Session 2: SECOND PART Energy Production from Carbohydrates
1/67
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
68 Terms
What are some regulatory mechanisms of glycolysis
- Substrate availability
- Product inhibition
- Feedback inhibition (allosteric)
- Allostery - binding of activator/inhibitor to allosteric site of enzyme
- Covalent modification of enzymes - phosphorylation/dephosphorylation
What is the name of the lactic acid cycle?
Cori cycle
Summarise what happens in the lactic acid cycle (cori cycle)
Lactate that is released into the blood is taken up by the liver.
Lactate is oxidised to pyruvate.
Pyruvate is then converted to glucose via gluconeogenesis, where it is released back into the blood.
How do you define the cori cycle?
The cycling of lactate and glucose between peripheral tissues (muscle) and liver
In what scenarios is lactate utilisation impaired?
Liver disease
Vitamin deficiencies - e.g. thiamine
High alcohol intake
Enzyme deficiencies
How much lactate is produced without exercise everyday (g)?
40-50g/day (RBC, skin, brain, skeletal muscle, G.I.)
How much lactate is produced WITH exercise everyday (g)?
30g/5 minutes
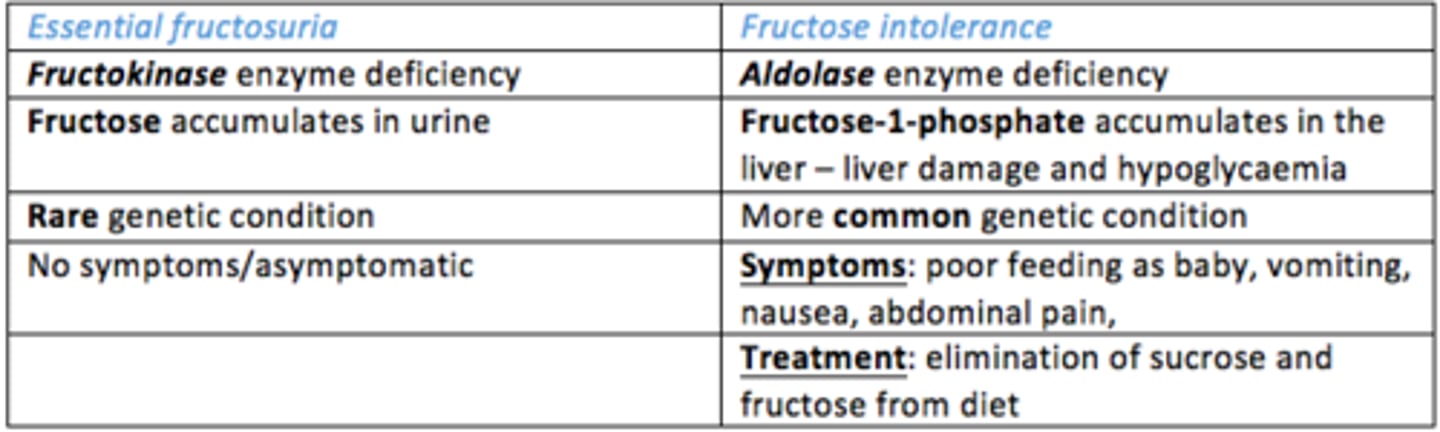
What are some examples of fructose metabolism disorders and what are the causes?
- Essential fructosuria = caused by fructokinase deficiency
- Fructose intolerance = caused by aldolase deficiency
What are the products of sucrose metabolism?
Fructose + glucose
What are the products of lactose metabolism?
Galactose + glucose
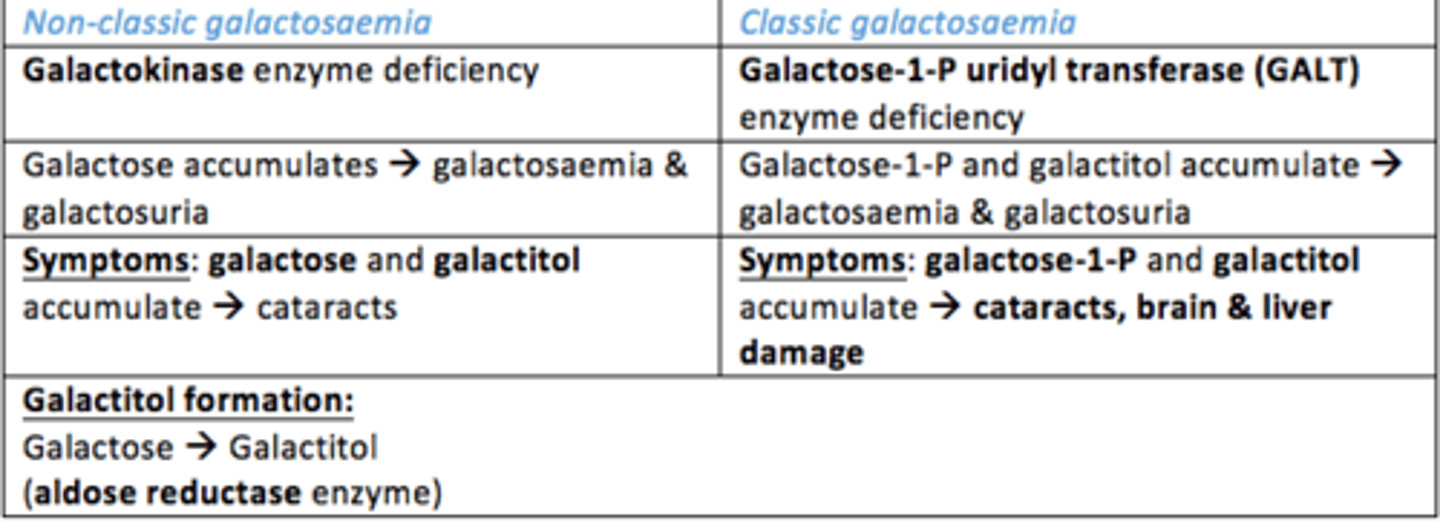
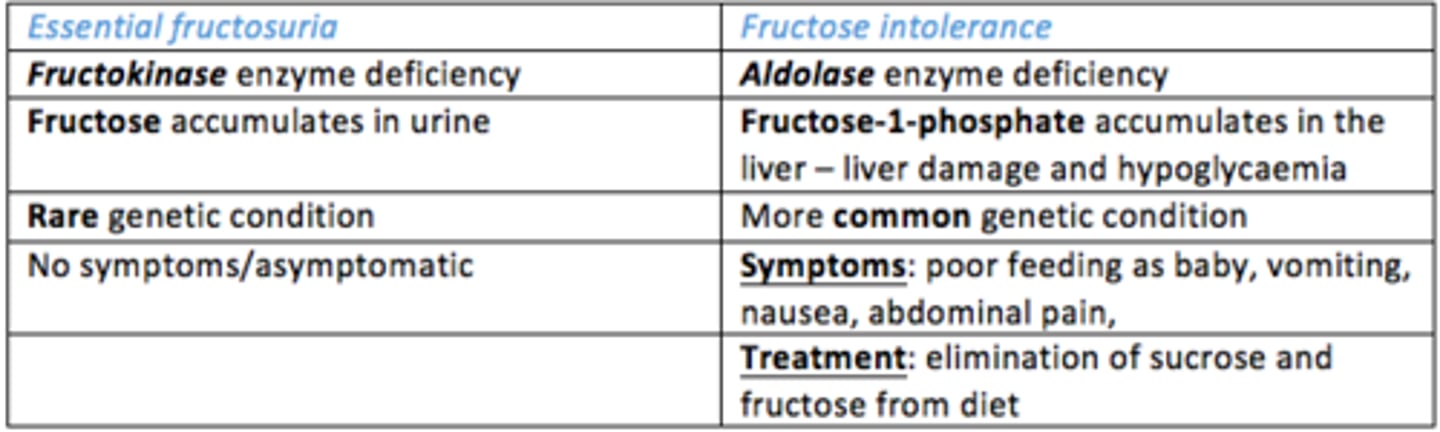
What are some causes of Galactosaemia (deficiency of galactose)
- Galactokinase deficiency = non-classic galactosaemia
- GALT deficiency = classic galactosaemia
What are symptoms of galactosaemia
