disorders of the liver - lecture 24
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
46 Terms
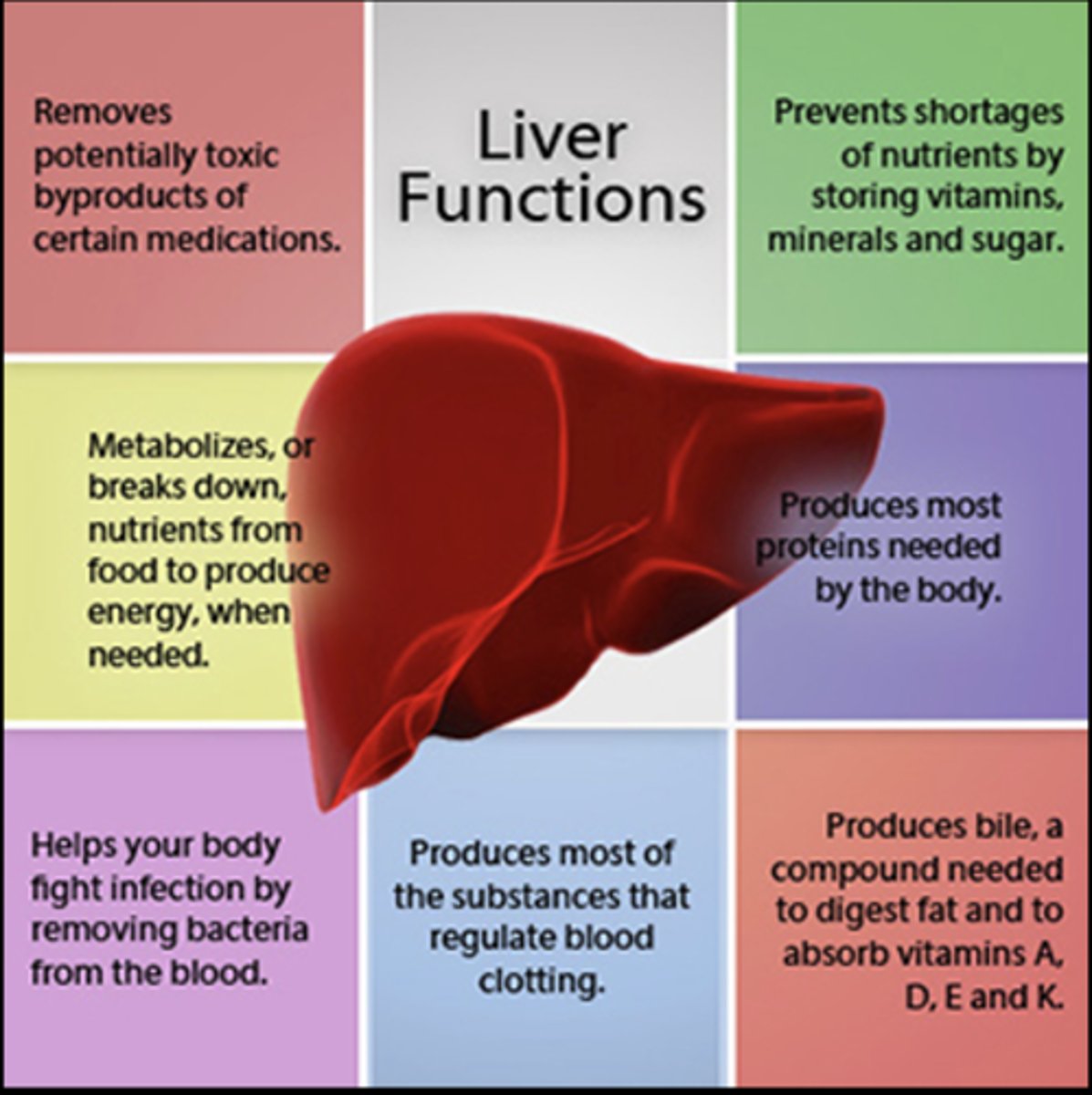
liver function
liver function
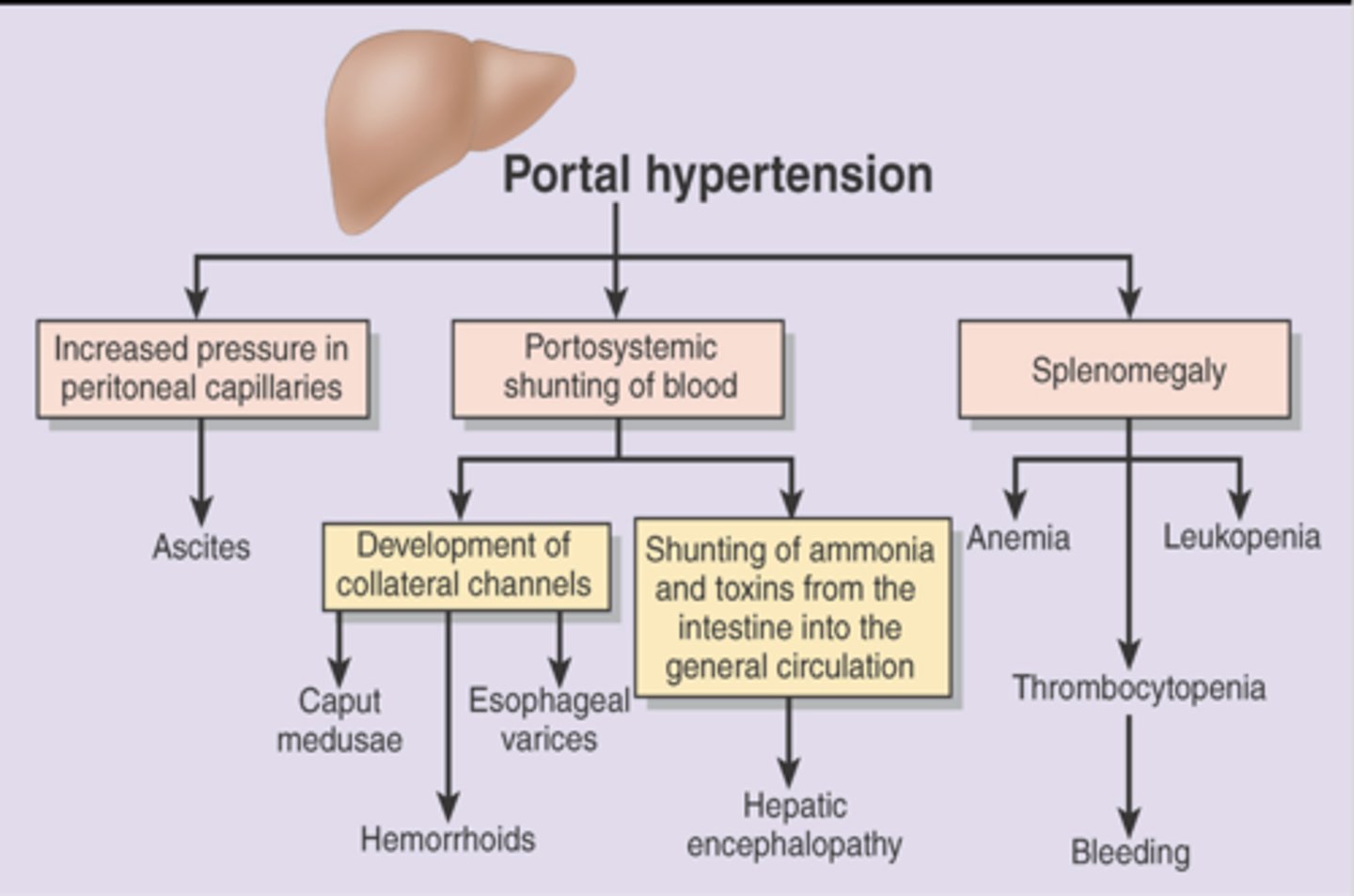
Manifestations of Liver Disease (Portal Hypertension)
Abnormal high blood pressure in the portal venous system due to resistance to portal blood flow
–Causes
- Liver damage
- Liver disease (main cirrhosis)
Consequences
- Varices
- Lower esophagus, stomach, rectum
- Splenomegaly
- Ascites
-Hepatic encephalopathy
Treatment
- Preventing or managing the complications
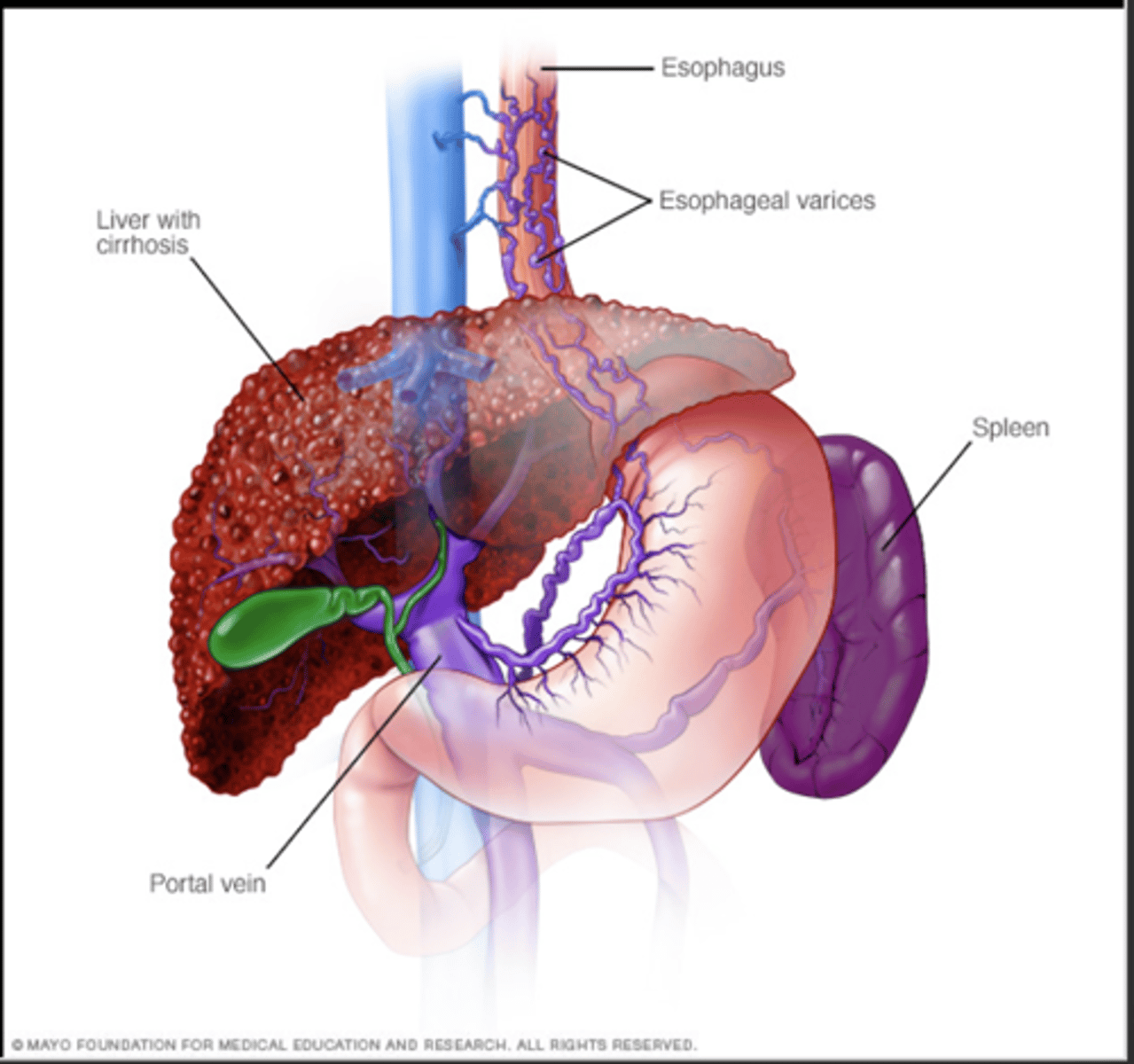
Portal Hypertension Consequences
Portal Hypertension Consequences
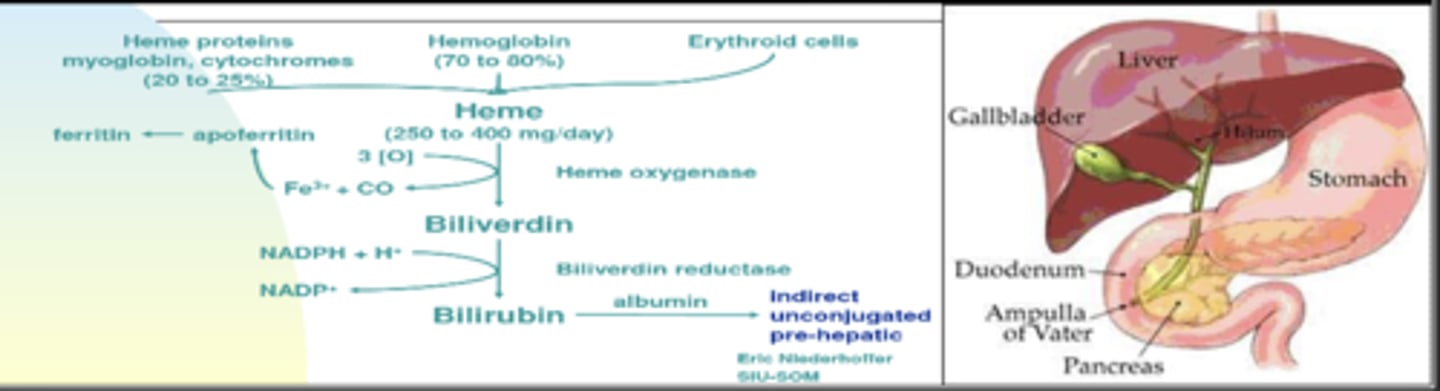
Manifestations of Liver Disease(Jaundice or Icterus)
Excess bilirubin
Water insoluble product of heme metabolism (unconjugated bilirubin)
Taken up by liver and conjugated to become water soluble so it can be excreted in bile and into bowel
Patient looks Jaundiced if total bilirubin >2.5 (unconjugated + conjugated – normal 0.3-1)
*If patient is vomiting GREEN, then they have bowel obstruction below the level of the Ampulla of Vater (sphincter of oddi exit)
Obstructive jaundice
Intrahepatic obstruction
Extrahepatic obstruction
