4.3 Coughing Dog & Cat
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
38 Terms
what does cough indicate?
-quick, forceful expiration against closed glottis
-response to mechanical/
chemical irritation of larynx, pharynx, trachea, or airways-> can indicate disease in a variety of respiratory tract locations
-productive vs non-productive
-acute (sudden onset) vs chronic (more than 6 weeks)
-when to investigate depends on history, chronicity, & severity
major differentials for acute cough
allergic/inflammatory:
pharyngitis/laryngitis (irritants i.e. smoke, dust chemicals)
infectious:
CIRDC (dog)
distemper (dog)
lungworm
-A. vasorum, C. vulpis, F. osleri (dog)
-Aelurostrongylus abstrussus (cat)
heartworm (D. ommitus)
pneumocystis (dog)
herpes 1, cowpox, virulent calici (cat)
toxoplasmosis (cat)
miscellaneous:
aspiration pneumonia (d>c), might have bacterial component
tracheal/bronchial foreign body
non-cardiogenic pulmonary edema
airway trauma/iatrogenic
major differentials for chronic cough
allergic/inflammatory: feline lower airway disease (asthma, bronchitis)
eosinophilic bronchopneumopathy (dog)
chronic bronchitis (dog)
laryngitis/
pharyngitis
infectious: chronic/recurrent aspiration, possibly with bacterial component
lungworm
-A. vasorum, C. vulpis, F. osleri (dog)
-Aelurostrongylus abstrussus (cat)
fungal
-blastomycosis, histoplasmosis, coccidiomycosis, aspergillosis, pythiosis (dog, non-UK)
mycobacteria (C>D)
degenerative:
tracheal collapse (dog)
bronchiectasis (dog), secondary to other pathology
pulmonary fibrosis (dog)
neoplastic:
primary airway or lung tumors
metastasis
miscellaneous:
tracheal/bronchial foreign body
ciliary dyskinesia
cardiovascular:
left-sided heart failure (dog)
left atrial enlargement (dog)
cough rare in cats with CHF
signalment & history
signalment: infectious cause in young animals vs neoplastic/
degenerative in older animals
history: chronicity, acute vs chronic onset, nature of coughing, inciting event or management change, vaccination & anti-parasite treatment, contact with other animals, travel history, risks for aspiration ex. recent regurgitation, vomiting, swimming, laryngeal dysfunction
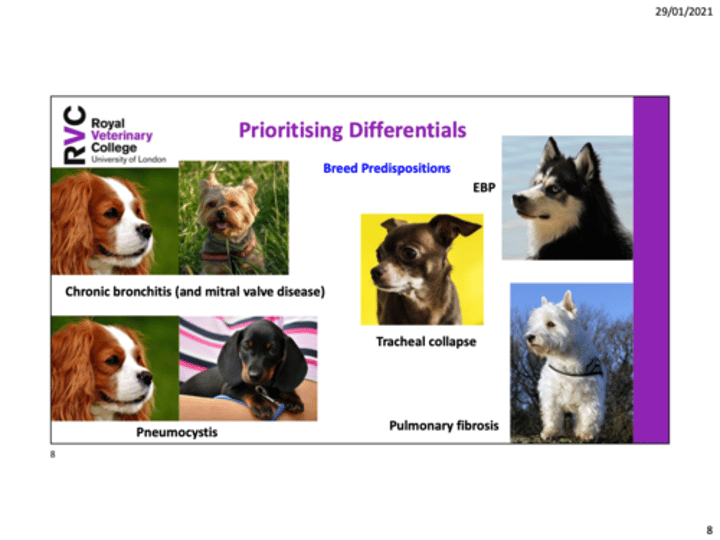
breed predispositions (image)
general physical exam
often stable, but may require gentle handling & stabilization
mucous membranes: cyanosis, pallor, ecchymoses
mass lesions
lymphadenomegaly
body weight & condition
body temp
hands-off respiratory exam
respiratory rate
effort (inspiratory vs expiratory, abdominal)
noise
orthopnea
hands-on cardiorespiratory exam
auscultate all lung areas & heart
wheezes- partial airway obstruction
crackles- alveolar disease, ex: pulmonary edema, fibrosis, & pneumonia
auscultate upper airway (referred sounds)
heart rate & rhythm
murmurs- location, intensity
investigative techniques: hematology & biochemistry
do not perform investigations in well CIRD cases
hematology & biochemistry: prior to GA, bronchoscopy, airway sampling etc.