Poor feeding, vomiting and diarrhoea
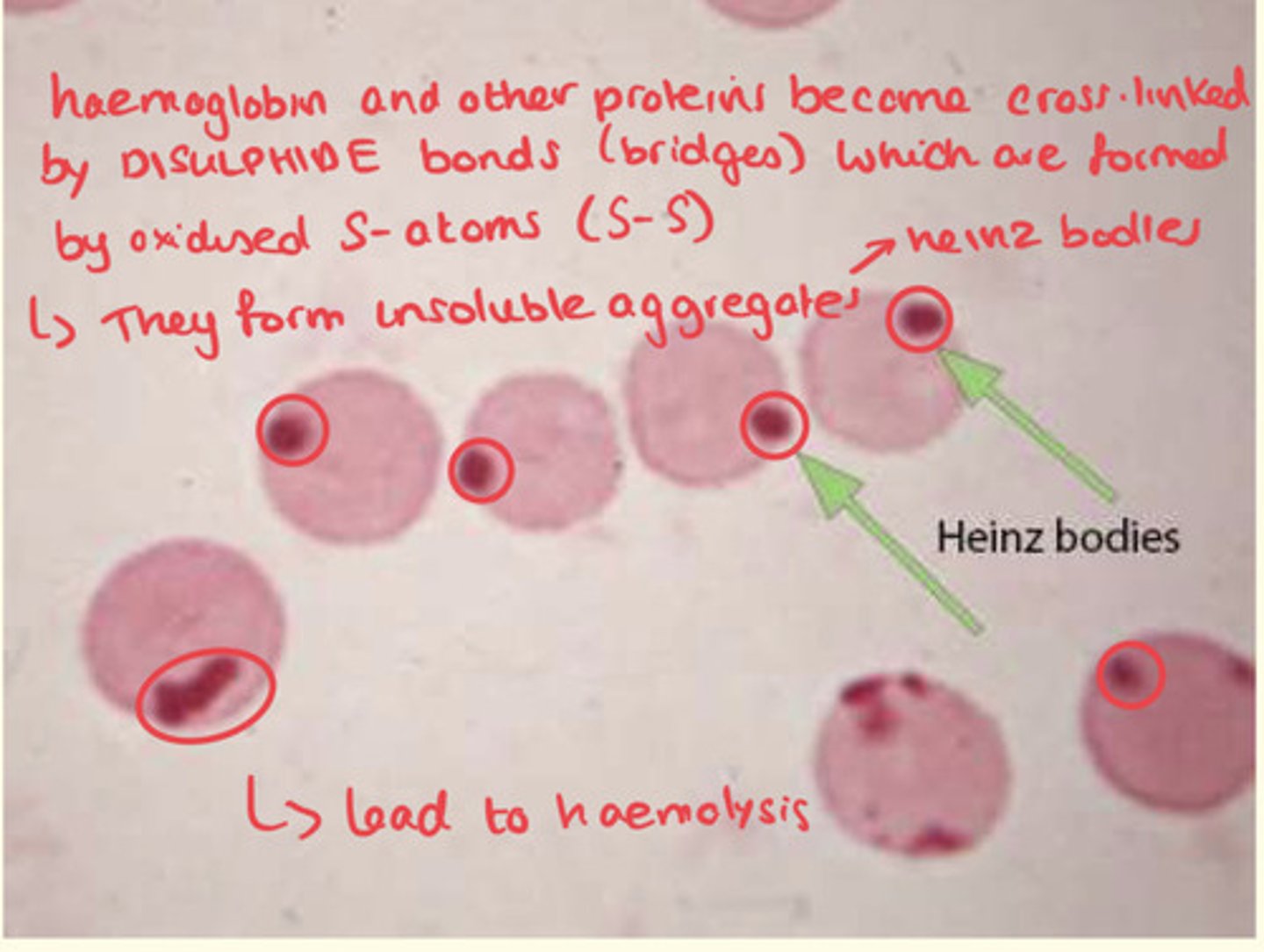
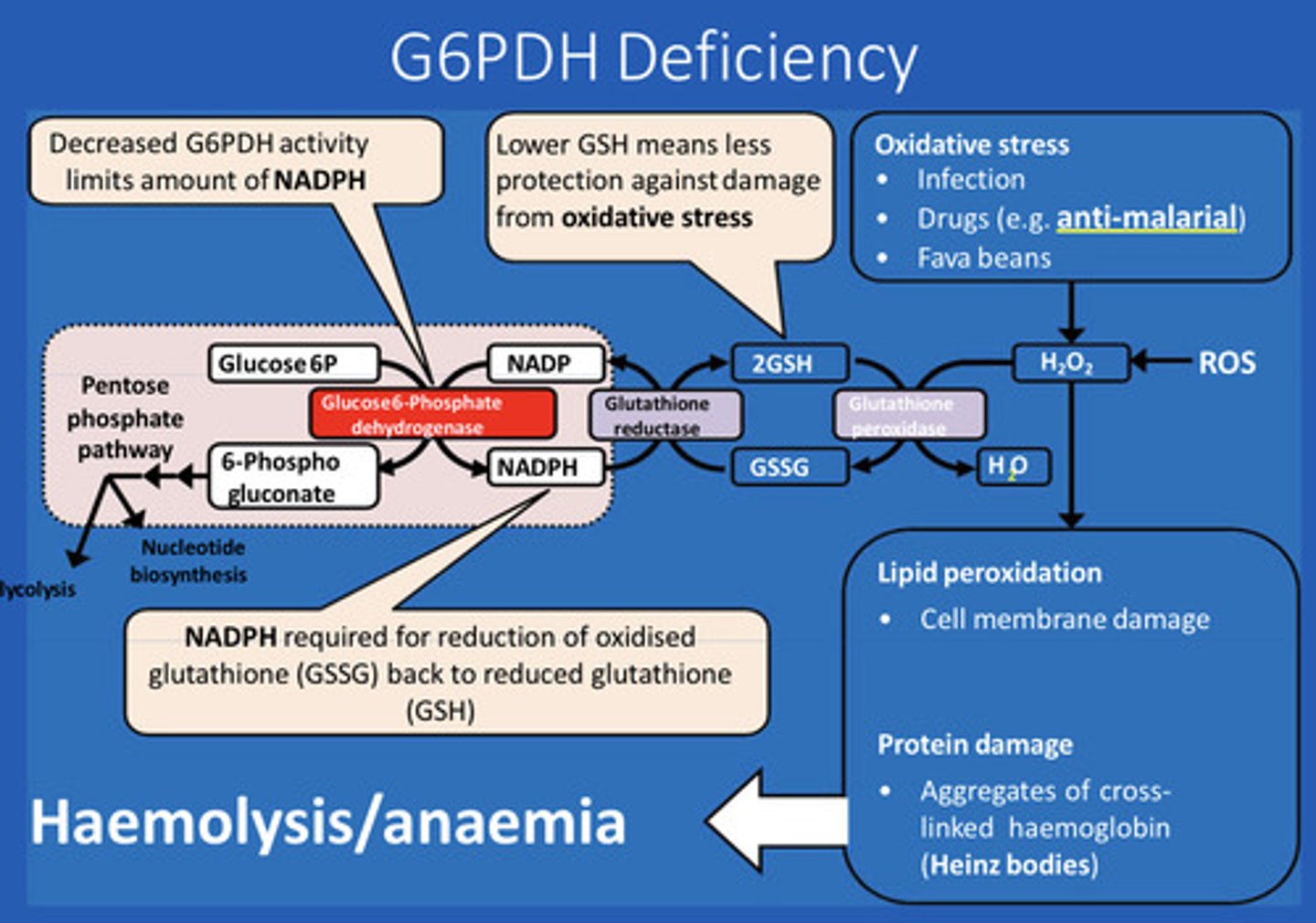
What is the clinical presentation of Glucose-Phosphate Dehydrogenase Deficiency (G6PDH deficiency)?
Haemolytic anaemia, fatigue, pale colour of skin, shortness of breath, jaundice
What are the names given to the insoluble aggregates that attach to RBC membranes in G6PDH deficiency?
Heinz bodies
What is the consequence of attachment of Heinz bodies to RBC membranes?
This leads to destruction of RBCs and causes haemolysis by the spleen
What are some common triggers of G6PDH deficiency?
Certain chemicals in medications (e.g. antimalarials such as primaquine), antibiotics, certain foods (fave beans), and infections
Why is there a need for regeneration of NAD+ that isn't reliant on oxidative phosphorylation (aerobic respiration)?
- RBCs have no mitochondria - no stage 3/4 catabolism
- Kidney medulla, lens & cornea have fewer mitochondria - inefficient oxidative phosphorylation
- Absence of oxygen during e.g. vigorous exercise or poorly oxygenated tissues (hypoxia) due to shock (insufficient blood flow), congestive heart failure or arterial disease = this would make stage 4 ineffective
The rate of lactate production = the rate of lactate __________
The rate of lactate production = the rate of lactate utilisation
In what situations is lactate utilisation impaired?
- Liver disease
- Vitamin deficiencies (e.g. thiamine)
- High alcohol intake
- Enzyme deficiencies
What are plasma lactate concentrations determined by?
- Production of lactate
- Utilisation of lactate (decreased in liver disease, vitamin/enzyme deficiency, high alcohol intake)
- Disposal of lactate (by kidneys)
What is considered high lactate (lactic acidosis) in the blood?
>5mM
What are the major enzymes involved in fructose metabolism?
