Physiology: Female Reproduction (Lecture 20)
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
34 Terms
Learning Objectives:
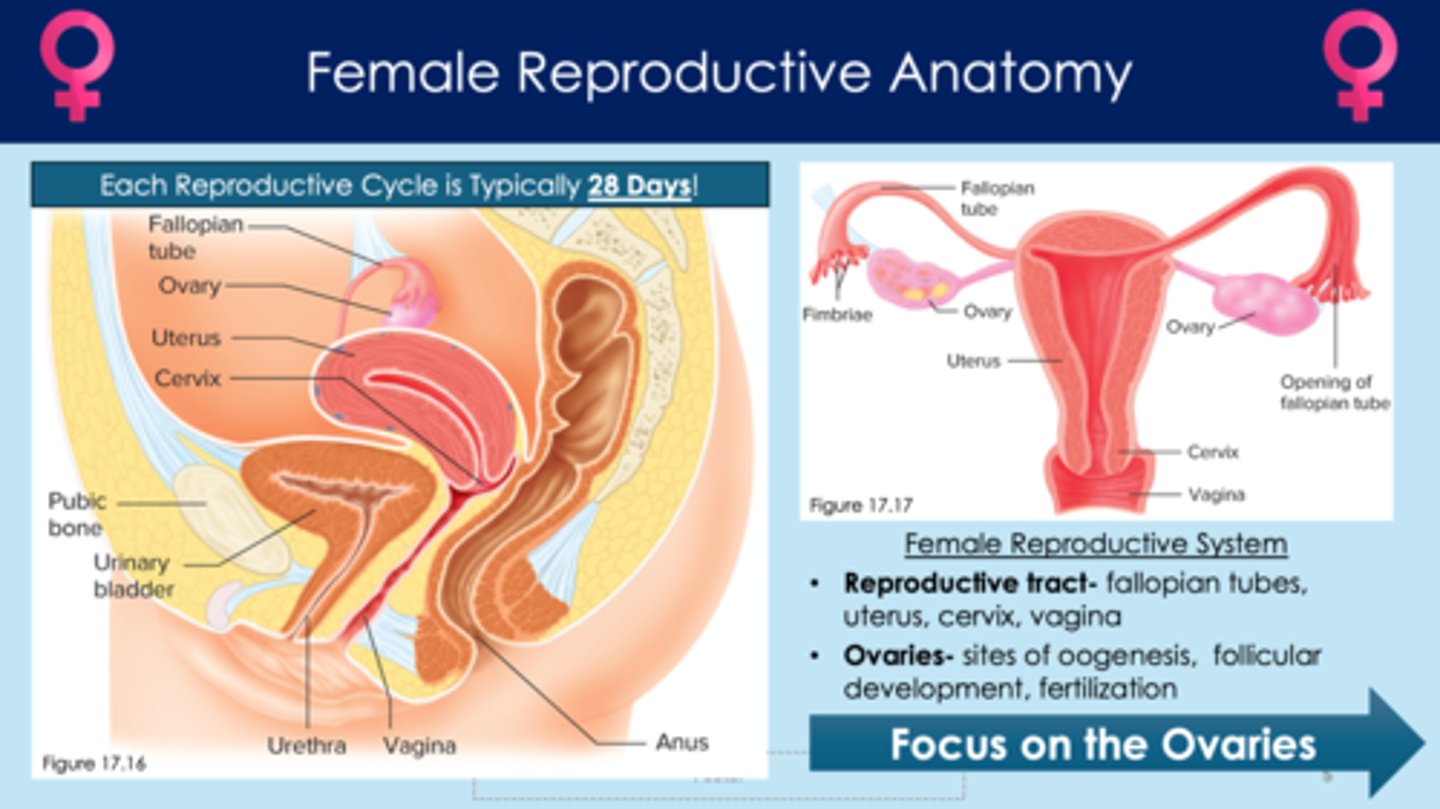
In females, what are the five structures in the reproductive system?
1. fallopian tubes
2. uterus
3. cervix
4. vagina
5. ovaries
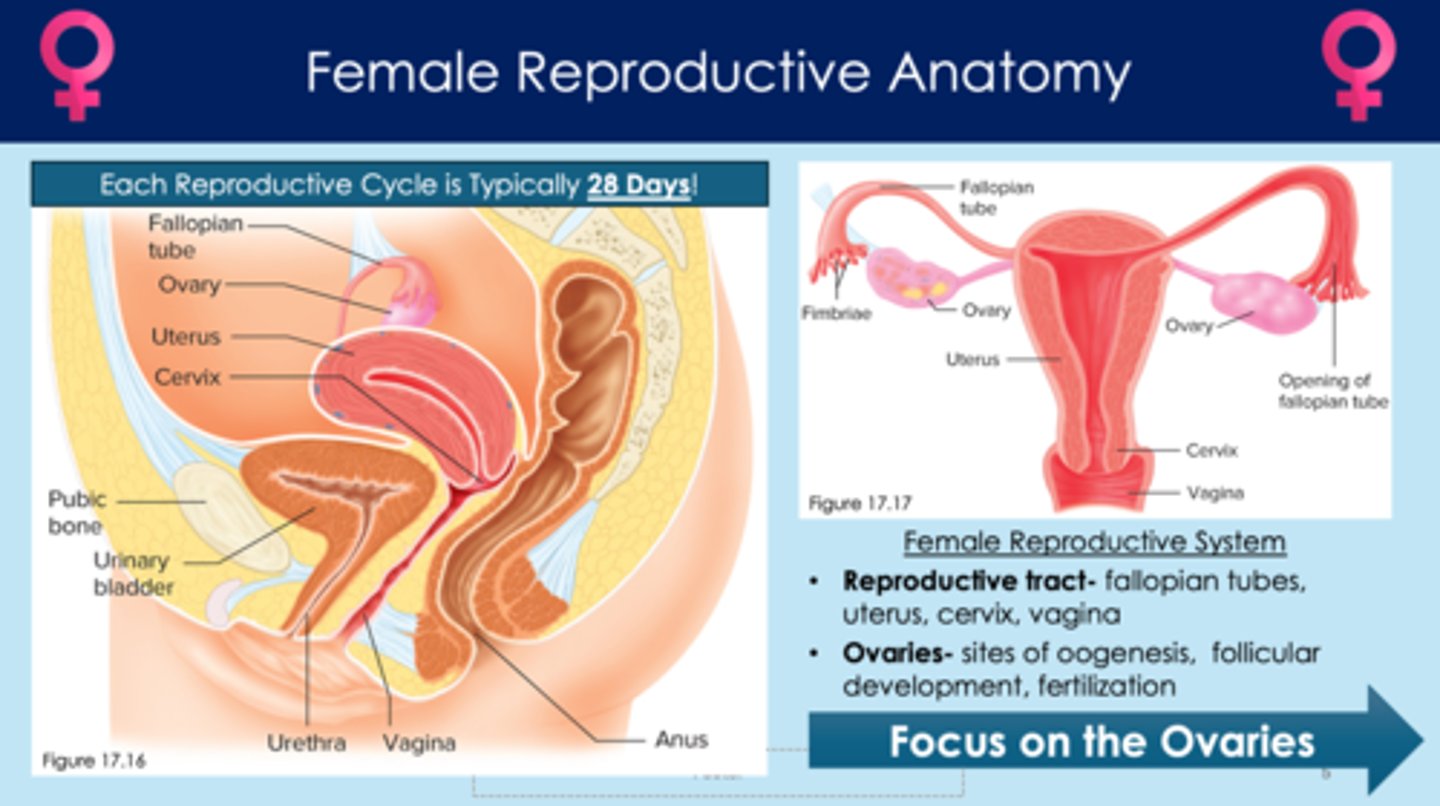
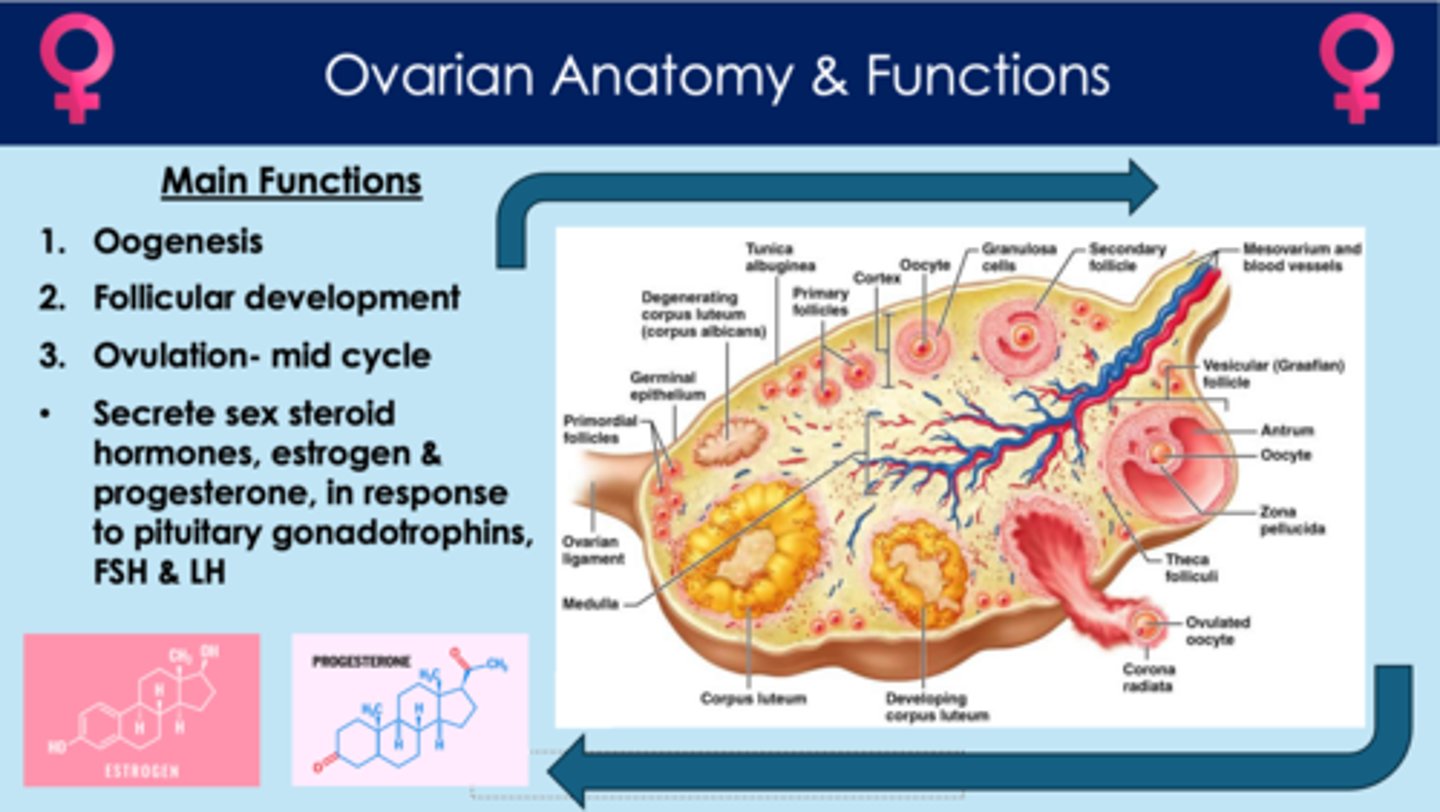
What are ovaries? What are the four functions of ovaries?
1. oogenesis - creates oocytes; located in follicles
2. follicular development
3. ovulation - secondary oocyte is released from a follicle
4. secrete sex steroid hormones, estrogen and progesterone (in response to FSH and LH)
In females, how long does the reproductive cycle take?
- 28 days
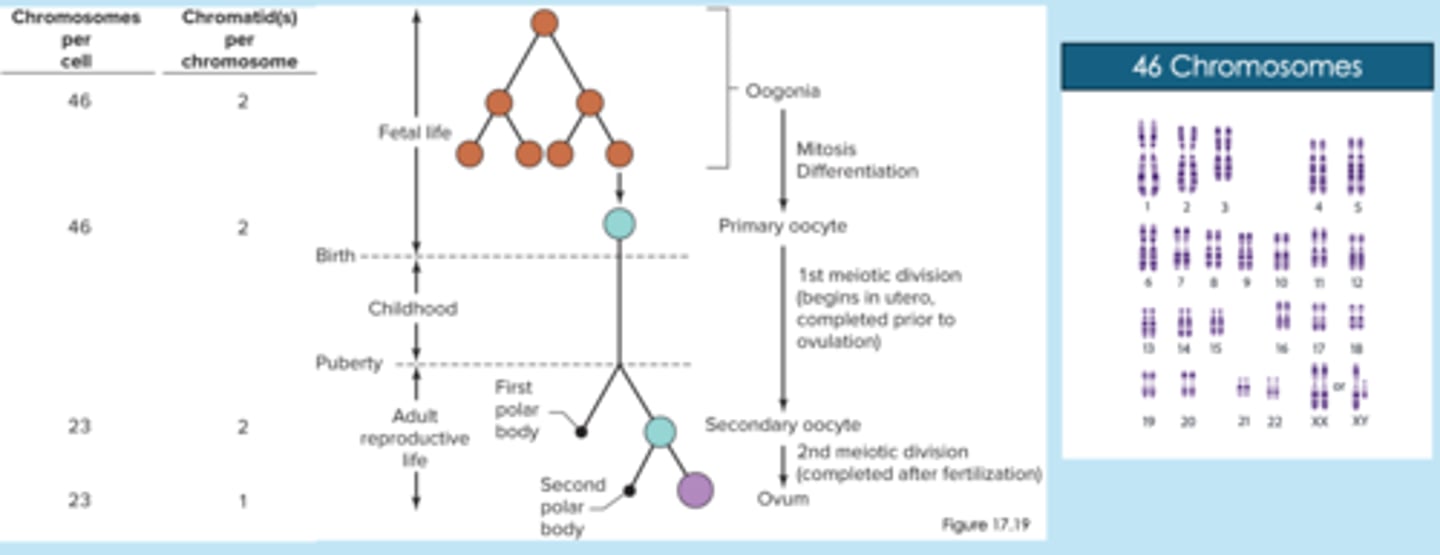
What are the stages of oogenesis?