possible findings: inflammatory leukogram, eosinophilia (allergic/asthma, parasitic, EBP), erythrocytosis, biochem often unremarkable
coagulation times: A. vasorum
investigative techniques: idexx angio detect ELISA
rapidly detects angiostrongylus vasorum adult worm antigen
sensitivity 95.7%, specificity 94%
may allow earlier detection than other methods
disadvantages: false negatives (first 3-6 weeks of exposure), false positives (treated or naturally cleared infections-antigen detectable for 3-9 weeks after), does not detect all canine lungworm species or feline lungworm
investigative techniques: Baermann's fecal sedimentation
detects all lungworm types
best for feline lungworm detection
use pooled sample
negative in pre-patent period
consider microscopic fecal smear examination-> sensitivity 54%, specificity 95%, also detects larvae of other lungworms
investigative techniques: distinguish cardiovascular vs respiratory
physical exam: sinus arrythmia or normal, regular heart rate excludes CHF, intensity of murmur (louder associated with CHF)
radiographic findings
NT-proBNP: N-terminal pro b-type natriuretic peptide, differentiation of CHF & pulmonary disease
echocardiography: left atrial enlargement, contractility, structural disease, identification of pulmonary hypertension
other miscellaneous tests
-blood gas analysis
-TFAST
-feline infectious rhinitis/
rhinotracheitis testing
