1. Cell Injury and Host Defenses
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
37 Terms
Etiology
bottom line cause that starts the disease process
Pathogenesis
stepwise changes that occur in disease development
Manifestations
Morphologic manifestations (changes seen in tissue due to disease), clinical manifestations (changes seen in pt due to disease): signs and symptoms
Three patterns of response to stress an noxious stimuli:
Adaptaiton
occurs in the setting of low level but persistent stress or pathologic stimulus
the cell has time and opportunity to change its functions in order to meet the demands of the new situation
allows function to continue; this is a change and live strategy
potentially reversible
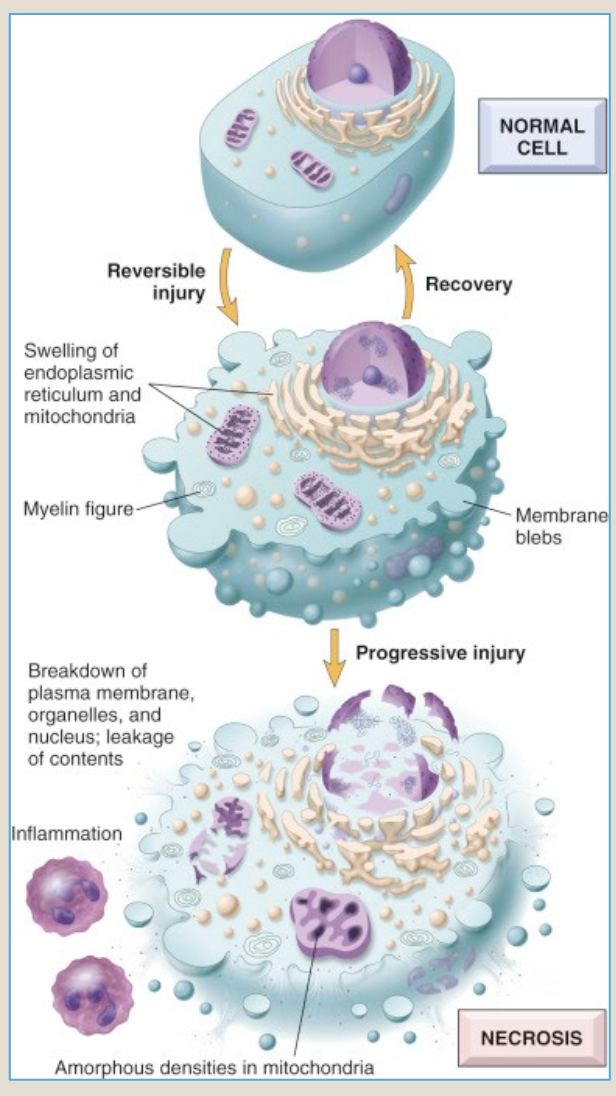
Three patterns of response to stress an noxious stimuli:
Reversible injury
occurs in several circumstances
when the adverse stimulus is of sudden onset and increases sharply, hence there is no time to utilize adaptive strategies
when no adaptive response is possible due to severity or nature of the stress
when the adaptive capability of the cell is exceeded
Cell injury will compromise cell integrity and/or function
cell injury may be reversible, leading to recovery of function, or the cell may die
