Digestion and Absorption
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
27 Terms
What is absorbed and what is digested?
Macromolecules digested
Nutrients absorbed
Where does absorption mainly occur and what does it require for it to occur?
• Mainly in the Small Intestine → mostly in the duodenum, but also water in the colon
• Requiring a variety of transport mechanisms specific for particular molecules
What is the main objective of Digestion and where does it occur? What are the different types of enzymes that are secreted?
Objective: to break macromolecules down into monomer or dimer units for absorption
• Localised to different areas of the gut where (most occurs in the duodenum:
- The optimal pH of enzymes differ
- Some enzymes may be secreted as inactive precursors, and need enzymatic activation
- Some enzymes exist as membrane bound forms (by the epithelial border)
What is needed if transport is against a conc. gradient
Energy must be used (primary or secondary active transport)
Mainly driven by Na-ATPASE-K pump
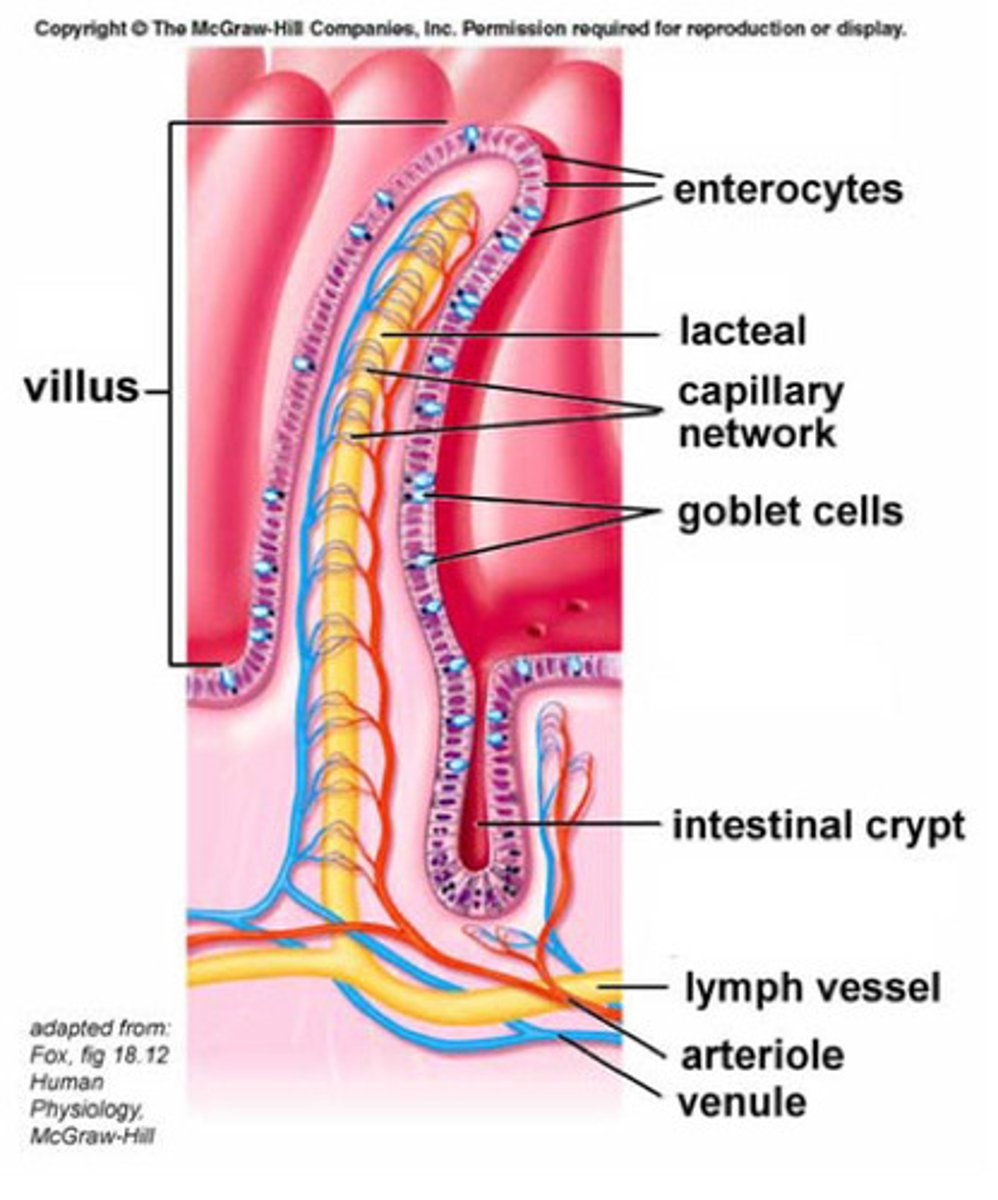
Small intestine structure reminder - what features does it have to help it carry out its functions oabsorption and digestion?
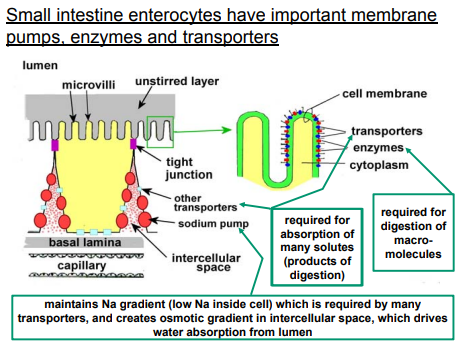
What are the most important membrane pumps, enzymes and transporters of the small intestine enterocytes?
