Pulmonary Physiology: Perfusion and Ventilation
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
100 Terms
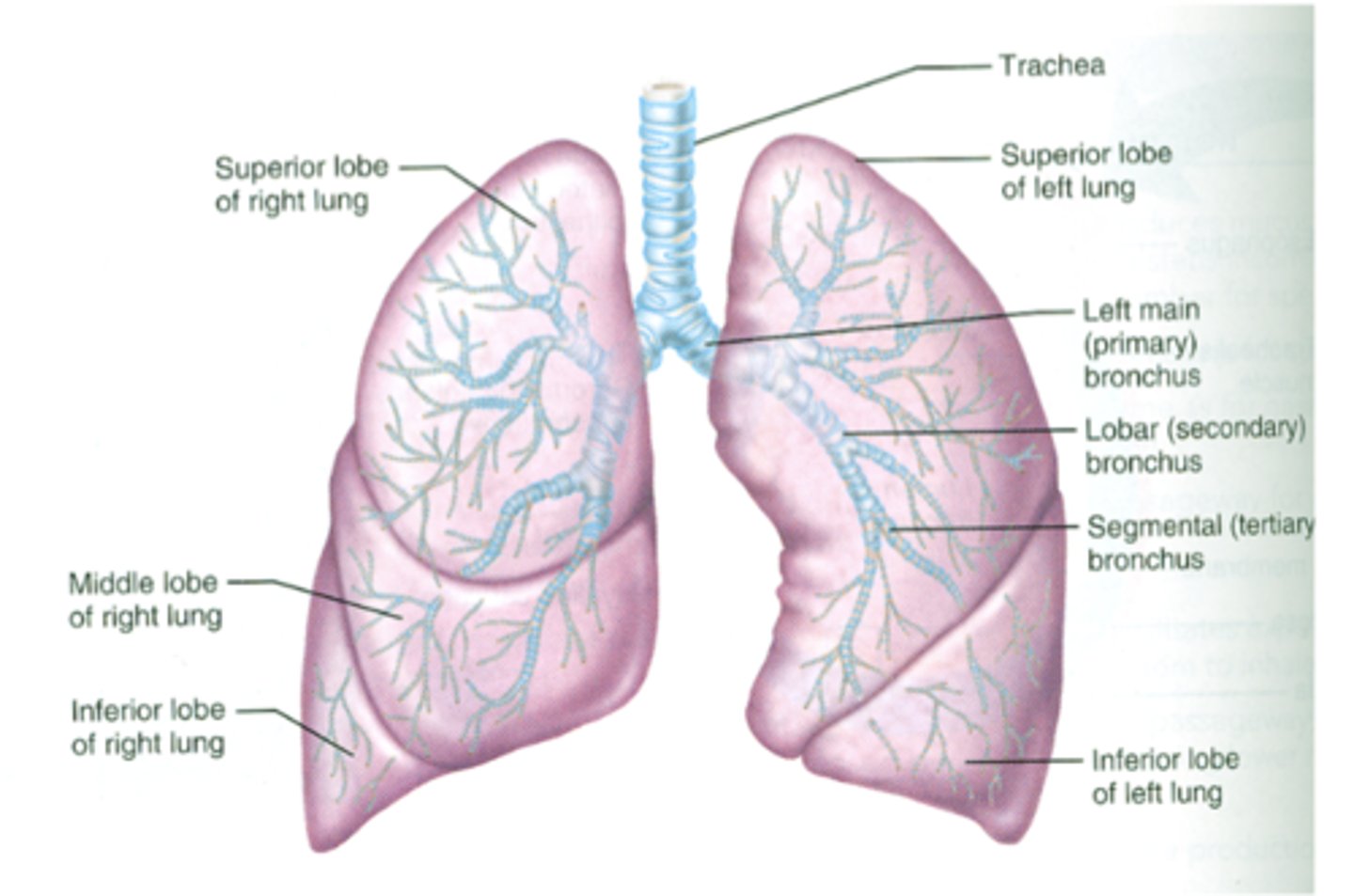
What's considered to be apart of the conducting zone of the lungs?
What is the air-blood interface?
50 - 100 m^2 in area
What is the purpose of the air-blood interface?
large area for exchange of O2 & CO2
What is perfusion?
the flow of blood through the lungs
describe the vasculature in the respiratory zone
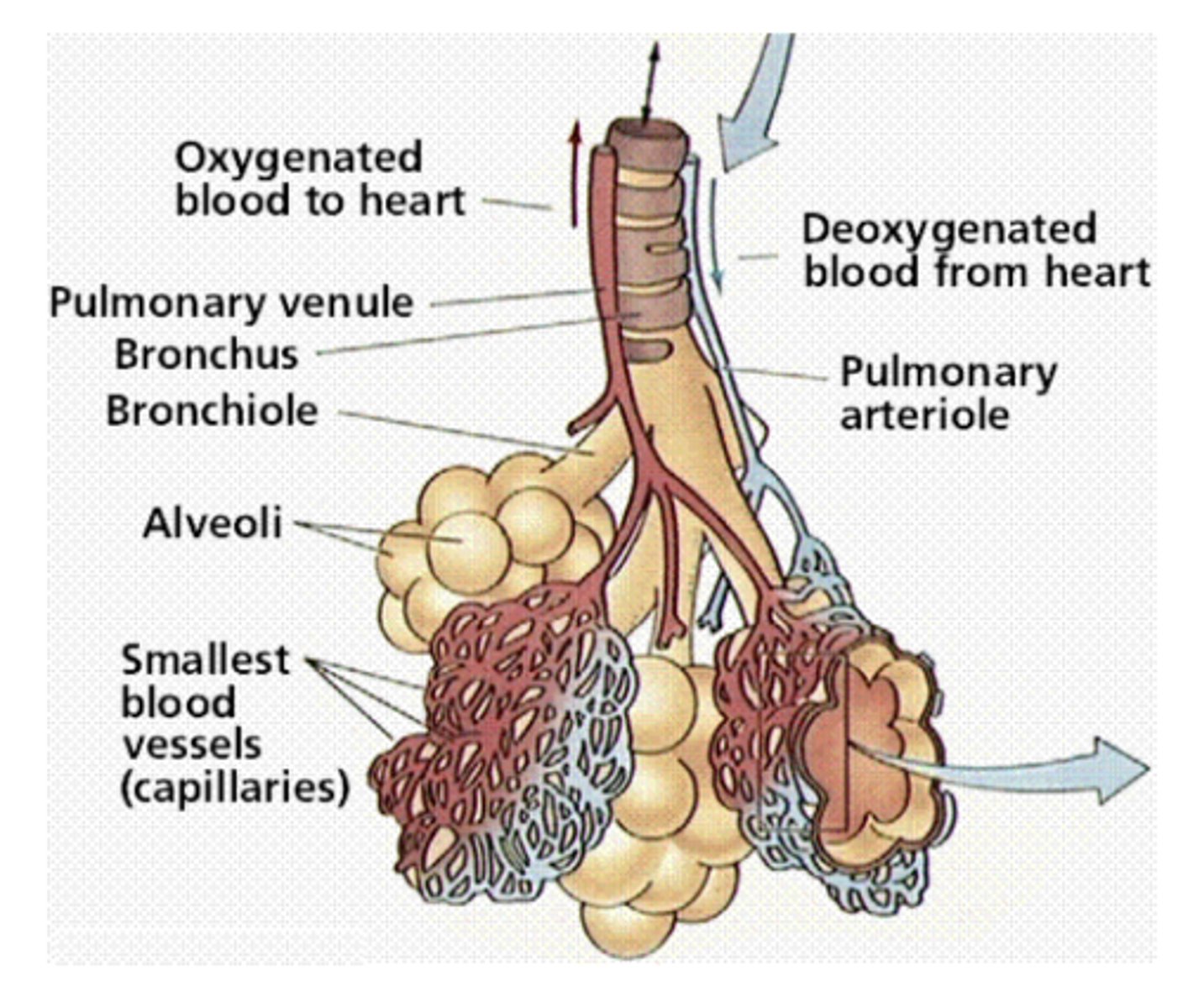
branches of the pulmonary arteries follow the branching of the airways as far as the terminal bronchioles--> then split into capillary beds surrounding the alveoli --> capillary beds fuse --> allows alveoli to be surrounded by a flowing sheet of blood surface area for gas exchange --> capillaries converge ultimately to forms 4 pulmonary veins --> leads to left atrium
What makes up the respiratory zone?
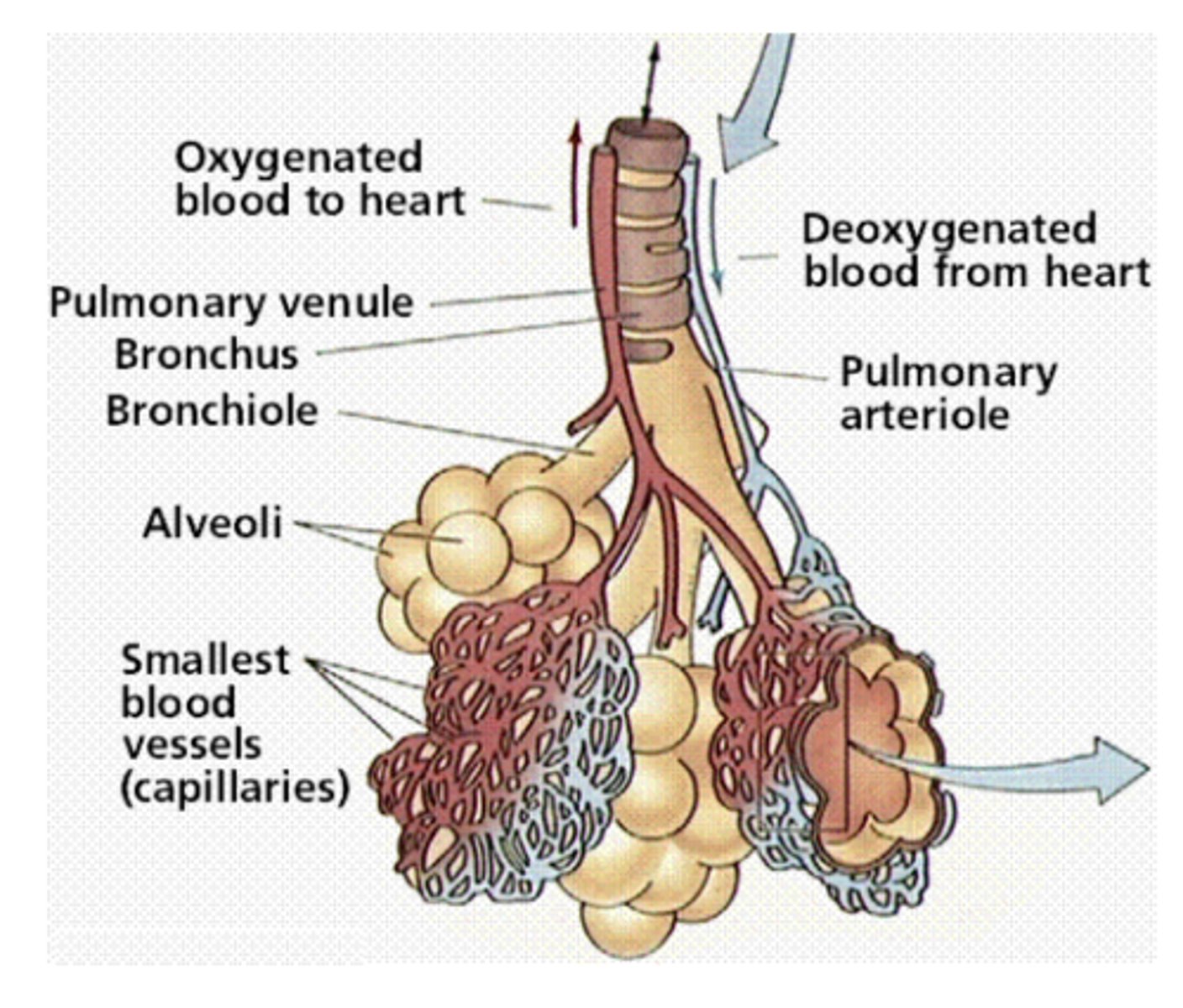
What is the surface area for gas exchange within the respiratory zone of the lungs?
air-blood interface = 50 - 100 m^2
What is the air-blood barrier comprised of?
-alveolar epithelium
-capillary endothelium
-basement membrane = approx 0.5um thick
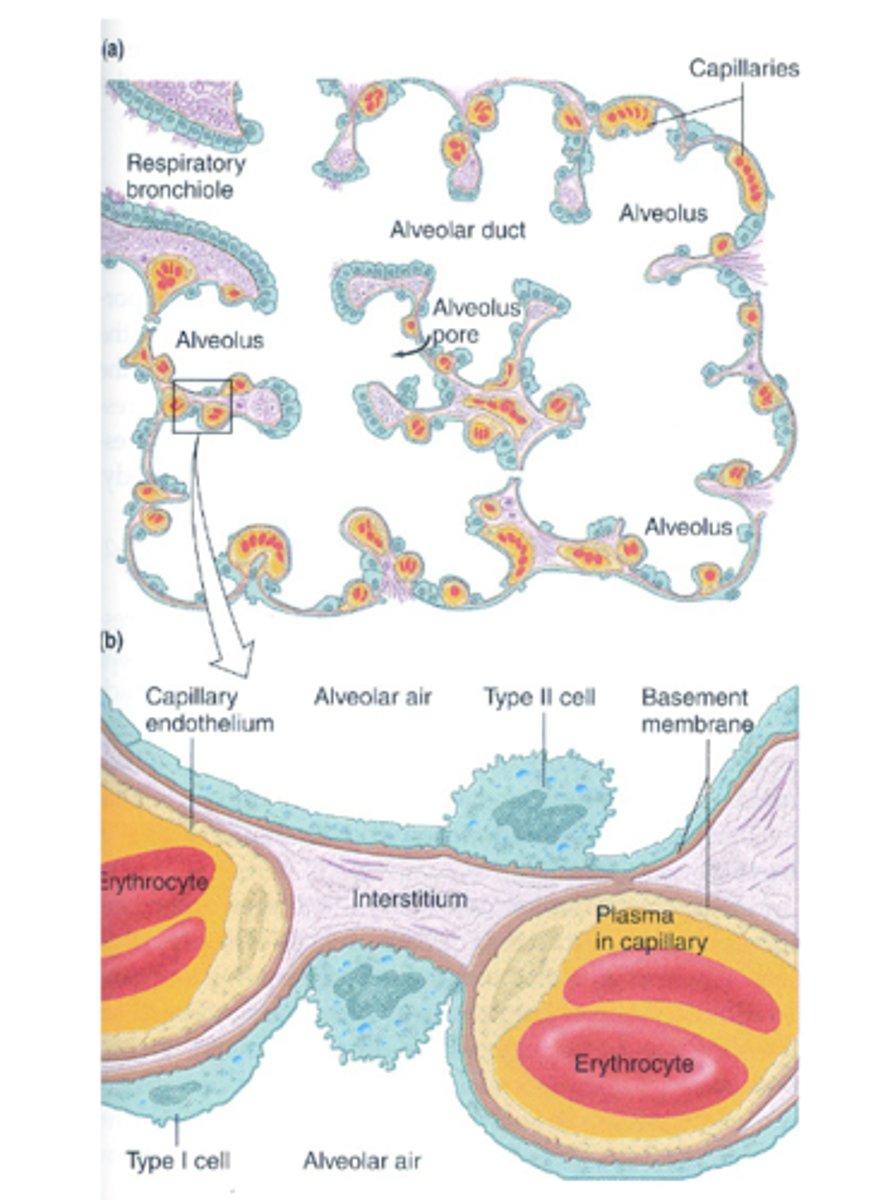
How thick is the basement membrane of the air-blood barrier?
approx 0.5 um
True or False: The pulmonary system handles the same blood flow as does the systemic circulation
True ==> 5 L/min --> flows thru the pulmonary system differently tho
How much blood flows through the pulmonary system every second?
83 mL/ second
How much blood flows through the pulmonary system every minute?
5 L/ min
True or False: Both systemic and pulmonary circulation systems are high pressure
False ==> pulmonary is low; systemic is high
What is the total circulation rime through the pulmonary system at rest?
4 - 5 seconds
At rest, how much blood is in the pulmonary capillary bed in an upright person?
75 mL
At rest, how long does the average erythrocyte take to pass through the alveolar capillary bed?
0.75 seconds
What is the average pulmonary systolic pressure?
