Simmons 501 Week 6 Exam 2 Prep MASTERY GUIDE: Health Assessment, Clinical Diagnostics & Expert-Verified Q&A + Diagrams & rationales (NCLEX-Aligned | GUARANTEED SUCCESS
1/156
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
157 Terms
Ovaries
paired organs that flank the uterus and are composed of an outer cortex and an inner medulla
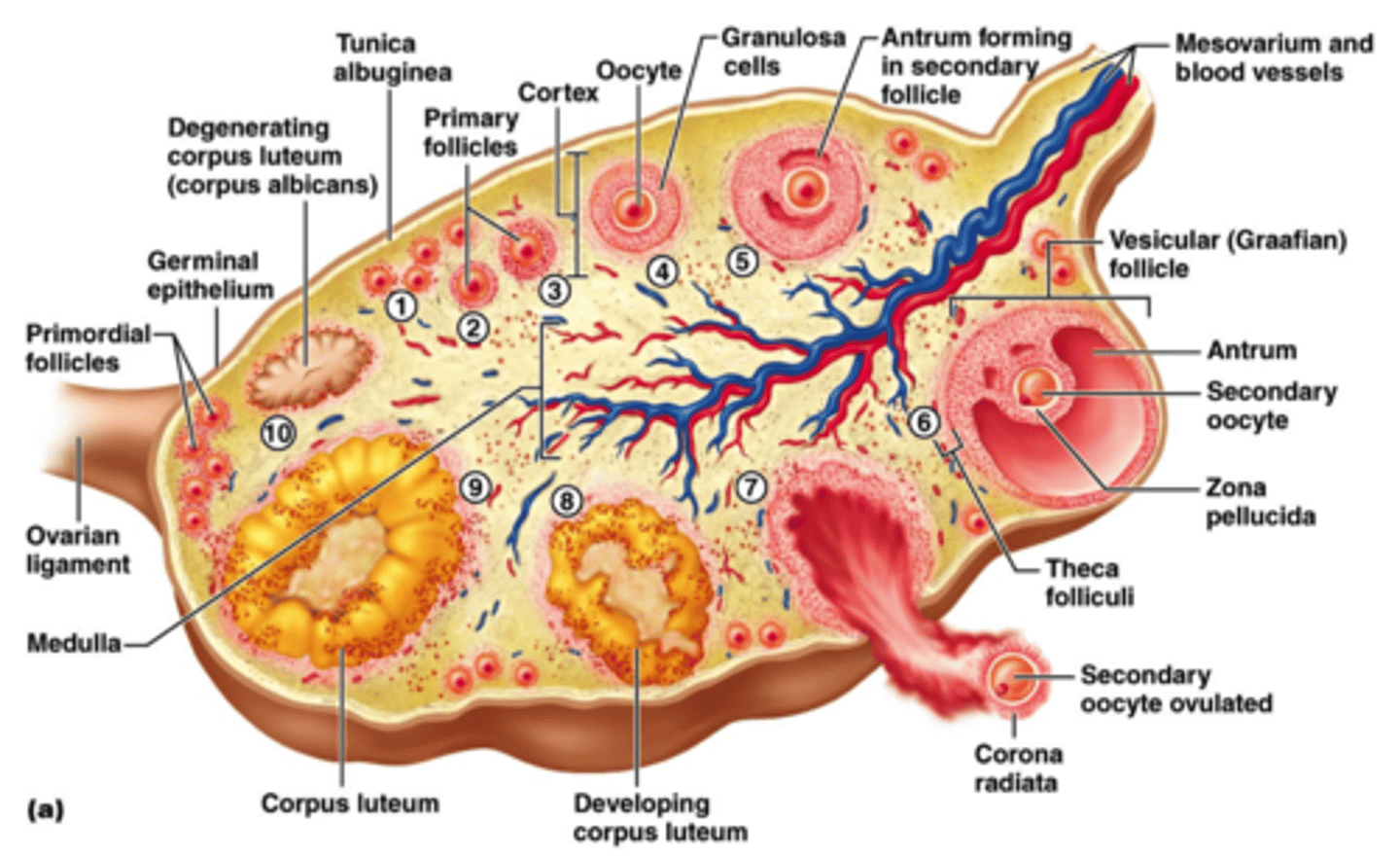
Cortex
highly vascular connective tissue that contains ovarian follicles
Follicles
oocyte (immature egg) surrounded by granulosa cells
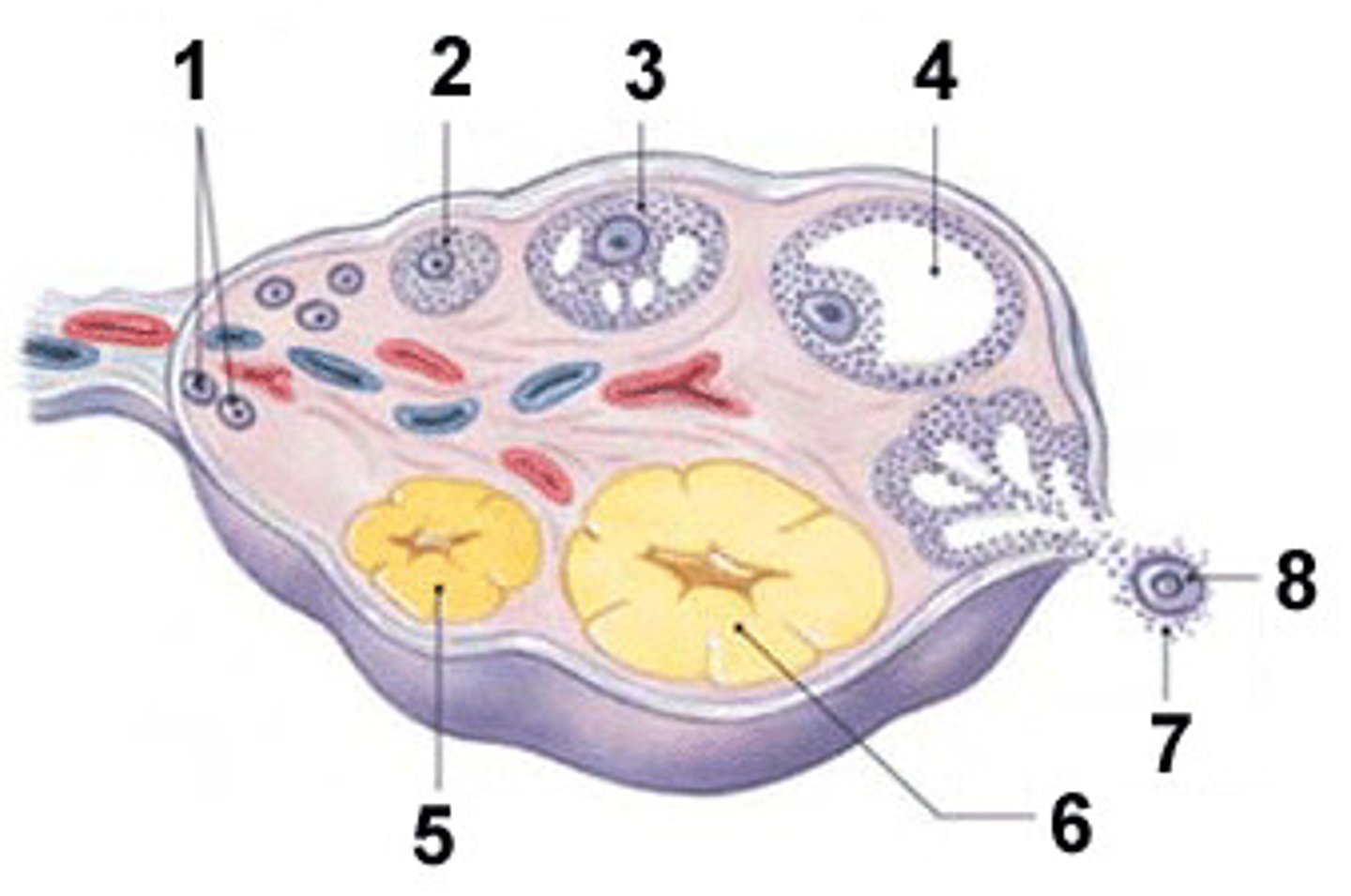
Antrum
the fluid-filled cavity in the center of the follicle that forms as granulosa cells proliferate

Graafian follicle
the mature follicle that ruptures once a month (ovulation)

Ovulation
