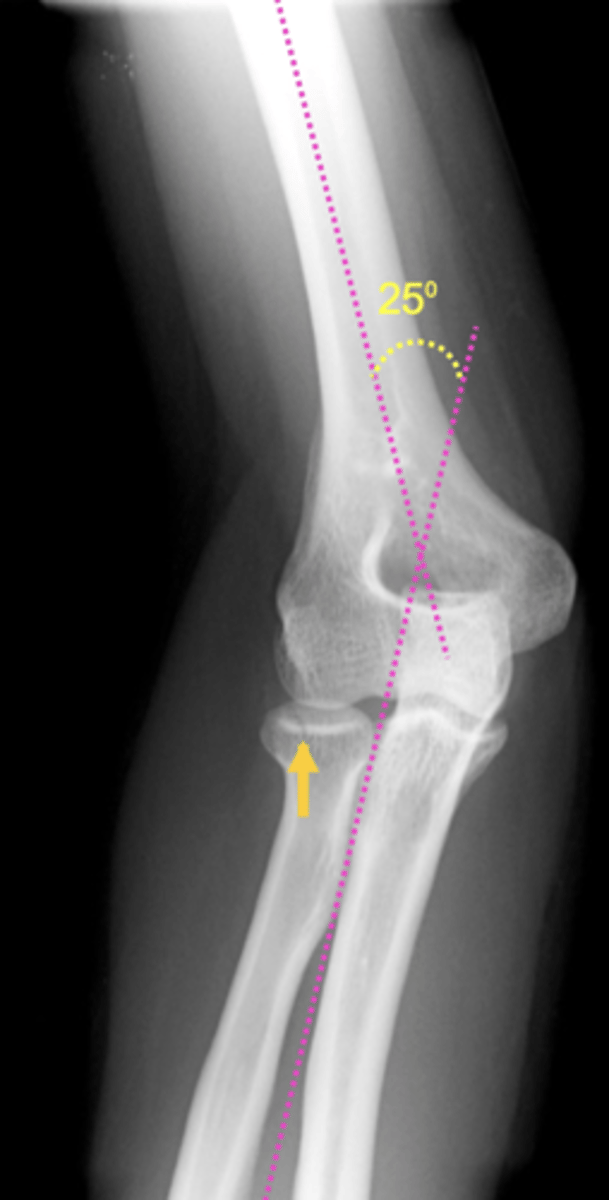
What commonly occurs w/ elbow fractures?
Increased carrying angle (should be 15 degrees)
Who is THE radiologist expert on MSK ultrasound?
Jon Jacobson
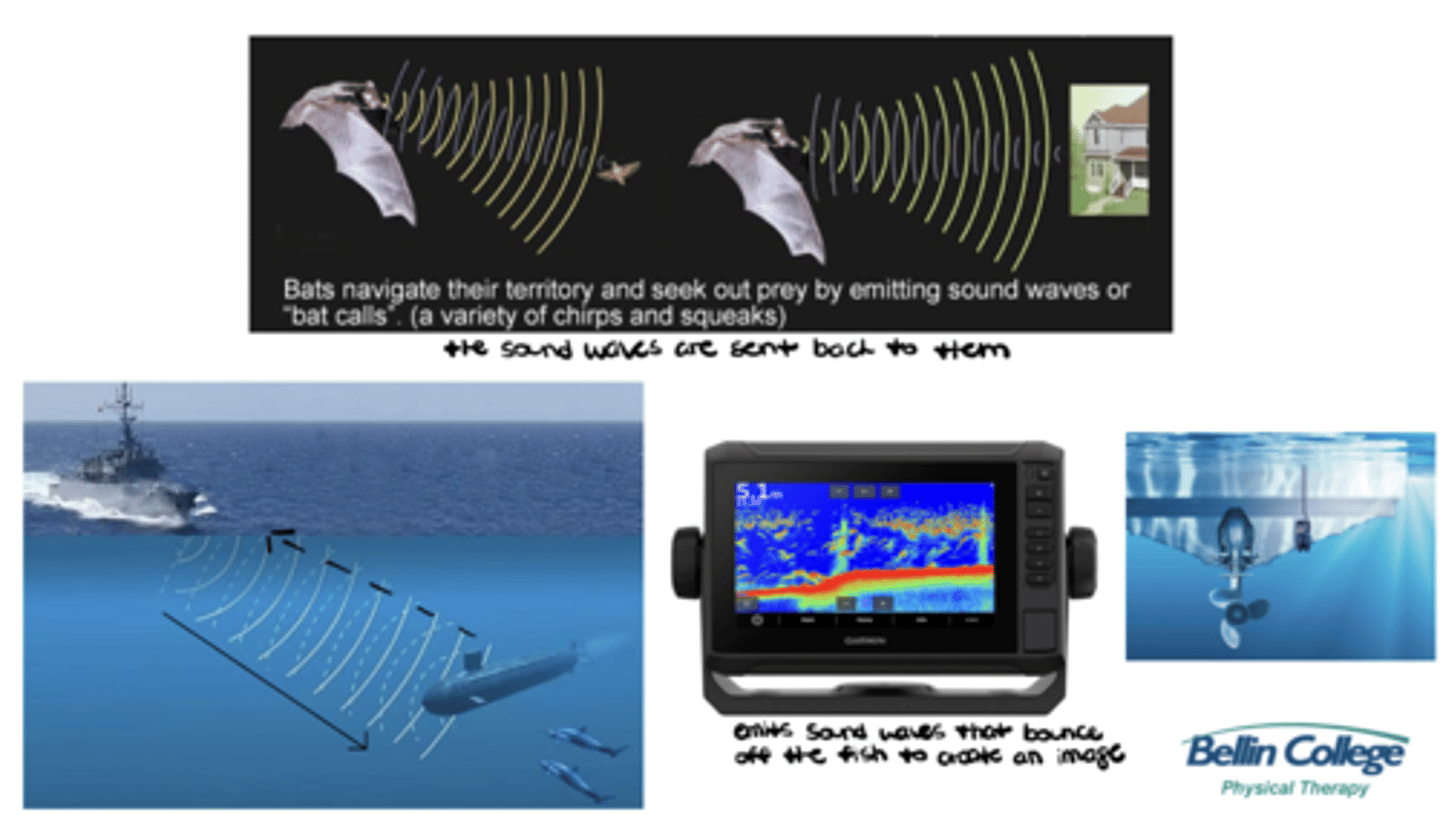
Describe the basic physics of diagnostic ultrasound in simple terms.
Ultrasound utilizes piezoelectrical crystals to emit sound waves and interpret them as they bounce off the tissues and return to the transducer (i.e., sound waves are sent out --> bounce off objects --> sent back)
What is the most important element of the ultrasound machine?
The transducer!!
What is the GOLD STANDARD certification in MSK sonography by the Alliance for Physician & Advancement (APCA) and credentialed under the American National Standards Institute (ANSI) under the International Organizations for Standardization (ISO)?
Registered in Musculoskeletal (RMSK) sonography certification
Who is able to apply for an RMSK credential?
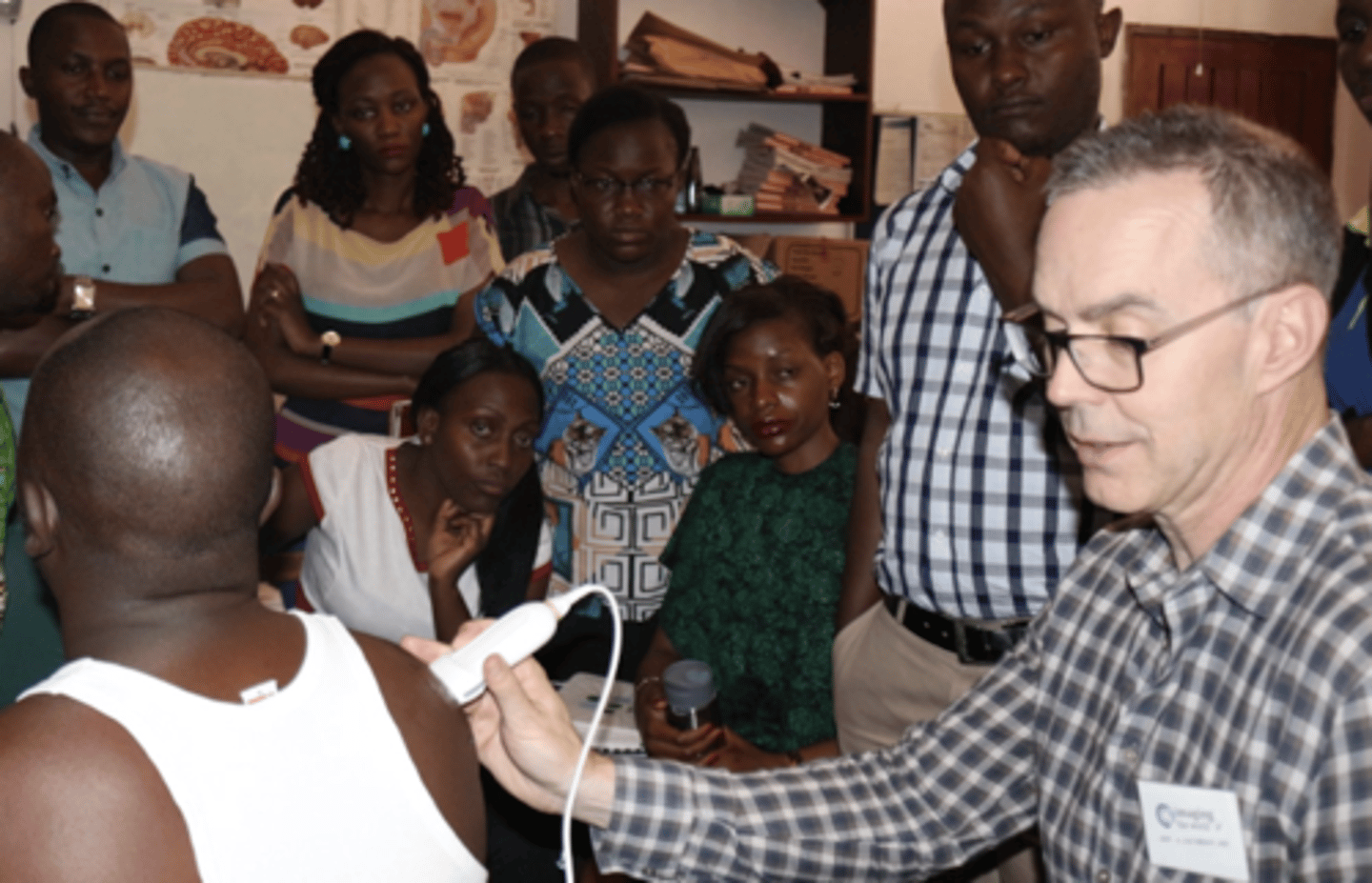
Physicians (ortho surgeons, ortho specialists, family med, sports med, physiatrists, radiologists, rheumatologists) & PHYSICAL THERAPISTS (plus chiropractors, NPs, and PAs)
What are the requirement for an RMSK credential?
Log 150 cases + pass a SUPER HARD exam
List the advantages of using diagnostic ultrasound for MSK care.
