Commissaris Ch 12 ligands and receptors
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
_______________ is the process by which cells release, transmit, receive, and respond to info from their environment
cell signaling
what is the foundation of pharmacology
physiology
= drugs work as ligands at receptors involved in already existing processes
what are the 3 main players involved in intercellular signaling
1. signaling cell= makes the ligand
2. ligand= transmits info from signaling cell to recipient cell
3. recipient cell= receives ligand
endogenous ligand
any substance, produced within the body, that selectively binds to the type of receptor that is under study to initiate some change
using insulin as an example, identify the 3 main players of cell signaling
signaling cell= pancreatic beta cells (release insulin)
ligand= insulin
recipient cell= insulin receptors in muscle
explain the steps of intercellular signaling
1. synthesis and/or storage of ligand
2. release of ligand (via stimulus) and transport to target
3. formation of ligand-receptor complex
4. receptor-based change in cell function
5. removal of ligand
what is the difference between substrate-enzyme and drug-receptor
sub/enz= substrate is CHANGED to form new PRODUCT
drug/receptor= drug LEAVES receptor while EFFECT happens (drug is not changed!)
what are the 4 ways endogenous ligands can be classified
1. chemistry/structure
=charged vs non-charged; small organic vs protein
2. receptor with which it interacts
=extracellular or intracellular?
3. anatomy and phys
=NT (local), hormones (distant), steroids (intracellular)
4. signal transduction mechanism
CRAS
what determines whether a ligand acts extracellularly or intracellularly
whether it can penetrate membrane
hydrophilic ligand= cell surface
hydrophobic ligand= intracellular
T/F: a polar ligand will work on intracellular receptors
false!
-polar ligands are hydrophilic and work on the cell surface.
-nonpolar ligands are hydrophobic and can get pass the bilayer
exocrine vs endocrine glands
Exocrine glands secrete their products into ducts, NOT BLOOD STREAM (ex: sweat, salivary)
Endocrine glands secrete hormones directly into the bloodstream
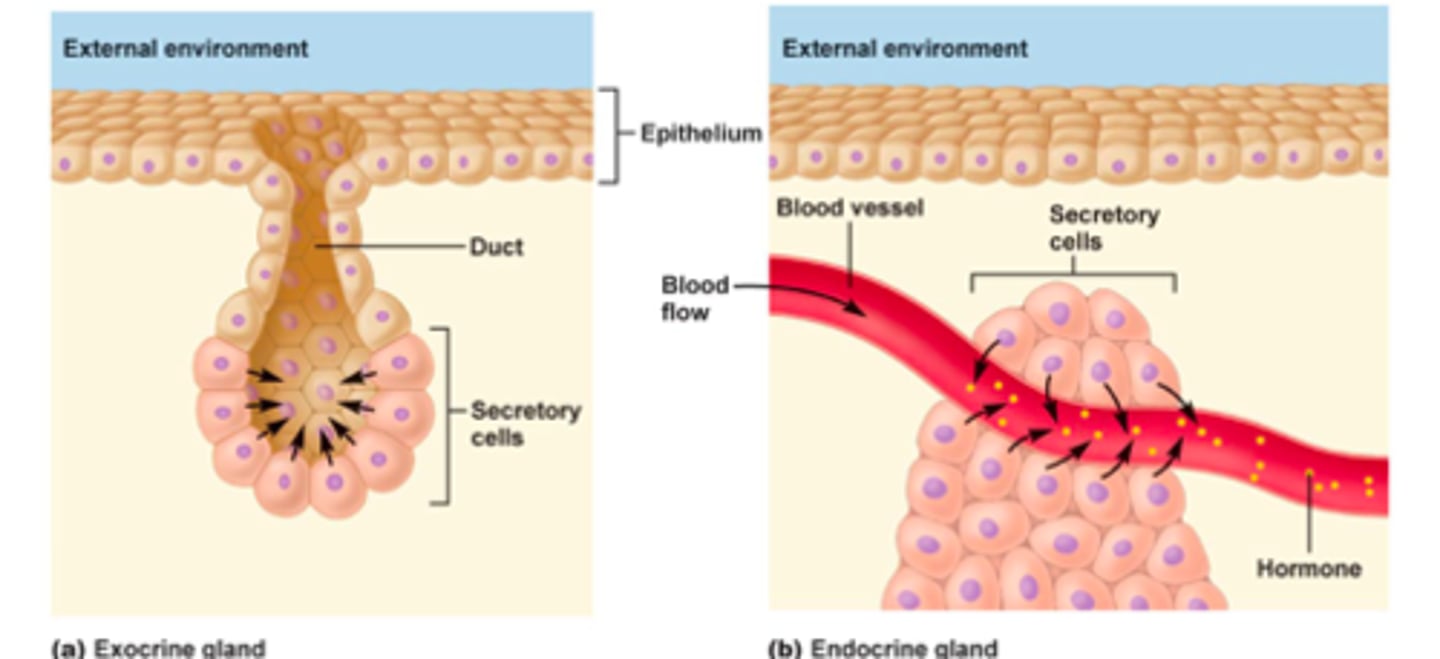
hormones
chemical messengers that are manufactured by the endocrine glands, travel through the bloodstream, and affect other tissues (ex: insulin)
3 types of hormones based on chemistry
1. steroids
2. amino acid derivatives
3. peptides/proteins
intracellular hormones are hydro____ and _________ the cell membrane
hydrophobic; can cross cell membrane (or can be transported into cell)
what do most intracellular hormones modulate
gene expression in target cells
