Managing steroids in practice
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
38 Terms
2 main scenarios for steroids
steroids to supress inflammatory process A
steroid replacement where body doesnt make enough B
Glucocorticoid properties
regulate carbohydrate,protien and fat metabolism
anti-inflammatory immunosuppressant
mineralocorticoid properties
regulate fluid and electrolyte levels
equivalent anti inflammatory potencies of CCS
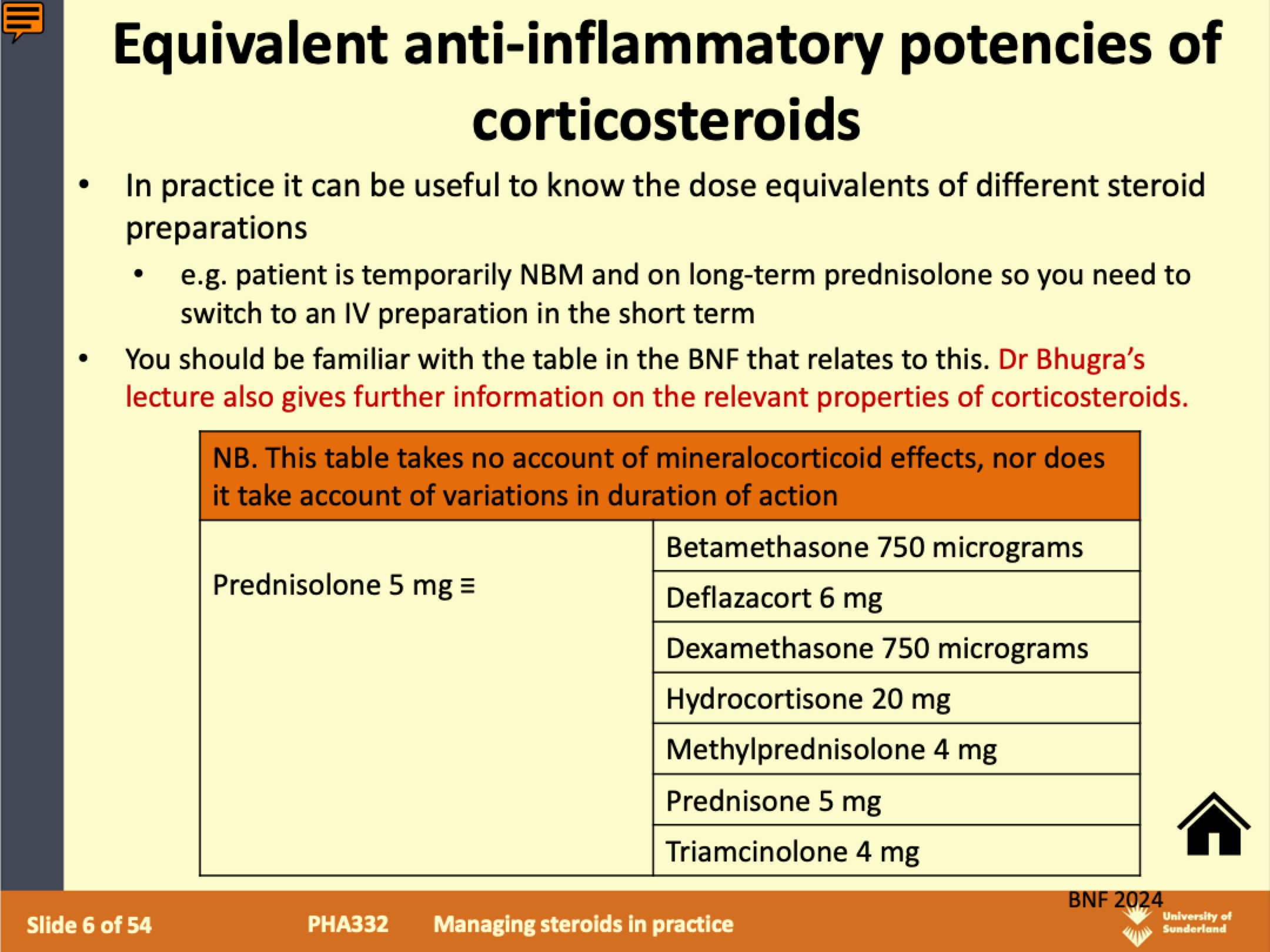
B- psychiological replacement in deficiency states
-chronic adrenal insufficiency
like addisons disease,hypopituitarism,congenital adrenal hyperplasia
do NOT stop steroids in these patients! even if tapered
physiological replacement in chronic adrenal insufficiency
Adrenal cortex normally secretes:
– Cortisol (glucocorticoid activity + weak
mineralocorticoid)
Primary hormone of importance in acute adrenal crisis
– Aldosterone (mineralocorticoid)
Acts to promote reabsorption of sodium and increase
potassium excretion. ...Promotes sodium retention
Deficiency can lead to sodium loss, volume depletion,
hypotension
Note that in hypopituitarism, mineralocorticoid replacement
not required (fludrocortisone) as aldosterone also regulated
by renin-angiotensin system
hydrocortisone steroid replacement of cortisol
Taken orally in chronic conditions
Prescribing should mimic natural cycle of corticosteroid release
Usually 15 – 25mg daily in divided (2-4) doses
Larger dose given in morning (e.g. 10mg OM, 5mg LT, 5mg TT)
Q. Shift workers? Routine or clock?- Given IV or IM in suspected adrenal crisis
fludrocortisone steroid replacement for aldosterone
Potent mineralocorticoid effect in relation to its glucocorticoid
activity
