Control of Cardiac Output and Blood Pressure
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
60 Terms
Why do complex multicellular organisms require a cardiovascular system?
-only in single celled and simple multi cellular organisms: just diffusion
-complex multicellular organisms: req circulatory system to transport these substances around body by bulk flow
what does cardiovascular system include?
-heart
-large vein
-venule
-large artery
-arteriole
-capillary
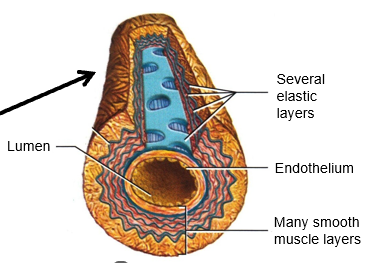
large artery diagram
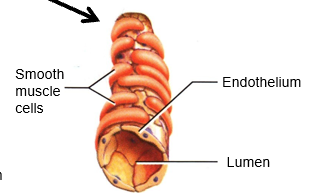
arteriole diagram
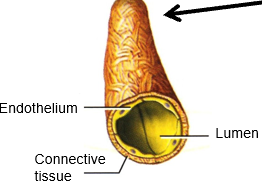
capillary diagram

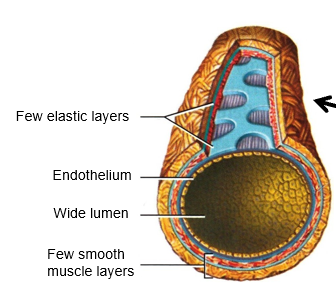
venule diagram
large vein diagram
What is the primary function of Large Arteries (e.g., Aorta)?
-low-resistance
-conducting vessels that carry blood away from the heart
What is the primary function of Arterioles?
-main resistance vessels
-actively constrict or dilate to control regional blood flow
What is the primary function of Capillaries?
-site of exchange for gases, fluids, nutrients, and waste products between the blood and the tissues.
What is the primary function of Venules and Large Veins (e.g., Vena Cava)?
-capacitance vessels: hold or "store" a large percentage of the body's blood volume at rest
-low-resistance vessels that return blood to the heart.
How is blood flow generated?
By the pumping action of the heart.
Why is blood pressure important?
-the driving force (pressure gradient) required to support blood flow around the body
What is the relationship between flow and pressure?
directly proportional (Flow ∝ Pressure)
What is Cardiac Output (CO) and what is its typical value at rest?
-total blood flow through the entire body per minute
-At rest, it is approximately 5 L/min.
What factors can cause short-term fluctuations in Mean Arterial Pressure (MAP)?
-Posture (e.g., standing up/ lying down)
-exercise
-sleep (bp lower when youre sleep)
-stress
-fluid balance (e.g., sweating).
What is the "Darcy's Law" equation for the cardiovascular system?
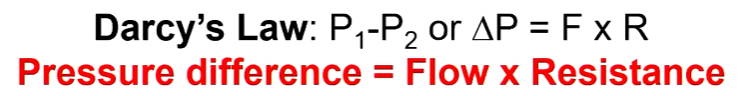
What is the fundamental equation for Mean Arterial Pressure (MAP) in the whole body?
mean arterial pressure = cardiac output x total peripheral resistance

Why is it critical to regulate Mean Arterial Pressure (MAP)?
-MAP must be maintained within normal limits
-ensure that sensitive organs (especially the brain and kidneys) receive sufficient blood flow
-but not so much that the high pressure causes damage.
What are the dangers of MAP being too low for too long (hypotension)?
Insufficient blood flow to organs, leading to fainting (syncope) or tissue death (e.g., gangrene).
What are the dangers of MAP being too high for too long (hypertension)?
Increased risk of stroke, kidney damage, and heart failure (e.g., hypertrophic cardiomyopathy).
What is the cardiovascular "balancing act" required during exercise?
-Cardiac Output (CO) must increase significantly to meet the high metabolic demand of the muscles
-must be done without Mean Arterial Pressure (MAP) rising to a dangerously high level.
What two main factors determine Cardiac Output (CO)?
Stroke Volume (SV): The volume of blood ejected in each heartbeat
Heart Rate (HR): The number of beats per minute.