1. oogonia (stem cells) undergo mitosis and makes copies of oogonia and primary oocytes; this process starts before birth and then stops; doesn't continue again until puberty
2. during puberty, first polar bodies discard extra chromosomes from primary oocytes so that they don't have more than 23 chromosomes
3. primary oocytes undergo meiosis and produces secondary oocytes (genetically unique)
4. if fertilization occurs, second polar bodies discard extra chromosomes from secondary oocytes; secondary oocytes finish meiosis and produce ovum (after the egg has begun to be fertilized by sperm)
**females are born with all the primary oocytes they'll ever have before birth
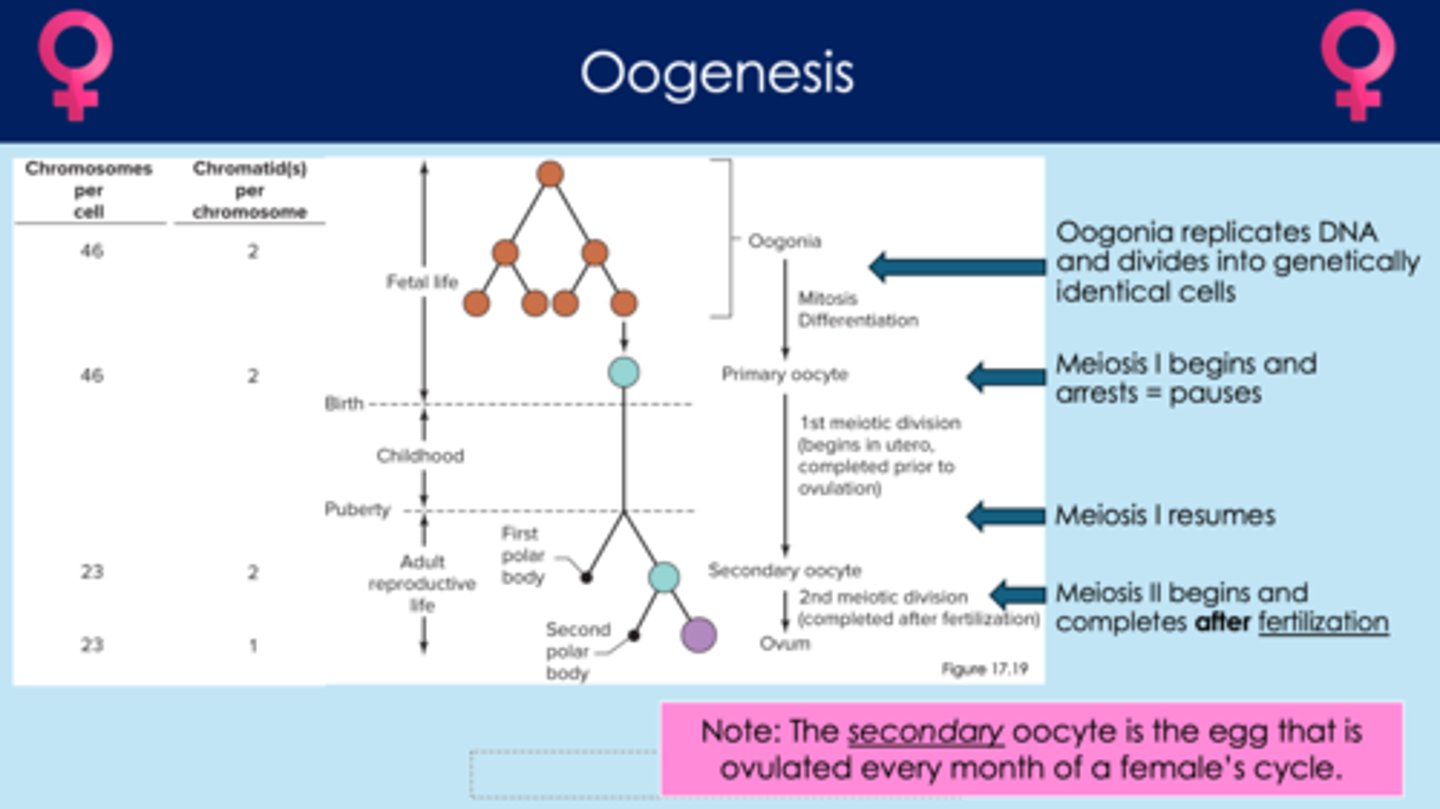
When does oogenesis begin?
- begins before birth
- oogenesis creates primary oocytes, then stops
- picks up at puberty; this is when primary oocytes begin to divide into secondary oocytes
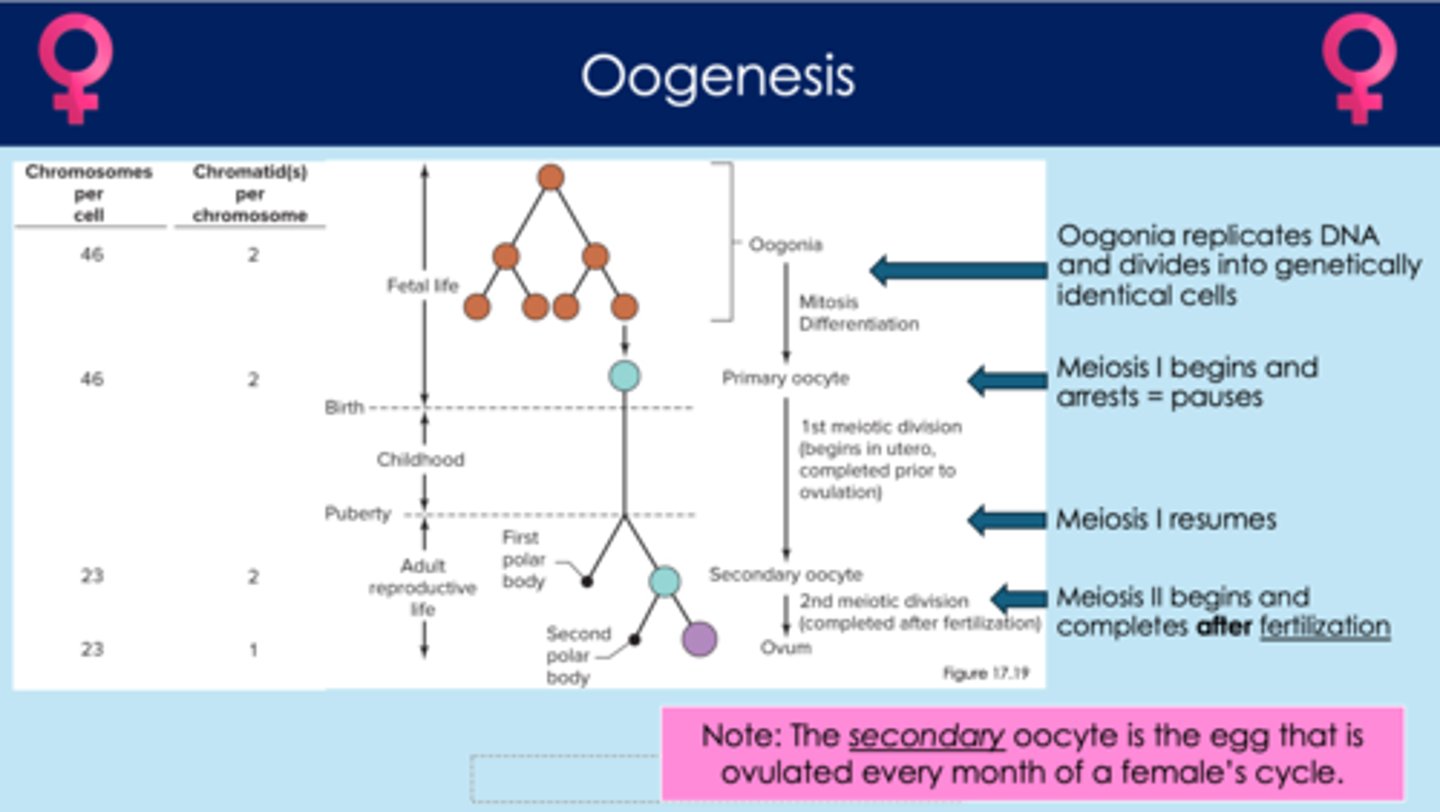
What are the number of chromosomes associated with each step of oogenesis?
1. oogonia (46 chromosomes)
2. primary oocytes (46 chromosomes)
3. secondary oocytes (23 chromosomes)
4. ovum (23 chromosomes)
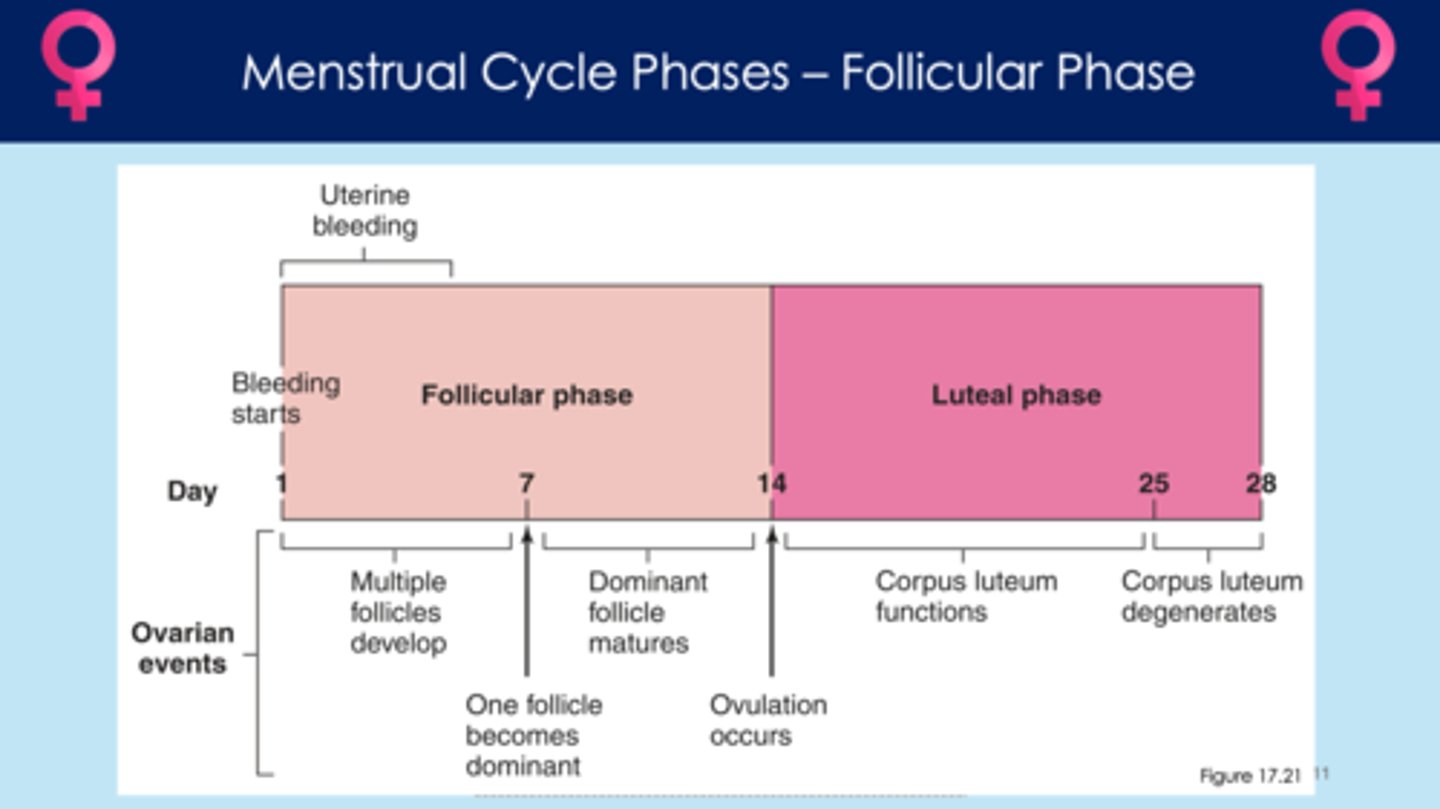
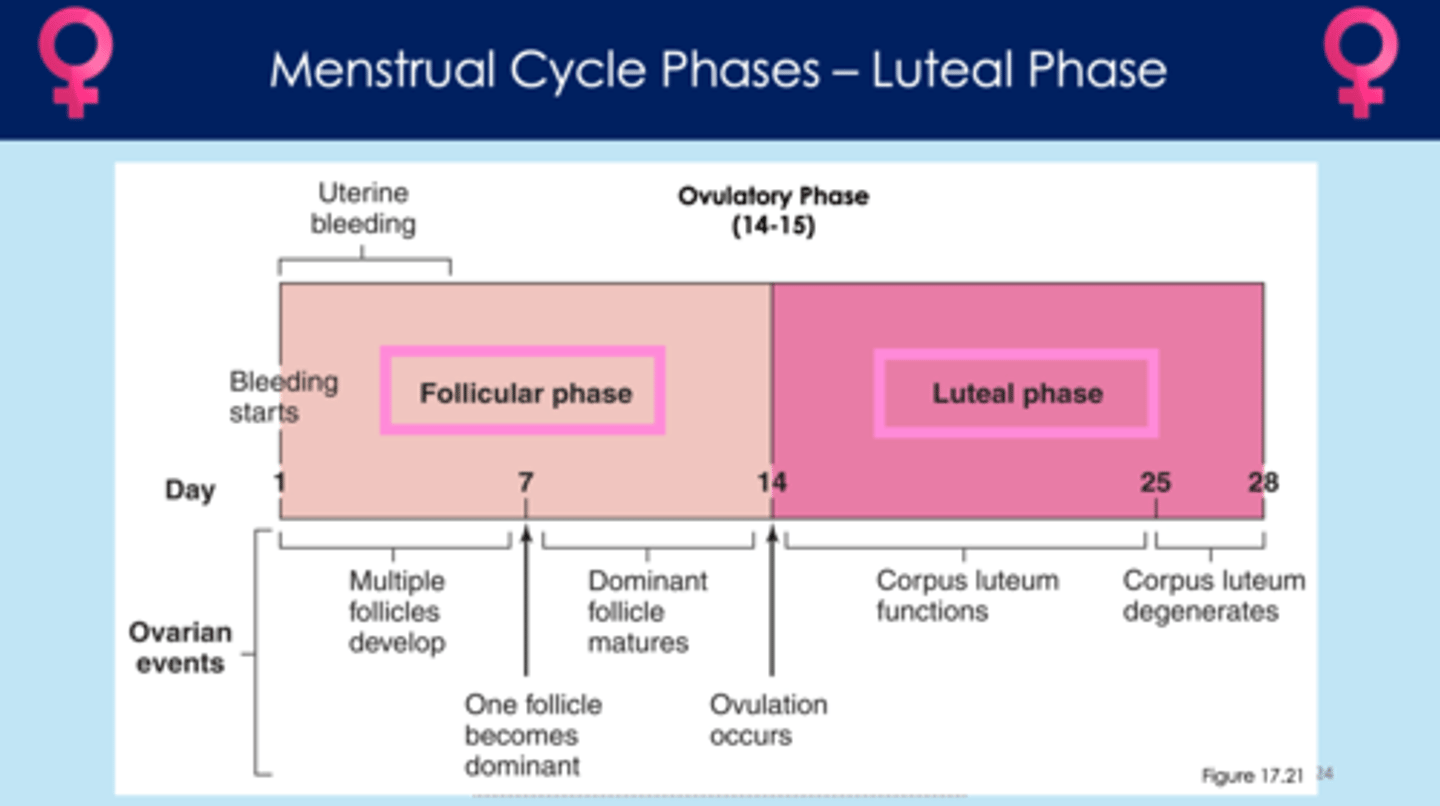
What are the two phases of the menstrual cycle?