-heartworm (D. immitis) antigen or antibody testing (adult worm antigen test, antibody detection in cat)
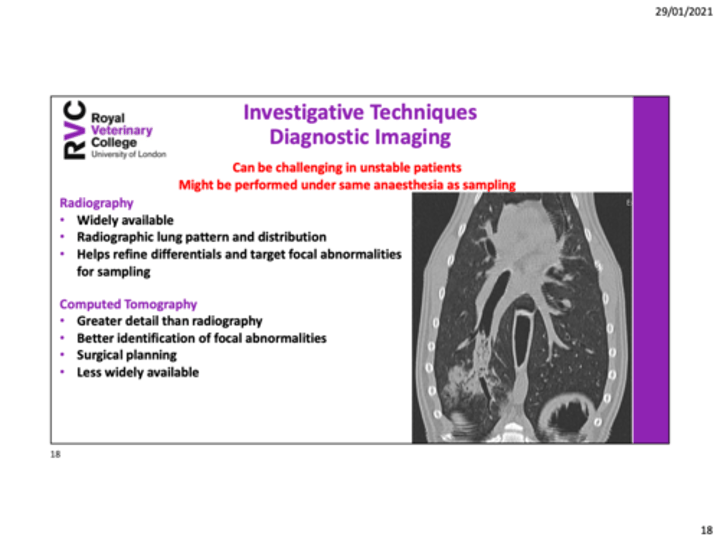
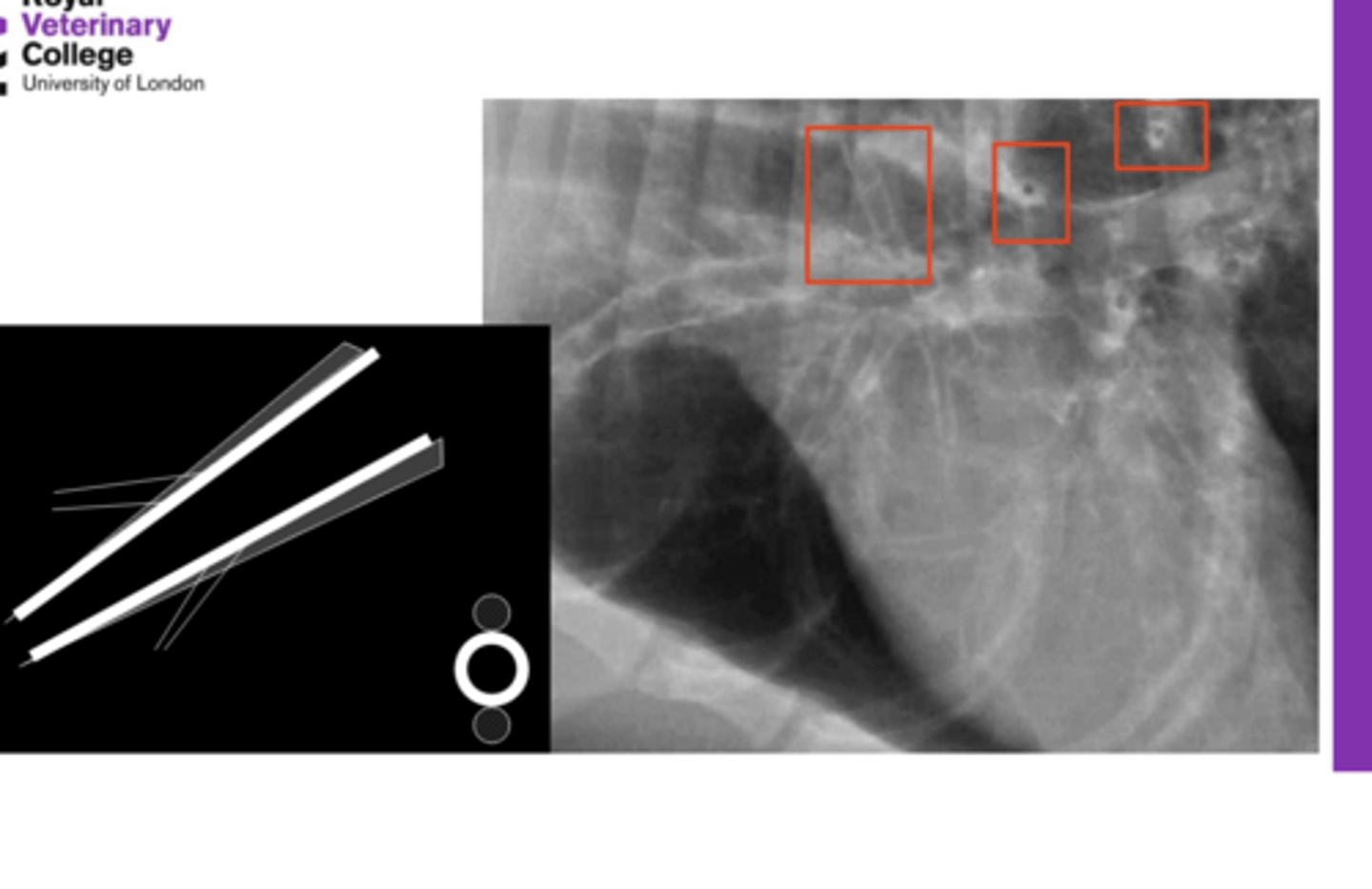
investigative techniques: radiography & computed tomography
radiography: widely available, radiographic lung pattern & distribution, helps refine differentials & target focal abnormalities for sampling
computed tomography: greater detail than radiography, better identification of focal abnormalities, surgical planning, less widely available
investigative techniques: fluoroscopy & bronchoscopy
fluoroscopy: referral procedure, performed conscious, real time evaluation of breathing & food ingestion, investigation of esophageal function in aspiration pneumonia or tracheal collapse
bronchoscopy: foreign body retrieval, airway examination, sampling, consider patient size & stability (cats)
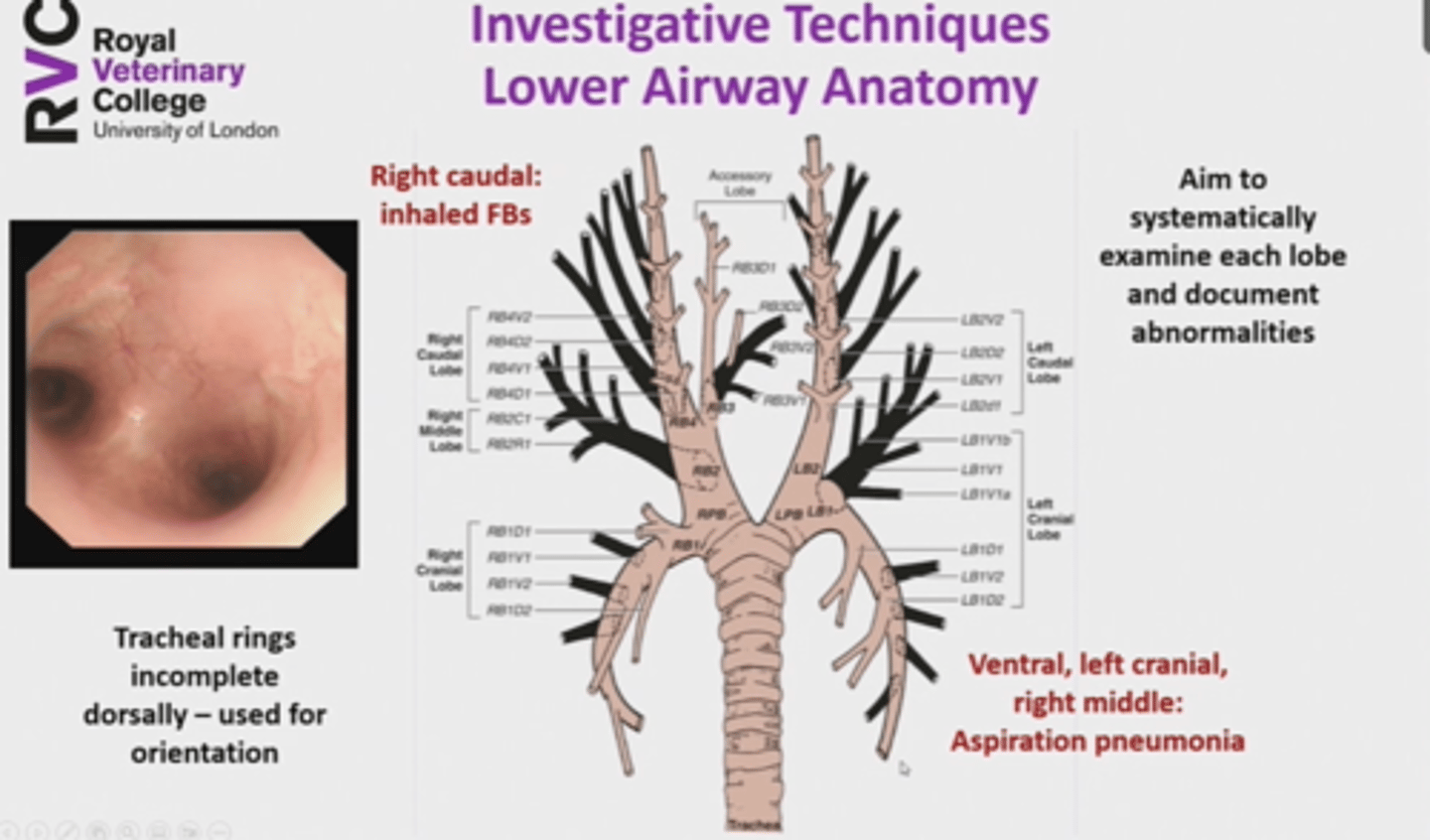
investigative techniques: lower airway anatomy
right caudal-> inhaled FB
ventral, left cranial, right middle-> aspiration pneumonia
tracheal rings incomplete dorsally
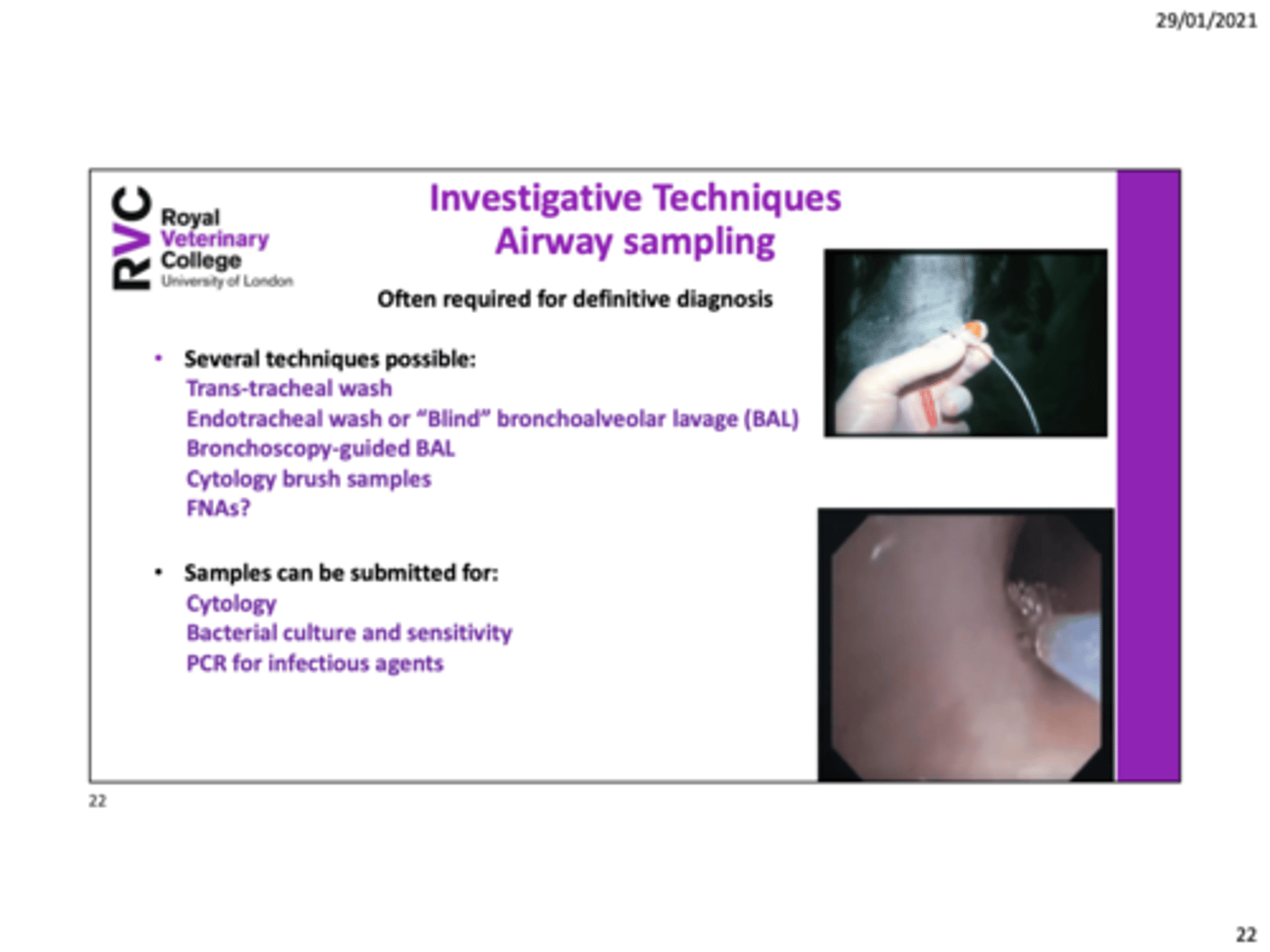
investigative techniques: airway sampling
transtracheal wash, endotracheal wash or "blind" BAL, bronchoscopy-guided BAL, cytology brush samples, US guided FNA (airway biopsy)
samples submitted for cytology, bacterial C&S, PCR for infectious agents (histology or electron microscopy)
canine chronic bronchitis: etiology, clinical history, & physical exam