ejection of oocyte and formation of corpus luteum from follicle remnants
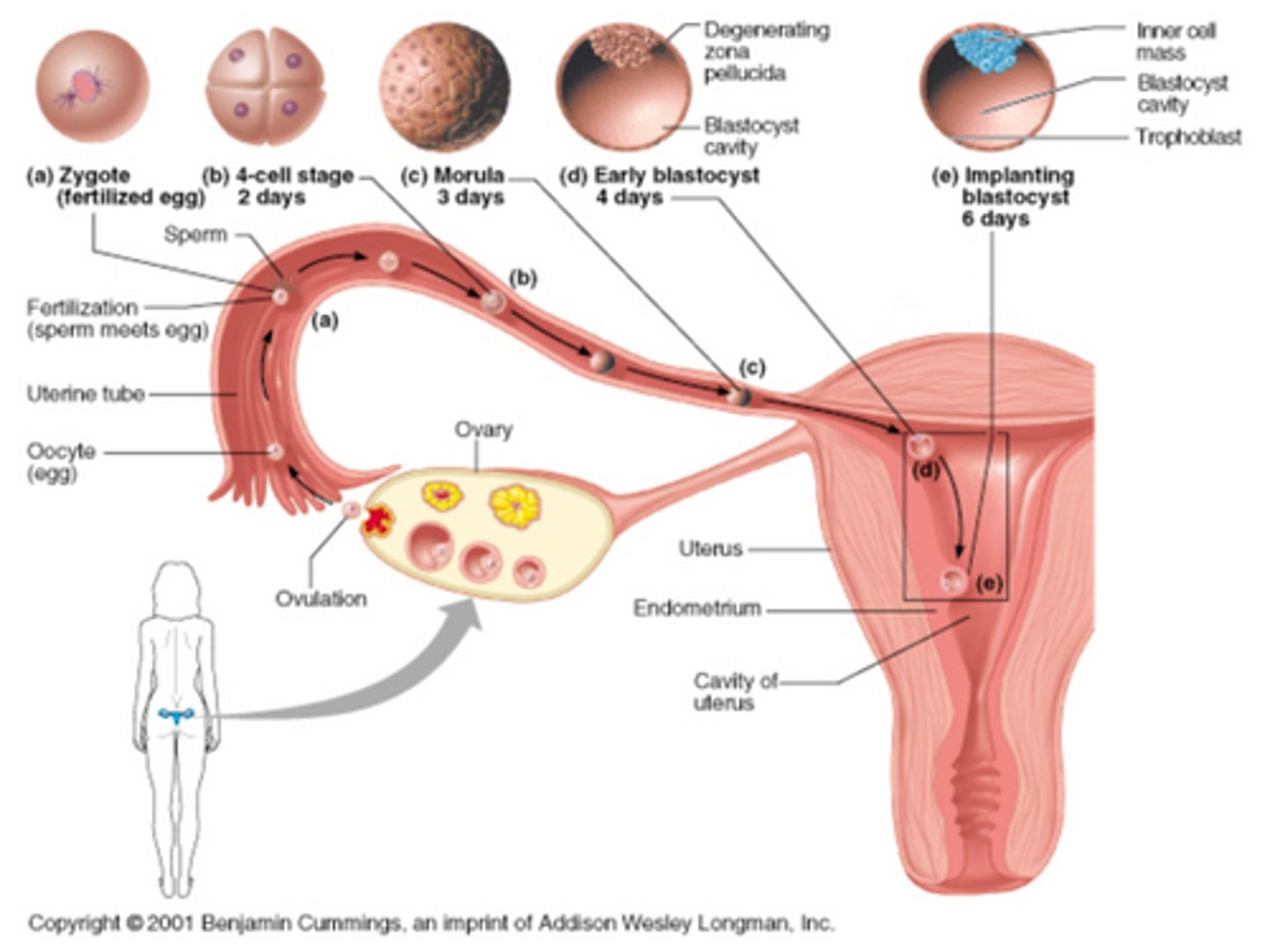
Uterine tubes
(fallopian tubes and oviducts) receive ovulated oocyte
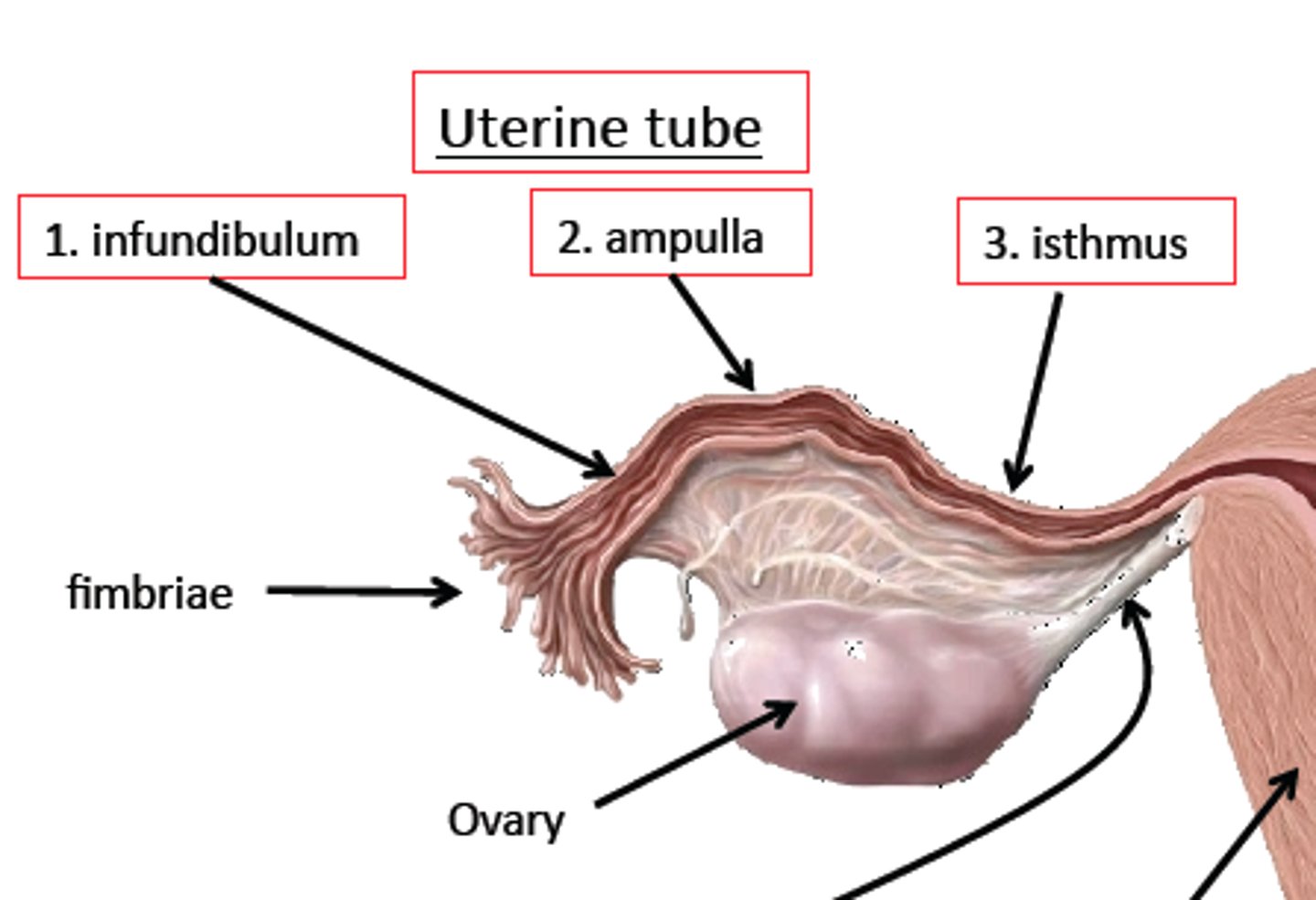
Oocyte's path in uterine tubes
Swept into the uterine tube by fimbriae - Curves around ovary and ampulla (usual site of fertilization) - Empties into uterus via isthmus (narrow region just before the uterus)
Uterus
Located in pelvis anterior to the rectum and posterosuperior to the bladder; consists of fundus - body—isthmus—cervix - Internal os - cervical canal—external os—vagina - Cervical glands - (cervical canal) secrete mucus
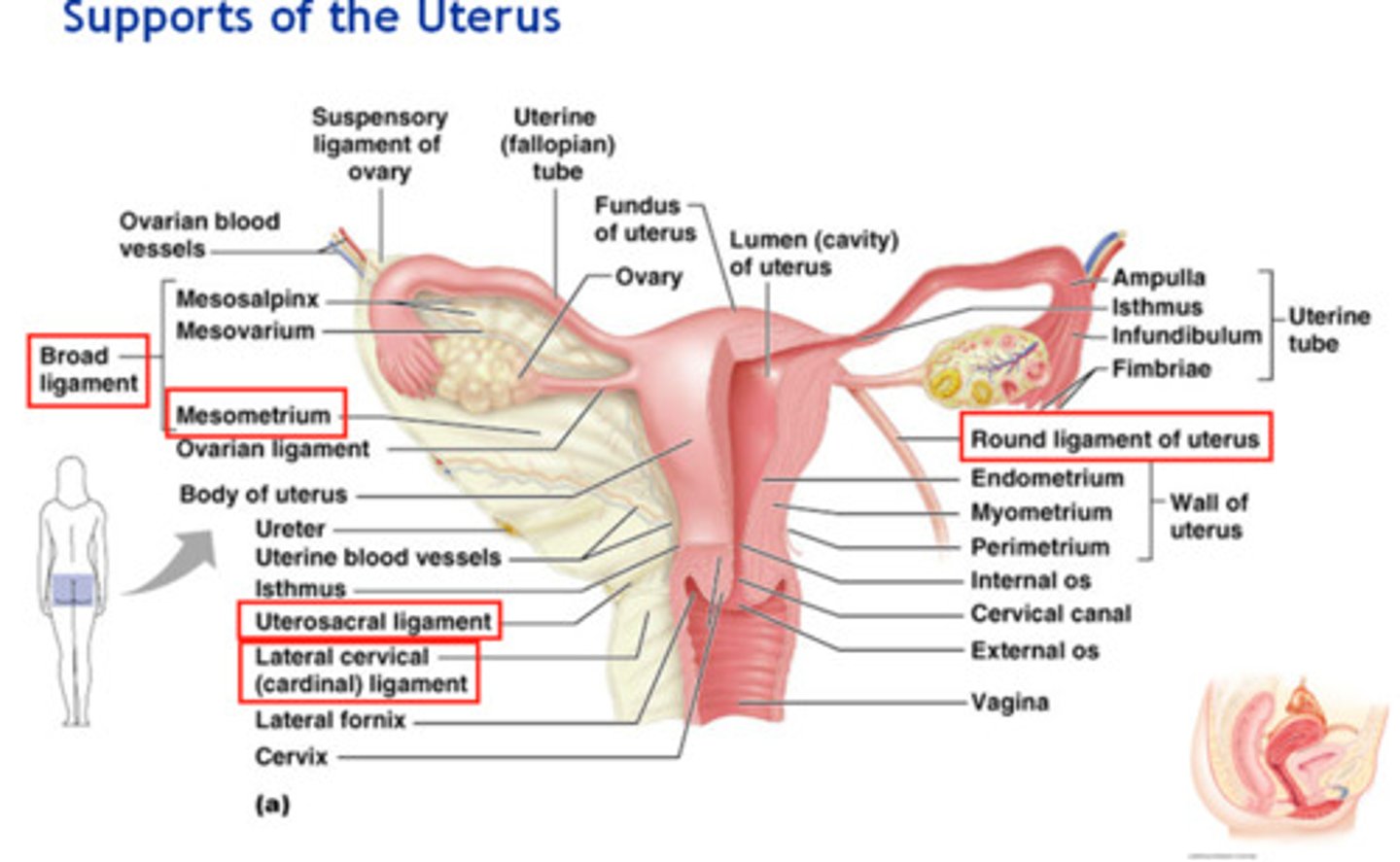
Uterine Wall
contains the perimetrium, myometrium, endometrium, stratum functionalis, stratum basilis uterine glands
Perimetrium:
outermost serous layer
Myometrium:
smooth muscle layer
Endometrium:
mucosal lining of uterine cavity
Stratum functionalis:
functional layer of endometrium
Stratum basilis:
basal layer of endometrium
Uterine glands:
located in endometrium, uterine arteries, and veins (sinusoids)
Vagina
Consists of thin-walled tube between bladder and rectum that extends from cervix to exterior of body; Embedded in anterior wall is urethra; Acts as birth canal, passageway for menstrual flow and delivery of infant; Contains adventitia, muscularis, mucosa (rugae); Contains dendritic cells
External Genetalia
consists of vulva, mons pubis, labia, clitoris, vestibule structures; Note: Female urinary and reproductive tracts are separate.
