Fungi and Mycobacteria
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
70 Terms
Rocky Mountain Spotted Fever (RMSF - report in 1 week)
A potentially fatal tick borne illness caused by Rickettsia rickettsii that affects both healthy and immunocompromised individuals (children 5-14 at higher risk)
American dog tick (D. variabilis), Rocky Mountain wood tick (D.andersoni), brown dog tick (R. sanguineus - arizona outbreaks) - requires a long attachment time, ticks maintain infection
Vectors for RMSF (no person-to-person)
Rickettsia rickettsii (intracellular gram neg incubates for 2-14 days) spreads via the bloodstream to vascular endothelium
Etiology for RMSF
Doxycycline 🥇, Chloramphenicol 🤰, fluids, O2, antipyretics, organ monitoring, hospitalization for extreme cases
A lumberjack from Arkansas presents to your office for flu like symptoms (fever, HA, malaise, and muscle aches). He also reports N/V and abd pain. On physical exam you note a blanching rash all other even the palms and soles. What is your treatment plan?

thrombocytopenia, hyponatremia, Mild transaminitis (ALT/AST), serology confirms but lags, PCR may work, immunohistochemistry confirms through skin biopsy
RMSF is a clinical diagnosis, but what might the labs look like?
confusion, seizures, ataxia, pneumonitis, myocarditis
Progressive and late stage symptoms for RMSF
multisystem organ failure
Complications of RMSF
avoid tick invested areas, use DEET or permethrin treated clothing, perform full body tick checks, prompt tick removal, control tick exposure in pets
RMSF prevention

mouth, vulvocaginal, intertriginous folds
Common sites for cutaneous candidiasis
erythema, satellite pustules, white scrapable plaques
Classic signs of cutaneous candidiasis
clinical + KOH prep
Diagnosis of cutaneous candidiasis
topical azoles, oral fluconazole
Treatment of cutaneous candidiasis
Invasive Candidiasis
A leading cause of bacteremia for hospitalized patients - especially those with hematologic malignancy, transplant, or uncontrolled DM
Central lines, ICU admission, TPN, neutropenia, recent surgery
RIsk factors for Invasive Candidiasis
Fever
What is often the only early symptom of Invasive Candidiasis?
blood cultures, Beta-D-glucan, ophthalmologic exam (endophthalmitis), imaging to r/o abscesses or organ involvement, call ID
Workup for Invasive Candidiasis
echinocandin → fluconazole (if susceptible, 14 days after 1st negative blood culture), remove central line
Treatment plan for Invasive Candidiasis
Histoplasmosis (not reportable)
An infection endemic to the Ohio/Mississippi river valleys that can cause severe diseases in immunocompromised patients (CD4 under 150)
immunosuppression, construction, farming, cave exposure, old buildings, bird/bat enriched soil
Risk factors for Histoplasmosis
Histoplasma capsulatum (dimorphic fungi - converts to yeast in lungs and spreads through lymphatics to spleen, liver, bone, or CNS); no person-to-person
Etiology and transmission of Histoplasmosis
dry cough, fever, chest pain, malaise, hilar/mediastinal lymphadenopathy
Acute pulmonary symptoms for Histoplasmosis
Cavitary disease, weight loss, hemoptysis (LOOKS LIKE TB)
Chronic pulmonary symptoms for Histoplasmosis
fever, weight loss, hepatosplenomegaly
Progressive disseminated Histoplasmosis (PDH) symptoms
Ulcers, bleeding, diarrhea, meningitis, mass lesion, cutaneous lesions, visual symptoms (POHS)
Other symptoms for histoplasmosis
urine and serum antigen testing, blood cultures (PDH), tissue biopsy with silver stain (definitive), H and M bands (antibody), bone marrow/liver biopsy inadvanced disease, CXR/CT (cavitary or millet seed), CSF (for CNS symptoms)
Diagnostic for histoplasmosis
itraconazole or observation
Management for mild to moderate histoplasmosis
liposomal amp B → itraconazole for up to 12 months (CNS); corticosteroids for mediastinal lymphadenitis or pericarditis
Management for moderate to severe histoplasmosis or PDH
pulmonary fibrosis, disseminated infection to liver, spleen, CNS, or GI tract, bone marrow suppression, pancytopenia, visual impairment, meningitis, mass lesions, mediastinal fibrosis
Complications for histoplasmosis
Avoid soil or dust exposures, use respiratory protection, educate high risk patients, itraconazole prophylaxis if CD4s under 150, screen transplant and TNF inhibitor patients
Prevention of Histoplasmosis
Pneumocystis Jirovecii (PCP - not reportable)
A life-threatening ubiquitous fungal infection that is historically associated with AIDS but is now more common in non-HIV patients
CD4 under 200, TNF inhibitors, chronic glucocorticoids, rituximab, solid organ/stem cell transplant
Risk factors for Pneumocystis Jirovecii
over 60, mechanical ventilation, high LDH
What increases mortality in Pneumocystis Jirovecii
Pneumocystis jirovecii that lives in the alveoli causing foamy exudate and impaired gas exchange; transmitted via airborne route (no person to person)
Etiology and transmission for Pneumocystis Jirovecii
Subacute onset of nonproductive cough, dyspnea (dry rales), and fever, tachypnea, hypoxia especially with exertion, spontaneous pneumo
Signs and Symptoms of Pneumocystis Jirovecii
TMP-SMX (🥇 - atovaquone, dapsone, clindamycin/primaquine, pentamidine) , Corticosteroids (Aa above 35, PaO2 under 70), Check ART regimen, monitor drug toxicities, consider ID
45 y/o male presents to the clinic for cough and fever. His past medical hx is positive for HIV. Chest x-ray has a batwing pattern, ABG reveals a widened A-a gradient of 45. There’s an elevated LDH and 1,3 B-D glucan and BAL with silver stain is positive. What is your treatment plan?
BAL with silver stain or PCR 🏆
Gold standard for Pneumocystis Jirovecii
Acute respiratory failure needing ventilation, pneumothorax, drug reactions (rash, neutropenia, AKI, hyperkalemia), IRIS after ART initiation, superimposed bacterial/fungal, chronic dyspnea or fibrotic lung, DEATH
Complications for Pneumocystis Jirovecii
HIV with CD4 under 200 or 14%, transplant, cancer, or prolonged steroid use
Who’s getting prophylaxis for Pneumocystis Jirovecii (under 3+ months on art or CD4s over 200)
MAC (avium + intracellulare), M. Kansasii 🫁 , M.Marinum, M,abscessus
Most common atypical mycobacterial diseases in the USA
Structural lung disease (bronchiectasis, COPD), older age, low BMI
Risk factors for MAC and M.kansasii pulmonary NTM
Chronic cough, sputum, weight loss, fatigue
Symptoms of pulmonary NTM
tall, thin elderly women (lady windermere syndrome)
MAC is common in who?
positive culture from 2+ sputum samples or 1 bronchial wash + symptoms/imaging; imaging looks similar to TB
Diagnosis for pulmonary NTM
macrolide-based triple therapy (azithromycin, rifampin, ethambutol) for 12+ months after culture conversion
Treatment for pulmonary NTM
M. Marinum
Linked to fish tanks, aquariums, and swimming pools that presents as chronic skin nodule or ulcer after trauma/exposure