- Safe (no ionizing radiation)
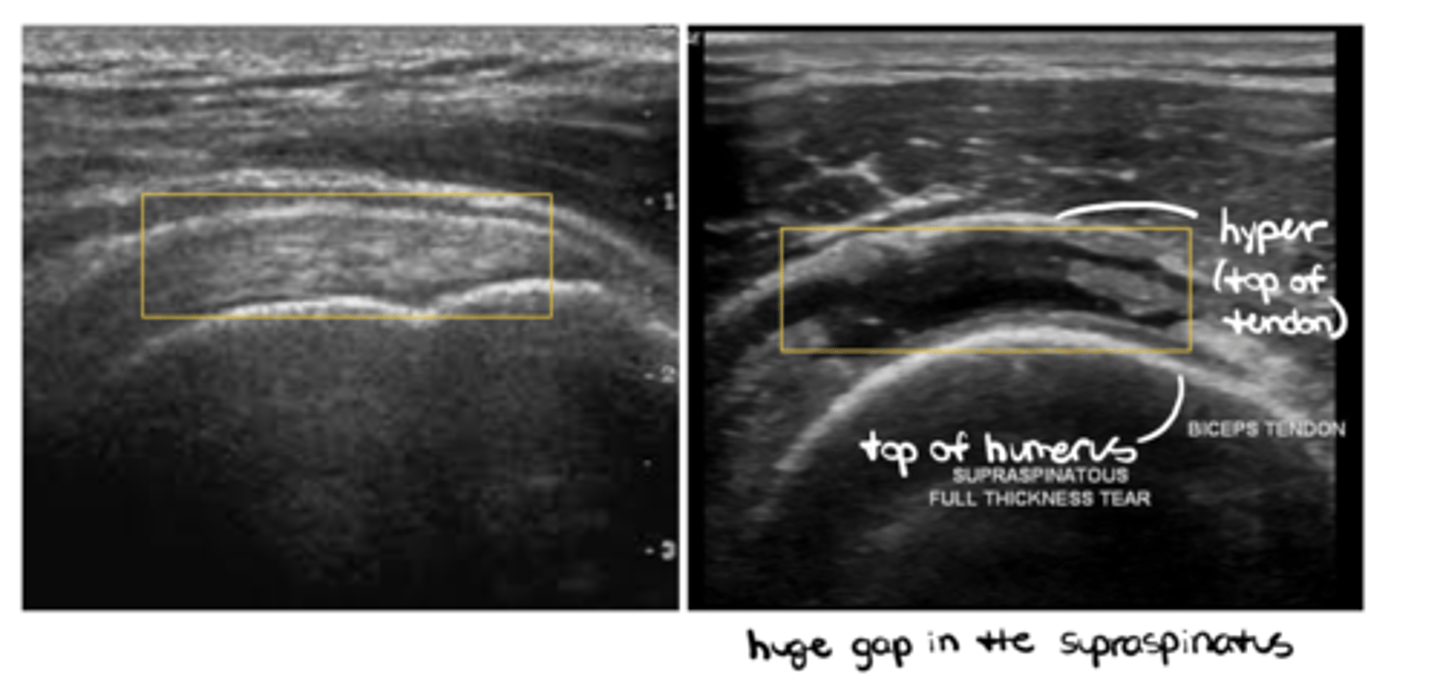
- Excellent visualization of soft tissues (ex: tears, sprains/strains, joint or muscle swelling)
- Fast/efficient (point of care)
- Sometimes portable
- Low cost
- Real time w/ bilateral comparison
- Dynamic
List the disadvantages of using diagnostic ultrasound for MSK care.
- Steep learning curve
- Operator dependent
- Limited field of view
- Artefacts
- Bone blocks sound waves
- Incomplete evaluation of joints (can only see superficial tissues, so NOT ACL, meniscus, cartilage, etc.)
__________: category of ultrasound in PT practice that emphasizes "Is there damage" (ex: supraspinatus tear)
Diagnostic -- diagnose and monitor pathology (hemarthrosis, sprains, strains, healing stage, lesions, disease)
Which specialties utilize diagnostic ultrasound?
Radiologists, sonographers, radiographers/technicians, ortho, sports med, rheumatology, family med, physical med, physiatry, AND PTs!!
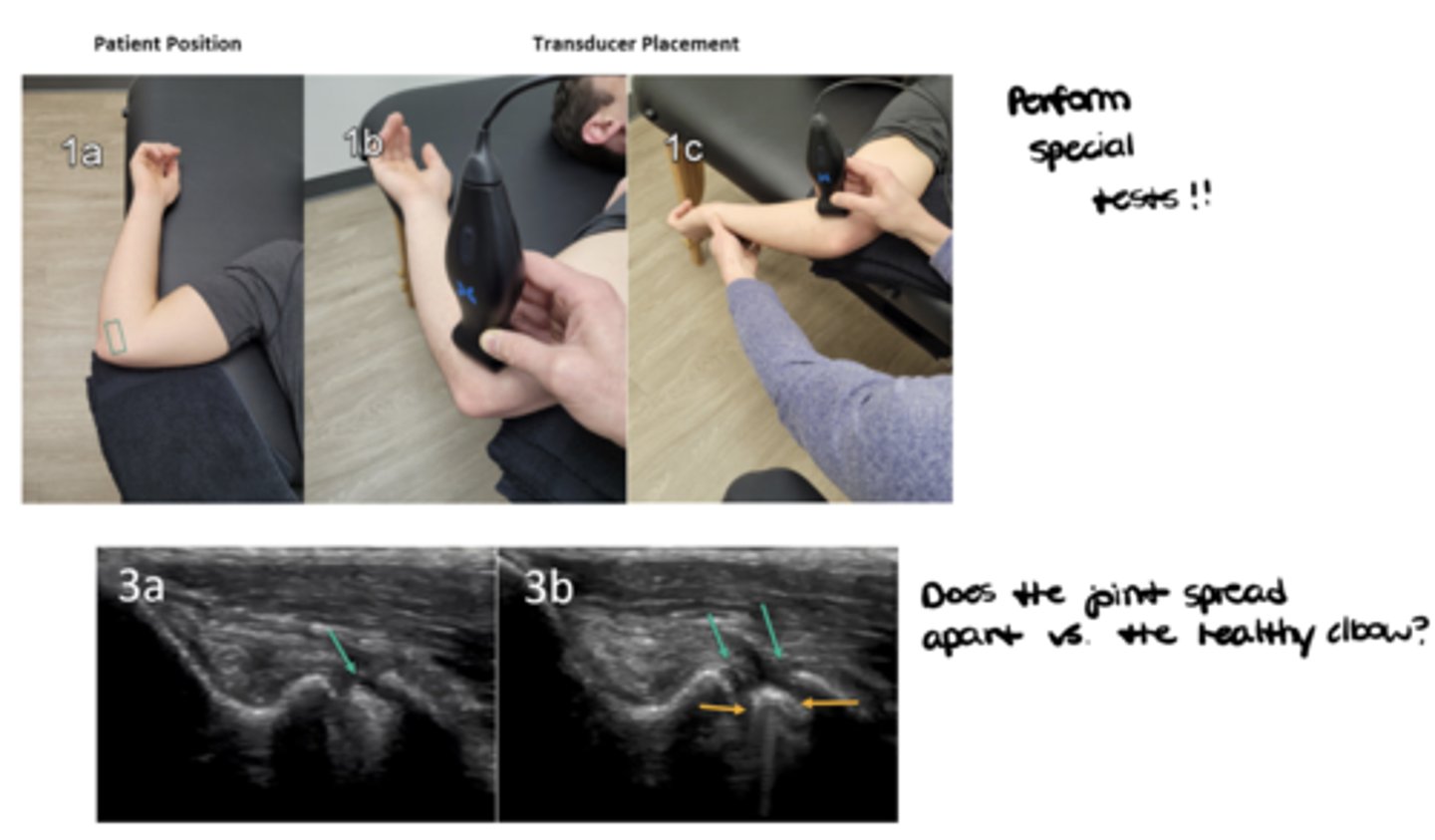
Report some examples of how a PT could use dynamic diagnostic ultrasound.
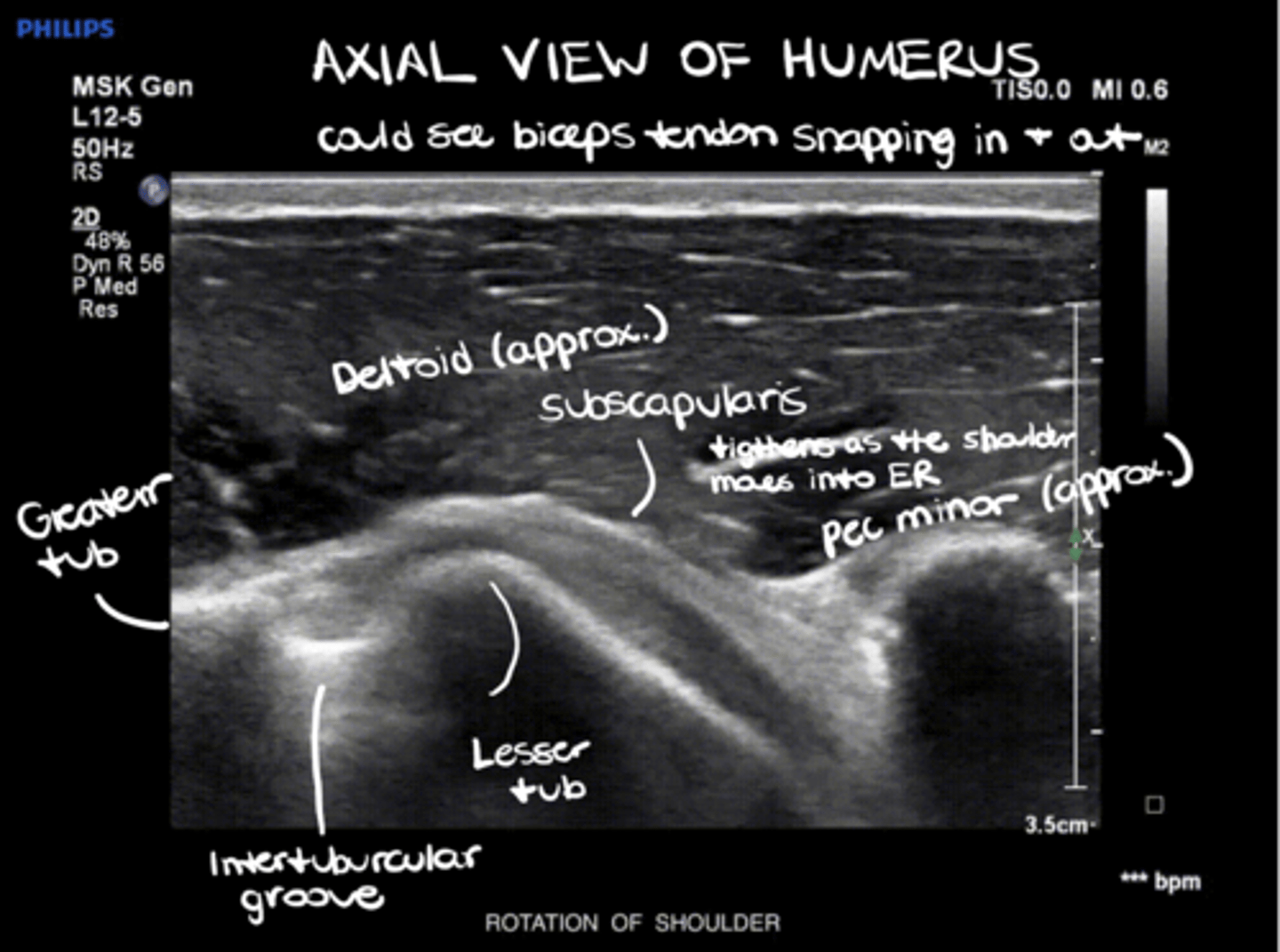
1. Analyze the structure implicated -- what is causing the patient's symptoms (ex: move the shoulder joint to see the biceps tendon snap in and out of the intertubercular groove OR see the impingement of the rotator cuff musculature)
2. Perform special tests -- does the joint spread apart vs. the healthy joint (ex: valgus/varus stress tests)
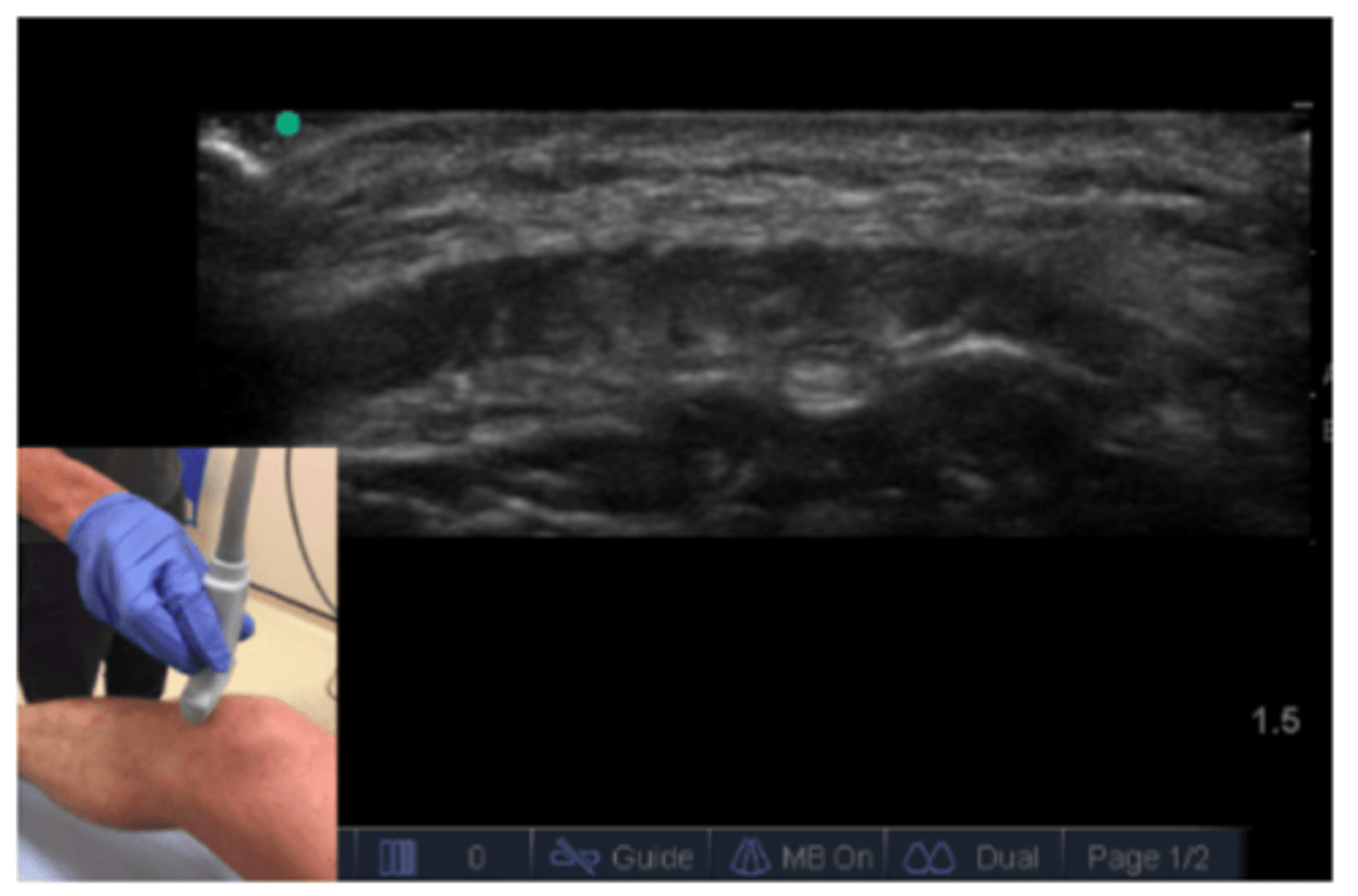
What are some features you might notice when examining rotation of the shoulder joint under ultrasound?