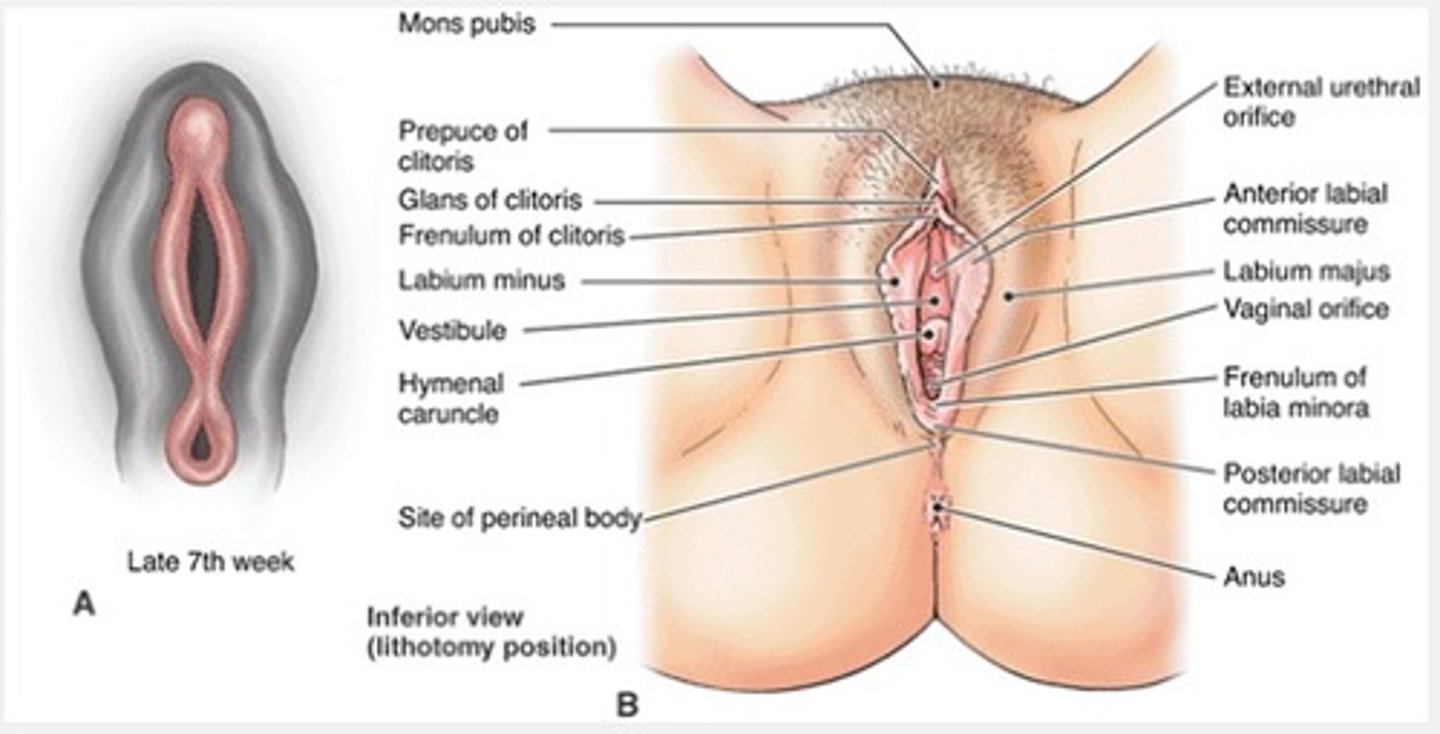
Vulva:
mons pubis, labia, clitoris, and vestibule structures
Mons pubis:
fatty, rounded area overlying pubic symphysis
Labia majora:
female counterpart to scrotum
Labia minora:
female counterpart to ventral penis that enclose vestibule
Greater vestibular glands:
female counterpart to bulbourethral glands, flank vaginal opening
Clitoris:
female counterpart to penis composed of erectile tissue anterior to vestibule, richly innervated with sensory nerves, contains corpora cavernosa but lacks corpus spongiosum
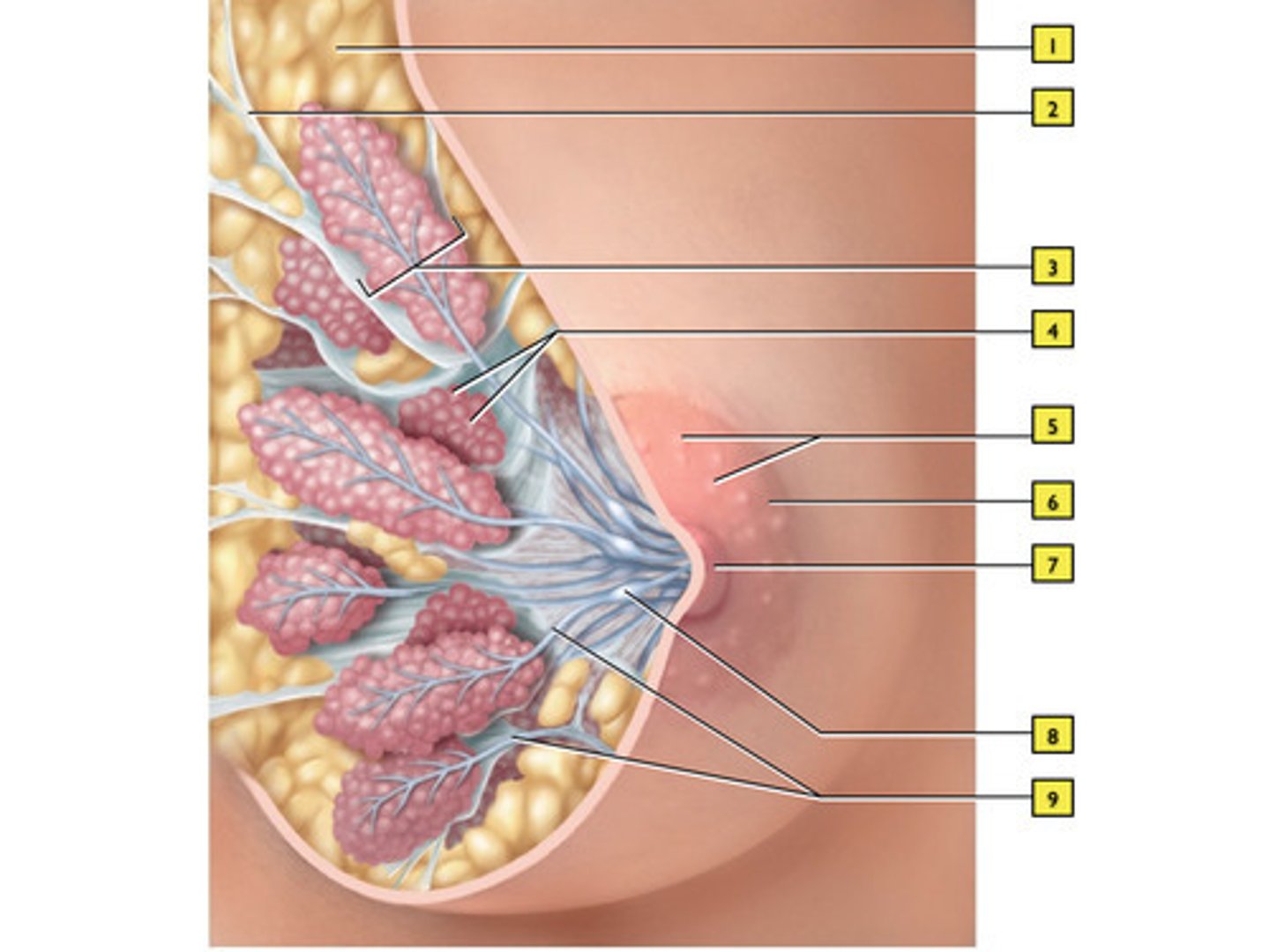
mammary glands
Present in both male and female, but functional only in female; Produce milk to nourish newborn baby; Contain lobes that are subdivided into lobules containing glandular alveoli; Milk released during lactation from alveoli into lactiferous ducts (sinuses) that open to outside at the nipple
Embryonic overview
Embryology depends on genetic and environmental factors; organism of billions of cells arises from a simple zygote (two cells together); Development occurs cephalocaudal (head to toe); involves growth, differentiation, organization; Preembryonic development occurs from zygote to week 2; Involves cleavage reactions
Preembryonic development
Blastocyst divides, forming inner group of cells with outer shell; Inner group of cells becomes embryo; Outer group of cells becomes membrane and placenta; Implantation of blastocyst occurs around day 6.
