Behavioral health
1/132
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
133 Terms
Psychiatric mental health nursing
specialty area of nursing committed to the promotion of mental health and the treatment of behavioral issues, psychiatric disorders, and substance use disorders
Mental health nursing care in all settings
All nurses are responsible for promoting the health, well-being, dignity, and humanity of all, including the individual client, family, and community
Goal of client care
Recovery
Therapeutic milieu
psychotherapeutic-based treatment focused on modifying or controlling the immediate environment in which the client is living
Components of therapeutic milieu
Individualized client-centered treatment based on partnership and collaboration.
Organized in a comprehensive environment that promotes well-being.
Therapeutic relationships, communication, and a trauma-informed approach.
A multidisciplinary team is essential in considering client needs.
Determine individual needs for support and services.
Implement an individual plan, including a program plan, and adherence to a therapeutic schedule of activities and therapies.
Ongoing evaluation of the effectiveness of treatment toward the goal of developing social and life skills
Nurse responsibilities
Providing education
Orienting client and family
Establishing a welcoming trauma-informed environment.
Selecting and advocating for activities
Ensuring culturally sensitive care is provided.
Providing ongoing support and safety
Trauma-informed approach to care
Autonomy
refers to the right to make decisions about one’s own care without undue interference or coercion from others
Competence
A client’s ability to understand information, use reasonable thought processes, communicate their wishes, and understand the consequences of their decisions.
Compacity for decision making
Refers to a client’s ability or inability to make decisions about proposed medical treatments or aspects of their health care
Nonmaleficence
a principle based on the oath of nursing practice to “do no harm.
Beneficence
preventing harm by removing harmful conditions to benefit the client or others or ‘doing good” often defined by actions of kindness and compassion
Fidelity
principle rooted in keeping promises to clients and showing faithfulness while displaying integrity
Veracity
considers the importance of being truthful and authentic with clients during nurse-client interactions
Justice
Ensures that the element of fairness influences nursing decisions and care
Boundary violations
can be either intentional or unintentional, involving the crossing of established boundaries between client and nurse
informed consent
individuals voluntary agreement to participate in treatment or medical procedures based on their understanding of the risks and benefits as well as any alternative treatments
Burden of treatment
interventions, medications, and treatments that may complicate a clients conditions resulting in poor adherences, reduced self-care, and potentially worsening outcomes including increased hospitalizations and poor quality of life
Voluntary admission
Request of client
Client recognition of need for care
Involuntary admission
24-72 hours
Danger to self
Danger to others
Unable to meet basic self-care needs
Mental illness preventing recognition or need for care
Emergency admission
Temporary admission
Client imminent danger to self or others
For evaluation of mental illness
Outpatient mental health clinic
Include a psychiatrist, psychologist, nurse practitioners, clinical nurse specialists, physician assistants with mental health training, nurses with mental health training, and therapists or counselors.
Case management
A case manager helps the client to coordinate their mental health treatment, such as medications, appointments, or arrange transportation
Home based services
a mental health care professional, such as a nurse or social worker, goes into the client’s home to provide services, such as assisting clients to take their medications and monitoring the client’s mental health status
Assertive community treatment
provides the services of an inpatient psychiatric treatment facility with medical staff trained in psychiatric care needs while the client is in their own home
Telehealth
uses virtual technology such as a computer or smartphone with a camera for health care professionals to meet with clients
Mobile mental health crisis teams
specially trained mental health professionals who provide emergency psychiatric care onsite at the client’s location.
Day treatment
provides mental health care and nonclinical support, such as job training
Family services
equips the client’s family and other caregivers with the tools and support to care for the client
Peer services
pair clients with others who have similar symptoms of mental illness, and they are trained to provide support
Process of neurotransmission
A presynaptic neuron interacting with a postsynaptic neuron.
1) Neurotransmitter is released from the
presynaptic neuron
2) Neurotransmitter binds to a specific receptor
3)Returns to presynaptic cleft – reuptake channel
a)Stored for later use
b)Deactivated – enzyme degrades neurotransmitter
c)Diffused away from synaptic connection
4) Binds to specific receptor on presynaptic
neuro for feedback regulation
Dopamine
is an excitatory neurotransmitter that is responsible for transmitting information about emotional responses, complex movements, and cognition. Is responsible for an individual experiencing pleasure and reward from behaviors and its neurotransmission can be affected by stress
Serotonin
an inhibitory neurotransmitter that is responsible for emotional regulations, sexual behaviors, temperature regulation, sleep, and pain management
Norepinephrine
an excitatory neurotransmitter that is responsible for learning, sleep, mood, memory, and attention.