Used to replace aldosterone where the adrenal cortex is destroyed
(Addison's disease)
–50 - 300 micrograms daily in the morning
Also used in management of hypotension due to fluid retaining
properties (unlicensed use)
identification of adrenal insufficiency- ADDISIONS
A ppetite loss, unintentional weight loss, abdominal pain
D iscolouration of the skin (hyperpigmentation in primary insufficiency)
D ehydration
I ncreased thirst and polyuria
S alt cravings
O ligomenorrhoea
N o energy/fatigue/low mood
S ore/weakness in muscles/joints
Patients with adrenal insufficiency may remain well until concurrent illness or times of stress -> decompensate -> adrenal crisis (medical emergency)
adrenal crisis- medical emergency
adrenal glands can’t cope with the demand for extra corticosteroids needed and life-threatening symptoms can develop
acute deterioration in health status with hypotension (systolic
<100mmHg or at least 20mmHg comparative drop) with marked improvement within 1-2h of parenteral glucocorticoids)
symptoms + treatment of adrenal crisis
GI: severe vomiting and diarrhoea, leading to severe dehydration
– Abdominal pain (Abdominal tenderness/guarding)
– Severe muscle weakness/cramps
– Severe drowsiness/fatigue
– Pyrexia
– Dizziness, low BP
– Confusion
– Limb and back pain
– Delirium or loss of consciousness
treatment includes IV fluid and steroids
can lead to hypovolaemic shock, altered consciousness, seizures,
biochemical abnormalities including hyperkalaemia/hyponotraemia,
stroke or cardiac arrest. If left untreated, it can be fatal
patient advice for steroid dependancy
-Lifelong replacement required- do not stop
-Free prescriptions (Addison’s, hypopituitarism- not for general steroid meds)
-Important to renew prescriptions in good time to avoid running out