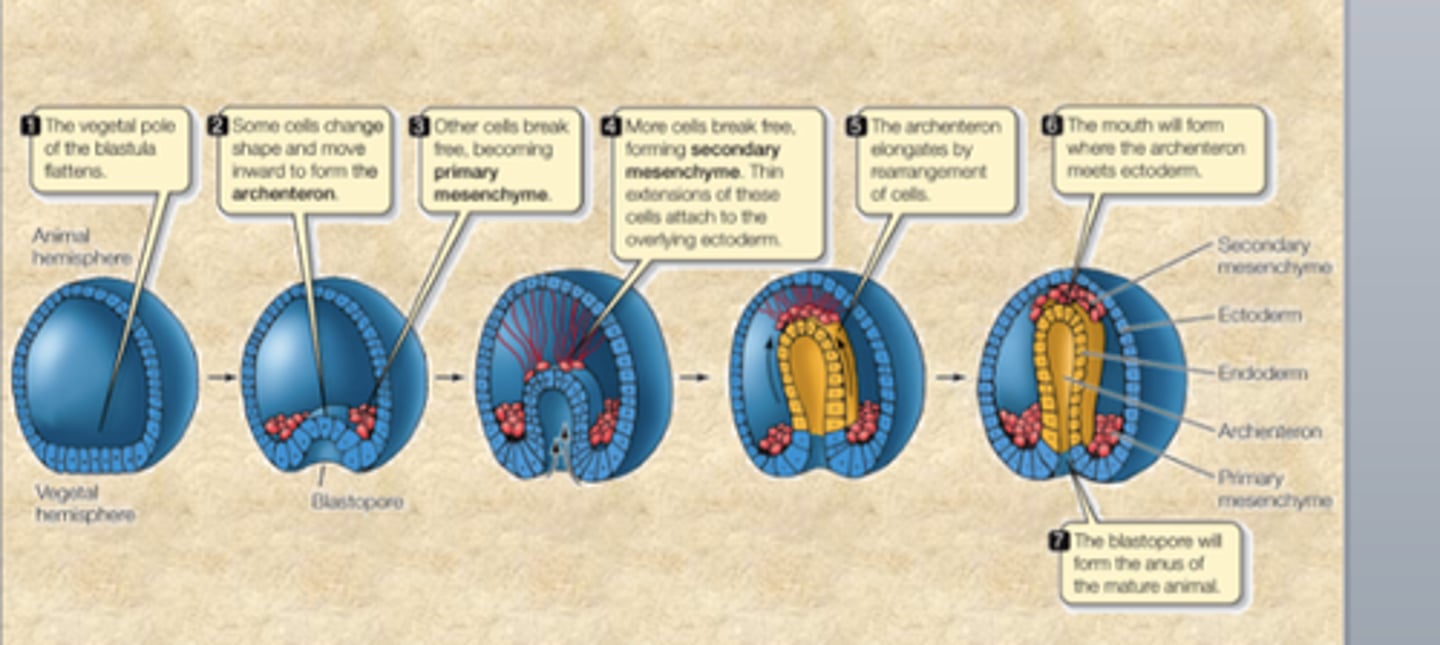
Embryonic Development
Blastocyst convers to gastrula. Blastocyst contains outer trophoblast and inner cell mass. Gastrulation occurs.
Gastrulation:
formation of three primary germ layers and development of embryonic membranes.
• Formation of primary germ layers
• Early phase in embryonic
development
• Single-layer blastula reorganized into
trilaminar (three-layer) structure
• Structures organized into sheets by
connected cells (mesenchyme)
• Primitive streak: structure that will
establish bilateral symmetry in embryo
Embryonic Membranes
Divided at first and fuse later in pregnancy - amnion, yolk sac, allantois, chorion
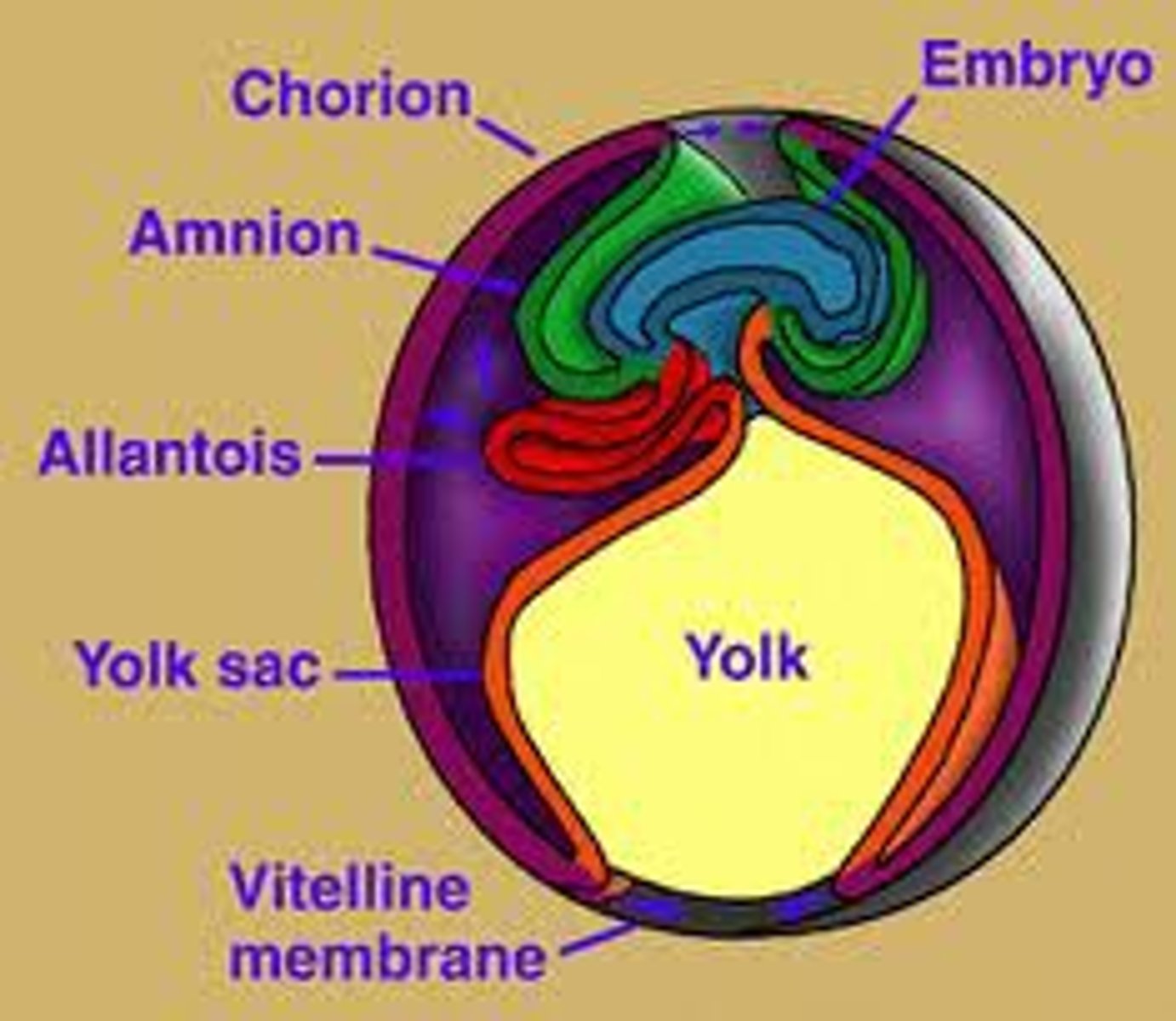
Amnion:
transparent membranous sac that fills with amniotic fluid
Yolk sac:
comes from hypoblast, forms digestive tube, produces blood cells and vessels and gonads (primordial germ cells)
Allantois:
outpocket of caudal end of yolk sac, forms umbilical cord and urinary bladder
Chorion:
helps form placenta, encloses embryo and other membranes
Fertilization:
capacitation of sperm, acrosomal reaction, block to polyspermy, meiosis II, formation of zygote
Preembryonic development:
cleavage reactions, formation of blastocyst, implantation
Embryonic development:
formation of embryonic membranes, gastrulation (formation of endoderm, mesoderm, ectoderm), organogenesis
Fetal development:
development of systemic structures
Implantation I
Blastocyst reaches uterus on day 6 of cycle
Implantation II
Trophoblast adheres to endometrium. Trophoblast releases digestive enzymes
Implantation III
Trophoblast forms two layers: Cytotrophoblast: inner layer, maintains cell boundary and Syncytiotrophoblast: outer layer, invades endometrium
Implantation IV
Human chorionic gonadotropin (hCG) is secreted by trophoblast, maintains corpus luteum.