Hemolytic jaundice
Prehepatic jaundice (increase unconjugated bilirubin)
-- Excessive hemolysis of red blood cells or absorption of a hematoma
Pathophysiologic Consequences of Liver Disease
Changes in protein synthesis
Changes in exocrine gland function:
A.Cholesterol – only site of cholesterol excretion is bile. Excess may lead to formation of gallstones
B.Bile Acids – markers of both liver and small bowel function
C.Bilirubin – conjugated/unconjugated ratio in plasma indication of type of liver malfunction
D.Blockage of bile ducts leads to reflux of bile into plasma (jaundice, nausea, skin itching, and even cognitive impairment)
hepatitis
Causes:
–Viral infections (common)
–Alcohol use disorder (AUD)
–Drug toxicity
–Autoimmune disorders
Chronic hepatitis (liver inflammation for more than 6 months)
-- Main cause of chronic liver disease, cirrhosis, and hepatocellular cancer
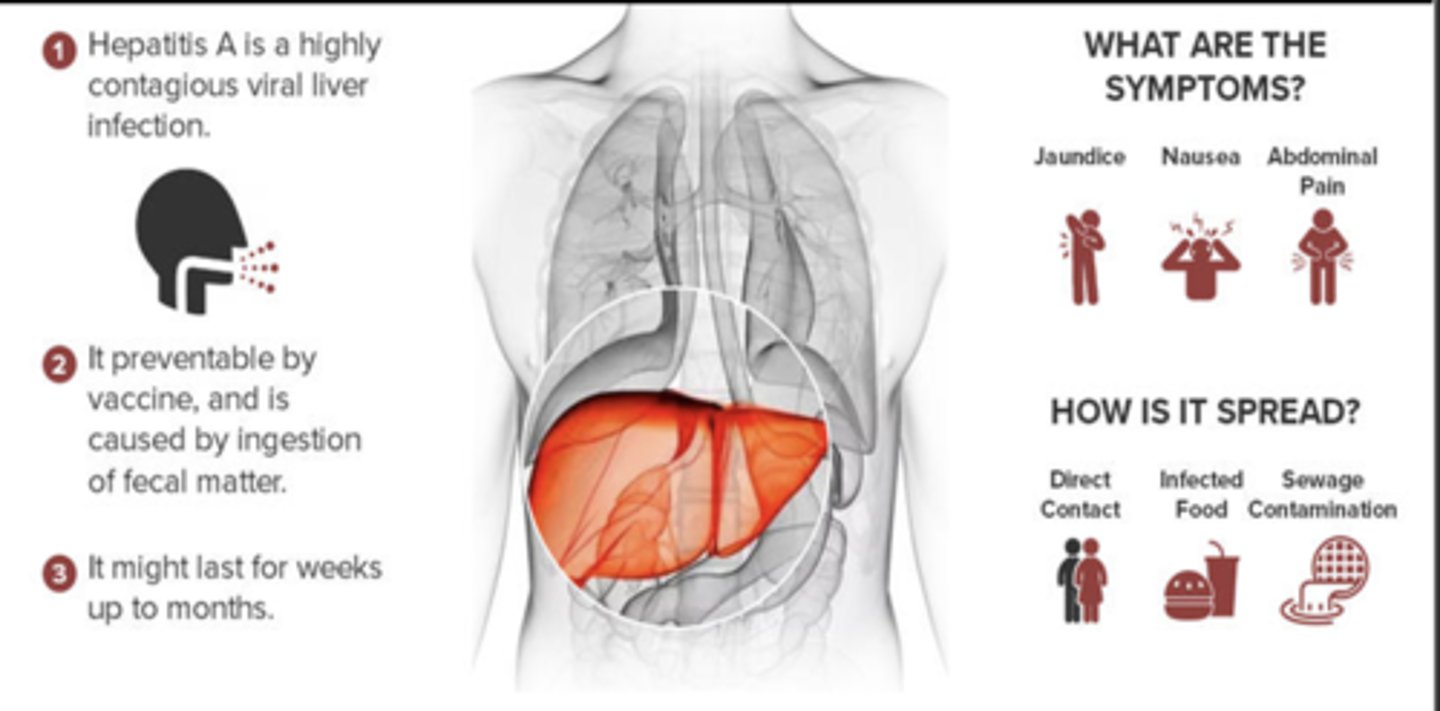
hepatitis A
hepatitis A
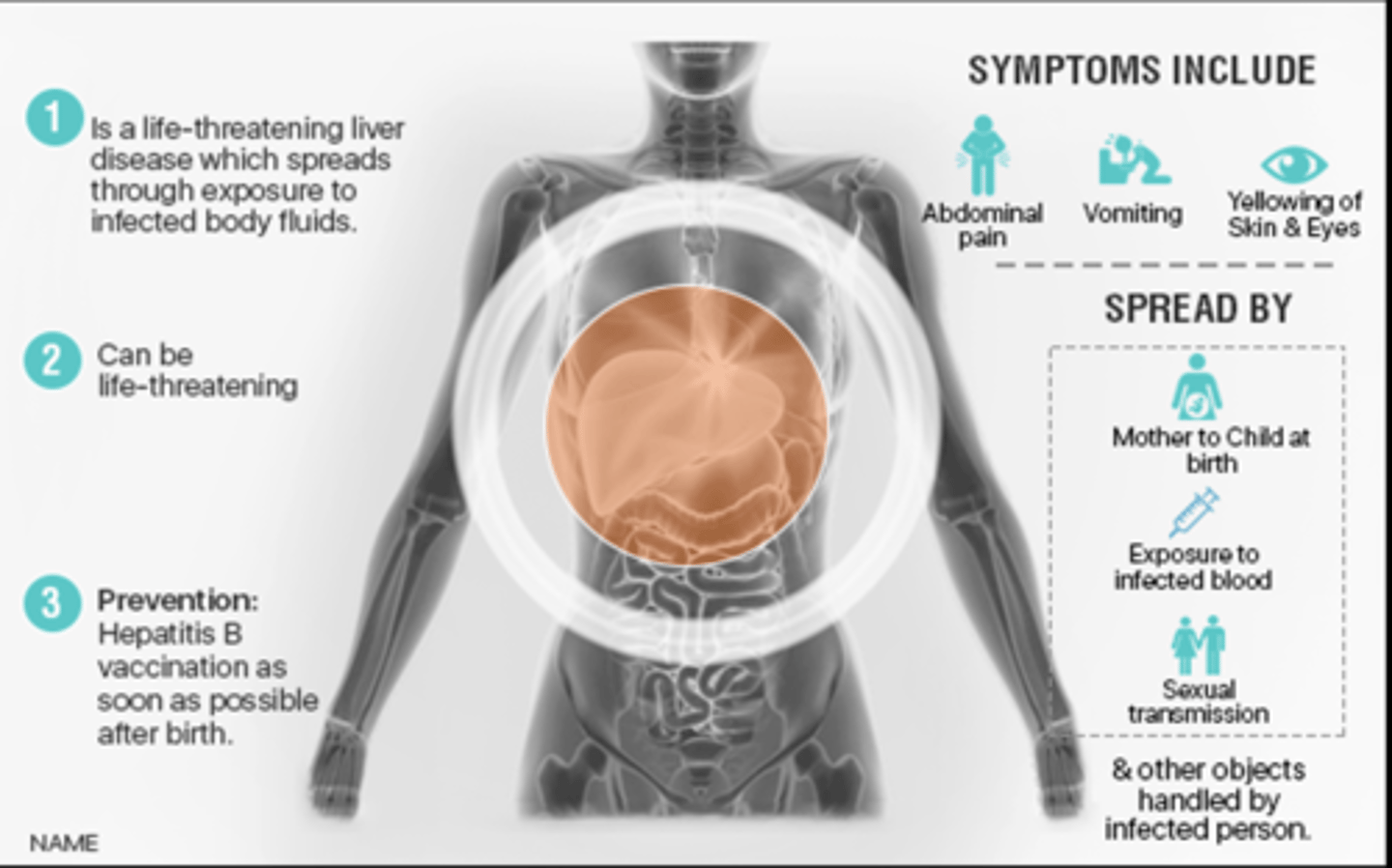
hepatitis B
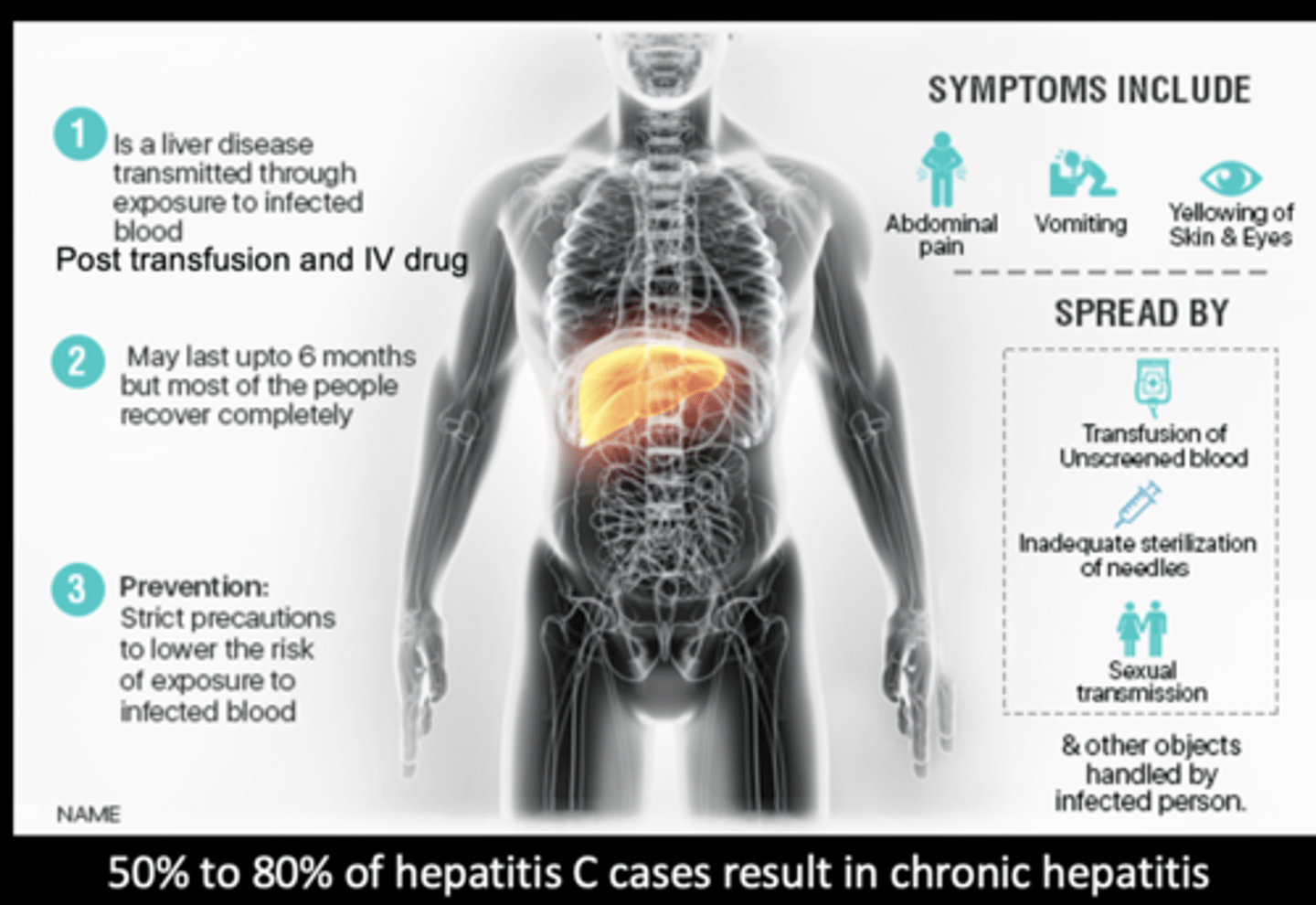
hepatitis C
hepatitis C
Hepatotoxicity
the leading cause of acute liver failure in the US
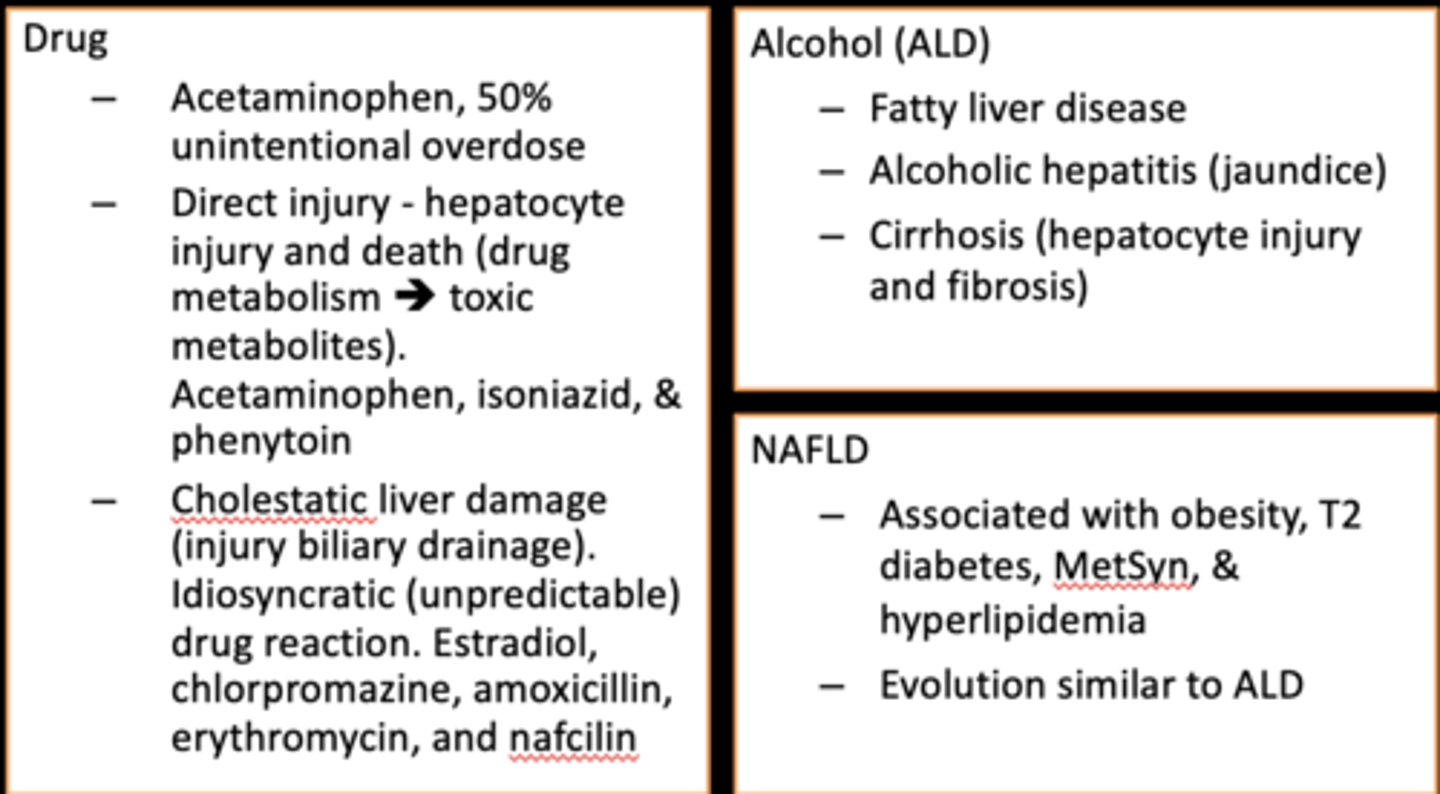
Drug, Alcoholic, and Nonalcoholic Liver Disease