Three patterns of response to stress an noxious stimuli:
Cell Death = Irreversible Injury
Occurs when the cell cannot cope with severe acute stress that is rapid in onset and/or persistent stress
The injury passes the point of no return
In cell death, the injury is irreversible and there is TOTAL loss of cell function
Causes of cell injury:
Oxygen deprivation = Hypoxia
Oxygen deficiency such that there is compromised aerobic oxidative respiration
ischemia: hypoxia due to local loss of blood supply
loss of oxygen supply
lung and/or airway disease causing inadequate oxygenation of blood
anemia: decreased oxygen- carrying capacity of the blood
Causes of cell injury:
Work overload
metabolic demands may outstrip blood supply
metabolic activity may create harmful intracellular contitions
Causes of cell injury:
Physical agents
trauma
extremes of temp
radiation
electrical shock
sudden changes in atmospheric pressure
Causes of cell injury:
chemicals
including poisons, toxins and medications
affect vital functions of the cell in various ways such as altering cell membrane permeability or compromising enzymes
Causes of cell injury:
Infectious agents
bacteria, viruses, fungi and parasites may all cause injury
mechanisms of injury by biologic agents are diverse
Causes of cell injury:
Immunologic reactions
Immune reactions to exogenous antigens, such as anaphylaxis
loss of self-tolerance resulting in autoimmune diseases
Causes of cell injury:
Genetic defects
may be inherited or acquired
may result in gross physical defects of subtle intracellular alterations
may involve a gross defect in chromosomal material or only a point mutation at a molecular level
tumors, both benign and malignant, arise due to genetic defects in cellular growth and differeations
Causes of cell injury:
Nutritional imbalances
protein- calorie deficiency
vitamin and mineral deficiencies
nutritional excesses
Cellular adaptations to stress:
Hypertrophy
increase in the size of cells
increases cell size is due to larger numbers of organelles and other cellular components
allows cell to reach new equilibrium with metabolic demands
caused by:
increased functional demand (increased workload)
hormonal stimulation
growth factor stimulation
example: cardiac hypertrophy secondary to hypertension or valve dysfunction
Cellular adaptations to stress:
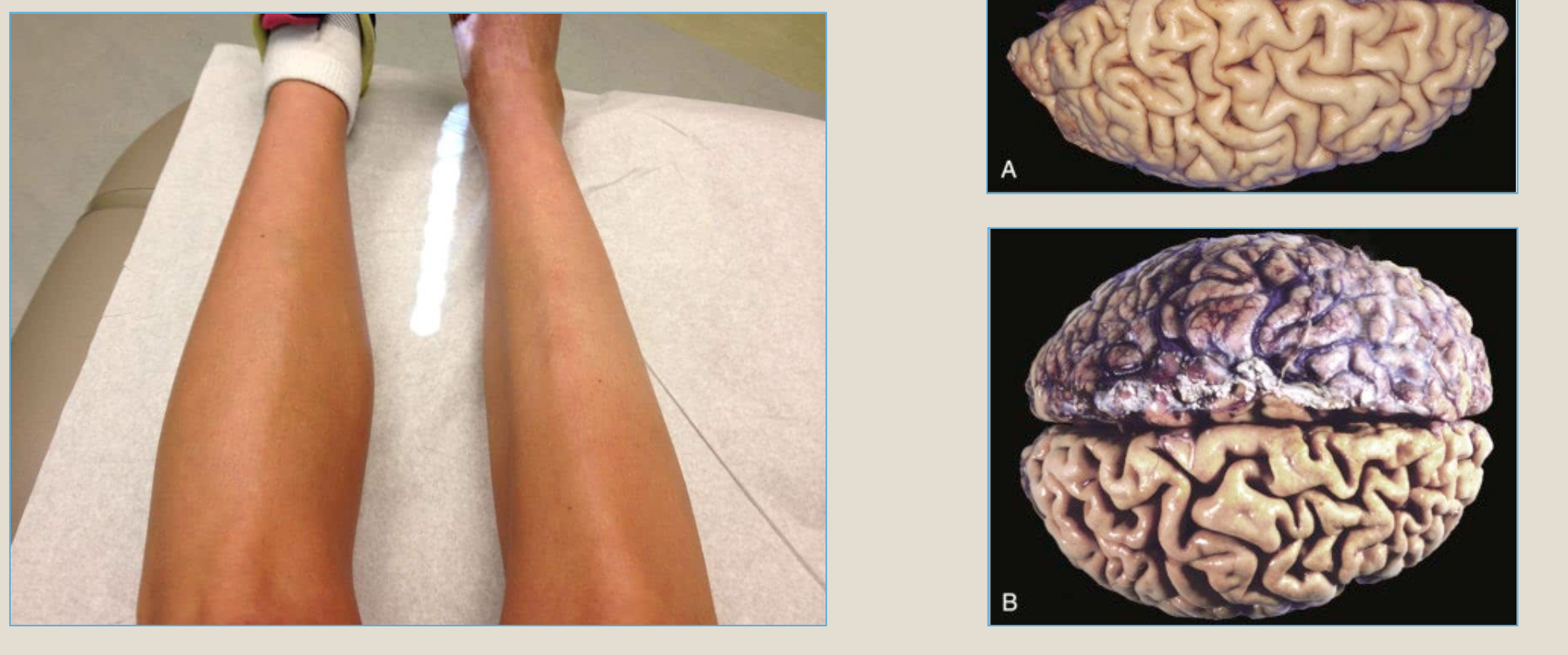
Atrophy
shrinkage in the size of a cell due to loss of cell substance
caused by:
decreased workload - immobilization
loss of innervation
diminished blood supply