25 mmHg
What is the average pulmonary diastolic pressure?
8 mmHg
What is the average pulmonary mean arterial pressure?
15 mmHg = mean pulmonary pressure
What is the average pulmonary alveolar capillary pressure near the arterial end?
12 mmHg
What is the average pulmonary alveolar capillary pressure near the venule end?
8 mmHg
What is the driving force for blood flow in the pulmonary system?
the difference bwtn pulmonary mean arterial pressure - pulmonary venules
15 - 8 = 7 mm Hg
How does the driving force for blood flow in the pulmonary system compare to the driving force for systemic blood flow?
pulmonary blood flow driving force is only 8% of the driving force for systemic blood flow
-pulmonary = 7 mmHg
-systemic = 93 mmHg
How does the pulmonary vascular resistance compare to the vascular resistance of systemic circulation?
pulmonary vascular resistance is only 8% of the systemic vascular resistance
What is the average systemic mean arterial pressure?
95 mmHg
What is the driving force for systemic blood flow?
difference between mean arterial pressure - venule pressure
= 95 - 2 = 93 mmHg
What are the factors that affect pulmonary blood flow? (5)
-compliance of pulmonary vessels
-fluctuations in transmural pressure of alveolar vessels
-lung volume
-hypoxic vasoconstriction
-gravity
What contributes to the high compliance of pulmonary blood vessels?
pulmonary vessels have thin walls & less smooth muscle than systemic vessels
-allows vessels to expand --> can accept large amounts of blood that shift from lower limbs to lungs when a person moves from standing to recumbent position (laying down)
-allows vessels to dilate in response to moderate increases in pulmonary arterial pressure
-causes pulmonary flow to be pulsatile
Why does pulmonary circulation have relatively low pressure?
due to the high compliance of pulmonary vessels
What is the average pulmonary pulse pressure?
pulmonary systolic pressure - pulmonary diastolic pressure
25 - 8 = 17 mmHg
What causes pulmonary capillary flow to be pulsatile?
high compliance of pulmonary vessels (no high resistance arterioles to dampen the pulse like in systemic circulation)
What allows the pulmonary vessels to accept large amounts of blood from the lower limbs when a person moves from standing to a recumbent (laying) position?
high compliance of pulmonary vessels
What allows the vessels to dilate in response ti moderate increases in pulmonary arterial pressure?
high compliance of pulmonary vessels
How does an increase in pulmonary arterial pressure affect the resistance of the pulmonary vessels?
increase in pulmonary arterial pressure = decrease in resistance = increase in pulmonary blood flow
*increase in arterial pressure in cases of increased cardiac output (ex: exercise)
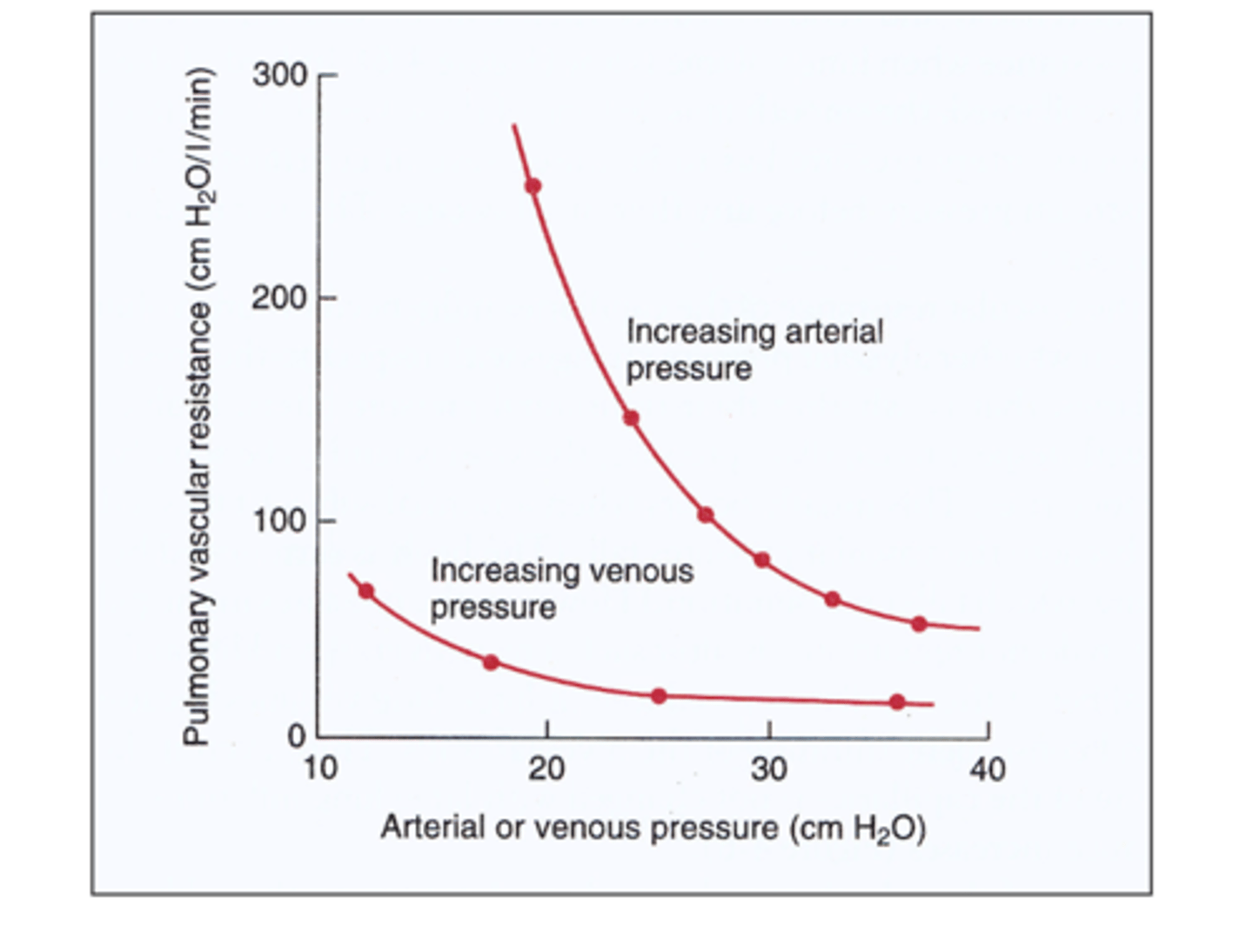
What effect will an increase in cardiac output have on pulmonary arterial pressure and pulmonary vascular resistance?
-increased pulmonary arterial pressure
-decreased pulmonary vascular resistance --> allows more blood to flow thru lungs for more gas exchange
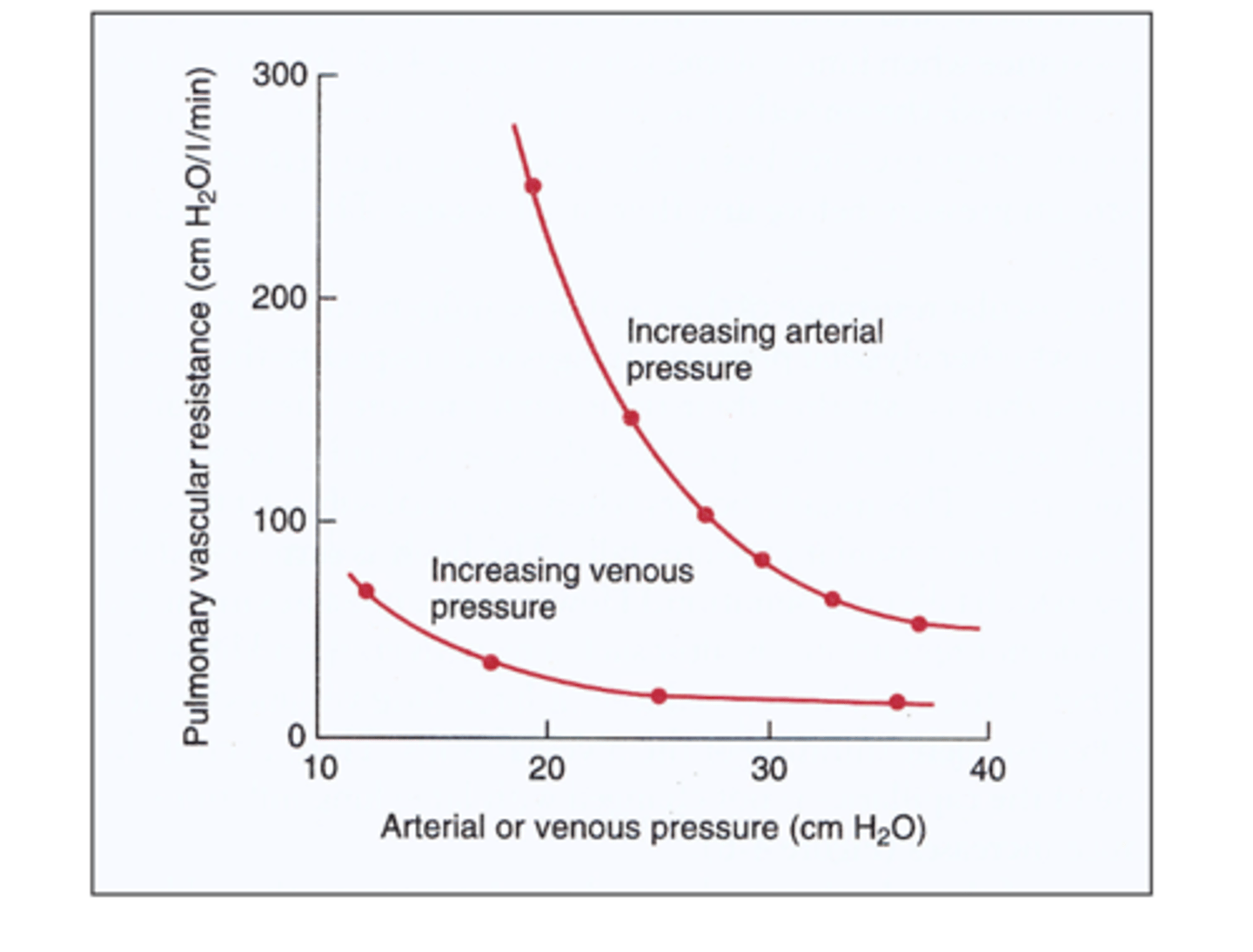
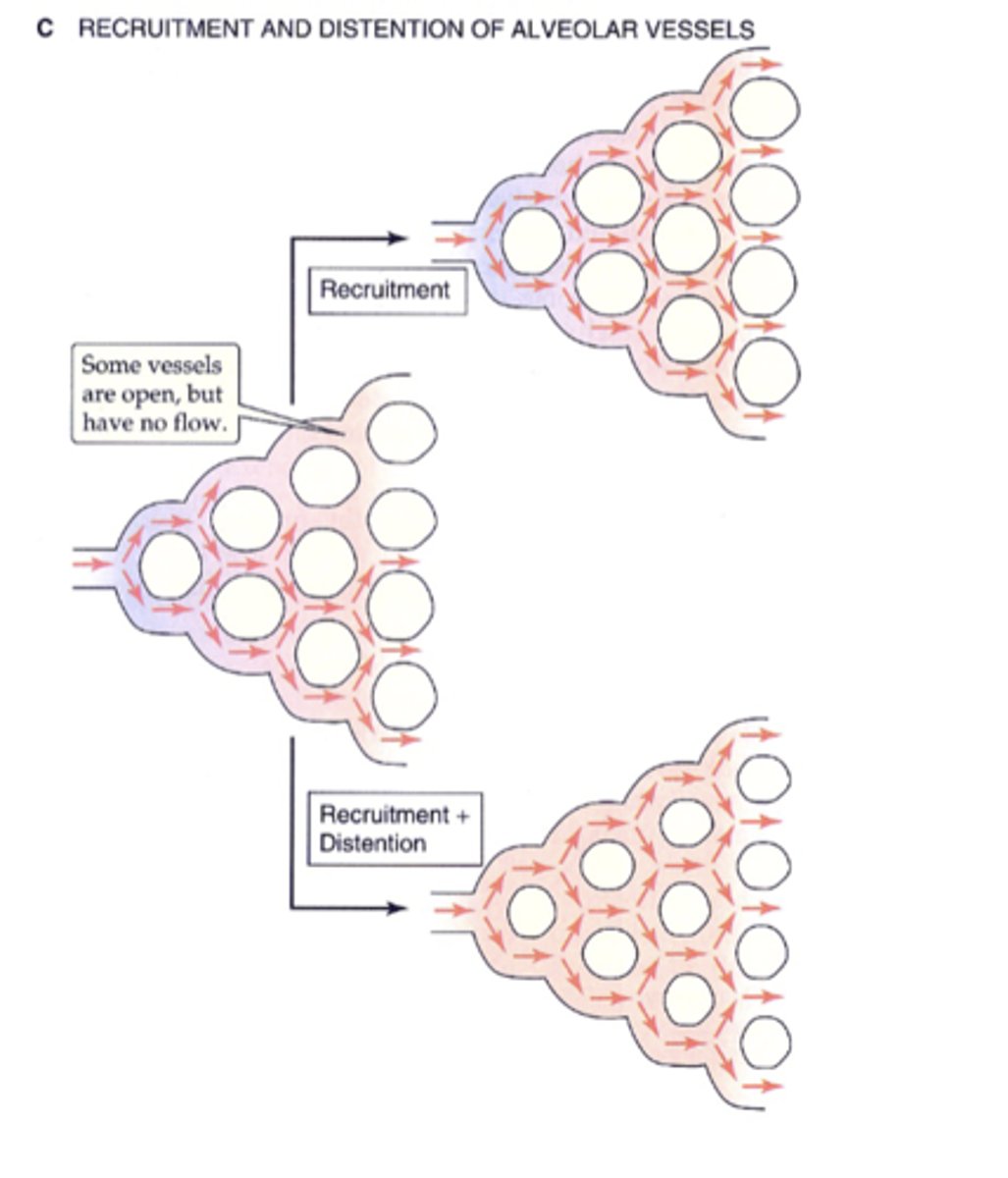
Why does an increase in pulmonary perfusion result in decreased pulmonary vascular resistance?
-recruitment --> previously collapsed pulmonary vessels open up
-distension --> individual capillary segments increase their radii
transmural pressure (PTm)
intravascular pressure of pulmonary vessels - pressure in the alveoli (surrounding)
PTm= PIv - PA
True or False: The intravascular pressure of pulmonary capillaries rises slightly when the heart is in systole.
True ==> & falls slightly when heart is in dystole
True or False: Pulmonary intravascular pressure (PIv) varies with the cardiac cycle
True
True or False: Pulmonary alveolar pressure (PA) varies with the cardiac cycle.
False ==> varies with the respiratory cycle
When is the pulmonary alveolar pressure equal to the transmural pressure?
when there is no air flow
How is pulmonary alveolar pressure (PA) affected by inspiration?
PA decreases
How is pulmonary alveolar pressure (PA) affected by expiration?
PA rises above atmospheric pressure
True or False: The cardiac and respiratory cycles are synchronous
False ==> their effects may sometimes cancel each other out or be additive at other times
In general, at what pulmonary intravascular pressure (PIv) & pulmonary alveolar pressure (PA) dilates the pulmonary vessels and decreases their resistance?