Fructokinase
Aldolase
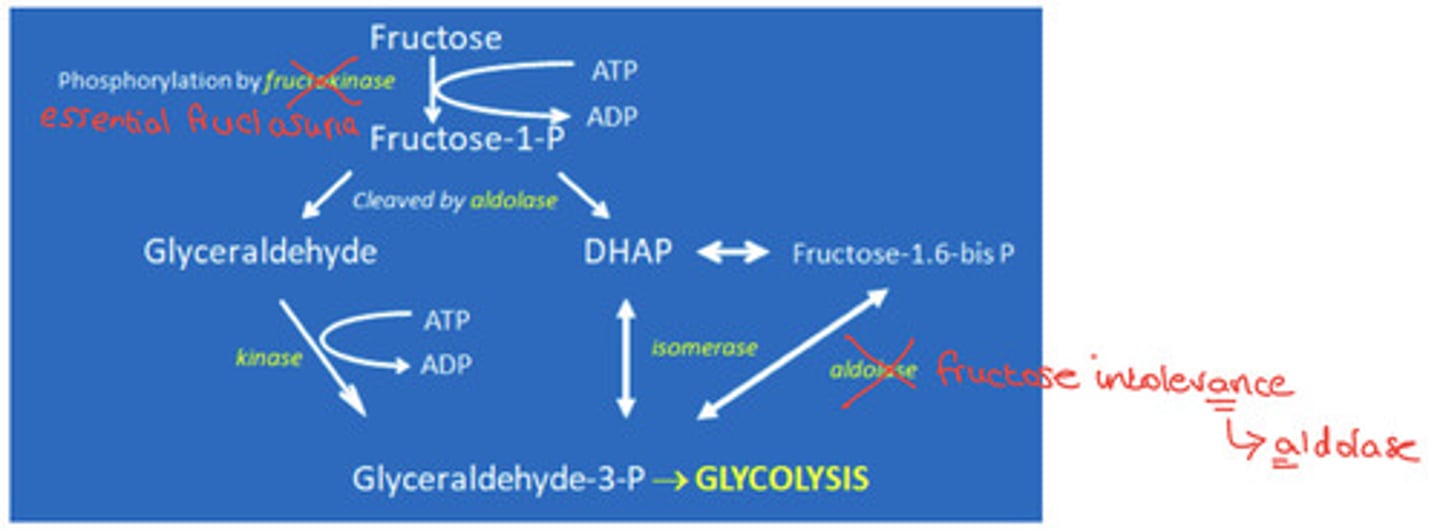
Where is fructose metabolised?
In the liver
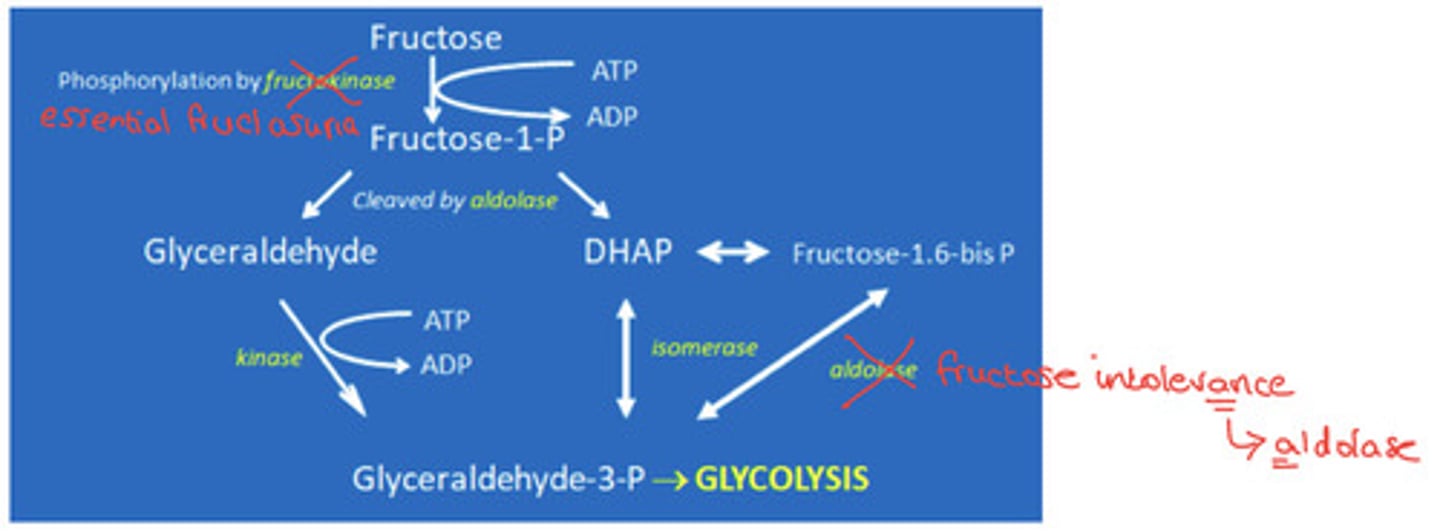
What is the process of fructose metabolism?
Fructose is phosphorylated to fructose-1-P by fructokinase enzyme.
Fructose-1-P is cleaved by aldolase enzyme into 2 constituents...
1) Glyceraldehyde = this is converted to glyceraldehyde-3-phosphate
2) DHAP = this is converted to glyceraldehyde-3-phosphate
Glyceraldehyde-3-phosphate then enters glycolysis
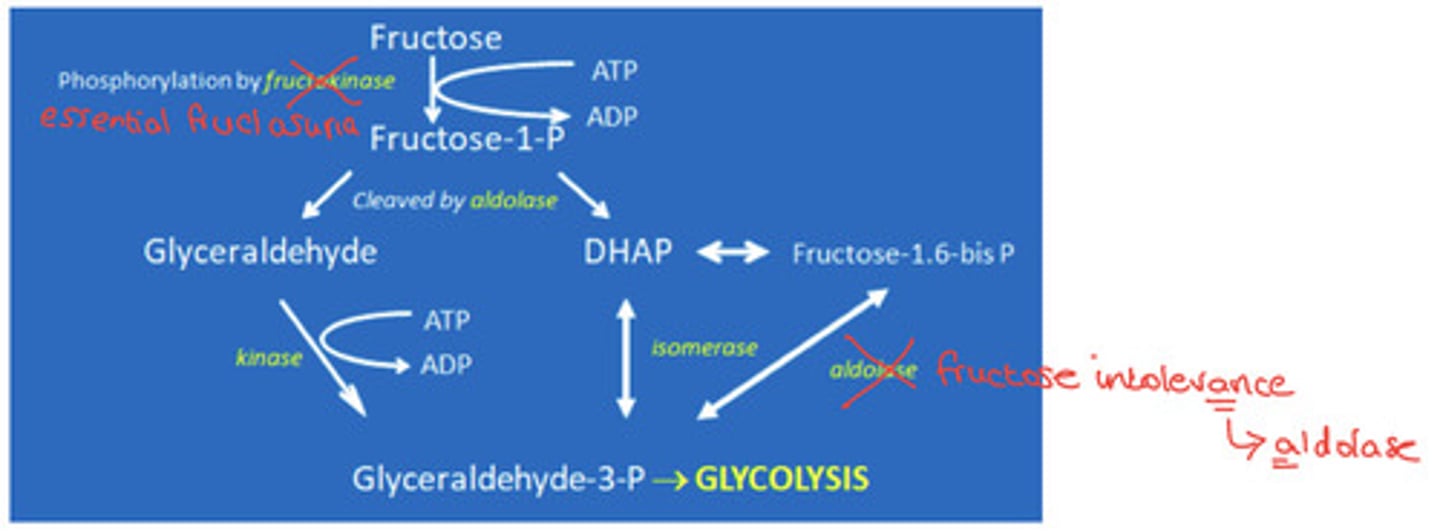
Cause/pathogenesis of fructose intolerance
Aldolase deficiency
- Fructose 1,6-bisphosphate accumulates in the liver
- This leads to liver damage, hypoglycaemia
- This is more common (1:20,000 births)
- Genetic
What are the symptoms of fructose intolerance?
Poor feeding in babies, nausea, vomiting, abdominal pain
What is the standard treatment for fructose metabolism disorders...
Elimination of sucrose (sucrose -> glucose + fructose) and fructose from diet
Where is galactose metabolised?
Galactose is metabolised in the liver
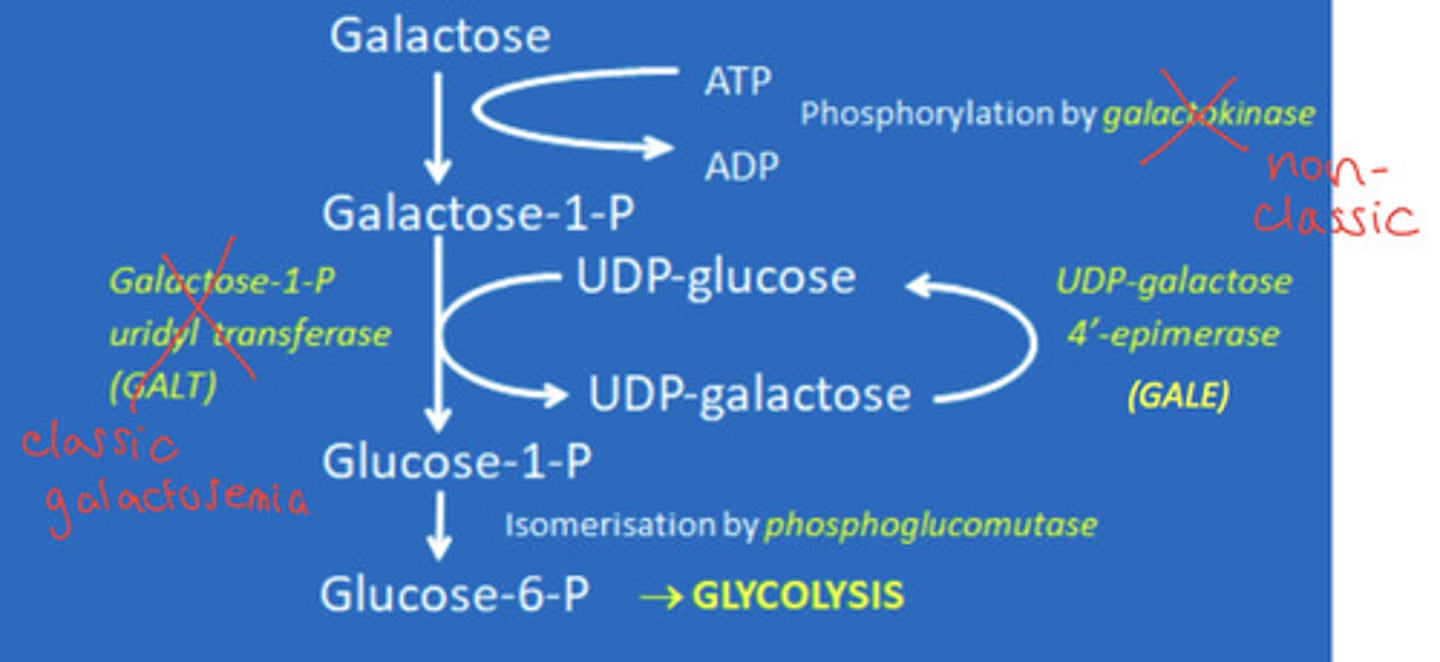
What are the main enzymes involved in galactose metabolism?