-Carry extra medications while travelling
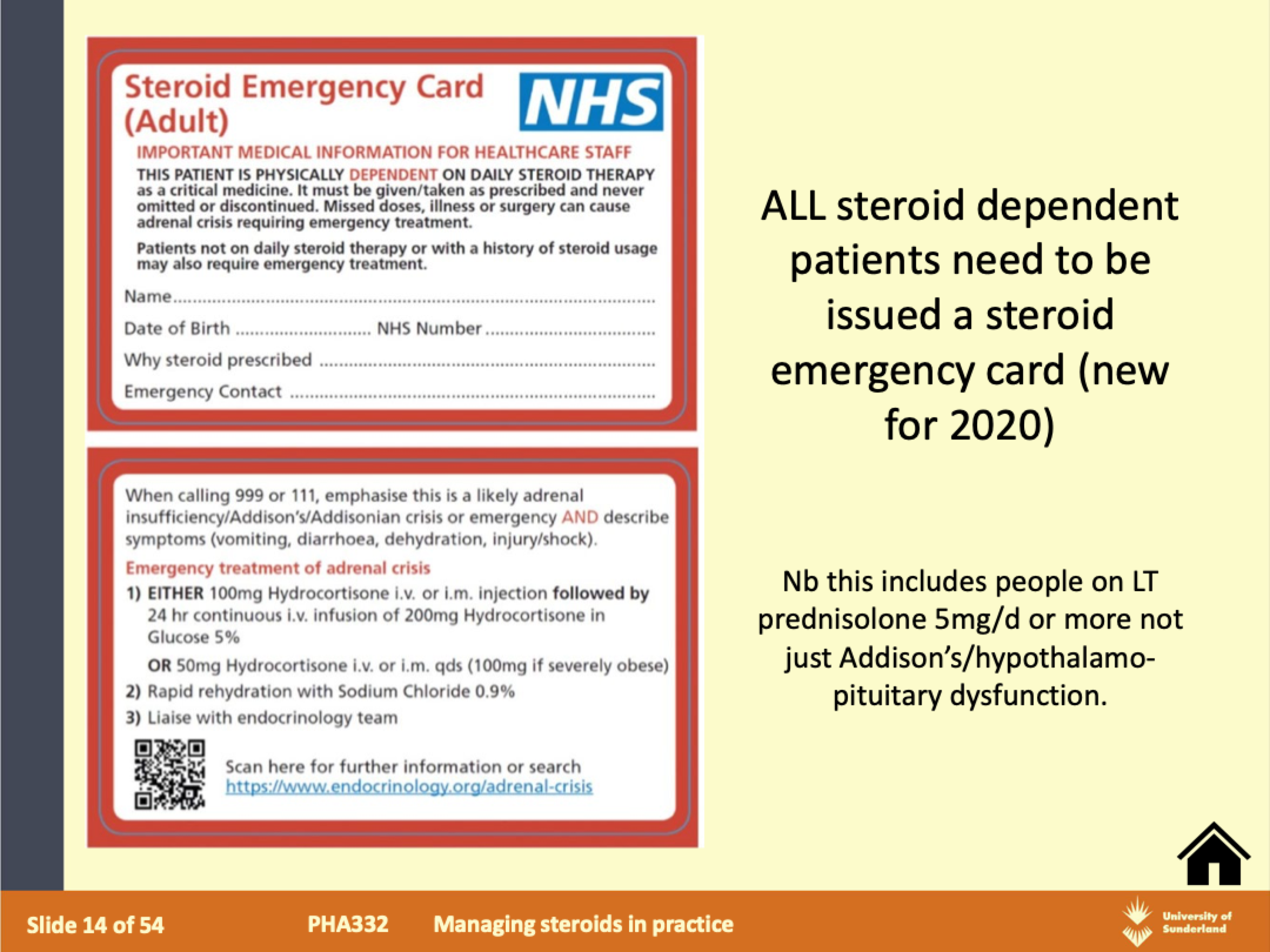
-Steroid treatment card/steroid emergency card/bracelet indicating the diagnosis and replacement therapy should be carried/worn
-Ensure healthcare professionals aware e.g. if undergoing surgery, dental surgery etc
-Discuss long/short-term side-effects due to under or over replacement
-Sick Day Rules
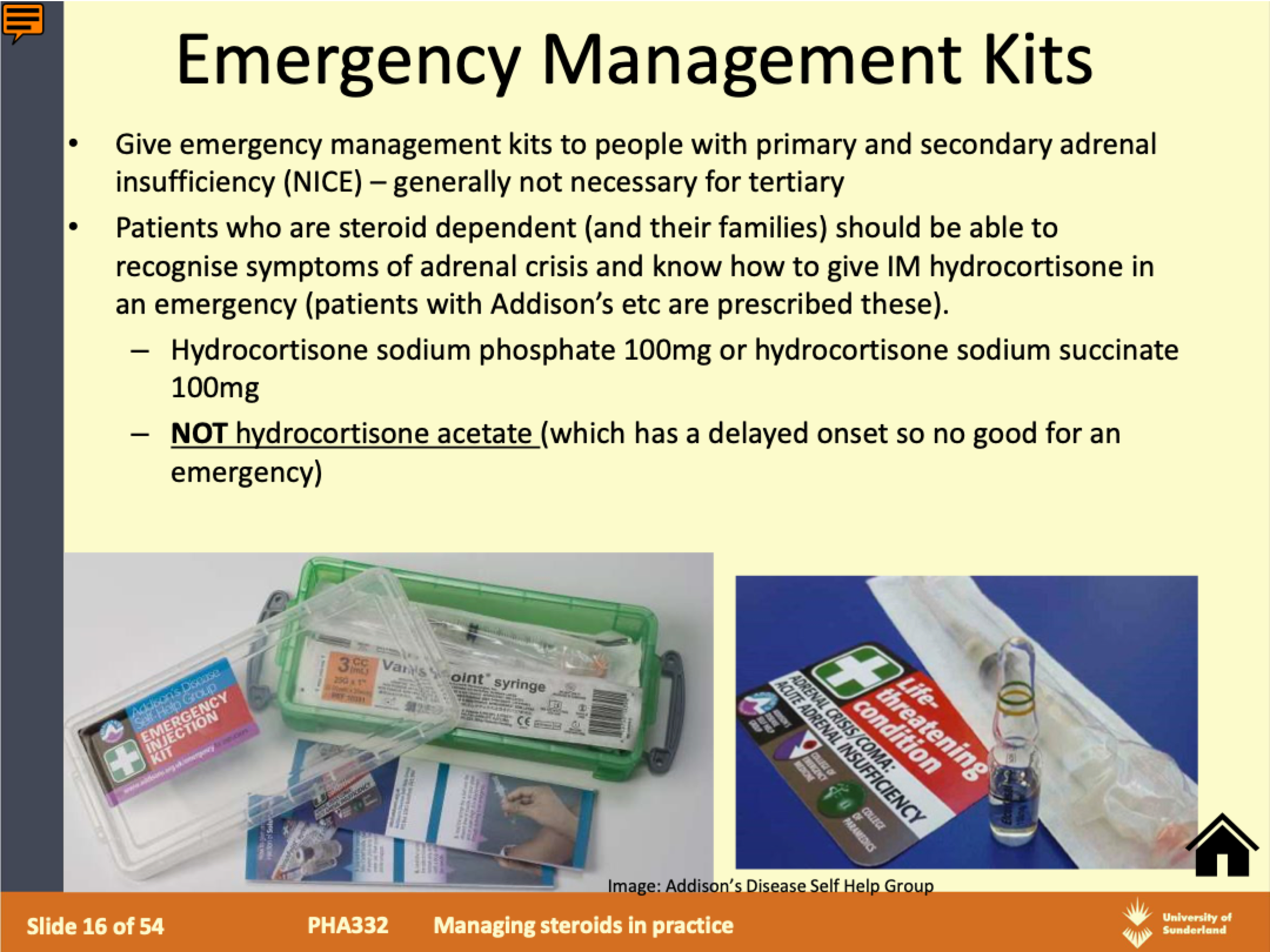
sick day rules for steroid dependant patients
-patient is ill, injured or undergoes strenuous exercise-important that corticosteroid cover is increased to reduce the risk of adrenal crisis
-Patients may have individualised plan on how to do this w specialist team, and guidelines differ (!) but generally...
– Increase steroid dose (short periods)
– Some guidelines suggest double dose
NICE: Offer at least 40mg hydrocortisone daily in 2-4 divided doses (or if on prednisolone at least 10mg oral prednisolone 1-2 divided doses)
-Vomiting illness can be dangerous- further dose if vomit within 30 min, if
more vomiting emergency hydrocortisone injection and seek immediate
medical attention
glucocorticoid therapy A examples
Respiratory diseases
– inhaled and systemic
Rheumatoid arthritis.
Osteoarthritis (injection)
Intestinal diseases
– ulcerative colitis, Crohn’s disease, coeliac disease
Collagen diseases
– systemic lupus, polyarteritis nodosa,, nephrotic syndrome, glomerulonephritis
Malignancies
Organ transplantations and skin allograft
Eye diseases
– as eye drops or ointment in allergic conjunctivitis, iritis, keratitis.
skin diseases:
– topically in many exzematous skin diseases
Cerebral oedema
– due to tumours, meningitis
Severe allergic reactions
Autoimmune diseases