-high PIv
-low PA
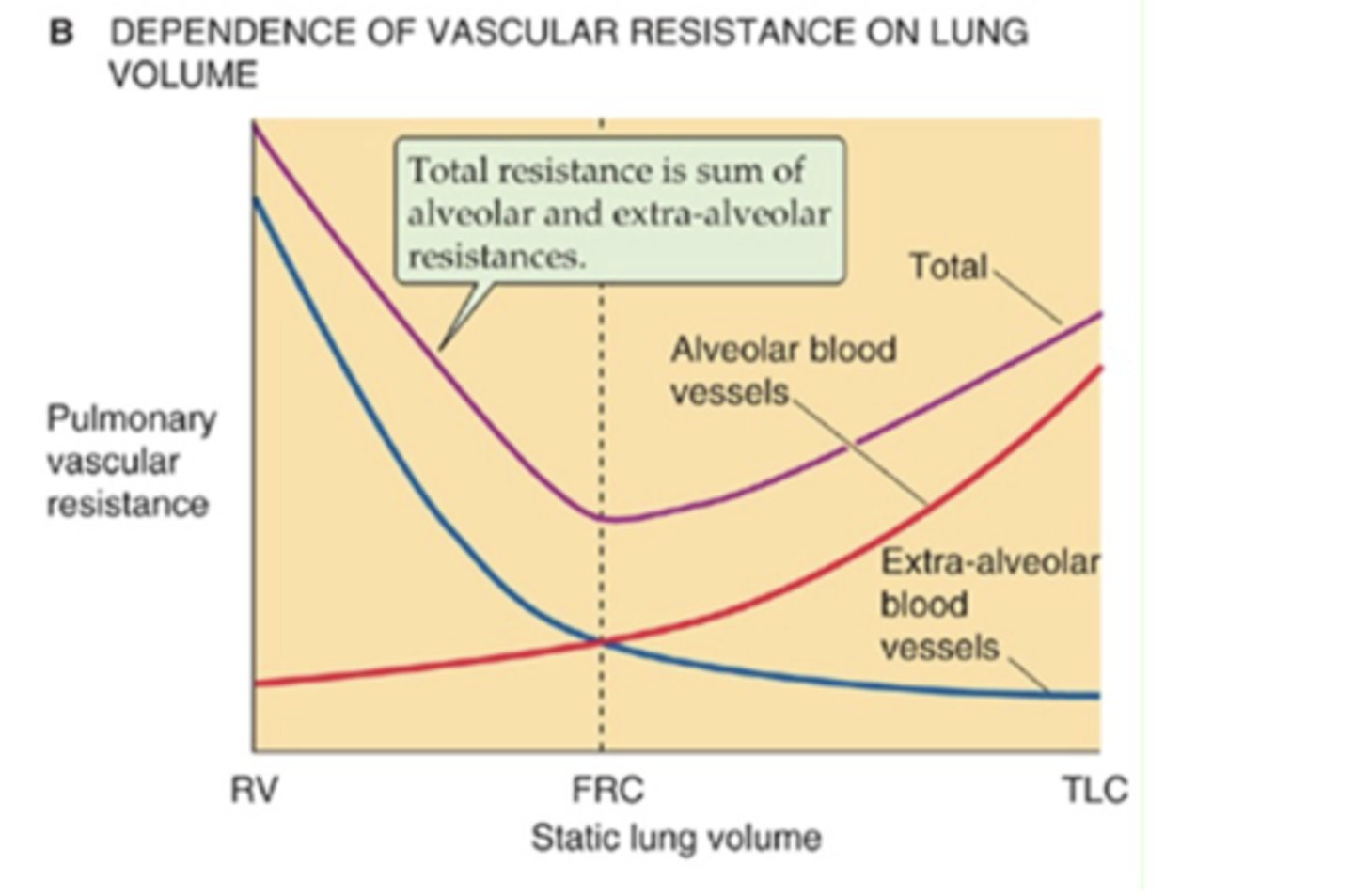
True or False: The effects of lung volume on pulmonary blood flow depend upon whether the pulmonary vessels are alveolar or extra-alveolar.
True
How are the alveolar vessels affected by lung expansion?
when the lungs expand the alveolar vessels are compressed = increased resistance
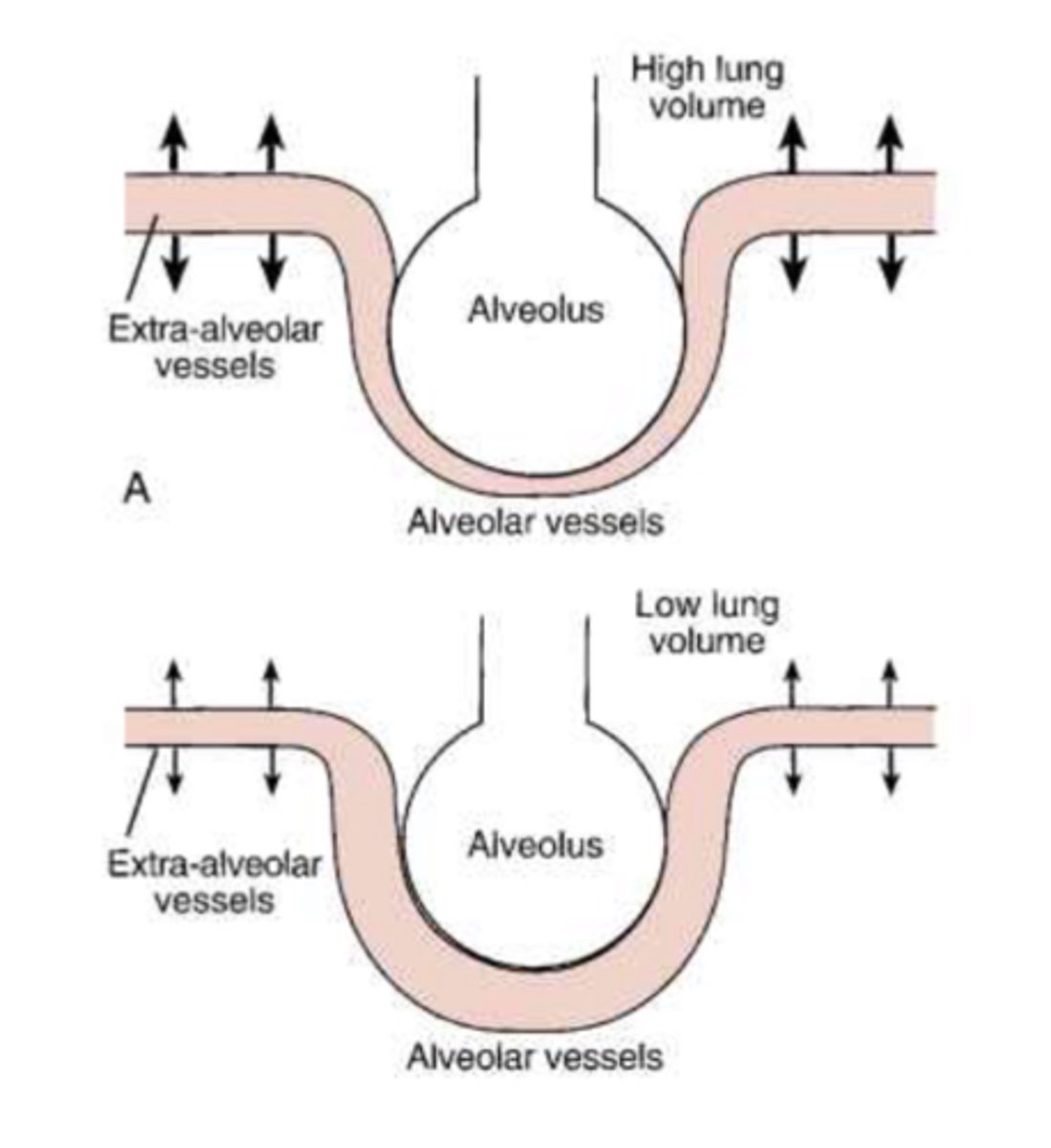
How are the extra-alveolar vessels affected by lung expansion?
when the lungs expand, the extra-alveolar vessels get pulled open by the expansion of the attached parenchymal tissue
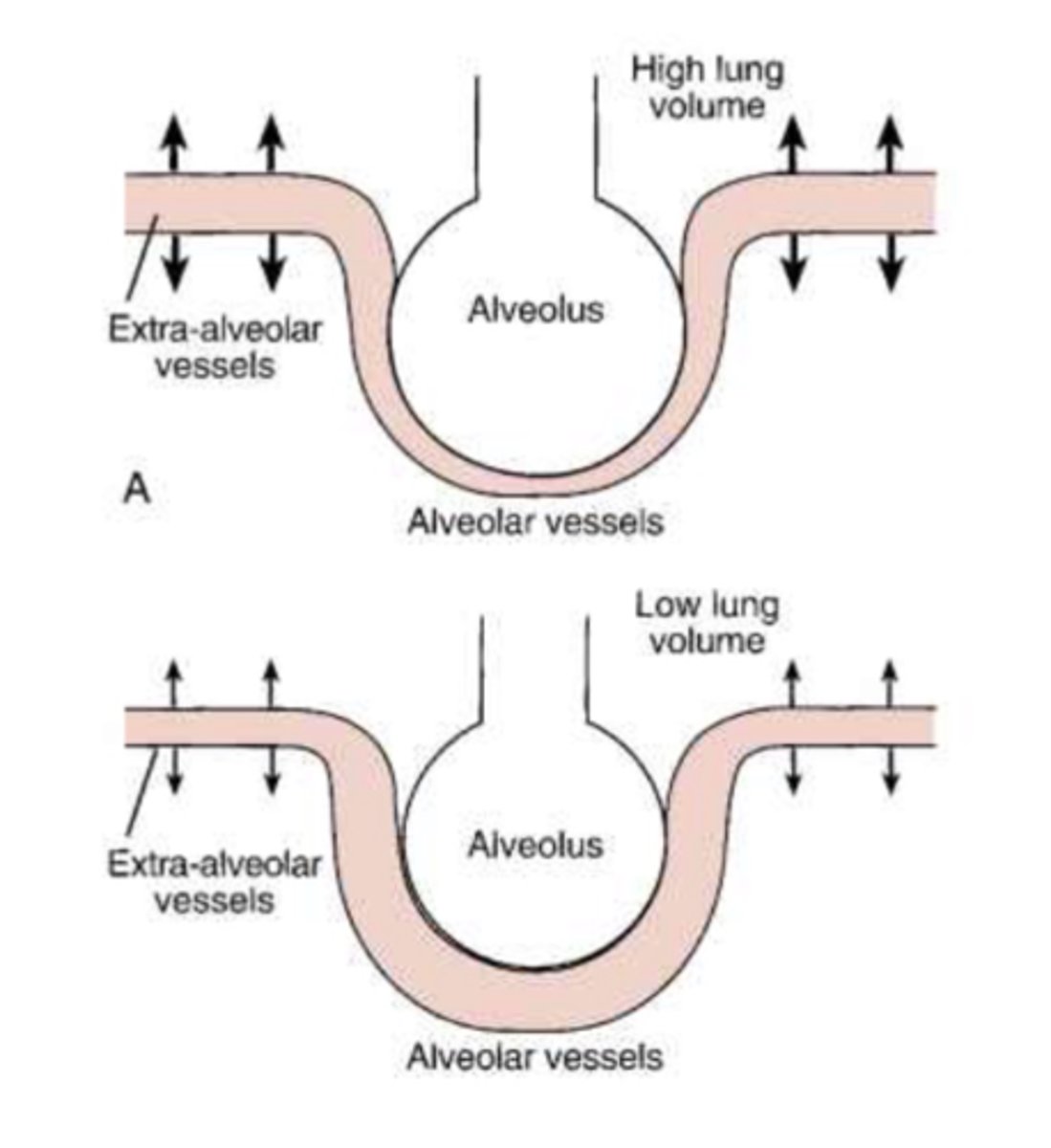
At low lung volumes, what is the overall resistance to pulmonary blood flow?
overall resistance is high to blood flow @ low lung volumes b/c extra-alveolar vessels are compressed
During inspiration, what is the overall resistance to pulmonary blood flow?
decreased resistance ==> b/c extra-alveolar vessels are pulled open

At higher lung volumes, what is the overall resistance to pulmonary blood flow?
increased resistance ==> b/c alveoli expansion is compressing the alveolar capillaries
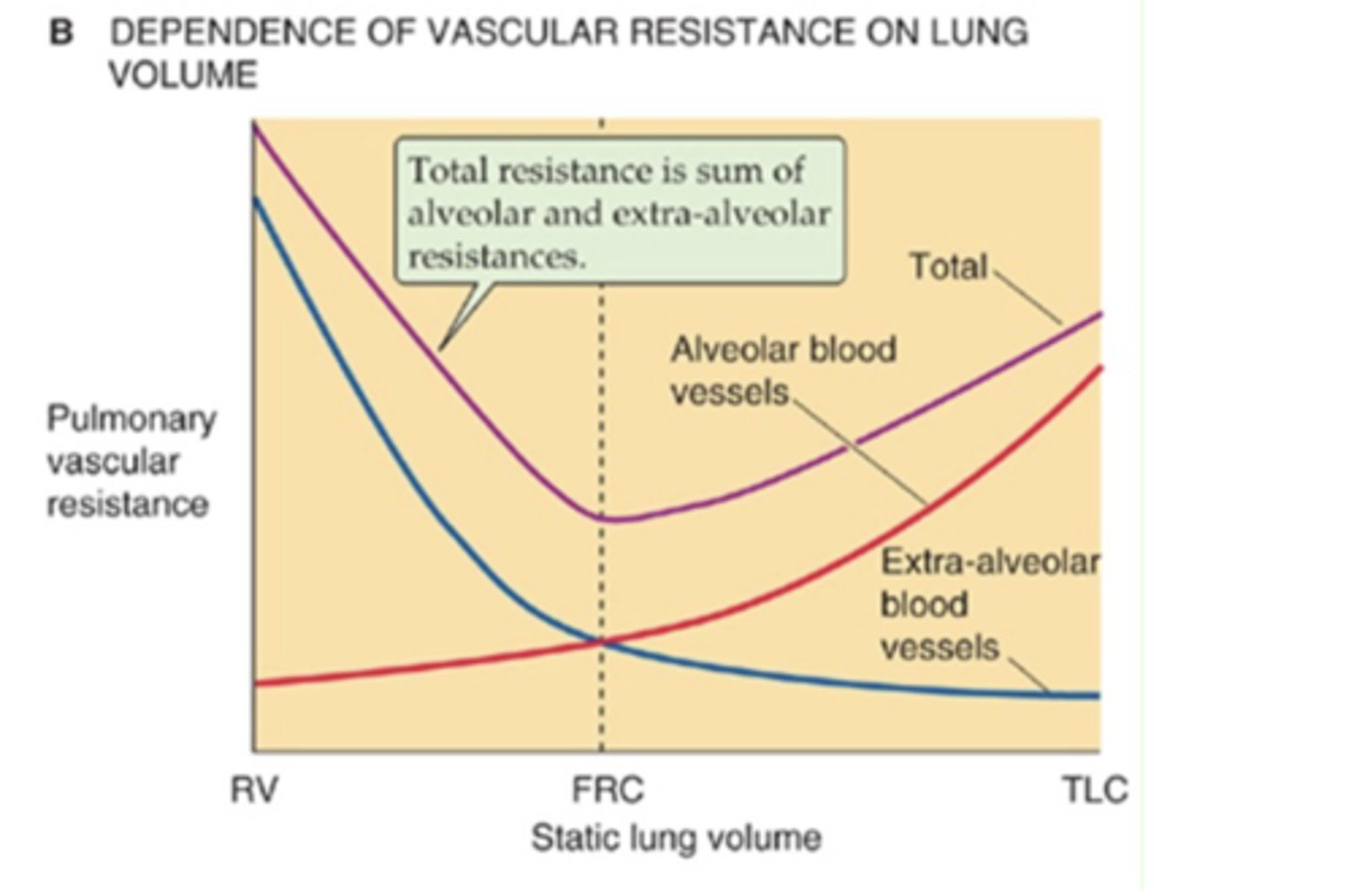
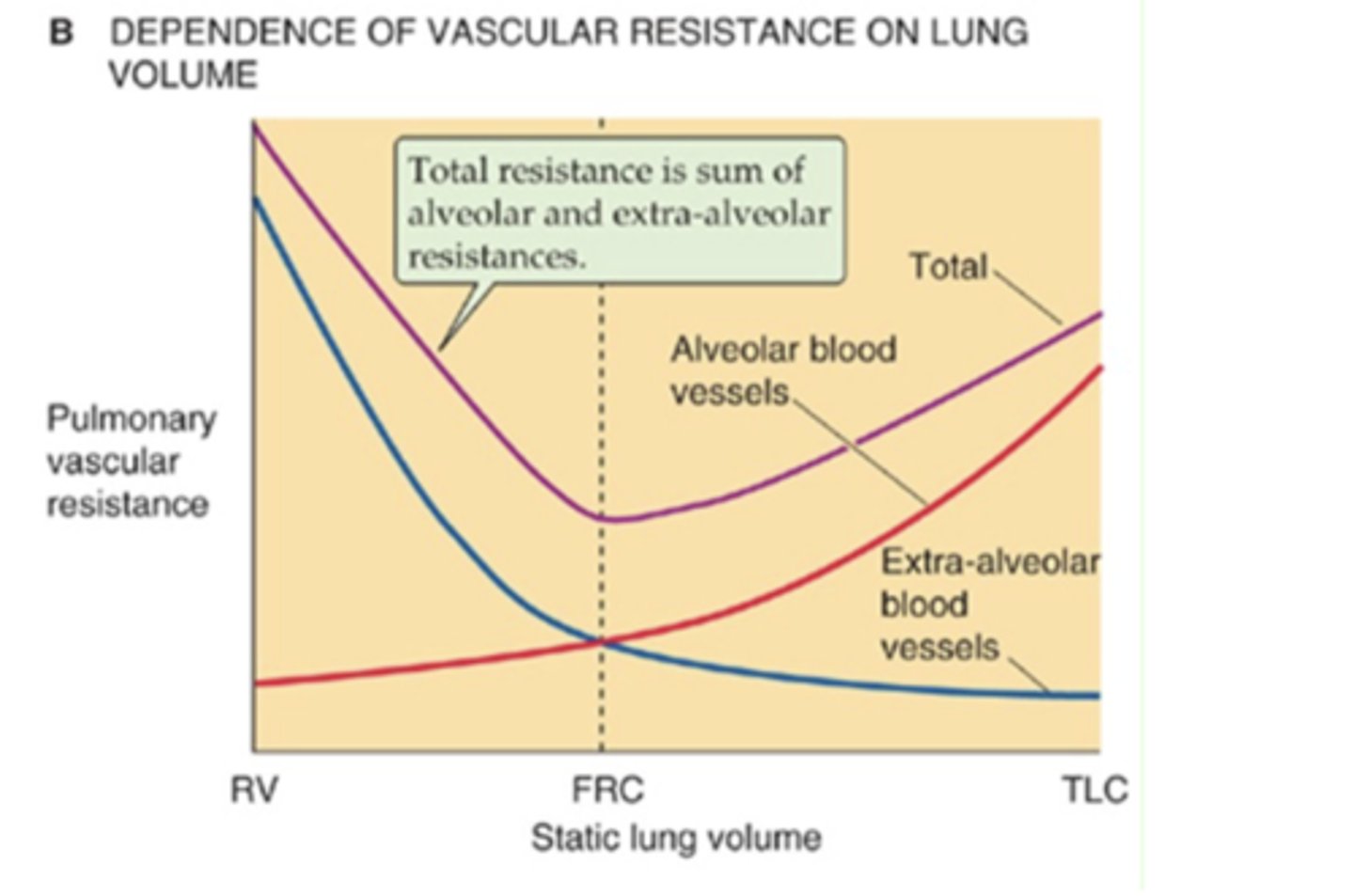
What determines the total pulmonary vascular resistance?