1. follicular phase
2. luteal phase
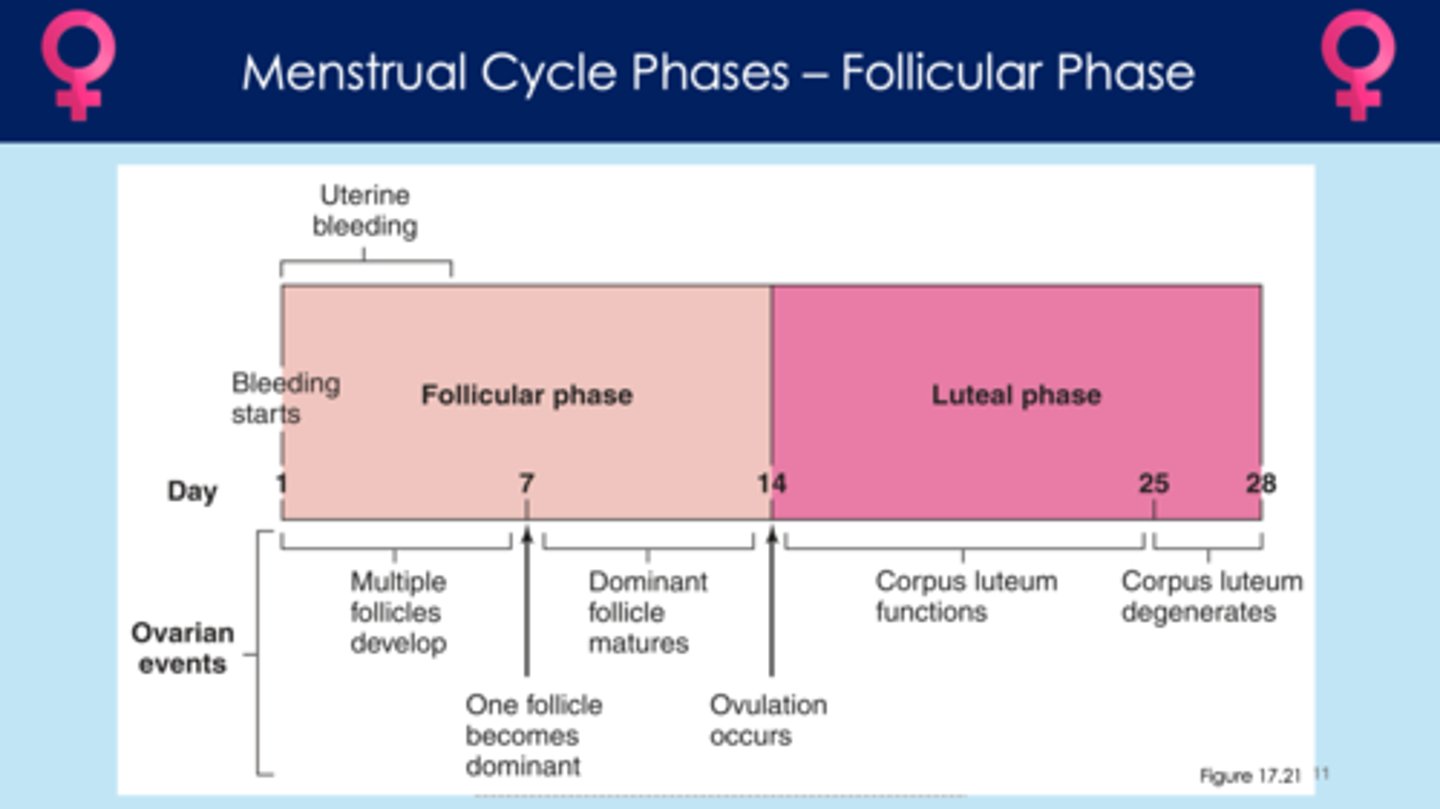
In the menstrual cycle, what happens during the follicular phase?
- follicle matures
- LH and FSH are important hormones for follicular development
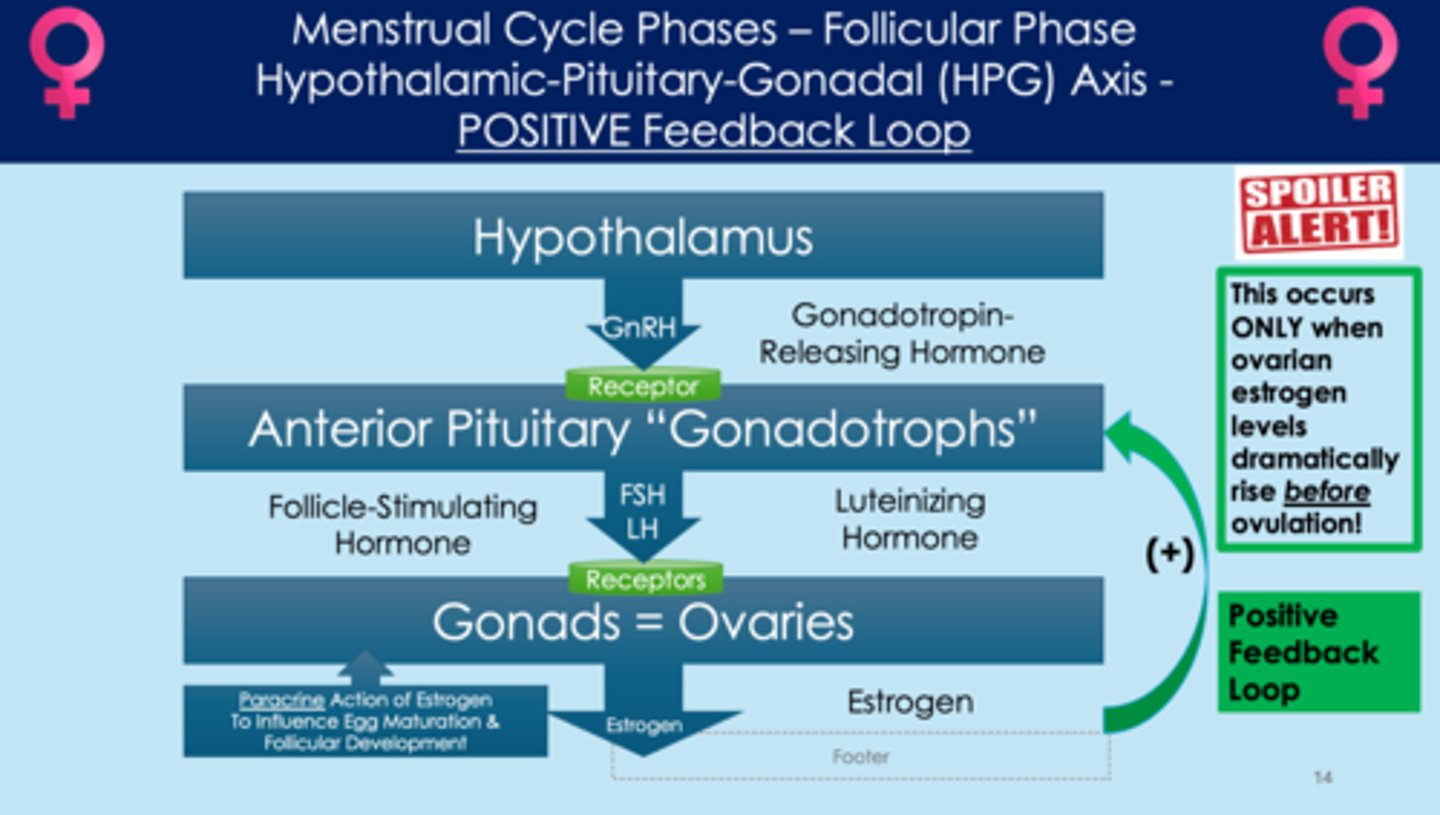
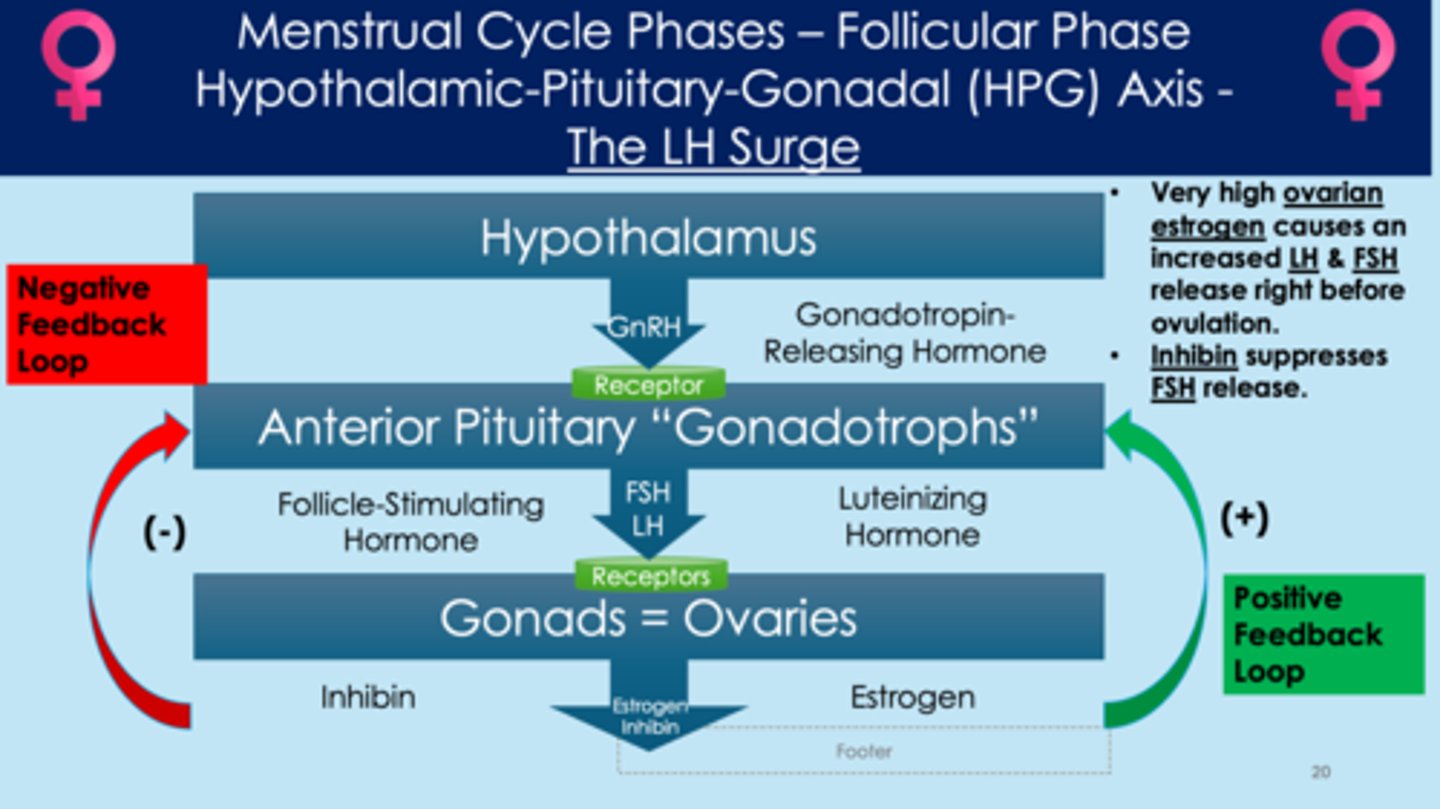
What are the steps in the hypothalamic-pituitary-gonadal (HPG) axis in the follicular phase?
1. hypothalamus release gonadotropin-releasing hormone (GnRH)
2. GnRH binds to receptors on anterior pituitary "gonadotrophs"
3. anterior pituitary releases follicle-stimulating hormone (FSH) and luteinizing hormone (LH)
4. FSH and LH bind to receptors on ovaries
5. ovaries release estrogen
6. if estrogen levels are high, estrogen acts on the anterior pituitary gland and stops the release of FSH and LH; also acts on the hypothalamus and stops release of GnRH (negative feedback)
7. if estrogen levels are extremely high (before ovulation), estrogen acts on the anterior pituitary gland and stimulates the release of more FSH and LH
*estrogen has paracrine action on egg development; influences egg maturation/follicular development
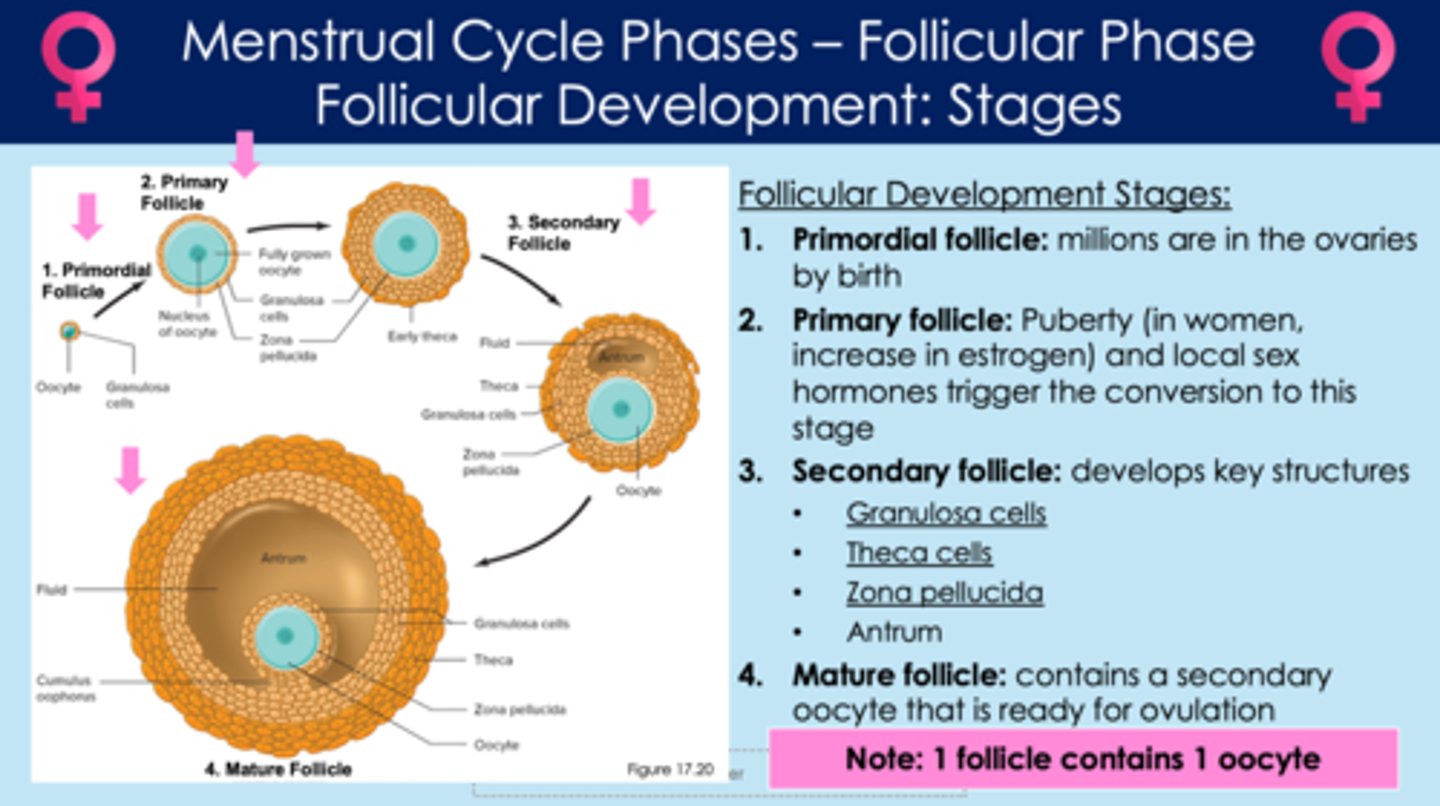
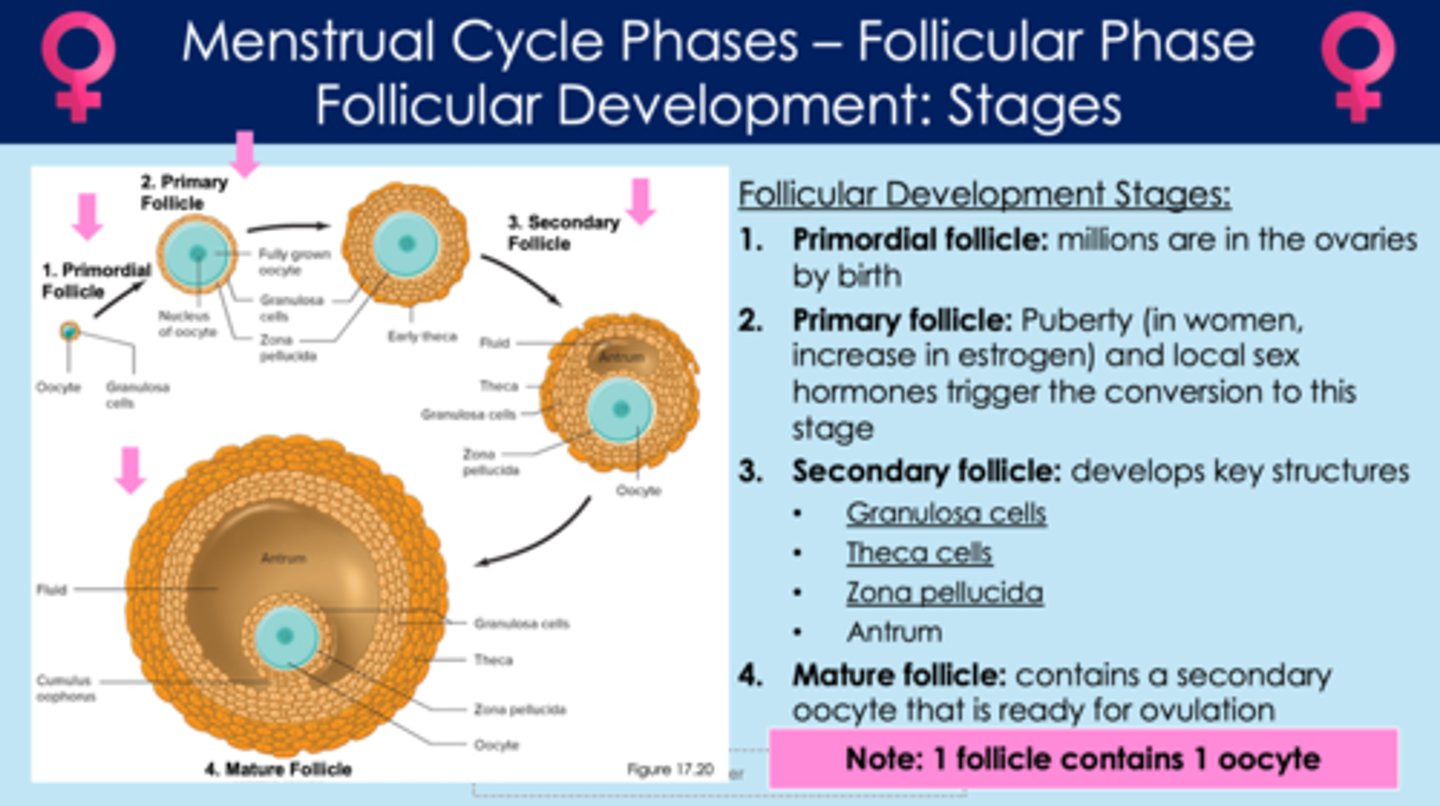
What are the four steps in follicular development?