See image.
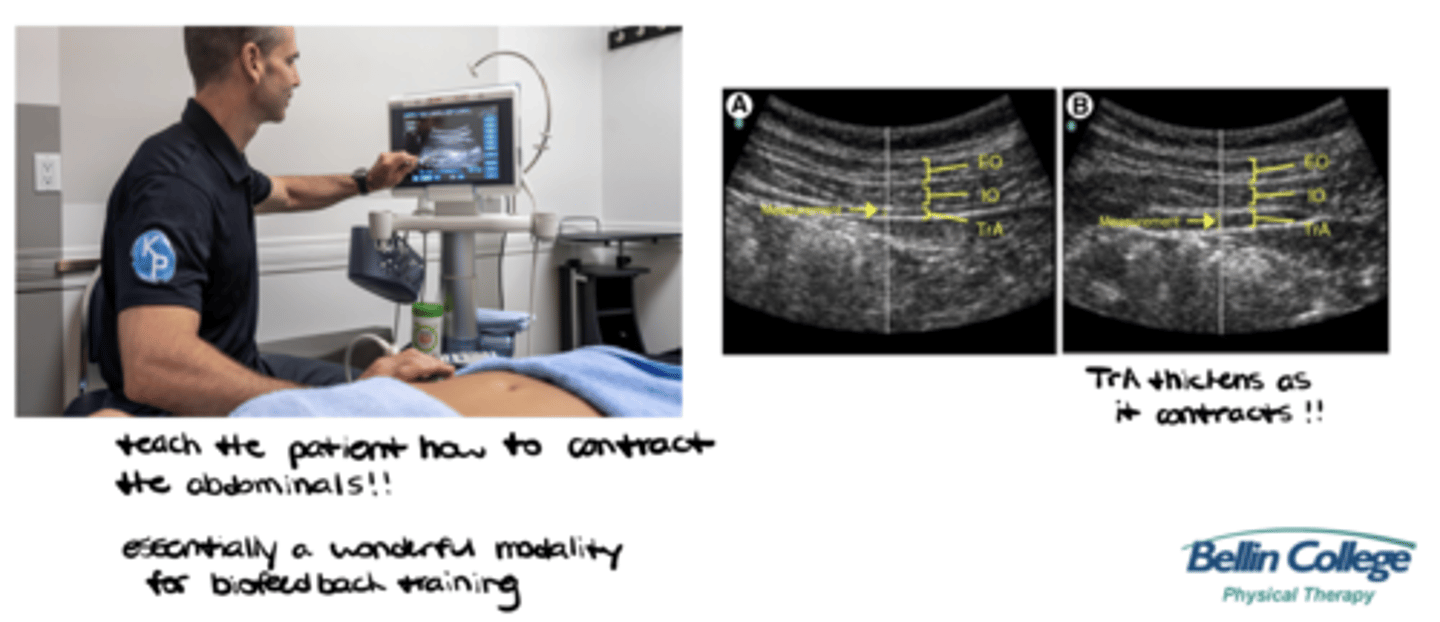
__________: category of ultrasound in PT practice that emphasizes "How do the muscles function? How do they contract?" (ex: teach the patient how to contract their abdominal muscles through evaluation/biofeedback)
Rehabilitative (evaluate muscle and other soft tissue structure and function during physical tasks)
Which specialties utilize rehabilitative ultrasound?
Predominantly PTs!!
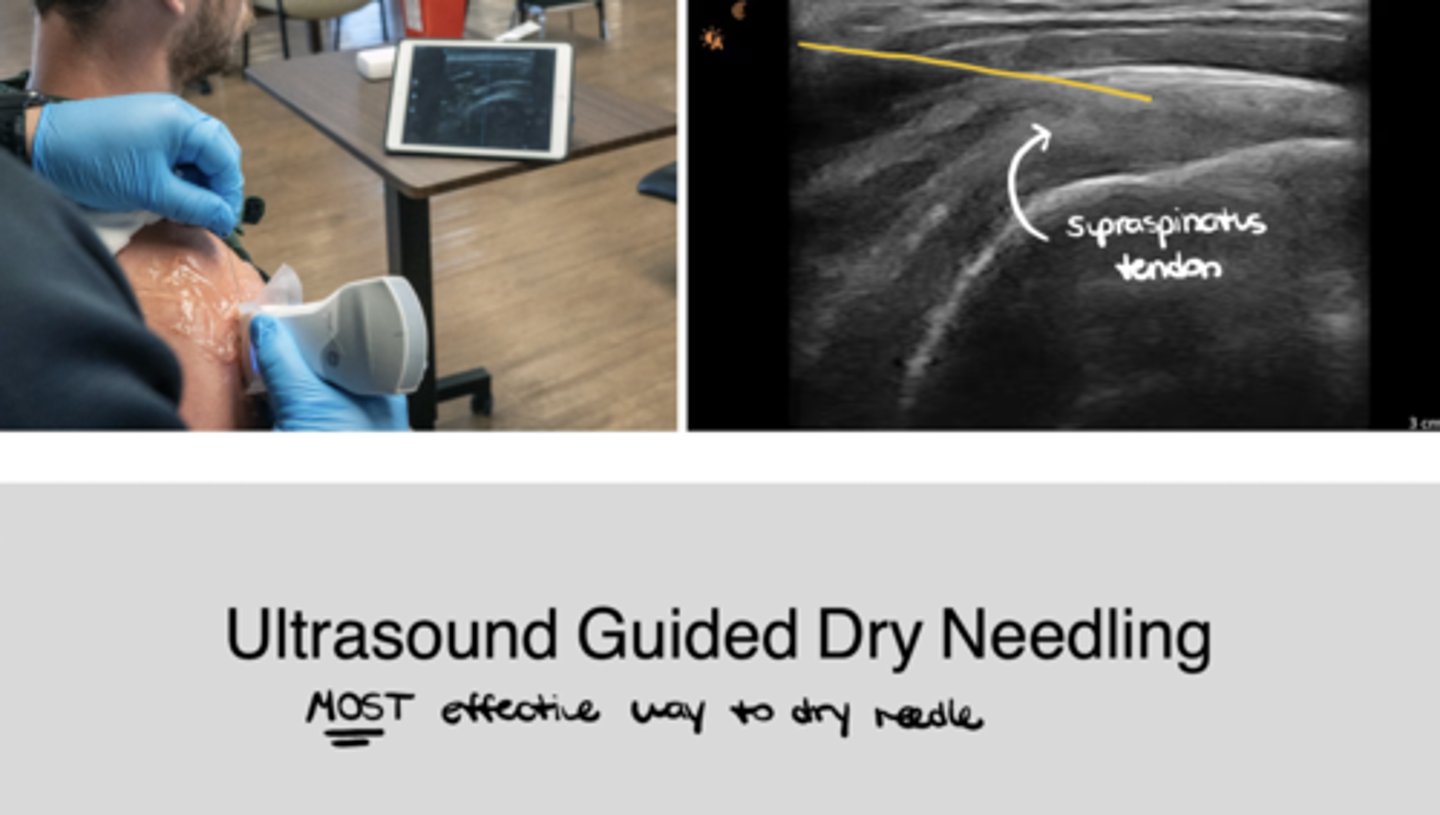
__________: category of ultrasound in PT practice that emphasizes guided percutaneous procedures involving 'dry' (acupuncture) or 'wet' needling (injection)
Interventional
__________: category of ultrasound in PT practice that emphasizes measurement, explores muscle and soft-tissue structure and function, and develops and evaluates screening tools and interventions
Research
___________: mode of ultrasound that is STANDARD; sound waves bounce down --> bounce back --> give you a 2D image. It's dynamic, you can move it, and you can see the image change as you move the sound head, but it's like a picture -- it's ONE slice of a SMALLER area (ex: one portion of the quadriceps)
B-Mode (2D Mode/Greyscale)