Villi highly vascularised as they take the nutrients to the rest of the body
—
Enterocytes are important for absorption of nutrients and digestion
Each enterocyte has microvilli (the brush border) to increase SA to make absorption as efficient as possible
—
Single epithelial layer to promote absorption of nutrients
Tight junctions to stop pathogens and foreign cells and certain inflammatory markers getting into circulation
—
Lots of transporters on cell membrane required for absorption of many solutes (products of digestion)
Lots of enzymes on the cell membrane also required for digestion of macromolecules
—
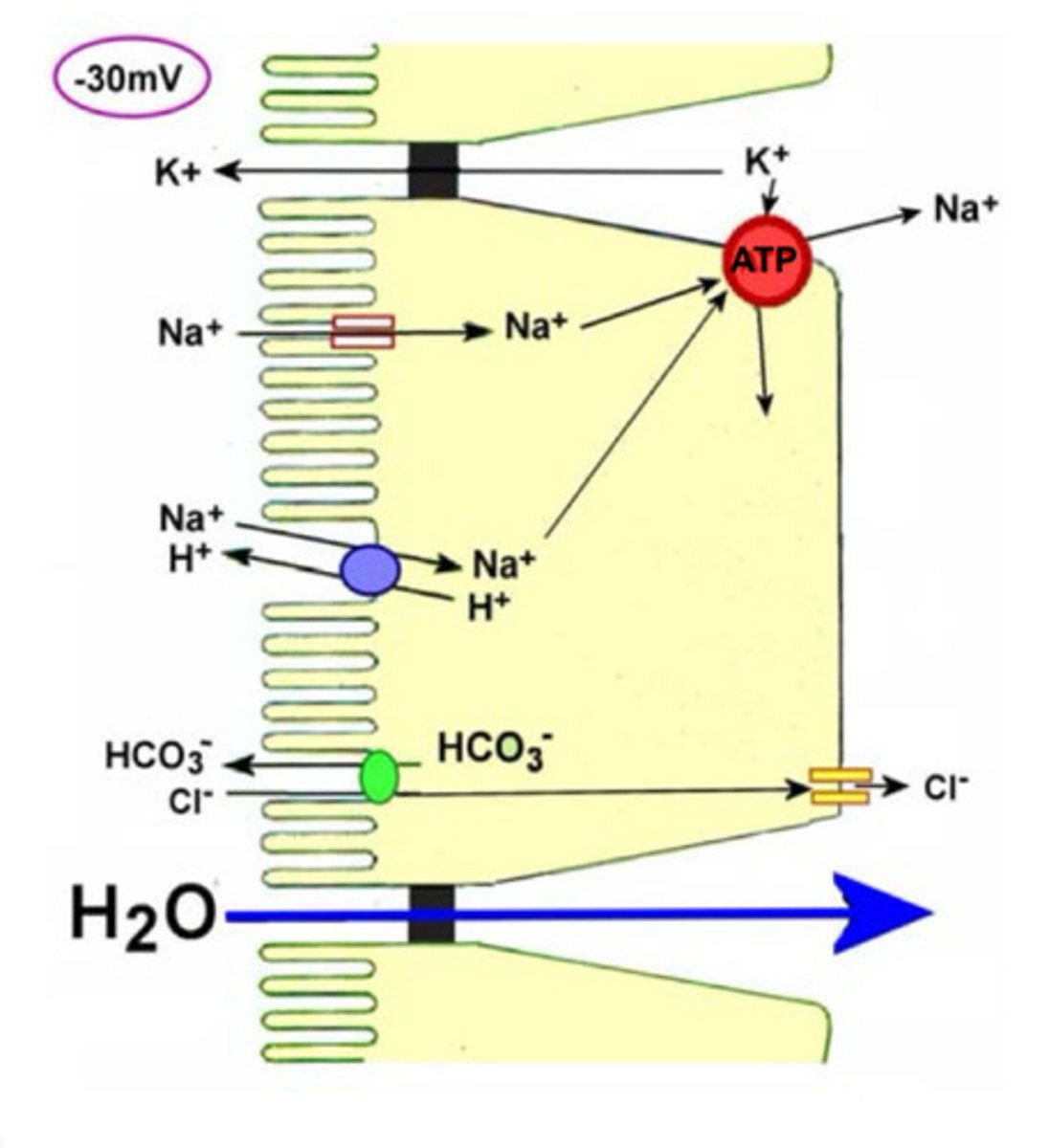
The sodium-atpase pump maintains Na gradient (low Na inside cell) which is required by many transporters, and creates osmotic gradient in intercellular space, which drives water absorption from lumen
Amino acids and monosaccharides go straight into the capillaries into blood circulation but lipids go into the lacteal system (distributes fats all over the body and dump fats into the blood stream) first.
What are the most important membrane pumps, enzymes and transporters of the small intestine enterocytes? part 2
The small intestine enterocytes rely on several key membrane pumps, enzymes, and transporters for nutrient absorption and digestion:
Membrane Pumps: The sodium-potassium pump (Na+/K+-ATPase) is the most critical, maintaining a sodium gradient across the cell membrane, which drives water and nutrient absorption.
Enzymes: Brush border enzymes like maltase, sucrase, lactase, and peptidases are essential for breaking down disaccharides and peptides into absorbable monosaccharides and amino acids.
Transporters: Sodium-dependent glucose transporters (SGLT1) and amino acid transporters (e.g., B0AT1) are vital for absorbing glucose and amino acids, respectively, using the sodium gradient.
Additionally, fatty acid transporters (e.g., FAT/CD36) facilitate lipid uptake.
Transporters and Enzymes on Microvilli: The microvilli have a cell membrane with embedded transporters and a glycocalyx (a carbohydrate-rich coating). Enzymes like maltase, sucrase, lactase, and peptidases are anchored in the glycocalyx, breaking down macromolecules (e.g., starches and proteins) into smaller, absorbable units (e.g., glucose, amino acids). Transporters on the luminal side (e.g., SGLT1 for glucose, amino acid transporters like B0AT1) move these nutrients into the cell.
Luminal and Basolateral Transporters: Transporters on the luminal (apical) side bring nutrients into the enterocyte, while basolateral transporters (e.g., GLUT2 for glucose) move them out into the bloodstream or interstitial space. This directional flow ensures efficient nutrient delivery.
Sodium-Potassium ATPase Pump: Located on the basolateral membrane, the Na+/K+-ATPase pump maintains a low sodium concentration inside the cell by pumping sodium out into the interstitial space. This creates a sodium gradient that drives nutrient absorption (e.g., via SGLT1) and an osmotic gradient that pulls water from the lumen into the interstitial space, aiding absorption.
Water Movement: Water is absorbed both paracellularly (between cells via tight junctions) and transcellularly (through cells via aquaporins), driven by the osmotic gradient created by sodium movement.
These components work together to ensure efficient digestion and absorption of macronutrients.