Histamine
has a unique role in neuromodulation.
The pre and postsynaptic receptors for histamine regulate the release of histamine, glutamate, serotonin, and gamma amino butyric acid (GABA). The known postsynaptic receptors for histamine in the brain mediate the effects of alertness and wakefulness
Gama Amino Butyric Acid (GABA)
an amino acid that serves as an inhibitory neurotransmitter.
Similar to histamine, GABA modulates other neurotransmitters.
Glutamate
an amino acid that serves as an excitatory neurotransmitter.
Helpful with memory.
Acetylcholine
a neurotransmitter that has inhibitory and excitatory properties. With receptors found throughout the body particularly in the skeletal muscles.
Regulates the sleep-wake cycle and is a primary neurotransmitter for muscle functioning.
Neurobiology
Mental health is associated with genetics or that mental illness can be inherited.
Family Study: A type of study that seeks to understand the cause of behaviors among those who share a genetic history.
Adoptive Study: A type of study that seeks to understand the cause of behaviors when comparing those who share and do not share a genetic history but are raised in identical environmental conditions.
Twin Study: A type of study that seeks to understand the cause of behavior when comparing genetically identical people
Psychiatric pharmacogenomic testing
strategy that a health care provider may choose to use that improves the likelihood of selecting an effective psychotropic medication based on the client’s genes.
Stress and psychoimmunology
field of science that attempts to expand knowledge related to the impact of psychosocial stress on the body’s immune system
Infection r/t mental illness
mental illness can be described according to previous or current infection
It is theorized that viral infection possibly alters genetic composition in the central nervous system leading to the presentation of mental illness.
There is a causal association. however, none of these studies are conclusive
Neuroplasticity
refers to the brain’s ability to adapt synaptic connections, particularly in response to stress or learning or after experiencing an injury.
Explains why some manifestations of mental illness increase in severity over time, such as Major Depressive Disorder, and cannot be cured through a single dose of medication
Stressor
An event, situation, or condition that results in psychological or physical stress
can be internal (in the individual) or external (outside the individual)
Stress response
The human body is designed for experiencing. It is a survival response that helps an individual respond quickly to a threatening situation.
Acute response
results in physiological changes such as an make your heart rate increase, muscles tense, and your breathing increase. Following acute stress response, the individual returns to a state of equilibrium)
Repeated or excessive response
there is a risk that a sequence of physiological and hormonal changes or repeated stress experiences can result in an overreaction to the stressors.
Biological and physiological response
Perceived (thinking about the stress) or experienced stress (actual occurrence)
Maladaptive stress
A type of stress response that includes characteristics both biological and behavioral that are detrimental and interfere with optimal functioning and coping with life.
Resilience
ability to successfully adapt to difficult or challenging life experiences that are mentally and emotionally challenging, requiring flexibility in behaviors to adapt to external and internal demands.
Chronic stress
when stress becomes a problem when an individual is repeatedly exposed to stress, or stressors continue over a period of time, leaving the individual no opportunity for recovery
Stress system pathway
1) Stressful Event Experienced
2) amygdala (command center)
3) Hypothalamus (CRH) begins Hypothalamic-Pituitary-Adrenal (HPA) Axis (ACTH)
4) Autonomic Nervous System (ANS) & Central Nervous System (CNS)
5) Stress Response Communicated Throughout the Body
Physiological effects of stress
endocrine system: releases cortisol, adrenaline and noradrenaline. Resulting constriction of blood vessels. Less growth hormone is released, and fewer sex hormones are produced.
heart: beats more rapidly, pumping more blood. Increased blood flow t mussels while blood flow to organs decreases. Blood pressure rise.