extracellular hormones are hydro____ and _________ the cell membrane
hydrophilic (charged); cannot cross cell membrane
how is endocrine hormone signaling terminated
elimination of hormones from blood (via liver metabolism)
3 features of local signaling of endogenous ligands
1. no bloodstream transport needed
2. effects are near the source of the signal
3. short-term effects
(ex: neurotransmitters)
3 types of local signaling
1. paracrine= cell A to cell B
2. autocrine= cell A to cell A
3. juxtacrine= direct contact btwn cell A and cell B
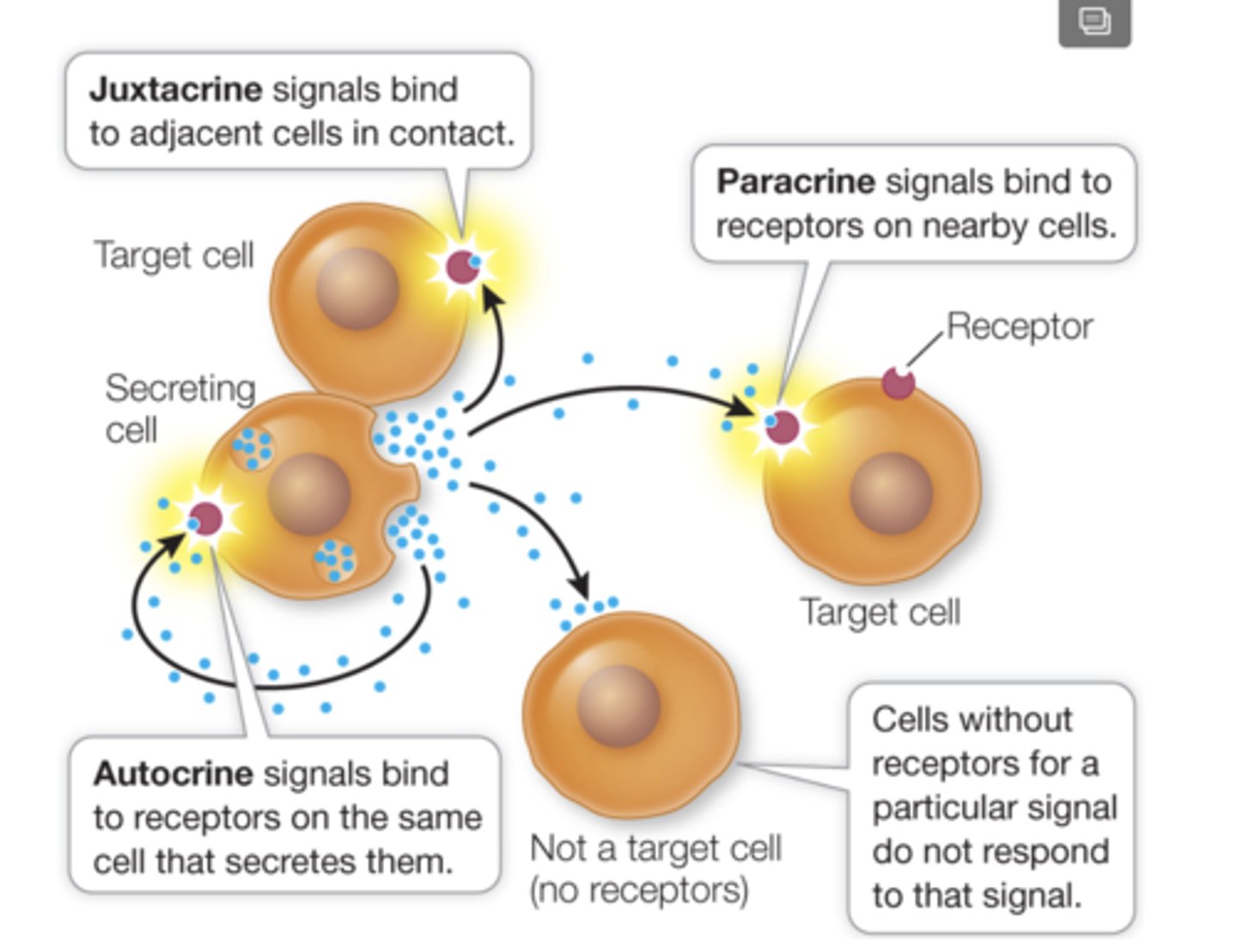
what is the most prevalent form of local signaling
paracrine (cell A to cell B through fluid)
T/F: exocrine glands play a small part in intercellular signaling
false. they are not a part of cell signaling. they immediately release product into ducts
3 ways you get specificity of ligand-receptor interactions
1. chemical specificity of ligand-receptor
2. anatomical specificity via receptor location
3. limited distribution of ligand in body
If TSH goes everywhere in the body when it is released, why does it only act on the thyroid?
1. chemical specificity= only binds to thyroid receptors
2. anatomical specificity= receptor is only found in thyroid gland tissue
even though NE can bind to many tissues and many receptors, what allows it to only act on one specific target?