- Galactokinase
- Galactase-1-P uridyl transferase (GALT)
What is the process of galactose metabolism?
Galactose is phosphorylated by Galactokinase into galactose-1-phosphate.
Galactose-1-phosphate is converted to glucose-1-phosphate by galactose-1-phosphate uridyl transferase enzyme (GALT).
Glucose-1-phosphate can then be converted into glucose-6-phosphate and sent to glycolysis
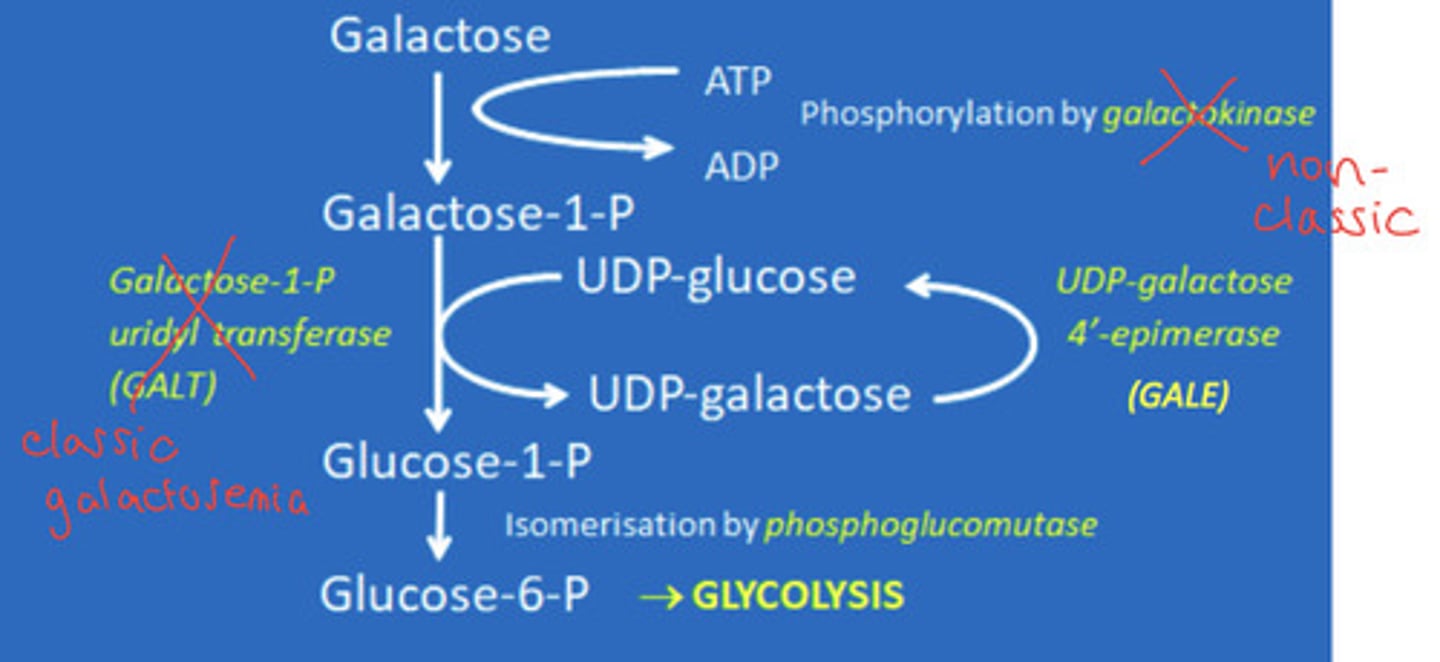
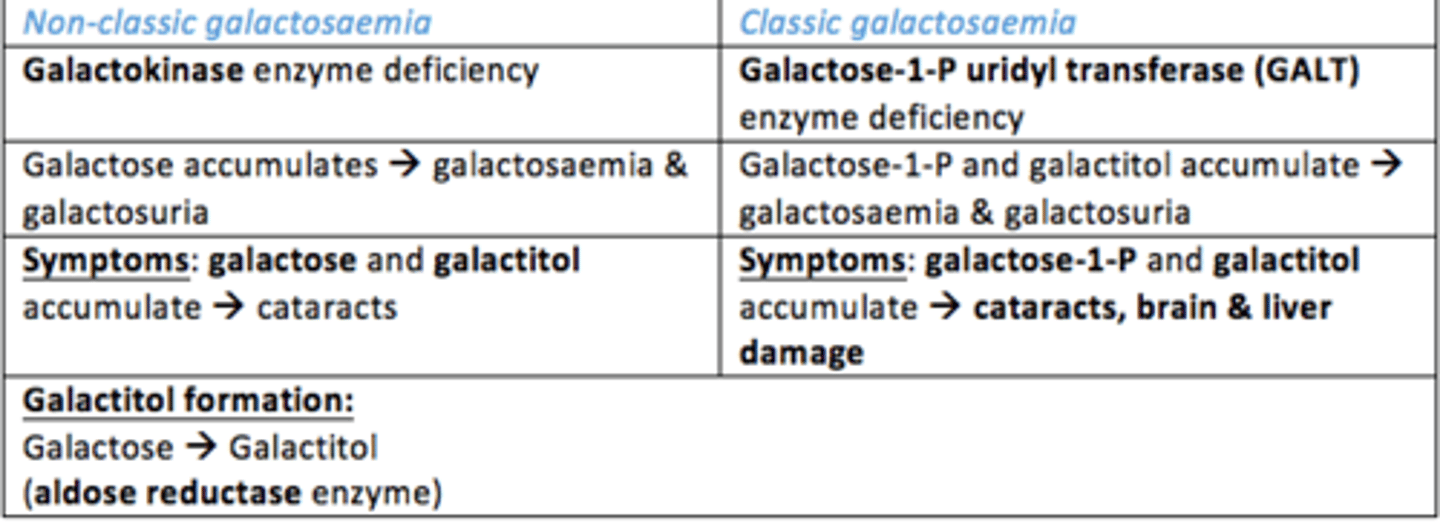
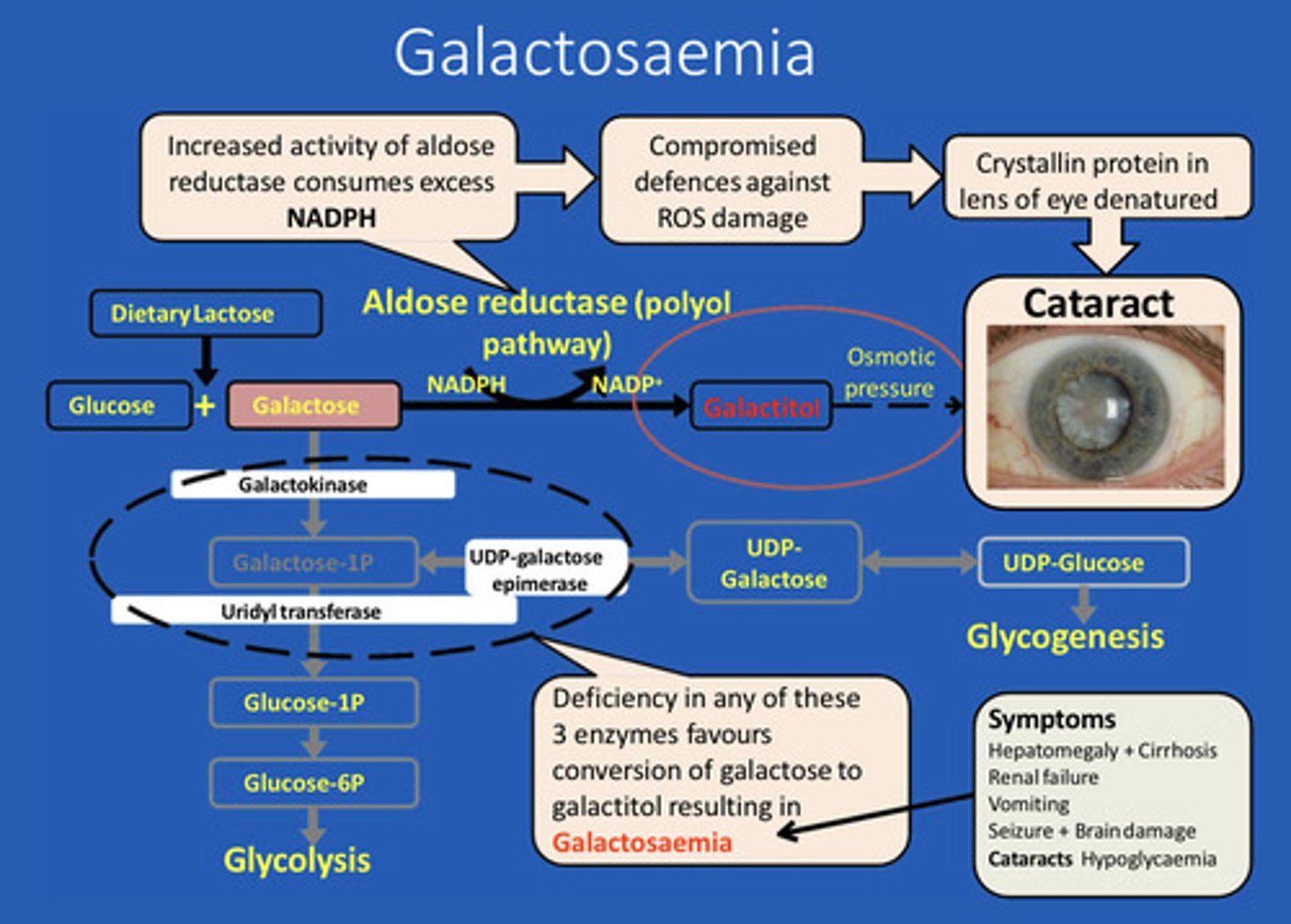
What is non-classic galactosaemia?