sum of alveolar & extra-alveolar resistances
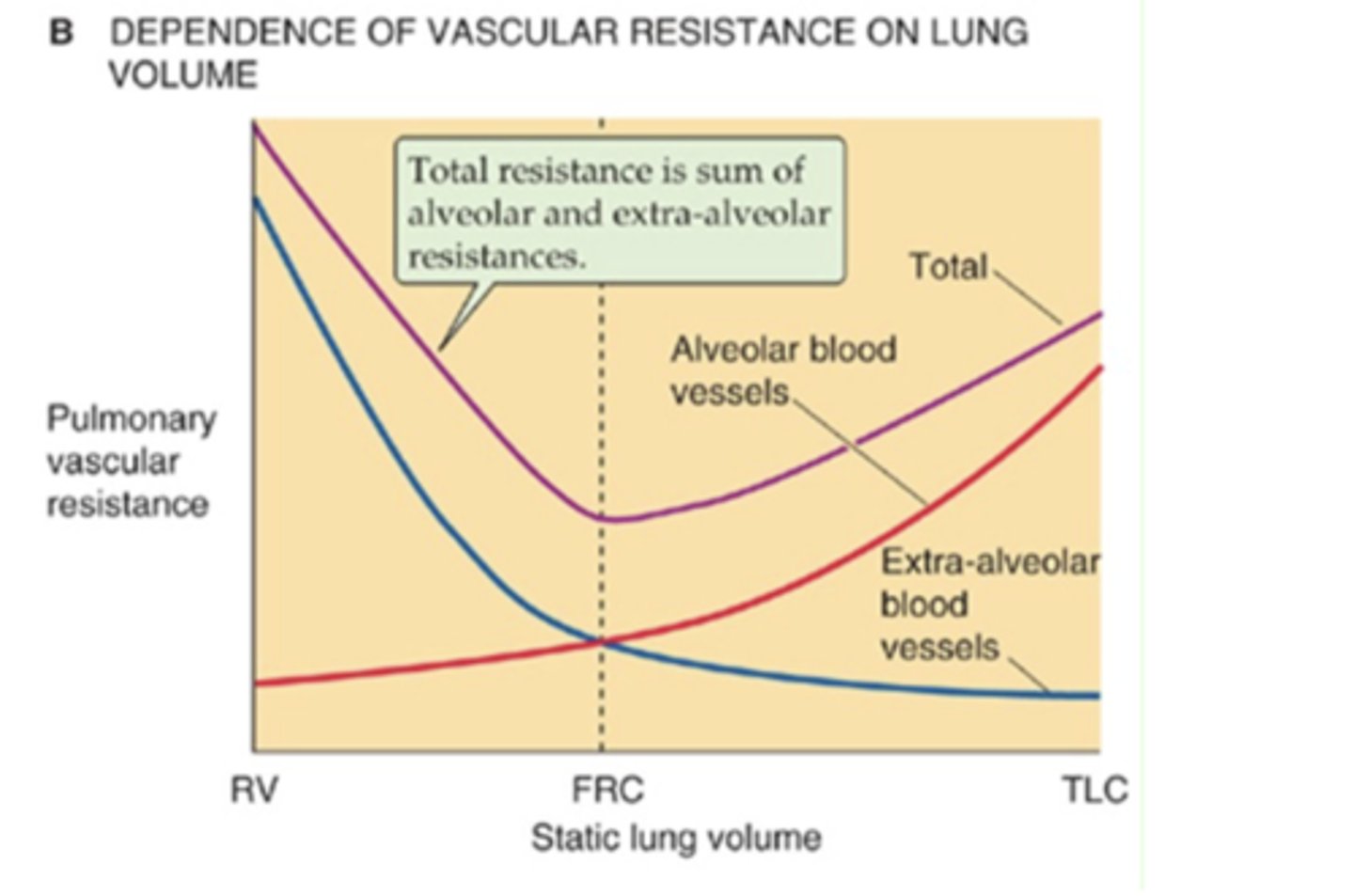
Describe the net changes in pulmonary resistance to blood flow
-low lung volumes ==> high total resistance due to compressed extra-alveolar vessels
-inspiration ==> decreased total resistance b/c extra-alveolar vessels are pulled open
-higher lung volumes ==> increased total resistance b/c alveolar vessels are compressed by alveoli
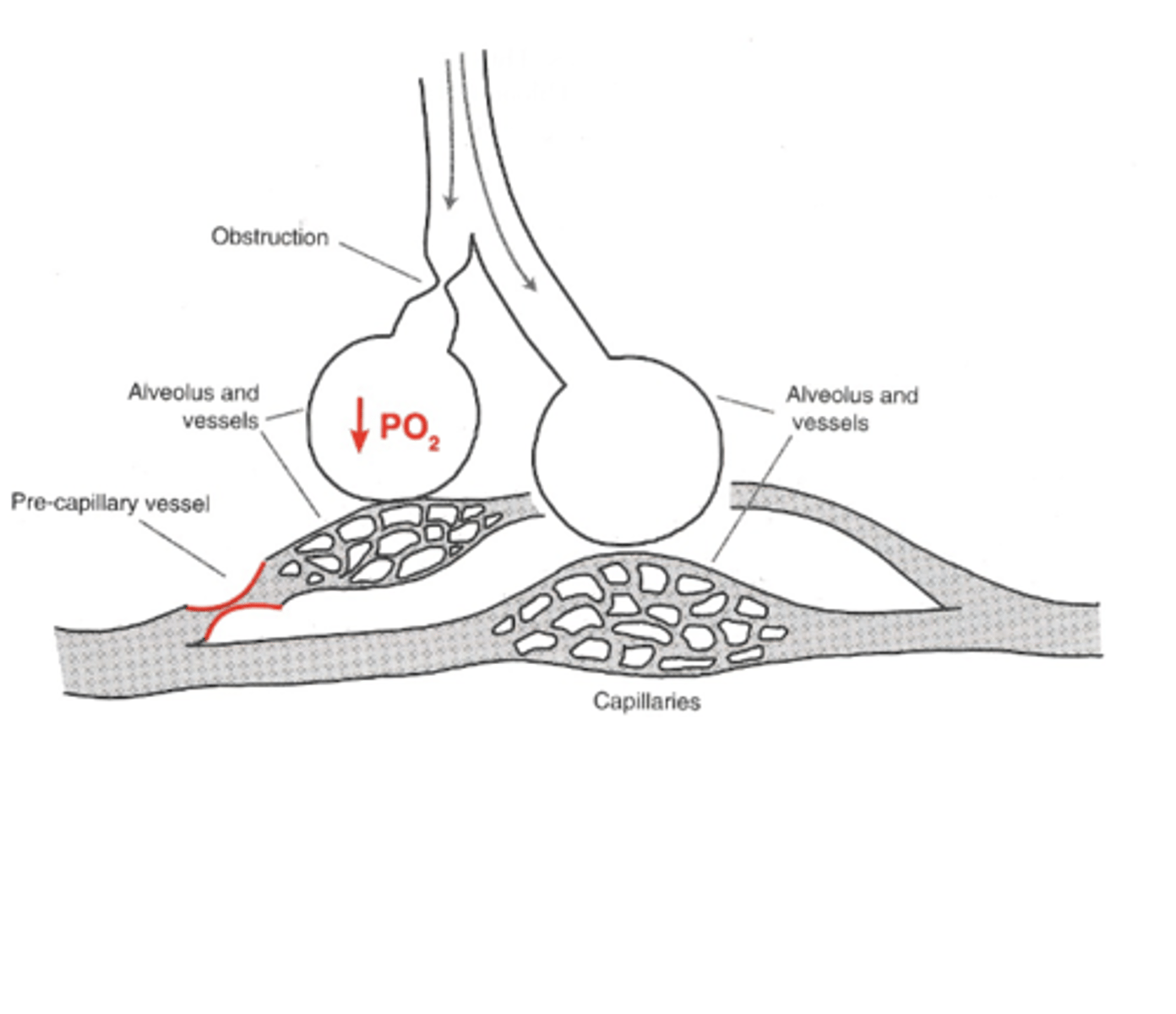
True or False: Pulmonary blood vessels dilate in response to local hypoxia
False==> pulmonary vessels contract when their surrounding alveoli are hypoxic (vasoconstriction in response to local hypoxia)
*the other pulmonary vessels dilate to compensate
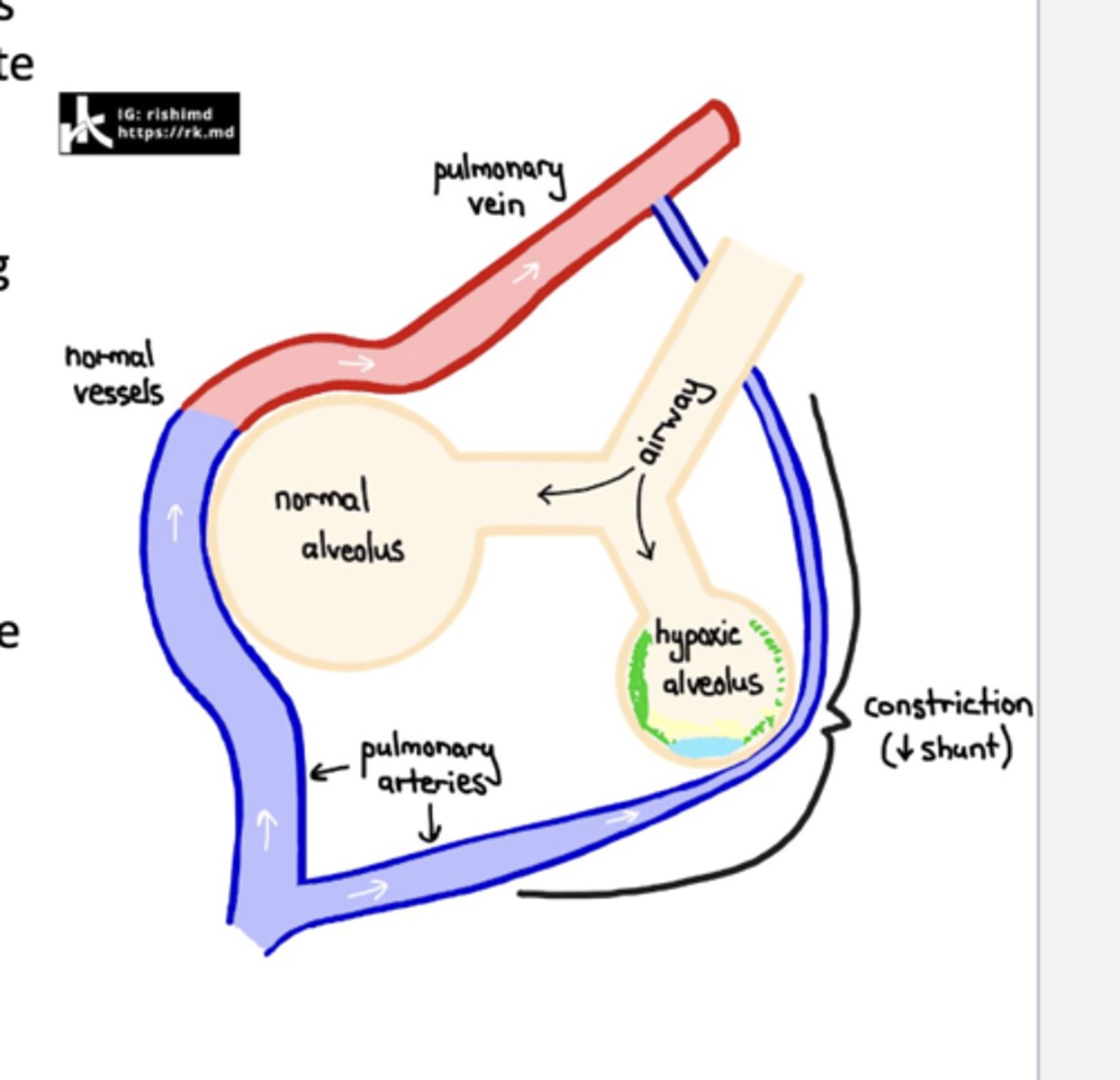
How do you know that hypoxic vasoconstriction of the pulmonary vessels doesn't involve nervous or hormonal signaling?
b/c it acts on isolated excised pieces of lung tissue
How does hypoxic vasoconstriction of pulmonary vessels likely take place?
local action on vascular smooth muscle==> possibly by inhibition of voltage-gated K+ channel --> influx of Ca2+ --> smooth muscle contraction
How do the lungs respond to hypoxic alveoli?
hypoxic vasoconstriction of vessels near poorly ventilated alveoli & dilation of the other vessels --> flow diverted away from poorly ventilated alveoli to alveoli that are well ventilated
*ensures maximum exchange of O2 bwtn alveoli & blood
How does gravity affect pulmonary blood flow?