etiology: minimum 2 months, chronic inflammatory airway disease of unknown exciting cause
clinical history: middle-aged/older small breed, possible concurrent tracheal collapse, bronchiectasis, mitral valve disease, pulmonary hypertension, overweight/obese, paroxysmal, usually unproductive cough, exacerbated by excitement/
exercise/change in environmental temperature
physical exam: otherwise well, overweight, mild tachypnea, wheezes, murmur & location, sinus arrhythmia
canine chronic bronchitis: starting investigations & echocardiography
investigations: CBC, biochemistry, angiostrongylus/
heartworm testing
echocardiography: murmurs common, identification of pulmonary hypertension (may require treating)
canine chronic bronchitis: deeper investigations
diagnosis of exclusion
thoracic radiographs (or CT): bronchial pattern, bronchiectasis, other cardiopulmonary diseases
fluoroscopy: dynamic airway collapse
bronchoscopy: non-specific, erythema, irregular mucosa surface, mucous, bronchiectasis, bronchomalacia
BAL cytology: non-degenerate neutrophils with increased mucous, mild hemorrhage
bacterial culture & mycoplasma PCR
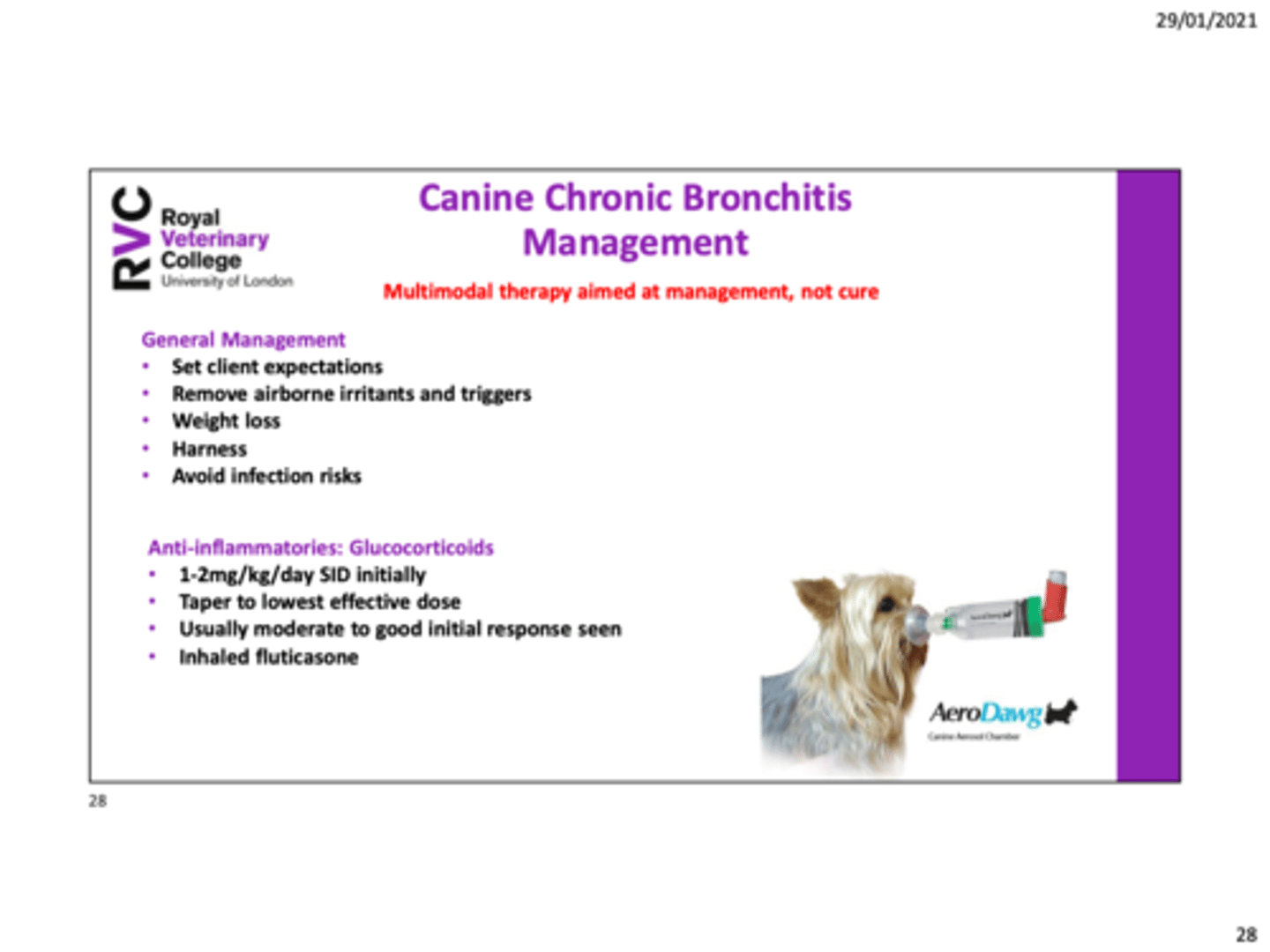
canine chronic bronchitis: management
set client expectations (no cure), remove airborne irritants & triggers, weight loss, harness, avoid infection risks
anti-inflammatories: 1-2mg/kg/day SID, taper to lowest effective dose, usually moderate to good initial response seen, inhaled fluticasone