Lungs: More oxygen is consumed, and more carbon dioxide is expelled. Breathing is faster and shallower
Skin: Sweating
Pancreas: Releases glucagon, produces less insulin and blood glucose rises
Fight-Flight-Freeze-Faint-Fawn
Fight: Facing the stressor or situation ready to confront or flight
Anger, aggression, stomping, kicking punching, stomach in knots, nausea, vomiting
Flight: Running away from or fleeing the stressor
Anxiety and feeling trapped, tension, wide eyes, restlessness (feet, legs), fidgeting
Freeze: Unable to respond or react against the stressor or situation
Dread, heart pounding and numbness, pallor, holding breath
Fawn: Attempting to please or give in to the stressor or situation
Self-directed anger, lack of boundaries, feeling no identity, trying to please aggressor, ignoring own desires
Faint: Limiting exposure to stress by physically fainting or experiencing syncope
Changes in vision, feeling lightheaded, blacking out, falling
General adaptation syndrome
Explanation was based on physical responses and the Selye model explains how the body wants to adapt (reduce stress) and that the body has limits and can run out of energy
Alarm (acute) stage
when the sympathetic nervous system is activated, resulting in two substages:
Shock—resulting in a decrease in blood pressure, temperature, muscle tone, and a loss of bodily fluid—
Countershock, where the adrenal glands release the catecholamine adrenaline resulting in increased sympathetic nervous system (SNS) activity
Resistance Stage also described as the adaptation stage, is when the body attempts to adapt to the stressor. An individual remains on alert and prepared to respond for self-protection as it did in the alarm stage
If the stressor diminishes, the individual can return to homeostasis.
If stressor does not diminish, the individual moves into the final stage of exhaustion
Exhaustion stage
the body has depleted its resources and can no longer adapt to the stressor. Internally, the body’s tissues and organs are depleted, and the result can lead to illness, disease, or death.
Prolonged or chronic stress response system
Body learns experiences of stress, fear, or trauma are normal occurrence
Any age but particularly harmful during childhood
Experience of sustained stressors
Physical or emotional maltreatment, chronic neglect, exposure to violence, family economic hardship, or a caregiver's substance use disorder or mental health disorder.
Often referred to as adverse childhood experiences (ACES)
Long term/lifelong complications r/t toxic stress
Stress-related disorders
Cognitive impairment and complications in learning
Physical health issues
Mental illness
Psychological and behavioral manifestations of stress
Anxiety
Irritability
Depression
Panic attacks
Increased sadness
Excessive worry
Eating disorders
Substance use disorders or addictive behaviors such as gambling
Alterations in executive functioning, including language and problem-solving
Delayed development or regression
Compulsive behaviors such as shopping and sex
Stress response risk factors
Feeling a lack of control,
hopelessness,
negative self-talk,
internalizing/externalizing problems/situation,
racism,
reduced social interaction or negative interactions,
previous or repeated exposure to trauma,
poverty,
adverse childhood experiences,
discrimination,
genetics,
Protective factors
Perception of control,
hardiness,
realistic expectations,
healthy lifestyle
positive- safe-secure work,
home, and school environment,
positive-secure relationships,
parental bonding,
connection to culture,
beliefs,
spiritual practices
Problem focused coping
requires adjusting or managing the problem that has caused the stress. It is action-focused.
Example: A client who creates a list or a plan on how to tackle the issue and reduce stress.
Emotion focused coping
styles vary and are action-focused. These coping styles reduce the negative emotions associated with stress.
Example: A client who seeks out support and resources that nurture their emotional health.
Avoidant coping
described as cognitive and behavioral efforts directed toward diminishing, ignoring, or denying stressful situations in an effort to avoid dealing with the stressor and is a passive way of coping that focuses on ignoring the stressor.
Example: A client who avoids the stressor by drinking or
sleeping.
Anxiety
Feelings of worry or fear or nervousness when stressed or threatened
Temporary anxiety can be motivational
Persistent or excessive can interfere with function
Normal response to stress and a common human experience
physiologic expression of anxiety optimally serves an adaptive function to protect an individual from dange
When does anxiety become a disorder
when it interferes with function
Feelings of anxiety occur at inappropriate times or situations.
Frequency of anxiety increases.
Intensity of anxiety affects a person’s ability to function.
Duration of anxiety becomes increasingly prolonged.