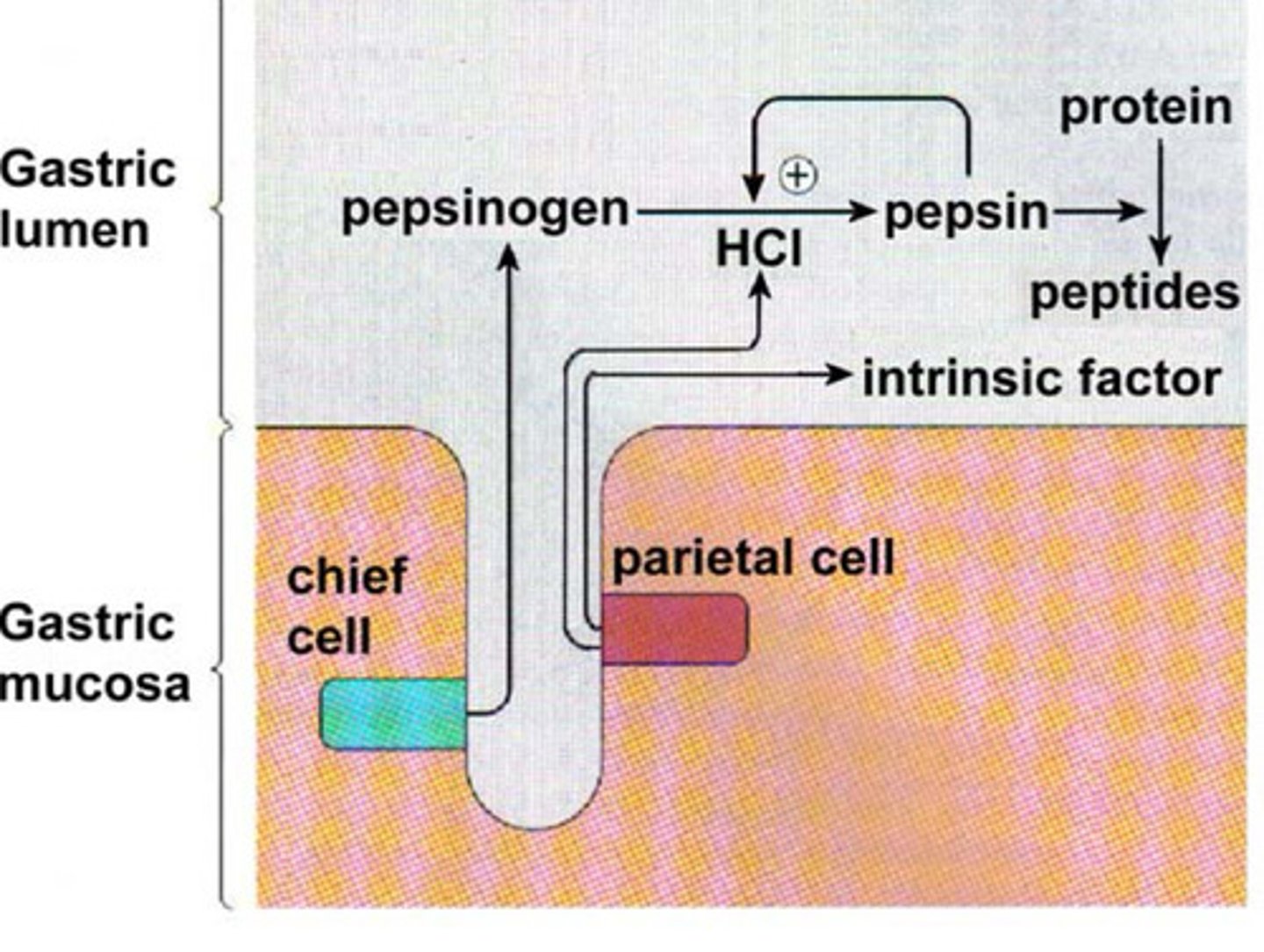
1) Describe the process of digestion of proteins in the stomach
STARTS with Pepsin + HCl in stomach
Pepsinogen, released by the chief cells under HCL (creates acidic stomach condition) which drives the conversion of pepsinogen into pepsin (-inogen = it is inactive (Pepsin is its active form) to break down protein into peptides
The parietal cell is what releases HCL and intrinsic factors
Stomach gradually releases chyme into the duodenum
What is Chyme, what is its pH and what does it contain?
Released from the stomach (Pyloric Sphincter)
Low pH (acidic)
Contains:
Solubilised, slightly digested carbohydrates
Solubilised, partly digested proteins
Slightly digested fats
Intrinsic factor which enables Vit B12 to be absorbed in the small intestine
What is required for further digestion of foodstuffs to take place:
• Other enzymes are supplied (from pancreas or made by enterocytes) Pancreatic: Trypsin, lipase, amylase (break down proteins, fats, carbs). / Brush border: Lactase, peptidases (final digestion).
• pH has to be neutralised (Bicarbonate (HCO₃⁻) from pancreas/Brunner’s glands raises pH to ~6–7.)
• Bile salts needed for fat digestion (Emulsify fats → form micelles for absorption.)