___________: mode of ultrasound that records motion; used a lot in echocardiograms to see the chambers of the heart as it beats OR in PT to scan the ENTIRE quadriceps all in one shot -- not used 99% of the time
M-Mode (motion mode)
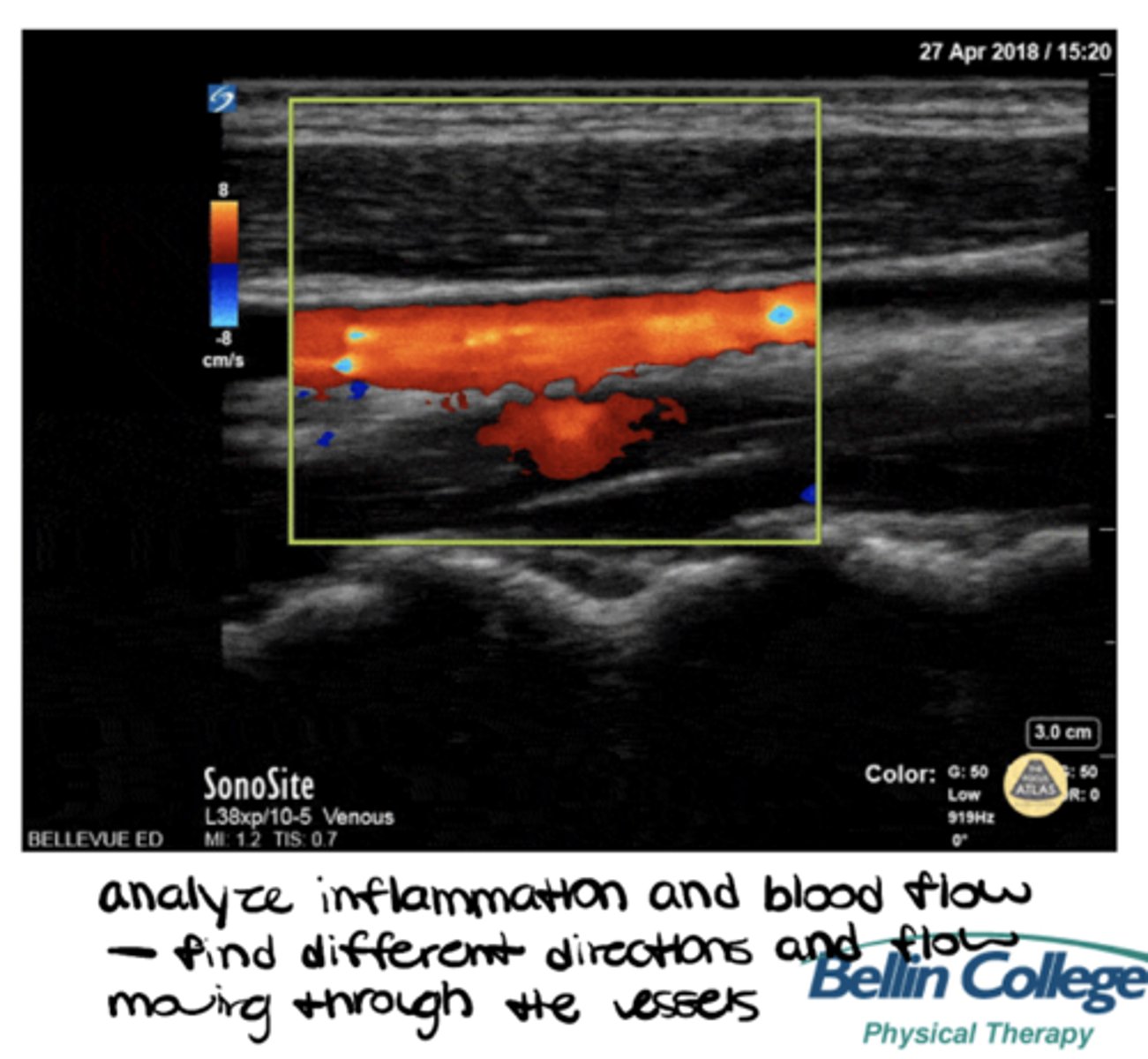
___________: mode of ultrasound that records blood flow (veins and arteries) and inflammation
Doppler (fluid mode)
___________ frequency + ___________ wavelengths = SUPERFICIAL structures (note: also has high resolution)
High frequency + short wavelengths
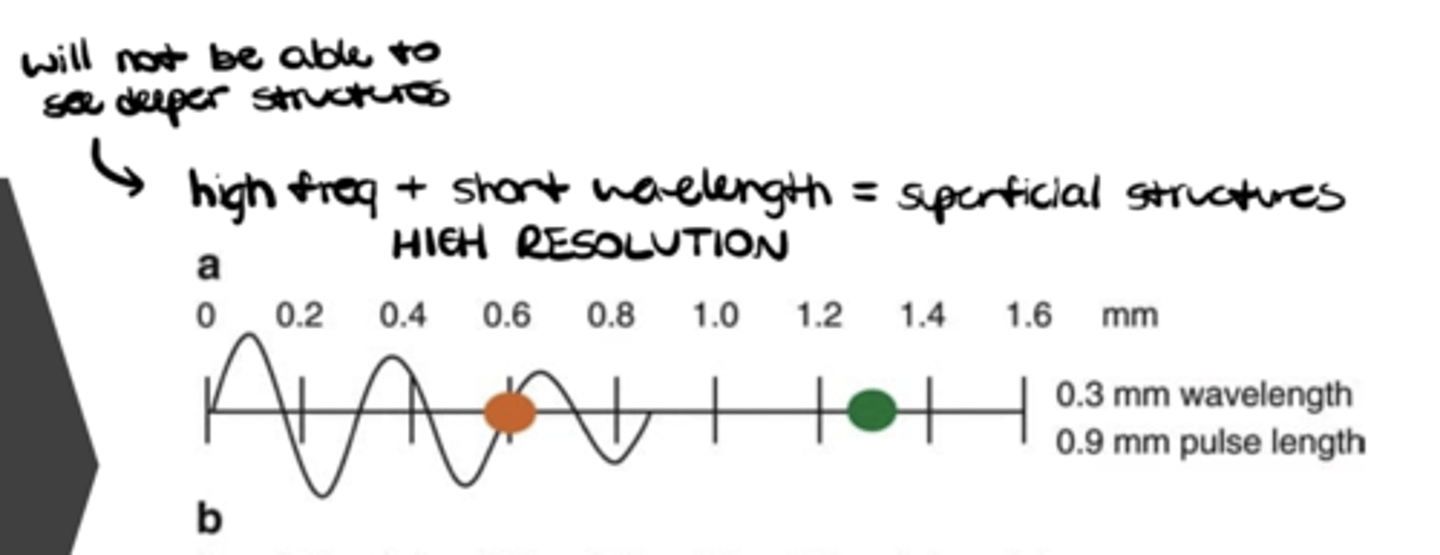
Which structures are "superficial"?
Tendons, ligaments, muscles, joints (first inch or two)
Which type of probe is MOST appropriate to view superficial structures?
Linear with the HIGHEST frequency -- used 99% of the time
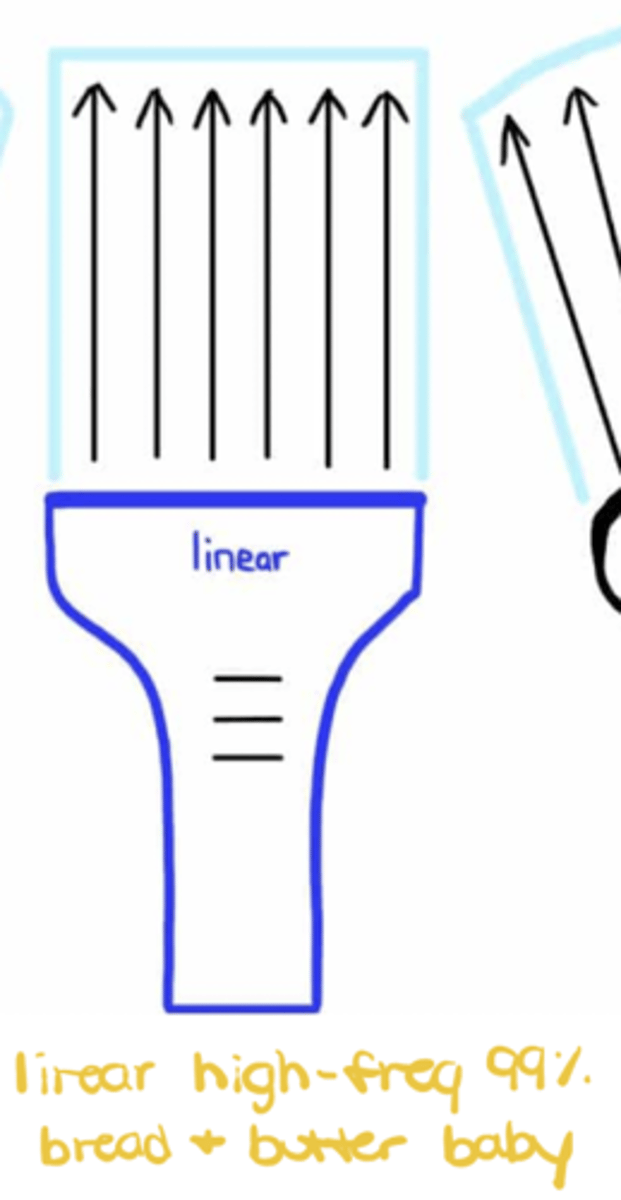
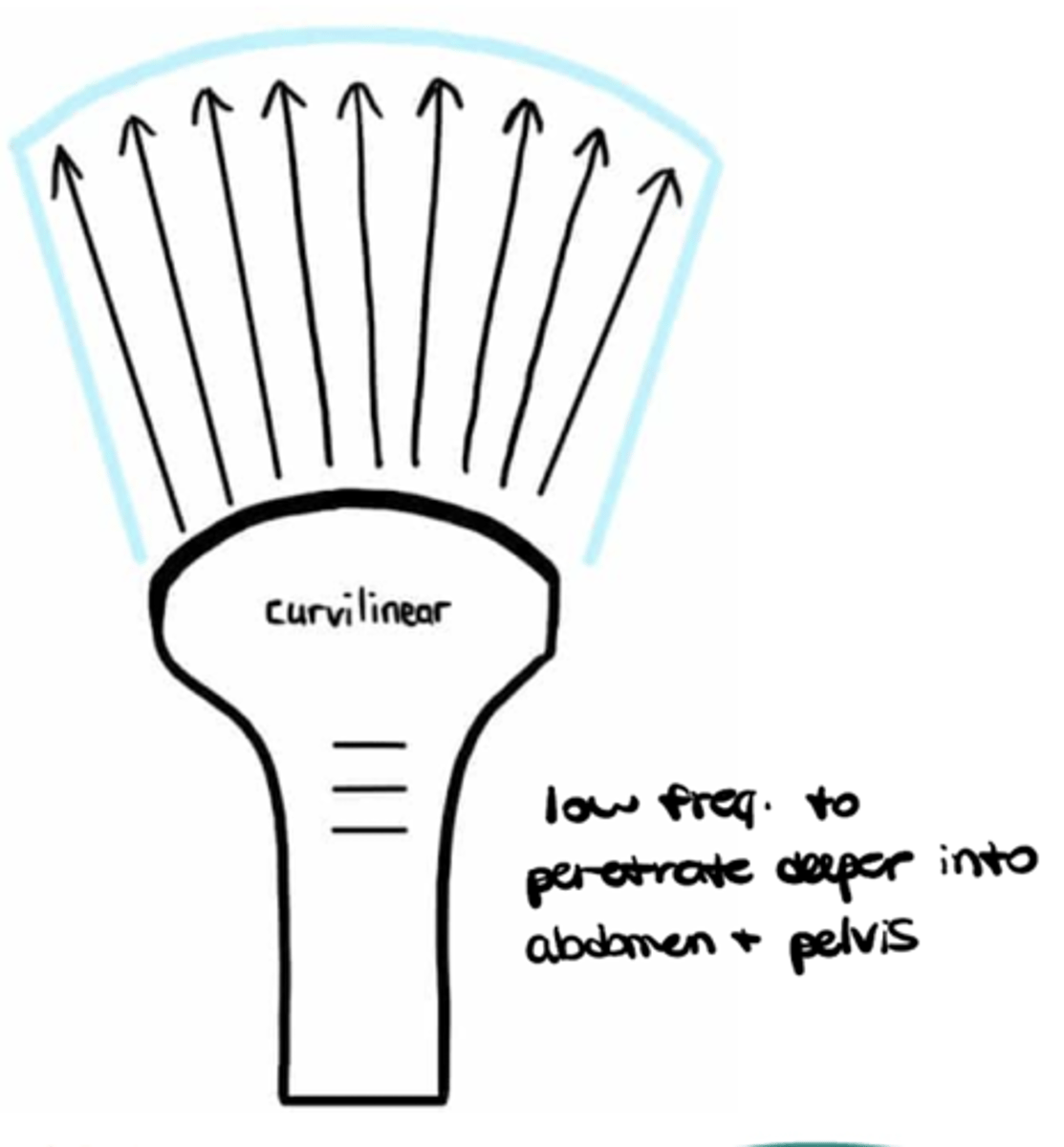
___________ frequency +. ___________ wavelengths = DEEP structures (note: also has low resolution)
Low frequency + long wavelengths
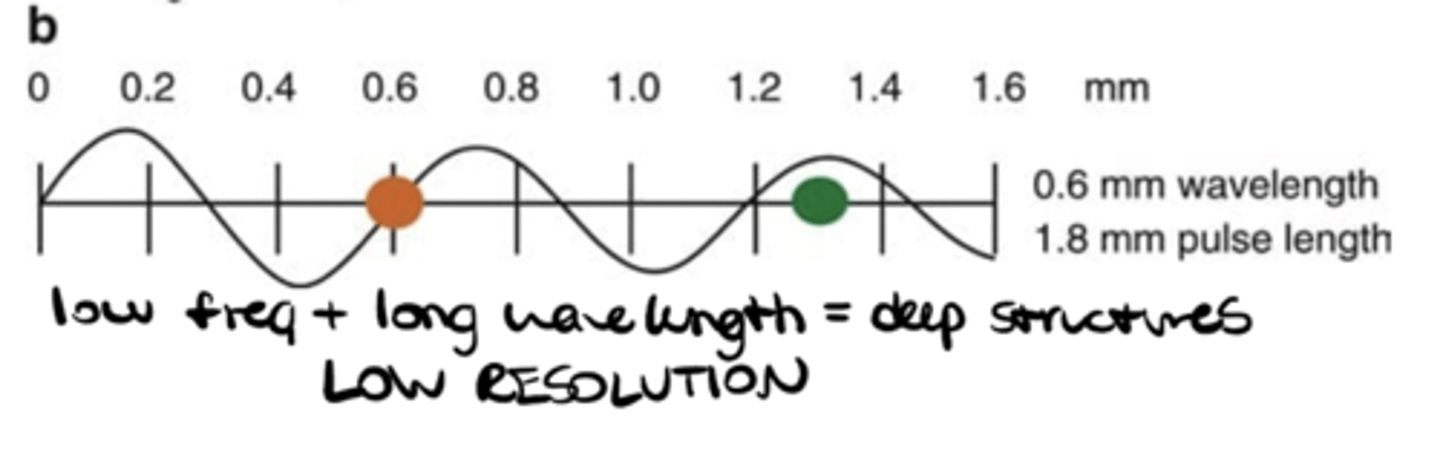
Which structures are "deep"?