Drug, Alcoholic, and Nonalcoholic Liver Disease
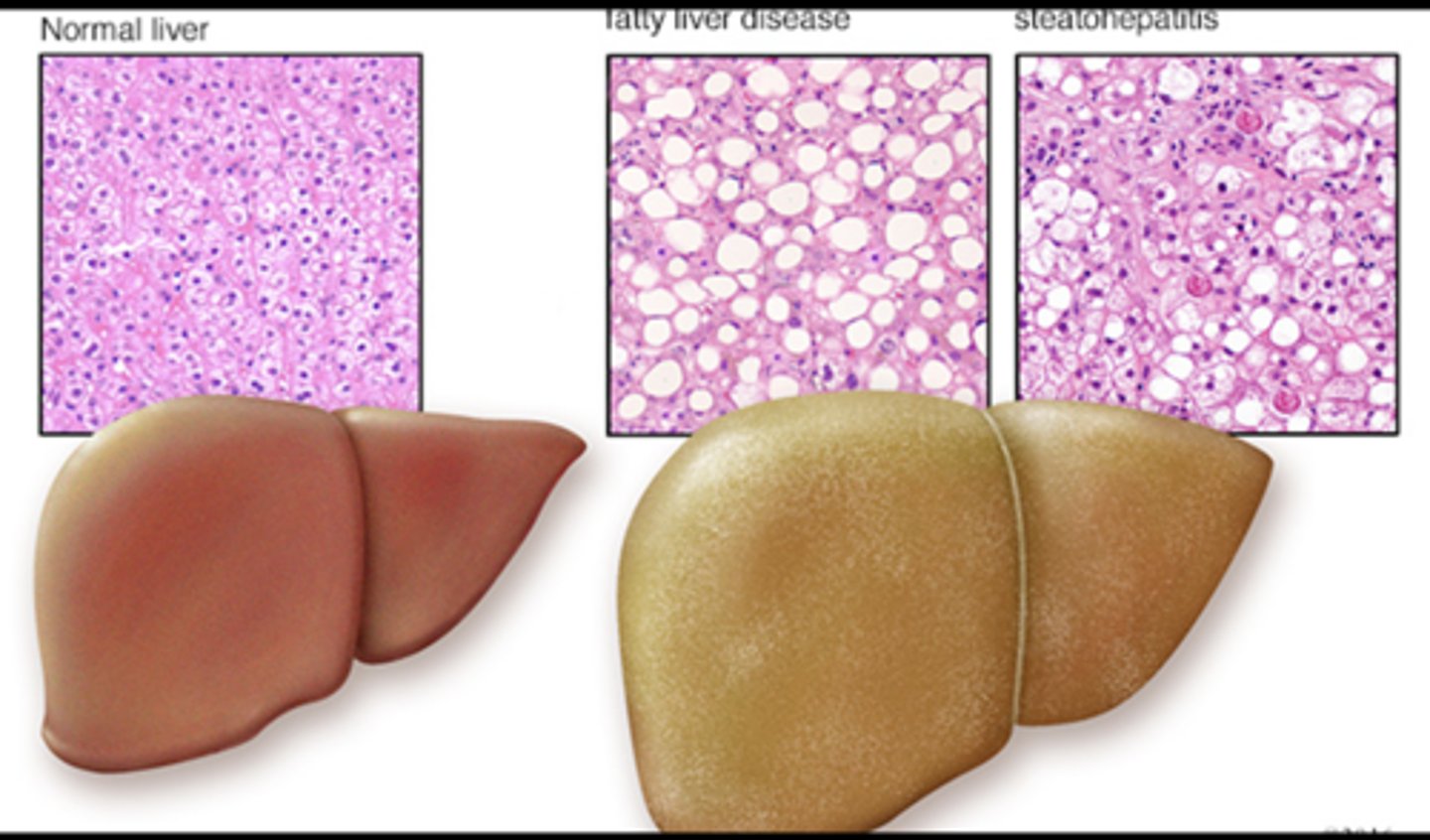
cirrhosis
Final, common end-stage for a variety of chronic liver diseases
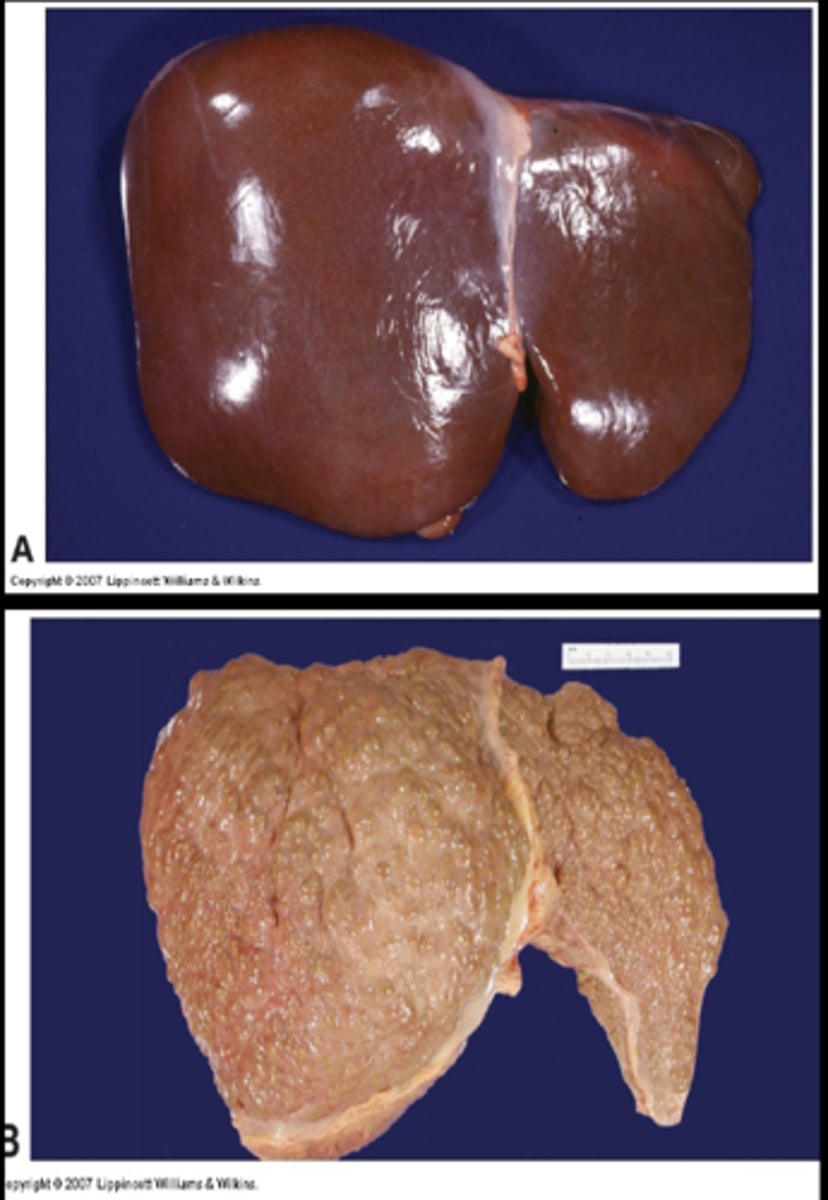
cirrhosis
1.Irreversible inflammatory disease
2. decrease hepatic function due to fibrosis
Alcoholic
-- The oxidation of alcohol damages hepatocytes
Biliary (bile canaliculi)
-- Cirrhosis begins in the bile canaliculi and ducts
-- Primary biliary cholangitis (PBC-autoimmune cirrhosis)
-- Secondary biliary cirrhosis (obstruction)
Postnecrotic
-- Consequence of chronic disease (hepatitis B and C, PBC)
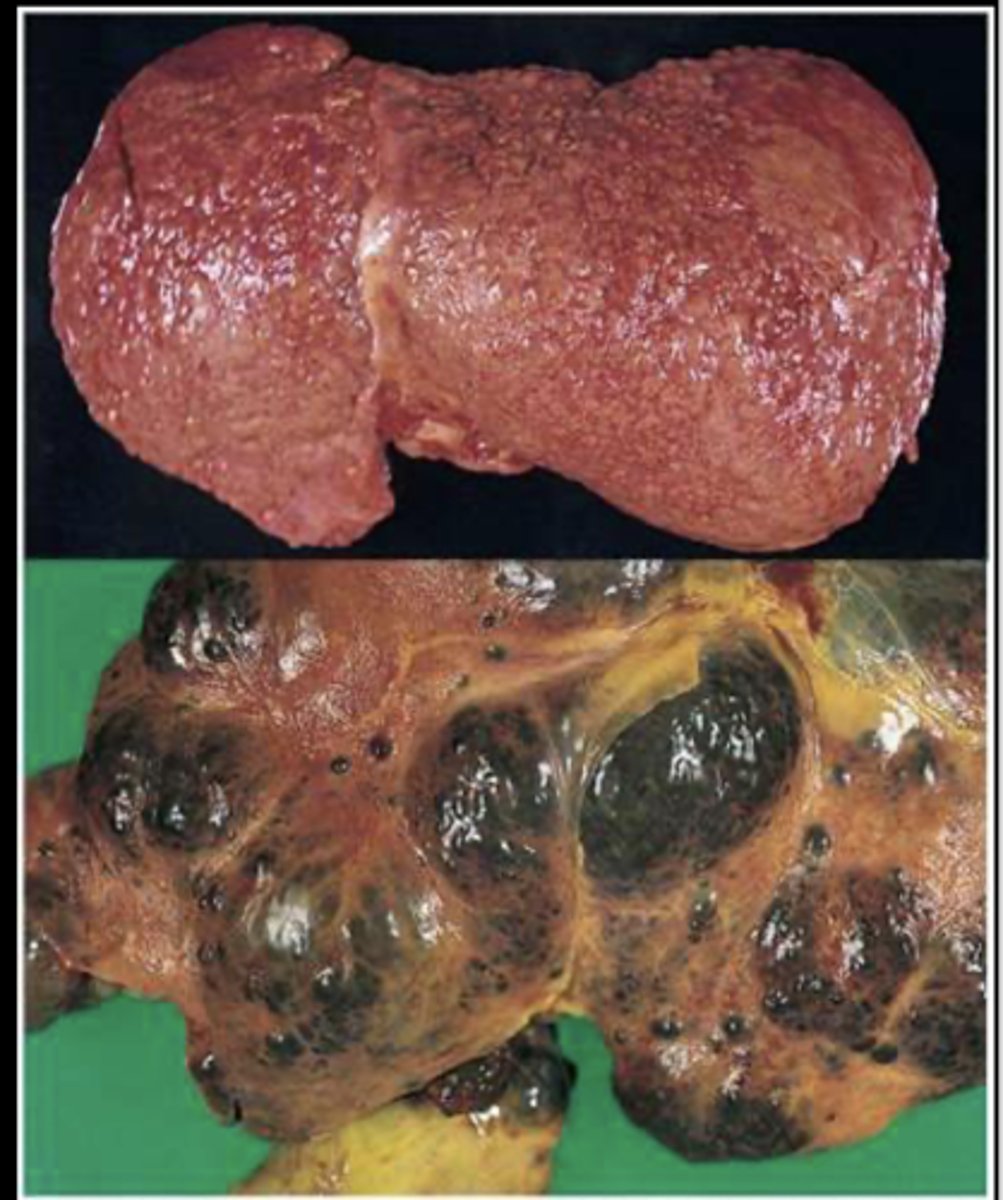
hepatic failure
Die within a few weeks or months
May be sudden injury or chronic injury
Loss of 90% of function
Clinically:
- jaundice
- ascites
- fetor hepaticus (ammonia and ketones in breath)
- hypoalbuminemia
- hypoglycemia
- palmar erythema
- spider angiomata
- testicular atrophy
- balding
- gynecomastia
- bleeding disorders
- hepatorenal syndrome
- hepatic encephalopathy (cells in the nervous system are vulnerable to neurotoxins absorbed from the GI tract that, due to liver dysfunction, circulate to the brain)
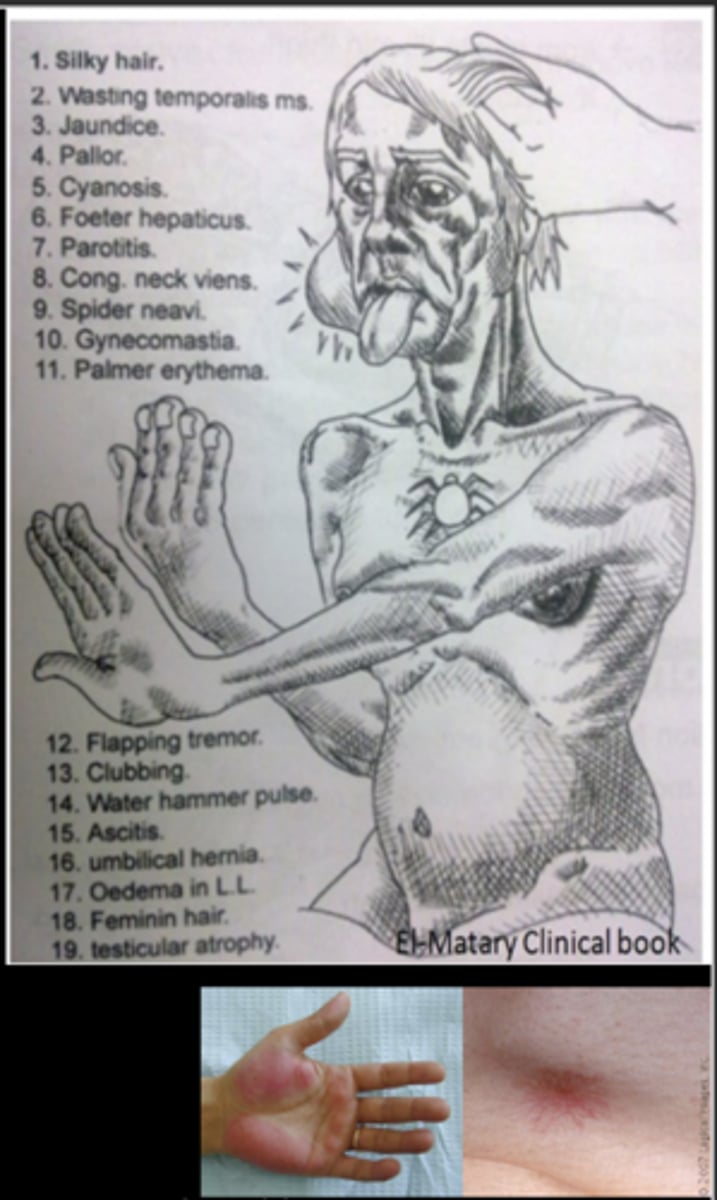
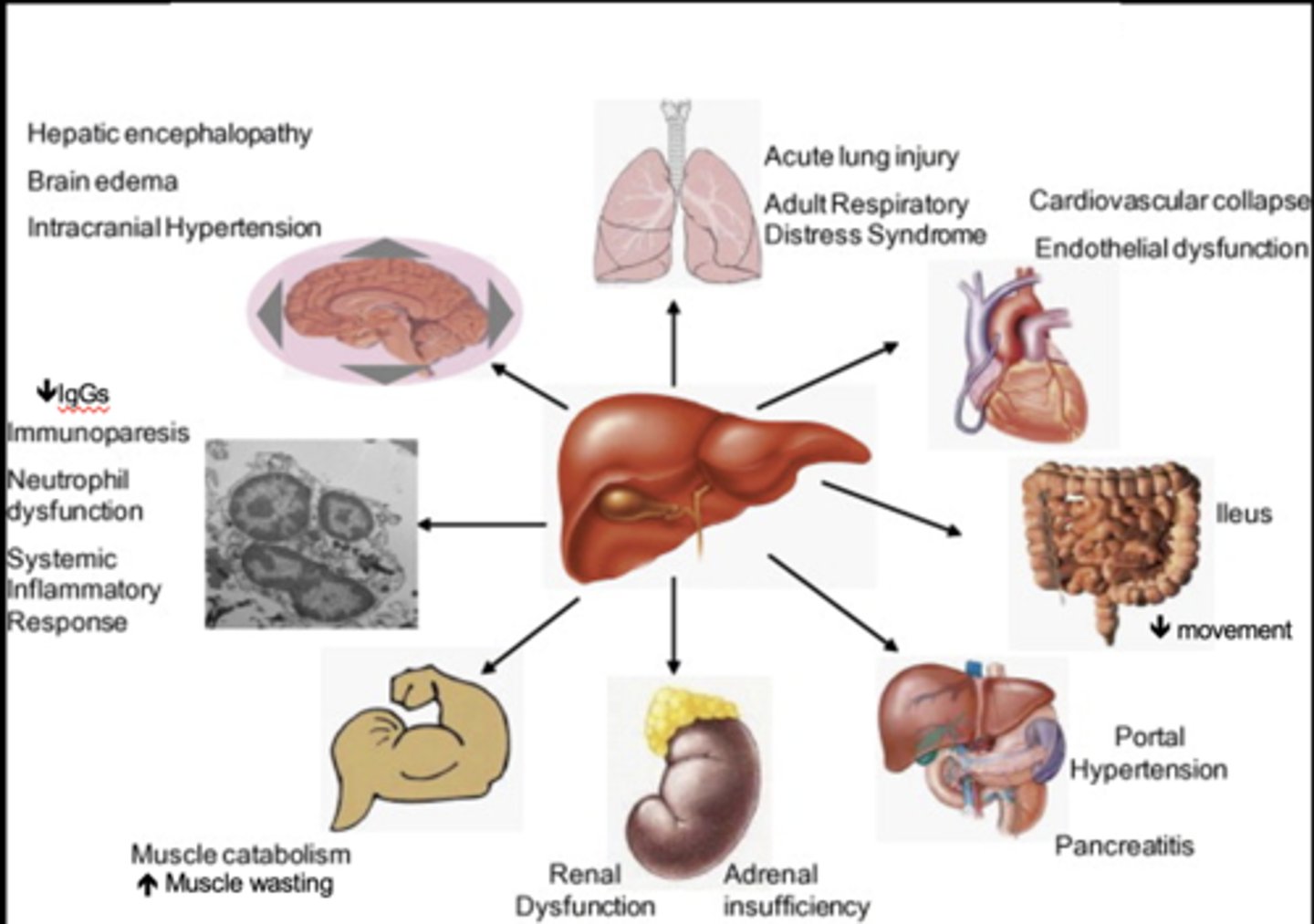