1. limited distribution
= the neuron it is released from is close to target cell; little opportunity to diffuse to affect other cells
stereoselective
describes receptors; they prefer one stereoisomer over another of a ligand
ex: levothyroxine: levo fits better than dextro
stereo complementarity
ligand must be the correct stereoisomer to fit stereoselective binding site of receptor
recognition
ligand binds to receptor (usually reversible)
noncatalytic vs catalytic receptors
non= majority
-ligand is agonist/antagonist on RECEPTOR; released UNCHANGED
catalytic= minority
-works on enzymes
- ligand can be ENZYME inhibitor, or SUBSTRATE for enzyme (changed)
ex: lisinopril= ACE inhibitor
what are receptor subtypes
groups of receptors with similar binding domains but different signal transduction mechs
= so same ligand, different effect
ex: NE -> alpha 1, alpha 2, beta 1, beta 2
T/F: if 2 receptors are both noradrenergic receptors, they have identical signal cascades
false. they may be different NE subtypes and have different response
ex: alpha 1, alpha 2, beta 1, beta 2
what are some differences between drugs that bind to only one receptor subtype and those that bind to many subtypes
one subtype: drug is selective
many subtypes: may cause unwanted side effects
__________________ refers to the process by which an extracellular ligand-receptor interaction causes an intracellular change
signal transduction