the higher the pulmonary blood vessel, the lower the intravascular pressure ==> gravity resists the blood of flow upwards (harder to keep a lot of blood flow up b/c gravity is pushing it back down)
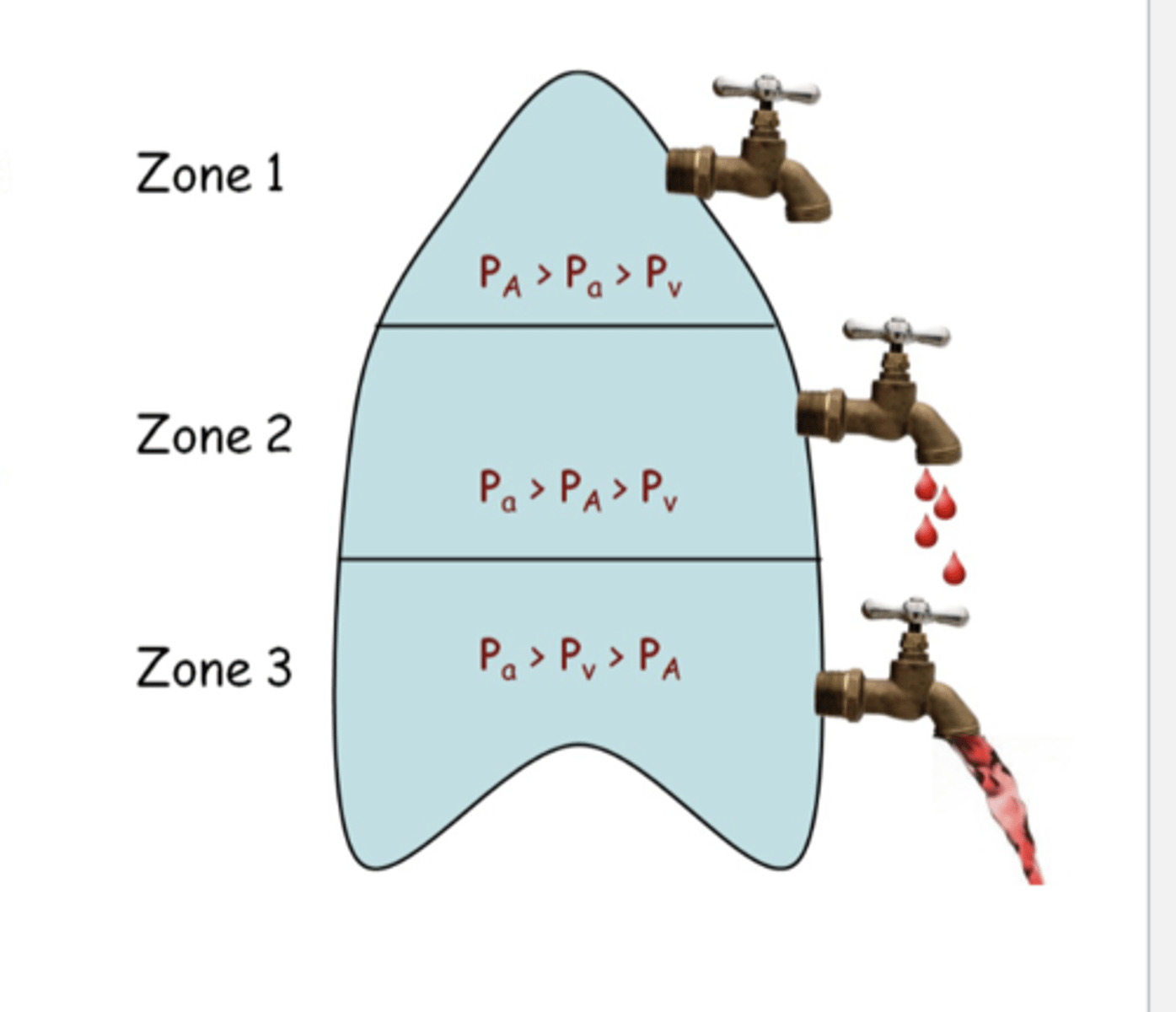
In the upper portion of the lung (Zone 1), how does the alveolar pressure (PA), arterial pressure (Pa) , & venous pressure (Pv) compare to one another?
PA > Pa > Pv
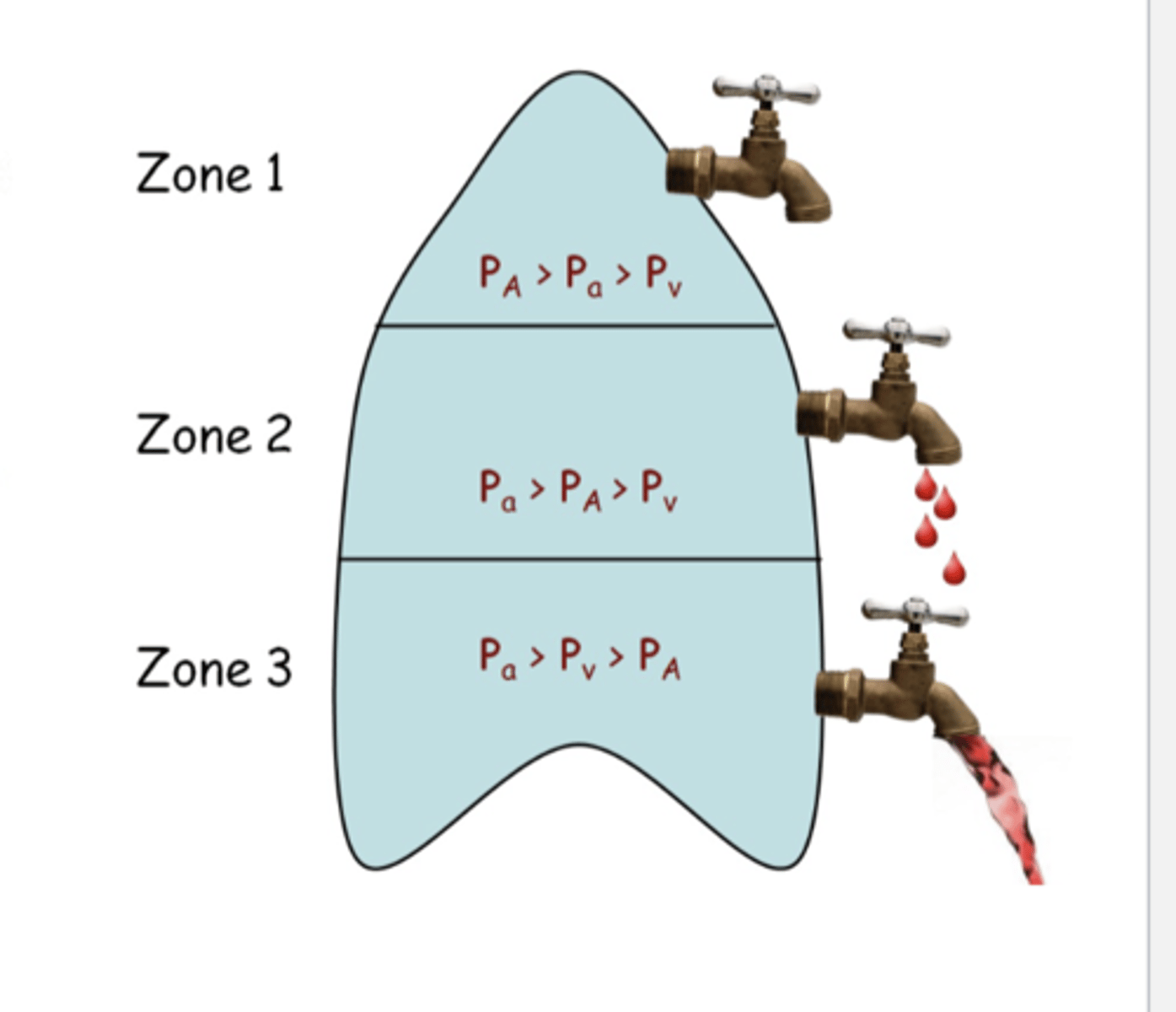
In the middle portion of the lung (Zone 2), how does the alveolar pressure (PA), arterial pressure (Pa) , & venous pressure (Pv) compare to one another?
Pa > PA > Pv
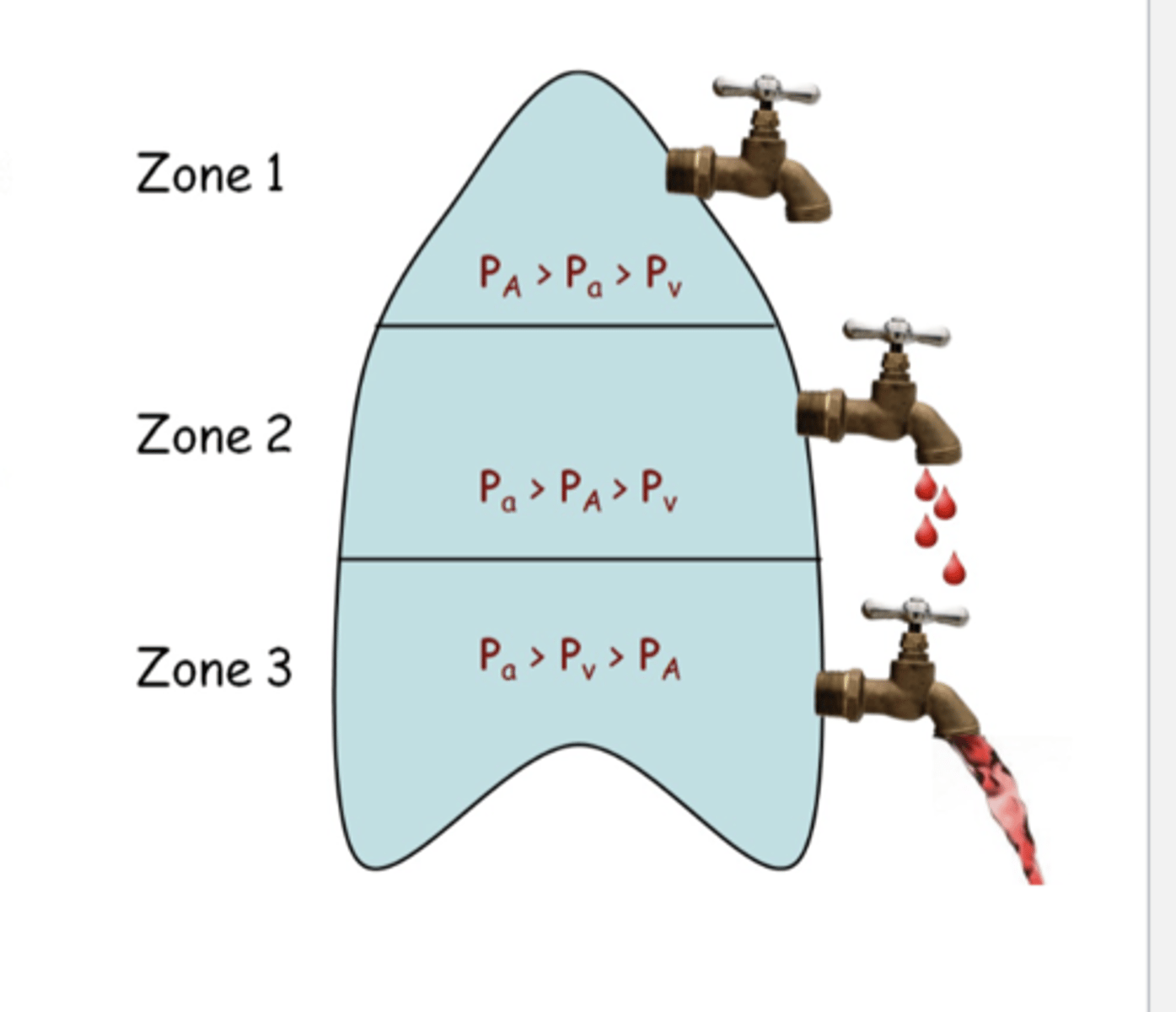
In the lower portion of the lung (Zone 3), how does the alveolar pressure (PA), arterial pressure (Pa) , & venous pressure (Pv) compare to one another?
Pa > Pv > PA
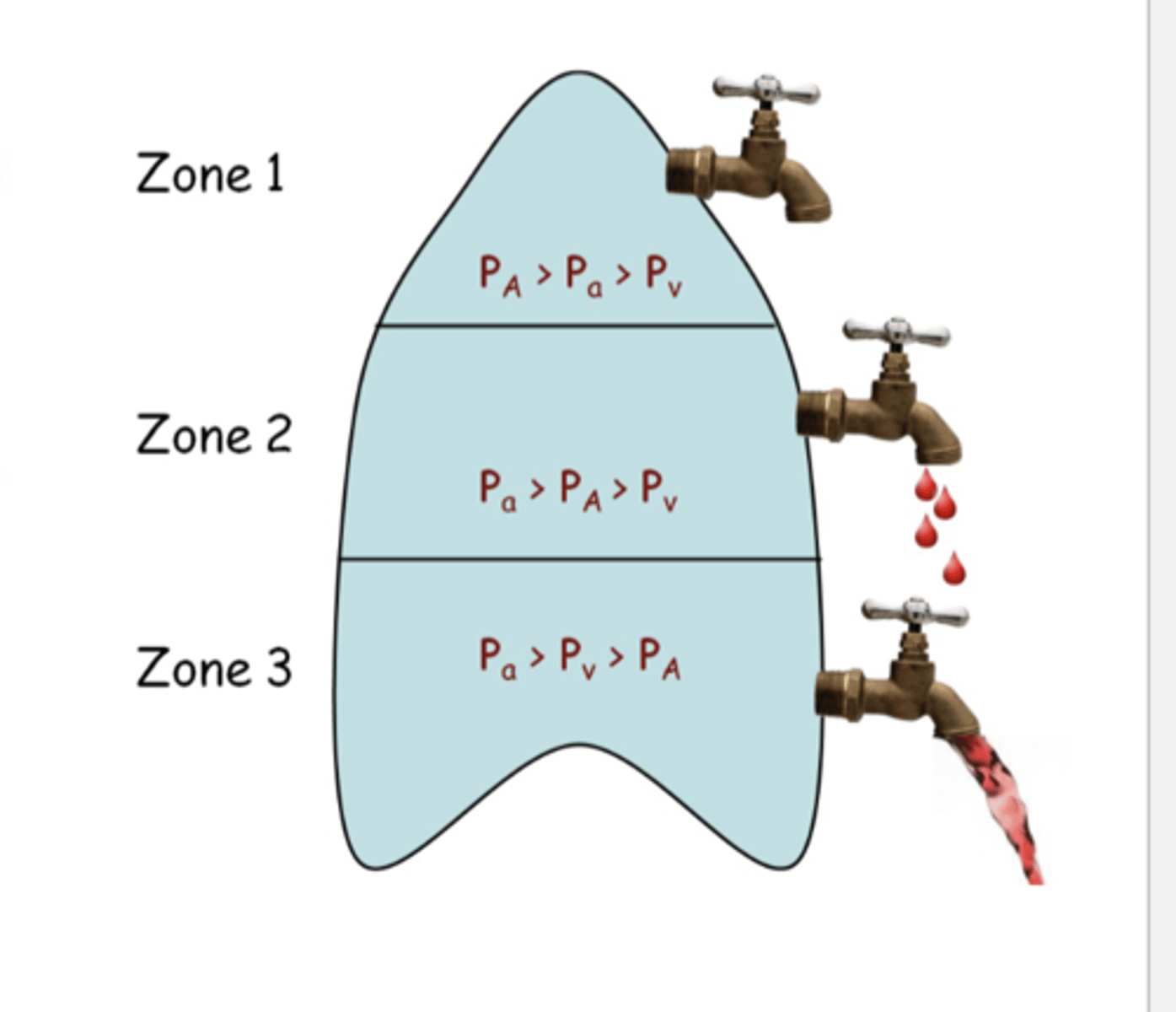
For each cm in height above the left atrium, the hydrostatic pressure of pulmonary arterioles and venules falls by _________________.
approx 0.68 mmHg (1 cm H2O)
For each cm in height below the left atrium, the hydrostatic pressure of pulmonary arterioles and venules rises by ___________.
approx 0.68mmHg (1 cm H2O)
Several hundred mL of fluid leave the pulmonary capillaries and enter the interstitium every day. How is the fluid removed?
-vaporization in the alveoli
-reabsorption into venules
-uptake by the lung lymphatics
When do patients have pulmonary hypertension?