1. primordial follicle
2. primary follicle
3. secondary follicle
4. mature follicle
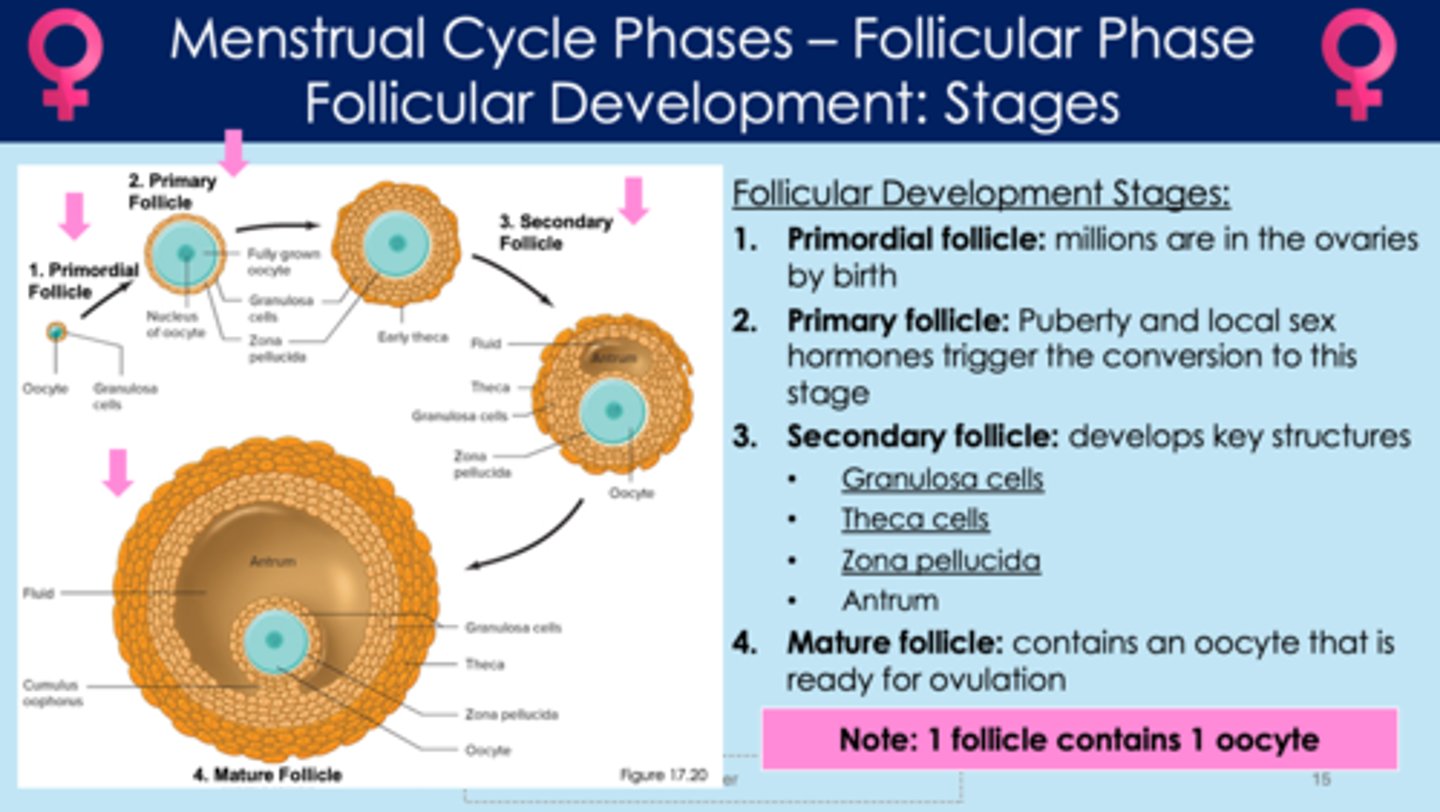
In follicular development, what is a primordial follicle?
- earliest form of follicle
- millions are in the ovaries by birth
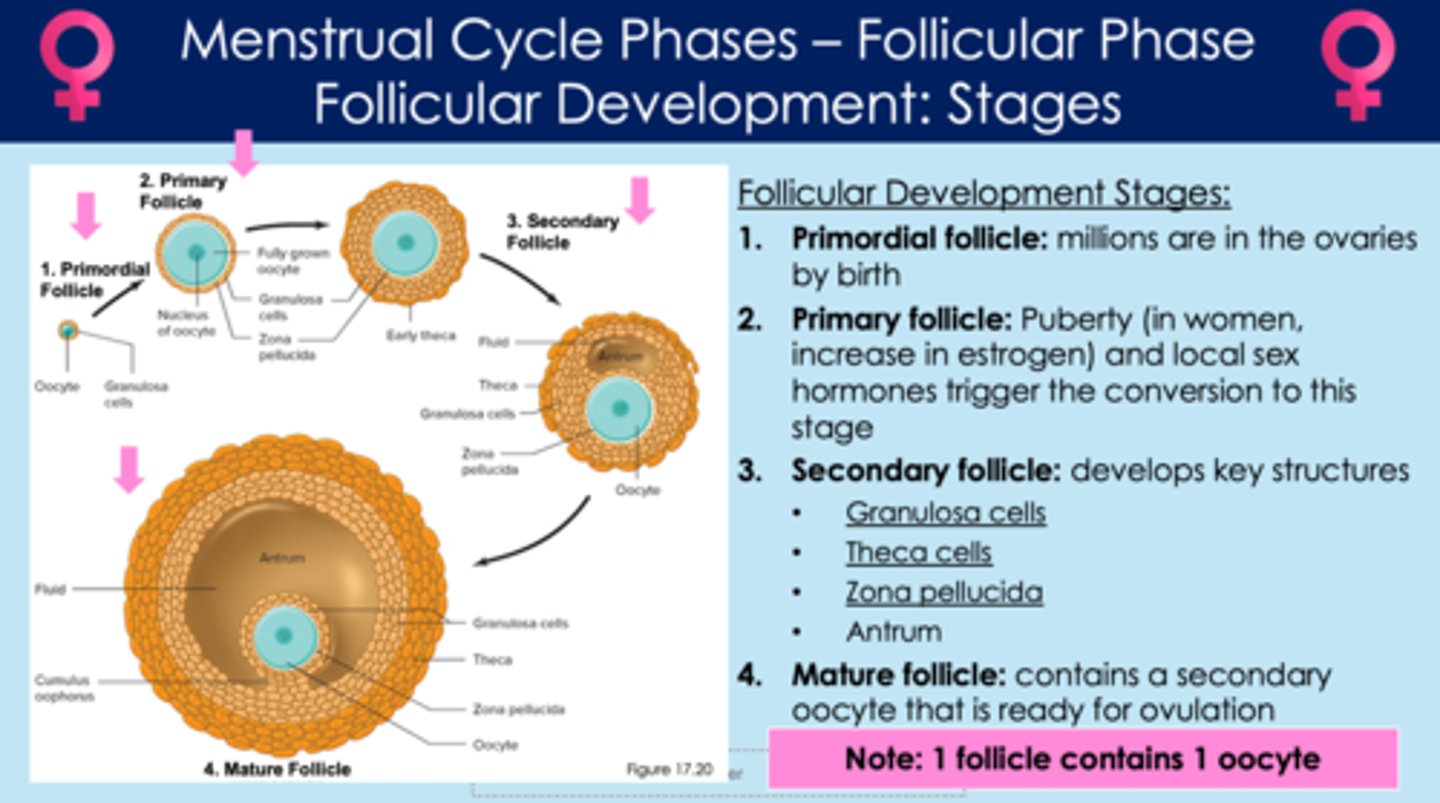
In follicular development, what is a primary follicle?
- puberty stimulates primordial follicles to grow into primary follicles
- estrogen and sex hormones cause primordial follicles to transform into primary follicles
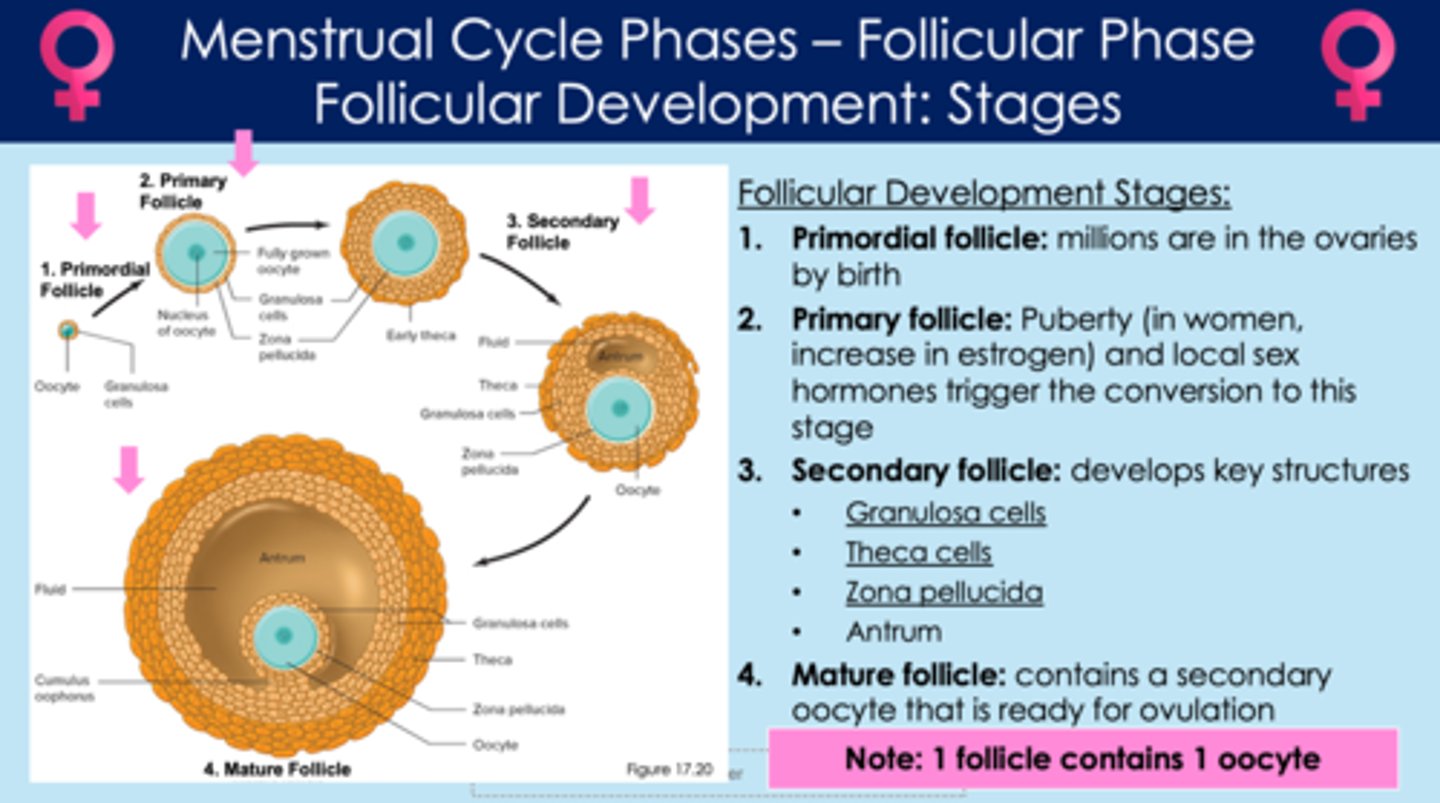
In follicular development, what is a secondary follicle?