Systemic Manifestations of Liver Failure
Systemic Manifestations of Liver Failure
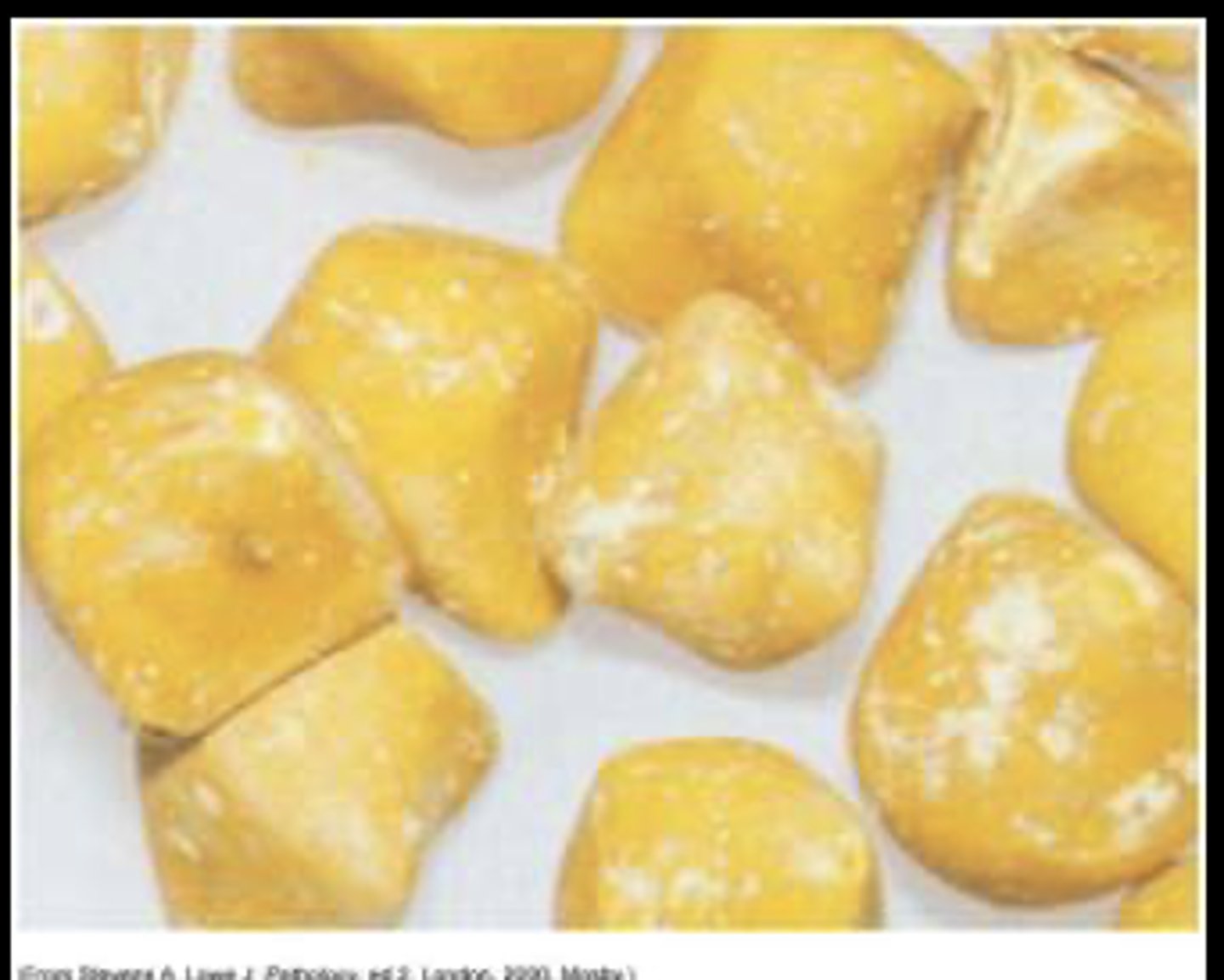
gallstones
Obstruction or inflammation (cholecystitis) is the most common cause of gallbladder problems
Cholelithiasis—gallstone formation
Types
-- Cholesterol (most common) and pigmented (consequence of cirrhosis)
Risks
-- Obesity, middle age, female, Native American ancestry, and gallbladder, pancreatic, or ileal disease
Interesting Facts in Pancreatic Disease
Interesting Facts in Pancreatic Disease
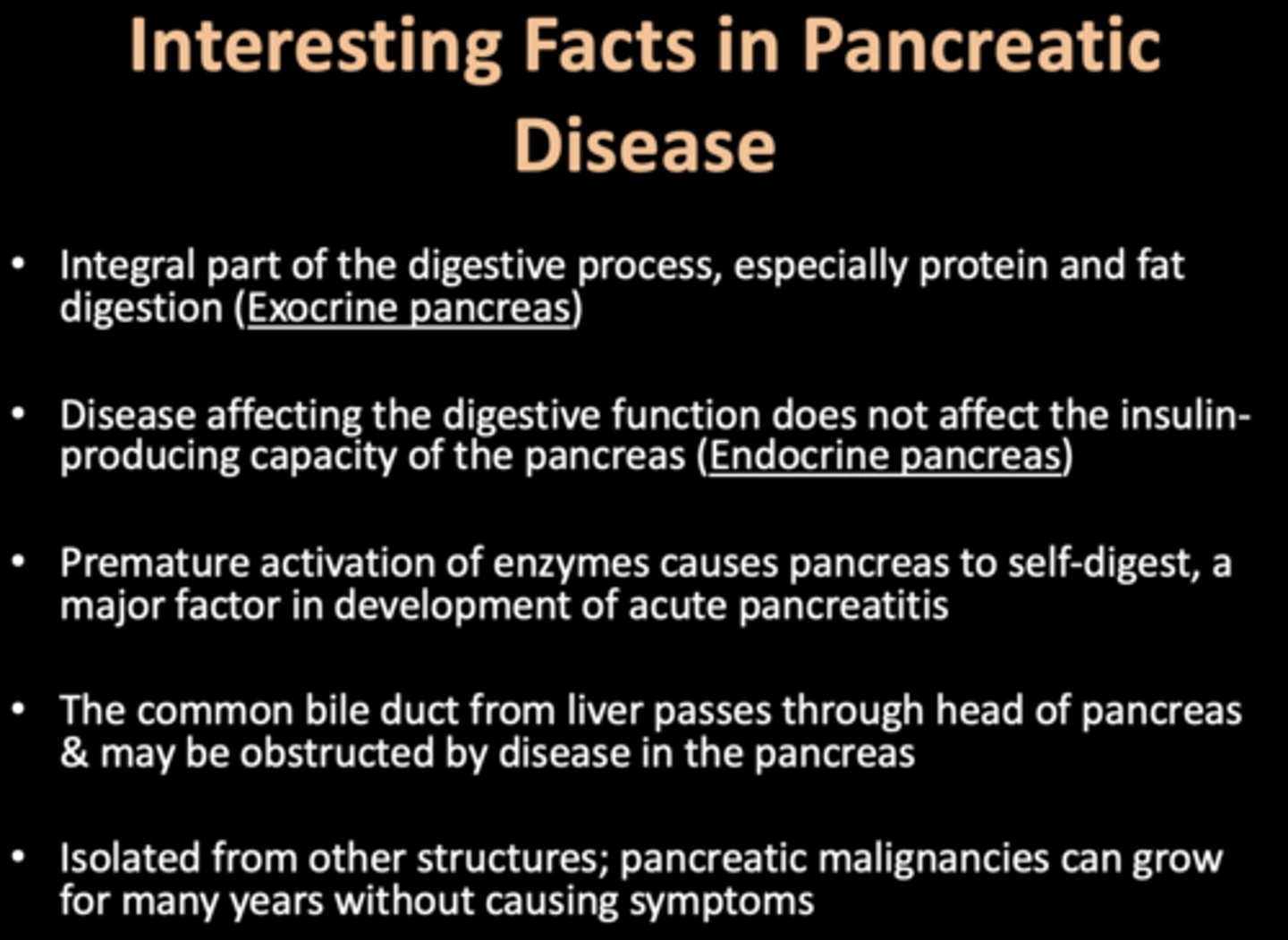
Proteolytic
________ enzymes secreted in the inactive form (zymogens)
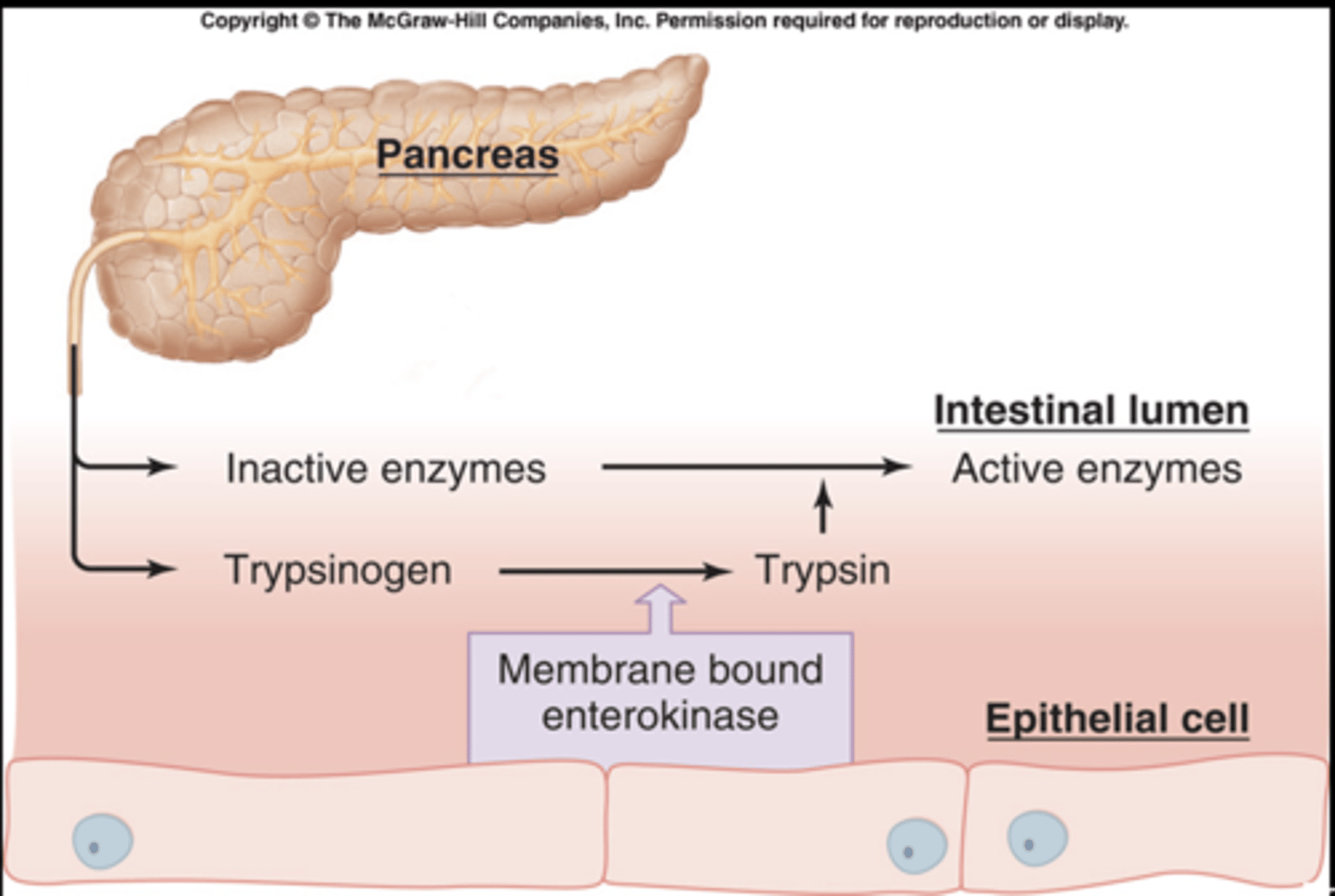
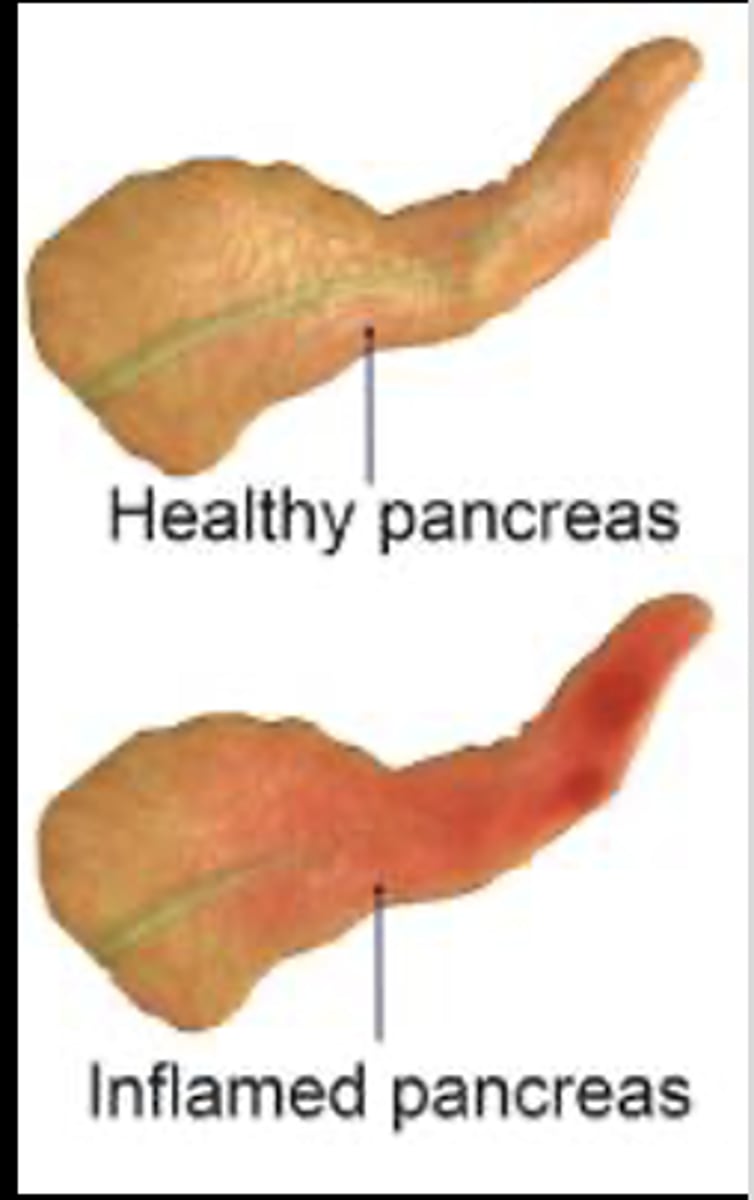
Pancreatitis
Inflammation of the pancreas
Associated with several other clinical disorders
-- Caused by an injury or damage to pancreatic cells and ducts, causing a leakage of pancreatic enzymes into the pancreatic tissue
These enzymes cause auto-digestion of pancreatic tissue and leak into the bloodstream to cause injury to blood vessels and other organs
Risk Factors for pancreatic disorders
Longstanding biliary disease from cholelithiasis, excessive alcohol ingestion, hypertriglyceridemia Most common cause: alcohol!