inadequate nutrition
loss of endocrine stimulation
allows cell to survive in adversity by operating at a lower level of function
Cellular adaptations to stress:
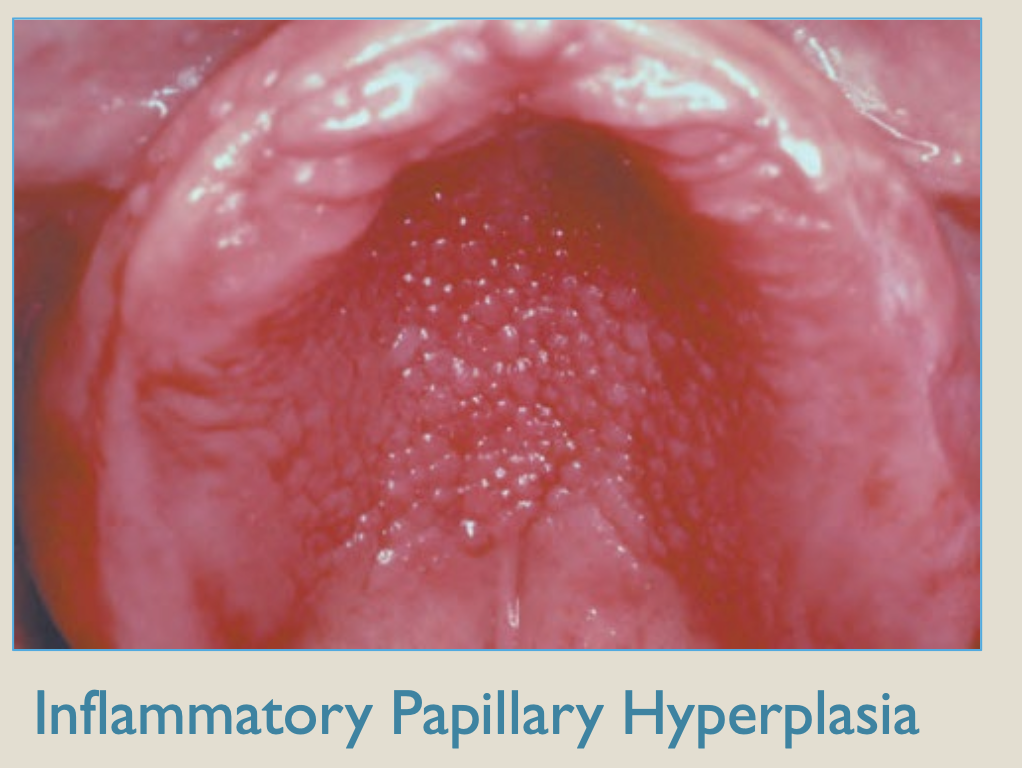
Hyperplasia
increase in the number of cells in an organ or tissue
proliferation change
often in response to the same physiological stresses or pathological stimuli as hypertrophy and may even occur concurrently in tissue capable of cell division
Cellular adaptations to stress:
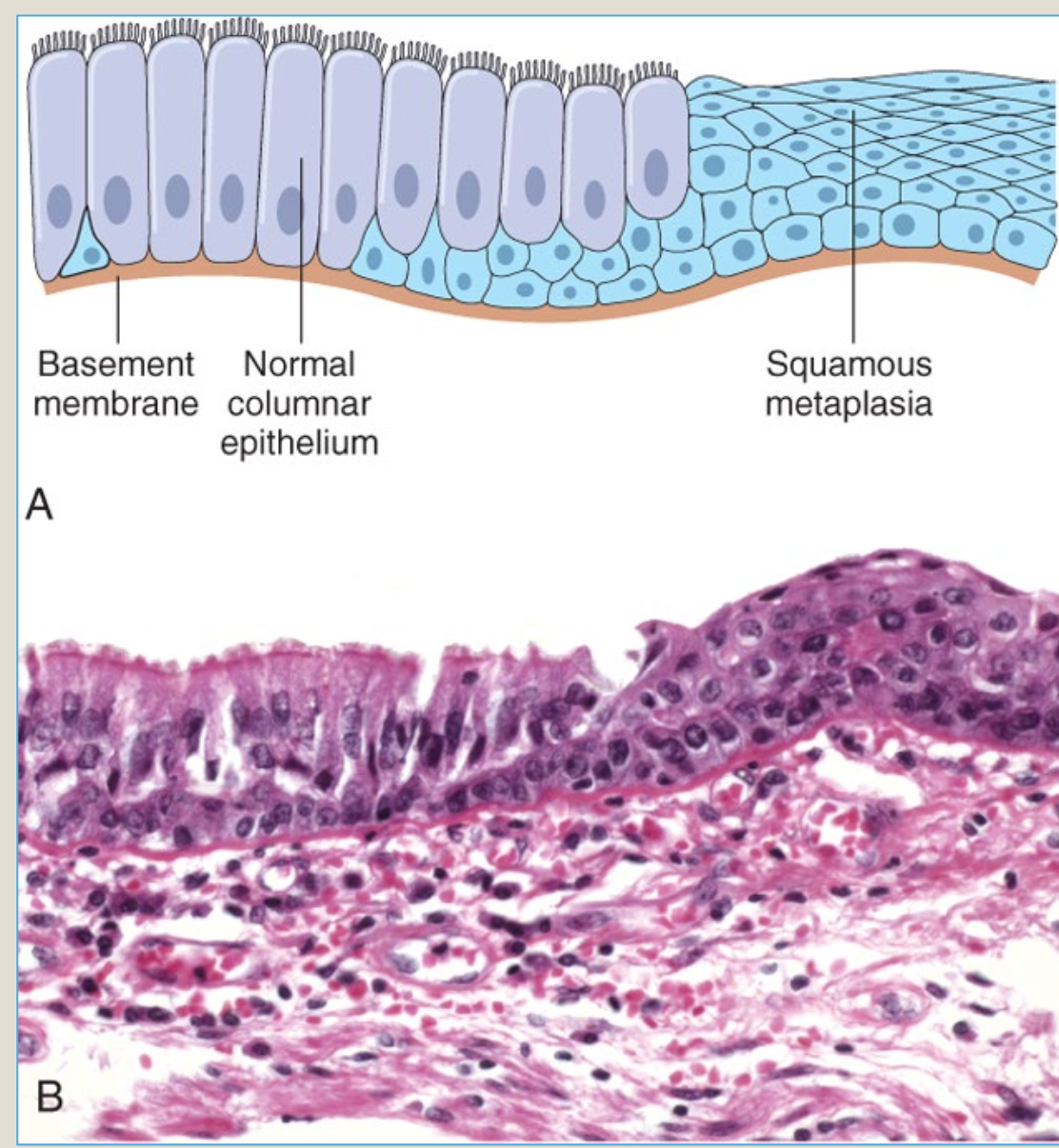
Metaplasia
change in cell differentiation form one adult cell type to another adult cell type
confers better protection in the setting of a noxious environment
most commonly involves epithelium
ex: squamous metaplasia
respiratory epithelium transforms into stratified squamous epithelium in response to long term assault by cigarette smoke
further assault by carcinogens in smoke may transform these squamous epithelial cells into cancer cells
Cellular adaptations to stress:
Hyperkeratosis
production of excess keratin on epithelial surfaces
bolsters the surface barrier and protects the tissues beneath
may also be caused by genetic damage affecting epithelial cell growth and differentiation
Reversible cell injury:
Cellular swelling