- follicle that contains granulosa cells, theca cells, zona pellucida, and antrum
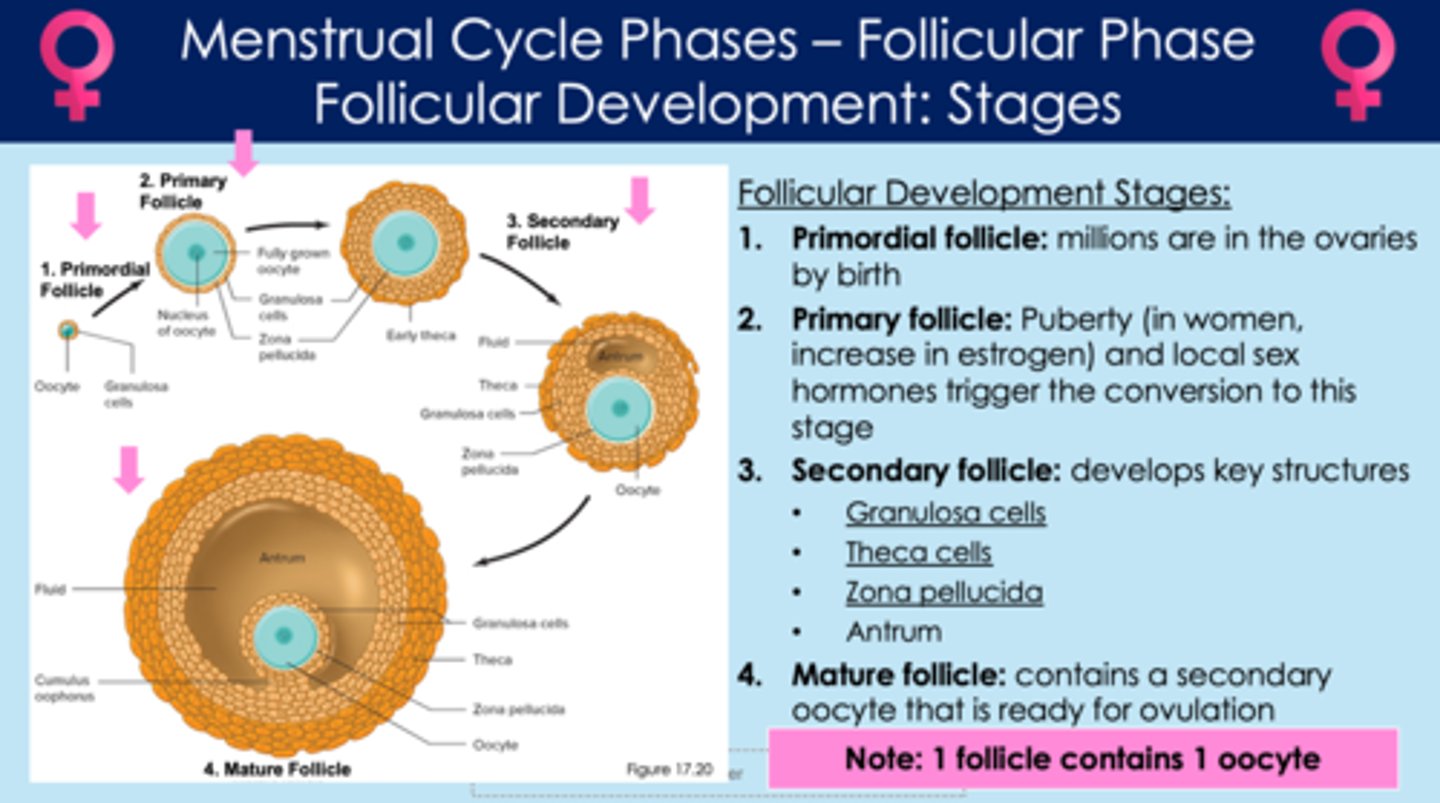
What are the four structures found in secondary follicles?
1. theca cells
2. granulosa cells
3. antrum
4. zona pellucida
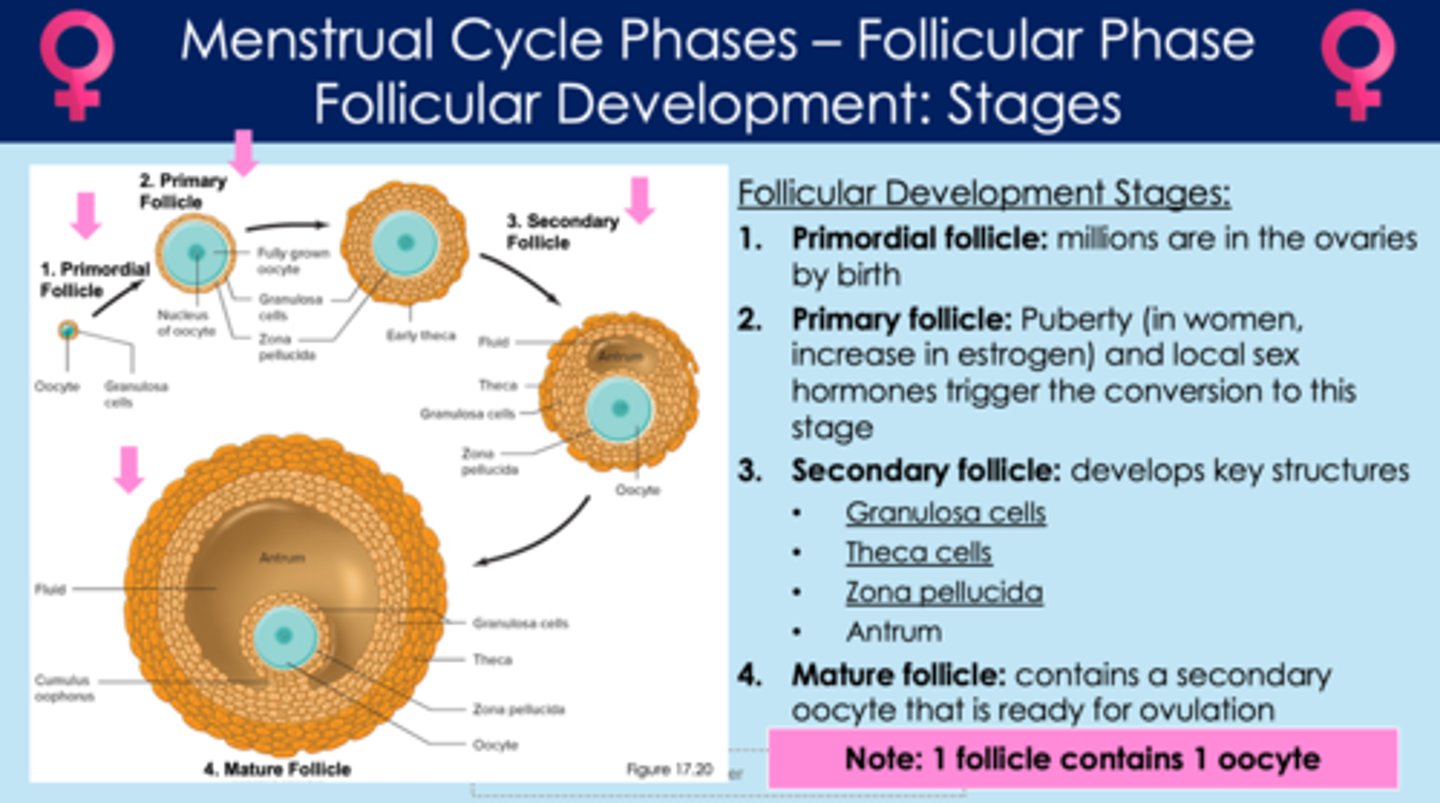
In secondary follicles, what are theca cells?
- thin outermost layer of the follicle
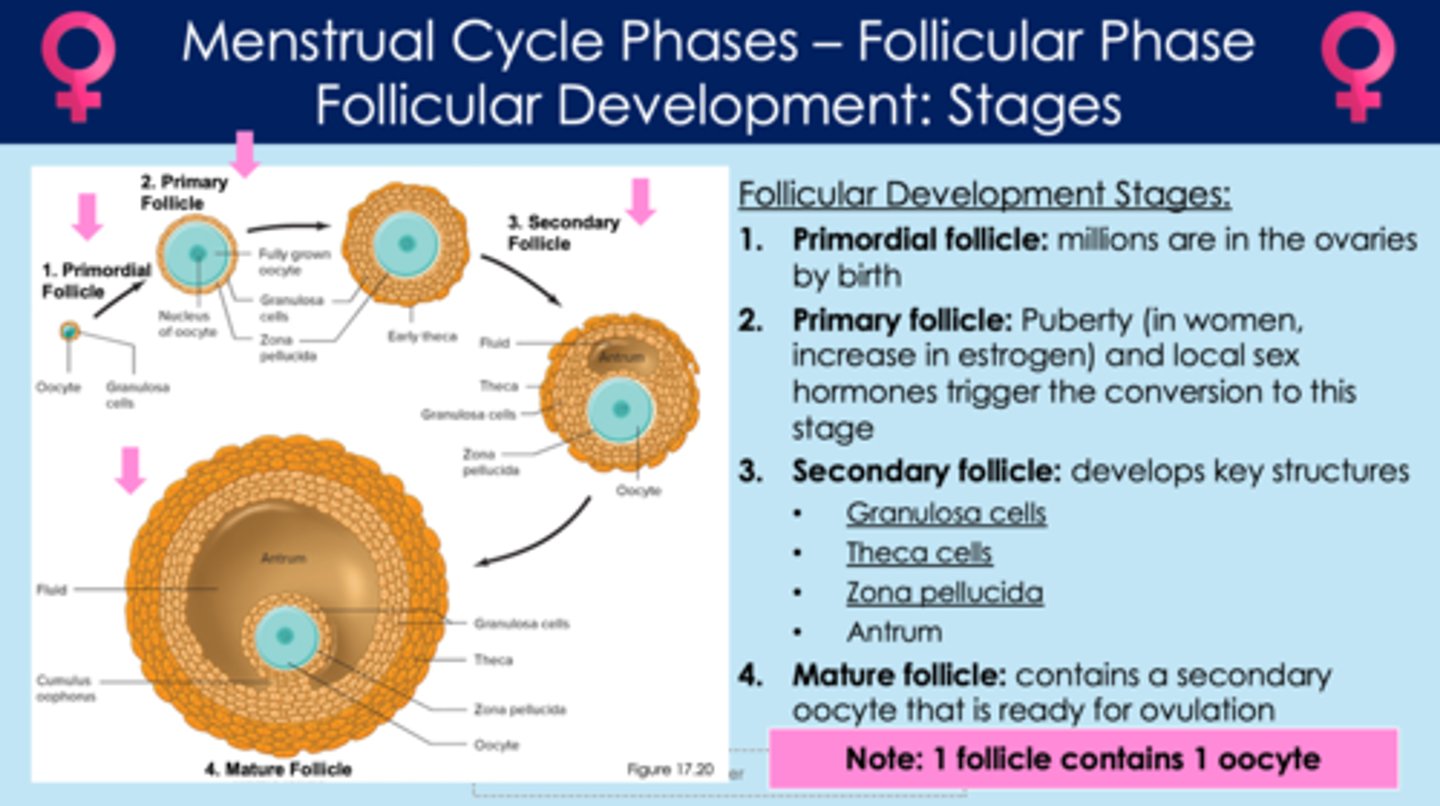
In secondary follicles, what are granulosa cells?
- second layer of follicle
- granulosa cell growth helps to make the secondary follicle bigger
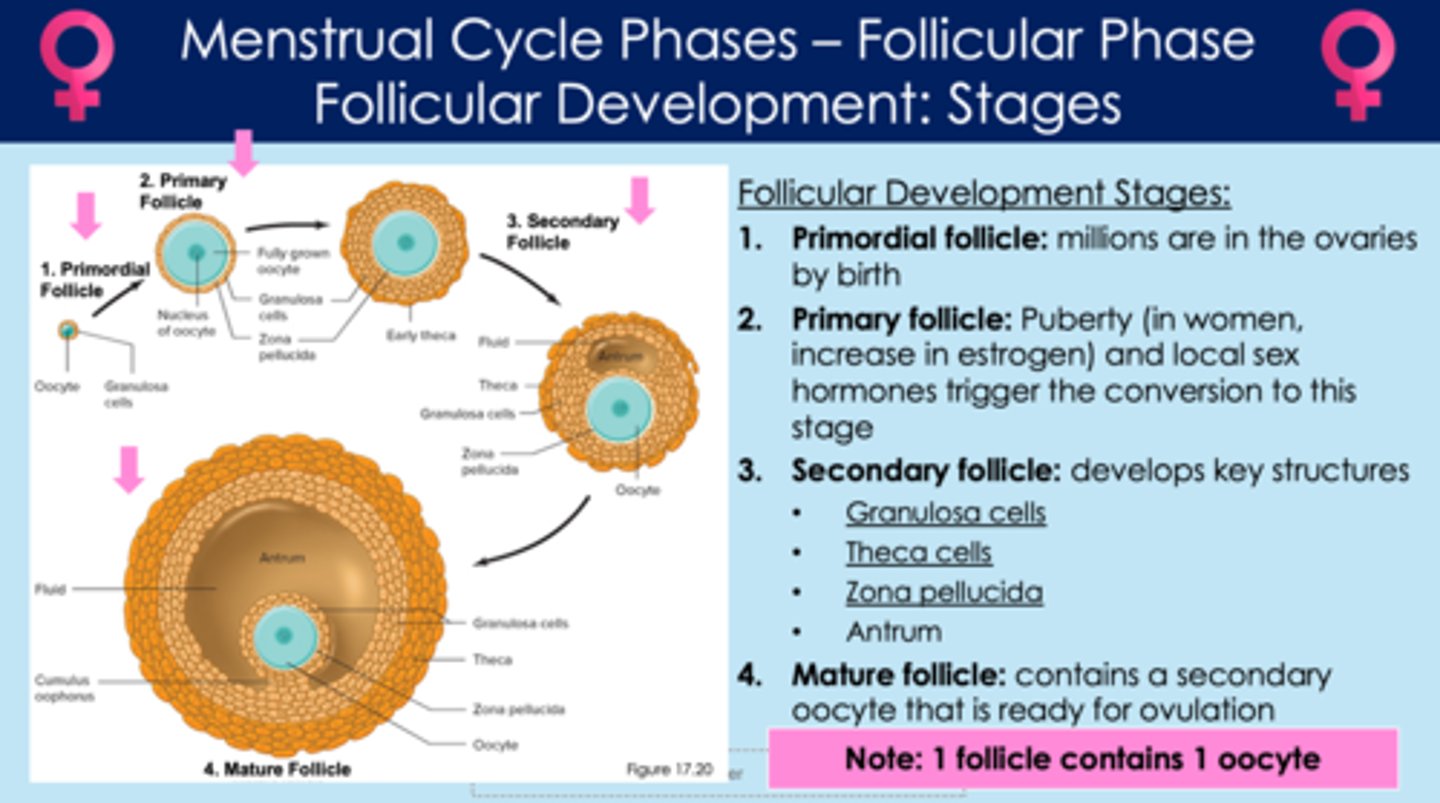
In secondary follicles, what is the antrum?