Autoimmune pancreatitis
is uncommon and accounts for less than 1% of cases of chronic pancreatitis
pancreatitis
Manifestations and evaluation:
- Epigastric pain radiating to the back
- Fever and leukocytosis
- Hypotension and hypovolemia
- Enzymes increase vascular permeability
- Characterized by an increase in a patient’s serum amylase level
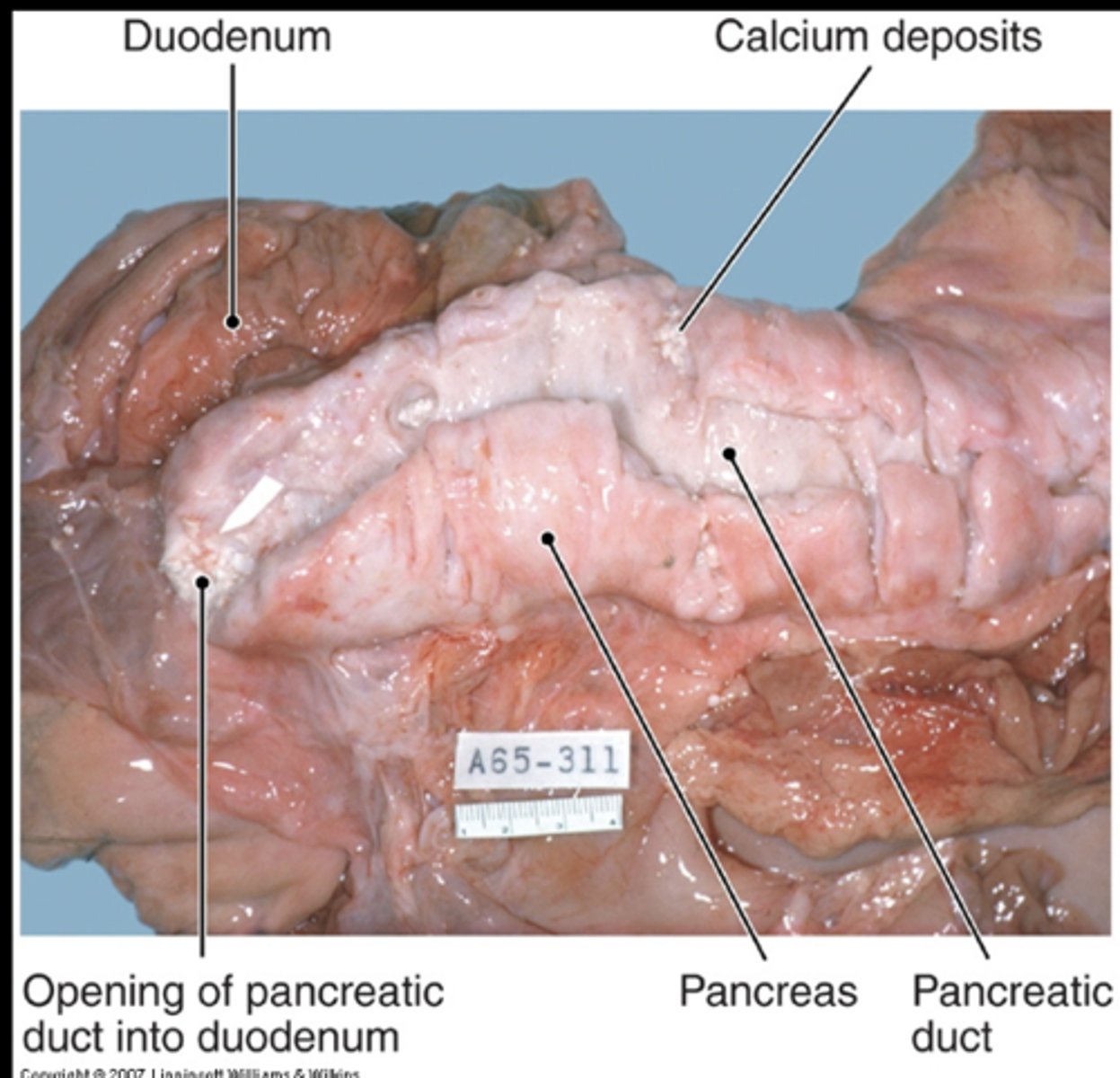
Chronic pancreatitis
- Mostly related chronic alcohol abuse
Cullen sign
bluish discoloration around umbilicus resulting from blood in peritoneal cavity b/c of hemorrhagic pancreatitis

Grey-Turner sign
reddish-brown discoloration along flanks resulting from retroperitoneal blood dissecting tissue planes

Acute Pancreatitis
Acute Pancreatitis

Chronic Pancreatitis
About 2/3 of cases due to chronic alcoholism, the remainder usually have no known cause
Gallstones are not involved
About ½ have evidence of prior acute pancreatitis
Dense scar tissue, dilated ducts, gritty calcification
Could render patient diabetic
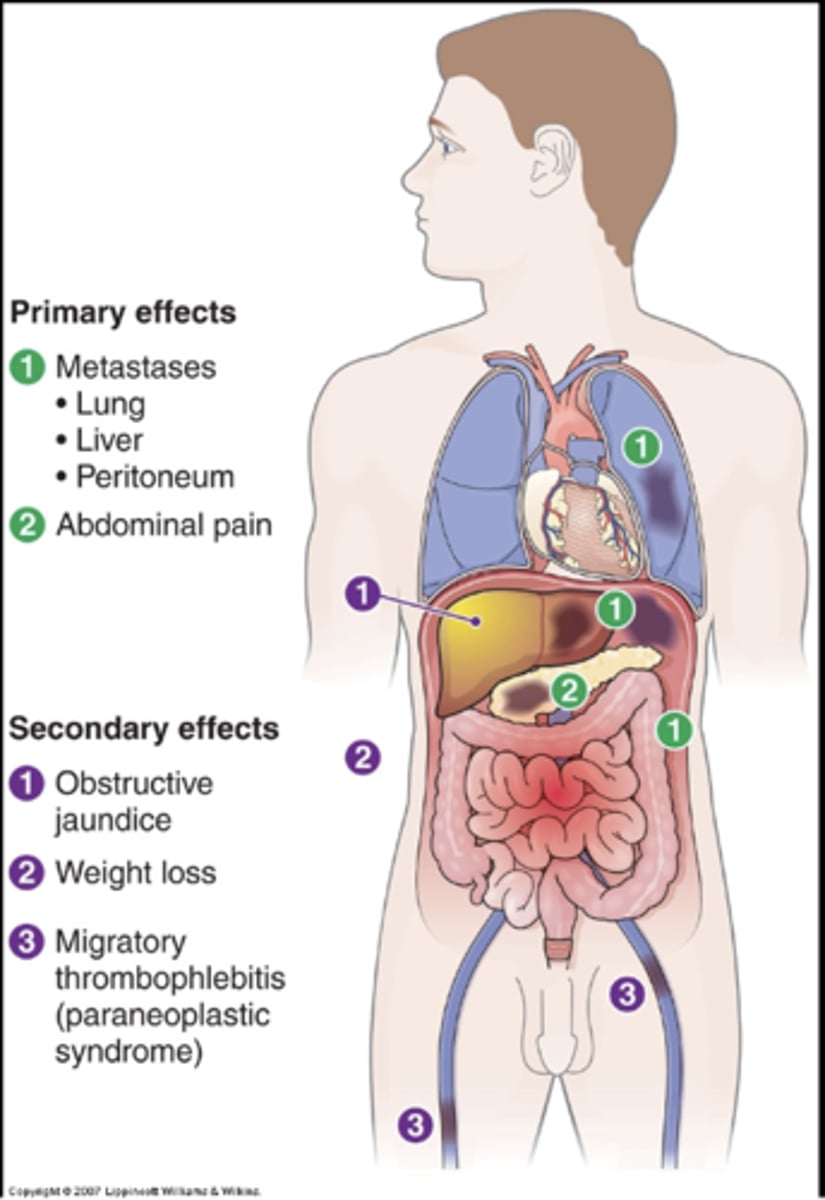
Pancreatic Carcinoma
Adenocarcinomas that arise in the ducts
Common
Usually older adults
Insidious
Know little about cause except that smokers 2X as likely to develop as nonsmokers
Most arise in the head & can obstruct the common bile duct
Those in the body & tail can be quite large by the time they are detected