bronchodilation: theophylline
pulmonary hypertension: sildenafil
antibiotics: confirmed/highly suspected infection
cough suppressants: butorphanol, codeine, or hydrocodone
progressive, chronic=> therapy likely to require alteration over time
tracheal collapse: history, clinical signs, & physical exam
history & clinical signs: toy breeds (chihuahuas, yorkies), honking, "quaking" cough, may progress to dyspnea or collapse episodes
physical exam: generally normal, characteristic cough on tracheal pinch, deformed tracheal cartilages might be palpable
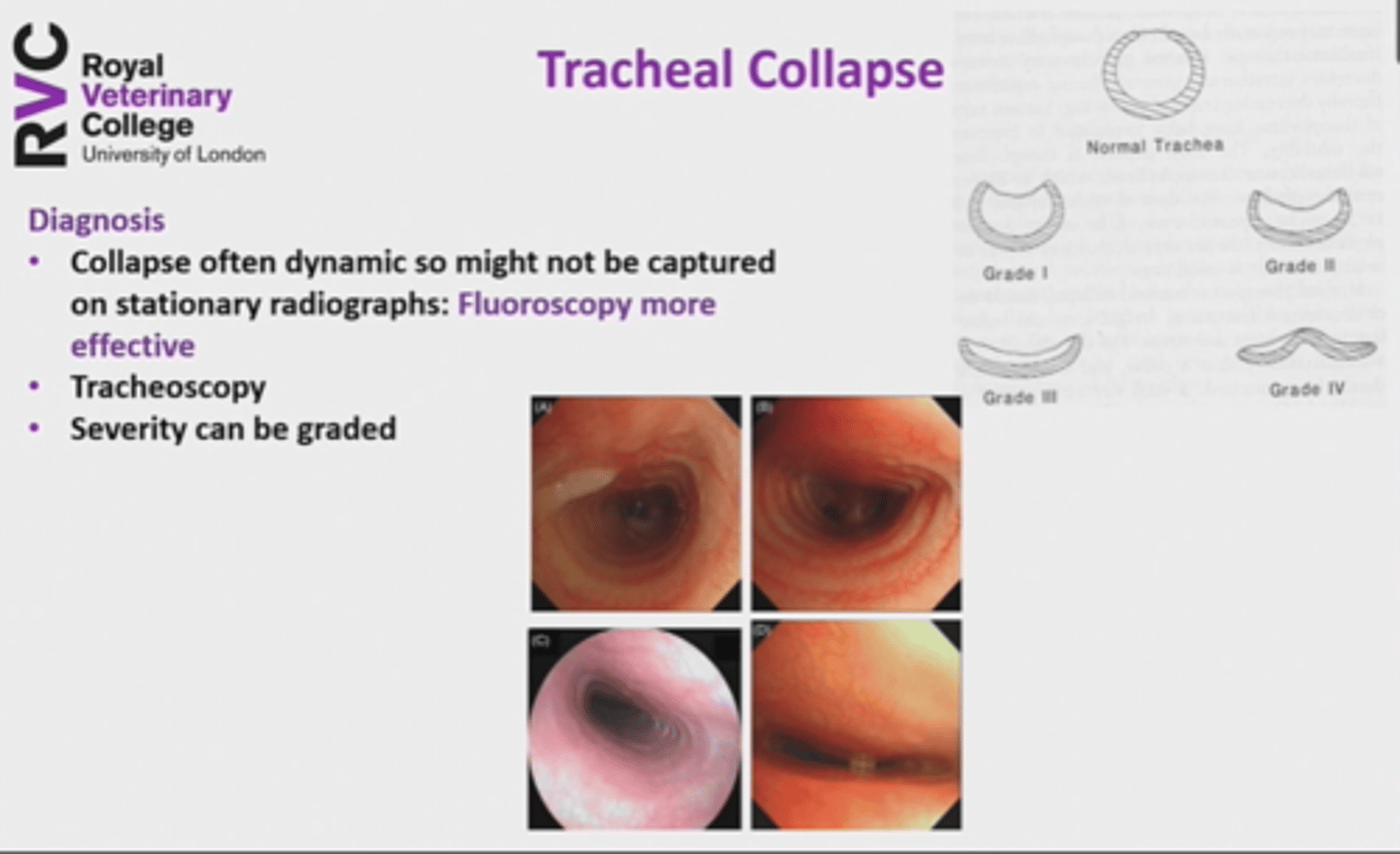
tracheal collapse: diagnosis
-collapse often dynamic so might not be captured on radiographs
-fluoroscopy more effective
-tracheoscopy
-severity can be graded
tracheal collapse: treatment
similar to chronic bronchitis, esp. cough suppressants, avoiding triggers, & harness walking
surgical options: extraluminal rings for cervical collapse, intraluminal stents, reserved for severely-affected cases
eosinophilic bronchopneumopathy: etiology, clinical signs, & signalment
etiology: infiltration of bronchial mucosa and/or pulmonary parenchyma with eosinophils, cause unknown in almost all cases, better termed "idiopathic" EBP
clinical signs: coughing, gagging, retching, decreaed exercise tolerance, wide spectrum of severity, up to 50% have concurrent nasal discharge
