lecture 14, immune system II
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
the adaptive immune system
active immunity
passive immunity
active immunity
natural
complete immune response occurs following a natural encounter with an antigen
ex. a cold
you do everything
day to day inoculation
artificial
complete immune response happens following exposure to an antigen artificially
ex. vaccine
passive immunity
natural
mother to child transmission of antibodies
ex, IgG transmission across the placenta, IgA transmission via breast milk (baby doesn’t know how to make it)
artificial
injection of premade antibodies to help neutralize infectious material
ex. post-exposure to rhabdovirus
you were given it
major histocompatibility complex
two types
different in each person
responsible for transplant rejection
MHC I: embedded in the plasma membrane of all nucleated cells in the body
every nucleated cell has this (RBC wont)
characteristic of you
MHC II: embedded in the plasma membrane of antigen presenting cells
only antigen presenting cells
macrophage would have both (antigen resenting and nucleated)
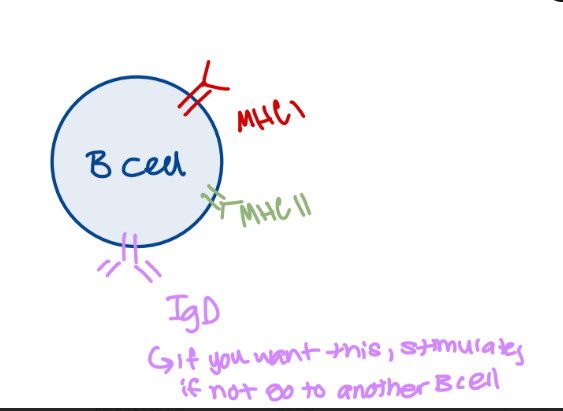
b lymphocytes
naïve B lymphocytes (haven’t been stimulated yet) develop into antibody secreting cells
antibody=immunoglobin (both proteins)
Ab=Ig
antibody is inserted into plasma membrane
when specific antigen binds, B cell is activated
each b lymphocyte is responsible for antibody production against a single epitope
develops into a clonal population of cells once exposed to antigen (consequence of mitotic division)
clonal population consists of
a large fraction of plasma cells
short lived effectors that actively secrete antibody
small fraction of memory cells (some saved for later, could be years)
long lived cells that are important for future exposure to antigen
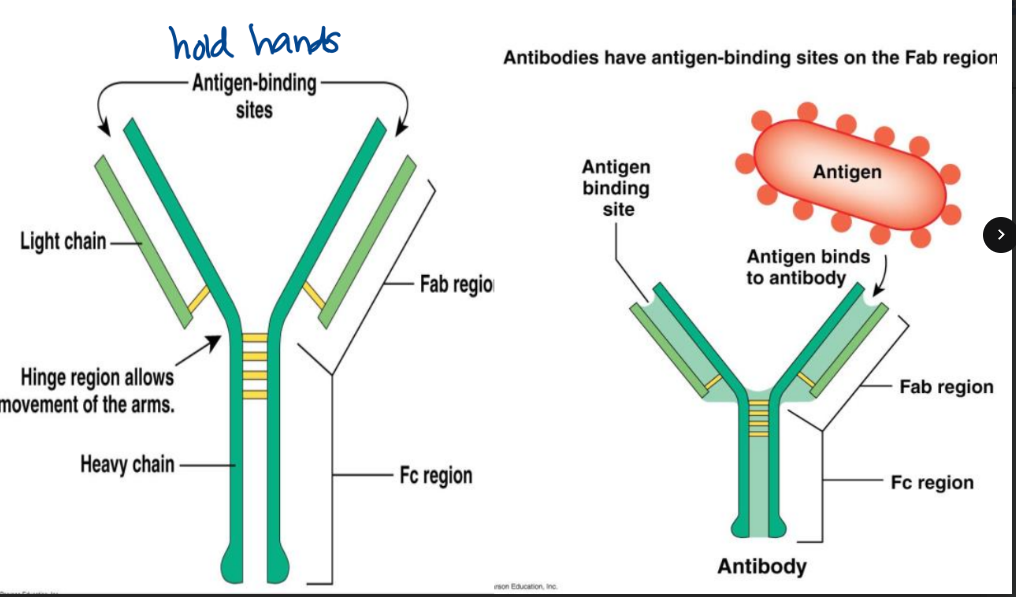
antibodies consist of
two identical heavy chains
two identical light chains
each b lymphocyte produces an antibody specific to only one antigen
unique Fab fragment
variable segment of the antibody
two per antibody
constant region-Fc region
five different classes
IgA
IgG
IgD
IgE
IgM
IgM
pentamer (2×5=10)
first to be secreted in response to antigen
primary immune response
class switching leads to the production of a different Fc variety
always first every time