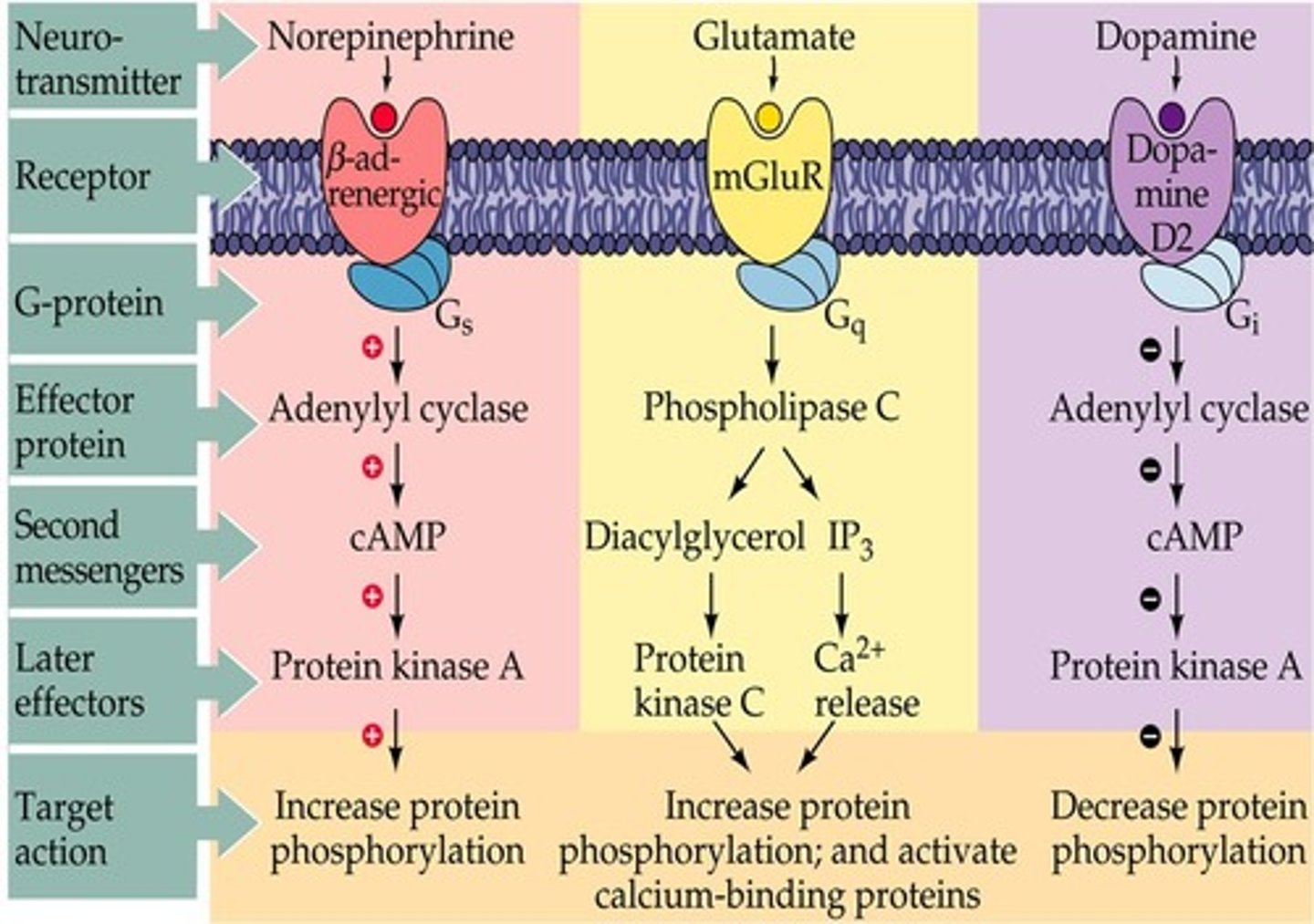
first vs second messengers
first= original ligand that binds to receptor
second= short lived compound within cell that transmits signal
examples of second messengers
cAMP, calcium ions, IP3, DAG
old way vs new way of receptor classification
1. old way= receptor classified by what LIGAND it binds
ex: NE receptor
2. new way= based on location and type of SIGNAL TRANSDUCTION pathway
ex: GPCR
3 types of extracellular cell-surface receptors
1. ion channel
2. GPCR
3. enzymatic
** ligands cannot cross membrane (hydrophilic, polar)
2 types of intracellular receptors
1. transcription regulation (nuclear)
2. intracellular enzymes
**ligands cross cell membrane (hydrophobic)
common ions that pass through ion channels
Na, K, Ca, Cl
T/F: ions can pass through the lipid membrane and act on intracellular receptors
false. ions are charged, therefore they cannot pass the membrane and require ion channels
ligand vs voltage gated ion channels
1. Ligand
- ligand binds to ion channel receptor= conformational change
- change opens ion channel and allows ion movement
2. Voltage
-membrane voltage reaches threshold= triggers opening of channel
-occurs in excitable cells (neuron, cardiac)
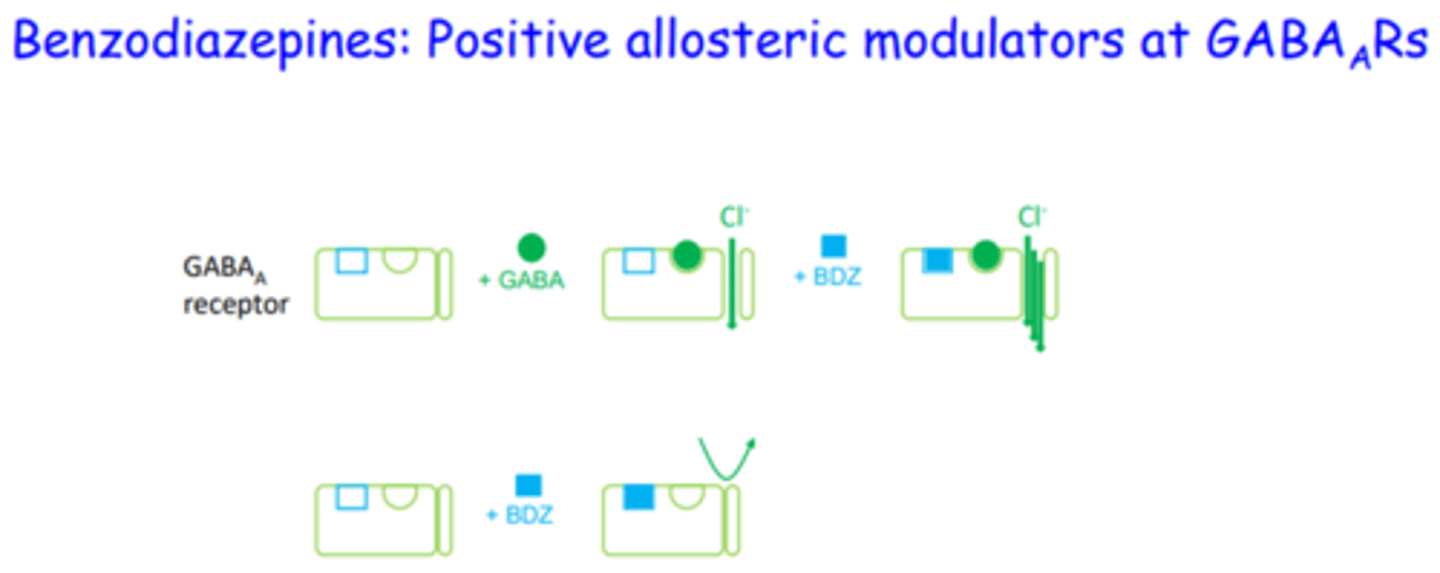
the GABA receptor is an example of what kind of receptor? how does it work?