- Galactokinase deficiency = leading to accumulation of galactose and galactitol
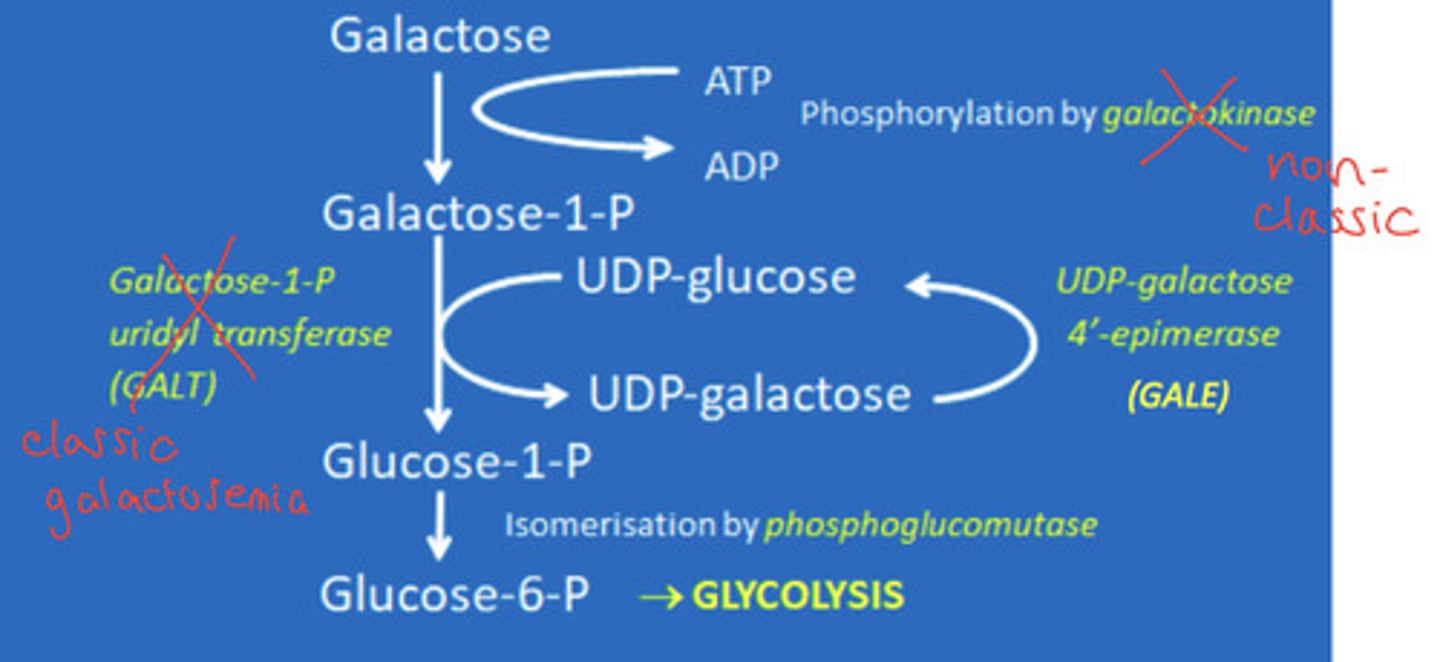
What is classic galactosaemia?
- Galactose-1-phosphate uridyl transferase (GALT) deficiency - Leading to accumulation of galactose-1-p and galactitol
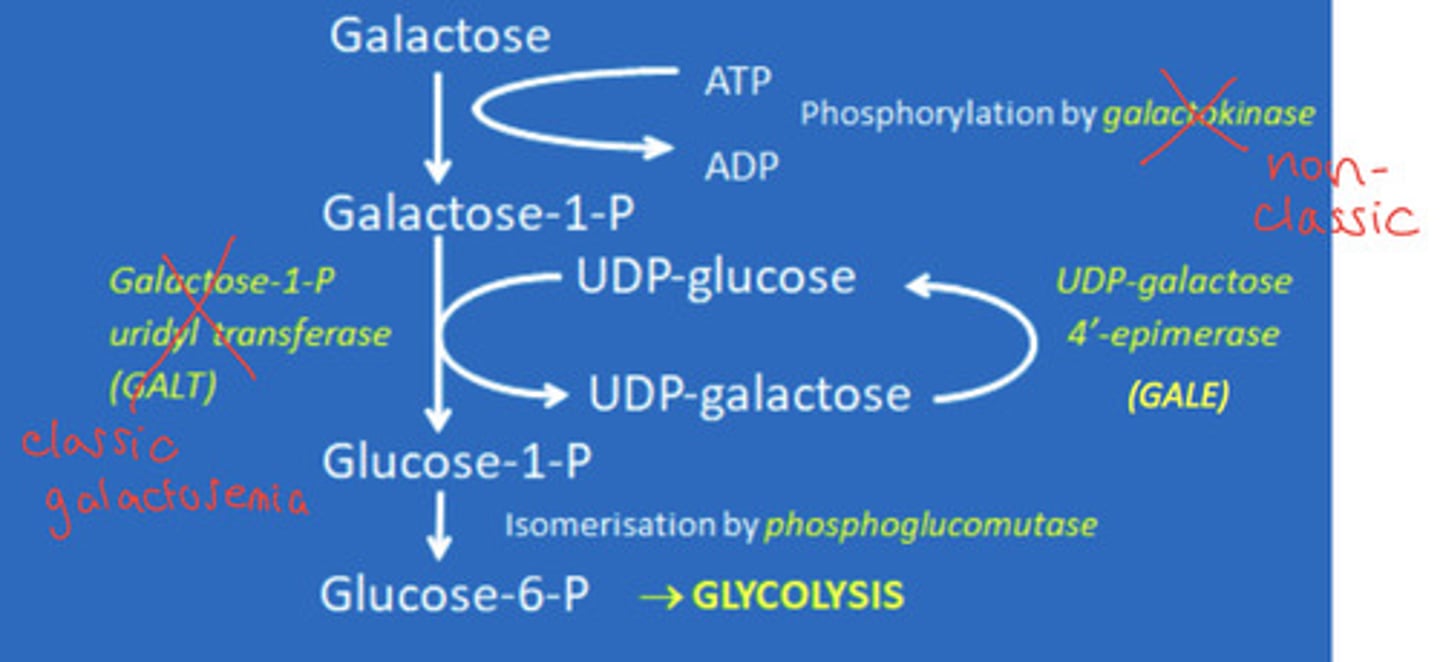
What are the pathological consequences of galactose metabolism disorders?
Cataracts due to galactitol accumulation.
Brain and liver damage
What are the symptoms of galactosaemia?
Poor feeding, vomiting, diarrhoea
What is the standard treatment for galactose metabolism disorders?