really good against one type
IgA
dimer (2×2=4)
secreted at mucosal sites
important in neutralization of pathogens that are able to move past mucosal membranes
released in breast milk, digestive tract, respiratory tract, reproductive tract
IgG
monomer (present in blood and tissue)
∼75% of plasma antibody
crosses the placenta (how they come up with vaccine schedule for babies) born in sterile sac
involved in secondary antibody response
spray into nasal → IgA
flu shot → IgG
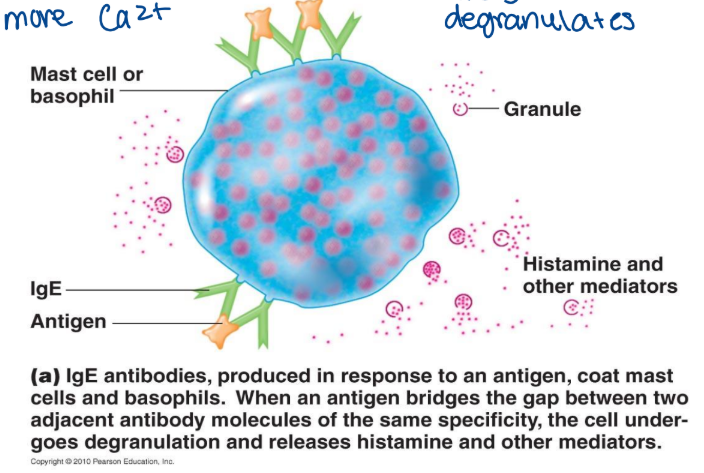
IgE
monomer
important for destruction of parasites
also released in response to allergens
can bind to mast cells leading to degranulation
FcIgE receptor on basophil → for allergen allows to bind to allergen and causes degranulation of HIS
IgD
monomer
located on the surface of B lymphocytes (sits on surface)
unknown function
advertisement
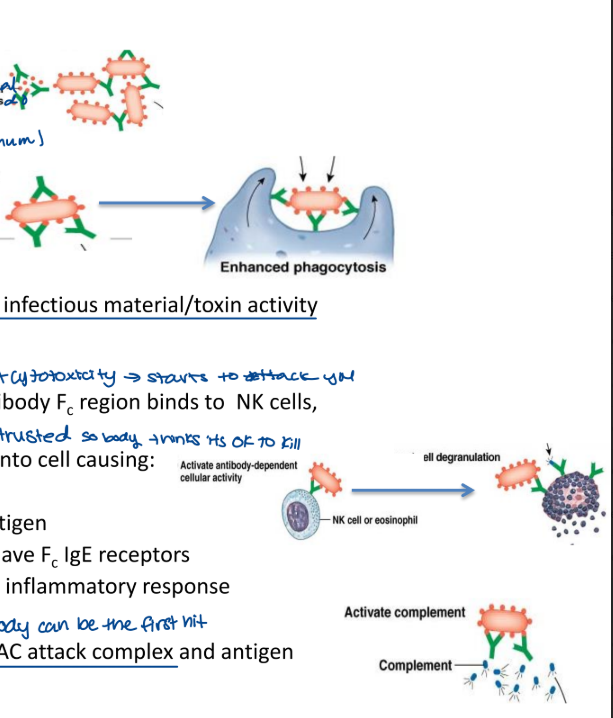
antibody functions
works to:
agglutinate antigens
behave like a mop
pick up 2 antigens at once (minimum)
stops what foreign material was going to do
opsonize foreign material
enhances phagocytosis
Fc region lets it talk to other immune cells
trusted sources
neutralize antigen
prevents infection/spread of infectious material/toxin activity
cytotoxicity (antibody dependent cytotoxicity → starts to attack you)
when bound to antigen, antibody Fc (trusted source so the body thinks its ok to kill) region binds to NK cells, mast cells
triggers calcium entry into cell causing degranulation
destroys antigen
mast cells specifically have Fc IgE receptors
important for the inflammatory response
complement activation
leads to the formation of MAC attack complex and antigen destruction (antibody can be first hit)
antibody response
work to neutralized exogenous antigen (outside cell, ECF, ISF, plasma) (humoral, antibody)
bacteria, toxins, viral particles (anything that is foreign from outside)
secreted from activated plasma cells (effector cells)
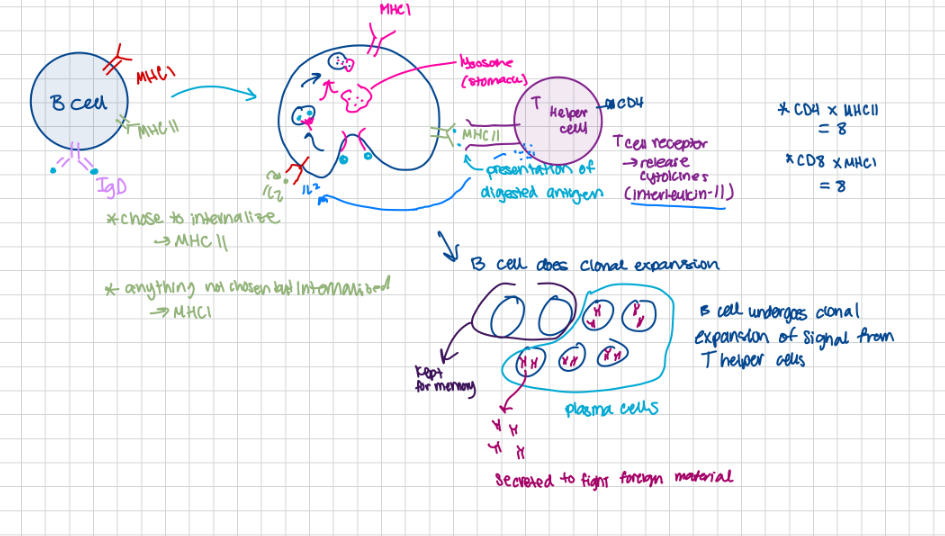
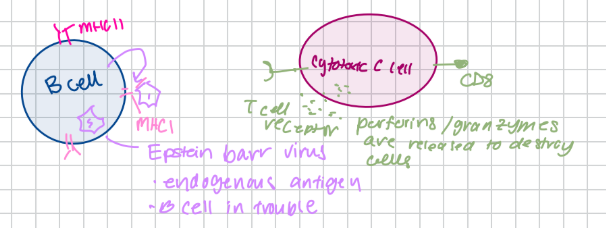
ex. B cells bind and internalizes antigen
antigen is digested and trafficked to the cell surface atop MHCII
antigen is presented
T helper cells come along and bind antigen-MCHII complex
Th cell releases cytokines that activate B lymphocyte to proliferate and begin secreting antibodies