What four main determinants regulate Stroke Volume (SV)?
Venous Return (related to the Frank-Starling mechanism)
Cardiac Muscle Contractility (Inotropy)
Venous Capacitance
Blood Volume
Why must the outputs from the left ventricle (LV) and right ventricle (RV) be equal over time?
-Because the systemic (body) and pulmonary (lung) circulations are arranged in series (one after the other).
-If they were unequal, blood would pool in one of the circuits.
-temp changes in HR but mechanisms ensure maintained back to same
What is the Frank-Starling mechanism (or Starling's Law of the Heart)?
-intrinsic property of the heart whereby an increase in venous return (the amount of blood filling the ventricle)
-leads to an increase in the stretch of the ventricular muscle
-in turn causes a stronger contraction and an increased Stroke Volume (SV). (In short: "more blood in = more blood out").
What is the cellular mechanism behind the Frank-Starling mechanism?
-Stretching the cardiac muscle (due to increased filling) increases the sarcomere length.
-This leads to an increased sensitivity of the contractile fibers to Ca2+
-resulting in a greater contractile force without a change in the intracellular Ca2+ concentration.
How does the Frank-Starling mechanism ensure that the outputs of the RV and LV remain matched?
-If the RV output temporarily increases, it sends more blood to the lungs
-in turn, increases the venous return to the left atrium and ventricle (LV)
-LV stretches more and, via the Frank-Starling mechanism, its stroke volume increases to match the new, higher output of the RV.
What percentage of total blood is typically "stored" in the veins and venules at rest?
Approximately 60%. This is known as venous capacitance.
What is orthostasis, and how does it affect venous return and stroke volume?
-Orthostasis is standing upright.
-Gravity pulls blood into the distensible (stretchy) veins of the lower body, increasing venous capacitance. This "pooling" of blood reduces the central venous pressure, which decreases venous return to the heart and therefore decreases stroke volume (this can cause fainting).
How does dynamic exercise increase venous return and stroke volume?
Muscle & Respiratory Pumps: The contraction of skeletal muscles and the action of breathing squeeze the veins, pushing blood back to the heart.
Venoconstriction: Sympathetic nerves cause active constriction of the veins, which reduces venous capacitance and increases central venous pressure. Both actions increase venous return, which increases stroke volume (by the Frank-Starling mechanism).
How does a drop in blood volume (e.g., from hemorrhage or diarrhea) affect stroke volume?
A drop in blood volume reduces central venous pressure, which decreases venous return. Due to the Frank-Starling mechanism, this reduced "filling" (preload) leads to a reduced stroke volume.
What is "inotropy"?
Inotropy refers to the intrinsic contractility (force of contraction) of the heart muscle, which is independent of the muscle stretch (Frank-Starling mechanism).
What are "positive inotropes," and what is their effect on stroke volume?
Positive inotropes are substances that increase heart contractility (e.g., adrenaline and noradrenaline from the sympathetic nervous system). They cause the heart to contract harder and eject more blood, leading to an increased stroke volume for any given filling pressure.
What is "chronotropy"?
Chronotropy refers to factors that change the heart rate (HR). A positive chronotrope increases HR; a negative chronotrope decreases HR.
How does the parasympathetic nervous system control heart rate (chronotropy)?
It releases acetylcholine (ACh) via the vagus nerve. ACh acts as a negative chronotrope, slowing the heart rate.
How does the sympathetic nervous system control heart rate (chronotropy)?
It releases noradrenaline. Noradrenaline (and the hormone adrenaline) acts as a positive chronotrope, increasing the heart rate.
What is the "pacemaker potential" in the SA node?
It is an unstable (steadily depolarizing) resting membrane potential. When this potential slowly depolarizes to a certain threshold, an action potential is triggered, causing the heart to beat. The rate of this depolarization sets the heart rate.
How does sympathetic stimulation (noradrenaline) increase heart rate at the SA node?
It increases the slope (or rate) of the pacemaker depolarization. This causes the SA node to reach the action potential threshold sooner, resulting in a faster heart rate.
How does parasympathetic stimulation (acetylcholine) decrease heart rate at the SA node?
It decreases the slope (or rate) of the pacemaker depolarization. This causes the SA node to take longer to reach the action potential threshold, resulting in a slower heart rate.
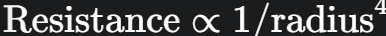
What is the relationship between resistance and the radius of a blood vessel?
Resistance is inversely proportional to the radius to the fourth power. This means a small change in radius (e.g., halving it) causes a massive (16-fold) increase in resistance.
Which blood vessels are primarily responsible for regulating Total Peripheral Resistance (TPR)?
The arterioles, which can actively change their radius through vasoconstriction (narrowing) or vasodilation (widening).
List four major vasoconstrictor stimuli
Noradrenaline (from the sympathetic nervous system)
Adrenaline
Angiotensin II
Vasopressin (ADH)
List three major vasodilator stimuli.
Adrenaline (in some tissues, like skeletal muscle)
Atrial Natriuretic Peptide (ANP)
Histamine
What is the body's primary mechanism for the rapid, short-term control of Mean Arterial Pressure (MAP)?
The Baroreceptor Reflex.
What are the key components of the baroreceptor reflex?
Sensors: Baroreceptors (stretch/pressure sensors) located in the carotid sinuses and aortic arch.
Integrating Centre: The medulla of the brain stem.
Efferent Pathways: The Sympathetic and Parasympathetic nervous systems.
Effectors: The heart (SA node and muscle), veins, and arterioles.
(Baroreflex) What happens when Mean Arterial Pressure (MAP) decreases?
Baroreceptors decrease their firing rate.
The medulla (integrating center) detects this.
The medulla responds by increasing sympathetic drive and decreasing parasympathetic drive.
This coordinated response raises MAP back to its set-point.
(Baroreflex) In response to a drop in MAP, what is the effector response that raises it back to normal?
Heart: Heart rate and contractility increase (↑HR & ↑SV), which increases Cardiac Output (CO).
Veins: Veins constrict (venoconstriction), which increases venous return, further increasing Stroke Volume (SV).
Arterioles: Arterioles constrict (vasoconstriction), which increases Total Peripheral Resistance (TPR).