signalment: female young adult dogs, huskies, malamutes, akitas, & dachshunds?, reported in many breeds, systemic hypereosinophilic syndrome in Rottweilers
eosinophilic bronchopneumopathy: diagnosis
consistent clinical signs & signalment
hematology: up to 50% have peripheral eosinophilia
exclusion of other causes of eosinophilia: angiostrongylus antigen test, fecal float & baermann;s, heartworm antigen if endemic region
airway sampling required for definitive diagnosis
blind BAL, bronchoscopy guided (examine respiratory mucosa, visualize sampling area, cytology-brush samples), cytology BAL fluid +/- cytobrush, bacterial culture of BAL
BAL findings
increased cellularity, increased eosinophil count BUT often not predominant cell type, increased neutrophil count, mucous
exclude parasite disease & bacterial pneumonia prior to EBP treatment

eosinophilic bronchopneumopathy: management
glucocorticoid therapy: prednisolone, tapered over several months, consider second immunosuppressive if necessary
inhaler therapy: fluticasone, likely best introduced shortly after starting oral prednisolone, long-term maintenance treatment if requiring on-going medication
eosinophilic bronchopneumopathy: prognosis
response to glucocorticoids generally good
monitoring response to therapy: peripheral eosinophilia, clinical signs
relapse possible: consider inhaler, low-dose prednisolone, second immunosuppressive
inhaler/2nd agent useful if severe steroid side-effects
lungworm: predilection & clinical signs