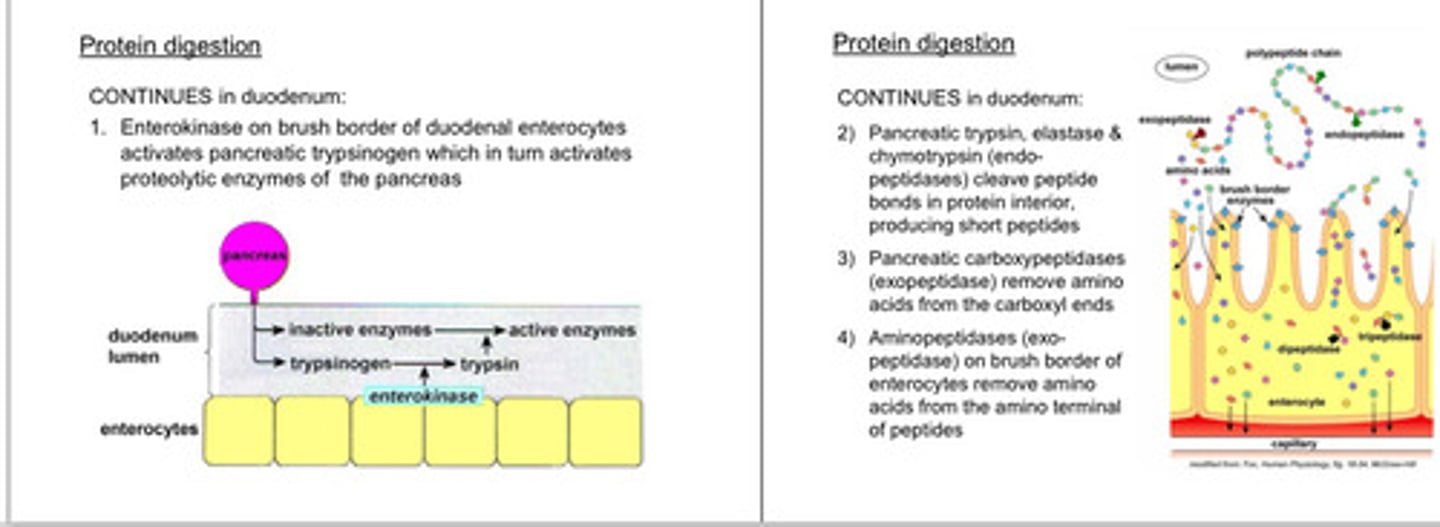
2) Describe the process of digestion of proteins in the Duodenum
-Protein digestion continues in the duodenum
Steps:
1. Enterokinase on brush border of duodenal enterocytes activates pancreatic trypsinogen which in turn activates proteolytic enzymes of the pancreas
2) Pancreatic trypsin, elastase & chymotrypsin (endopeptidases) cleave peptide bonds in protein interior, producing short peptides
3) Pancreatic carboxypeptidases (exopeptidase) remove amino acids from the carboxyl ends
4) Aminopeptidases (exopeptidase) on brush border of enterocytes remove amino acids from the amino terminal of peptides
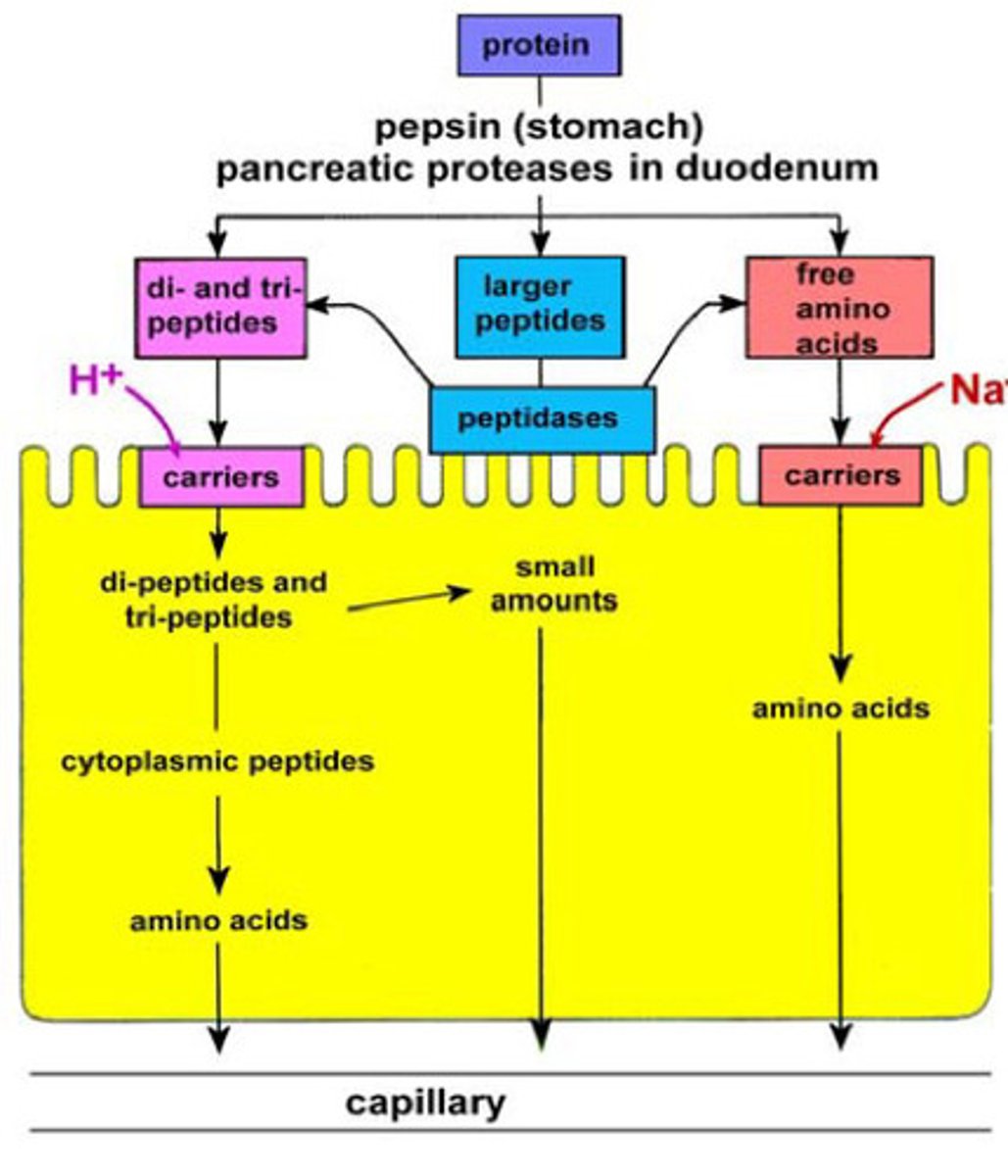
How are amino acids and peptides absorbed?
• amino acids absorbed via Na+-linked lumenal transporters, then exit on basolateral side
• di- and tri-peptides absorbed via H+-linked lumenal transporters (co-transported with H+ ions), then hydrolysed to amino acids before exiting on basolateral side. A small amount of di and tri peptides can be absorbed but not very efficient, what we really want is everything in amino acid form for good absorption.
-If we get larger peptides at this point that has escaped some digestion - these are broken down into di and tri peptides or free amino acids by peptidases
How do infants absorb amino acids and peptides?