-mean pulmonary pressure exceeds 25mmHg at rest
-mean pulmonary pressure exceeds 35 mmHg during exercise
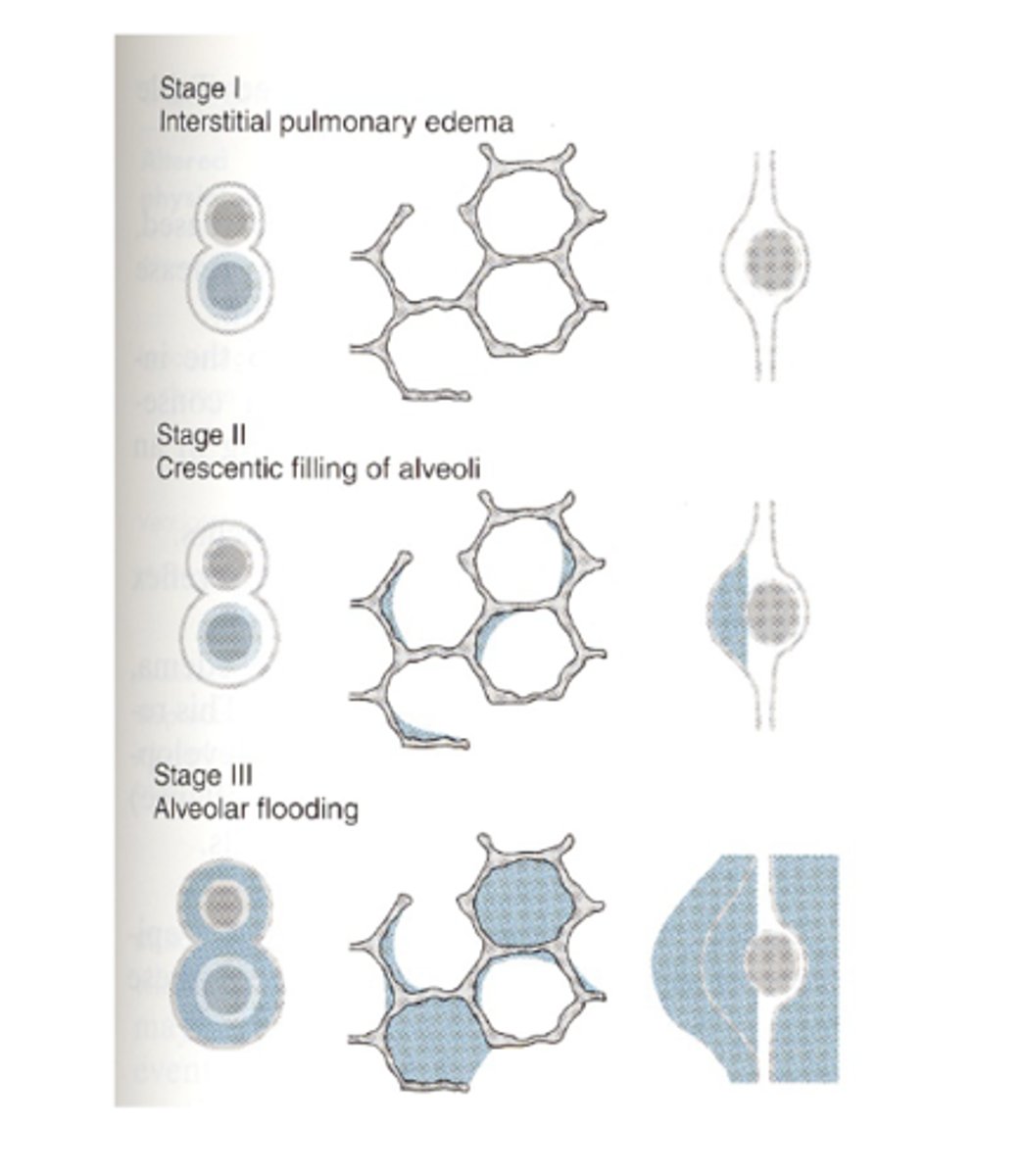
what is pulmonary edema?
excessive fluid in the interstitial tissue or alveoli
When does pulmonary edema occur?
when pulmonary capillary pressure is <25 mmHg ==> excessive fluid accumulates in the interstitial tissue or alveoli --> fluid flux out of the capillary exceeds the capacity of the lymphatics to drain the interstitium
Describe how pulmonary edema progresses?
flooding of peri-capillary interstitial spaces --> crescentic filling of alveoli --> flooding of individual alveoli with loss of gas exchange
What is ventilation?
transport of gas from the atmosphere to the alveolar surface
What are the components of the atmosphere?
mixture of gases, such as:
-nitrogen (mainly)
-oxygen
-water vapor
-carbon dioxide
Dalton's Law of Partial Pressures
the total pressure exerted by a mixture of gasses is the sum of the partial pressures exerted independently by each gas in the mixture
Ptotal = P1 + P2 + P3 . . .
*the pressure each gas contributes is in proportion to its relative amount
ex: If P1 is 25% of total gas, then P1 = P total(0.25)
How much nitrogen is in dry atmospheric air?
79% ==> PN2 = 597 mmHg
How much oxygen is in dry atmospheric air?
21% ==> PO2 = 159 mmHg
How is the partial pressures of gases in tracheal air calculated?
air is humidified when breathed in, so you have to take H2O into account (PH2O = 47 mmHg)
ex: PO2 (tracheal) = (Ptotal - PH2O) x 0.21
What is the partial pressure of H2O of the air in the lungs?
47 mmHg
True or False: Gases in the air are diluted when inhaled
True ==> air humidified when breathed in (PH2O = 47 mmHg)
How is air modified when it is in inhaled?
-humidified (PH2O = 47 mmHg)
-O2 diffuses from air into the blood
-CO2 diffuses from the blood into the alveoli
minute ventilation (mL/min)
respiratory rate (breaths/min) x tidal volume (mL/breath)