most common in dogs, A. vasorum most prevalent
clinical signs: cough, tachypnea, dyspnea, hemoptysis, generalized coagulopathy (A. vasorum)
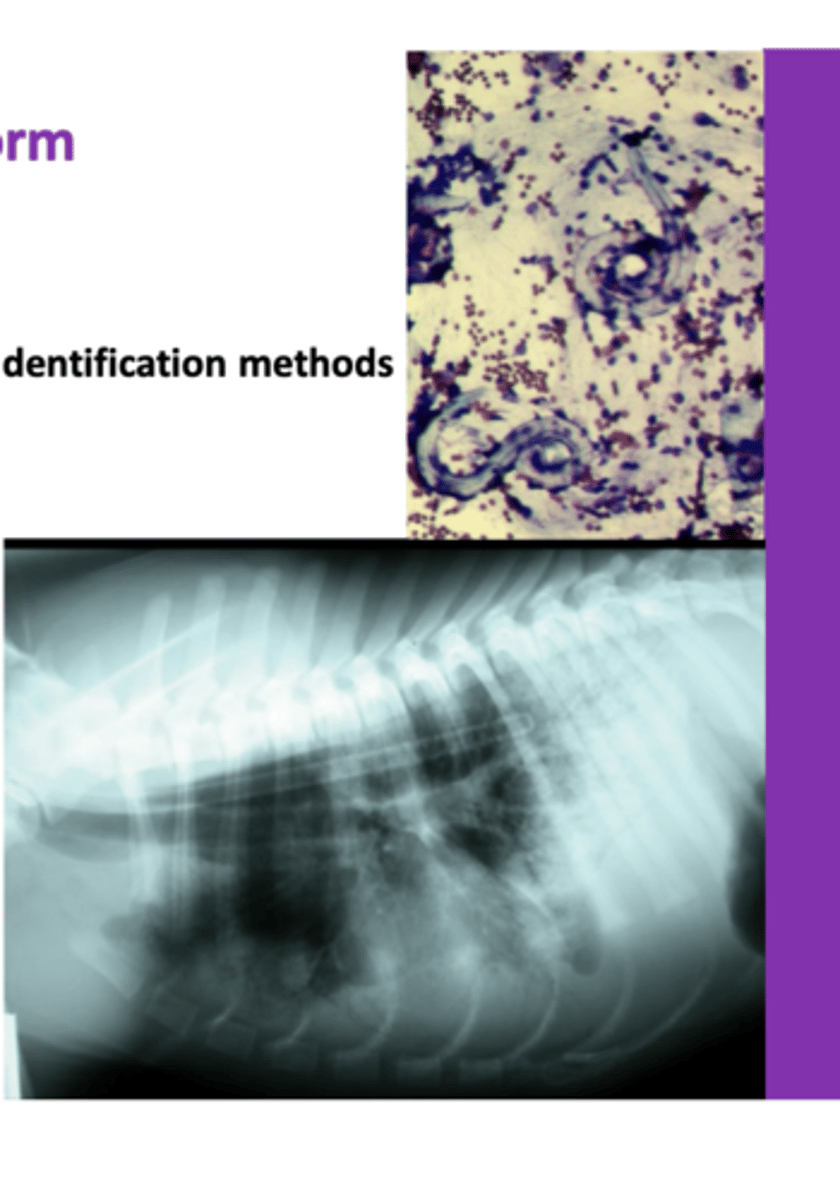
lungworm: diagnosis
bloodwork, previous lungworm identification methods
thoracic radiography: peripheral alveolar pattern, bronchial & nodular-interstitial
larvae in BAL/TT wash samples, but ideally diagnose non-invasively
tracheal nodules (filaroides)
lungworm: treatment & prevention
treatment:
-7 day course oral fenbendazole (unlicensed)
-oral milbemycin (once weekly for 4 weeks)
-some spot-on moxidectin products
-anti-inflammatory steroids in severe cases
-supportive care
prevention:
-oral/spot-on moxidectin or oral milbemycin
feline asthma (and chronic bronchitis): etiology & clinical presentation
etiology: allergic, type 1 hypersensitivity to inhaled aeroallergens, findings overlap with other diseases, esp. chronic bronchitis, most common cause of chronic cough in cats
clinical presentation: young, siamese, asthmatic crisis-> tachypnea, open-mouth breathing, orthopnea, expiratory "push", longer term history of a cough, chronic
-> coughing, hacking, poss. vomiting?
feline asthma (and chronic bronchitis): physical exam findings
tachypnea, positive tracheal pinch, expiratory wheeze, can be remarkable
feline asthma (and chronic bronchitis): acute medical therapy
bronchodilation: inhaled albuterol/
salbutamol or terbutaline SQ/IM, epinephrine/