endogenous (inside cell, antibody can’t help you, cell mediated)
antibody function
cytokines produced by Th cells include (coordinated response):
interferon-y
activated macrophages (phagocytes)
interleukins
activate antibody production and Tc cells
activate eosinophils and mast cells
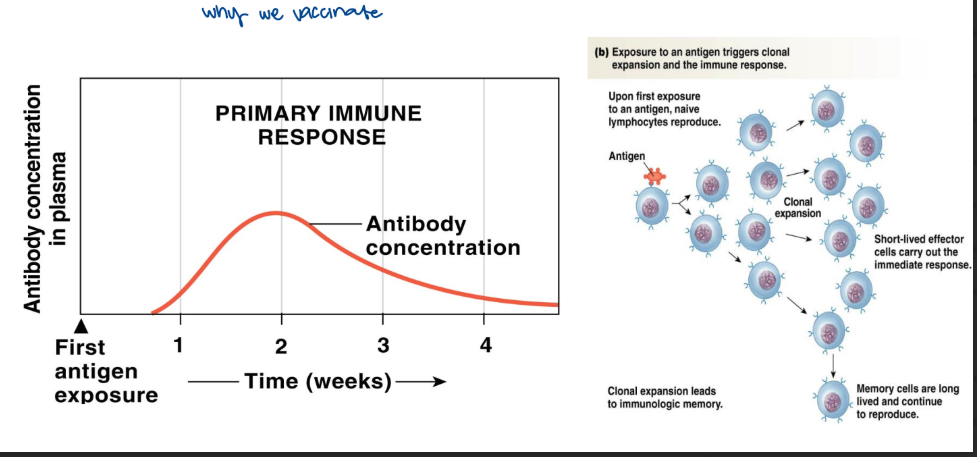
primary immune response
occurs in response to the initial exposure to antigen
slow production of low levels of antibody
key result: memory produced (sit on shelf)
memory cells activated upon every subsequent exposure to antigen (why we vaccinate)
7-10 days
first time you encounter specific epitode
low and slow (IgM)
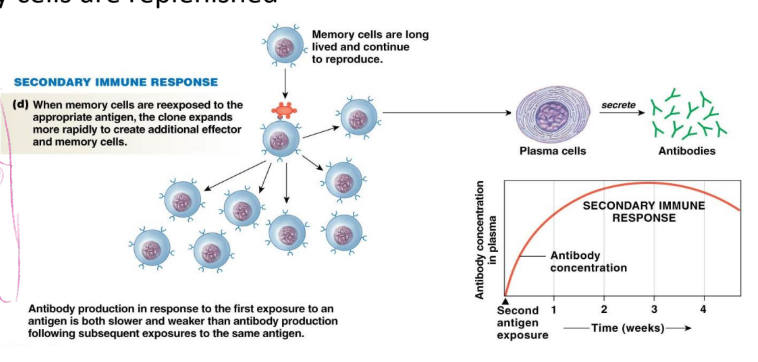
secondary immune response
occurs in response to each subsequent antigen exposure
memory cell encounters antigen and completes clonal expansion
results in rapid production of high levels of antibody
memory cells are replenished
swing into action
see something again
high and fast (antibody increase in 1-2 days)
cell mediated immunity
mediated by cytotoxic T cells (toxic cells → kill cel)
responsible for destruction of abnormal cells
endogenous antigens
recognize antigen displayed on surface of MHCI
binds to MHCI-antigen complex and secrete perforins (pokes holes) and granzymes (kills)
granzyme enzymes enters the compromised cell via channels created by perforins
trigger apoptosis of cell
self-recognizing Tc cells are destroyed during development (find them and got rid of them)
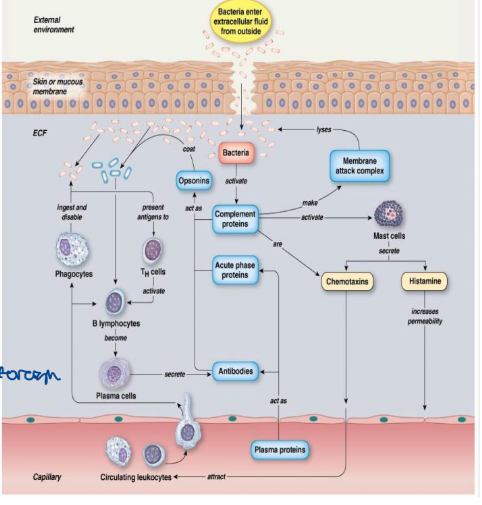
immune response to bacterial invaders
bacteria causes inflammatory response
also cause antibody production
complement activation
opsonization
mac attack (pore to allow cell to leak its content)
mast cell/ basophils degranulation
histamine release
vasodilation/increased vascular permeability
production of chemo-attractants (increase flow, increases immune cells)
recruits immune cells to match the foreign
phagocyte activation
non-encapsulated bugs only
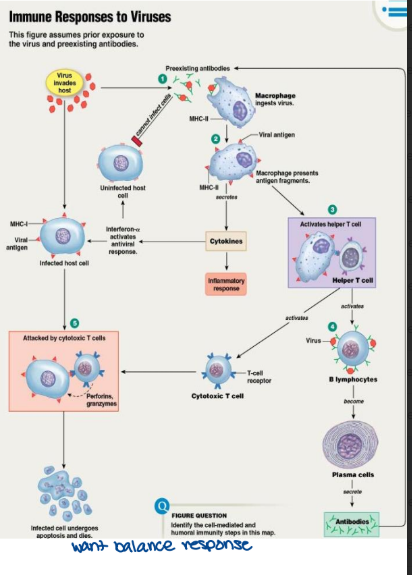
immune response to viral invaders
free viral particles will enter into host cells
infected host cells displays endogenous antigen with MHCI
activates cytotoxic T cells (destroy infected cell)
infected cell is destroyed → reservoir for viral production is eliminated
if previous exposure has taken place memory B cells are activated by virus