Abdomen, pelvic health, bladder
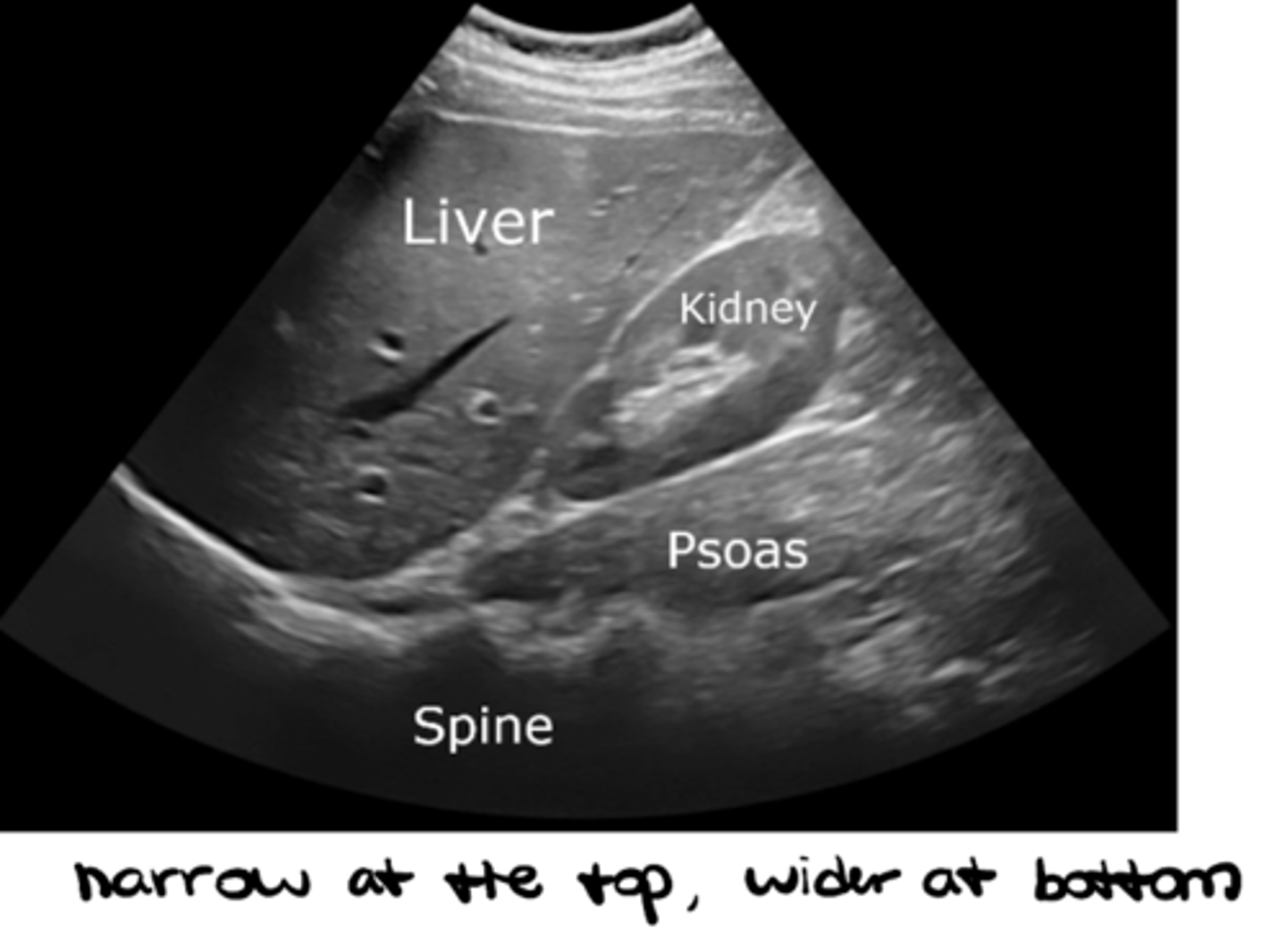
Which type of probe is MOST appropriate to view deep structures?
Curvilinear with LOW frequency (narrow at the top and wider at the bottom)
___________: level of greyscale in an image
Echogenicity
_______ (higher/lower) echogenicity = _______ (hyper- vs. hypo-echoic) = BRIGHT (bone/air)
Higher = HYPER-echoic = BRIGHT (bone/air)
_______ (higher/lower) echogenicity = _______ (hyper- vs. hypo-echoic) = GREY (soft tissues)
Lower = HYPO-echoic = GREY (soft tissues)
_______ (higher/lower) echogenicity = _______ (hyper- vs. hypo-echoic) = BLACK (fluid -- nothing to bounce off of)
Trick question!! LOWEST = AN-echoic = BLACK (fluid)
True or false: hyper- vs. hypo-echoic is all relative
TRUE!! (meaning one structure can be hyper-echoic in comparison to another structure BUT hypo-echoic in comparison to a different structure)

The abdominal wall is _______-echoic vs. the _______-echoic urine