adrenaline IM (not widely-used, suggested in agonal situations, not with other B2 agonists)
anti-inflammatory: dexamethasone
feline asthma (and chronic bronchitis): laboratory work & thoracic radiographs
laboratory work: peripheral eosinophilia (17-40% of cases), baermann's to rule out aelurostrongylus abstrusus, fecal float, heartworm testing
thoracic radiographs: broncho/
bronchointerstitial pattern, hyperlucency, lung lobe collapse (right middle), pneumothorax, normal in approx. 25%, CT more sensitive
feline asthma (and chronic bronchitis): bronchoscopy & BAL
bronchoscopy: consider whether safe, pre-treat with terbutaline, mucous accumulation, hyperemia, epithelial irregularities, airway collapse, bronchiectasis, non-specific
BAL: blind or bronchoscopy-guided, asthma-> eosinophilic & neutrophilic, chronic bronchitis-> non-degenerate neutrophilic, can be overlap, bacterial culture, mycoplasma culture or PCR
feline asthma (and chronic bronchitis): management
oral glucocorticoids: prednisolone, side-effects, unsuitable for some patients
inhaled glucocorticoids: fluticasone, using spacer, prednisolone for at least 10-14 days, esp. if moderate to severe signs
allergen avoidance & weight management
bronchodilators: not as monotherapy, inhaled salbutamol during crises, theophylline
clinical signs: waxing & waning, correspond poorly with severity of inflammation
repeated BAL cytology? invasive, costly