– haemolytic anaemia, thrombocytopenia, active chronic hepatitis
withdrawal of oral corticosteroids: taper when
>3 weeks any dose
>40mg prednisolone (or equivalent) for more than 1 week
Multiple recent repeated courses
Short course within a year of stopping a long course
Been given repeat doses in the evening
what does slow tapering or oral corticosteroids involve:
decreasing the steroid dosage e.g. by the equivalent of 2.5-5 mg of prednisone every three to seven days until the physiologic dosage is reached (7.5mg prednisolone widely quoted, 3-5mg of prednisone
NICE).
– then a more gradual reduction of prednisolone e.g. 0.5-1mg every 2 to 4 weeks
– Other examples of tapering e.g NICE
short term side effects of corticosteroids
insomnia
mood disturbances
GI disturbances
long term side effects
same as short course +
increased susceptibility to infection
Osteoporosis
Adrenal suppression
Cushingoid state (see Dr Bhugra’s lecture)
Diabetes
Ocular effects (cataracts/glaucoma)
Skin changes e.g. thinning, easy bruising
GI ulceration
Growth retardation
Hypokalaemia
Fluid retention
MHRA alert 2017: Patients should be advised to report any blurred vision or other visual disturbances if on corticosteroids (any route)
cautions of corticosteroids
Children and Adolescents
Elderly
Recent cardiovascular disease
Chronic heart failure
Peptic ulcer
Diabetes mellitus
Pregnancy
Osteoporosis
Psychosis
Epilepsy
Renal failure
Glaucoma
contra indications of corticosteroids
Systemic Infection (unless specific therapy given)
Avoid live virus vaccines
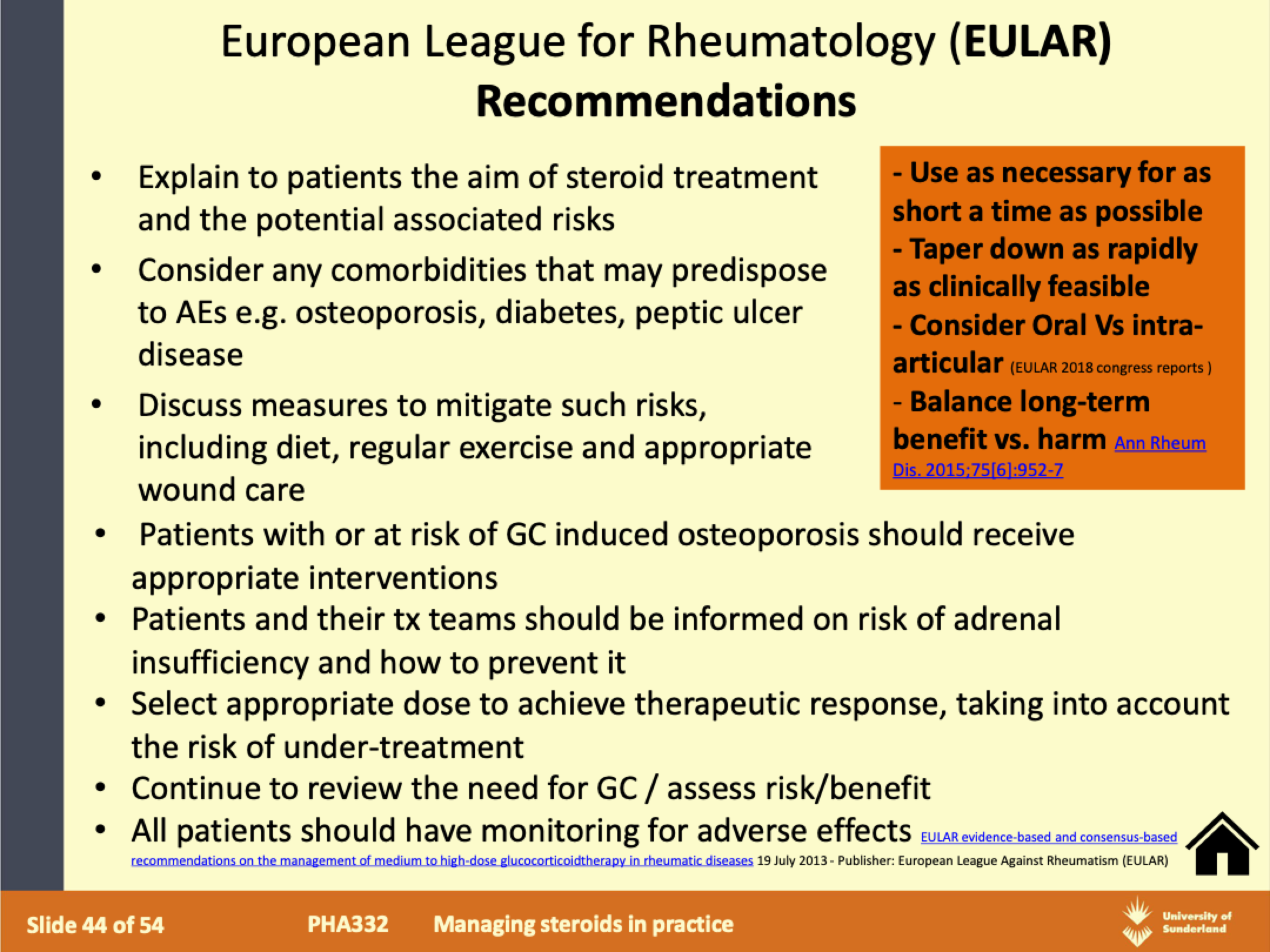
how to minimise side effects of steroids
Morning dosage (to avoid insomnia)
Minimise duration of course
Consider local application wherever possible