Teratogenesis
Any substance, organism, physical agent, or deficiency state present during gestation which is capable of inducing abnormal postnatal structures or function (biochemical, physiological, or behavioral) by interfering with normal embryonic and fetal development
Depends on:
Genotype of embryo and how agent interacts with that genetic environment
Timing of exposure and the developmental stage of the embryo
Specific cells or tissues agent acts on to cause pathogenesis
Access to embryo (determined by nature of agent)
Dosage (manifestations of deviant development increase with increasing dosage)
Final manifestations may be death, malformation, growth retardation, and functional disorders
Placentation
development of chorion, chorionic villi, endometrium, decidual capsularis and ultimately the placenta; Chorion develops from trophoblast; Chorionic villi form and extend into maternal blood.; erosion produces blood-filled lacunae in the functional layer of endometrium; Decidua basalis forms between chorionic villi and basal layer of endometrium.; Decidua capsularis surrounds all; Placenta forms between chorionic villi and decidua basalis.
Placenta
Formed and functional by third month, Does not allow mixing of maternal and embryonic blood, Secretes progesterone, estrogens, human placental lactogen, human chorionic thyrotropin and relaxin, maintains hormones for duration of pregnancy, Delivered after the infant
Trisomy 21
One of the most common genetic disorders encountered in pregnancy Prevalence is 1:629 births Significant burden of disease
Diagnostic testing readily available
safe options for pregnancy termination Associations and groups offering planning and support
Most common chromosomal abnormality among live births
Three chromosomes on chromosome 21 Characteristics: Moderate to severe intellectual disability; IQ of approximately 40, Short stature, Distinct facial features, Heart defects, Vision and hearing problems, Infections risks
appraoch to counseling about prenatal testing and genetic screening
Explain difference between screening test and diagnostic test:
Screening test shows potential problem; the diagnostic test is diagnosis.
Explain sensitivity and specificity of both screening and diagnostic testing.
Describe various screening tests.
Give options of diagnostic testing.
Explain risks associated with diagnostic testing.
Ensure patient understands timing and limitations of tests offered.
Consider the psychological implications of testing:
Patient must think about what she will do with the results before undergoing test.
Explain syndrome and implications.
Explain detection rates of other chromosomal abnormalities.
Tell patient length of time it will take for results come in.
Be ready to give information about pregnancy termination.
Candidates for Diagnostic Testing
•Previous pregnancy affected by trisomy
•At least two minor structural anomalies in the current pregnancy. Discovered in full fetal ultrasound
•Chromosomal translocation, inversion, or aneuploidy in patient or her partner
Noninvasive Screening Tests
•Use maternal serum marker levels interpreted with age-related risk
•May involve ultrasonographic measurements
•Allow patients to make further choices about diagnostic testing
•More markers make the test more accurate
First trimester combined test
•First-trimester nuchal translucency.
Measurement of back of baby's neck
•Gestational age by crown-rump length
•Serum markers associated with pregnancy.
Pregnancy-associated plasma protein (PAPP-A) and free or total beta-HCG
•Best for privacy and early diagnosis as it is done at 11 to 13 weeks
•In second trimester, patient will need different test for neural tube defects
Full Integrated tests
Entails first trimester combined test with alpha fetoprotein, estriol, hCG, and inhibin A
Obtained at 15 to 18 weeks
Is most accurate test with lowest screen-positive rate
Serum integrated test
Same as full integrated test but without nuchal translucency
Option for clients without access to nuchal translucency measurements
Disadvantage of integrated test
must wait until second trimester for results
Sequential screening
•First-trimester risk assessment
•CVS for clients with a risk greater than 1:50
•If screen shows patient is not at high risk, she will next be tested in second trimester
Three risk cut-offs (contingent testing)
•Immediate diagnostic testing for those at high risk (greater than 1:50)
•No further testing for those at low risk (less than 1:2000)
•Second-trimester screening for those at intermediate risk (more than 1:50 but less than 1:2000)
Alpha-fetoprotein
•Produced in fetal yolk sack in first trimester and later picked up by fetal liver
•Found in maternal serum and amniotic fluid
•Abnormally high levels are associated with fetal disorders, particularly open defect
Alpha-fetoprotein (MsAFP) Testing
•Offered in second trimester as part of the quadruple test or following ERA
•Positive test is not diagnostic; ultrasound is also needed
•99% detection in conjunction with ultrasound
•Detection of open defects:
Omphalocele at 89%
Gastroschisis at 100%
Fetal congenital nephrosis, teratomas, and
cystic hygromas
Quadruple Test
•Best available screening test for those that initiate prenatal care in second trimester
•Measures MsAFP, uE2, and inhibin A
•Can be done up to 22 weeks in most labs
Cell Free Fetal DNA Analysis
This test is also known as noninvasive prenatal testing or by brand names such as Panorama or Harmony:
• Genomic sequencing to detect trisomy 21, 13, and 18 after 10 week's gestation
• ACOG recommends this for the following:
o Maternal age over 35
o Sonographic findings associated with aneuploidy
o History of previous pregnancy with trisomy
o Parental translocation
• 99% accuracy
• Highly sensitive and specific
• Not diagnostic
• If test is positive, further testing is required
• Women with a family history of other chromosomal abnormalities or fetal structural anomalies should be offered diagnostic testing
Management of test results
• Results should be presented as risk assessment and not as positive or negative.
• Number should be presented along with visuals.
Screen Positive Testing meaning
• Risk of having a baby with Down's syndrome is above the marker level.
• Age-related risk must be taken into consideration.
• Ultrasound rules out other reasons for positive test result.
o For example, fetal anomalies or multiple gestation
• Repeat testing is not advisable.
• For diagnostic testing, offer CVS in first trimester and amniocentesis in second trimester.
Early Amniocentesis
• Done at 11 to 14 weeks of gestation
• Same technique as second trimester amniocentesis
Benefits:
• Early diagnosis of fetal disease or abnormalities
• Decreased rates of mosaicism compared to CVS
• Better chromosomal quality
Limitations:
• Greater expertise required
• Increased tenting and risk of ruptured membranes
• Multiple insertions may be necessary
• Delay in test results because cells have to grow
Early Amniocebntesis Complications
• Higher risks than in second trimester
o Fetal loss from membrane rupture: 7.6% vs. 5.6%
o Club feet: 1.3% vs. 0.1%
• Higher risk of fetal loss than CVS: 4.9% vs. 2.1%
• Membrane rupture/fetal demise: 12% to 40%
• Vaginal bleeding and fetal loss: 20%
• Neonatal respiratory problems and congenital anomalies depend on amount of fluid loss
Chorionic Villi Sampling (CVS)
• Small amounts of placenta obtained for DNA analysis
• Early diagnosis of chromosomal disorders, using larger amounts of DNA
Preprocedure:
• Cervical cultures:
o GC, chlamydia, GBS, and MCV
o Treat accordingly
o Also test for BV
• Ultrasound to rule out multiple gestation:
o Eliminates risk of sampling one baby and not the other
CVS Techniques
Transcervical:
• Contraindications:
o Vaginismus
o Cervical stenosis
o Cervical or lower uterine segment myomas
o Cervical infection
o Extreme uterine retroversion or anteversion
Transabdominal:
• Contraindications:
o Extreme uterine retroflexion
o Fetal position
• Relative contraindications:
o IUD
o Isoimmunization
CVS Complications
• Fetal loss:
o Greater chance with transcervical than with transabdominal
o Perinatal mortality same as amniocentesis
o Greatest loss predictors:
Small for gestational age (SGA)
Operator risk
• Limb reduction:
o Transverse limb abnormalities more common when done before 9 weeks
• Bleeding:
o Vaginal bleeding: 33%
o Frank bleeding: 6%; greater chance with transcervical
o Subchorionic hematoma: 4% after transcervical
o Fetomaternal hemorrhage: 40% to 70%; greater chance with transabdominal
o Risk of infection:
Chorioamnionitis: 0% to 0.5%
Maternal septic shock: three reported cases
Delivering Results of CVS
• Inform parents as soon as possible.