Hyper-echoic abdominal wall vs. anechoic urine

The fascial wall is _______-echoic vs. the _______-echoic abdominal muscles
Hyper-echoic fascial wall vs. hypo-echoic abdominal muscles

The a kidney stone is _______-echoic vs. the _______-echoic abdominal wall
Hyper-echoic kidney stone vs. hypo-echoic abdominal wall

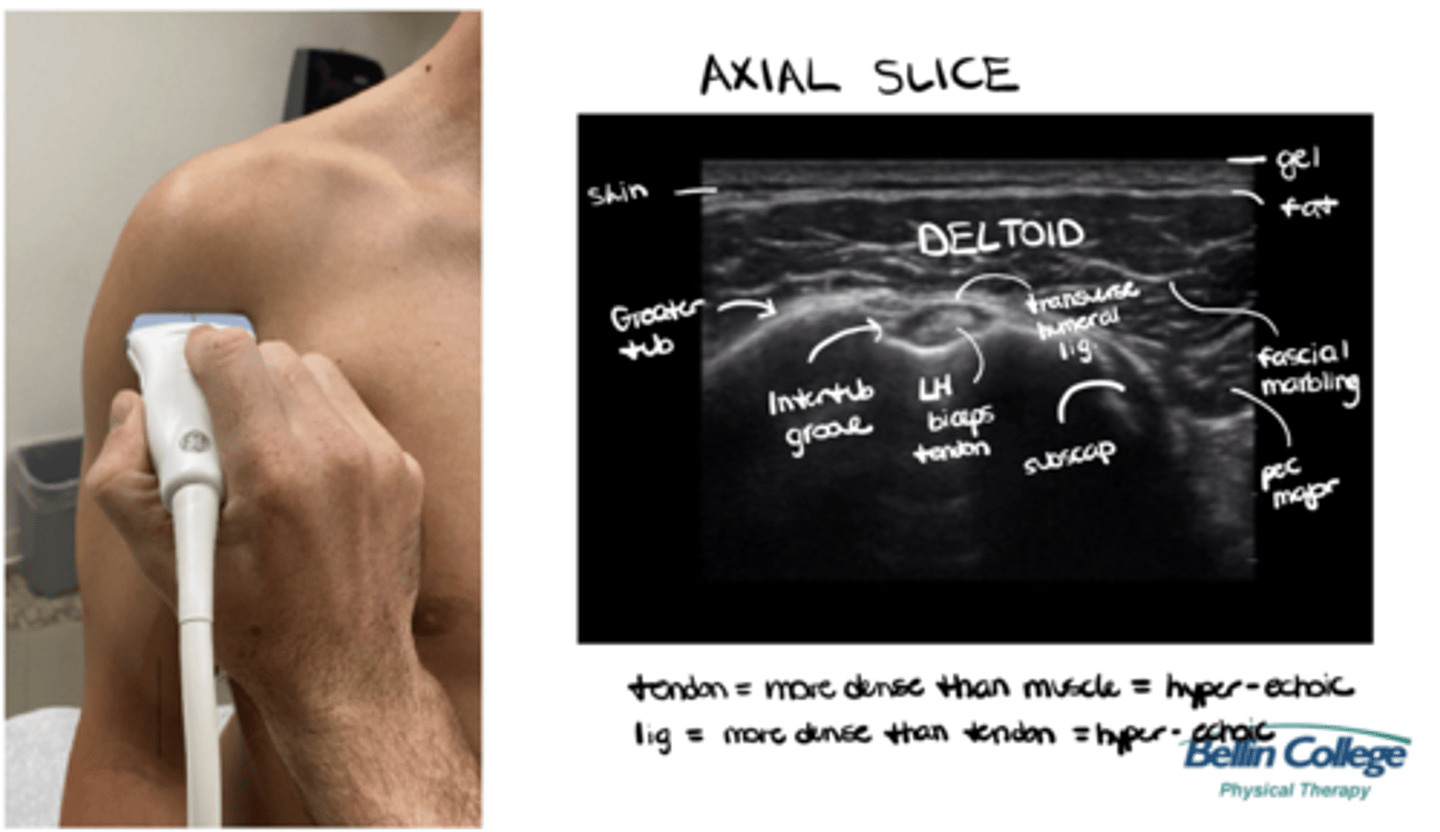
Tendon is DENSER than muscle = _______-echoic, BUT a ligament is DENSER than a tendon = _______-echoic
Hyper-echoic
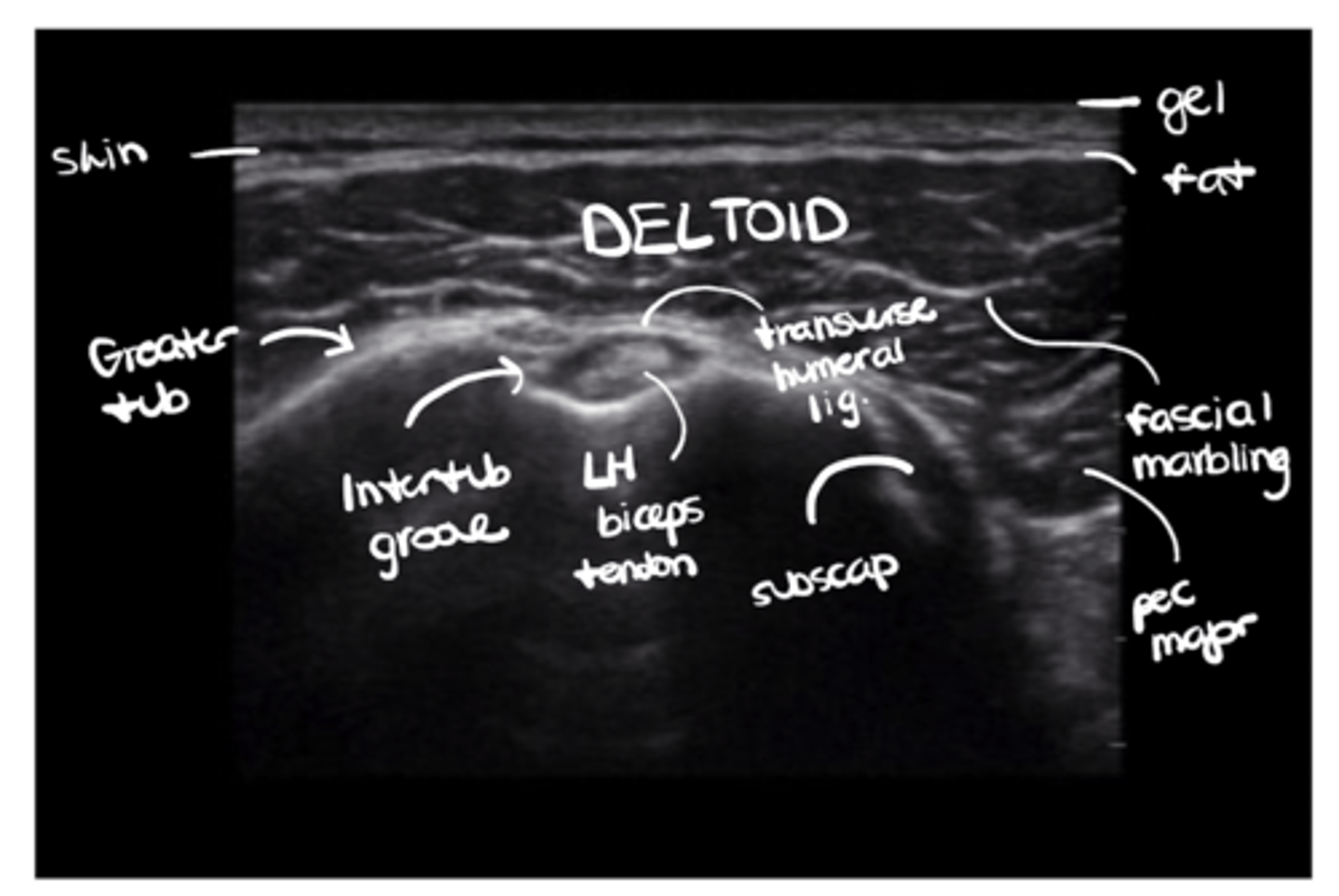
Run us through what you would see on an axial slice of the shoulder under ultrasound.
Gel --> skin --> fat --> deltoid w/ fascial marbling --> subscapularis + pec major in the mix --> greater tuberosity + transverse humeral ligament over the intertubercular groove --> LH biceps tendon
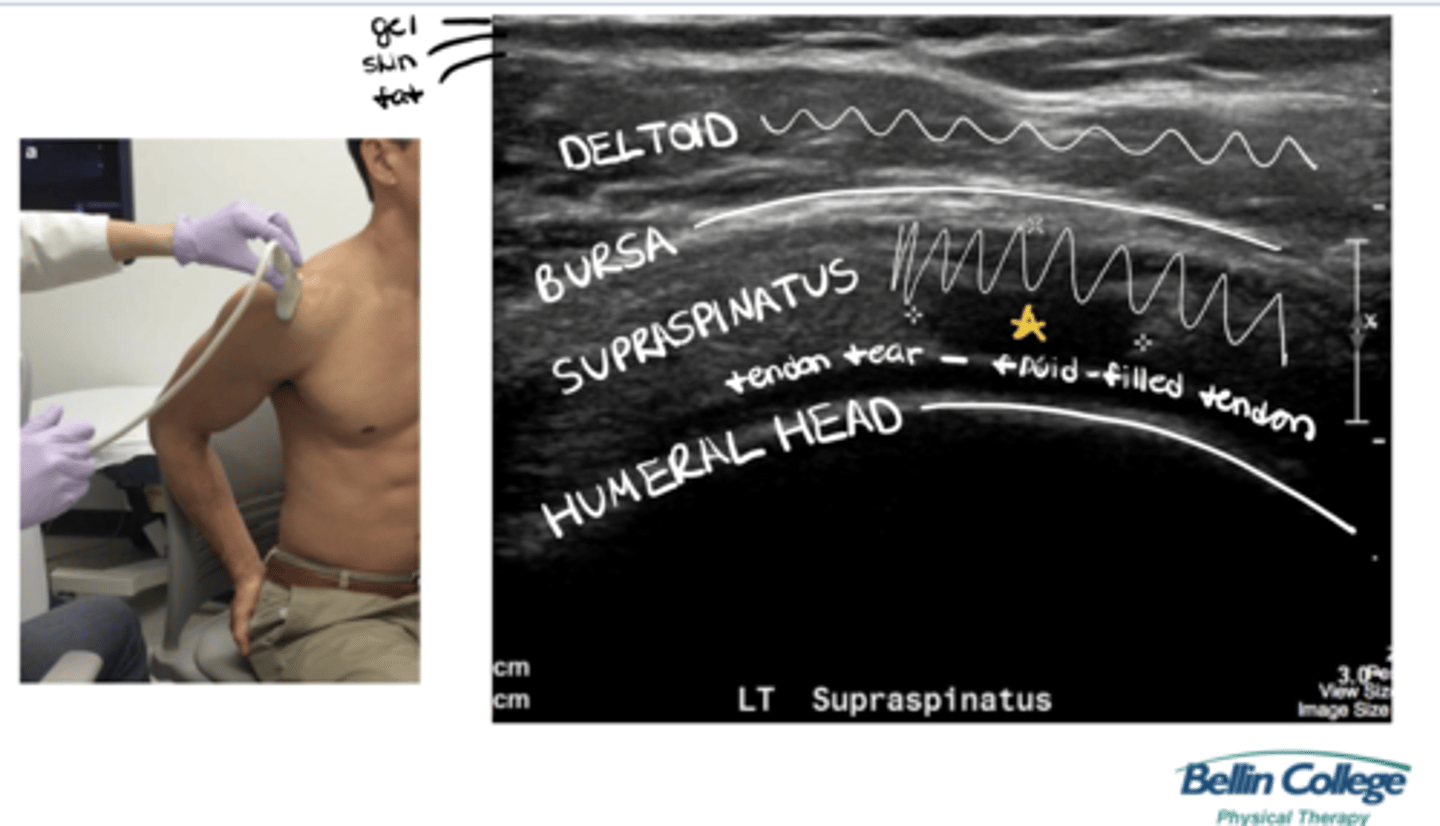
As the shoulder extends backwards, how would this image change? What if the supraspinatus was torn?