Small intestinal wall is permeable to peptides, allowing for absorption of growth factors & antibodies from colostrum (first milk)
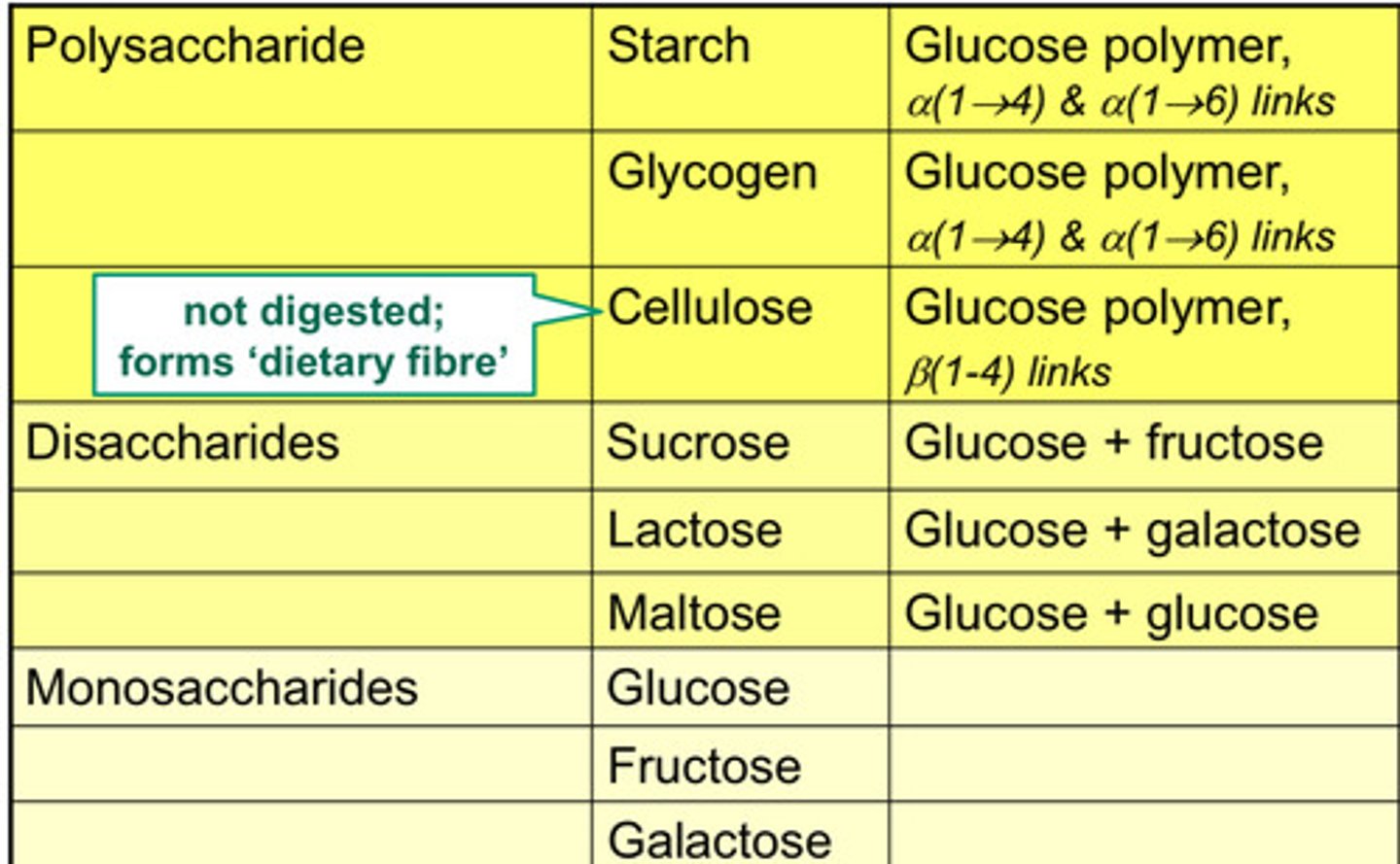
Formats of Carbs in food
-We want to break down Disaccharides into monosaccharides so we can absorb them efficiently
1) Describe the process of digestion of carbohydrates
3 Digestive sections:
- salivary amylase: - optimum pH is 6.8, so some hydrolysis in the mouth
- swallowed bolus then enters acidic stomach
- pancreatic amylase - mostly here: - optimum pH is 7.1
- cleaves straight chains but cannot cleave bonds at branch points
-produces short oligosaccharides, maltose (disaccharide) and maltriose (trisaccharide)
-further digestion of these and other disaccharides (lactose, sucrose) to monosaccharides by brush border enzymes (AIM IS TO MAKE EVERYTHING A MONOMER - GLUCOSE, FRUCTOSE AND GALACTOSE)
3. small intestine membrane-bound disaccharidases: - optimum pH values between 6 and 7
-Duodenal (the duodenum is part of the small intestine) pH therefore suitable for (2) and (3)
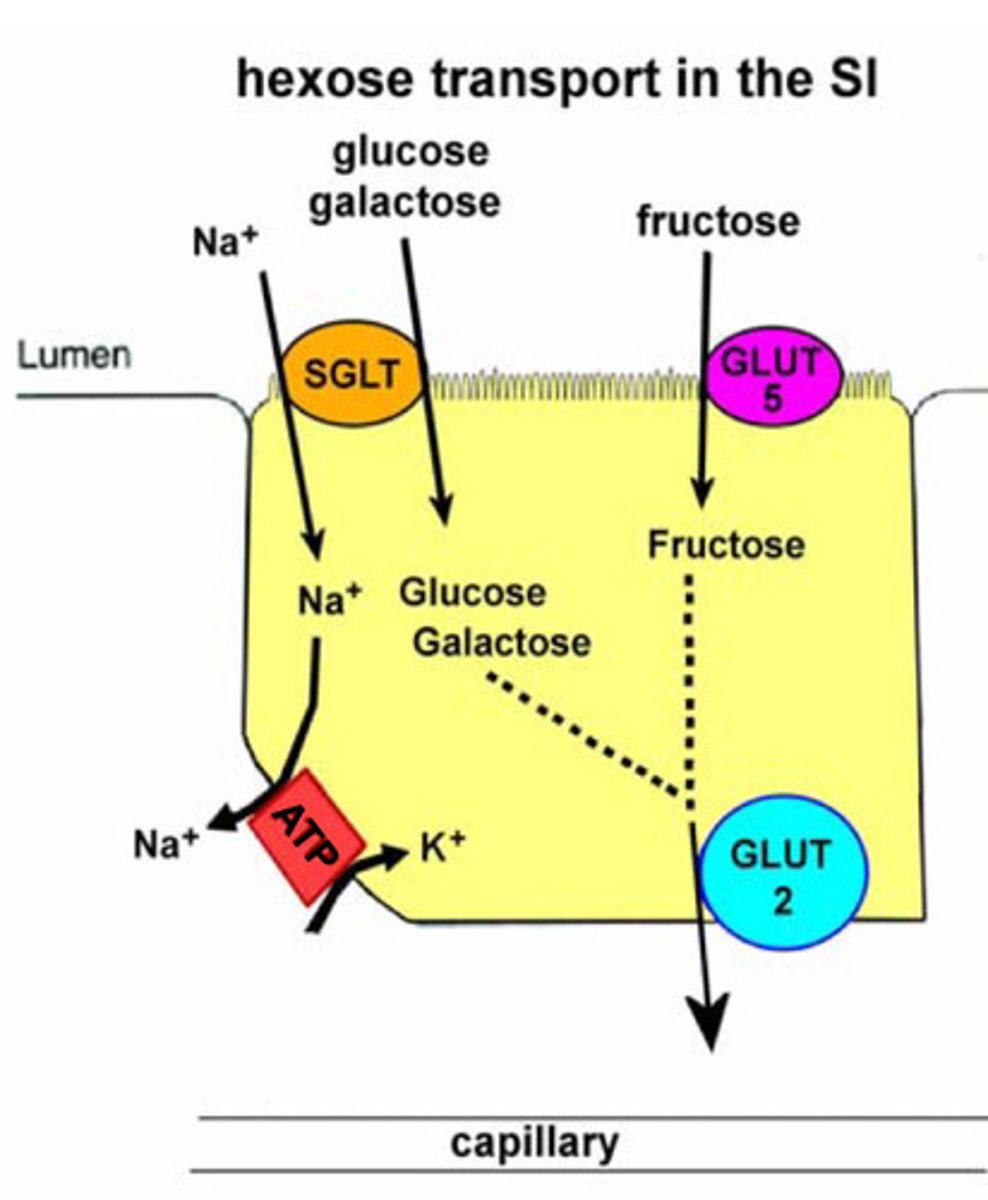
Describe how carbohydrates are absorbed into the bloodstream?