• Give diagnosis to both parents at once.
• Best if someone with sufficient knowledge of condition is present.
• Bring in interpreter if necessary.
• Avoid value judgments.
• Allow time for family to grieve.
• Offer family time alone.
• Provide both positive and negative aspects of syndrome.
• Provide informational resources for medical services and support groups.
• Provide referrals to other specialists.
• Discuss possible pregnancy outcomes.
• Provide sensitive pregnancy options.
Changes in Skin during Pregnancy
• Increased vascularity and melanocyte activity due to increased progesterone and estrogen
• Increased pigmentation of the face (chloasma), areola, abdomen (linea nigra), and genitalia
• Darkening of scars and moles:
o Check borders/size of preexisting skin lesions
o Recommend use of sunscreen
• Striae of breasts and abdomen
• Palmar erythema and spider nevi on face and upper body due to vasodilating estrogenic effects
• Pruritis without skin changes in 15% of women during third trimester due to elevation of bile salts:
o May involve mild increase in LFTs and Bilirubin levels
o Provide SxRx relief with skin lotions and/or antipruritics
Changes in Head and hair during Pregnancy
Mild changes in scalp, such as excessive oiliness or dryness
• May notice increased oiliness of scalp and straighter hair
• Loss at frontal and parietal areas is common
o There should be no bald spots or pluckable hair
• May notice more hair on the brush
Changes in face and eyes during Pregnancy
• Soft tissue fullness in midface late in pregnancy
• No facial edema and no lid edema, as this would indicate possible toxemia
Vessel dilation in the sclera
Changes in ears during Pregnancy
• Increased vascularity of the TMs (hyperemic)
• Blockage of eustachian tubes common
• Mild conductive hearing loss
• May require premedication with nasal decongestants and increased fluids before flying
Changes in nose during Pregnancy
• Chronic nasal congestion and nose bleeds more common due to increased vasodilation
• Six times greater risk for sinusitis
• Use saline nasal sprays, Chlortrimetron Cat. B, and Nasalcrom Nasal Spray (Cromolyn) Cat. B
Changes in mouth during Pregnancy
• Gingival hyperplasia without bleeding due to progesterone effects
o Gums appear swollen, but not sore or excessively friable
• Increased saliva production
Prenatal Care: Goals & Benefits
• To prevent, identify, and/or ameliorate maternal or fetal abnormalities that adversely effect pregnancy outcome, including socioeconomic and emotional factors as well as medical/obstetric considerations.
• Anticipatory guidance during the pregnancy, labor, and postpartum period and intervention to prevent or minimize morbidity.
• To promote adequate psychological support from partners, family, and caregivers, especially during the first pregnancy. This promotes successful adaptation to the pregnancy and the challenges of raising a family.
Prenatal Care: Definition
Definition: a continuum of family health care from the preconceptual period through the first postpartum year
• Commences with an extensive Hx and P.E.
• Includes an estimation of gestational age and determination of the EDC
• Includes drawing of routine lab tests
Initial Prenatal Assessment
• Ideally should be initiated by 10 weeks
• Guidelines set up by ACOG mainly for testing
• Care provider: There is no statistical significance perinatal morbidity of patients cared by midwife/general practitioner/ob/gyn in the United States.
• Guidelines for testing can take a risk-based approach vs. an universal-screening approach
Prenatal Complications Prevented or Minimized
• Anemia due to Fe or folic acid deficiency
• UTIs and pyelonephritis
• PIH
• Preterm labor and delivery
• IUGR
• STDs and their effect on the newborn
• Rh isoimmunization
• Breech presentation at birth
• Hypoxia or fetal death from postterm birth
• Major goal is to prevent or minimize complications so early identification is crucial
Initial Prenatal Visit
Overview
• Patient may present at any gestational age.
• Why did patient choose your practice?
o "Thanks for choosing me!"
• Review where the infant will be delivered, on-call arrangements, after-hours protocols, etc.
• Explain the roles of the different medical professionals who may be involved.
Initial Prenatal Visit OB/GYN hx
• Number of pregnancies:
o Full-term/preterm, ectopic, termination, miscarriage, twins
• For each pregnancy:
o Date of delivery
o Gestational age
o Location of birth
o Sex of the child
o Type of delivery
o Complications
• Menstrual history
• Last pap
• STD exposure
• DES exposure
• Genital tract procedures
• Last contraception use
Initial Prenatal Visit med/surg hx
• Endocrine
• Cardiovascular
• Migraines
• Exercise-induced asthma
• Hospitalizations
• Psychiatric disorders
• Allergies
• Medications
• Substance abuse (past and present
Initial Prenatal Visit - IPV
Domestic Violence
ACOG and AMA recommend that providers routinely assess pregnant women for domestic violence:
• Markers include bruising, improbable injury, depression, late prenatal care, missed prenatal appointments.
Initial Prenatal Visit - Genetics History
• Age at delivery
• Ethnic background
• Neural tube defects
• Congenital heart defects
• Down syndrome
• Cystic fibrosis
• Huntington's disease
• Birth defects
• Recurrent miscarriages
Who requires genetic counseling?
Anyone who:
• Has given birth to a child with, or has a family history of, chromosomal birth defects, chromosomal anomaly, or known genetic disorders
• Has given birth to a child with mental retardation
• Has given birth to a baby who died in the neonatal period
• Has had multiple fetal losses
• Has had abnormal serum screening results
• Is in a consanguineous relationship
• Has had maternal conditions predisposing the fetus to congenital abnormalities
• Has a history of teratogenic exposure
• Has had a fetus with suspected abnormal ultrasound findings
• Has a parent who is a known carrier of a genetic disorder
Initial Prenatal Visit - Psychosocial Assessment
• How does patient feel about the pregnancy?
• Who accompanies the pregnant woman?
• How were patient's previous pregnancies?
• How is patient doing with her children?
• If appropriate, what pregnancy options should she consider?
• What is her living situation, now and when baby is born?
Calculation of EDC - Initial Prenatal Visit
• Estimated date of confinement/due date
• Crucial for pregnancy management
• Naegele's rule: subtract three months from LNMP, add seven days, and add one year:
o Assumes a 28-day menstrual cycle
• Ultrasonography:
o Measurement of crown-rump
o Error of seven days:
The bigger the baby is, the more error you will have
Gestational Age - Initial Prenatal Visit
• Approximate estimation
o Uterine size in first trimester
o Time of quickening (16 to 20 weeks)
o Time fetal heart tones auscultated:
With electronic doppler: 10 to 12 weeks
With a nonelectronic fetoscope: 18 to 20 weeks
Initial Visit PE
• Pelvic exam:
o Pelvis: soft tissue, bony pelvis, pelvic inlet, midpelvis, pelvic outlet, pelvimeter
o Cervix: os, lacerations, length, appearance
o Uterus: size, shape, consistency, position
The Initial Physical Exam
Laboratory Testing: OB Panel
• Blood typing and antibody screen:
o All Rh-negative women will need Rhogam around 28 weeks, or if bleeding occurs.