Dietary restrictions of lactose and galactose
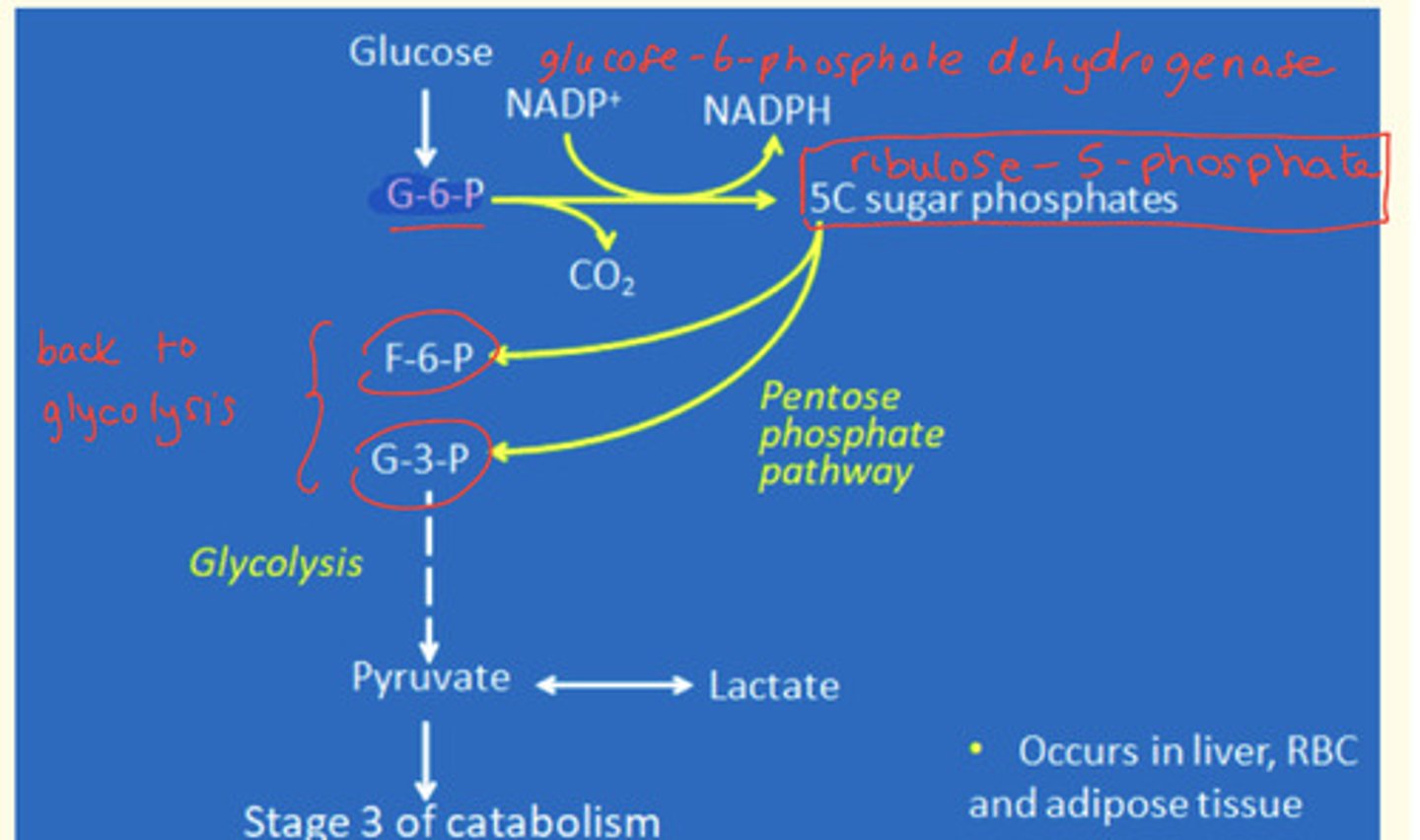
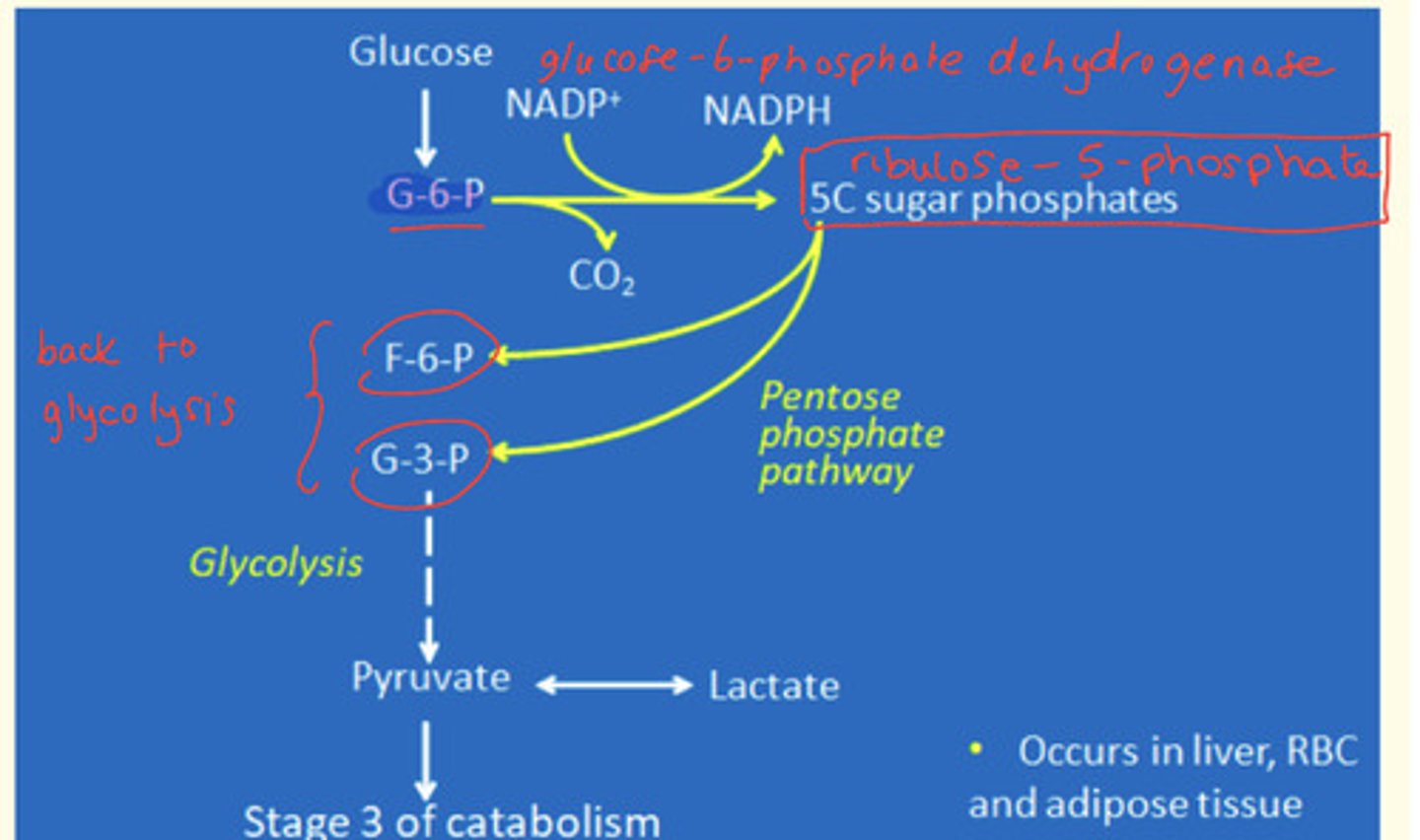
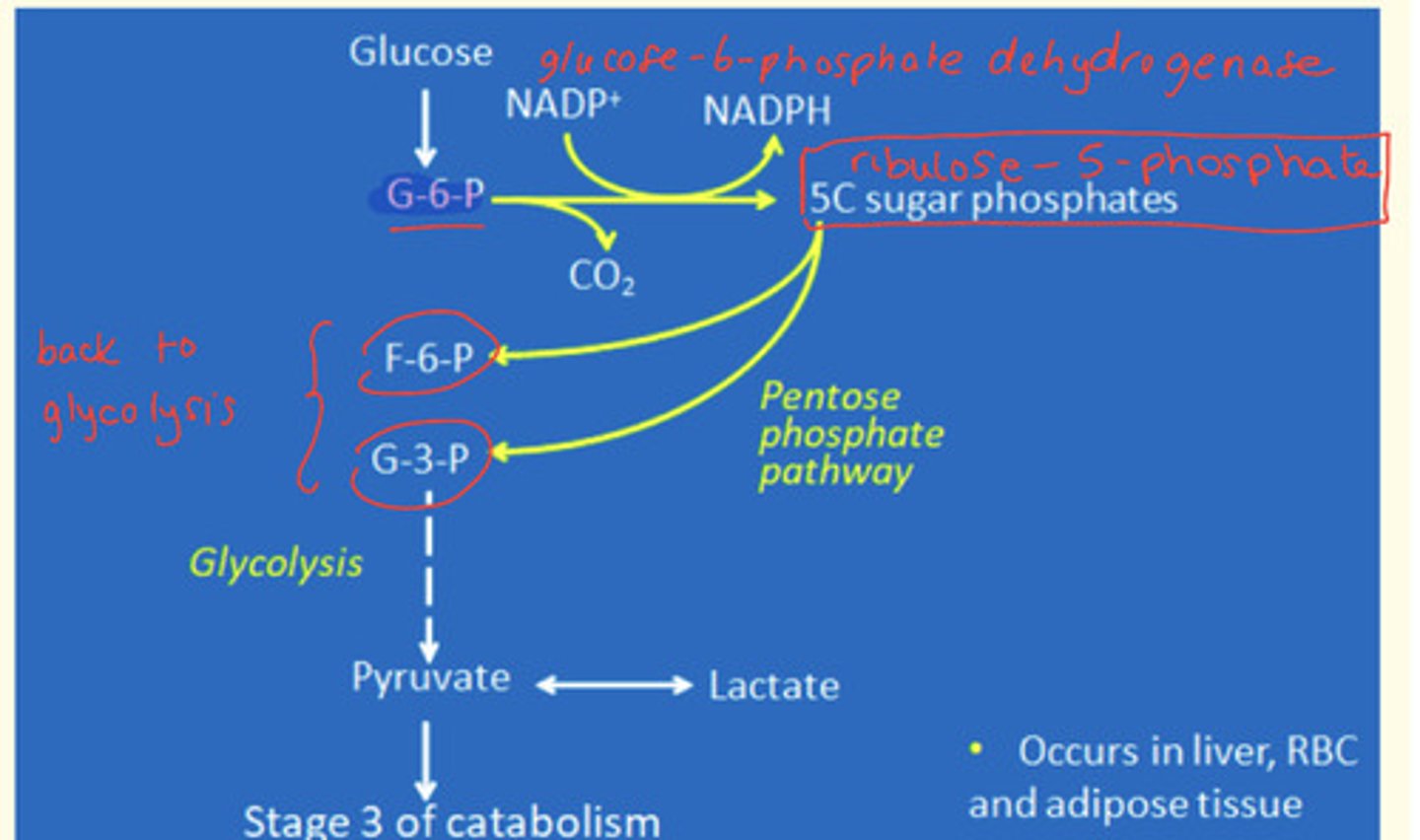
What are the two phases of the pentose phosphate pathway
Oxidative phase
Glucose-6-phosphate oxidised to ribulose-5-phosphate.