Alternate day dosing?
Appropriate Supportive therapies
– PPI for prophylaxis of GI irritation
– Bisphosphonates for prevention of osteoporosis (where appropriate)
monitoring long term side effects of corticosteroids
Body weight
Growth charts children
Blood pressure
Signs of oedema
Lipid levels
Glucose levels
Ocular pressure
Cardiac insufficiency
Bone Mineral Density/ FRAX
Any signs/symptoms e.g. peptic ulcers, fractures etc
diabetes and steroids
can worsen blood glucose
-Steroid induced hyperglycaemia (pre-existing diabetes)
-Steroid induced diabetes (no previous diagnosis of diabetes- may resolve or may not)
risk factors for hyperglycaemia w steroids
Existing diabetes
Risk factors for diabetes e.g. family hx, obesity or ‘pre-diabetes’
Previous hyperglycaemia with steroids
Usually results in rise in blood glucose 4-8 hours post oral steroid,
and may improve 24 hours after discontinuation.
increased monitoring of blood glucose should take place
May involve initiation or adjustment of oral antidiabetic agents or insulin therapies depending on severity of hyperglycaemia
surgery and steroids
likely to increase the steroid requirement as it is a time of physiological stress
Ensure anaesthetist is aware of patients steroid history
Depending on the time and extent of surgery, adjustments may need to be made to the patients usual steroid dose (if pt likely to have a degree of
adrenal suppression e.g. LT steroids)
may involve increasing the usual steroid dose/ IV steroids peri-operatively
– Hydrocortisone often given during surgery
– E.g. Just before anaesthesia 100mg IV or IM hydrocortisone and every 6 hours during operation (or continuous IV hydrocortisone infusion) and until eating and drinking.