½ die within 6 weeks of diagnosis
About 10% live a year
1% survive 5 years
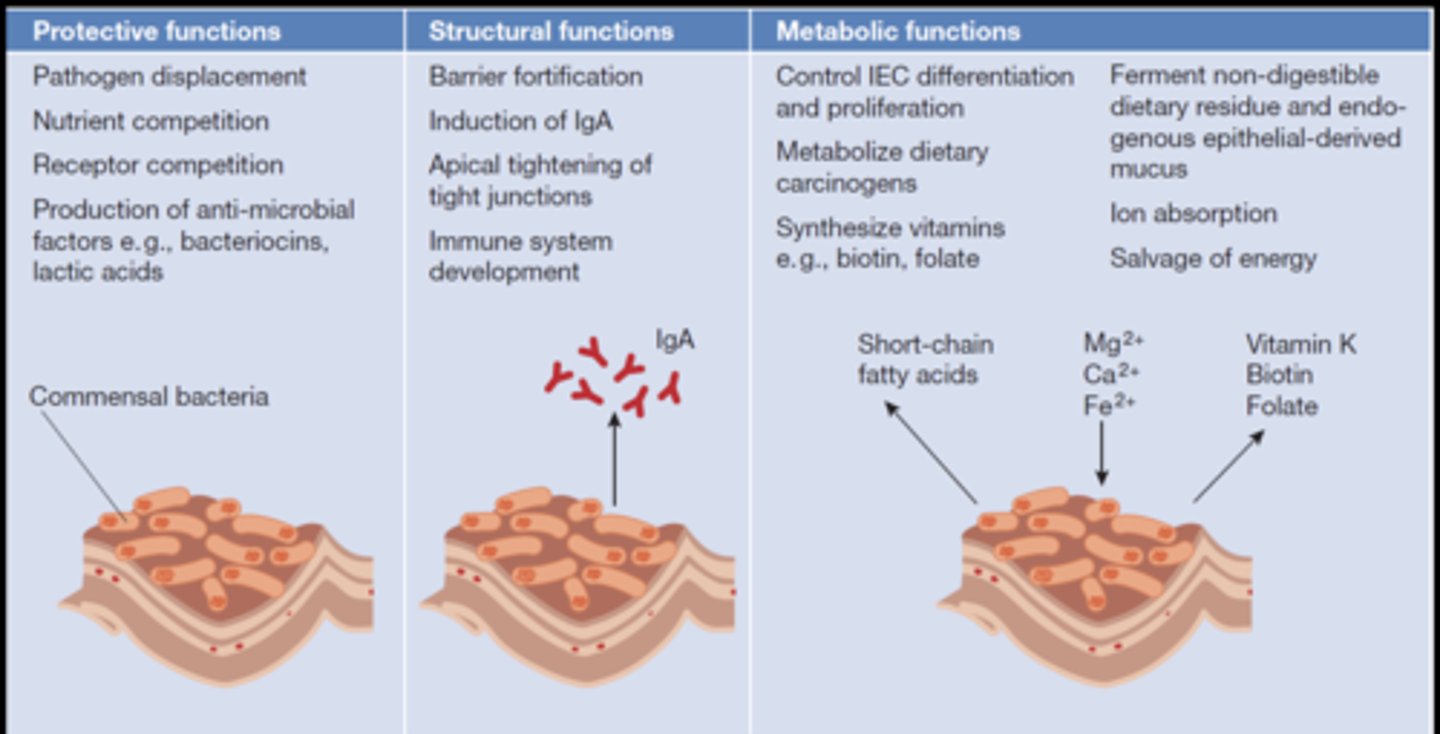
Functions of “good” gut flora
Functions of “good” gut flora
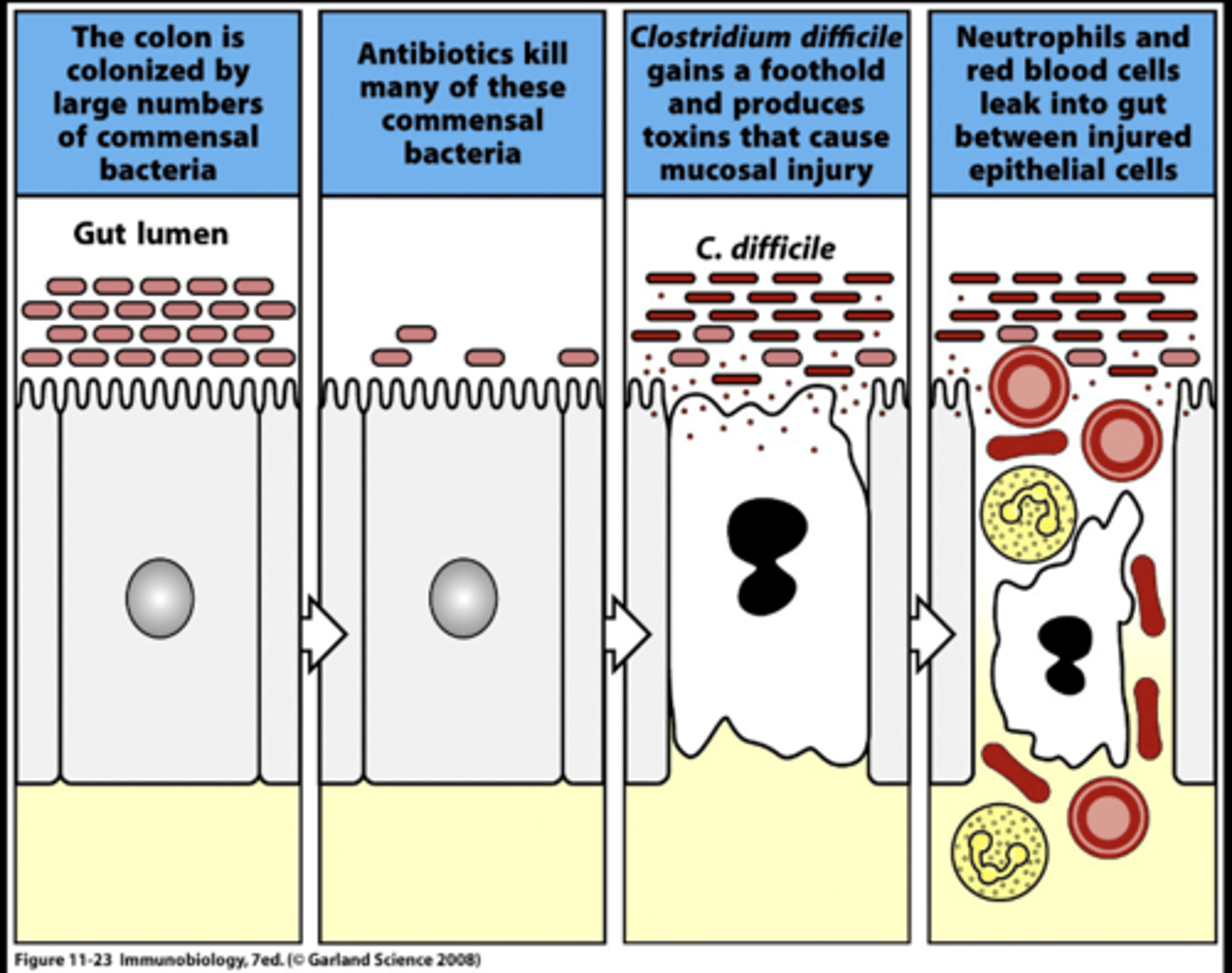
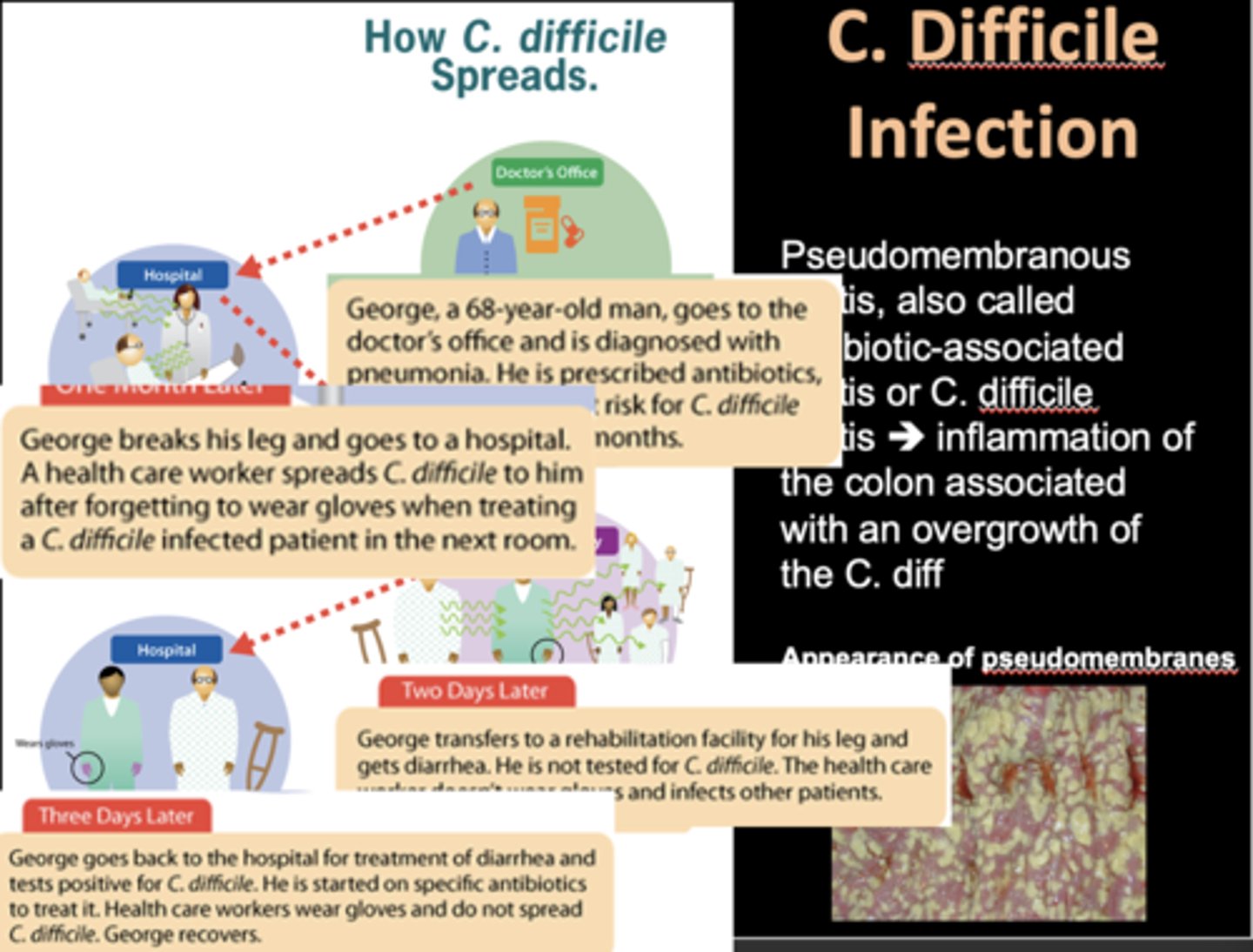
Chlostridium Difficile Infection
C. Difficile diarrhea - inflammatory diarrhea
Persistent infection following antibiotic treatment
Frequent relapse rate
Development of pseudomembranous colitis
Cause of death of 30,000 people
Chlostridium Difficile Infection
Chlostridium Difficile Infection
fecal transplant
fecal transplant

Bacteriotherapy!
Bacteriotherapy!
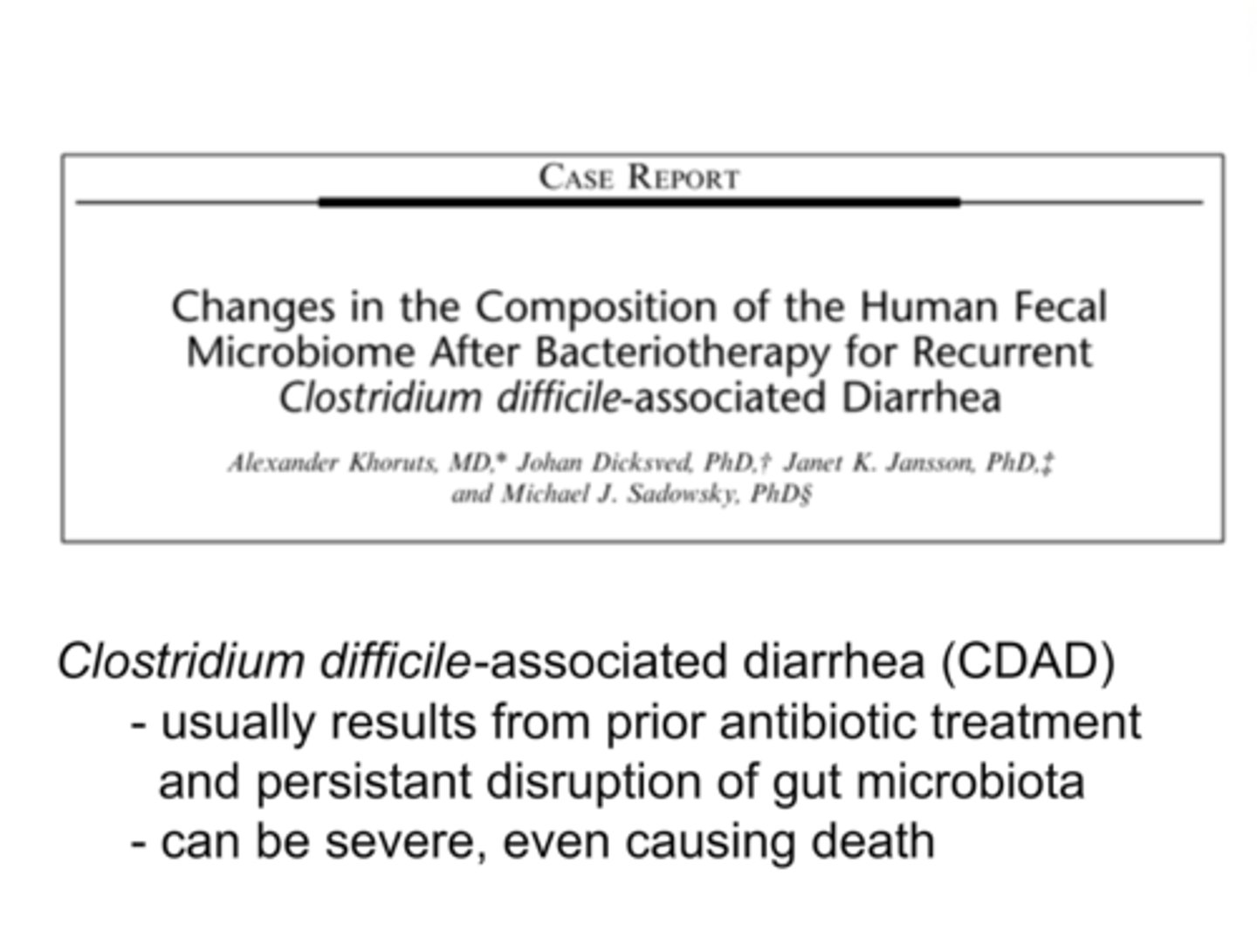
Fecal Microbiota Transplantation
Fecal Microbiota Transplantation
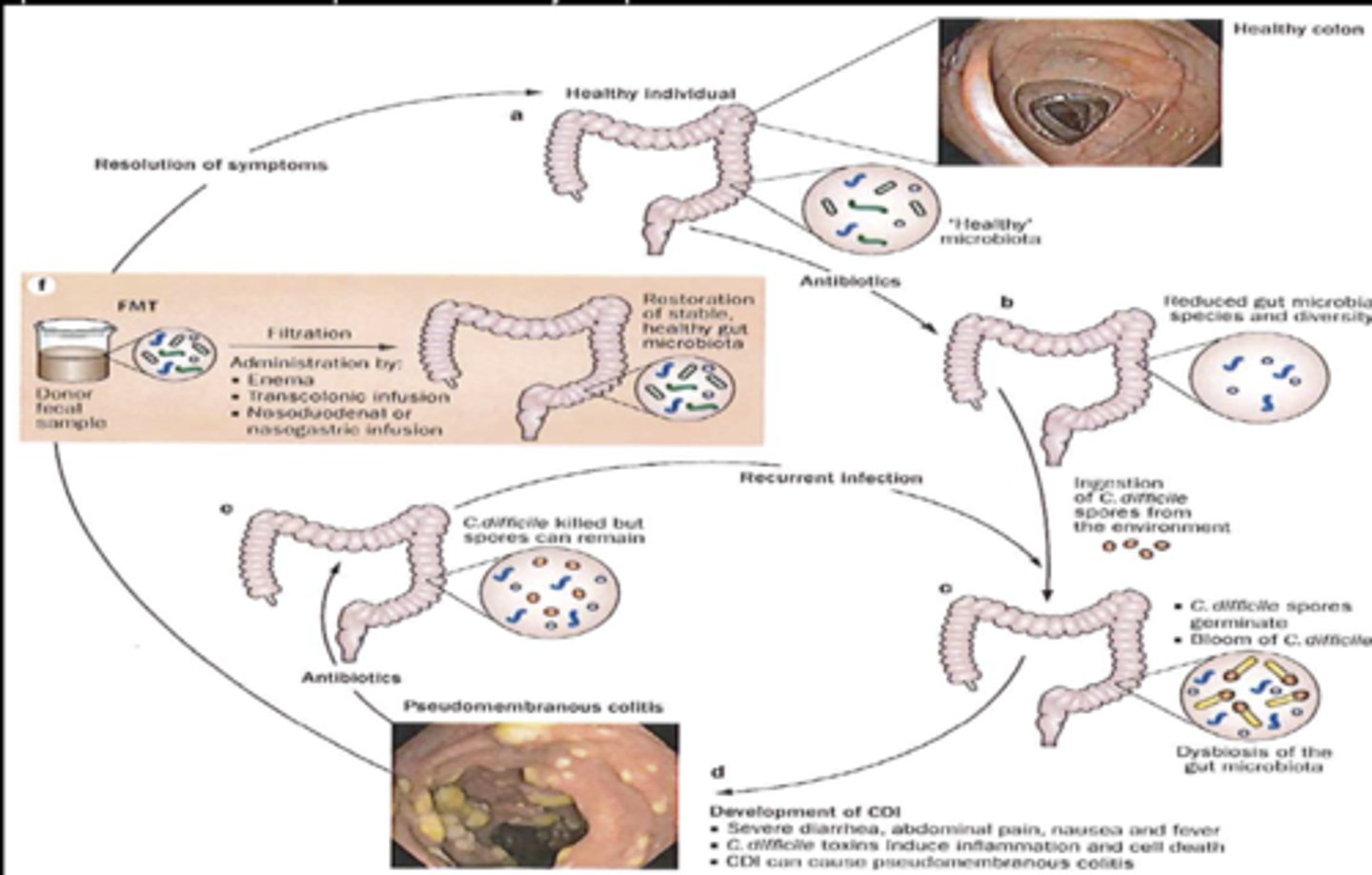
Bacteriotherapy – Patient 01
Bacteriotherapy – Patient 01

poop in a pill
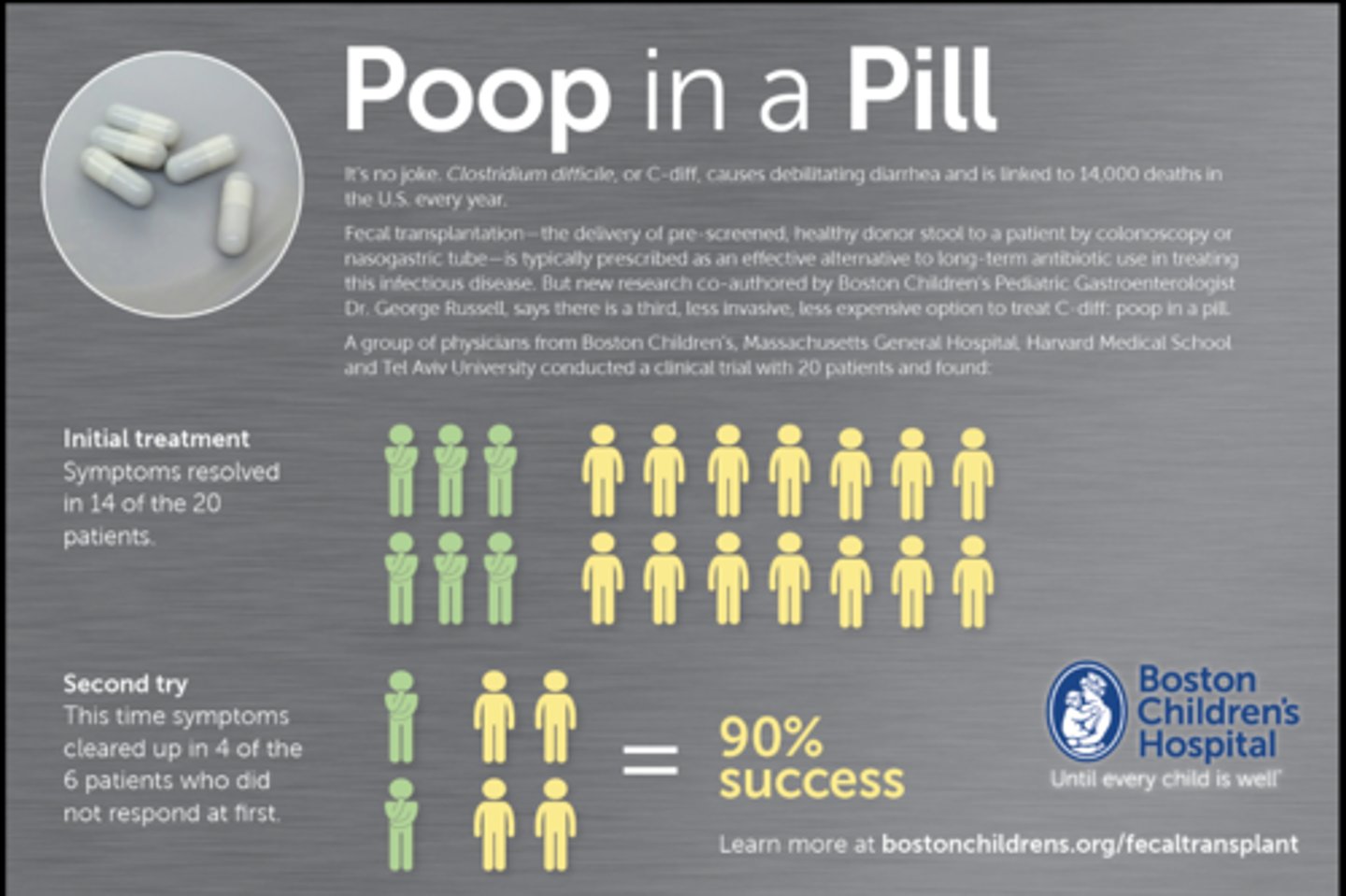
April 2023, FDA Approves New Fecal Transplant Pill (Vowst)
In the study of 182 people, 12% of those who took Vowst had a recurrence during an 8-week period, compared to 40% of people who were given a placebo pill
Each capsule of Vowst contains live bacteria, which is taken from human fecal matter from screened donor
The Vowst dosing plan is four capsules taken orally once a day, for 3 days in a row
ASSOCIATION OF MICROBIOTA WITH DISEASES OUTSIDE OF THE GASTROINTESTINAL TRACT