This is catalysed by glucose-6-dehydrogenase enzyme
Non-oxidative phase
Rearrangement of glycolic intermediates
Ribulose-5-phosphate converted to either F-6-P (Fructose-6-phosphate) or G-3-P (Glyceraldehyde-3-phosphate)
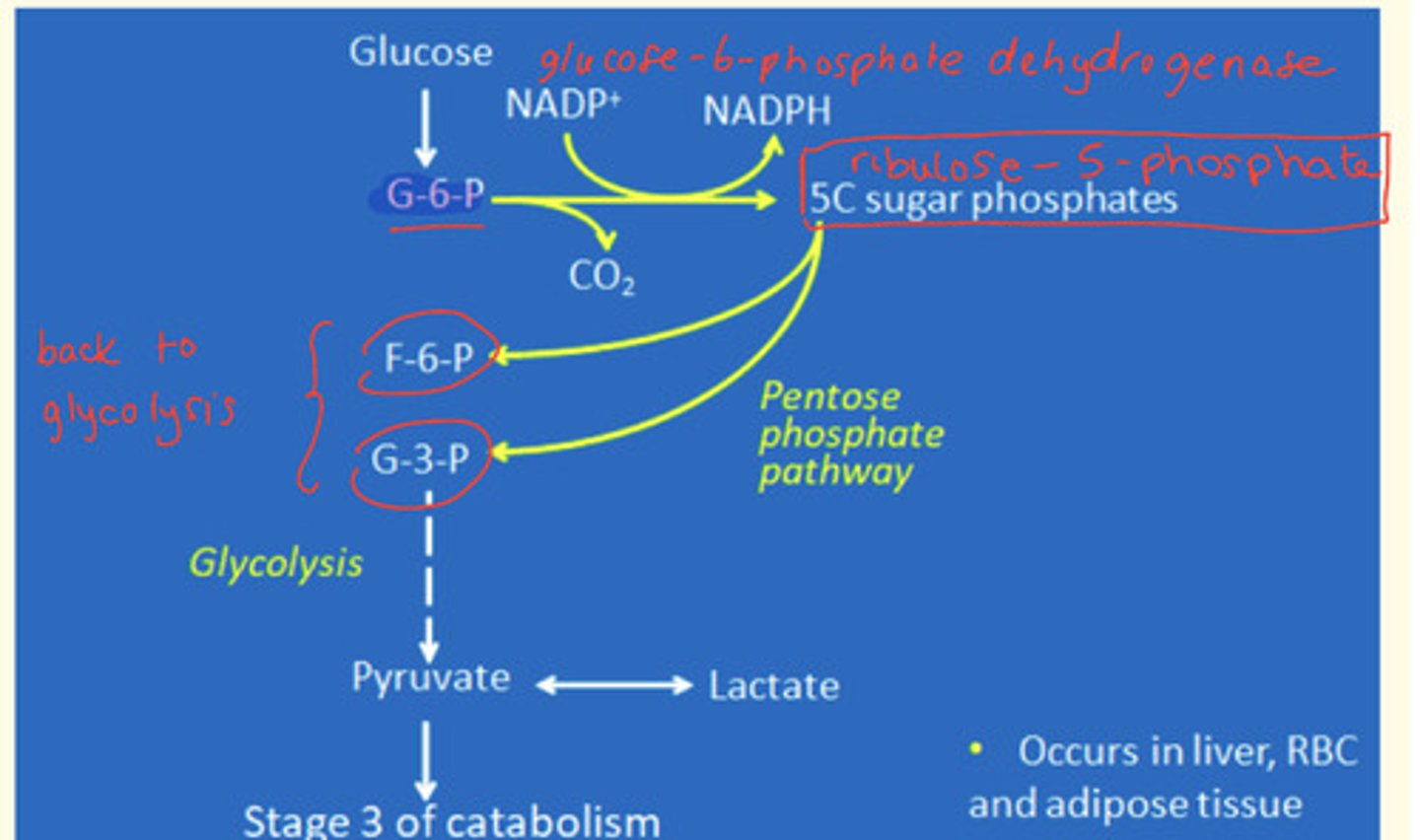
What is the major enzyme involved in pentose phosphate pathway catalysis?
Glucose-6-dehydrogenase enzyme
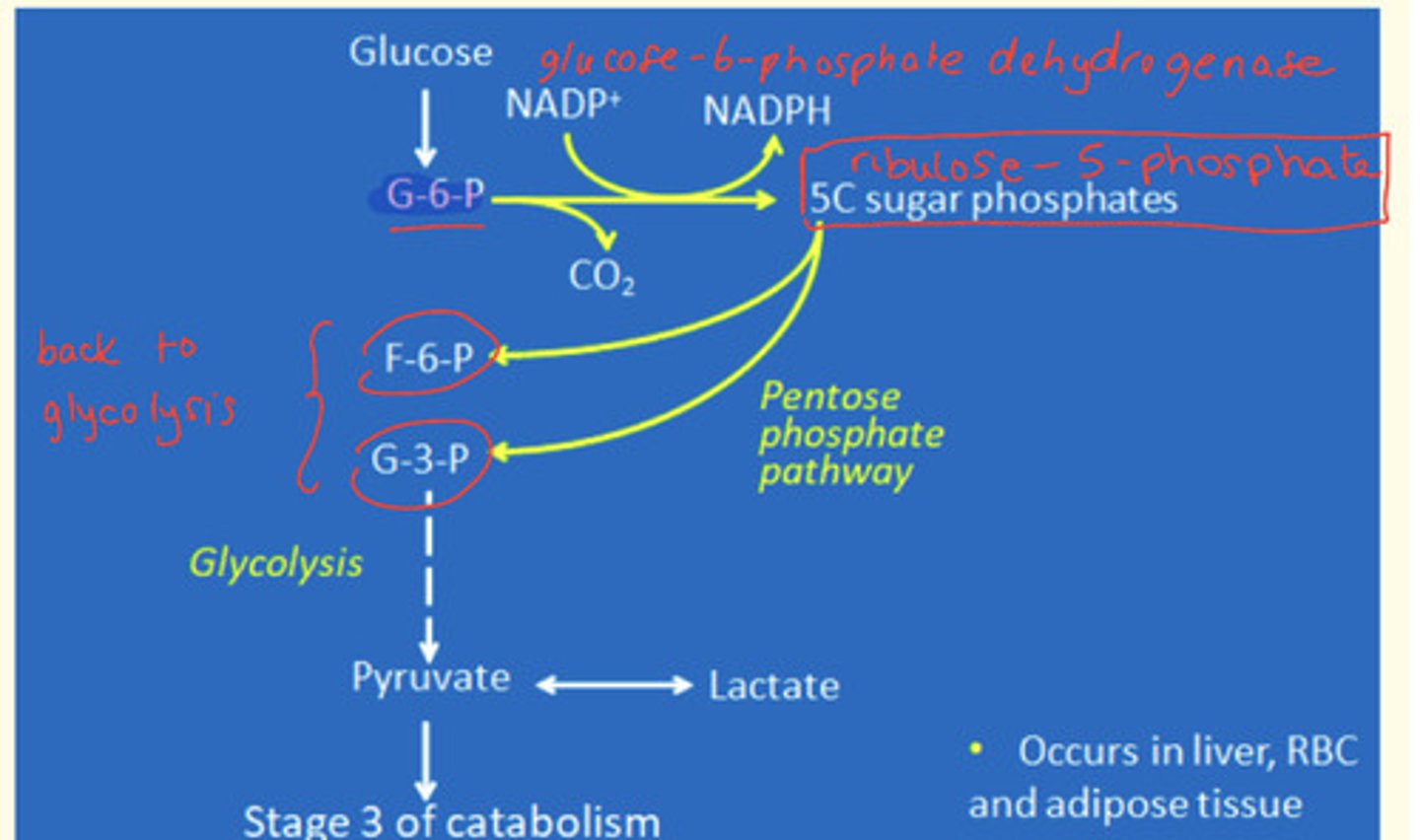
What are the primary functions of the pentose phosphate pathway?