Glucocorticoid induced osteoporosis
Rate of bone density loss highest at start of steroid treatment
Continued slower reduction with long-term use
Consider patients overall fracture risk (tools e.g. FRAX®) and take into account amount of steroid use
Consider DXA scan
If high risk don’t delay, start bone protection therapy (usually bisphosphonate +/- calcium and vitamin D)
High dose ICS can also potentially increase risk
Pregnancy and breastfeeding effects w corticosteroids
risk benefit analysis
variable ability of corticosteroids to cross placenta
• Betamethasone and dexamethasone readily cross placenta
• 88% prednisolone inactivated as crosses the placenta
– No significant evidence that systemic corticosteroids cause
congenital abnormalities
– Increased risk of intra-uterine growth restriction with
prolonged or repeated administration
– Adrenal suppression in neonate resolves spontaneously
after birth
– Small amounts found in breast milk but maternal doses up
to 40mg prednisolone unlikely to cause systemic effects in
infant
drug intercations of corticosteroids
no major interactions
Avoid concurrent use of other ulcerogenic agents where possible eg NSAIDS
Enzyme Inducers:
– Barbiturates, phenytoin, carbamazepine, and rifampicin may reduce the serum concentration of oral corticosteroids.
Cholestyramine:
– Inhibition of GI absorption of oral corticosteroids with cholestyramine and other binding agents. Doses of oral corticosteroids and cholestyramine should be separated
patient advice for corticosteroids
provided with a PIL
Advise how to take
– Single dose (if once daily) e.g. 30mg would be 6 x 5mg tablets taken
together
– After breakfast (if OD) – this reduces risk of insomnia and GI adverse
effects (but use pt friendly language!)
– Advise on most likely side-effects and tailor to short vs long-course
conducted in patient friendly language, tailored to situation whether they are taking LONG-term or SHORT- term therapy
advice to patients-mood changes
– Confusion, irritability, delusions and suicidal thoughts
– Usually associated with higher doses and occurs early in treatment or when being withdrawn
– Seek medical advice if any concerning psychological changes occur
Advice to patients (long-term/cases where tapering needed)
Steroid emergency card
Increased susceptibility to infections
– Avoid contact with people with chickenpox or measles unless already immune
– (Serious infections may go unrecognised)
Suppression of normal adrenal function
– Avoid abrupt withdrawal of long-term treatment (greater than 3 weeks)
– Inform healthcare professional about corticosteroid use when receiving treatment for any illness or injury
Additional corticosteroid treatment may be required
– Effects can last up to a year after withdrawal of corticosteroid
– Inform any healthcare professional providing treatment that patient prescribed steroids
Intra-articular steroid injection
inflammatory arthiritis to provide relief
e.g. Triamcinolone; methylprednisolone; dexamethasone.
Insoluble/long-acting steroid remains in the joint, contact with inflamed synovial surface, taken up by synovial cells absorbed into blood stream
similar side effects but less chance
local Side-effects
– Post-injection flare of pain, skin depigmentation, bleeding, infection
Prolonged steroid injection is associated with osteonecrosis
Limit on frequency
Injection should be given by trained personnel
rectal administration of steroids
Enemas or suppositories e.g. prednisolone in IBD affecting lower parts of the colon and rectum
IBD Budesonide sometimes given (oral)
– High first pass metabolism (liver) so limiting systemic exposure
– Fewer side-effects but less effective for flares
topical corticosteroids
indications:
Inflammatory condition of the skin other than infection.
E.g. eczema, contact dermatitis, insect sting, eczema of scabies
Contraindications: infection (bacteria/viral/fungal) unless
concomitant treatment e.g. antibiotic/antifungal, rosacea
BNF:
Potency grouped as Mild/Moderate/Potent/Very Potent- need
to add to dispensing label (find in BNF)
Use appropriate strength for the shortest possible duration
Ointments or creams?