antibodies neutralize free virus preventing infection of host cells
antibody-virus complexes are phagocytosed by macrophages
viral antigens are presented with MHCII
activates Th cells
activated Th cells will activate Tc cells and B lymphocyte
macrophages produces interferon-a
sparks anti-viral response in uninfected host cells (important for inflammation)
minimize the number of new cells that may become infected
macrophage produced pro-inflammatory cytokines
type of vaccines
attenuated whole agent vaccines
inactivated whole agent vaccines
toxoids
subunit vaccines
conjugated vaccines
attenuated whole agent vaccines
use weakened living microbes or weakened infectious virus
weakened because of an introduced mutation (makes it weak)
ex. virus that can enter host cell but cannot reproduce
exogenous → B cells will respond
closely mimics an actual infection
stimulates a cell mediated response and an antibody mediated response (exo and endo)
often confers life-long immunity
ex. MMR vaccine (measles, mumps, rubella)
guy has a gun, take gun away, still same guy, will just find another weapon
BEST
CON
the virus or bacterium may revert back to the original pathogenic form
can be very dangerous to immunocompromised patients (AIDS, cancer) and pregnant women
the organism may still be able to cause disease
inactive whole agent vaccines
use whole agents that have been killed
ex. viruses-rabies, influenza, polio
ex. bacteria- Vibrio cholera
very safe
take all out but looks the same outside
not endogenous cant get into cell!!
toxoids
inactivated toxins:
made from purified proteins (given to vaccinate people against the toxin)
“stand in” but cant act
the immune response acts against the toxoid
stimulates the antibody mediated response only (exogenous)
usually requires a series of injections for full immunity
immunity does not last as long
ex. DPT vaccine (former) (diptheria, pertussis, tetanus) DTaP
required a booster shot every ten years
subunit vaccines
contain purified components from viruses or bacteria (ex. show someone your eyes only → bits and pieces)
antigens most likely to induce an immune response
stimulates antibody mediated response only and memory (exogenous only)
ex. Streptococcus pneumoniae-purified capsular polysaccharide
pneumoshot: protects against pneumonia