M. Abscessus
A rapidly growing species that causes post-traumatic or surgical wound infections that is commonly transmitted in cosmetic procedures
biopsy or aspirates with acid-fast stain and culture
Diagnosis of NTM SSTIs
Macrolides + others (based on susceptibility) for 4-6 months or more
Treatment of NTM SSTIs
Disseminated NTM
Most common in patients with CD4 under 50 that presents with fever, night sweats, weight loss, diarrhea, and anemia often involving liver, spleen, bone marrow, and lymph nodes
azithromycin/clarithromycin + ethambutol + rifabutin → lifelong suppression may be needed
Treatment for Disseminated NTM
Leprosy (Hansen’s Disease)
A mycobacterium disorder that affects the skin, peripheral nerves, eyes, and mucosa that is endemic in parts of Texas, Louisiana, Florida (think Armadillos)
Clinical + biopsy showing acid-fast bacilli
A 23 y/o Texas cowboy presents to the clinic for muscle weakness and sensory changes. He states that he wrangles 9-banded armadillos in his spare time. On physical exam you note a hypopigmented, patch like rash. What are your diagnostic technqiues?

Rifampin + dapsone + clofazimine (6-12 months)
A 23 y/o Texas cowboy presents to the clinic for muscle weakness and sensory changes. He states that he wrangles 9-banded armadillos in his spare time. On physical exam you note a hypopigmented, patch like rash. Your culture comes back with mycobacterium leprae, what is your treatment plan?