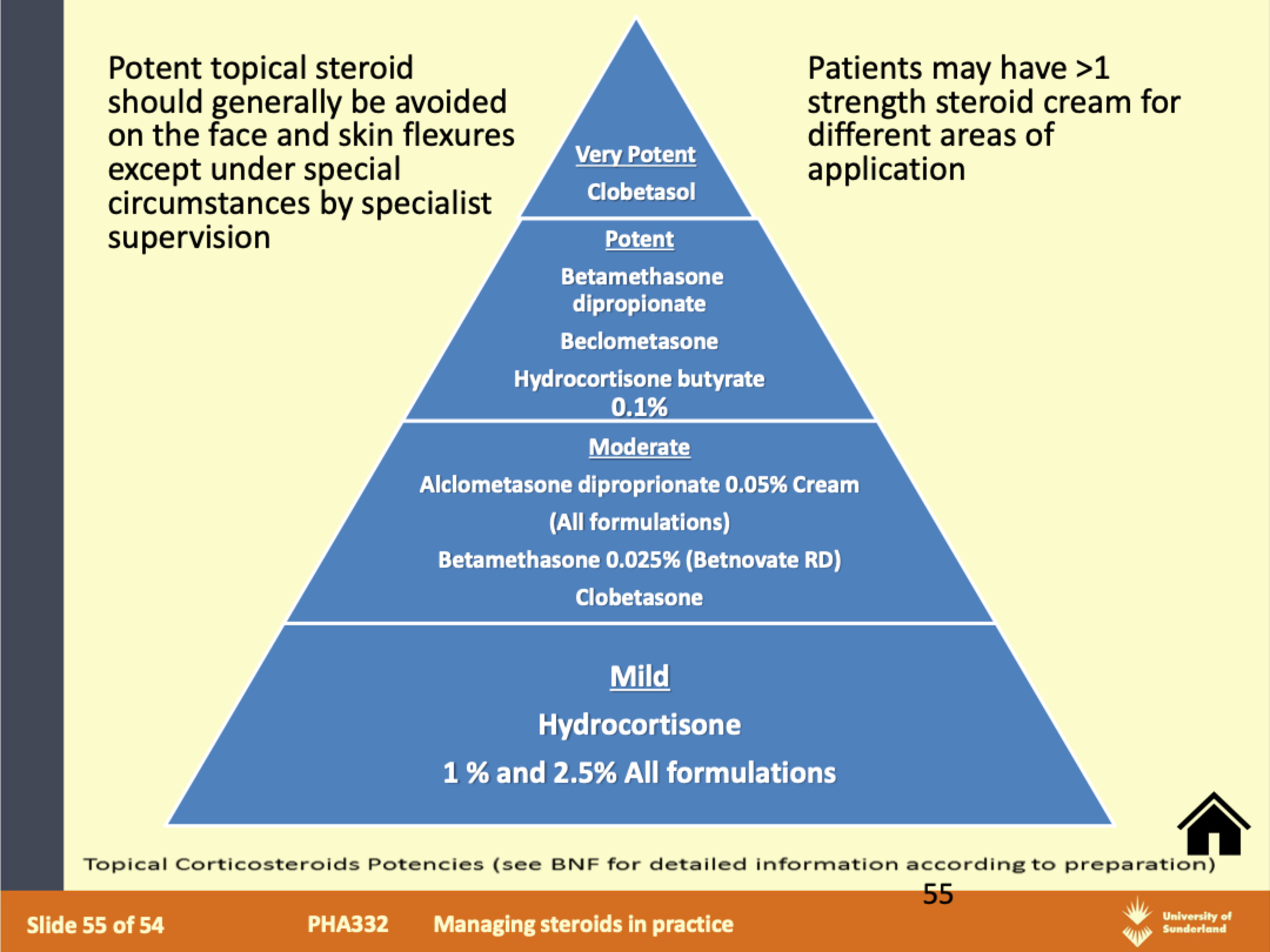
application of topical steroids
specific counselling
Finger tip application
– Enough for twice size of adult palm+fingers
– Details in BNF
No more frequently than twice daily (once daily normally sufficient) apply thinly to the affected area only
Use the least potent formulation which is fully effective
Avoid prolonged use on the face and keep away from eyes
Caution in children and during pregnancy
Suppression of pituitary adrenal axis and even cause Cushing’s syndrome with prolonged use in large area (some systemic absorption) but generally
less side-effects than oral preparations.
side effects w topical steroids
Spread/worsening of untreated infection (do not use on infected skin unless specific treatment for infection given alongside)
Thinning of skin with long-term use
Contact dermatitis
Perioral dermatitis
Acne, worsening of acne rosacea
Depigmentation
Hypertrichosis
Systemic effects
Topical steroid withdrawal reactions
TSW -topical steroid withdrawal
rare
Reactions reported when stopping treatment following long-term use of moderate or stronger potency topical steroids
– Usually starts a few days after stopping steroid
– Burning, red, stinging, can be oozy, then dry/itchy with shedding
– Can spread beyond the initial treatment area
– May be more sensitive and may have flares before fully recovers
– Can take weeks or years for skin to fully recover
Treatment: discontinue steroid (taper?), emollients, cold compresses, antihistamines, analgesia, psychological support, may need other specific treatment
Minimising risk of TSW
-Reducing frequency and potency once skin clears
-Avoid continued use of mod: potent topical steroids on face
-Minimise continuous prolonged steroid duration
-Reduce topical steroid potency and application from daily to twice weekly after 2-4 weeks of use.