Ligand gated ion channel receptor
1. GABA binds to receptor on Cl- ion channel outside of cell
2. conformational change= Cl- ions enter cell
3. negative Cl ions make cell hyperpolarized (more negative)= INHIBITORY EFFECT
T/F: GABA binds to its receptor on the Cl ion channel, allowing Cl to enter and an action potential to form
false. Cl- is negative and makes the cell hyperpolarized, meaning it is less likely for an AP to form
= GABA is inhibitory
T/F: when a ligand binds to its voltage gated ion channel, the ion channel opens
false. voltage-gated ion channels do not have ligand receptors
examples of excitable cells that have voltage gated ion channels
Neural and cardiac
= Na+ rushes in
which extracellular cell surface receptors are most often targeted by drugs
GPCRs (more than half of drugs on market)
which receptor is a single peptide with 7 transmembrane regions
GPCR
what are the 3 subunits of the G protein in GPCRs
1. alpha= GTP ->leaves and interacts with adenylate cyclase
2. beta
3. gamma
Gs, Gi= linked to ______
Gq= linked to ______
Gs, Gi= linked to _adenylate cyclase__
Gq= linked to __phospholipase C_
the beta 1 adrenergic receptor is a classic example of a ________
GPCR; increase in cAMP
describe what happens to the GPCR when NE binds
1. Ne binds-> GDP is exchanged for GTP on alpha subunit
2. GTP-alpha dissociates and interacts with adenylate cyclase
3. adenylate cyclase: ATP-> cAMP
3. cAMP (2nd messenger) produces intracellular response
4. GTP-> GDP, alpha migrates back
adenylate cyclase
Activated by a GTP-alpha. Converts ATP to cAMP
T/F: enzymatic receptors have 7 membrane spanning regions
false. GPCRS have 7, while enzymatic receptors have 1
which receptors are often found in pairs (dimers)
enzymatic
what happens when a ligand binds to an enzymatic receptor
triggers enzymatic activity inside cell
**the ligand is NOT the substrate for the enzyme
**enzyme can be continuous or non-continuous with receptor
the protein kinase receptor family is an example of what kind of receptor
enzymatic receptor
transcription regulation receptors are also known as __________ and act to ______-
nuclear receptors; ligand acts in nucleus to initiate transcription of RNA from DNA
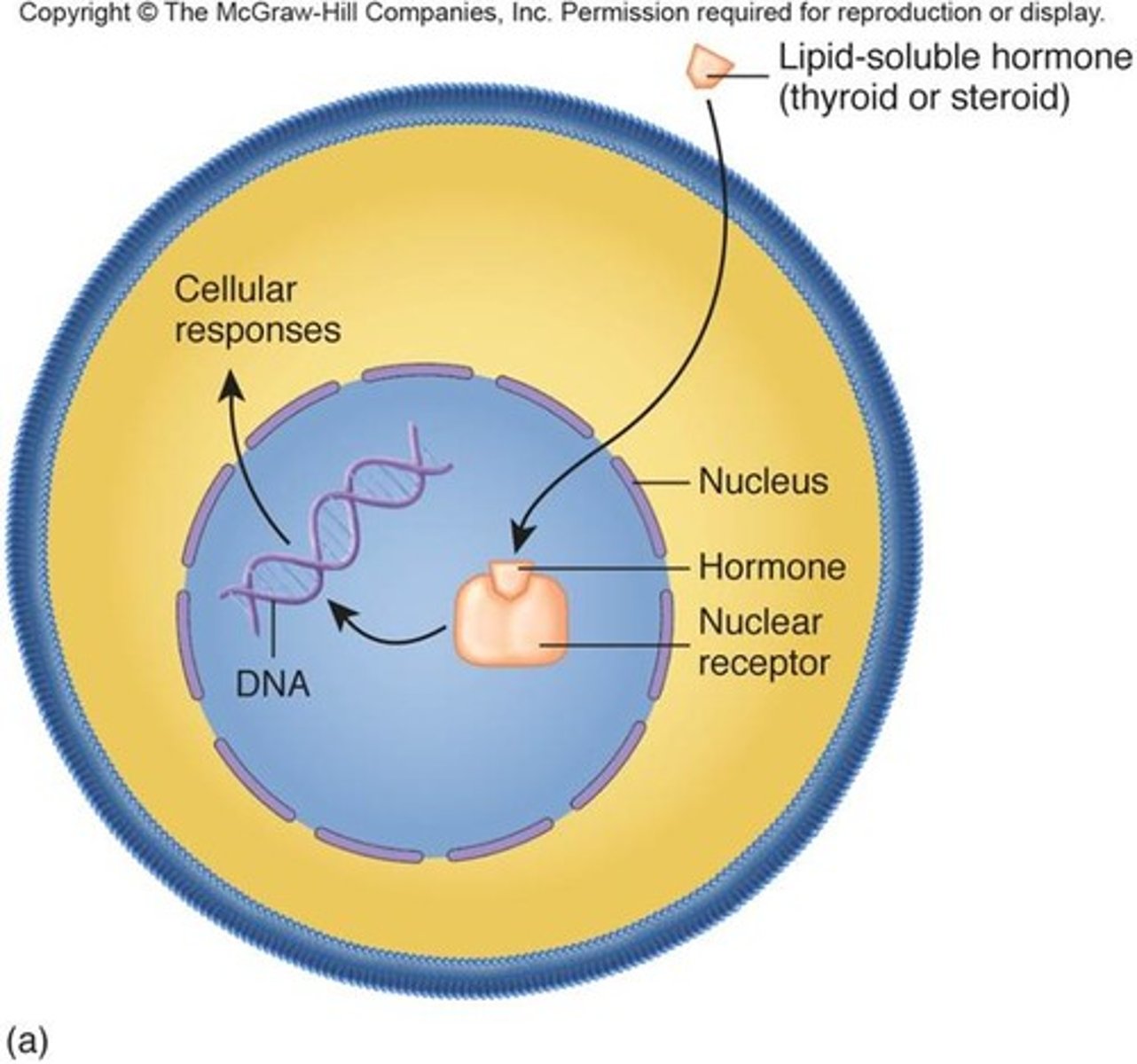
2 subcategories of nuclear receptors
1. steroid (corticosteroids, sex steroids..)