Separation anxiety disorder
The client experiences excessive fear or anxiety when separated from an individual to which the client is emotionally attached
Social anxiety disorder
The client experiences excessive fear of social or performance situations
Specific phobias
The client experiences an irrational fear of a certain object or situation. Specific clinical names are used to refer to specific phobias
Panic disorder
The client experiences recurrent panic attacks
Agoraphobia
The client experiences an extreme fear of certain places (the outdoors or being on a bridge) where the client feels vulnerable or unsafe
Generalized anxiety disorder (GAD)
The client exhibits uncontrollable, excessive worry for at least 6 months
Anxiety risk factors
Most anxiety disorders are more likely to occur in females (same with OCD except for hoarding) Anxiety and obsessive-compulsive disorders have a genetic and neurobiological link.
Clients can experience anxiety due to an acute medical condition, (hyperthyroidism or pulmonary embolism).
important to assess the manifestations of anxiety in a medical facility to rule out a physical cause.
Adverse effects of many medications can mimic anxiety disorders.
Trauma or negative life experiences such as adverse childhood experiences.
Lifestyle choices including poor diet, exercise, and substance use.
Substance-induced anxiety is related to current use of a chemical substance or to withdrawal effects from a substance (alcohol).
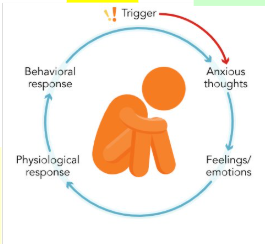
Anxiety cycle
trigger → anxious thoughts → feelings/emotions (fear, worry, dizziness) → physiological response → behavioral response
Separation anxiety disorder expected findings
The client exhibits excessive levels of anxiety and concern when separated from someone to whom they have an emotional attachment, fearing that something tragic will occur resulting in permanent separation.
The client’s anxiety disrupts the ability to participate in routine daily activities.
Physical manifestations of anxiety develop during the separation or in anticipation of the separation and include headaches, nausea and vomiting, and sleep disturbances.
Specific phobias expected findings
The client reports a fear of specific objects (spiders, snakes, or strangers).
The client reports a fear of specific experiences, (flying, being in the dark, riding in an elevator, or being in an enclosed space).
The client might experience anxiety manifestations just by thinking of the feared object or situation and might attempt to decrease the anxiety through the use of alcohol or other substances.
Agoraphobia expected findings
The client avoids certain places or situations that cause anxiety. This avoidance might disrupt the client’s ability to maintain employment or participate in routine activities of daily life.
The client’s fear and manifestations of anxiety are out of proportion with the actual danger of the place or situation.
Social anxiety disorder expected findings
The client reports difficulty performing or speaking in front of others or participating in social situations due to an excessive fear of embarrassment or poor performance.
The client might report physical manifestations (actual or factitious) in an attempt to avoid the social situation or need to perform.
Panic disorder expected findings
Panic attacks typically last minutes but may occasionally continue for longer periods.
Four or more of the following manifestations are present during a panic attack:
Palpitations
Shortness of breath
Choking or smothering sensation
Chest pain
Nausea
Feelings of depersonalization
Fear of dying or insanity
Chills or hot flashes
The client might experience behavior changes and/or persistent worries about when the next attack will occur
Generalized anxiety disorder
The client exhibits uncontrollable, excessive worry for the majority of days over at least 6 months.
GAD causes significant impairment in one or more areas of functioning (work-related duties).
Manifestations of GAD include the following:
Restlessness
Muscle tension
Avoidance of stressful activities or events
Increased time and effort required to prepare for stressful activities or events
Procrastination in decision making
Sleep disturbance
Low anxiety
More restless
Moderate anxiety
Trouble sleeping fr
Severe
Overwhelmed
Acting out
Unsure what to do
Panic
Feels terror
Exhausted
No longer responding to stimuli
Obsessive compulsive disorder
occurs when one experiences obsessions, which are persistent and recurrent thoughts or urges that are unwanted and become intrusive.
Compulsions are repetitive behaviors that are performed by the client with OCD to lessen or prevent anxiety brought on by their obsessions.
These obsessions and compulsions become time-consuming and interfere with the client’s ability to perform daily tasks.
precipitated by anxiety.
can be diagnosed in children and adults.