Apical/lumenal side:
• SGLT (Na-linked transporter) for glucose & galactose, Secondary active transport
• fructose via GLUT5, facilitated diffusion
basolateral side:
• GLUT2 transport for all three hexoses, facilitated diffusion
• Na pump maintains Na gradient
What are the requirements for Fat digestion and absorption?
- Enzymes: mainly pancreatic lipase but some gastric lipase
Other requirements for digestion in duodenal lumen
- Colipase
- Bile salts
- Right pH
1. Emulsification of fat in lumen (using bile salts)
2. Action of lipase to convert triglycerides (TGs) to monoglycerides (MGs) and fatty acids (FAs)
3. Formation of micelles (made of MGs, FAs, bile salts etc.)
4. Diffusion of micelles to epithelial cell brush border
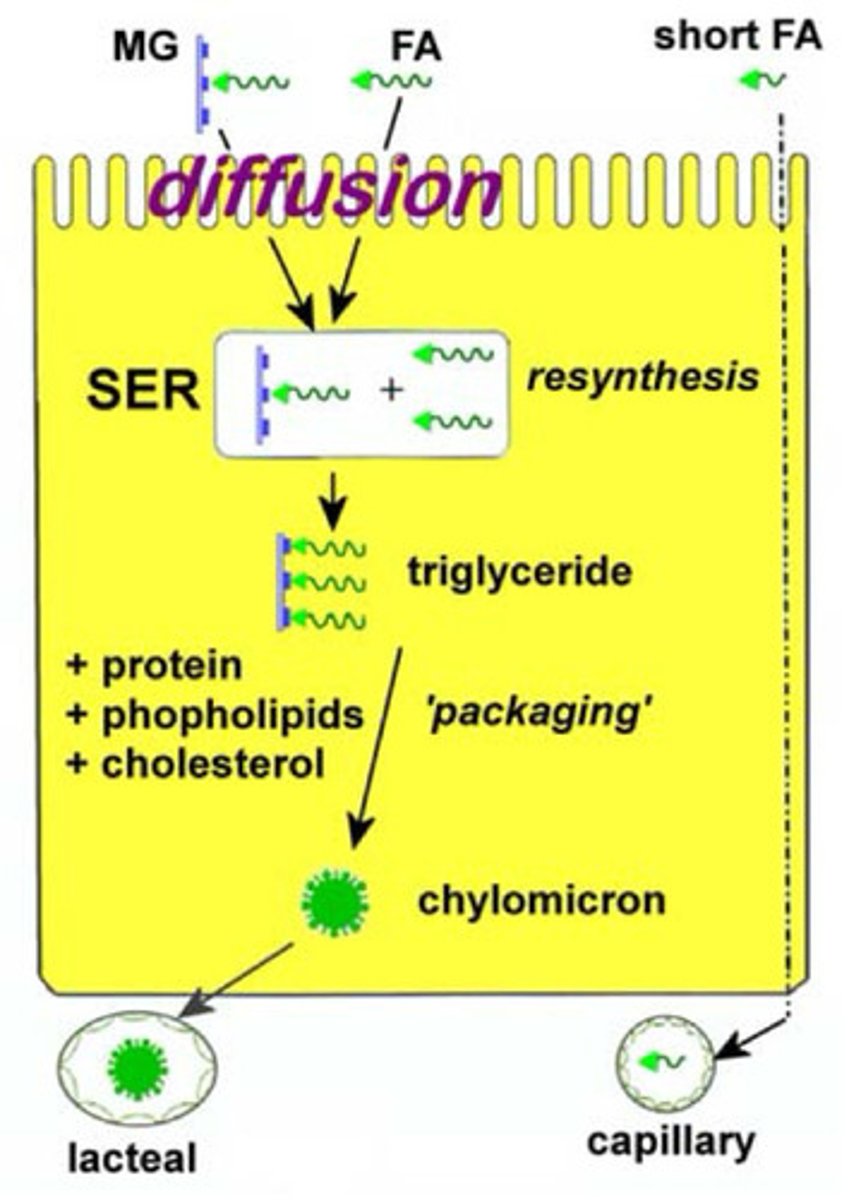
Fat absorption
Need beta-lipoprotein inside enterocyte to package lipid for export as chylomicrons
1. Trans-membrane transport of the free FAs and MGs (by diffusion through the lipid core)
2. Intracellular resynthesis of TG in SER Incorporation of the TG into chylomicrons, together with betalipoprotein, cholesterol, etc.