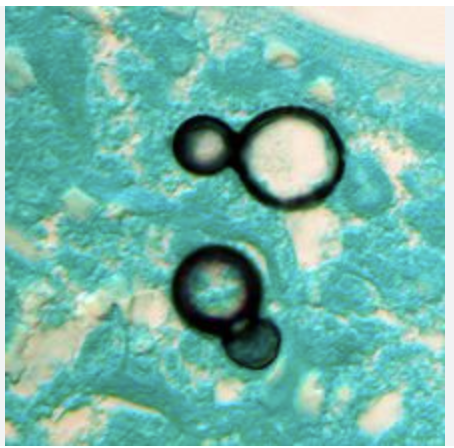
Cryptococcus neoformans (bird droppings), C. gattii (eucalyptus trees)
Etiology for Cryptococcosis
antigen testing (serum/CSF), Halo on India Ink stain, fungal culture
Diagnosis for Cryptococcosis

Amp B + flucytosine → fluconazole
Treatment for Cryptococcosis IF BRAIN
HA, fever, neck stiffness (meningitis)
Presentations for Cryptococcosis
Blastomycosis
A condition caused by Blastomyces dermatitidis (dimorphic fungus) that is found in moist soil and decaying organic material especially in Ohio/mississippi river valleys and the Great lakes
Verrucous/ulcerative skin lesions, pulmonary infection resembles TB or bacterial pneumonia, can disseminate to skin, bone, GU tract
Presentation for Blastomycosis
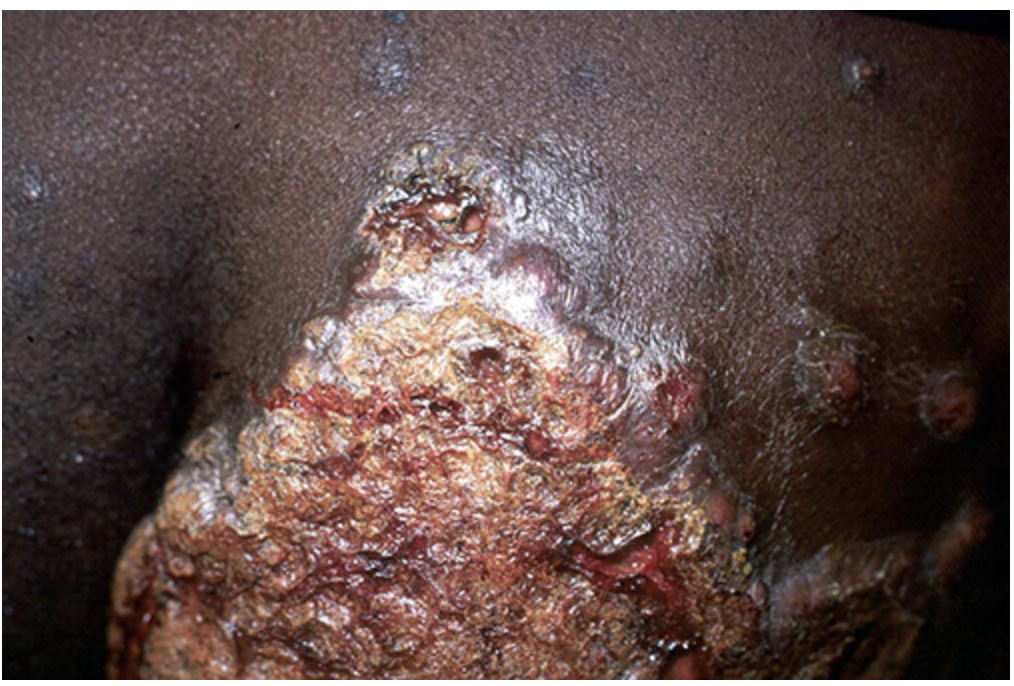
Culture, histopathology with broad-based budding yeast
Diagnosis for Blastomycosis
Itraconazole for mild/moderate, Amp B for severe/dissemination
Treatment for Blastomycosis
Coccidioides immitis, C. posadasii (endemic to the Southwest US)
Valley fever (Coccidioidomycosis) is caused by
Cough, fever, chest pain (can disseminate to skin, bones, or CNS (especially in immunosuppressed, Filipinos, African Americans, pregnant))
Presentation of Valley Fever
serology, culture, spherules on histopathology
Diagnosis of Valley fever
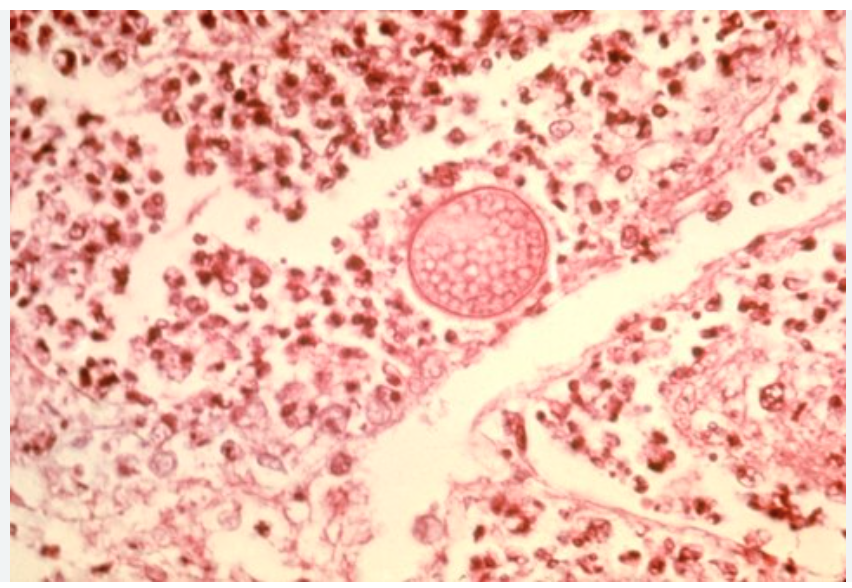
Fluconazole/itraconazole for moderate, Amp B for severe
Treatment of Valley fever
Pott Disease
TB in the skeleton (particular the vertebrae) that causes back pain and deformity