ex. hepatitis B
viral coat proteins produced by genetically modified yeast (spike protein/capsid)
EXTREMELY SAFE VACCINES: the disease causing agent is not present
conjugated vaccines
a polysaccharide antigen is combined with a protein antigen-resulting in a stronger immune response in children
ex. Haemophilus influenza capsule combined with diphtheria toxoid
can induce an immune response in children as young as 2 months
make it big like this so inexperienced immune system notice it
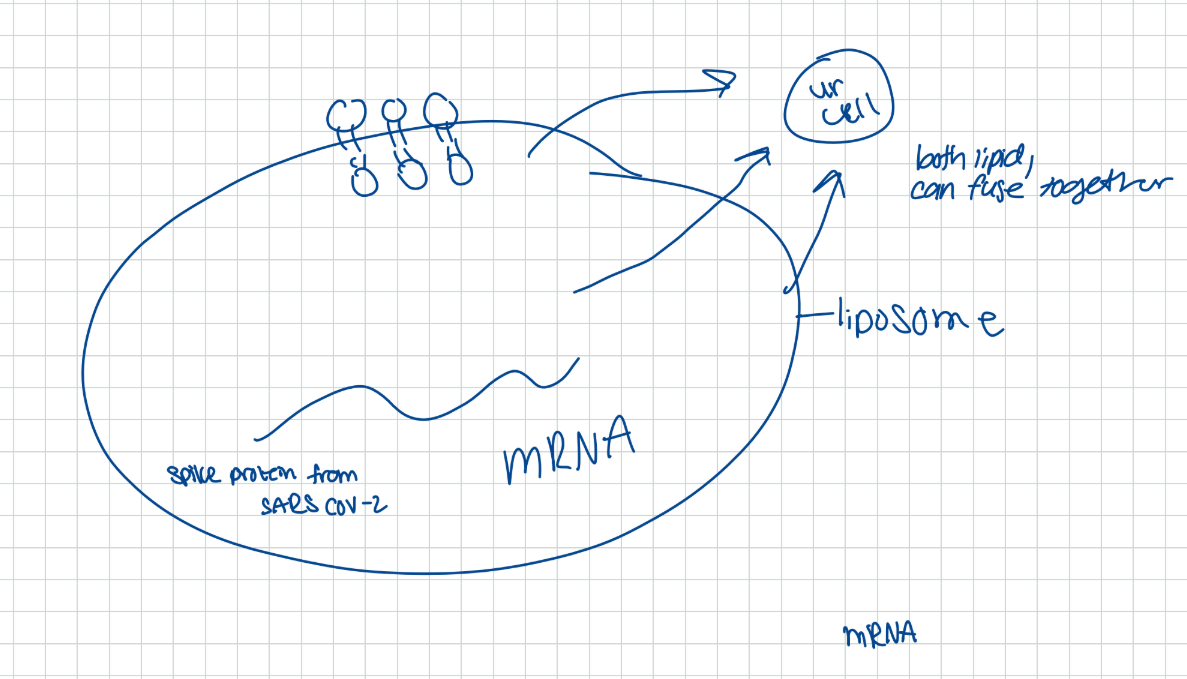
mRNA vaccine
hypersensitivity
also referred to as allergy
an abnormal immune response (shouldn’t freak out over a peanut)
immune response is mounted against allergen (would be there antigen/immunogen
too sensitive
5 types
type 1 hypersensitivity
this is referred to as an anaphylactic response
the 1st encounter with the allergen causes B cells to differentiate into plasma and memory cells (nothing happens)
the plasma cells make IgE which then binds to mast cells or basophils (seats self in the FcIgE spot)
there are no apparent symptoms (at start)
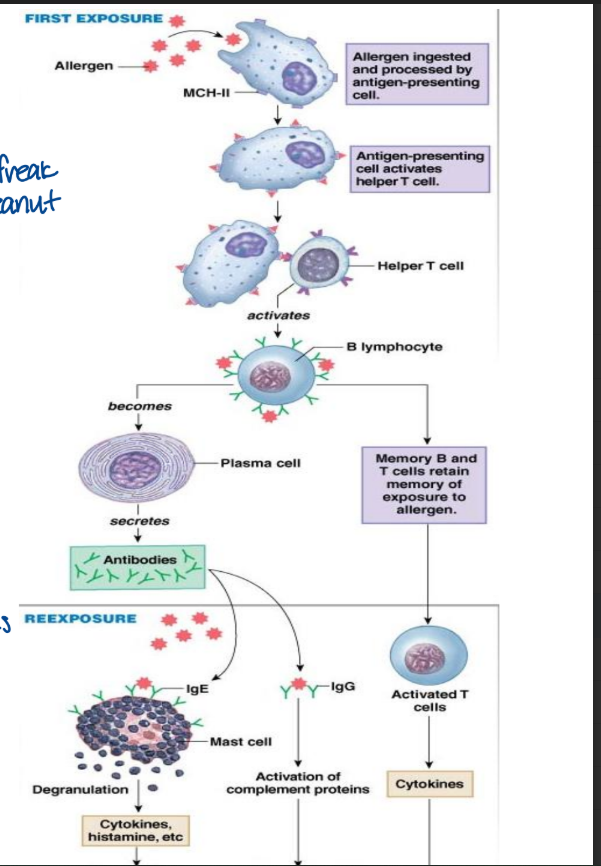
type 1 hypersensitivity: 2nd encounter with the allergen
IgE molecules bind to the antigen and mast cell or basophil releases histamine
histamine triggers vasodilation: redness, swelling, and decreases blood pressure (decrease blood volume and increase vessel diameter) anaphylactic shock
mucous production: tears, runny nose
contraction of bronchial muscles: difficulty breathing (bronchoconstrictor with more Ca2+)
allergen binds and degranulates
treatments
antihistamine
epinephrine
allergy shots
antihistamine
this blocks the action of histamine
histamine is still produced but cannot trigger responses
works well for mild symptoms, example: hay fever
stops it from causing problems
epinephrine
used to treat anaphylactic shock (severe allergy)
acts as a vasoconstrictor increasing blood pressure
the effects last for 20-30 minuets
this buys time to allow for administration of intravenous antihistamine
epi-pen
allergy shots
this is injected like a vaccine
increasing doses of the antigen are given over 2 years
this induces memory cells that produce IgG instead of IgE
IgG will bind to and neutralize the antigen to presenting it from binding IgE
this prevents the release of histamine