most common morphological pattern
injury affects plasma membrane integrity and/ or sodium pump function of the cell membrane
Sodium flows into cell, water follows, cytoplasm fills up with water
whole cell swells
many organelles within the cell may also take on excess water and swell
Reversible cell injury:
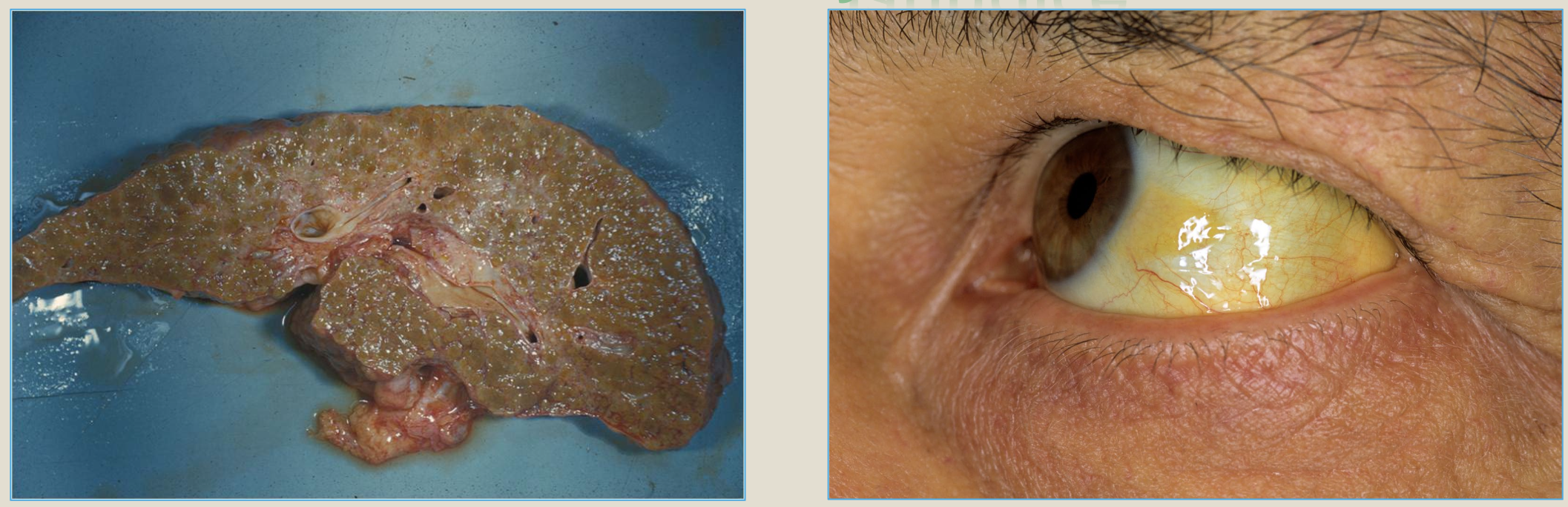
Fatty change
much less common than cellular swelling
occurs in cells involved in fat metabolism: liver, heart, and kidneys
injury causes accumulation of simple lipid within cells
may appear as small or large fat vacuoles of triglycerides
Necrosis
cell death as the consequence of cellular injury that has become irreversible
cell injury passes the “point of no return”
the usual and customary mode of cell death
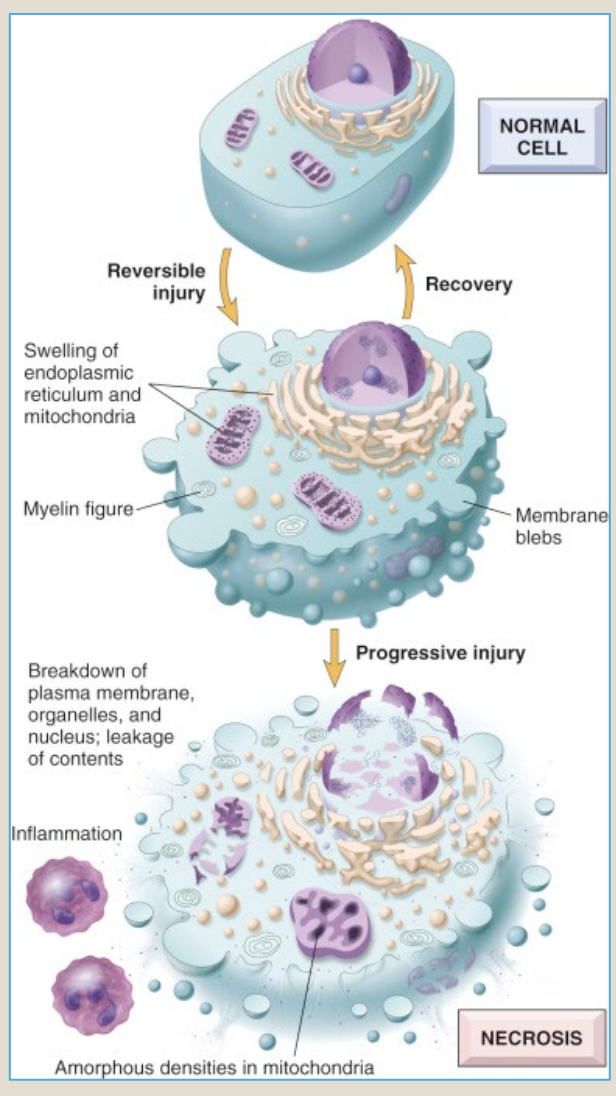
Necrosis = Irreversible cell injury
a sequence of morphologic changes that accompany cell death in cells that have sustained a lethal injury
enzymatic digestion of the cell
denaturation of proteins
nuclear hallmarks
karyolysis: fading of the nucleus
pyknosis: shrinkage and darkening of the nucleus
karyorrhexis: fragmentation of a pyknotic nucleus
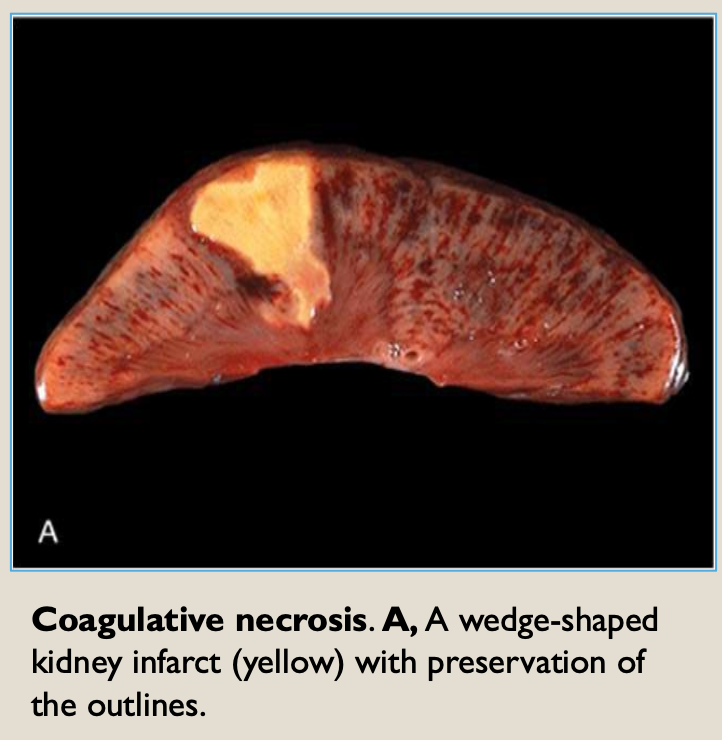
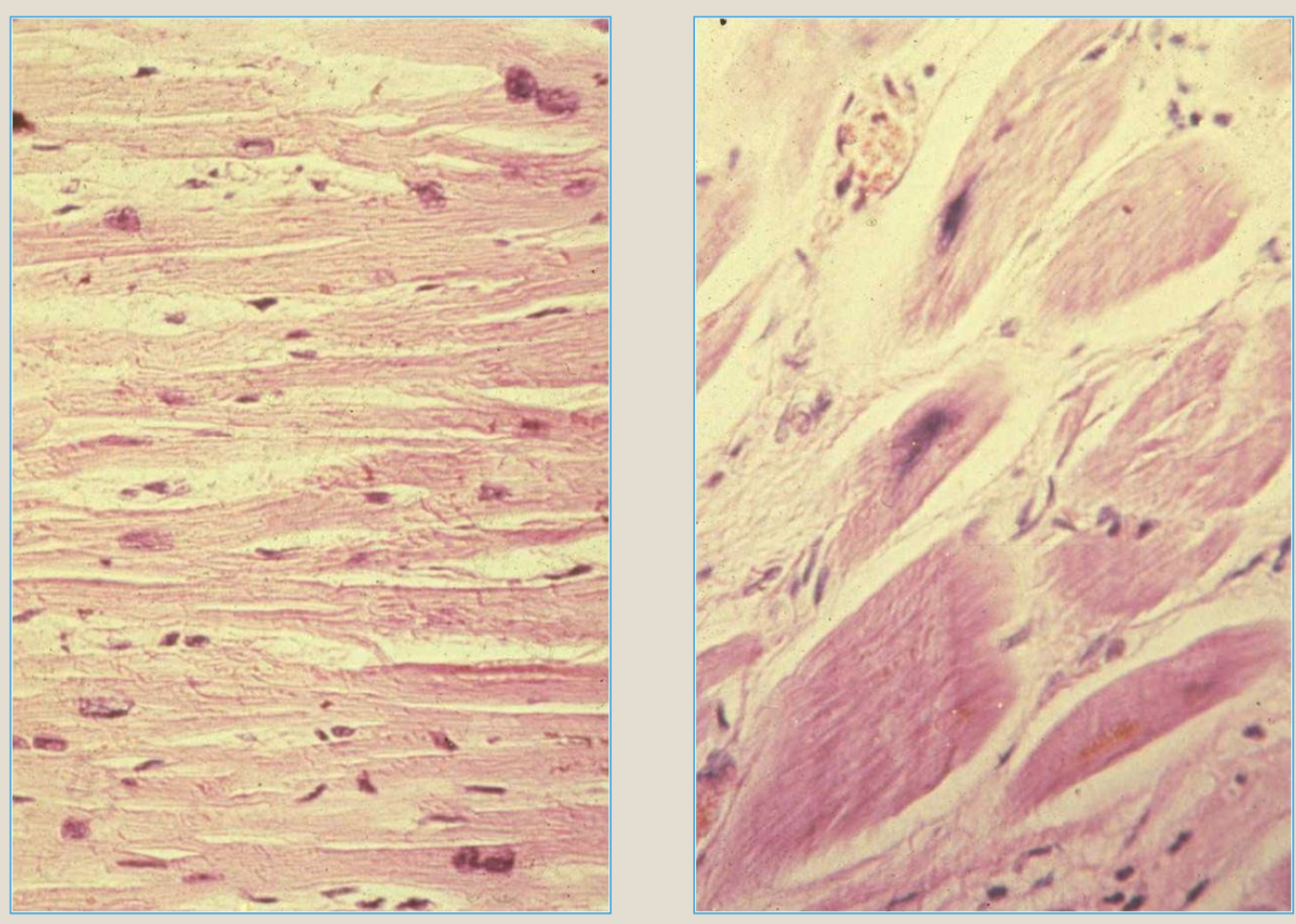
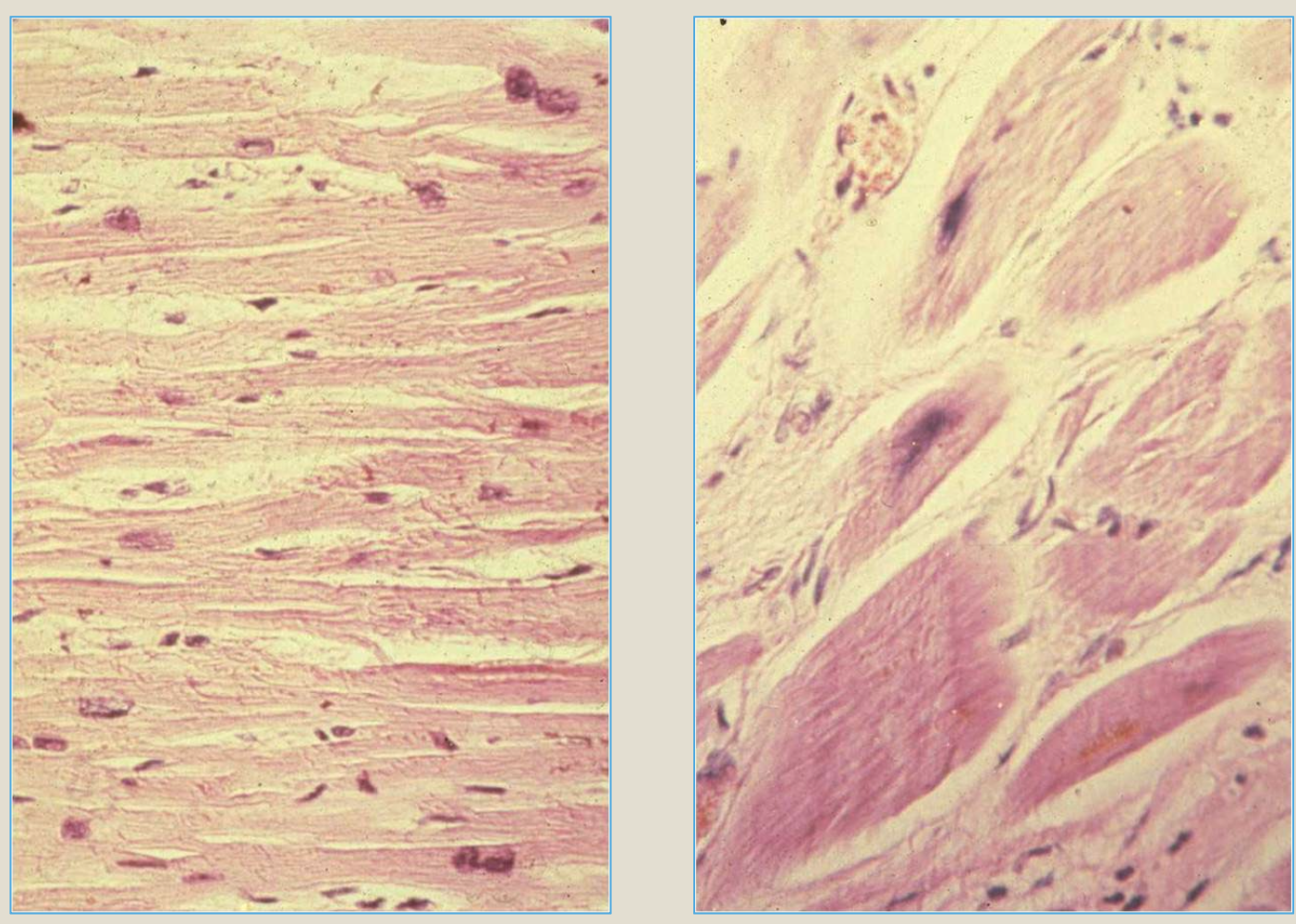