- fluid-filled center, surrounded by granulosa cells
- antrum growth helps to make the secondary follicle bigger
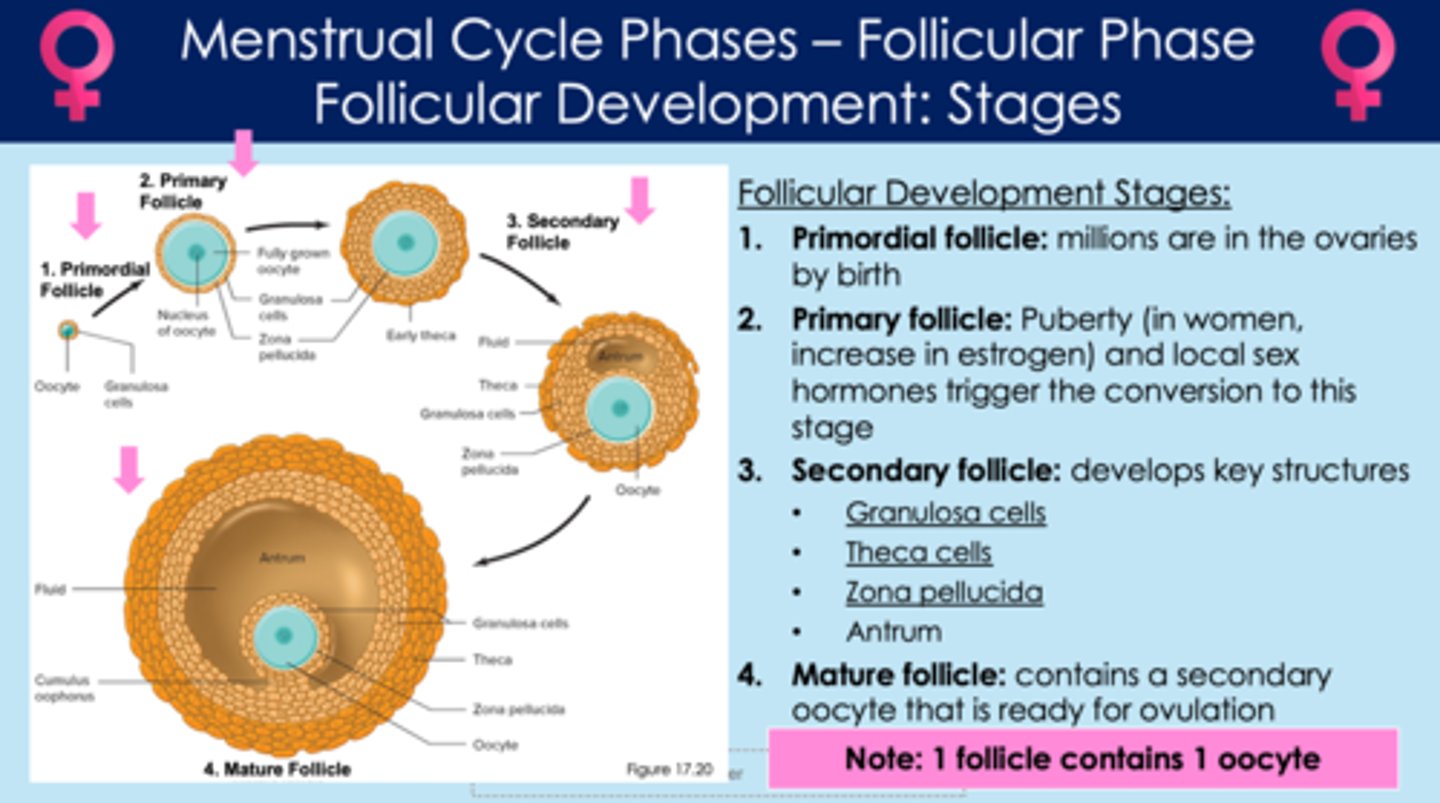
In secondary follicles, what is the zona pellucida?
- innermost layer of follicle; surrounds the oocyte
- gets activated when fertilization occurs; blocks out other sperm from entering the egg
*note: this layer remains around the egg after it's released from the follicle; it only breaks down when fertilization occurs
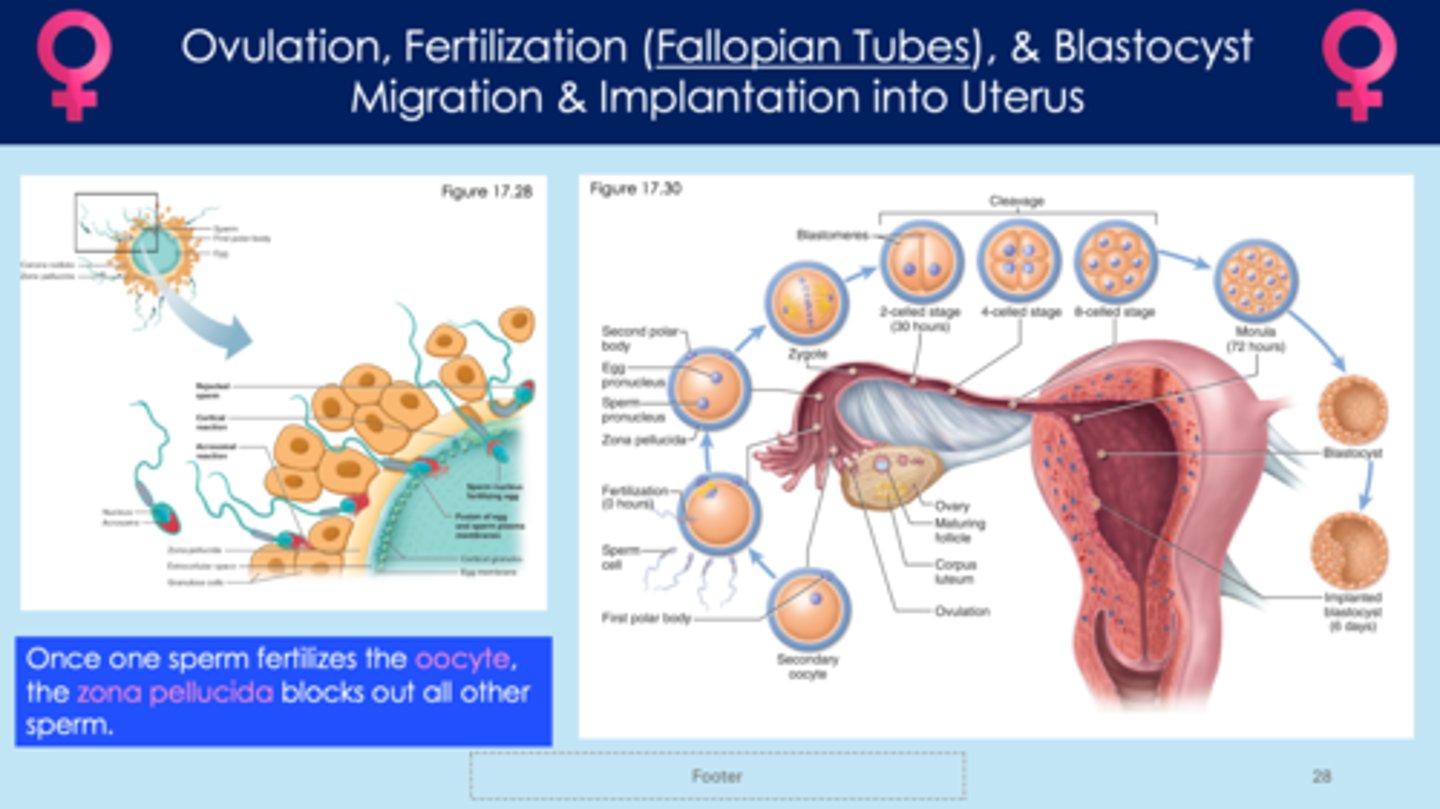
What is ovulation?
- mature egg is released from the follicle and is ready to be fertilized by sperm
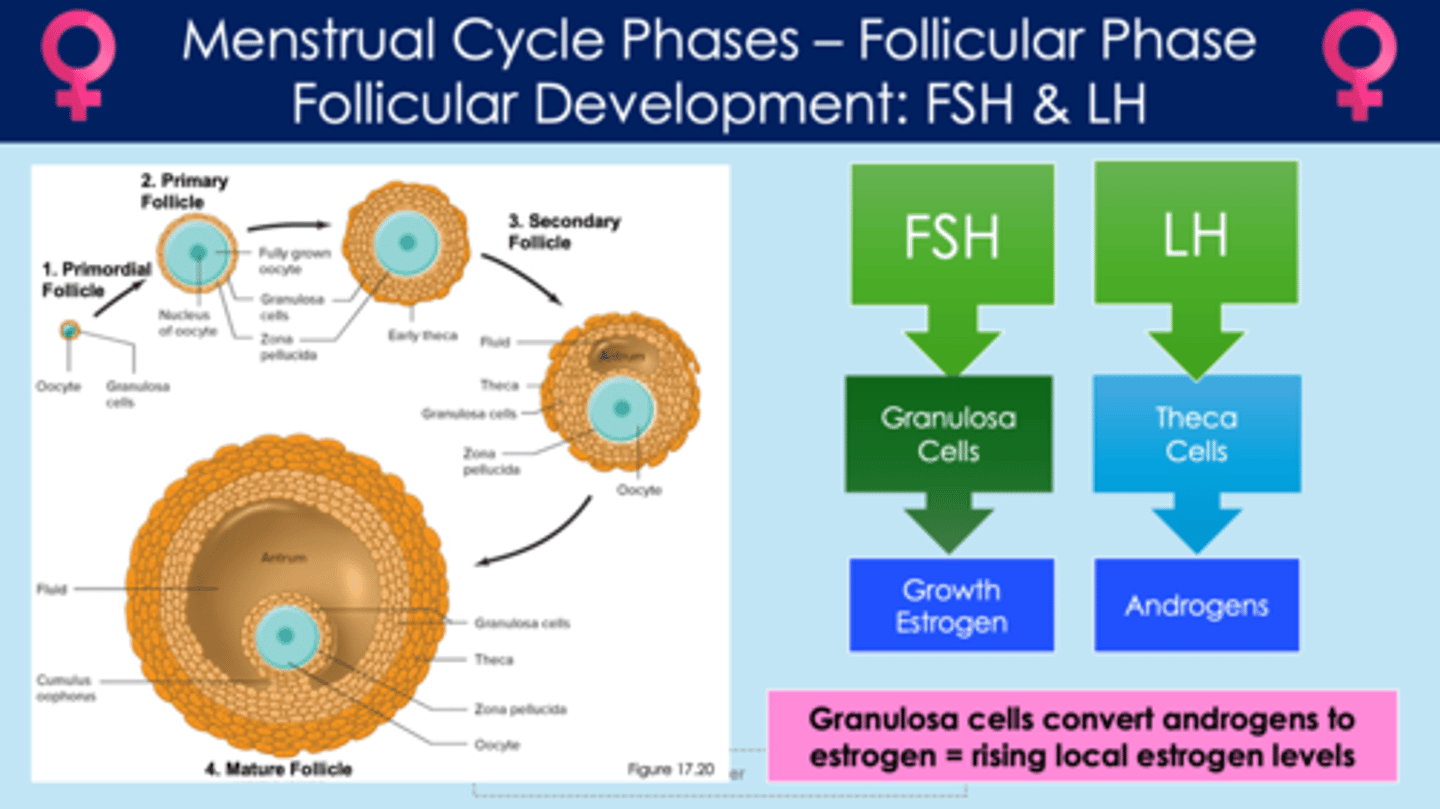
How does a follicle develop?
1. luteinizing hormone (LH) acts on theca cells
2. theca cells release androgens
3. follicle-stimulating hormone (FSH) acts on granulosa cells
4. granulosa cells grow and multiply through mitosis; then release estrogen
5. grandulosa cells convert androgens into estrogen
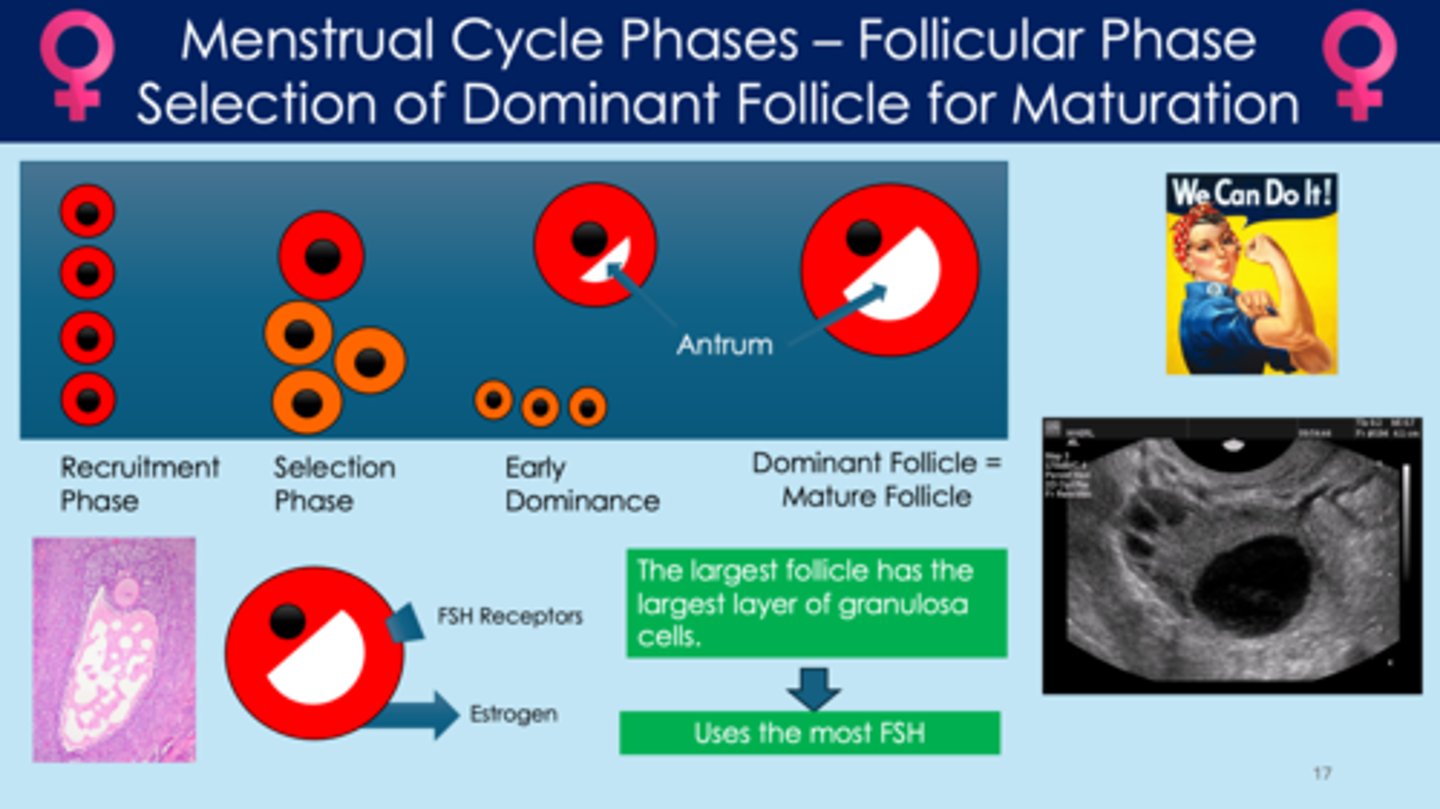
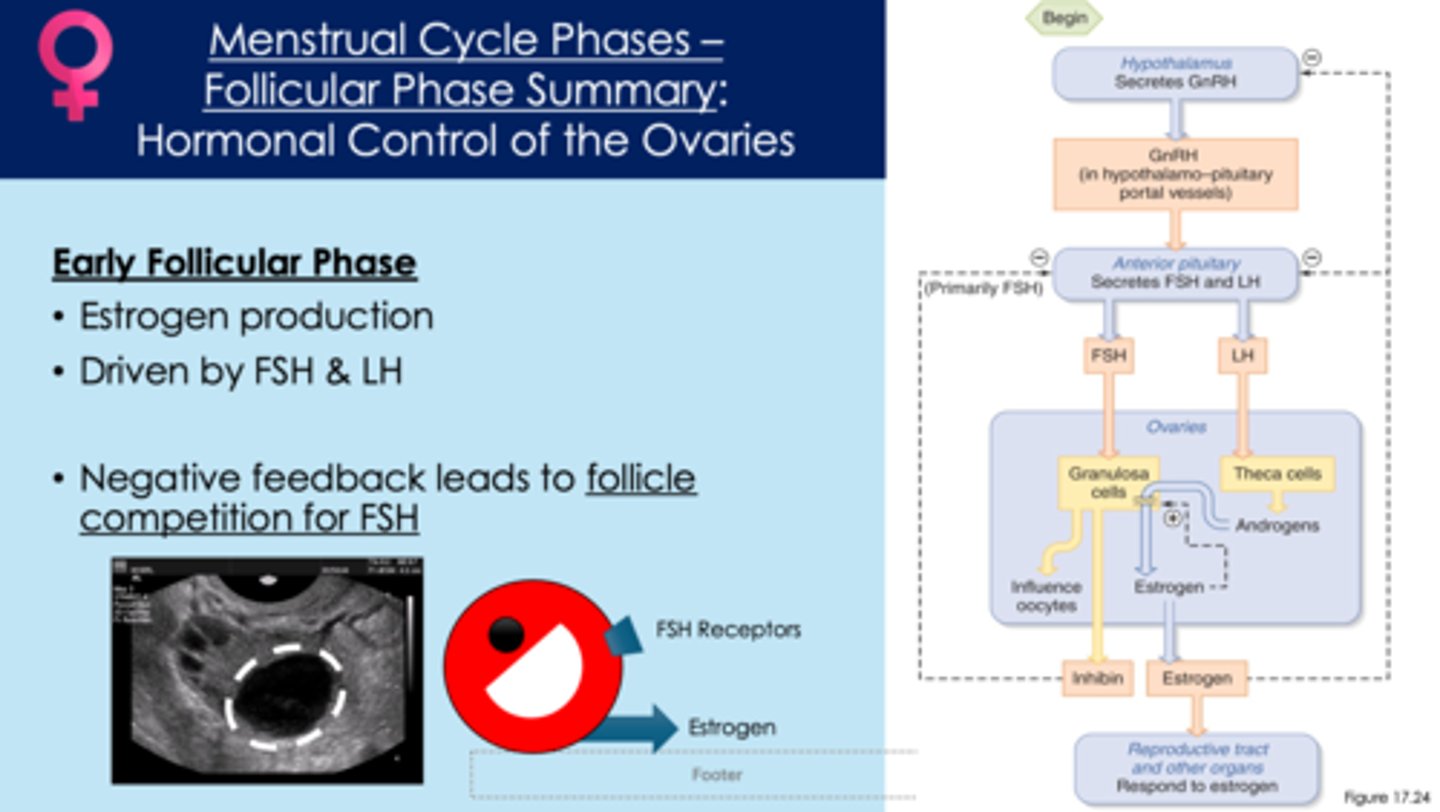
In early follicular development, what is selection of dominant follicle for maturation?