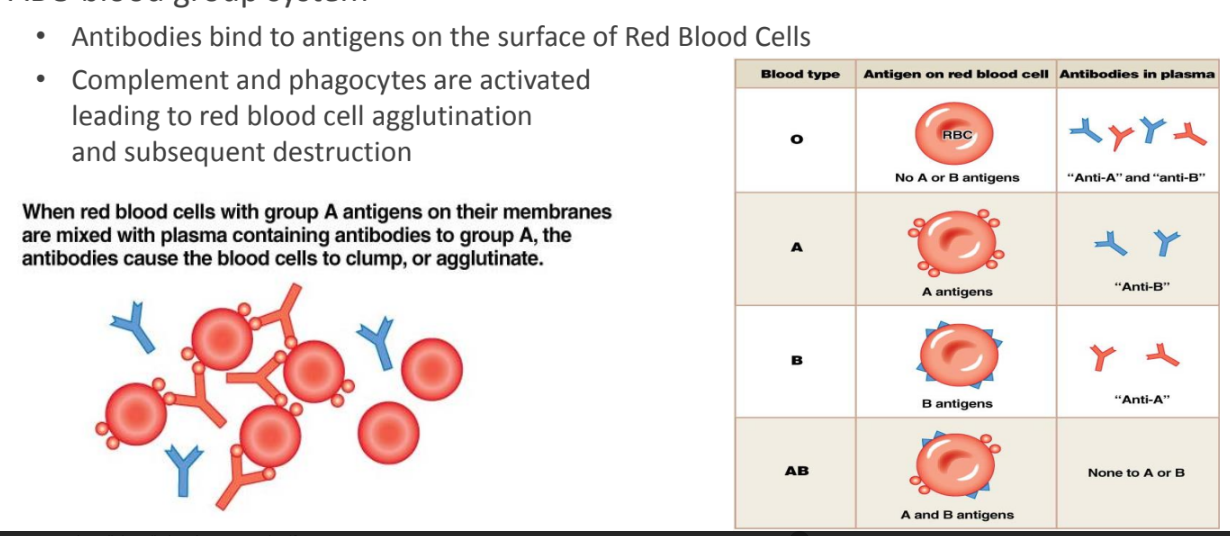
type II hypersensitivity
antibody dependent cytotoxicity
activated by foreign antigenic cells
leads to phagocytosis and complement activation against the foreign cell
ex. blood transfusion
ABO blood group system
antibodies bind to antigens on the surface of red blood cells
complement and phagocytes are activated leading to red blood cell agglutination and subsequent destruction
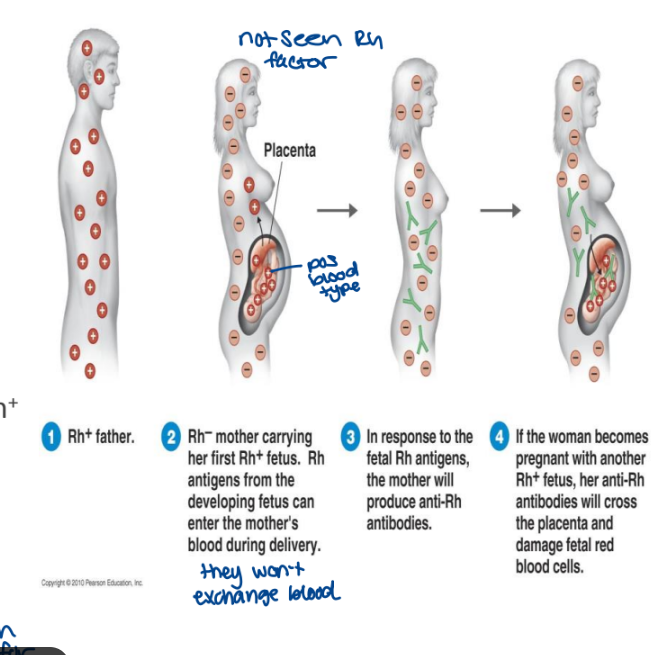
type II hypersensitivity: Rh factor
this only occurs on the 2nd or subsequent pregnancy
Rh is another surface antigen on red blood cells
can occur when:
a child is produced between an Rh- woman and a Rh+ man
the child has a 50% chance of being Rh+
if this happens the mother can make antibodies against the Rh+ cells which can kill the baby after birth (when birth can cause for them to mix and be exposed → develop Rh factors)
+=Rh
-=no Rh
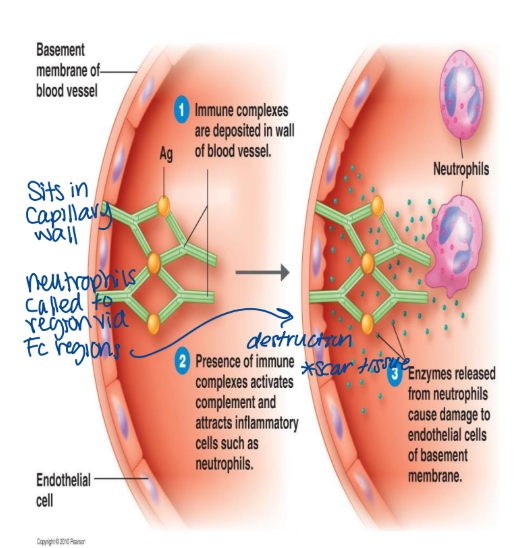
type III hypersensitivity
this is immune complex formation
it occurs when there are certain antibody to antigen ratios in the blood
the antibody forms small complexes with the antigen which then get trapped in the membrane causing problems
this also activate complement which in turn activates neutrophils to release enzymes
this can damage blood vessels
sits in capillary wall. neutrophils called to region via Fc region → destruction scar tissue
type iv hypersensitivity
this is delayed hypersensitivity
it is the result of cell mediated response (cytotoxic T cells)
not antibody mediated
this causes a delay reaction 24-72 hours after contact
it results from the activation of memory T cells
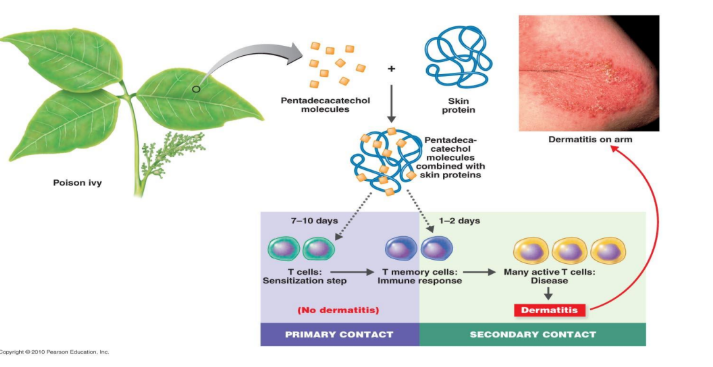
ex. contact dermatitis: chemical reactions
abnormal looking skin cells
how does it happen?
small chemicals interact with the skin proteins to from antigen
this causes a change in skin cells
the cell mediated immune response acts against foreign or abnormal cells
targets a localized area of the skin
cytotoxic T cells destroy skin cells: causes red, itchy, swollen skin
ONLY CELL MEDIATED
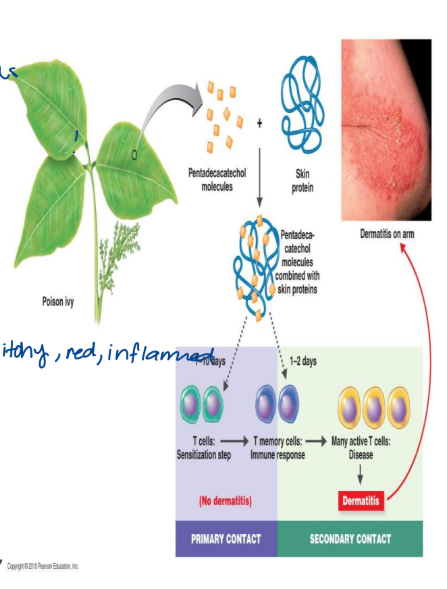
type IV hypersensitivity: poison ivy
first contact: limited response occur and there is no resulting dermatitis
memory T cells are produced
second contact: memory T cells differentiate into activated cytotoxic T cells