How does the sympathetic nervous system (activated by the baroreflex) affect the kidneys?
It directly constricts the renal afferent arteriole, which reduces the Glomerular Filtration Rate (GFR) to conserve water.
It stimulates juxtaglomerular (JG) cells in the kidney to secrete the enzyme renin.
What is the immediate, rapid effect of increased renin secretion?
Renin leads to the production of Angiotensin II in the blood. Angiotensin II is a potent vasoconstrictor that rapidly increases Total Peripheral Resistance (TPR), helping to restore MAP.
What is the primary determinant of Mean Arterial Pressure (MAP) in the long-term?
Blood Volume
What is the fundamental relationship between sodium ($\text{Na}^+$), water, and blood volume?
Total body extracellular fluid volume is coupled to the total extracellular Na+ content. Therefore, to regulate blood volume in the long-term, the body must regulate total Na+ content (because water follows salt via osmosis).
What is the full cascade of the Renin-Angiotensin-Aldosterone System (RAAS)?
Renin (from kidney) converts Angiotensinogen (from liver) into Angiotensin I.
ACE (Angiotensin-Converting Enzyme, from lungs) converts Angiotensin I into Angiotensin II.
Angiotensin II stimulates the adrenal gland (adrenal cortex) to secrete Aldosterone.
What is the main, long-term effect of Aldosterone?
Aldosterone is a steroid hormone that acts on the kidney's distal convoluted tubule and cortical collecting duct to increase the reabsorption of Na+ (and water follows). This increases blood volume and, therefore, MAP.
How does the macula densa in the kidney sense low blood volume?
It senses it indirectly. A drop in blood volume/pressure leads to a decrease in Glomerular Filtration Rate (GFR). This, in turn, causes a decrease in the amount of $\text{Na}^+$ delivered in the filtrate to the macula densa, which interprets this as low blood volume and signals the JG cells to release renin.
Why is the effect of Aldosterone considered "long-term"?
Because it is a steroid hormone, it works by altering gene expression to create more Na+ channels and pumps. This is a slow process that produces a lasting effect.
How does the RAAS respond to an increase in blood volume (e.g., from a high salt diet)?
The entire system is suppressed. The increase in blood volume/pressure leads to decreased renin secretion. This reduces Angiotensin II and Aldosterone levels, which in turn decreases $\text{Na}^+$ and water reabsorption, allowing the excess salt and water to be excreted in the urine.
What other hormone is released in response to increased plasma volume, and what does it do?
Atrial Natriuretic Peptide (ANP). It is released by the atria of the heart when they are stretched by high blood volume. ANP promotes the excretion of $\text{Na}^+$ and water by the kidneys (opposite effect of aldosterone), thus helping to lower blood volume and pressure.
If an arterial radius decreases 2-fold (is halved), by how much does resistance to flow change and in what direction?
Resistance increases by 16-fold

Which of the following will raise blood pressure: A vasoconstrictor, A vasodilator, A positive chronotropic agent, Stimulating the parasympathetic NS, Stress, Decreased $\text{Na}^+$ reabsorption?
A vasoconstrictor (increases TPR)
A positive chronotropic agent (increases HR, which increases CO)
Stress (activates the sympathetic nervous system)