2. non-steroid (thyroid, vitamin D, retinoic acid)
describe what happens in intracellular enzymes
ligand binds to enzyme inside cell and changes into product
OR ligand inhibits enzyme (suicide substrate)
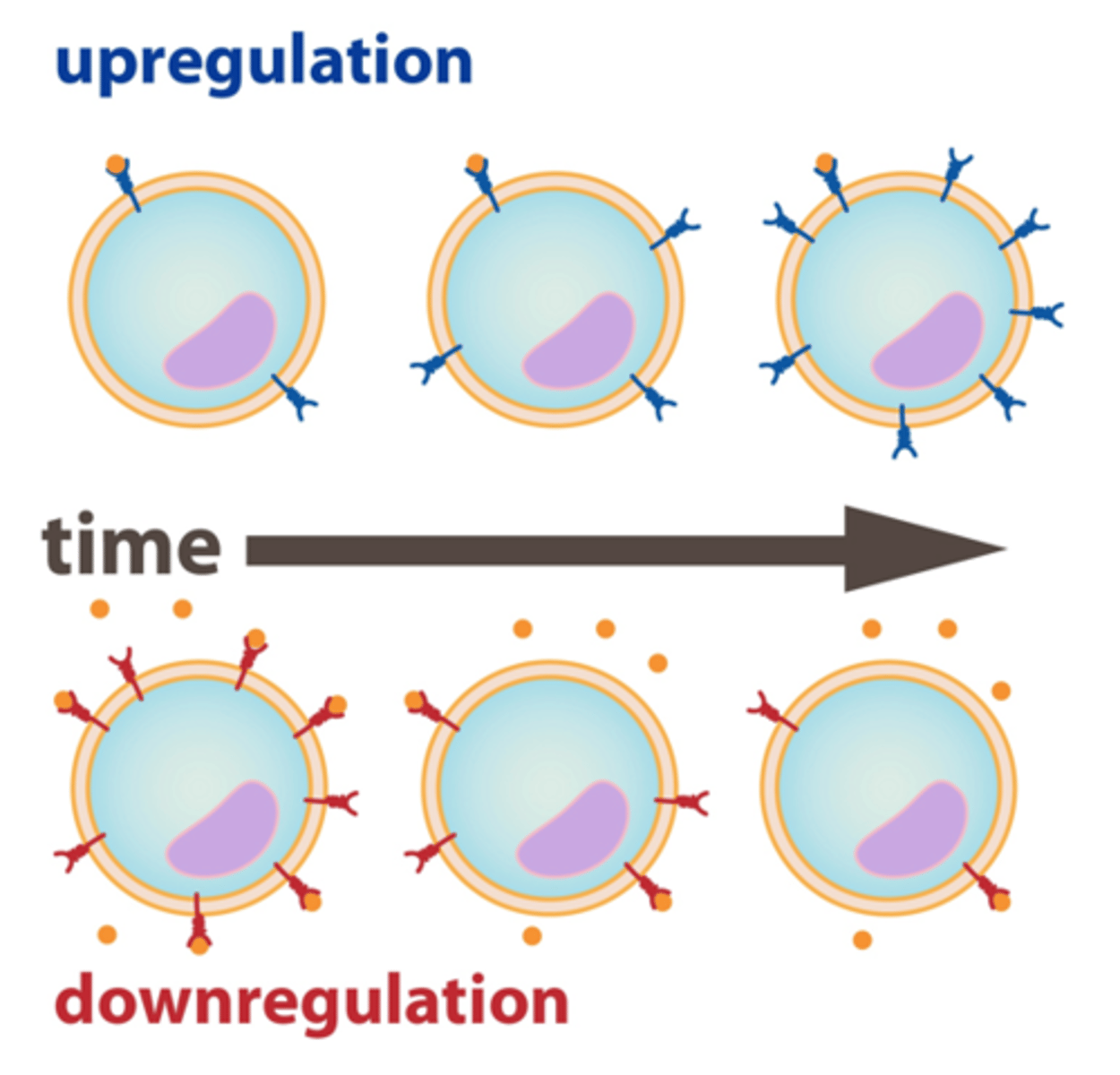
3 factors influencing ligand-receptor interactions
1. ligand concentration (more ligand= more binding)
2. receptor density
3. allosteric modulation
upregulation vs downregulation
1. upregulation: increase in number of receptors
- observed in absence of ligand
ex: increased dopamine receptors in Parkinsons
2. downregulation: decrease in number of receptors
-observed in excess of ligand
ex: chronic beta-agonist treatment (inhalers)
allosteric modulation
2 binding sites: one for ligand and one for modulator (allosteric site)
modulator alters the shape of the ligand binding site and, therefore, the binding characteristics of that site
describe the effect of benzodiazepines as allosteric modulators
BDZs bind to allosteric receptors, causing GABA to bind better to its ligand receptor and therefore increasing the amount of Cl ions moving in