• Rubella
• RPR/VDRL
• Hepatitis B
• Chlamydia and gonorrhea
• HIV:
o Universal screening
o Patient can opt out
• Hematocrit/hemoglobin/CBC/MCV:
o MCV of less than 80 warrants hemoglobin electrophoresis
The Initial Physical Exam
Laboratory Testing: Additional Testing for At-Risk Clients
• TSH:
o Have symptoms of thyroid disease
o Have personal or family history of thyroid disease
o Have predisposition, such as another endocrine disorder, goiter, iron deficiency, etc.
• Diabetes:
o If BMI over 30, consider a first-trimester glucose test and an Ha1c
• TB
• Toxoplasmosis:
o Routine in France, but not United States
• Hepatitis C
• Bacterial vaginosis (BV)
The Initial Physical Exam
Laboratory Testing: Optional Testing
• Cystic fibrosis:
o Should be available to all couples, especially those at high risk (Caucasian, European, Ashkenazi Jewish)
• Fragile X:
o Causes developmental delay/autism
• Tay-Sachs:
o Should be offered to those of Eastern European, Ashkenazi, Southern Cajun, or French Canadian descent
• Spinal muscular atrophy:
o Controversial:
The American Academy of Genetics recommends universal screening, but ACOG disagrees.
o Test if there is any history of SMA or SMA-like illness
Visit Schedule
Recommended by ACOG:
• Extensive initial visit:
o The timing will depend on where you work.
• Revisit every four weeks until 28 week's gestation.
• After 28 weeks, visits are every two weeks until 36 weeks.
• After 36 weeks, weekly visits until delivery:
o Remind patients that EDC is an estimation.
Subsequent Visits Recommended by ACOG:
• Visits tend to be shorter.
• Explore any problems.
• Document growth of fetus.
• Identify complications.
• Ensure they know how to reach a provider after hours.
• Ensure they are wearing seat belts.
o Show patients how to tuck the belt under their uterus.
o Remind patients that airbags should remain on.
• Ask about other issues:
o Nutrition
o Alcohol, tobacco, drugs
o Work
o Sexual activity
o Medications
FDA Pregnancy Category Classification
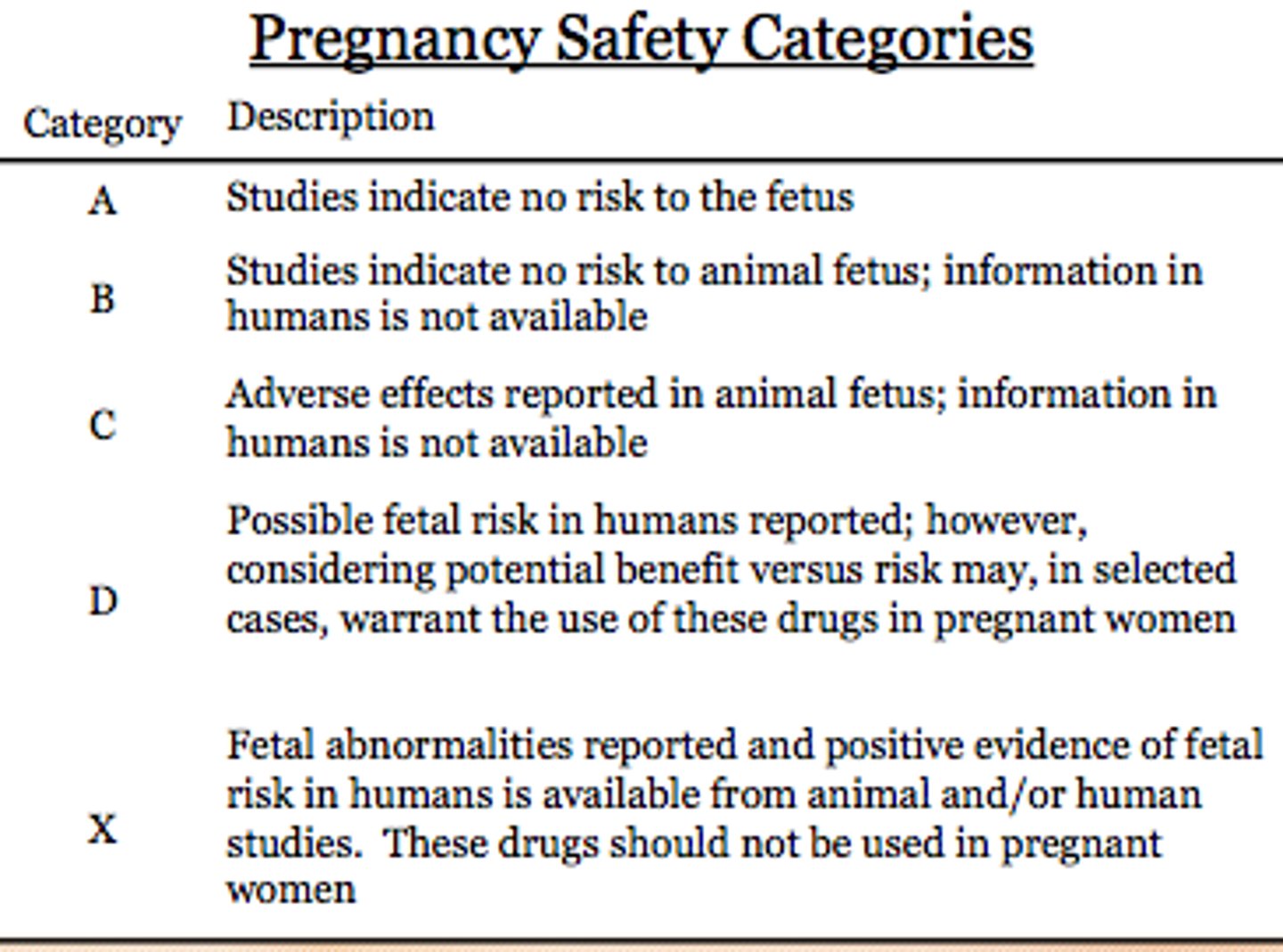
Category A
Category A Adequate and well-controlled studies have failed to demonstrate a risk to the fetus in the first trimester of pregnancy (and there is no evidence of risk in later trimesters)
Category B
Category B Animal reproduction studies have failed to demonstrate a risk to the fetus and there are no adequate and well-controlled studies in pregnant women OR animal studies have shown an adverse effect, but adequate and well-controlled studies in pregnant women have failed to demonstrate a risk to the fetus in any trimester
Category C
Category C Animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks
Category D
Category D There is positive evidence of human fetal risk based on adverse reaction data from investigational or marketing experience or studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks
Category X
Category X Studies in animals or humans have demonstrated fetal abnormalities and/or there is positive evidence of human fetal risk based on adverse reaction data from investigational or marketing experience, and the risks involved in use of the drug in pregnant women clearly outweigh potential benefits
Commonly Used Medications in Pregnancy
• Tylenol (acetaminophen)
• NSAIDs
• Opioids
o Heroin
o Pain medicine
• Cold and allergy medication
• Antiobiotics
• Medication for constipation and diarrhea
• Antiemetics and antinausea
• Medications for GERD
• Sleep aids
• If traveling:
o Provide resources
o Talk about infectious disease exposure
• Pesticides and hair treatments
Air Travel in Pregnancy
• Fetal heart rate will not be affected.
• Commercial travel is safe until about 36 to 37 weeks.
o After that time, the baby can come at any time.
• Restrictions on high-risk pregnancies.
• Discuss hydration, movement, appropriate clothing, and seat belts.
• Discuss effects of high altitude.