3. Efflux of chylomicrons on the basolateral side of the cell into nearby lacteals
NOTE
TGs: triglycerides
MGs: Monoglycerides
FA's Fatty acids
Describe the process of fat digestion
-Fats are not water soluble
Steps:
1. emulsification of fat in lumen -to increase the SA for enzymes to work properly (requires bile salts - turn the lipid droplets to a smaller size = increased SA)
2. action of lipase to convert triglycerides to Monoglycerides and Fatty Acids
3. formation of micelles (made of Monoglycerides, Fatty Acids, bile salts, etc)
4. diffusion of micelles to epithelial cell brush border - as they are fat soluble the micelles can just pass through the enterocytes membrane
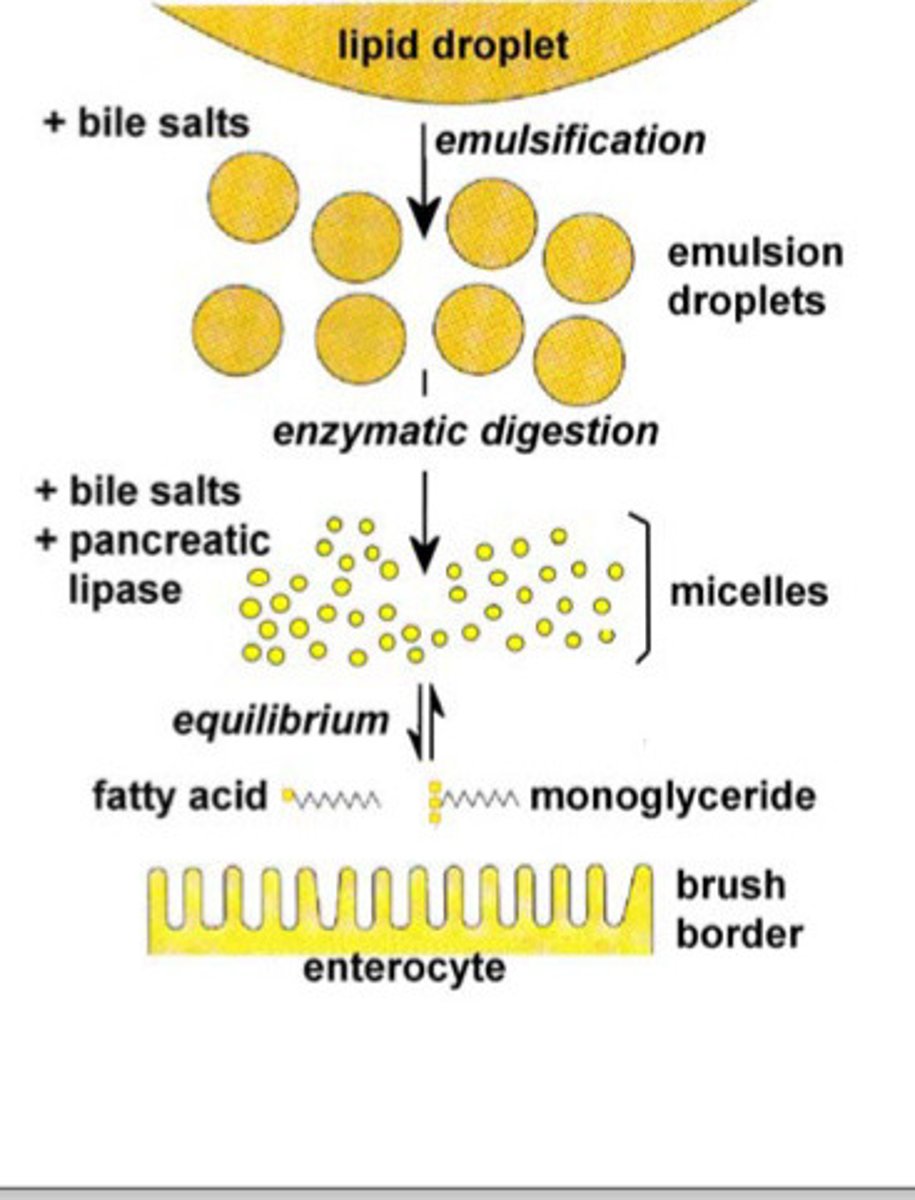
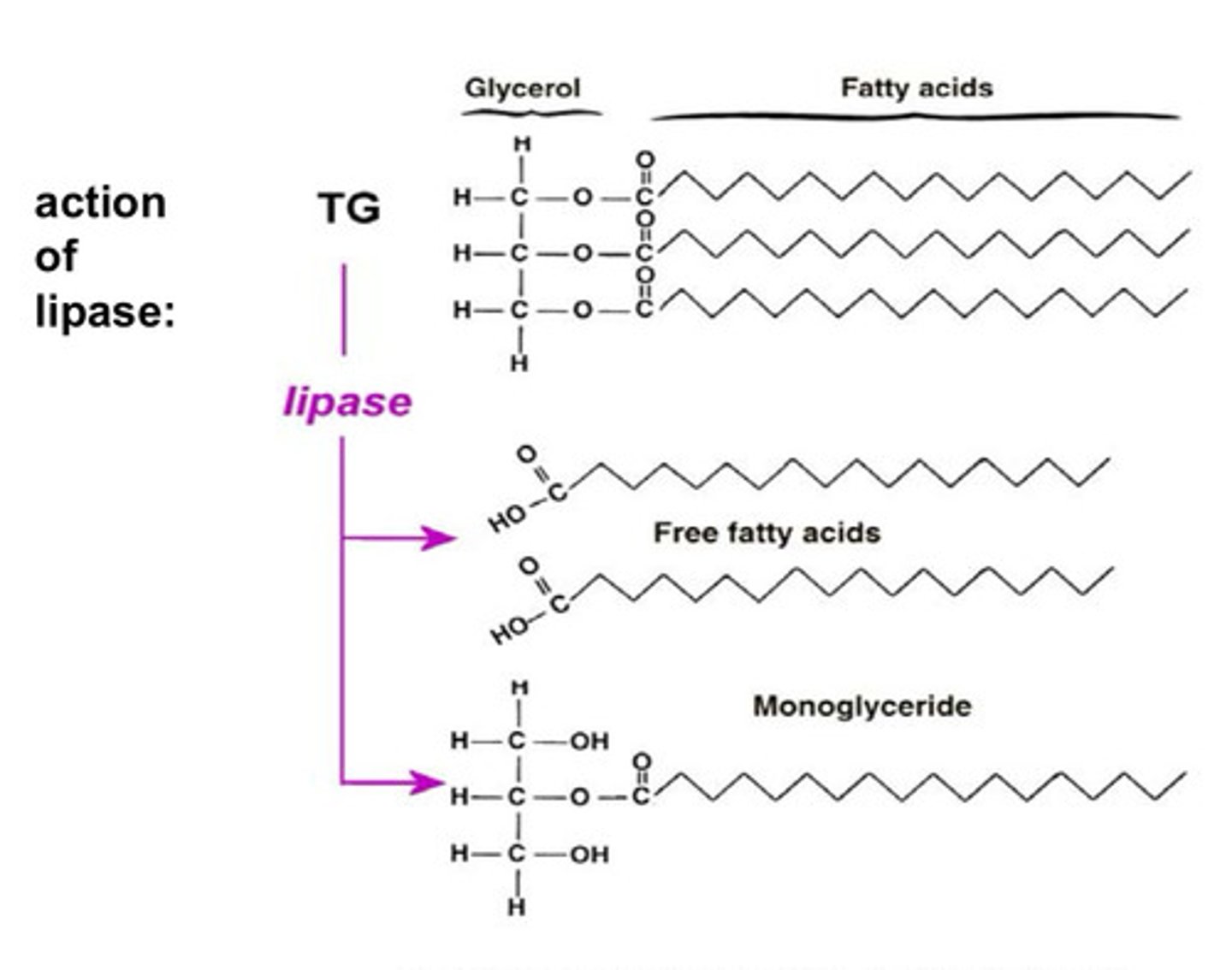
What does the action of lipase look like?