Examples of obsessions
Thoughts about being harmed or harming someone else
Fears for safety
Concern for cleanliness or germs
Fear that they are offending a higher power or deity
Fear of forgetting something important
Worry about how tidy or neatly arranged items are
Examples of compulsions
Checking and rechecking that a door is locked
Ritualistic order for handwashing
Repeating specific words of phrases
Hurting self, such as hair pulling
Counting objects, items, or actions
Repeating an activity a specific number of times
Hoarding disorder
the client has difficulty parting with possessions, resulting in extreme stress and functional impairments.
Body dysmorphic disorder
client has a preoccupation with perceived flaws or defects in physical appearance.
Manifestations of OCD
Experiencing a pattern of uncontrollable obsessive thought and associated compulsive behaviors or rituals.
Cleaning
Washing hands
Ordering or counting objects or behaviors
Taboo or forbidden thoughts
Manifestations of hoarding disorder
Demonstrating a persistent difficulty or inability to discard or part with possessions.
Differs from collecting as symptoms result in excess accumulation of possessions that clutter and overwhelm living areas.
Manifestations of body dysmorphic disorder
Persistent preoccupation with perceived defects or flaws in one’s appearance.
Mirror checking
Excessive grooming
Skin picking
Seeking reassurance about looks
Possible eating disorder
Manifestations of trichotillomania
Demonstrating a pattern of ritualized behavior defined by serially and intentionally pulling out one’s hair.
Behaviors are triggered by boredom and/or anxiety
Results of behavior reduce tension, lead to form of gratification, and pleasure or a sense of relief
Manifestations of excoriation disorder
Pattern of behavior defined by the recurrent picking at one’s skin, resulting in lesions
Physical manifestations commonly found on hands, face, arms, or multiple body sites
May pick pimples, scabs, or previous picked areas of skin
Extensive time daily is spent picking
Often client attempts to cover with clothing or makeup
Nursing care for anxiety
Providing trauma-informed care considers the client’s experience and requires the nurse to be aware, sensitive, and responsive.
Provide a structured interview to keep the client focused on the present.
Assess for comorbid condition of substance use disorder.
Provide safety and comfort to the client during the crisis period of these disorders, as clients in severe- to panic-level anxiety are unable to problem solve and focus. Clients experiencing panic-level anxiety benefit from a calm, quiet environment.
Remain with the client during the worst of the anxiety to provide reassurance.
Perform a suicide risk assessment.
Provide a safe environment for other clients and staff
use relaxation techniques with the client as needed for relief of pain, muscle tension, and feelings of anxiety.
Instill hope for positive outcomes (but avoid false reassurance).
Enhance client self-esteem by encouraging positive statements and discussing past achievements.
Assist the client to identify defense mechanisms that interfere with recovery.
Postpone health teaching until after acute anxiety subsides. Clients experiencing a panic attack or severe anxiety are unable to concentrate or learn.
Identify counseling, group therapy, and other community resources for clients who have anxiety.
Non-pharmacologic interventions
Psychotherapy
Talk therapy focused on the client’s specific anxiety
Cognitive Behavioral Therapy (CBT)
Psychotherapy directed at how the client thinks, behaves, and reacts to causes and feeling of anxiety
Cognitive therapy
Similar to CBT, it is focused on identifying the cause of anxiety and eliminating thoughts that are distorted or unhelpful regarding anxiety or stressors
Exposure therapy
The client is exposed to the underlying cause of anxiety that they are avoiding, such as driving in traffic or riding in an elevator, to gradually become more comfortable with the activity
support groups
Groups focusing on sharing and achieving goals related to anxiety management
Complimentary-integrative approaches
Therapy that focuses on relieving anxiety in specific situations, such as during a medical procedure. Practices include relaxation techniques (deep breathing, guided imagery, progressive body relaxation), hypnosis, massage therapy, mindfulness meditation, and music
Lifestyle management
Helping the client make better choices, including nutritional strategies (healthy diet), exercise, and avoiding excessive caffeine or substance use
Sedative hypnotic anxiolytics
Benzodiazepines: Alprazolam, Diazepam, Lorazepam
Sedative hypnotic anxiolytics MOA
Enhance Inhibitory effects of gamma-aminobutyric acid (GABA) in the CNS. Short-term use recommended due to dependence.
Sedative hypnotic anxiolytics therapeutic uses
GAD
PTSD, Hyperarousal, Insomnia, Muscle Spasms, ETOH withdrawal.