Gel --> skin --> fat --> deltoid --> bursa --> supraspinatus w/ a fluid-filled pocket --> humeral head
___________: general errors in imaging that can be caused by a number of factors, including the machine's assumptions about the data, or the interaction of sound waves w/ tissue
Artifacts (i.e., anything made or introduced artificially which misleads the results of an investigation, image, or teset)
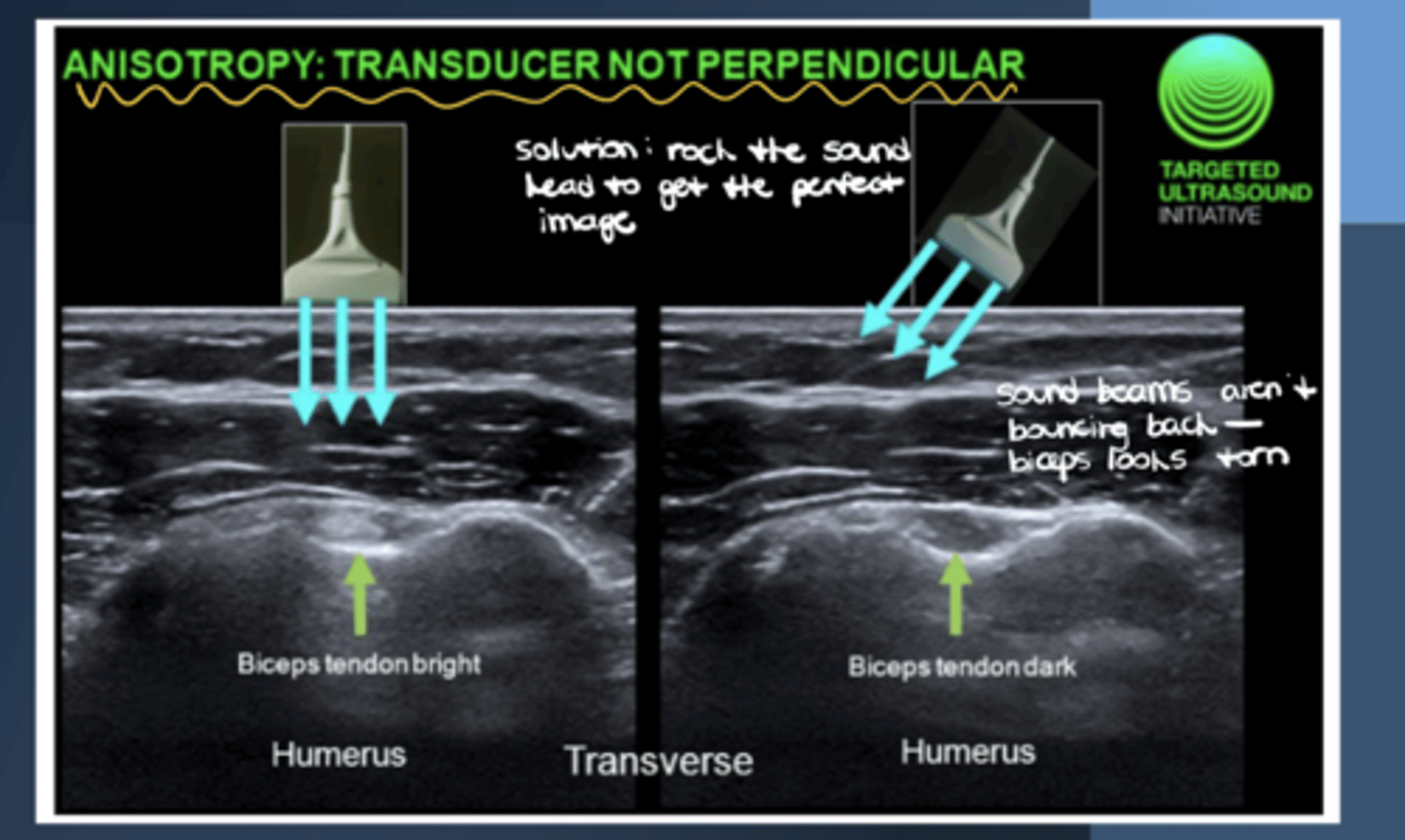
___________: a type of reflection artifact that occurs when sound waves are NOT perpendicular to the tissue being imaged, causing the image to appear darker and less resolved
Anisotrophy (i.e., may make a muscle/tendon look torn when it is not)
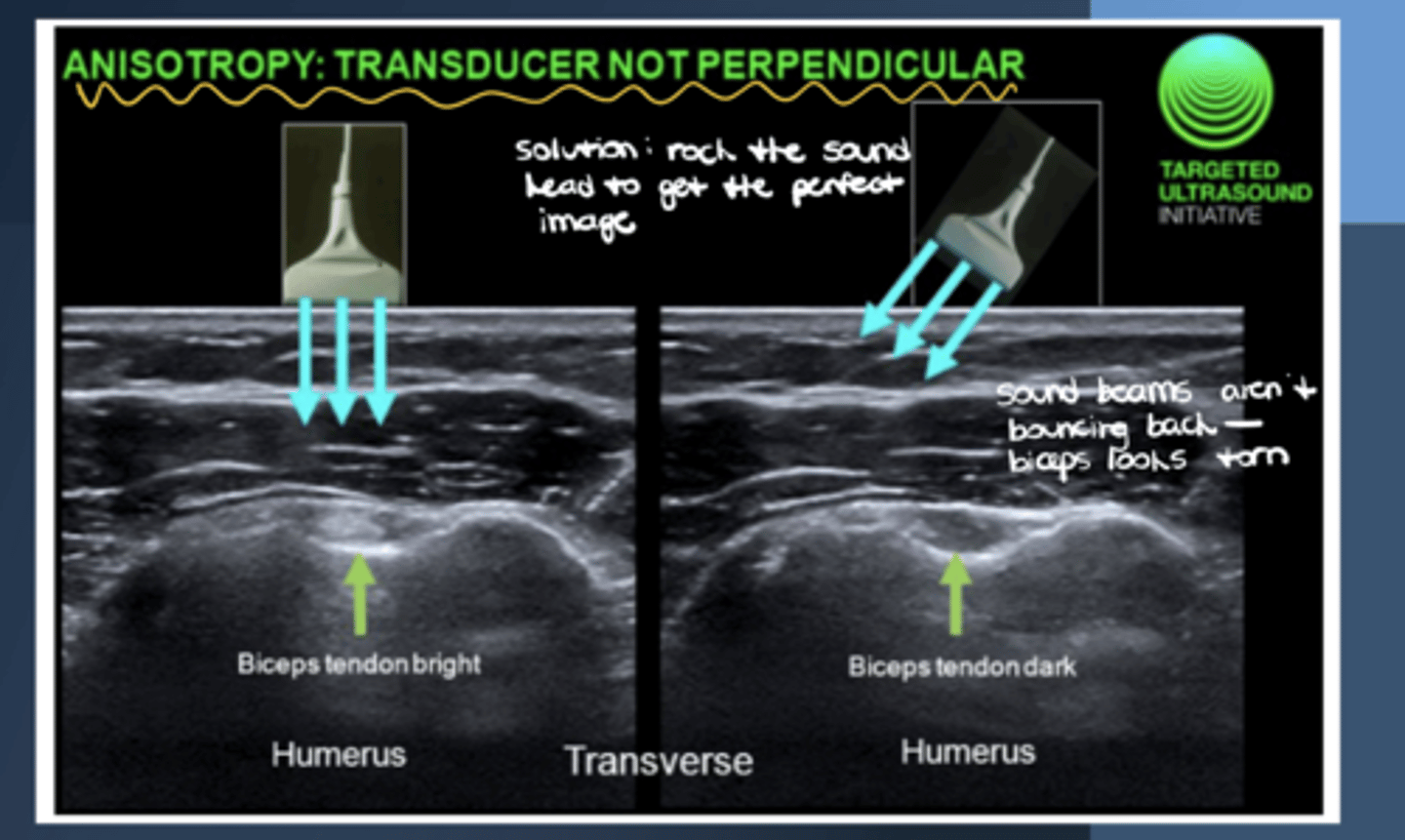
What is the solution to anisotrophy?
Rock the sound head to get the perfect image
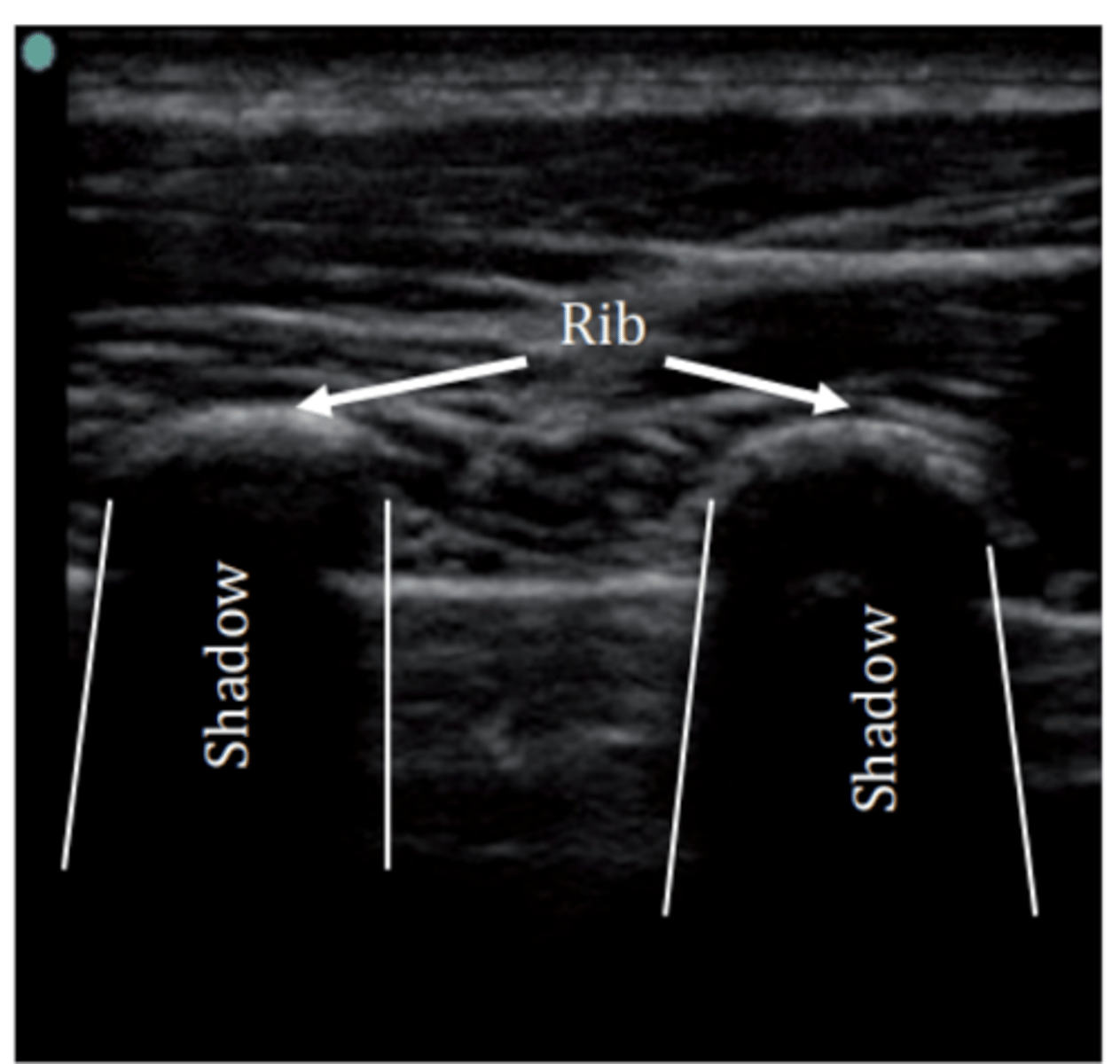