Lipase breaks down a triglyceride into 2 free fatty acid chains and one monoglyceride - these are absorbed
How are Fats absorbed?
the steps:
1. trans-membrane transport of the free FAs and MGs (by diffusion through the lipid core)
2. intracellular resynthesis of triglyceride (in the Sarcoendoplasmic Reticulum)
3. incorporation of the TG into chylomicrons, together with beta-lipoprotein, cholesterol, etc
4. efflux of the chylomicrons on the basolateral side of the cell, into nearby lacteals
What do we mean by Enterohepatic recirculation of bile salts?
-Produced in liver
-stored in gall bladder
-Enterohepatic circulation is the process by which substances like drugs, bilirubin, and biliary acids are circulated between the liver and the small intestine
- 95% bile salts reabsorbed, mainly in terminal ileum
• transported back to liver via portal vein, and re-extracted by hepatocytes to be re-exported in bile juice
• can be turned over 3-4 times during digestion of a single large meal
• overall loss of 5-10% per day in faeces compensated by new synthesis in liver
Why do we get net water absorption in the colon?
• net water absorption (following Na+ down osmotic gradient) - driven by Na-ATPASE pump - across luminal membrane of cell
-Due to osmotic potential of having high Na+ conc. on the basolateral side of the cell this causes Water to travel down the paracellular route as well as aquaporins that allow water to go across the cekk
• water and Na reabsorption stimulated by aldosterone
• resident microflora (bacteria in the colon) are prevented from crossing epithelial barrier, but they help to produce vit. K and folic acid which are absorbed here
Can humans digest cellulose?
No
due to: Lack of enzymes: Humans lack the enzymes needed to break down the beta acetal linkages in cellulose, which makes it difficult to digest.
Insoluble fiber: Cellulose is an insoluble fiber, meaning it doesn't dissolve in water.
Structure: Cellulose is a linear chain of glucose molecules that form dense microfibrils, which make it hard to break down
-it is used in the body as fibre which assists your digestive system
List some other absorptive functions of the GI tract
minerals
• specific mechanisms for absorption of mineral ions such as Ca2+, Fe2+ etc – see nutrition lectures
vitamins
• specific mechanisms for B & C vitamins – see nutrition lectures
• fat-soluble vitamins generally absorbed with lipids, in Small intestine
drugs
• absorbed best when non-ionised, both in the Small Intestine (right pH) and colon
• limited absorption of a few drugs (e.g. aspirin) across gastric mucosa
What are the 2 major causes of malabsorption and explain each ?
failure to digest macromolecules in chyme due to:
• interruption of the enterohepatic circulation of bile salts
• failure to deliver pancreatic enzymes e.g. cystic fibrosis patients
• poor co-ordination of gastric emptying with delivery of pancreatic & biliary secretions (too much chyme, don't neutralise the pH properly then trypsin won't work etc. = keeps more solutes in lumen which keeps water there = diarrhoea)
failure to absorb:
• failure to absorb lactose, because brush border lactase is absent, and lactose remains in lumen (alactasaemia)
• failure to absorb lipids because of lack of beta-lipoprotein required to make chylomicrons
• failure to absorb lipids because of failure of lipid digestion
• failure to absorb sufficient water because it is retained in lumen accompanying increased solute load
• failure to absorb sufficient water because of increased salt & water secretion caused by bacterial infection
• failure to absorb vit B12, folate & Fe2+ leading to anaemias .... see next slide
What are the major reasons for malabsorption leading to anaemia?
failure to absorb vit B12
• absorption in ileum (specific transporter recognises the vit B12 only when complexed with intrinsic factor - intrinsic factor and vit B12 make a complex for it to be absorbed, without this complex, Vit B12 will just go straight through you without being absorbed)
insufficient intrinsic factor results from:
• gastric atrophy,
• an autoimmune condition - patient mounts an immune response against his/her own intrinsic factor &/or the parietal cell
-result: disturbance in erythropoiesis, resulting in much fewer, but macrocytic rbc
failure to absorb iron
• absorption in Small Intestine, requiring specific transport mechanisms
• assisted by previous acid pH in stomach, which helps maintain the Fe3+ ions (iron ions must be converted from Fe2+ to Fe3+ to be absorbed) in a soluble state for later absorption
result: failure to make sufficient haemoglobin, resulting in microcytic rbc
What this looks like: you could spot this - pale gums due to anaemia, + changes to tongue surface & ‘glossitis’ (sore/burning’ tongue) in some cases
What are Types of Diarrhoea and why are they caused
Note: What is the outcome of diarrhoea - what else does it cause in the body
osmotic diarrhoea as a result of malabsorption:
• incomplete absorption leaves an increased solute load in the Small intestine lumen
• water stays with it (osmotic effect)
Outcome:
• much increased volume of lumenal contents, stimulating peristalsis
• undigested fats may also have a laxative effect
• many of the partially digested food stuffs are fermented in the Large Intestine (by local microflora), resulting in formation of gases (e.g. H2), distension (pain)
secretory diarrhoea in response to bacterial infection
• e.g. Vibrio cholerae and Escherichia coli toxins increase the secretory activity of intestinal crypt cells
diarrhoea secondary to intestinal mucosa damage
• e.g. coeliac disease (autoimmune condition mainly of Small Intestine caused by an adverse reaction to gluten)
• e.g. Crohn’s disease (inflammatory condition, mainly affecting ileum & colon)