Cutaneous TB
A TB infection of the skin that leads to scrofuloderma, lupus vulgaris (chronic nodules and ulcer)
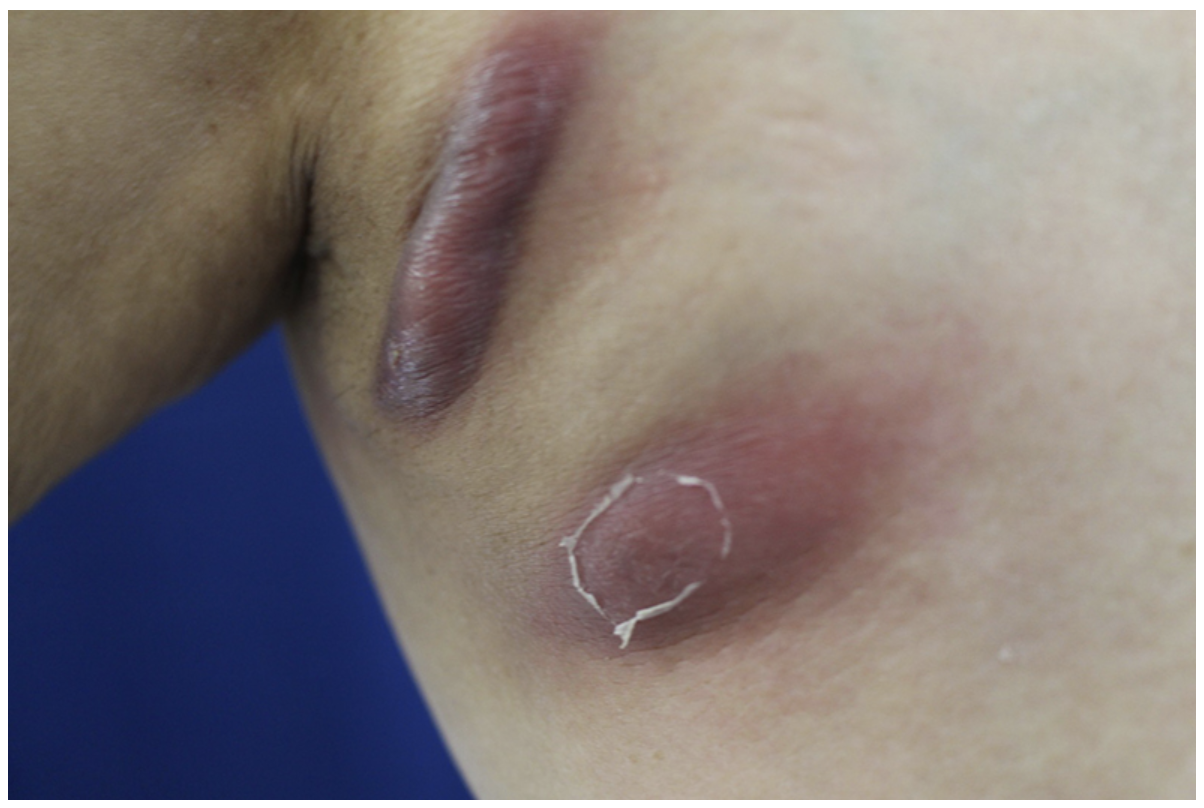
immunosuppression, endemic exposure, prior TB
Risk factors for extrapulmonary TB
biopsy + AFB stain/culture, PCR, imaging (CXR, MRI, CT)
Diagnosis of extrapulmonary TB
RIPE with public health notification and DOT, HIV testing is recommended
Treatment of extrapulmonary TB