causes contact dermatitis → look like abnormal skin cells
transplantation
tissue or organ rejection
involved both the antibody mediated response and the cell mediated response to foreign cells
both type II (start making antibodies MHC I) and type IV hypersensitivities
treatment: drugs that suppress the immune response (make person at risk for other infections)
cyclosporine, prednisone
since the immune system is suppressed transplant patients are very susceptible to infection
as a result these patients must be kept in isolation
graft vs host disease:
cytotoxic T cells from the donor tissue see the host’s body as foreign and attack
in the organ leftover Ct will start to attack host, your cytotoxic T will attack organ too
cyclosporine is used to suppress the immune response in order to prevent this attack
immunodeficiency disorders
results due to inadequate immune system (don’t have enough)
there two types:
congenital (inherited) immunodeficiency - present at birth
acquired immune deficiency
congenital (inherited) immunodeficiency - present at birth
ex, serve combined immunodeficiency disease (SCID)
non-functional T and B cells: no type of adaptive immunity is present
allows for severe infections to develop
acquired immune deficiency
ex. acquired immunodeficiency syndrome (AIDS)
this is the last stage of HIV infection
HIV infects and subsequently kills Y helper cells, macrophages and dendritic cells (lose function)
the patient is extremely susceptible to infection: both the antibody: both the antibody and the cell mediated immune responses are impaired
opportunistic infection
attack with viral spike protein
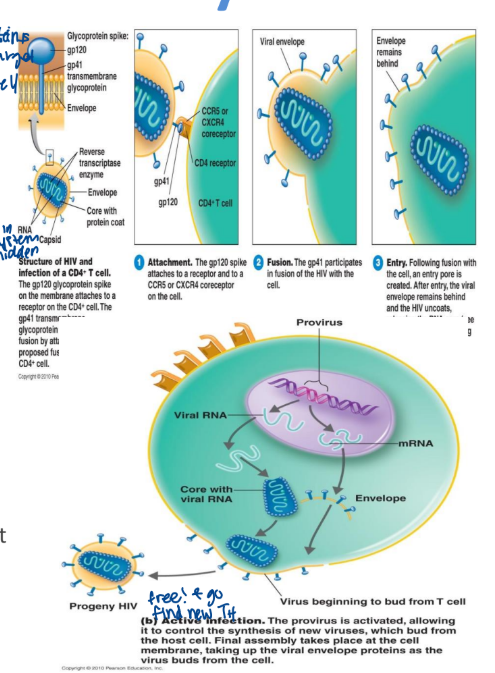
human immunodeficiency virus
HIV
spikes enable HIV to attach to and penetrate the host cell
viral DNA can integrate into host cell chromosomes as provirus
RNA → reverse transcriptase → DNA (hides HIV in DNA)
the virus remained latent here for a long time
this shelters the virus from the immune system
the virus may also cause active infection
new viruses produce bud out from the host cell
HIV is an enveloped virus
antigenic changes in HIV
HIV genome is highly susceptible to mutation
antigens change: helps the virus to invade to the immune system
reverse transcriptase (highly error prone)
two major groups of HIV viruses (with many sub-groups of each):