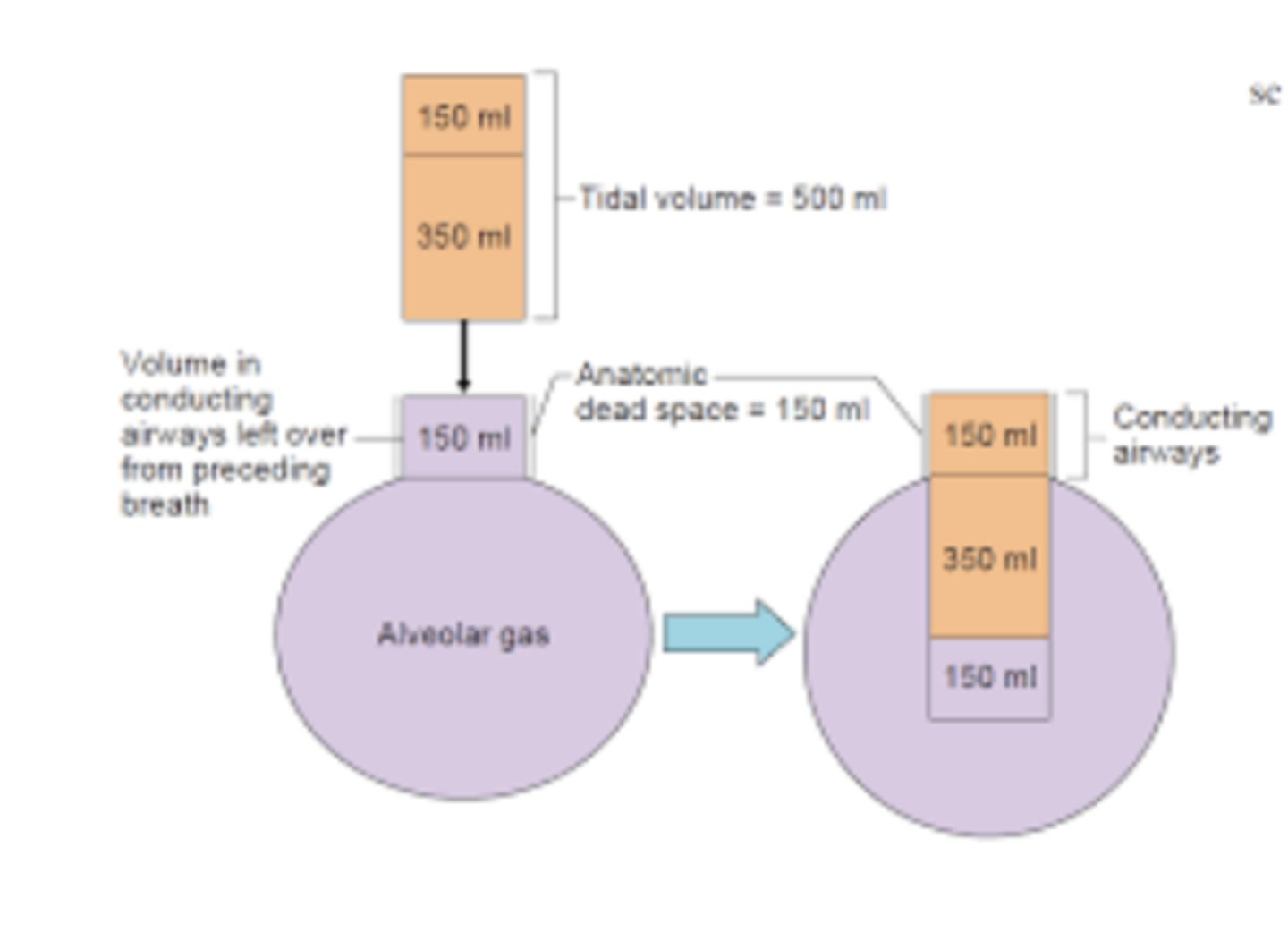
anatomic dead space
fact check this one*
the space where approx 150mL of inspired air doesn't reach alveoli for gas exchange (remains in the conducting airways)
*150mL remains in conducting airways --> pushed down into alveoli during next inspiration --> 150mL of new air remains in conducting airways
alveolar dead space (physiological dead space)
alveolar dead space results from alveoli that are ventilated but not perfused ==> gas entering doesn't exchange w/blood
*normally very small (barely there?), but significant in some pathologies (ex: pulmonary embolism)
What allows the there to be ample time for gas exchange between the pulmonary capillaries & the alveoli?
capillary transit time for RBCs is about 0.75 seconds, but equilibration of O2 & CO2 (1:1 even exchange) occurs in about 0.3 seconds
*plenty of time for gas exchange, even when exercise increases transit time
Describe the effect high altitude has on pulmonary blood flow.
high altitude = lower PO2 = decreased alveolar capillary partial pressure gradient ==> might not be enough driving force to fully load the blood within the transit time
Fowler's Single Breath N2 Washout
alveolar ventilation
flow of air into alveoli taking part in gas exchange
*tidal volume minus the anatomic dead space volume of fresh air reaches the alveoli per resting breath
= resp rate x (tidal vol. - anatomic dead space vol)
What does it mean if the partial pressure of CO2 is increased in pulmonary vessels?
not removing as much CO2 from blood as being produced ==> imbalance bwtn CO2 production & removal by ventilation
True or False: The partial pressure of CO2 in pulmonary vessels reflects the balance between CO2 production and removal by ventilation
True
PaCO2 = VCO2/ VA
-VCO2 = rate of metabolic CO2 production
-VA = alveolar ventilation
When ventilation fails, how is the partial pressure of CO2 in pulmonary arteries affected?
PaCO2 will rise rapidly
(*but this makes VA rise to decrease PaCO2)