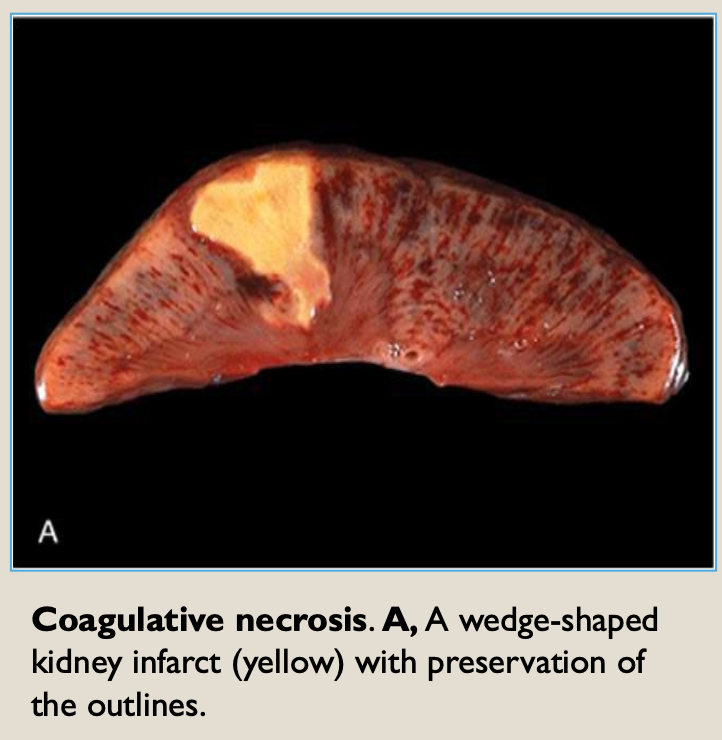
Coagulative Necrosis
denaturation of proteins dominates
basic outline of cell is preserved
characteristic in hypoxic cell death of all tissues, except CNS
ex: myocardial infarction: necrosis of cardiac muscle cells due to irreversible ischemic injury
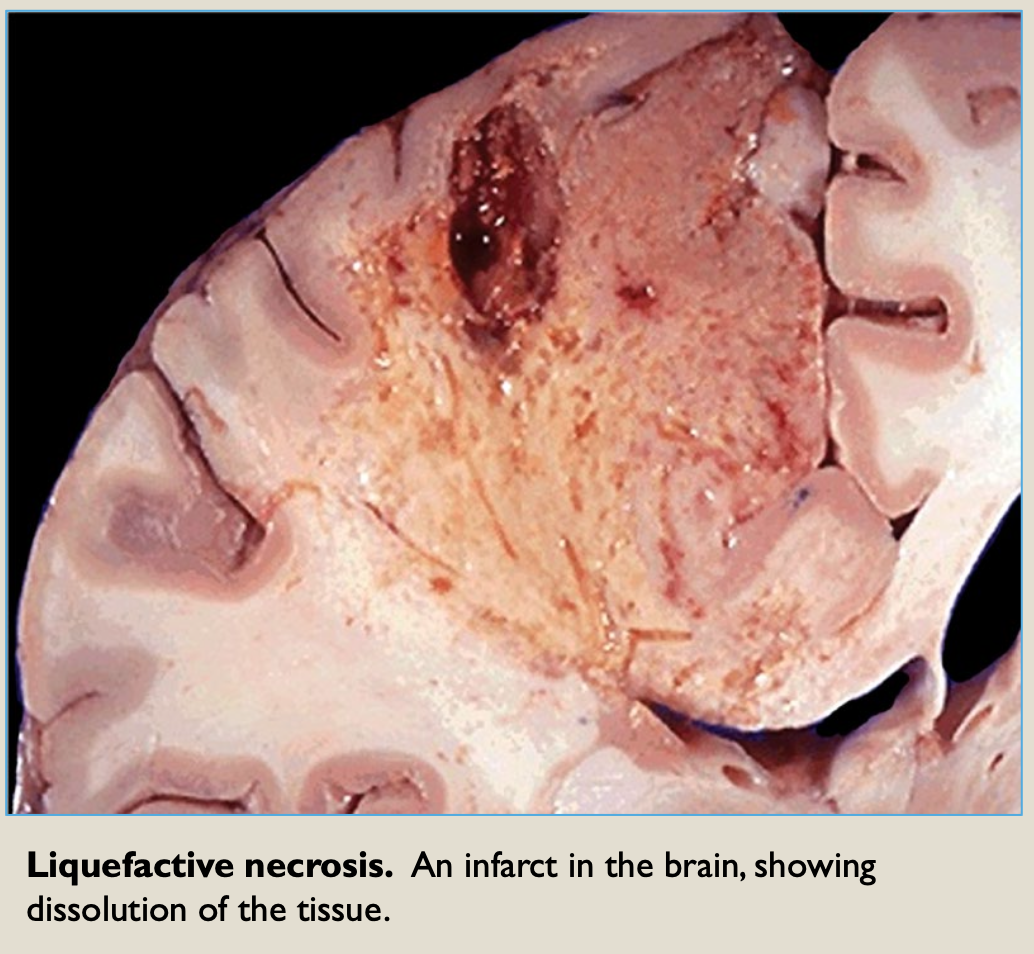
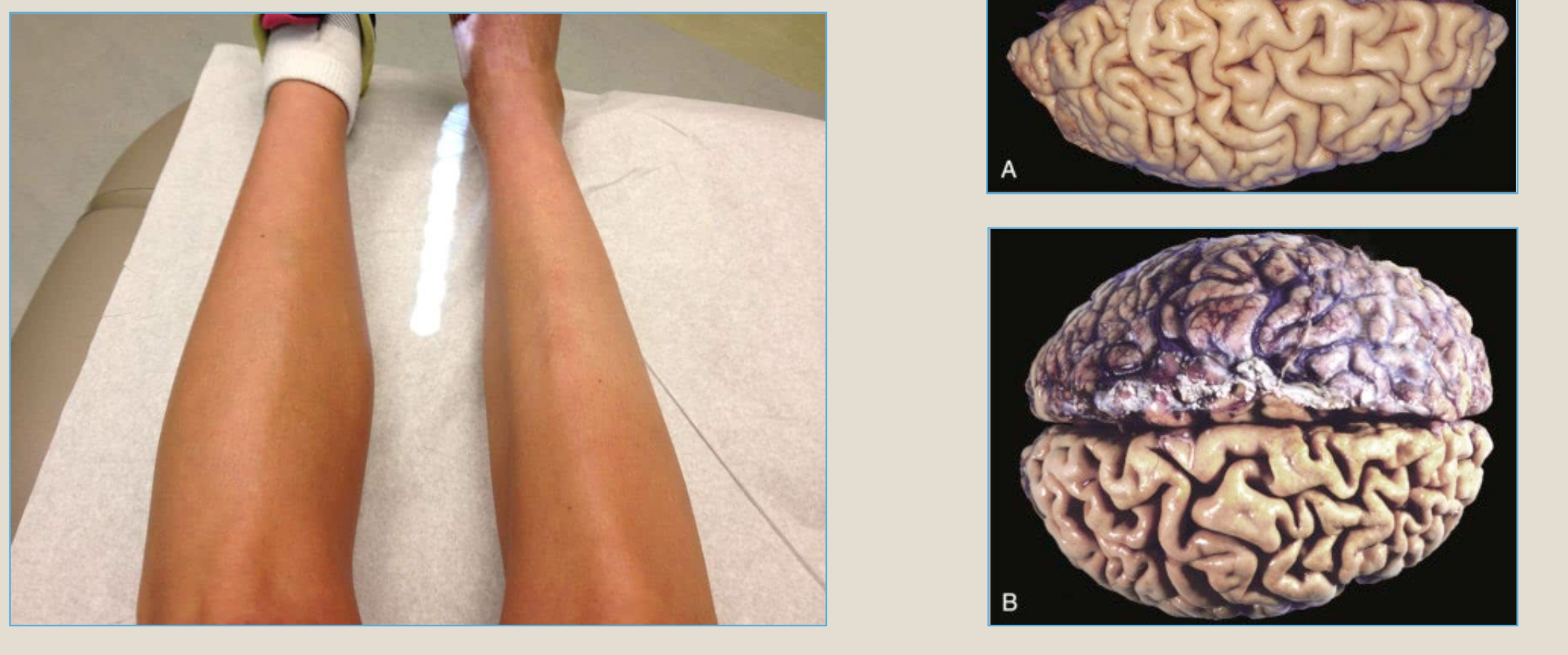
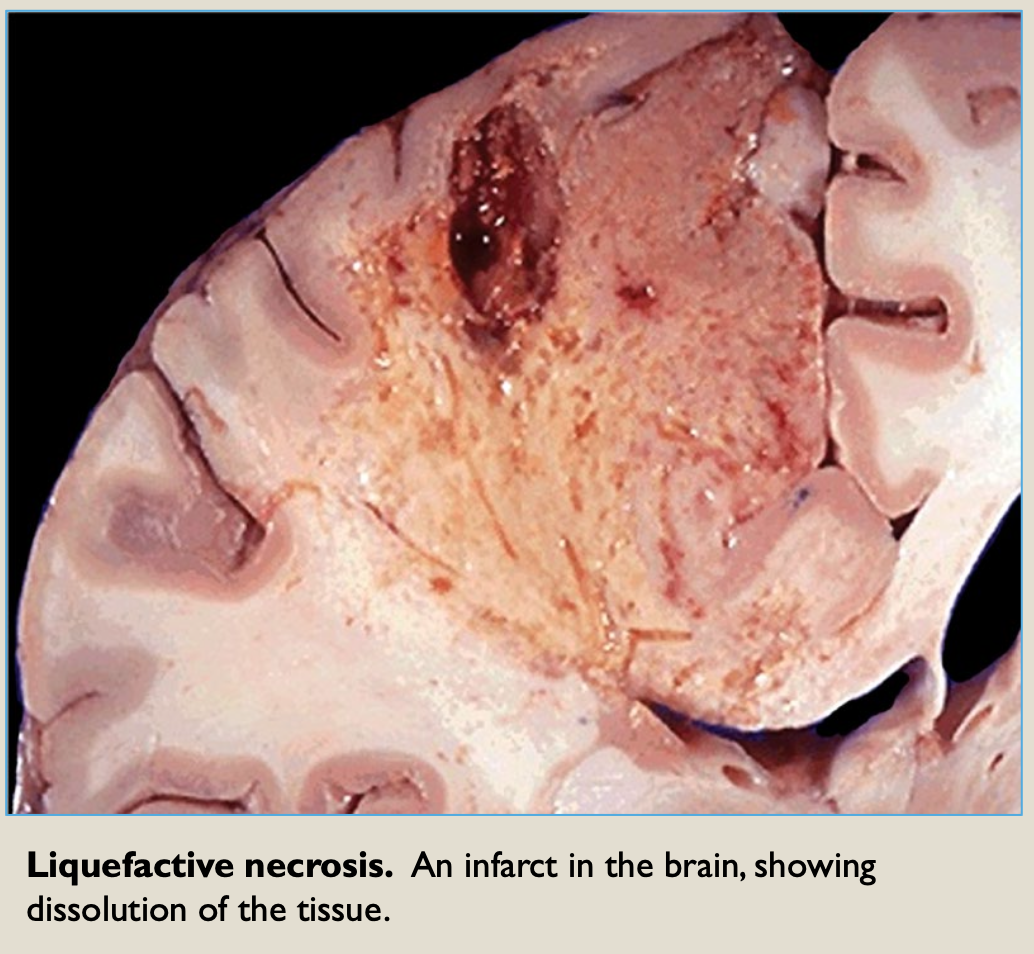
Liquefactive Necrosis
catalytic degradation of cell dominates
characteristic of cell death due to bacterial infections
characteristic of hypoxic death in the CNS
Apoptosis
distinctive and intentional mode of programmed cell death that is sometimes referred to as cell suicide
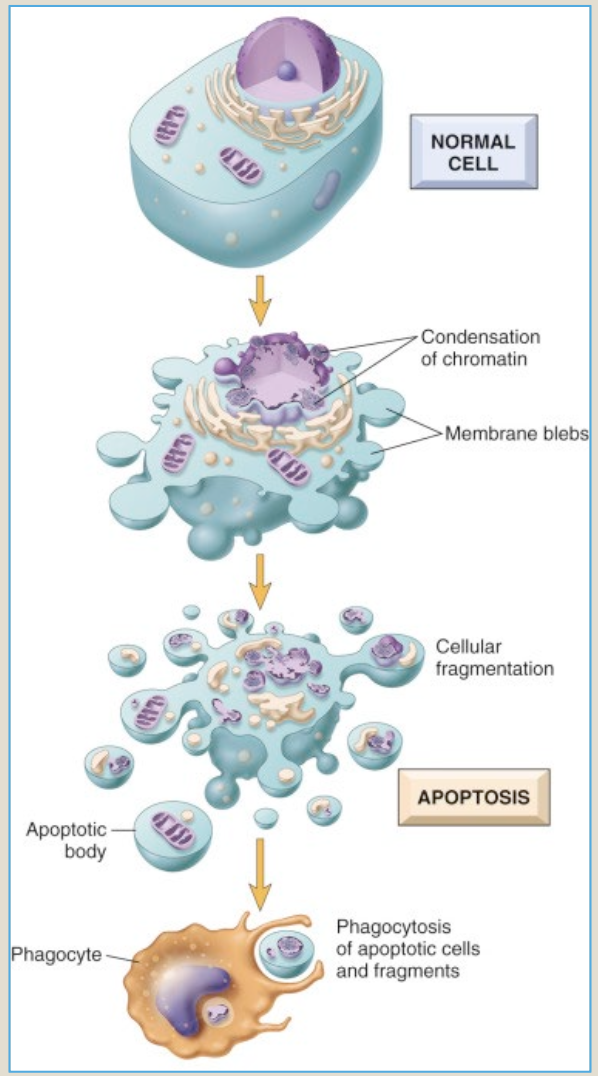
morphologic phases of apoptosis
nuclear chromatin in target cells condenses and the cytoplasm turn intensely red
the cell then dismantles into apoptotic bodies, each surrounded by intact cell membrane
apoptotic bodies are eliminated by WBC’s via process of phagocytosis
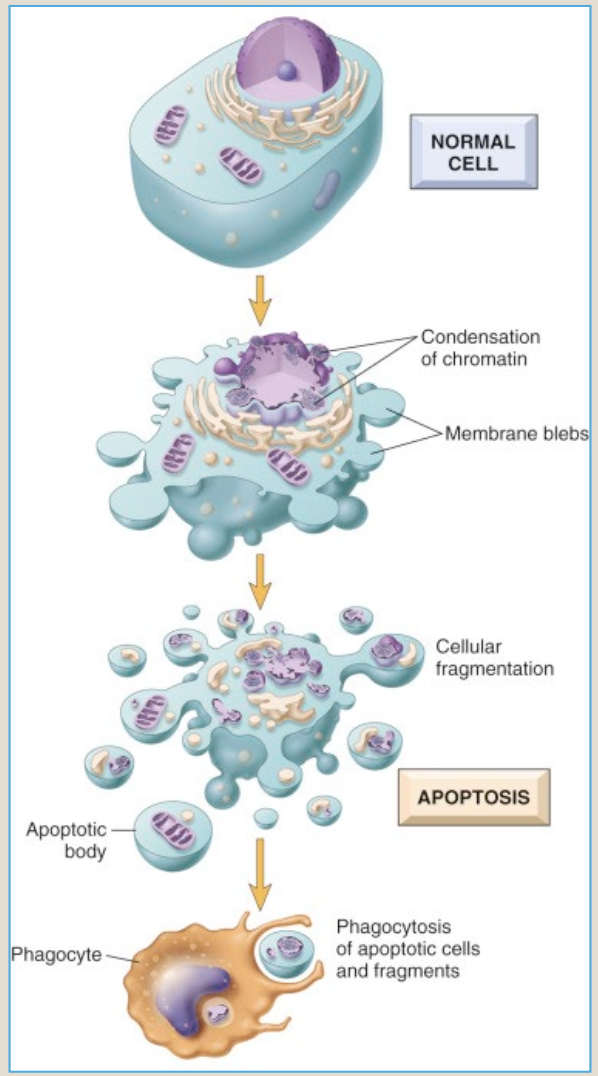
examples of apoptosis
programmed cell death during embryogenesis
hormone-dependent involution of endometrial and breast tissues
death of immune cells that are not functioning properly, such as a self-reactive lymphocytes