HIV-1: most common HIV virus worldwide (gets there faster)
HIV-2: found in western Africa: slower progression of disease
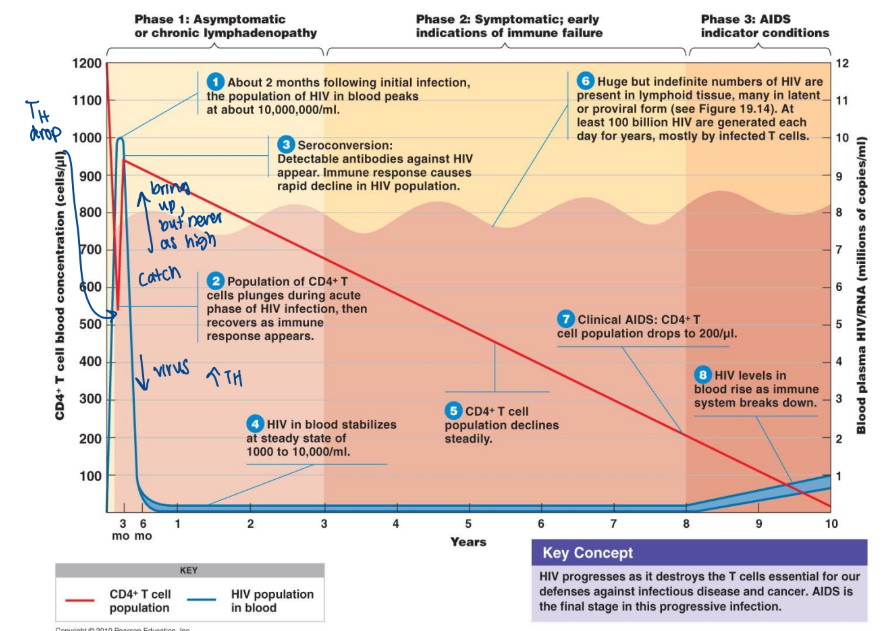
stages of HIV infection
category A: early stage
often asymptomatic but may cause flu like symptoms, swollen lymph nodes
when you first get infected
asymptomatic
category B: middle stage
may be asymptomatic
may lead to increased infection: example-yeast infections of the throat, mouth or vagina (TH infected are dying)
persistent diarrhea
shingles → reactivation of virus of chicken pox
HIV is reproducing but is killed and thus controlled by the immune system
HIV resides mostly in the lymph
this stage can last 10-20 years
category C: late stage
clinical AIDS defined by a decrease in T helper cells < 200 cells TH per mmm3 blood
persistent infections occur
ex. yeast infections of esophagus, bronchi, and lungs
kaposi’s sarcoma: rare herpes virus prevalent in AIDs patients
high prevalence of pneumonia, tuberculosis, etc. in these patients
HIV transmission
direct or indirect contact with infected bodily fluids
blood
contact with infected blood
ex. needle sharing, need stick at hospital (occupational hazard)
blood has 1000-100000 viruses/mL
1:4 infected blood exposure result in infection
semen/vaginal secretions
contact through unprotected sex
semen has 10-50 viruses/mL
1:1000 unprotected sexual encounters result in infection (if you have lesions it can be more prone)
mother to child
this form of transmission either occur during pregnancy, at birth or via breast milk
autoimmune disease
this is when the body mounts an immune response against itself (turns on itself)
this can occur in response to an infection or it can genetic (inherited)
rheumatoid arthritis
IgM, IgG and complement act against collagen in the joints (holds you together)
causes chronic inflammation
lupus
antibodies produced to chromatin which is a complex of protein, DNA and RNA
the chromatin-antibody complexes accumulate in the joints, kidneys and blood vessels (like type III hypersensitivity)
multiple sclerosis
T cells and macrophages attack myelin sheath covering neurons (insulating so don’t get ions everywhere)
symptoms range from mild fatigue to severe paralysis
this may triggered with Epstein-Barr virus (hard to spread impulses quickly because ions are going everywhere)