- one follicle is selected for development and gets all the hormones; the rest of the follicles stay small
- FSH controls this process
- the largest follicle has the largest amount of granulosa cells
- uses the most FSH and produces the most estrogen
recruitment phase > selection phase > early dominance > mature follicle/dominant follicle
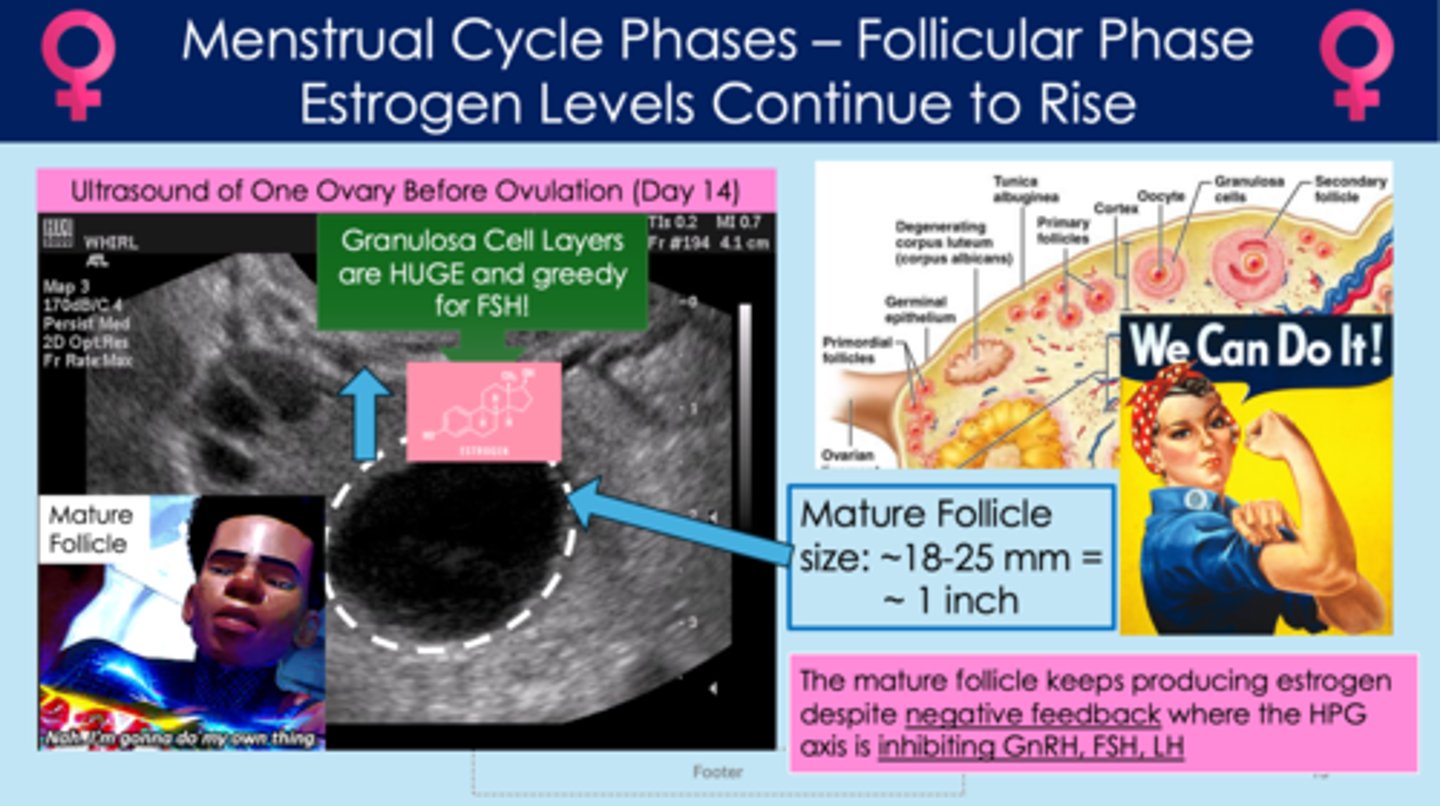
During the late follicular phase, how does the mature follicle get around the hypothalamic-pituitary-gonadal axis (HPG) negative feedback loop?
- the mature follicle releases lots of estrogen
- rising estrogen levels will inhibit LH, FSH, and GnRH release (negative feedback)
- BUT the mature follicle doesn't care! it uses its granulosa cells to pull surrounding FSH from other follicles and continues to produce estrogen, despite the negative feedback loop
- the ovarian estrogen is now extremely high; this estrogen to act back on the anterior pituitary gland and release more FSH and LH (positive feedback)
In the late follicular phase, what is the LH surge? What does the LH surge lead to?
- massive surge of luteinizing hormone (LH) causes granulosa cells to break down; due to positive feedback loop when estrogen levels get extremely high
- antrum size increases; blood flow
- walls of the follicle break down, and the egg leaves the follicle (ovulation)
- LH surge leads to ovulation
*entire pathway listed here*
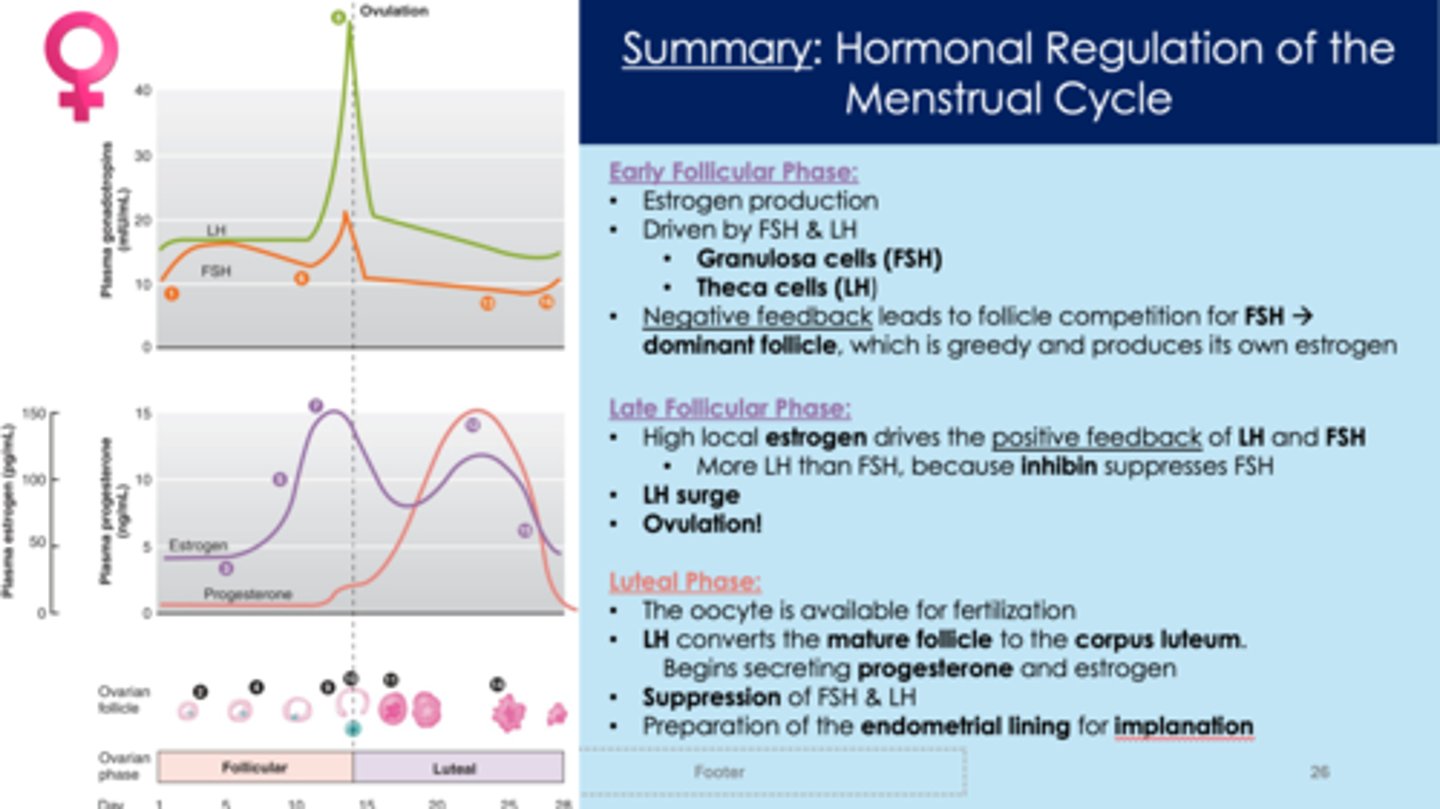
early follicular phase:
1. hypothalamus releases GnRH
2. GnRH acts on anterior pituitary "gonadotroph" receptors
3. anterior pituitary releases FSH and LH
4. FSH stimulates granulosa cell growth
5. LH stimulates androgen production
6. androgen is converted to estrogen by granulosa cells
late follicular phase:
7. during the late follicular phase, the follicle sequesters FSH; it continues to produce estrogen despite the negative feedback loop that estrogen typically follows under normal circumstances (positive feedback)
8. granulosa cells release inhibin and inhibits FSH release by anterior pituitary
9. massive surge of luteinizing hormone (LH) causes granulosa cells to break down, due to positive feedback
10. antrum size increases; blood flow increases
11. walls of the follicle break down, and the egg leaves the follicle (ovulation)
During ovulation, what happens?
- massive LH surge; granulosa tissue is broken down
- oocyte leaves the follicle
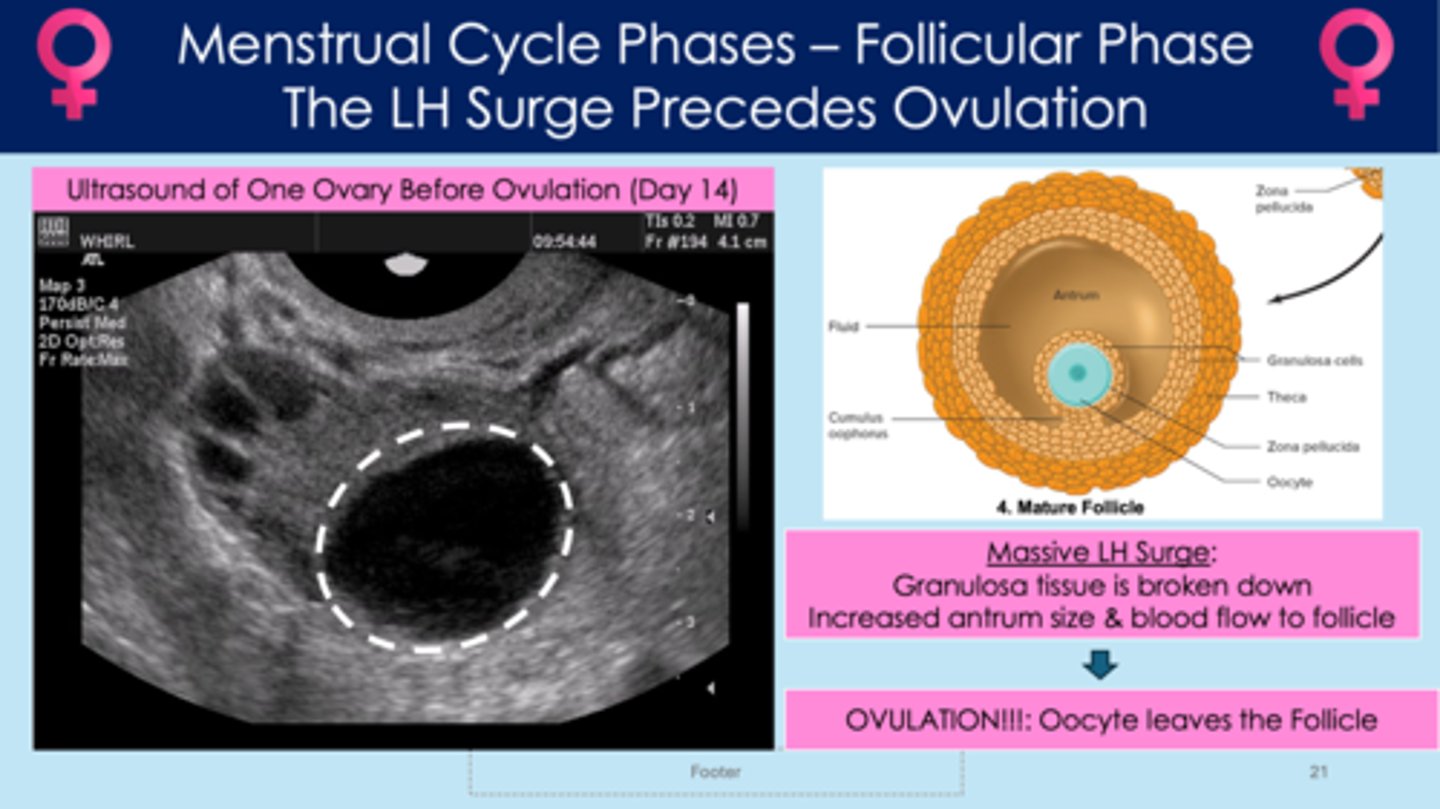
Around what day in the menstrual cycle occur?