programmed death of cells with damaged DNA that cannot be repaired - important in cancer prevention
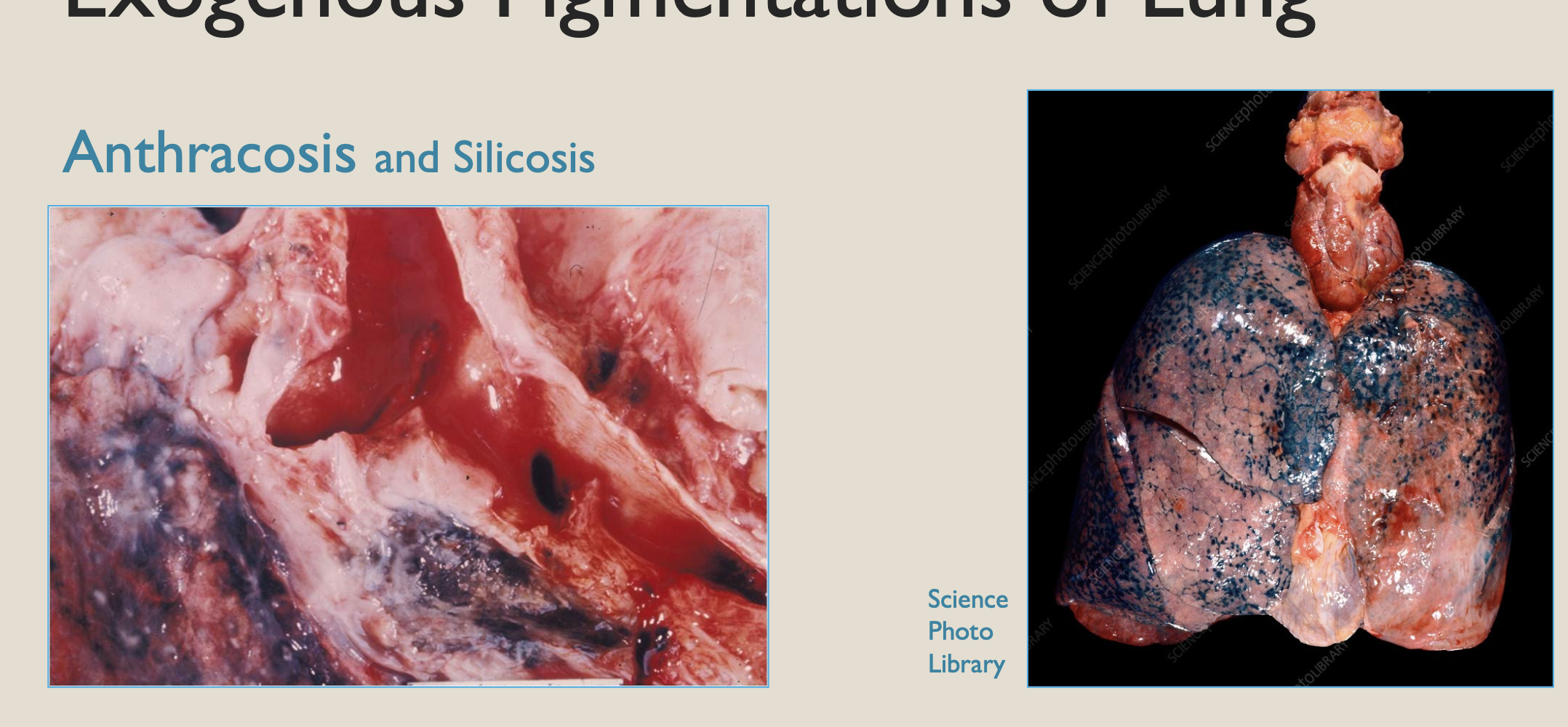
exogenous pigments
colored substances which originate from outside the body
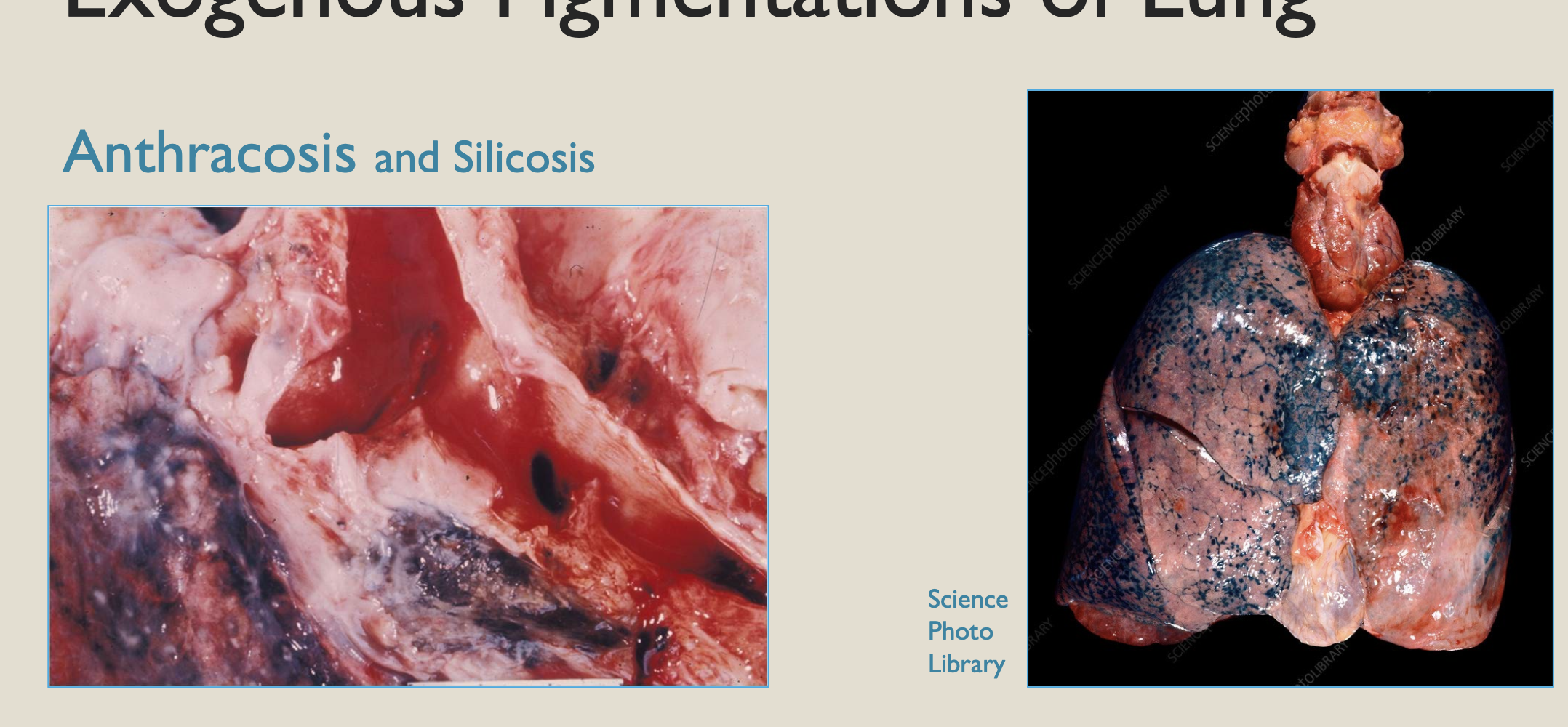
anthracosis
carbon dust particles accumulate in macrophages of the lunges
seen in the lungs of city dwellers, but does not cause problems
v heavy carbon deposits may greatly reduce respiratory function, such as in “coal worker’s pneumoconiosis” = “coal miner’s lung”
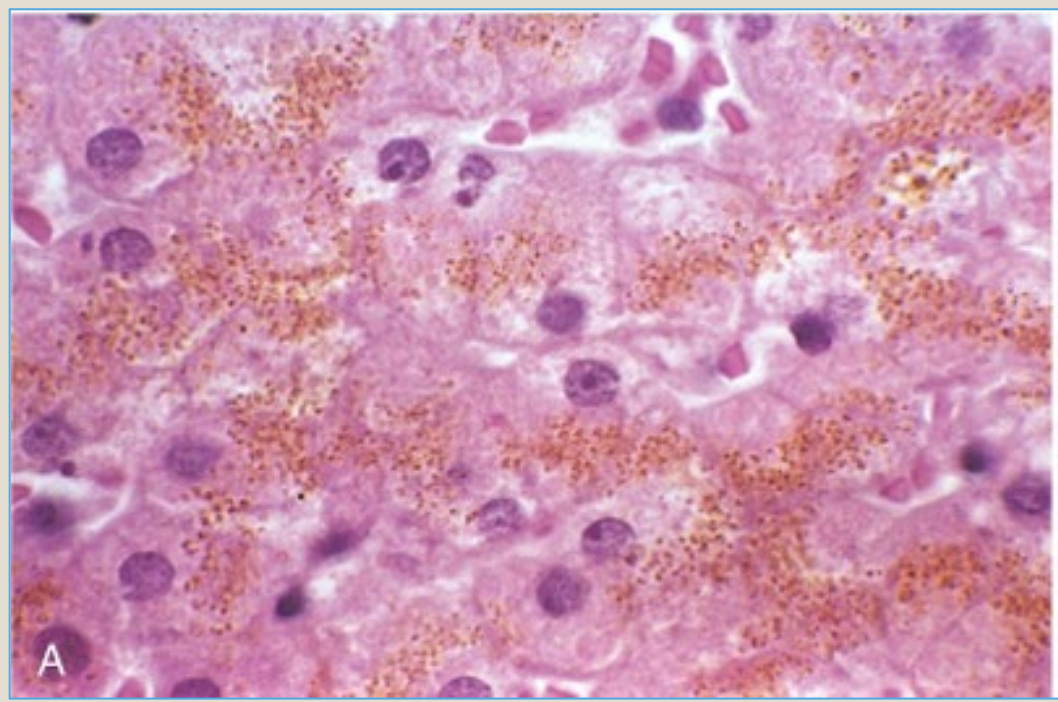
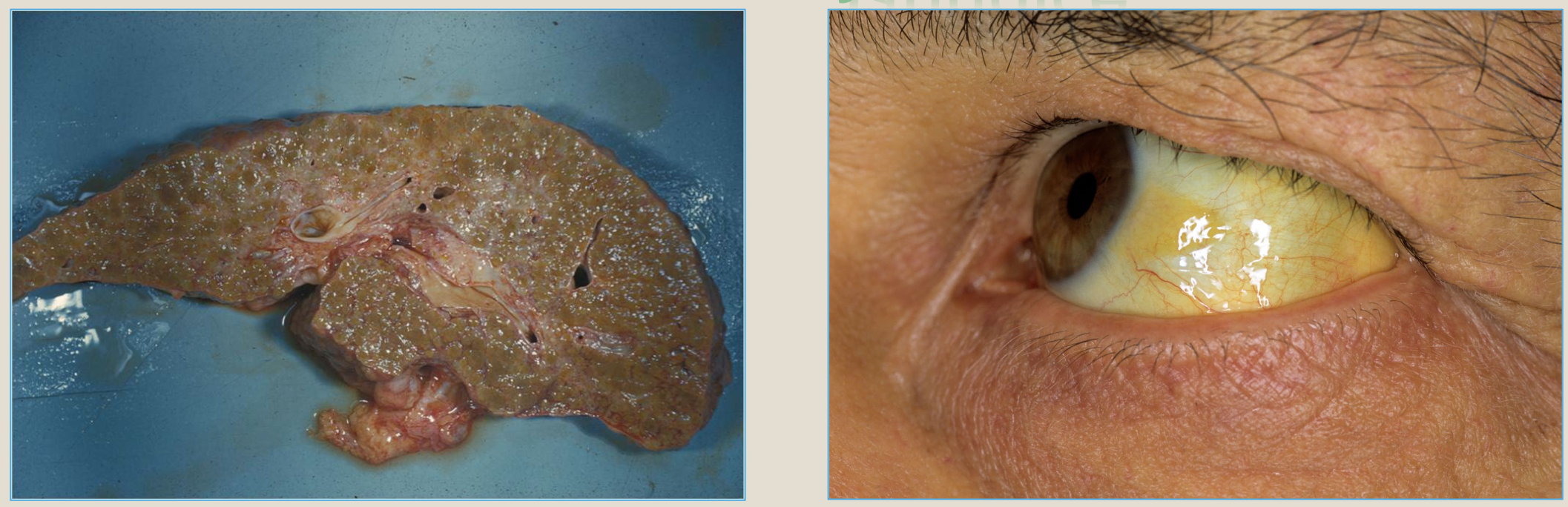
Endogenous pigements
synthesized within the body as part of the normal physiologic process
ex: hemosiderin, bilirubin (jaundice), melanin
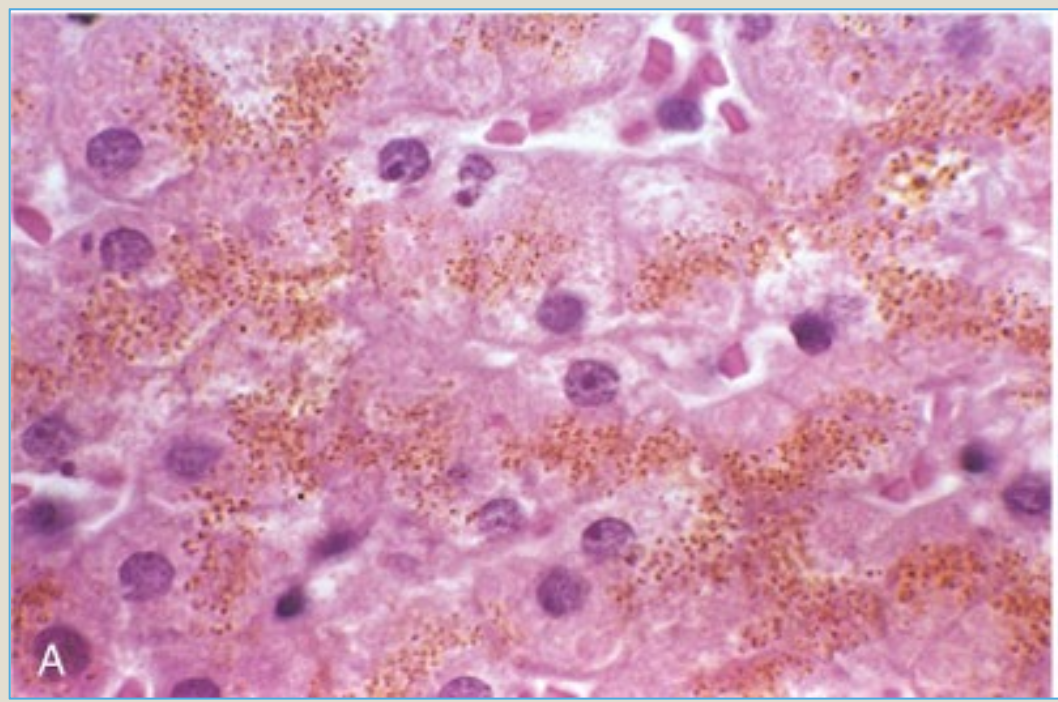
hemosiderin
golden yellow to brown pigment derived from hemoglobin breakdown
form of stored iron, usually within macrophages
ex: heart failure cells
bilirubin
green pigment derived from hemoglobin breakdwon
lipid soluble and carried through the bloodstream to the liver
liver process and excretes it in bile
jaundice is the clinical result of excess and is seen as yellow discoloration of the skin and sclerae
Innate Immunity
systems that neutralize an offending agent without requiring prior exposure to be effective
first line defense
physical barriers
chemical barriers or responses: mucus layer, complement
cellular responses: non- specific phagocytes, natural killer cells
adaptive immunity
acquired immunity responses to a previously encountered antigen
provided by lymphocytes
B cells confer humoral immunity
T cells confer cell-mediated immunity
second line of defense that works in conjunction with inflammation and repair mechanisms
Humoral Immune System
Antibody-mediated part of the immune system
antibodies are synthesized by plasma cells
antibodies aka immunoglobulins
Activation of complement (IgG and IgM)
Opsonization to enhance phagocytosis (IgG)
Mucosal immunity (IgA)
Neonatal immunity (maternal IgG)
Destruction of parasites (IgE)
Antigen-antibody complex: when an antibody binds with its matching antigen
triggers complement activation via the classic pathway
Complement system
part of innate immunity
precursor proteins circulate in the plasma and require chemical conversion to become active
complement is activated by the classic pathway in the presence of Ag-Ab complexes and by the the alternate pathway in the presence of microbial surfaces and polysaccharides
end product: membrane attack complex (C5-9)
complement cascade: kill bacteria