What are the factors that affect airflow? (3)
-airway resistance--> Poiseuille's Equation applies
-turbulence at branch points in the airways
-bronchial smooth muscle tone--> controlled by SNS, PNS, chemical irritants, allergens, etc.
How does parasympathetic stimulation influence bronchial smooth muscle tone?
bronchoconstriction via parasympathetic cholinergic
How does sympathetic stimulation influence bronchial smooth muscle tone?
bronchodilation via sympathetic adrenergic stimulation
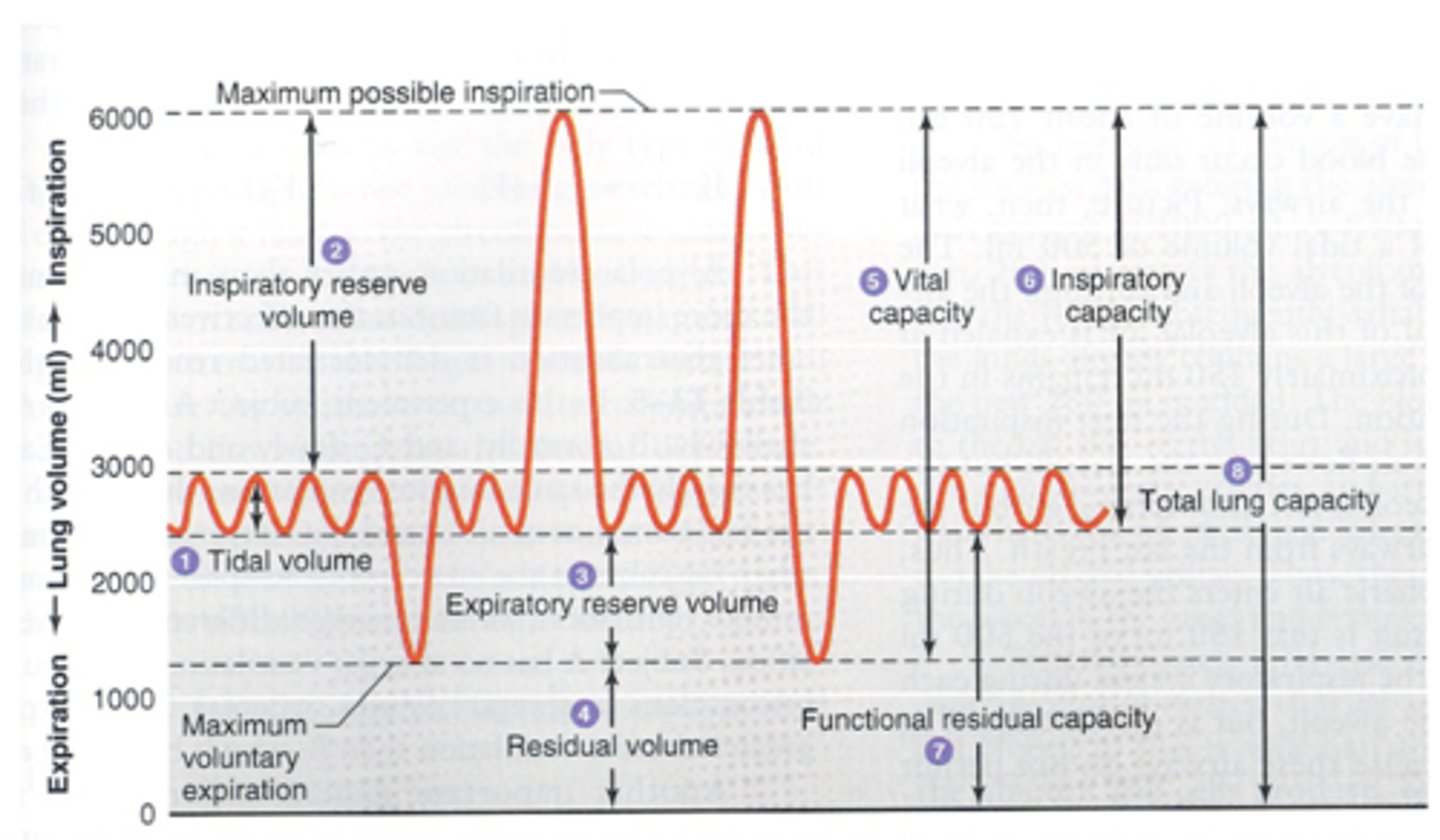
functional residual capacity (FRC)
the volume of air remaining in the lungs at the end of a normal exhalation
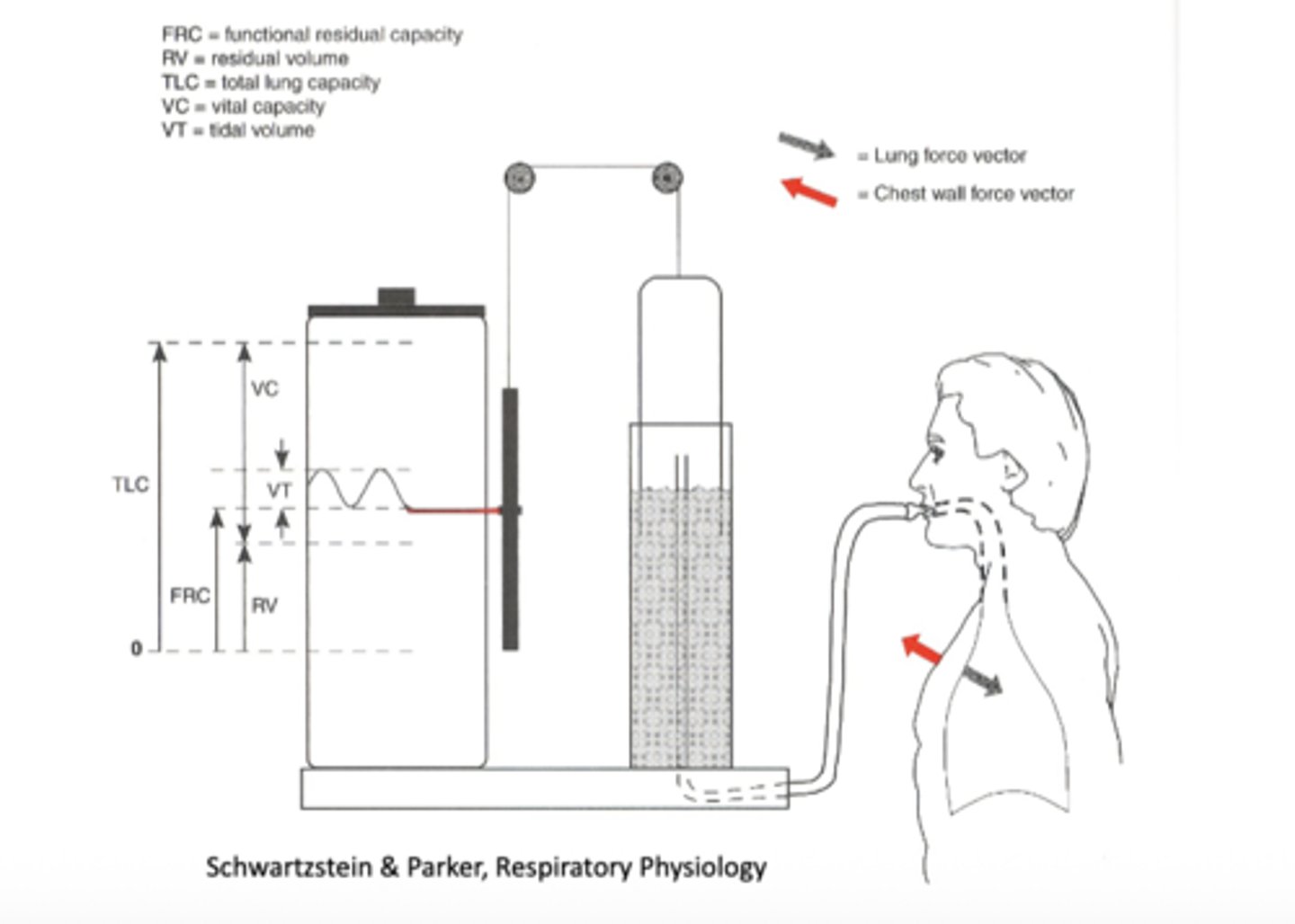
residual volume (RV)
the amount of air that remains in the lungs after a maximal exhalation
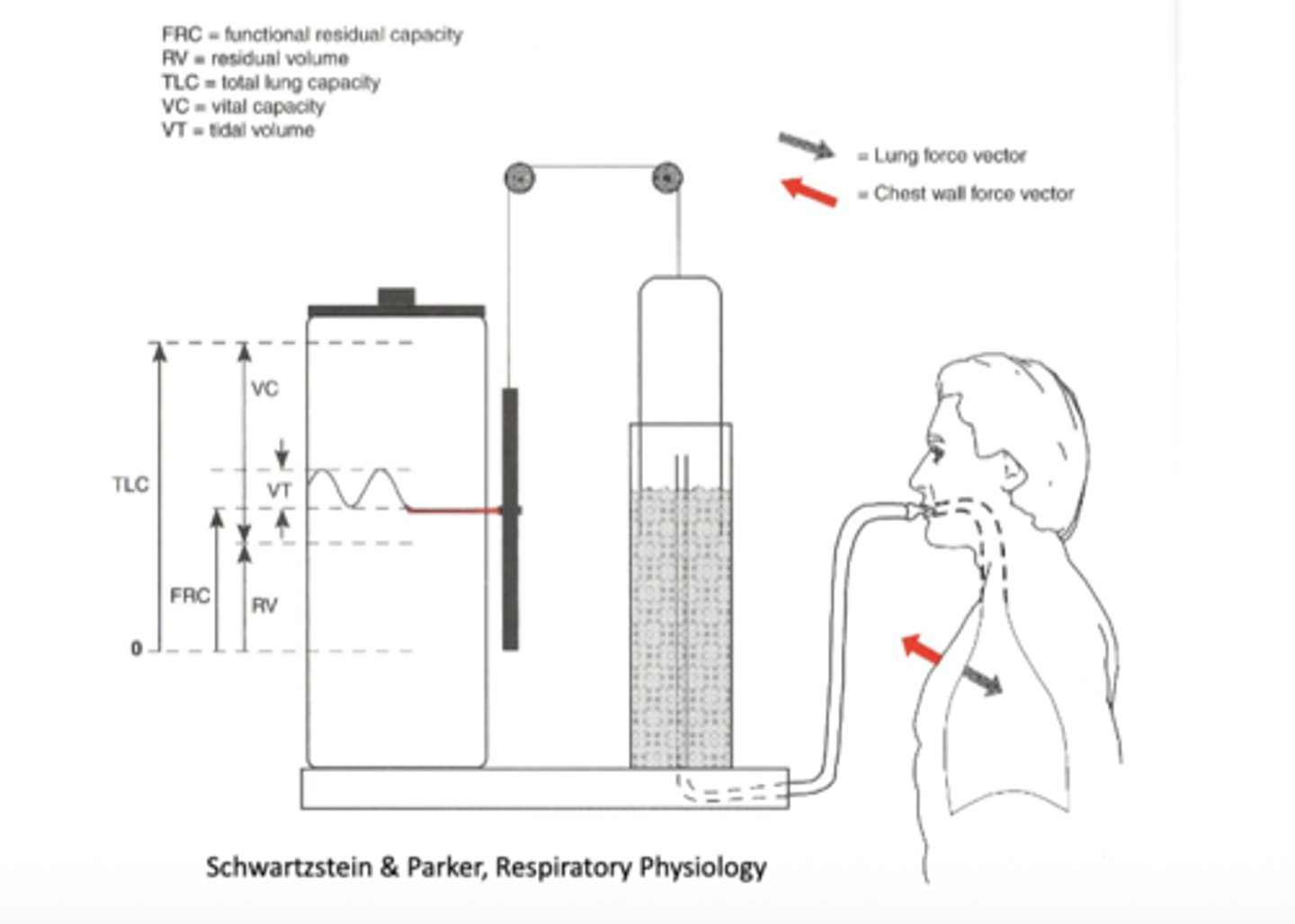
total lung capacity (TLC)
the maximum amount of air the lungs can hold when maximally inflated
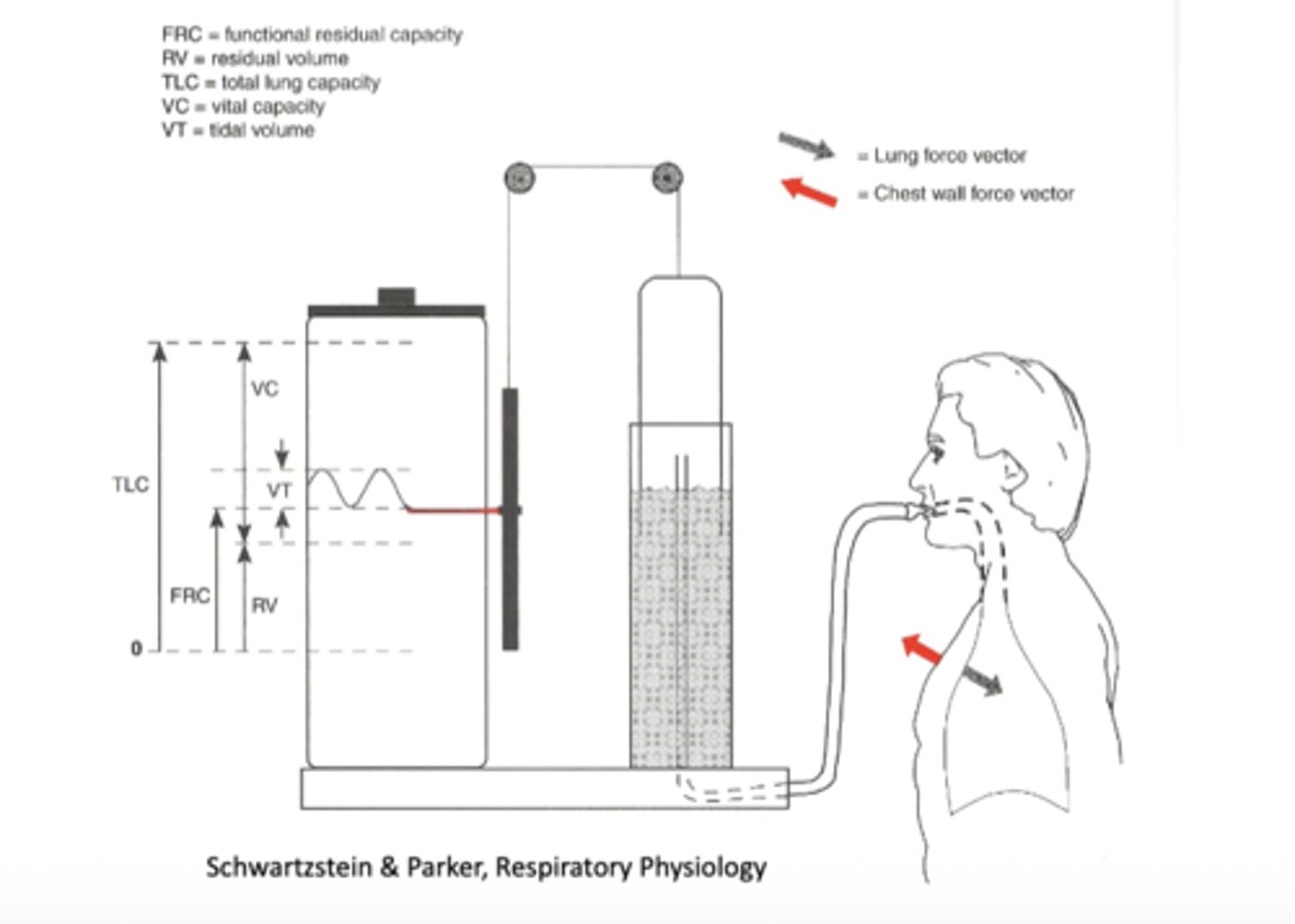
vital capacity (VC)
the greatest volume of air that can be expelled from the lungs after taking the deepest possible breath.
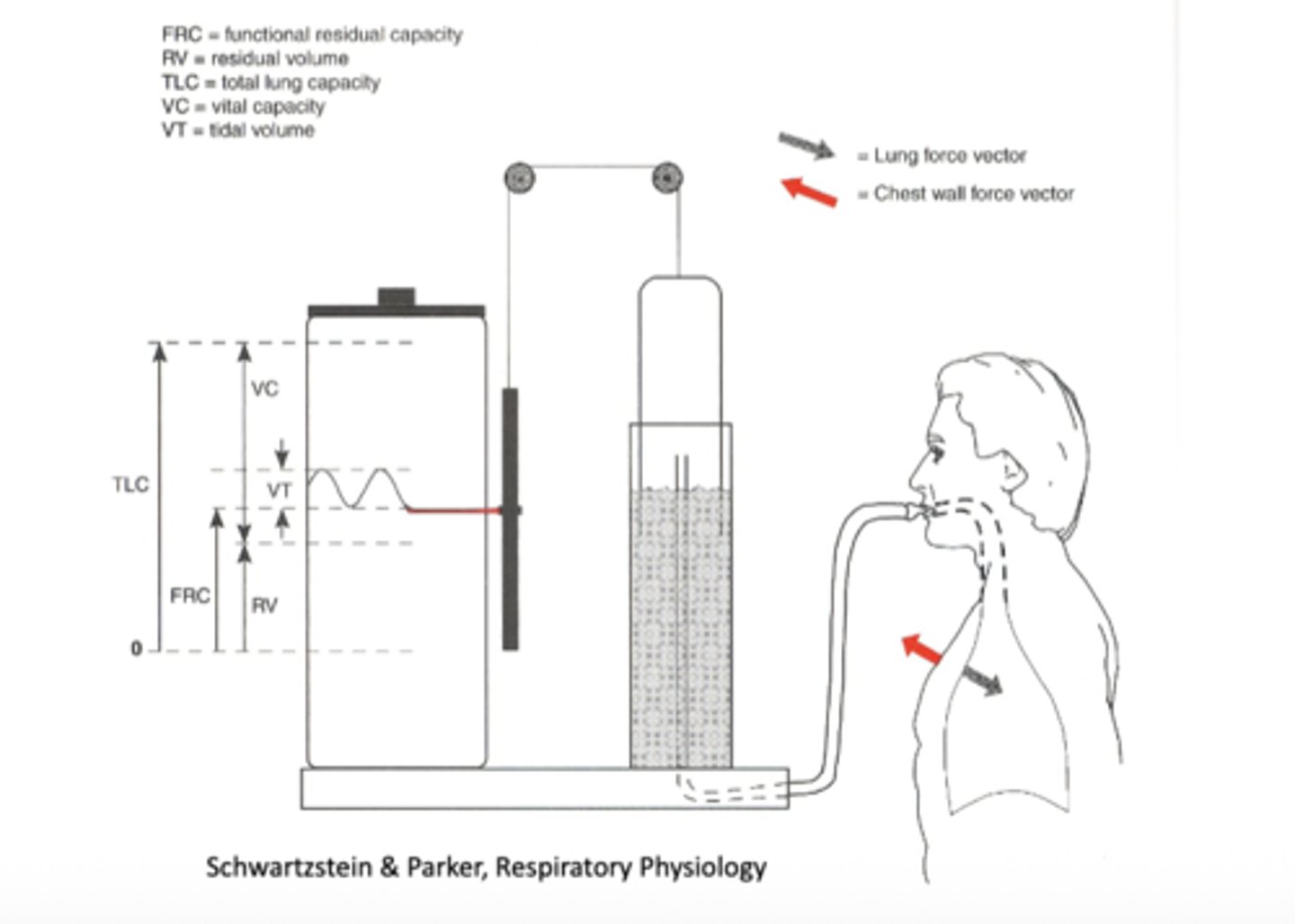
tidal volume (VT)
the amount of air inhaled and exhaled during a normal, unforced breath
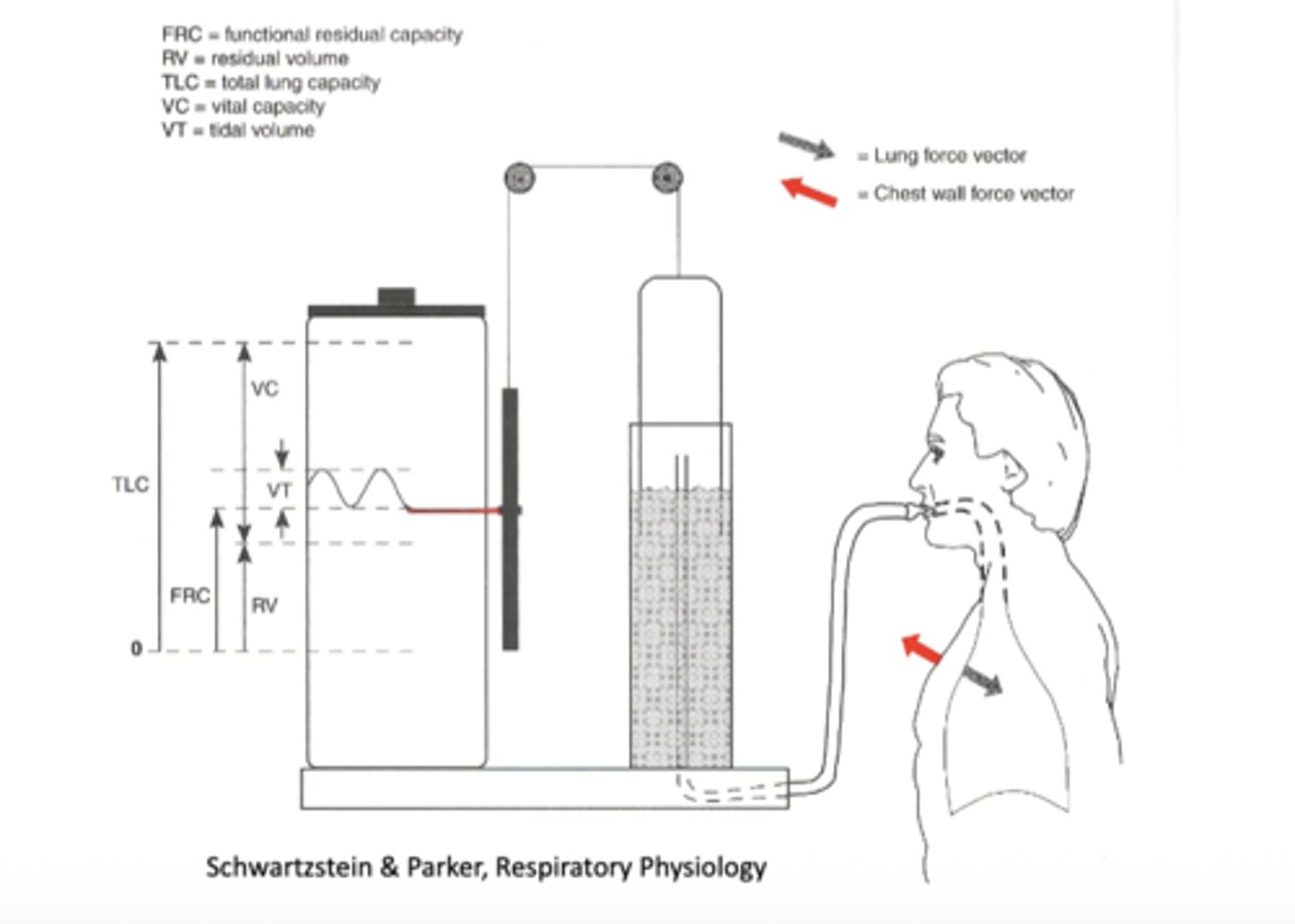
Inspiratory Reserve Volume (IRV)
the maximum amount of air that can be inhaled after a normal, quiet breath
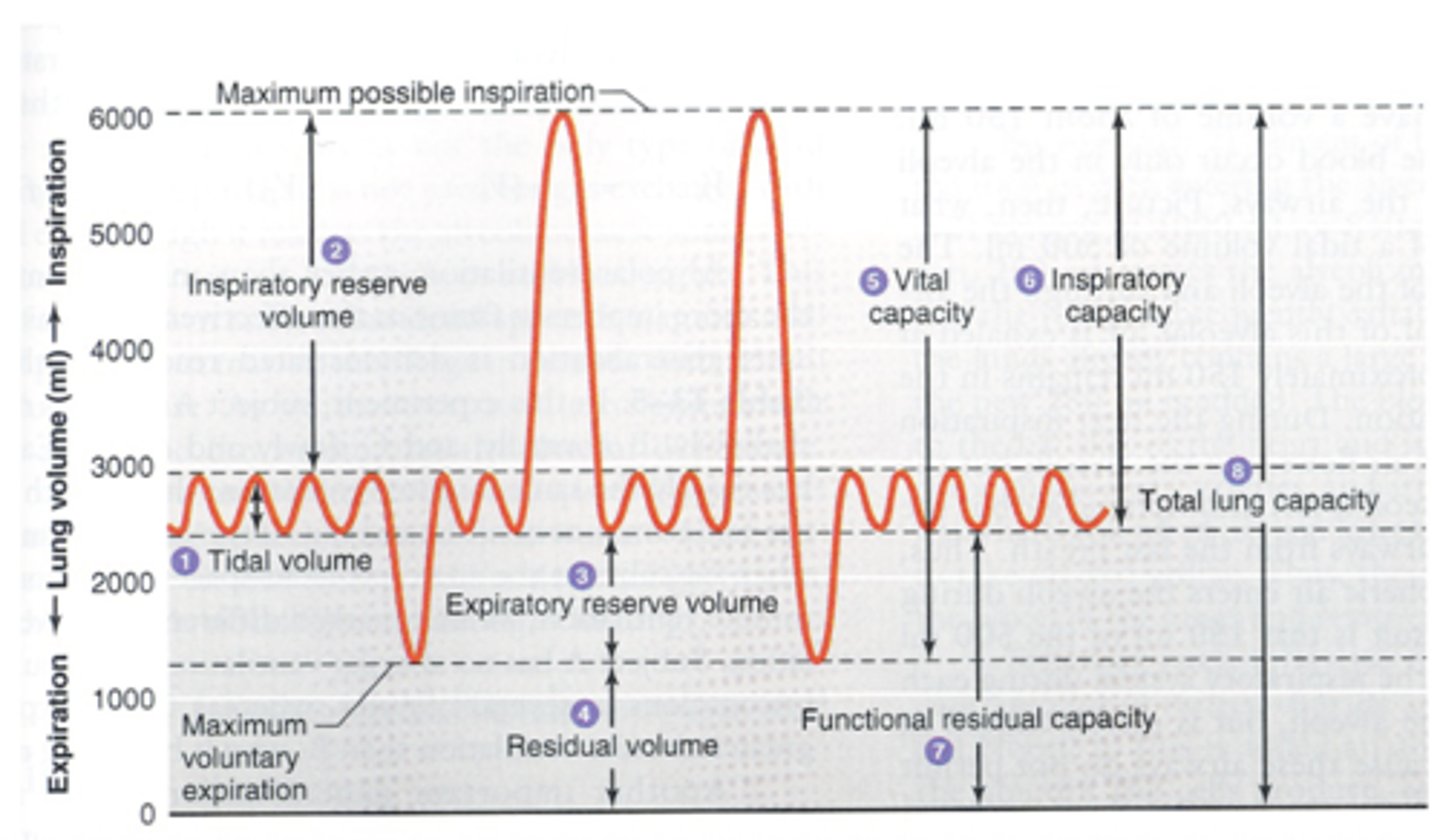
expiratory reserve volume (ERV)
the amount of air that can be exhaled forcibly beyond a normal exhalation
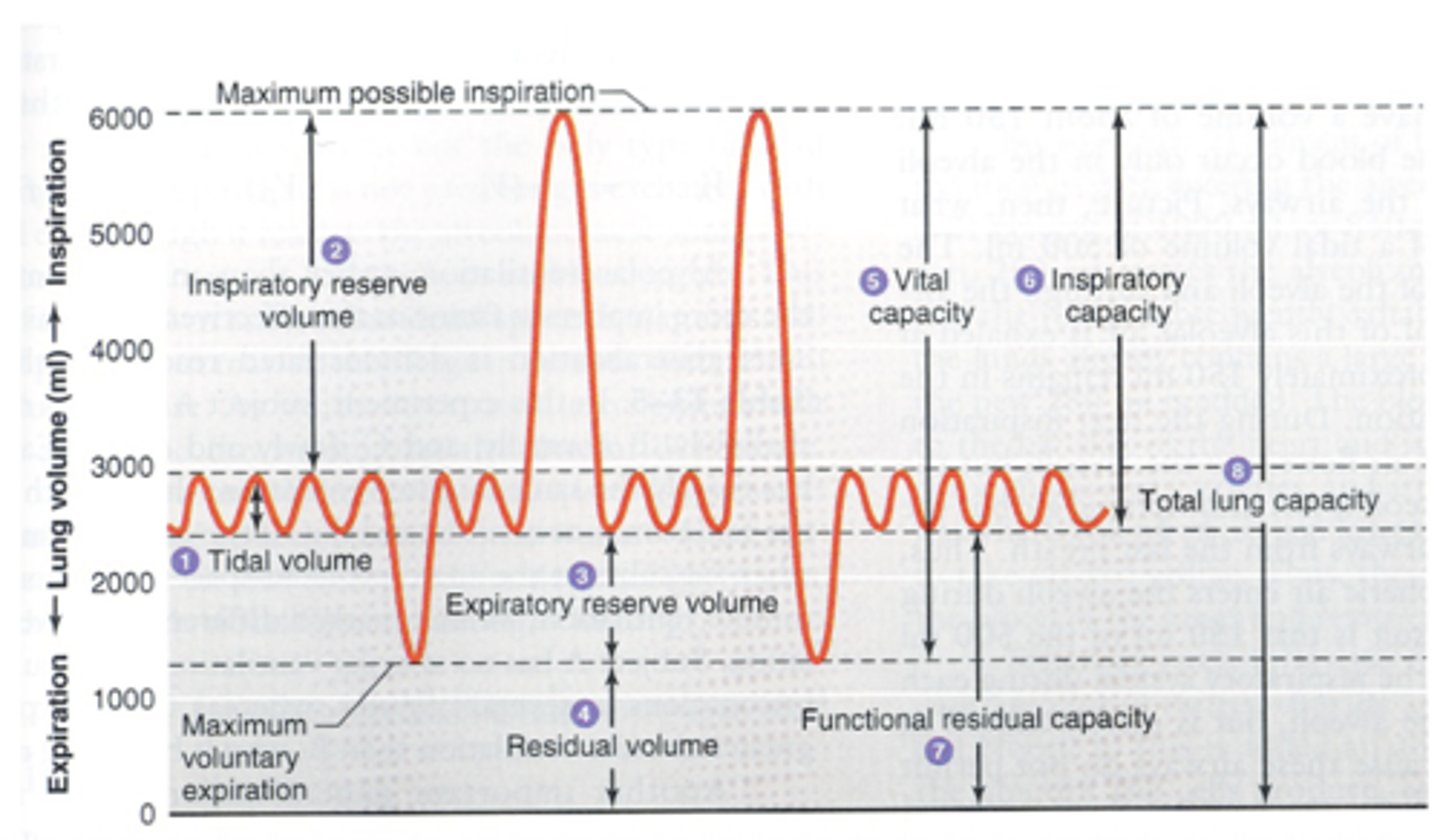
inspiratory capacity (IC)
the maximum amount of air that can be inhaled from the end of a normal, quiet expiration
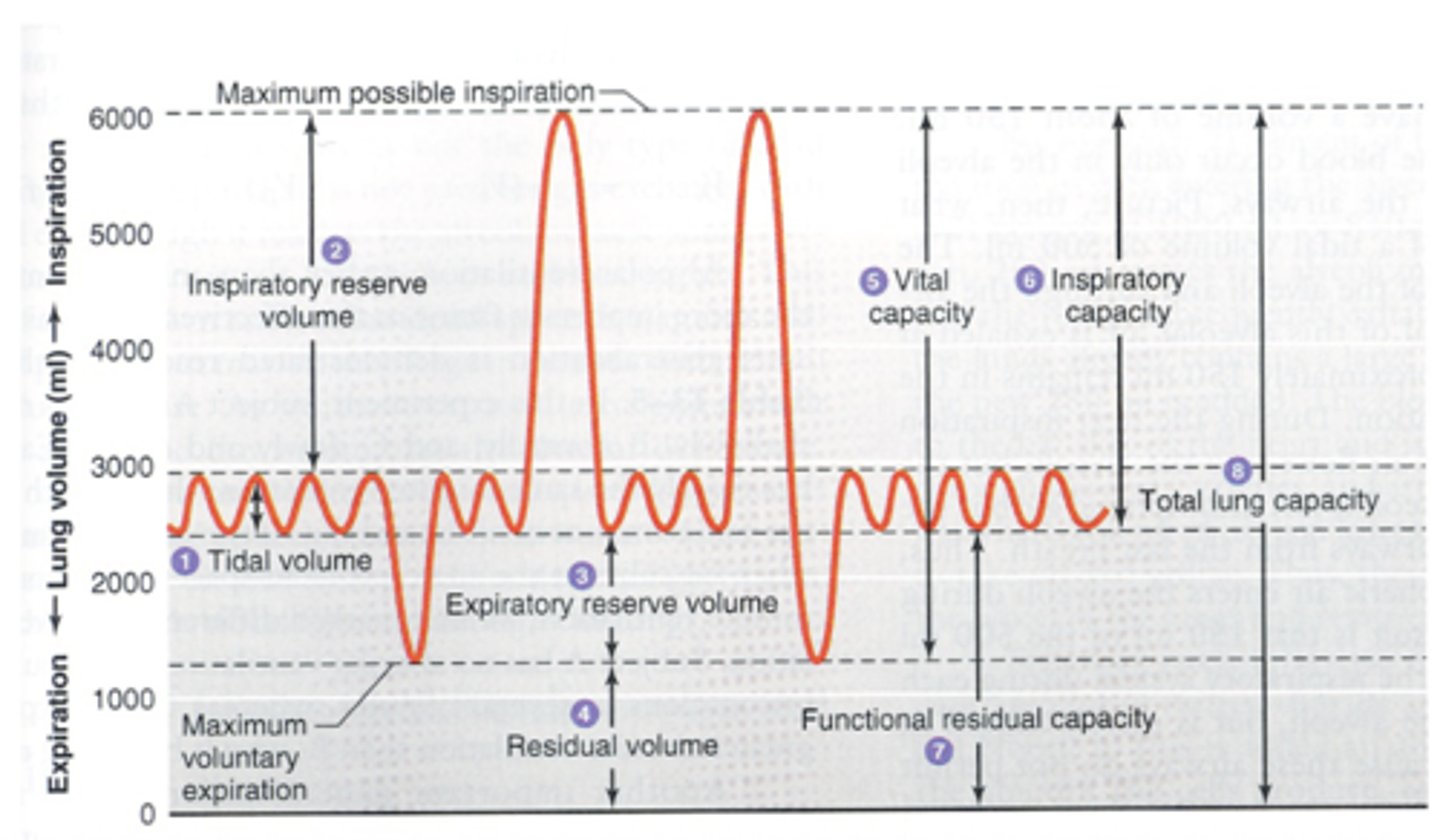
functional residual capacity (FRC)
the volume of air remaining in the lungs at the end of a normal, relaxed exhalation.
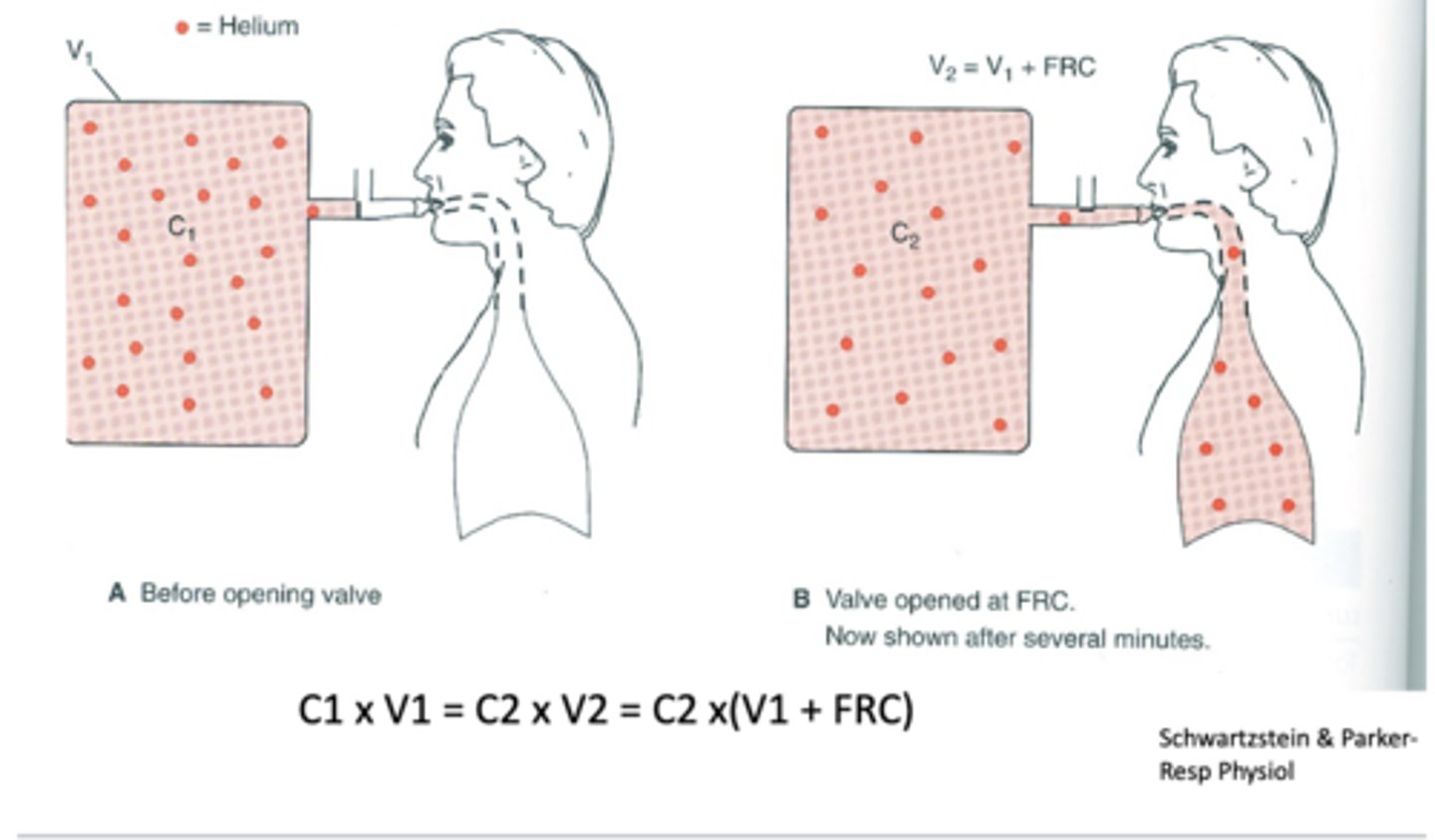
Helium Dilution Method
method to calculate residual volume
C1V1 = C2V2 = C2 x (V1 + FRC)