___________: phenomenon in ultrasound imaging where sound waves are blocked by certain tissues --> dark area on the screen (i.e., when you hit something SUPER dense, like the ribs, everything below it will be blocked)
Acoustic shadowing (other tissues include bone, calcifications, dense fibrous tissue, metal)
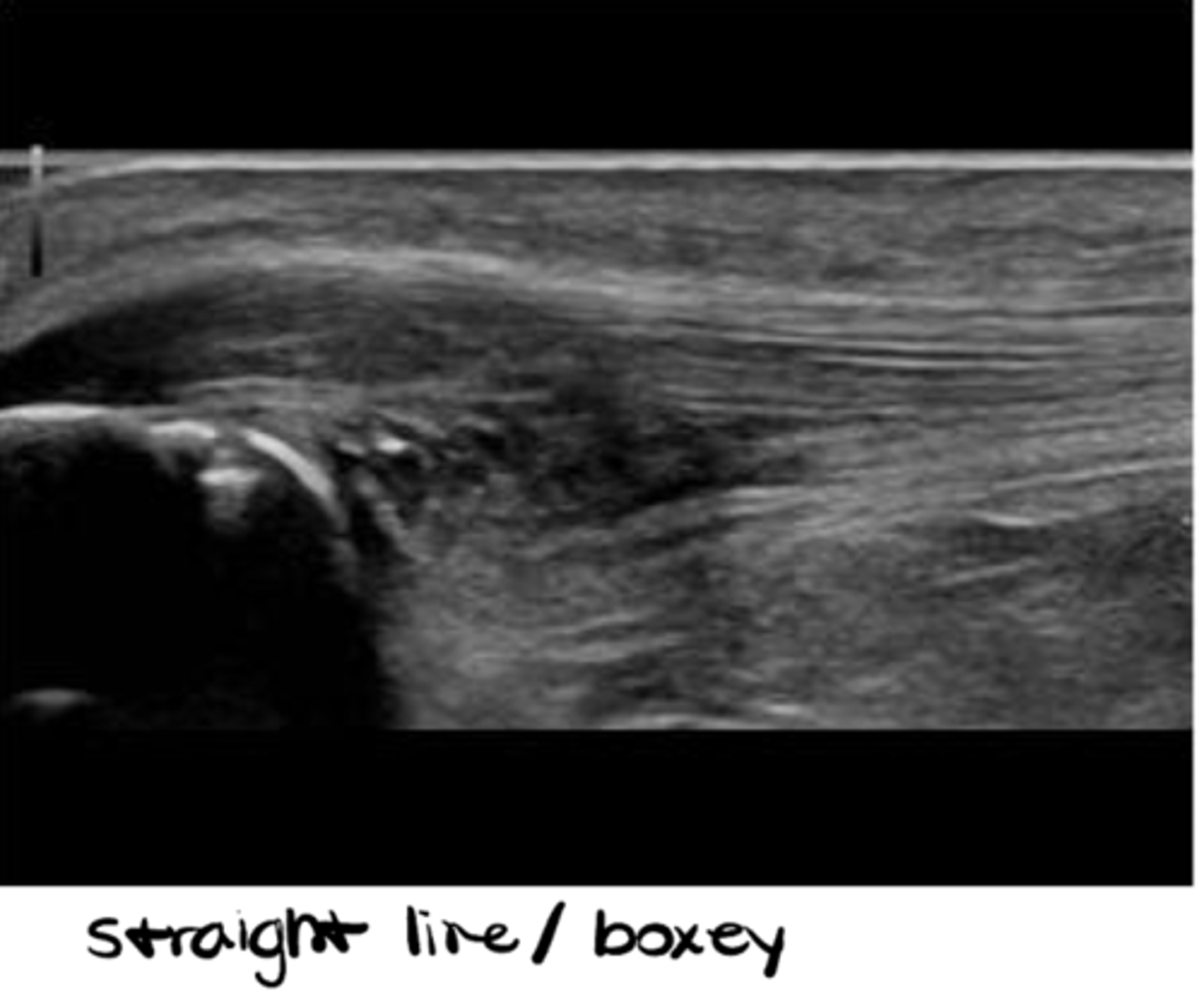
___________: probe orientation that allows for a longitudinal/vertical/up & down scan
Long axis
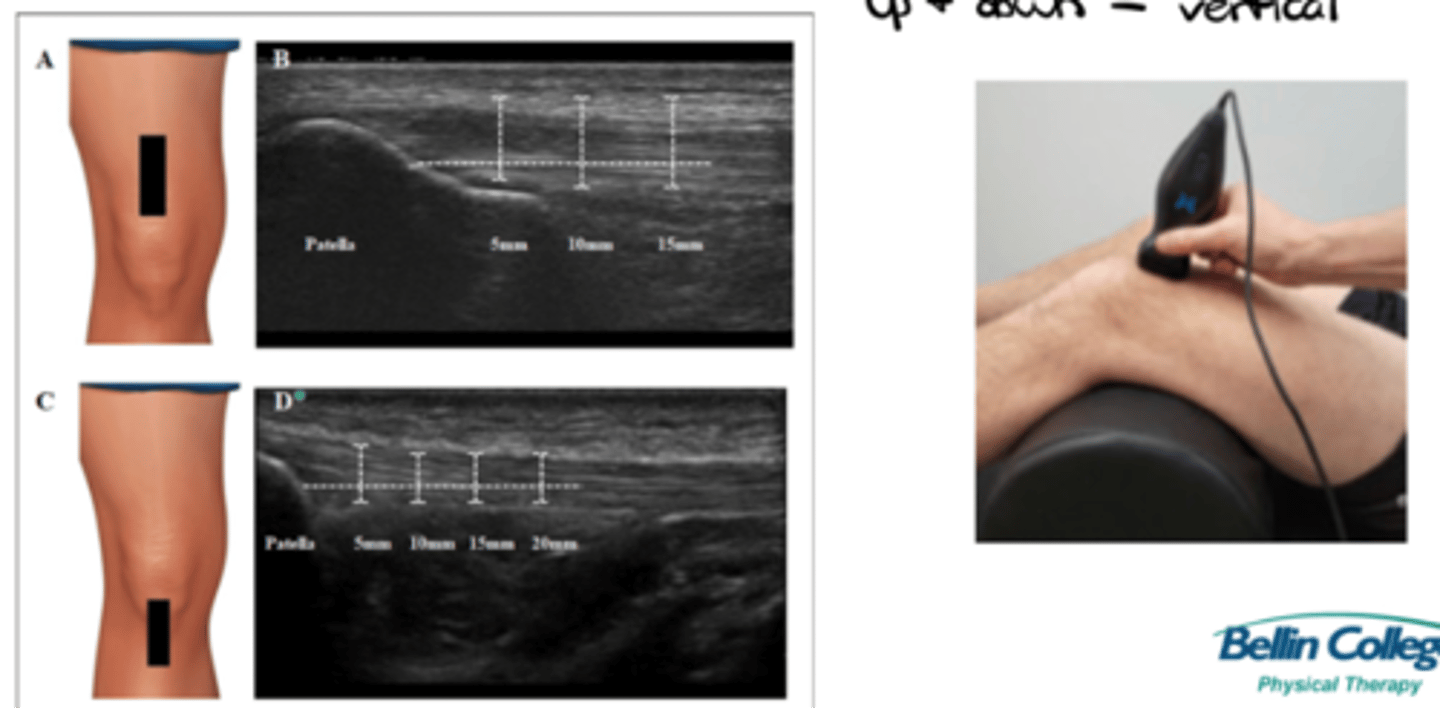
___________: probe orientation that allows for a transverse/horizontal/left & right scan
Short axis
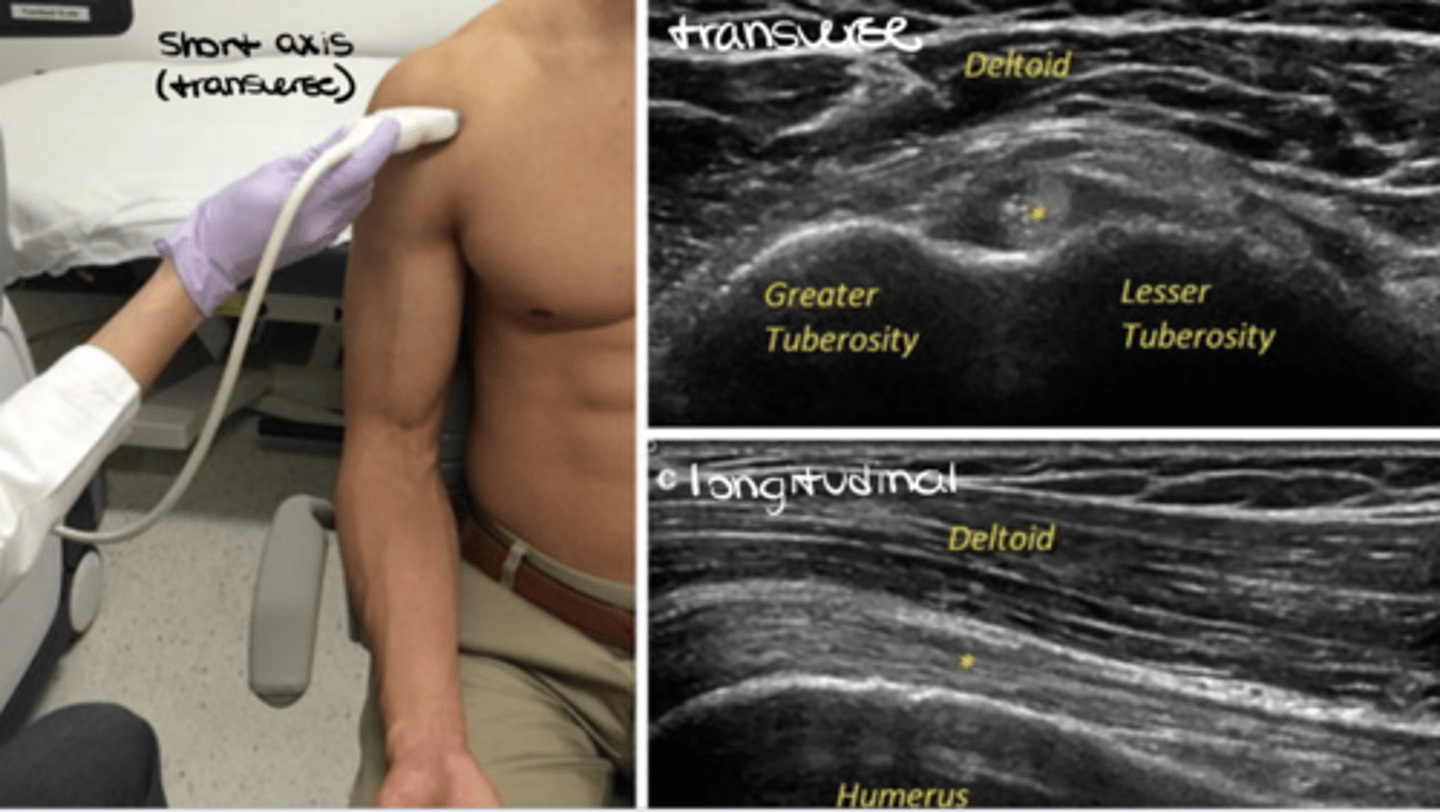
What would a transverse vs. longitudinal ultrasound of the shoulder look like?
See image.
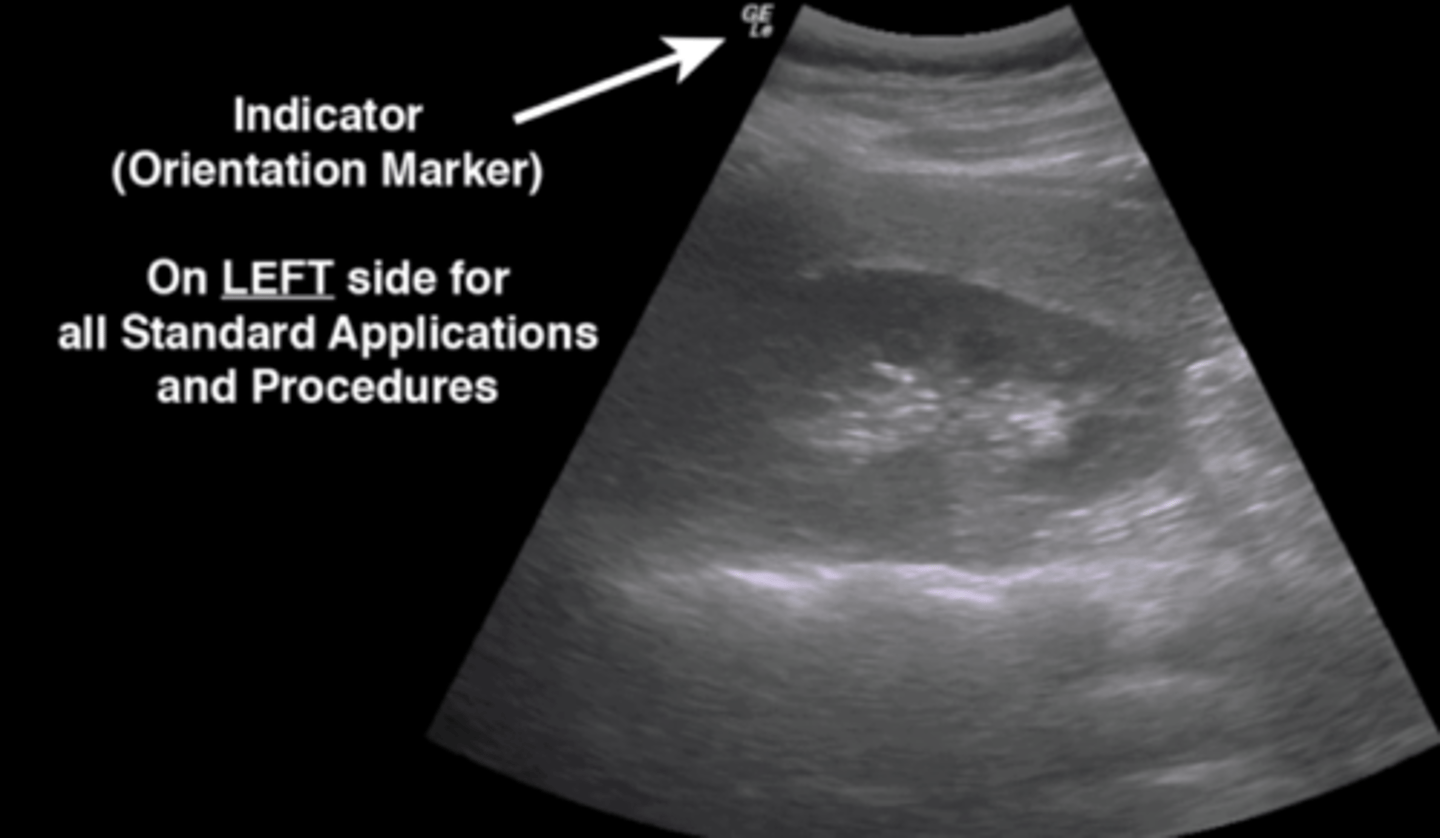
What is the purpose of the indicator on the probe?
Indicator = orientation marker; tells you right vs. left to orient you to the tissues
NOTE: on LEFT side for all standard applications and procedures