- day 14
Good helpful chart
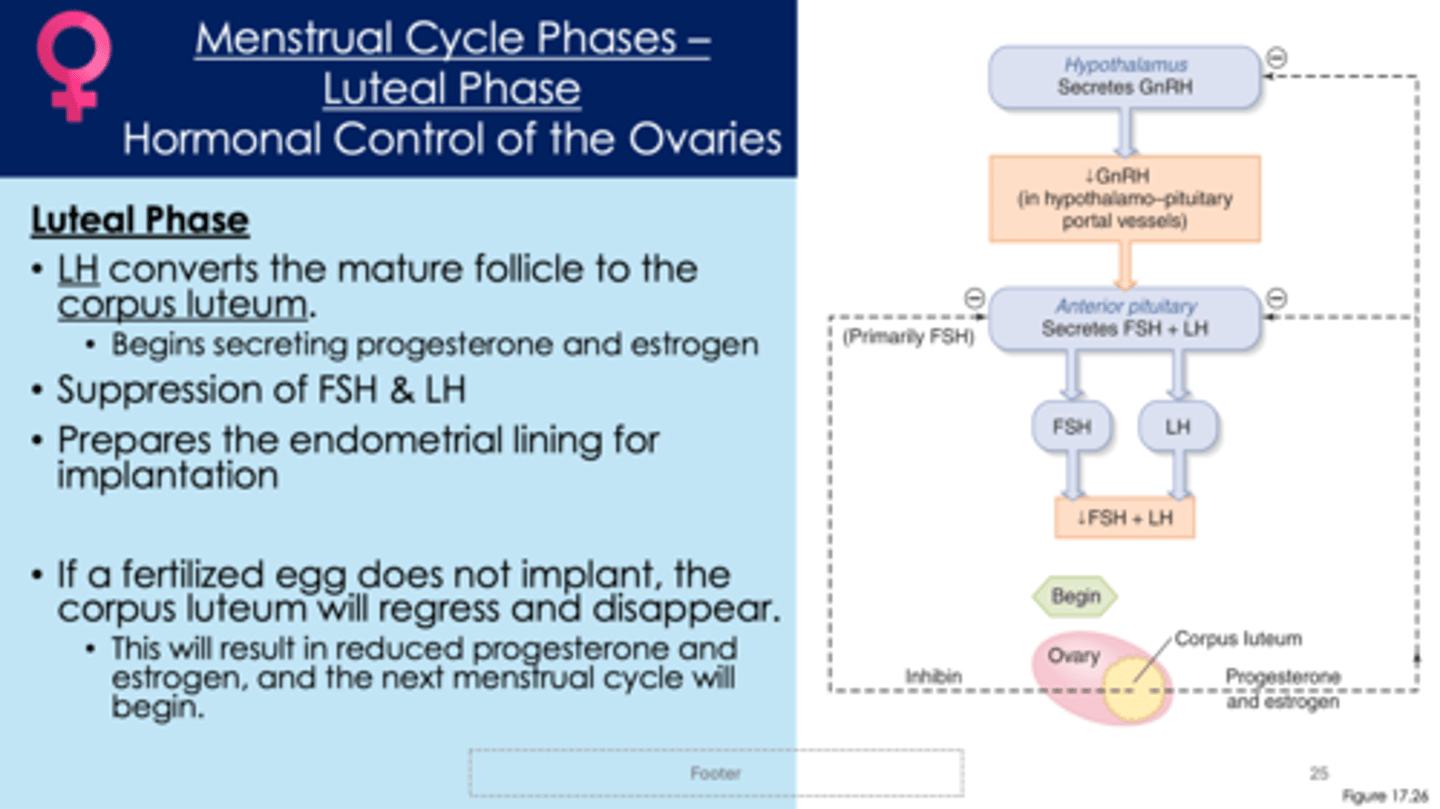
What is the luteal phase?
- second half of menstrual cycle
- the oocyte is available for fertilization
1. luteinizing hormone (LH) converts the mature follicle to the corpus luteum
2. corpus luteum creates its own progesterone and estrogen
3. FSH and LH get inhibited
4. prepares the endometrial lining for implantation
5. if a fertilized egg does not implant, the corpus luteum will regress and disappear; progesterone and estrogen decrease; the endometrial lining will be shed, triggering a period
Good summary chart
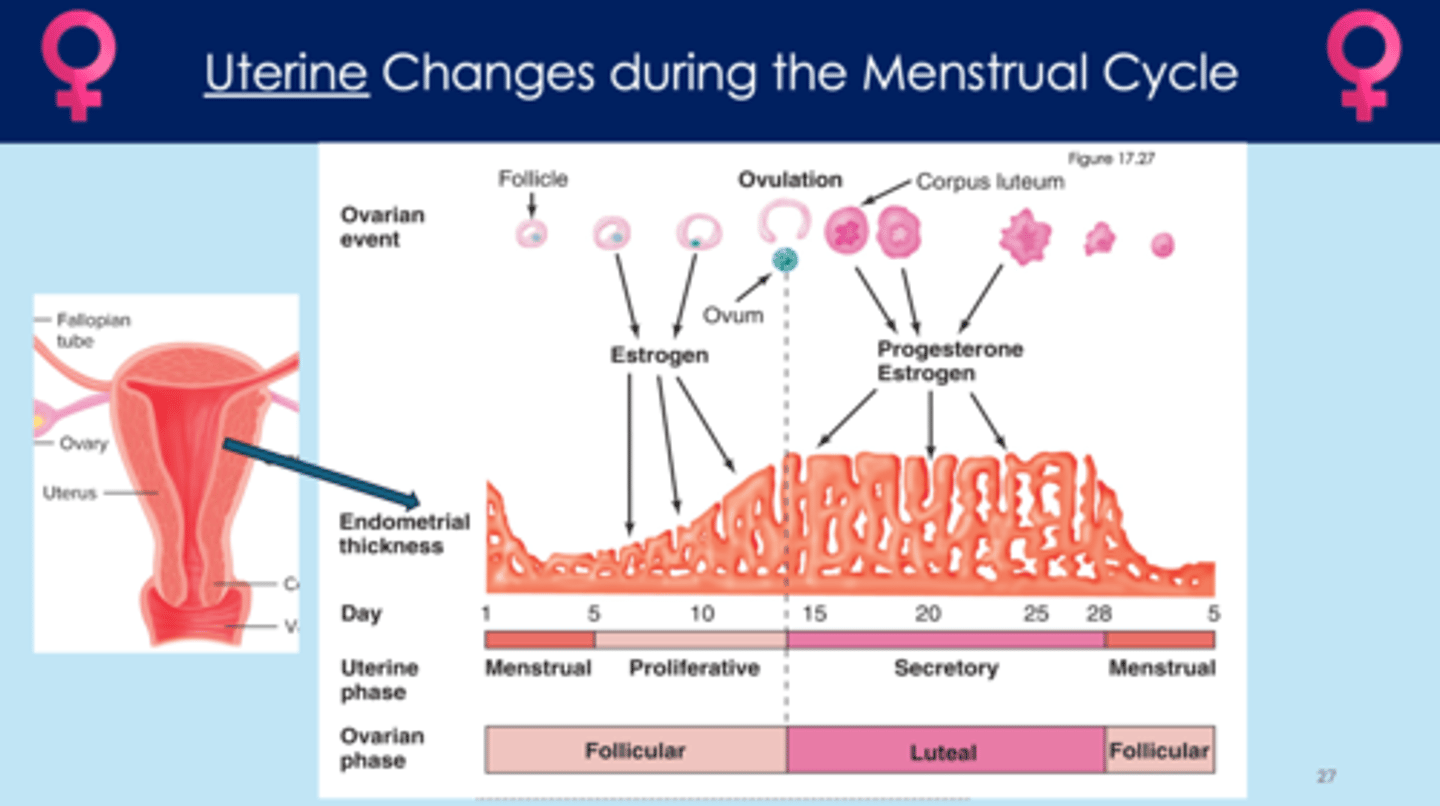
How does the uterus change during the menstrual cycle?
- estrogen released, increasing size/thickness of endometrial lining
- progesterone maintains the thick endometrial lining
- thick endometrial lining is important for implantation
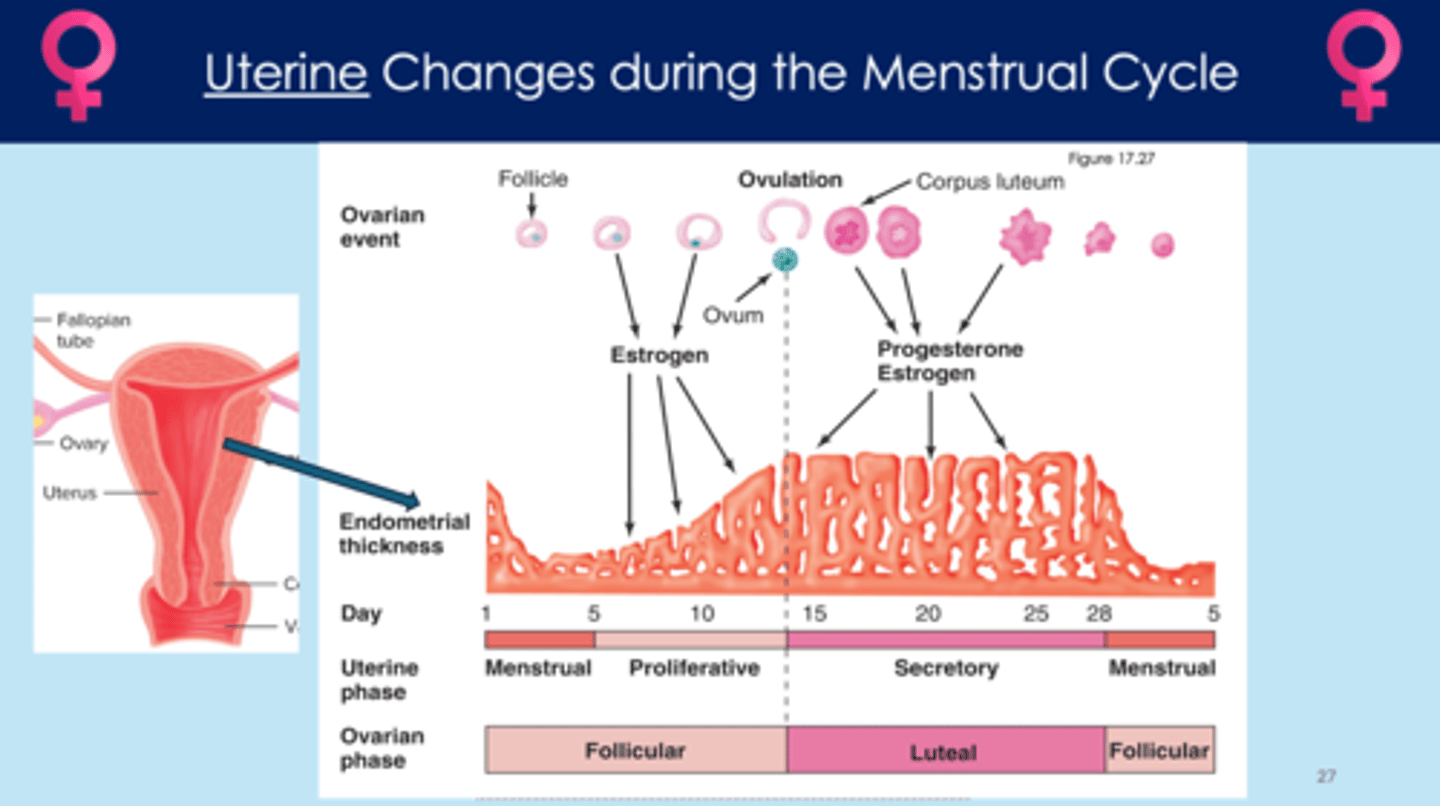
What is progesterone? Why is it important?
- maintains the size/thickness of the endometrium
When is the endometrium the thickest?
- during the luteal phase
After fertilization, what happens?
- sperm enters the egg
- zona pellucida prevents more sperm from entering the egg
- secondary oocyte; fertilized egg undergoes meiosis
- continues to divide and becomes a blastocyst (5 day process)
- blastocyst is an embryo that gets implanted into the uterus
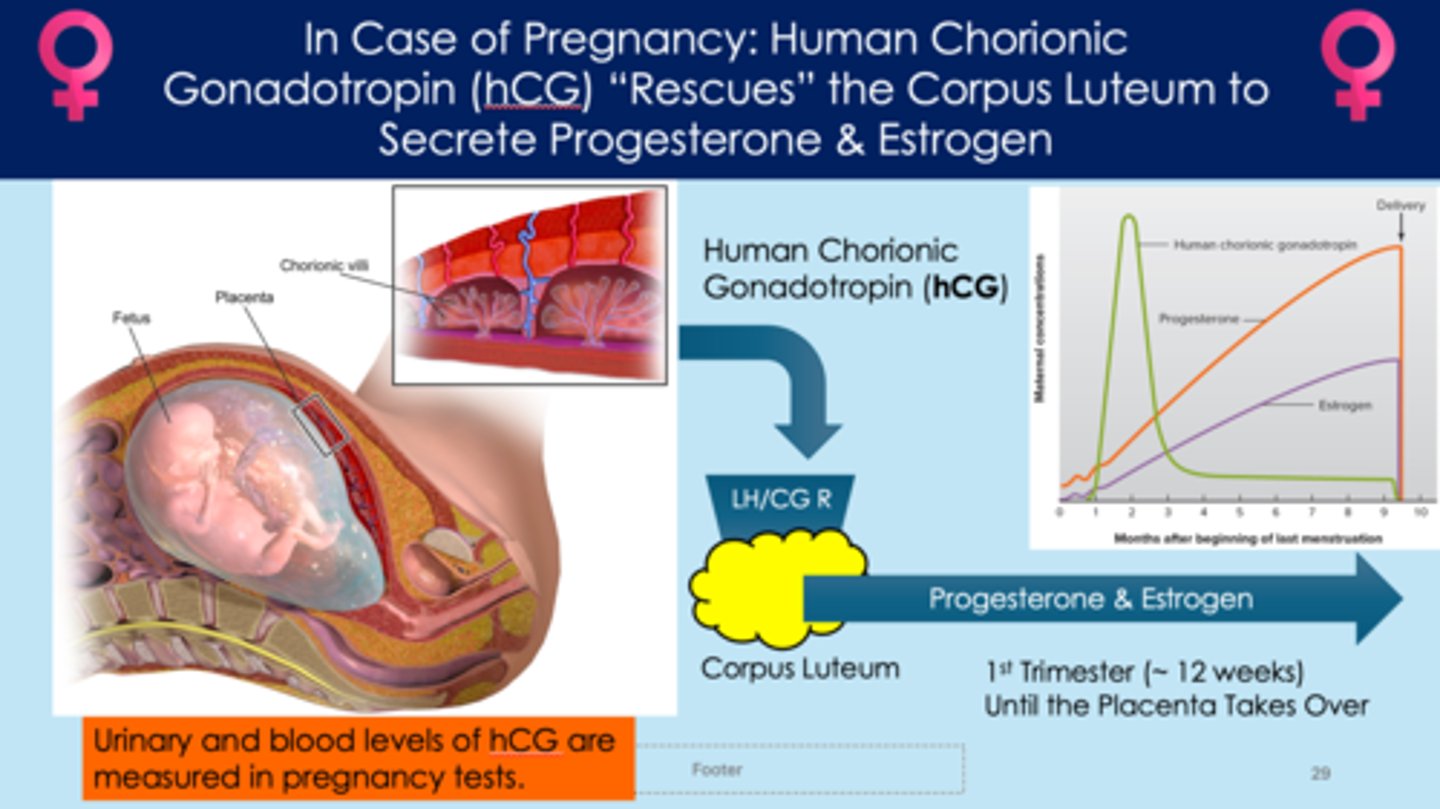
During a pregnancy, what hormone "rescues" the corpus luteum?
- embryo releases human chorionic gonadotropin (hCG)
- acts on corpus luteum; causes to continue producing progesterone and estrogen
- corpus luteum will continue to produce estrogen and progesterone until the placenta takes over around 12 weeks