Why is this pathway important?
- Production of NADPH+ and H+ (reducing power) = used in fatty acid synthesis in the liver, adipose tissue, lactating mammary glands. This also maintains a REDUCED state of GLUTATHIONE (GSH)
- Production of intermediates for glycolysis (fructose-6-phosphate; glyceraldehyde-3-phosphate)
- Production of C5 sugars for nucleotides in the nucleic acid synthesis (e.g. higher activity in dividing tissues like bone marrow)
What is the importance of the pentose phosphate pathway?
Provides NADPH+ and H+ reducing power which maintains a reduced state in glutathione (GSH) - this protects cells from oxidative damage via ROS and helps to maintain reduced states of sulfhydryl (SH) groups in proteins
What is G6PDH deficiency and its impact?
Glucose-6-phosphate dehydrogenase deficiency is a deficiency of the enzyme that catalyses the pentose phosphate pathway.
Impact:
- Reduced and low levels of NADPH+ and H+ produced (less reducing power)
- RBCs most severely affected as pentose pathway in these cells is the ONLY way of generating ATP (no mitochondria - no oxidative phosphorylation).
- Oxidative damage as glutathione is in an oxidised state (GSSG)
- Haemoglobin and other proteins become cross-linked by disulphide bonds (bridges) which are formed by oxidised S atoms (S-S)
What is the name of the insoluble aggregates formed from the cross-linking by disulphide bonds which are formed by oxidised S atoms (S-S) in RBCs (G6PDH deficiency)?
Heinz bodies
What happens when Heinz bodies attach to the RBC membrane?
Haemolysis by the spleen
What are the symptoms of G6PDH deficiency?
It is asymptomatic unless triggered by...
1. Certain chemicals in medications e.g. antimalarials (primaquine) or antibiotics
2. Certain foods e.g. fava beans
3. Infections
Haemolytic anaemia, fatigue, pale colour of skin (pallor), dyspnea (shortness of breath), jaundice
Where does the catabolism of galactose occur?
Liver
Name the reduced form of galactose that accumulates in tissues in galactosaemia
Galactitol
Name the metabolic pathway whose altering may lead to oxidative damage and the formation of Heinz bodies in erythrocytes
Pentose phosphate pathway
What is bilirubin?
a orange-yellow pigment formed in the liver by the breakdown of hemoglobin and excreted in bile
What does abnormally high levels of bilirubin in the blood lead to?
Excess bilirubin in the blood is known as 'hyperbilirubinemia'. This causes jaundice (yellow discolouration of the sclera and skin) resulting from accumulation of excess bilirubin in the body.
Propose an explanation for the presence of Heinz bodies in a patient's erythrocytes
Heinz bodies can be produced from glucose phosphate dehydrogenase deficiency (G6PDH) which is an important enzyme in the pentose phosphate pathway
In G6PDH deficiency - the enzyme activity is reduced.
This leads to low levels of [NADH + H+] or reducing power being produced.
The deficiency in RBCs leads to oxidative damage as glutathione is in an oxidised state (GSSG). Haemoglobin and other proteins become cross-linked by disulphide bridges which are formed by oxidised S atoms (S-S). These form insoluble aggregates known as 'Heinz bodies' that attach to RBC membranes - leading to haemolysis by the spleen.
Can anaemia and jaundice be related - how?
Anaemia causes the red blood cells (erythrocytes) to be degraded - and a product of haemoglobin degradation is a pigment of haem called bilirubin which when accumulates in the blood, leads to jaundice (yellowing of the sclera and skin).
What is the role of glucose-6-phosphate dehydrogenase enzyme?
Enzyme that catalyses first step of the pentose phosphate pathway
Why cant people with glucose 6 phosphate dehydrogenase deficiency (G6PDH) take antimalarial drugs such as primaquine and foods such as fava beans?
People with G6PDH deficiency struggle to produce enough NADPH in the Phosphate Pentose Pathway (PPP).
NADPH is needed to maintain glutathione protein in a reduced state which protects the RBC from oxidative damage by ROS - that's what help keeps the structure of the RBC intact.
Primaquine oxidises glutathione which leads to oxidative damage of the RBC - which leads to the production of Heinz bodies.
Is galactose a normal constituent of urine?
No
How could you account for the presence of galactose in a patient's urine?
- Blood concentration above the renal threshold of 8-9 mmol/L
- Kidney damage
What are the metabolic consequences of an absence of galactose-1-phosphate uridyl transferase enzyme?
Galactose and galactose-1-phosphate accumulate in the blood and tissues and enters abnormal pathways of metabolism (formation of galactitol).
Why do galactosaemic patients develop cataracts?
When the lens proteins (crystallins) are cross-linked - the lens becomes opaque (cataract).
Are the metabolic consequences of an absence of galactokinase similar to those of an absence of galactose-1-phosphate uridyl transferase?
No - metabolic consequences of absence of galactokinase are less severe as ONLY galactose accumulates. Patients suffer from cataracts but NOT liver, brain, GI tract or kidney problems.
What is standard treatment of a patient with galactosaemia
Dietary restriction of galactose/lactose (dairy free diet).
Replace with artificial milk e.g., soya bean
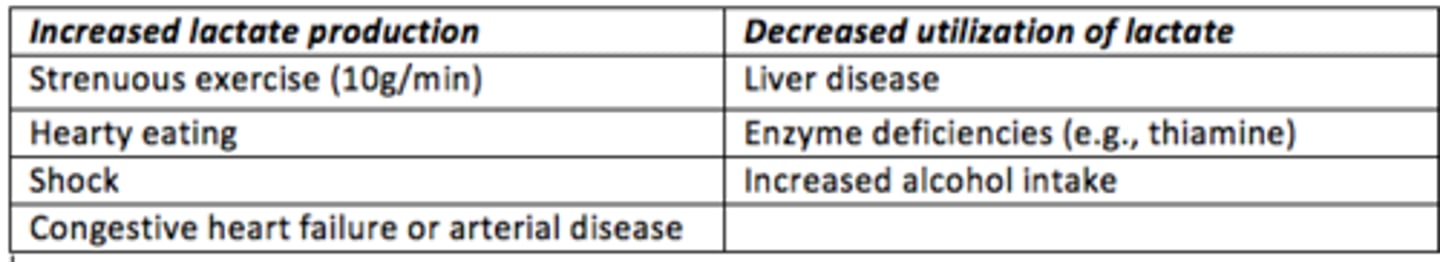
Define lactic acidosis and why it may occur
Lactic acidosis is the elevation of lactate that affects the buffering capacity of the plasma (i.e., there is a fall in plasma pH due to accumulation of lactic acid).
Increased lactate can be due to increased lactate production during e.g., strenuous exercise (up to 10g/min), hearty eating, shock and congestive heart disease.
Increased lactate can also be due to decreased utilisation of lactate which occurs during e.g., liver disease, enzyme deficiencies (thiamine deficiency), and increased alcohol intake
Case study
A male infant aged 4 weeks was admitted to hospital. He was a small, and lethargic baby with hepatomegaly and splenomegaly; jaundice was absent on admission, but had been observed the week prior. One week later urine and blood were positive for galactose.
Galactose-1-phosphate uridyltransferase (GPT) were present in the blood at low levels. At 8 weeks ocular examinations revealed faint central opacity and a difference in light refraction in the left eye.
What’s the diagnosis?
Galactosaemia
Case study
21-year-old male, working as a tour guide was admitted to A&E because of severe jaundice. History revealed he had taken as a prophylactic measure, an antimalarial, Primaquine, to protect himself. The day after intake of Primaquine he noticed yellowish discolouration of his face progressing down to the lower extremities.
Past history revealed a previous admission when he was 12 years old for the same complaint, when he was given Sulphonamides for a UTI.
Laboratory examinations revealed low haemoglobin, RBC’s showed Heinz Bodies.
What’s the diagnosis?
G6PDH deficiency
How much lactate is produced every day WITHOUT exercise?
40-50g/day
In what pathological situations is lactate production common?
- Shock
- Congestive heart disease
- Arterial disease
Examples of situations in which production of lactate is elevated
- Strenuous exercise
- Hearty eating
- Shock
- Congestive heart disease
- Arterial disease
Examples of situations in which production of lactate is depleted
- Liver disease
- Vitamin deficiencies (e.g., thiamine)
- High alcohol intake
Hyperlactatemia
2-5 mM in blood, below renal threshold, no change in blood pH
Lactic acidosis
>5 mM in blood, above renal threshold, blood pH is lowered
Which are the three regulatory steps of glycolysis?
Reactions 1, 3 and 10
Reaction 1 = Hexokinase
Reaction 3 = Phosphofructokinase
Reaction 10 = Pyruvate kinase