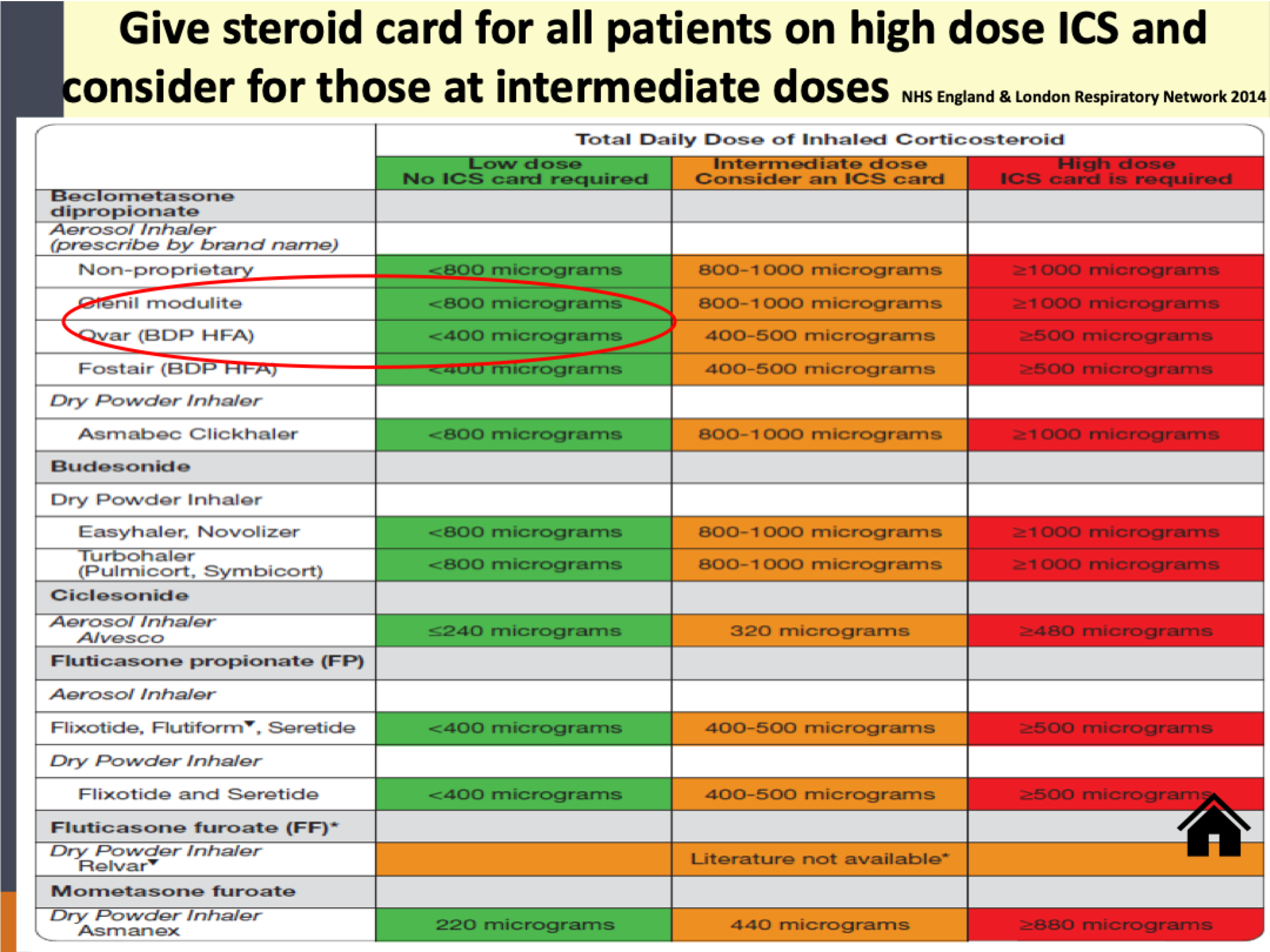
ICS
most effective preventer drug
and are safe and effective at standard doses
– Counselling on inhaler technique
– Consider range of devices available
– Counselling on avoiding candidiasis infection
Rinse mouth out after using
Risk of systemic effects, at high doses:
– Adrenal suppression
– Reduced bone mineral density
– Growth retardation (monitor growth in children)
– Lower respiratory tract infections
always check patient adherance! inhaler technique, smoking cessation etc before increasing ICS dose