ASSOCIATION OF MICROBIOTA WITH DISEASES OUTSIDE OF THE GASTROINTESTINAL TRACT
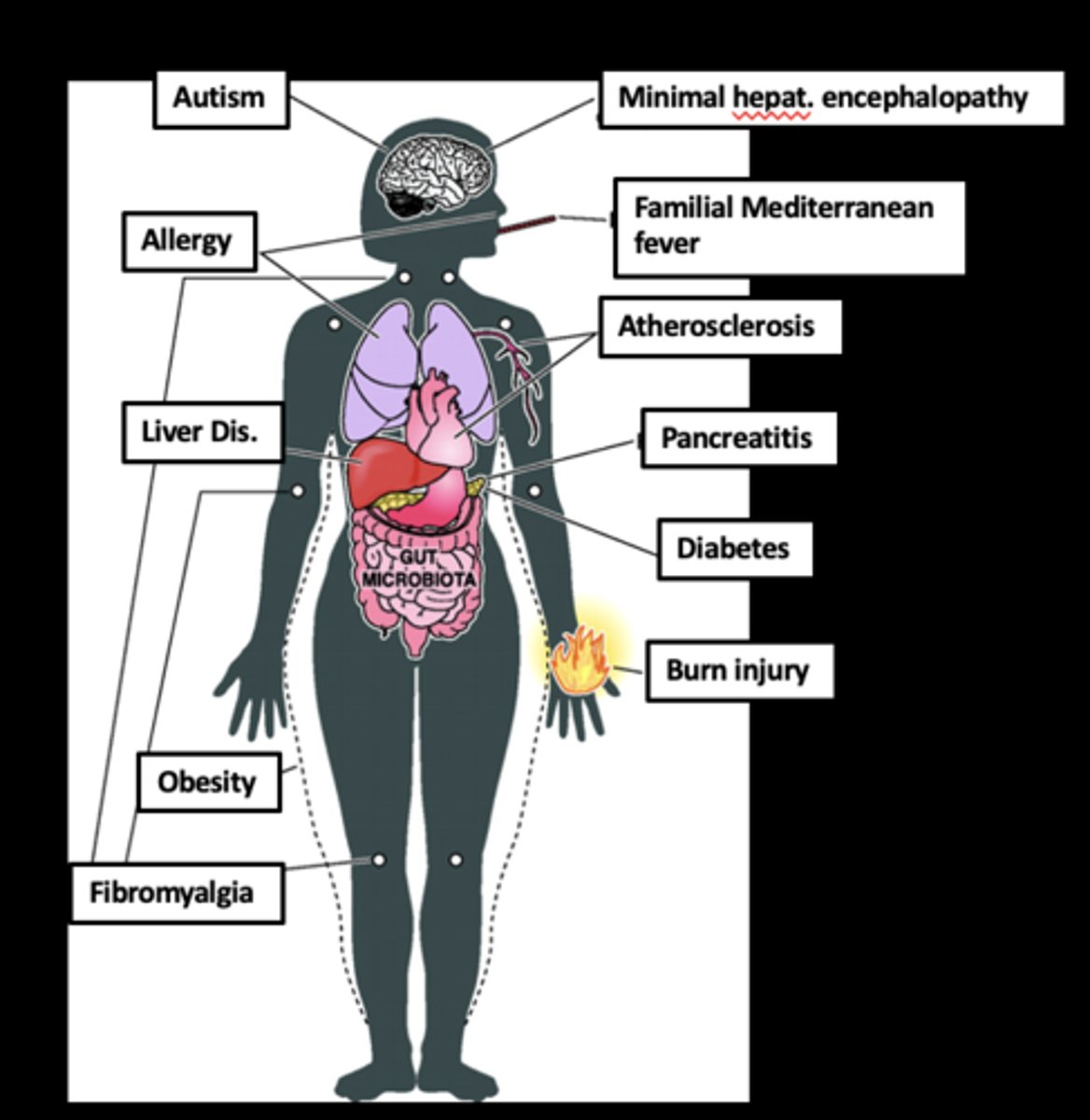
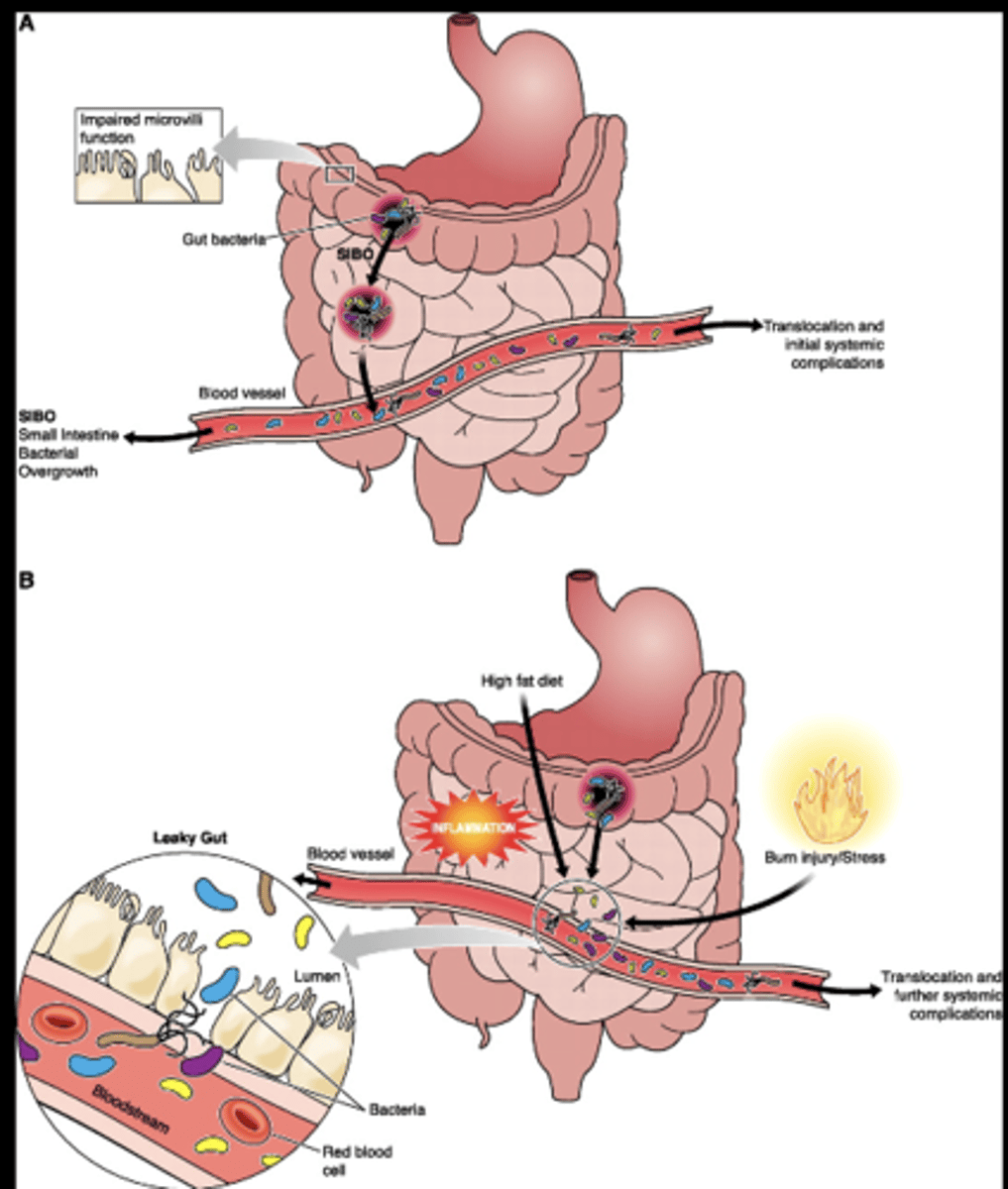
Gut Microbiota Systemic Translocation and Associated Diseases
External injury (e.g., burn injury, HFD, alcohol intake) results in gut microbiota translocation due to a "leaky gut"
Endotoxemia promote further systemic complications and damage to remote organ systems
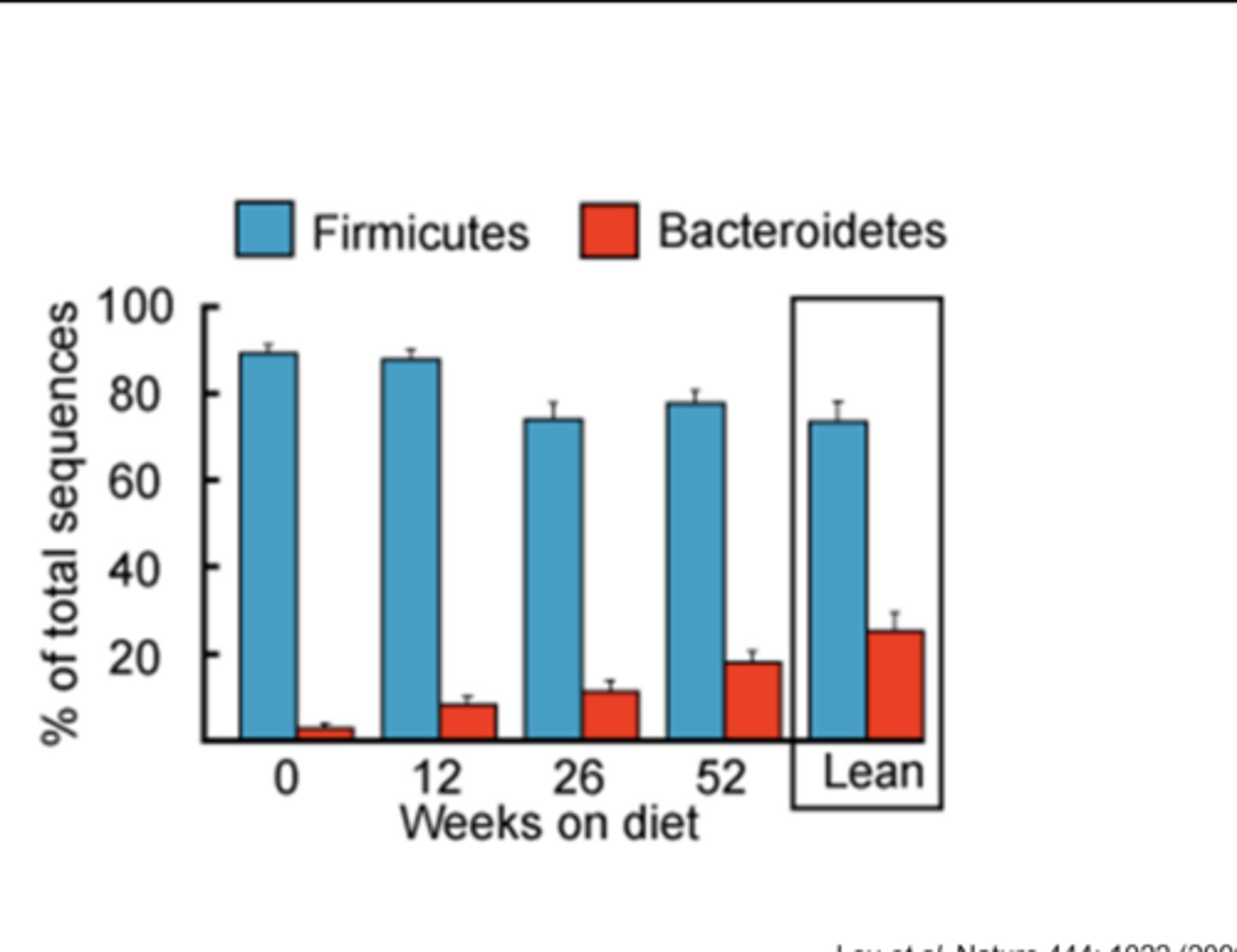
Effect of Dieting (Body weight loss)
Effect of Dieting (Body weight loss)
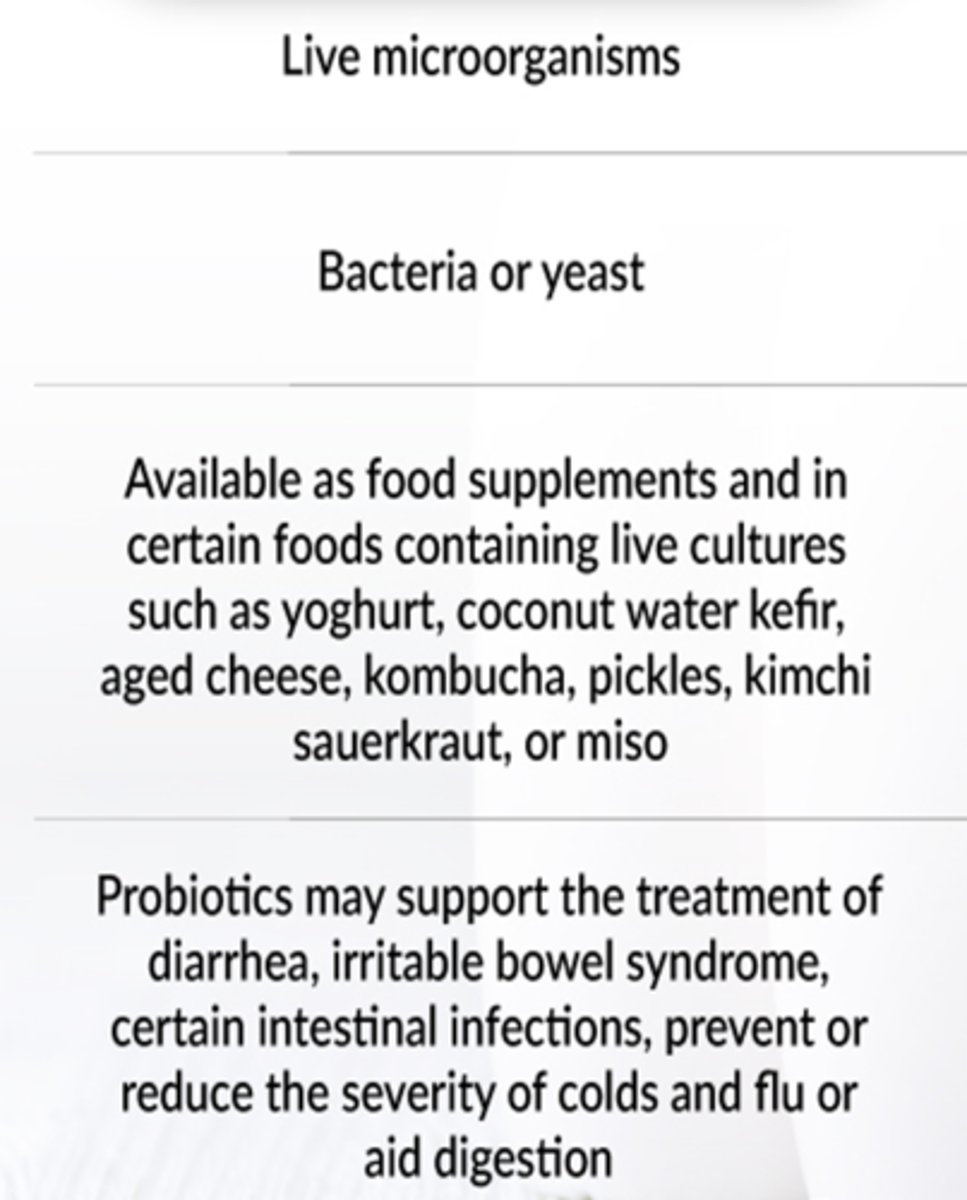
probiotics
probiotics
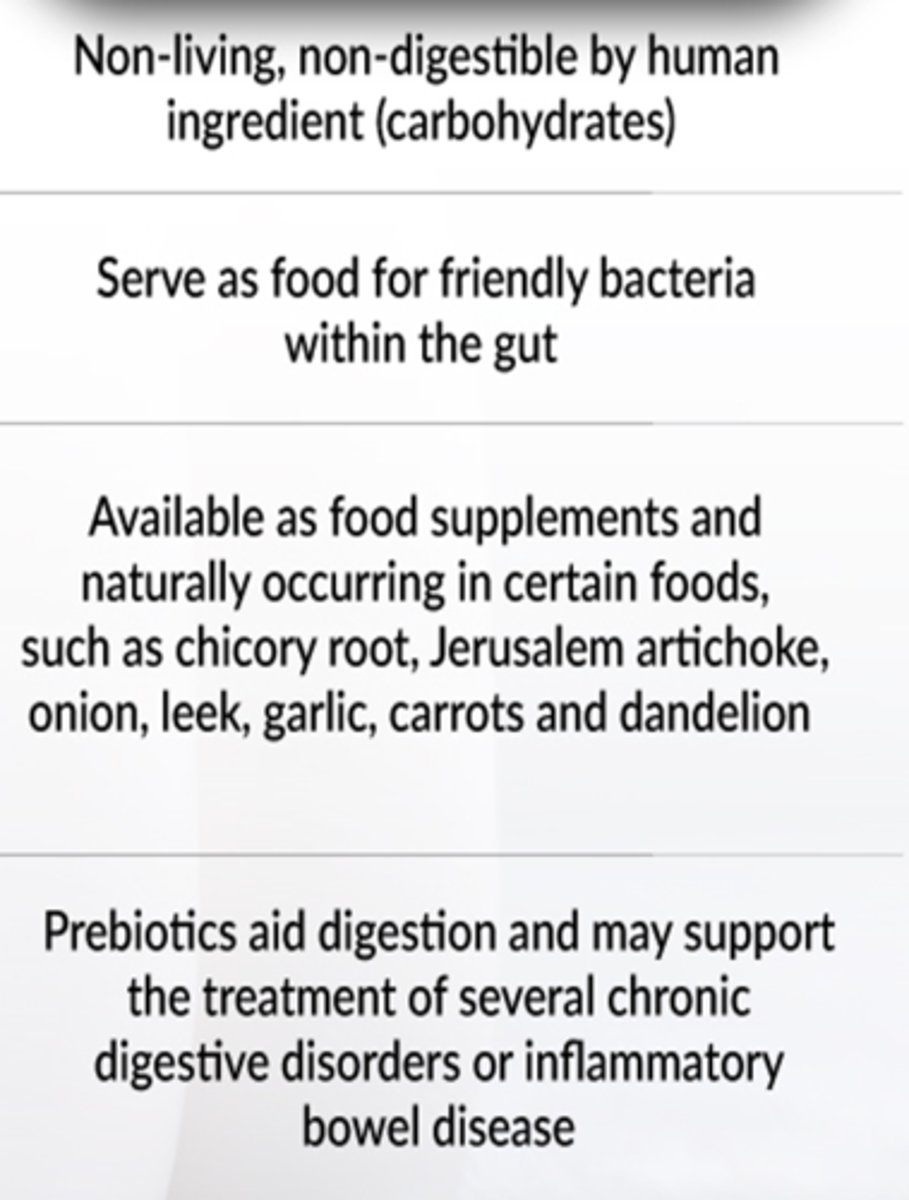
prebiotics
prebiotics
prebiotics and probiotics
prebiotics and probiotics
case study 1
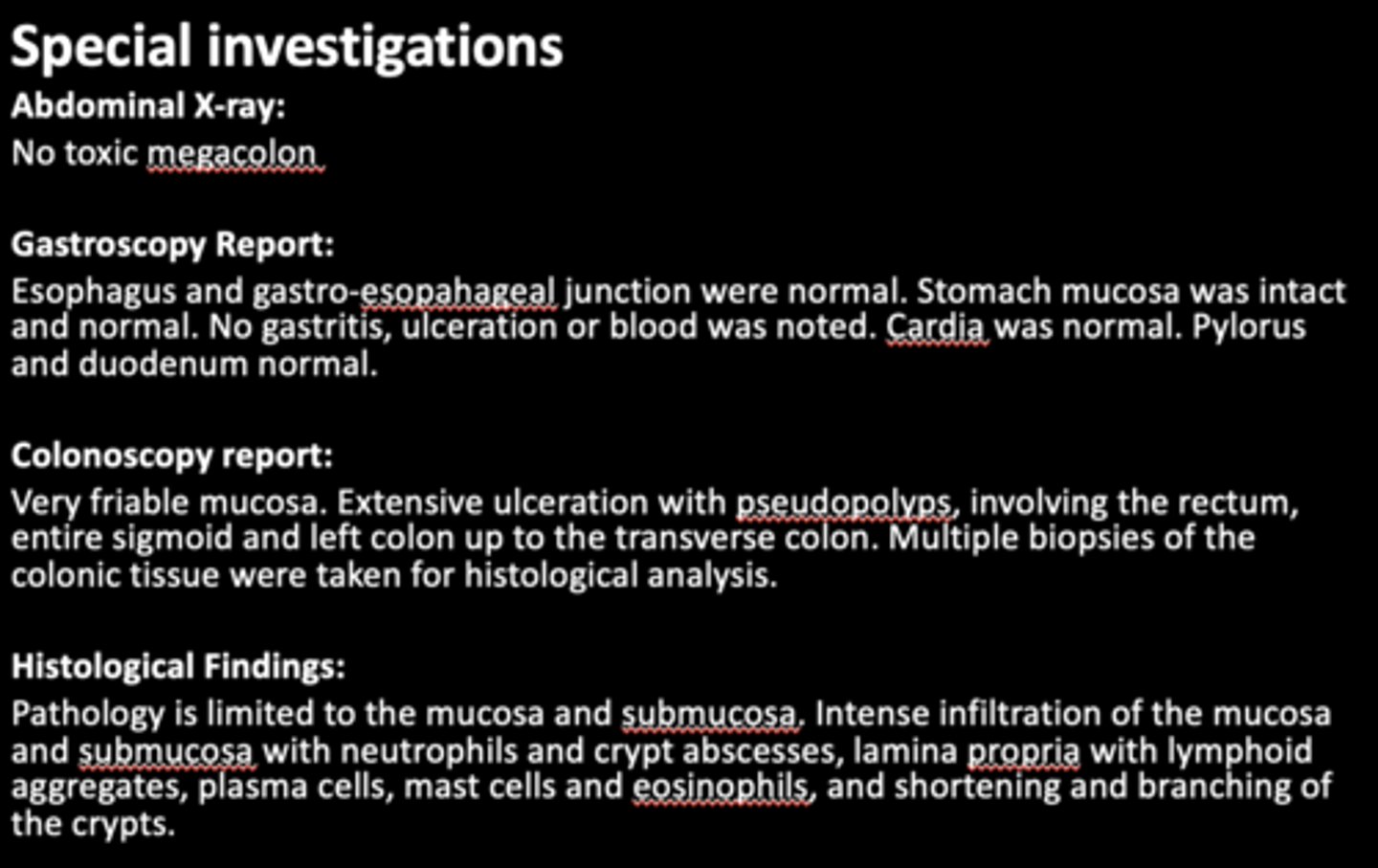
Patient is a 22 year old female who presented to the surgery department of a tertiary level hospital having been referred from a private clinic, with a two month history of severe abdominal cramps, persistent bloody and mucoid diarrhea, weight loss and tiredness.
Currently:
Patient is passing 10-20 liquid stools per day. Diarrhea is mucoid and bloody. Occurs day and night.
Patient complains of malaise, lethargy and anorexia. She has lost 8 kg in the past 2 months.
No past surgical historyNo significant medical history
Family history:
Mother – type 2 Diabetes MellitusNo other family members with chronic disease
No known allergies
Differential Diagnosis
Infection:
Cryptosporidium,
Shigella,
salmonella,
E.coli,
Campylobacter,
Clostridium difficile
If HIV positive consider- MAC, Isospera beli, cryptosporidium, TB
Functional bowel syndromes e.g. irritable bowel syndrome (IBS) MalabsorbtionCeliac diseaseInflammatory bowel disease (IBD)
Examination
Thin ill looking young woman, conscious and alert, in obvious discomfort.
Vitals
Heart rate: 80bpm Respiratory rate: 18 bpm
•Blood pressure: 120/70 Temperature: 37 ̊C
•Pale mucous membranes
Abdominal examination:
•Guarding and tenderness noted in the left iliac fossa and hypogastrium.
InvestigationsNo results available from previous admissions. All results are from current admission.
case study 2
Ms. F, 48 years old, has been admitted to the hospital with severe abdominal pain.
Earlier that day she had generalized abdominal pain, followed by a severe pain in the lower right quadrant of her abdomen, accompanied by nausea and vomiting.
That evening she was feeling slightly improved and the pain seemed to subside somewhat.
Later that night, severe, steady abdominal pain developed, with vomiting.
A friend took her to the hospital, where examination demonstrated lower right quadrant tenderness and mild abdominal rigidity. Fever and leukocytosis indicated infection.