Chapter 07: Bone Tissue and Its Functions
1/110
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
111 Terms
What is the living skeleton made of?
Dynamic tissues and cells are permeated with nerves and blood vessels. It continuously remodels itself and interacts with other organ systems.
What is the study of bone known as?
Osteology
What are some unique features of the bone?
It is vascular and stores all minerals in bone; if the bone does not work, the organs will not work properly—stress on bone= more dense bone.
Skeletal system
Composed of bones, cartilages, and ligaments.
What does cartilage do?
Forerunner of most bones, covers joint surfaces. Body starts off cartilage, then Calcium and Phosphate harden it
CHONDRO= CARTILAGE asvascular
What do ligaments do?
Connective tissues that hold bones together.
What do Tendons do?
Attach muscles to bones for movement.
What are the 6 functions of the skeleton
Support
Protection
Movement
Electrolyte balance
Acid- base balance
Blood formation
"Strong People Move Every Active Bone."
How does the skeleton provide SUPPORT the body?
Limb bones and vertebrae support body, jaw bones, support teeth, some bones support viscera.
How does the skeleton provide PROTECTION for the body?
•Protects the brain, spinal cord, heart, lungs, and more
How does the skeleton provide MOVEMENT the body?
limb movements, breathing, and other movements depend on bone
How does the skeleton provide ELECTROLYTE BALANCE for the body?
Regulates calcium and phosphate levels
How does the skeleton provide ACID-BASE BALANCE for the body?
Buffers blood pH via phosphate and carbonate.
How does the skeleton provide BLOOD FORMATION for the body?
Red bone marrow produces blood cells.
What are some extra information about the functions of the skeleton?
Calcium activates nuerons
Long bones mainly have red bone marrow
Parathyroid gland - cant regulate calcium without it ->die
Red marrow growing
yellow marrow puberty
What is Bone (Osseous tissue)?
Connective tissue with matrix hardened by calcium phosphate.
What is Mineralization/Calcification?
Process of hardening bone tissue.
Extra notes about bones and Osseous tissue?
Infant =less bone more cartilage, highest cartilage = growth
more flexible to come out of womb
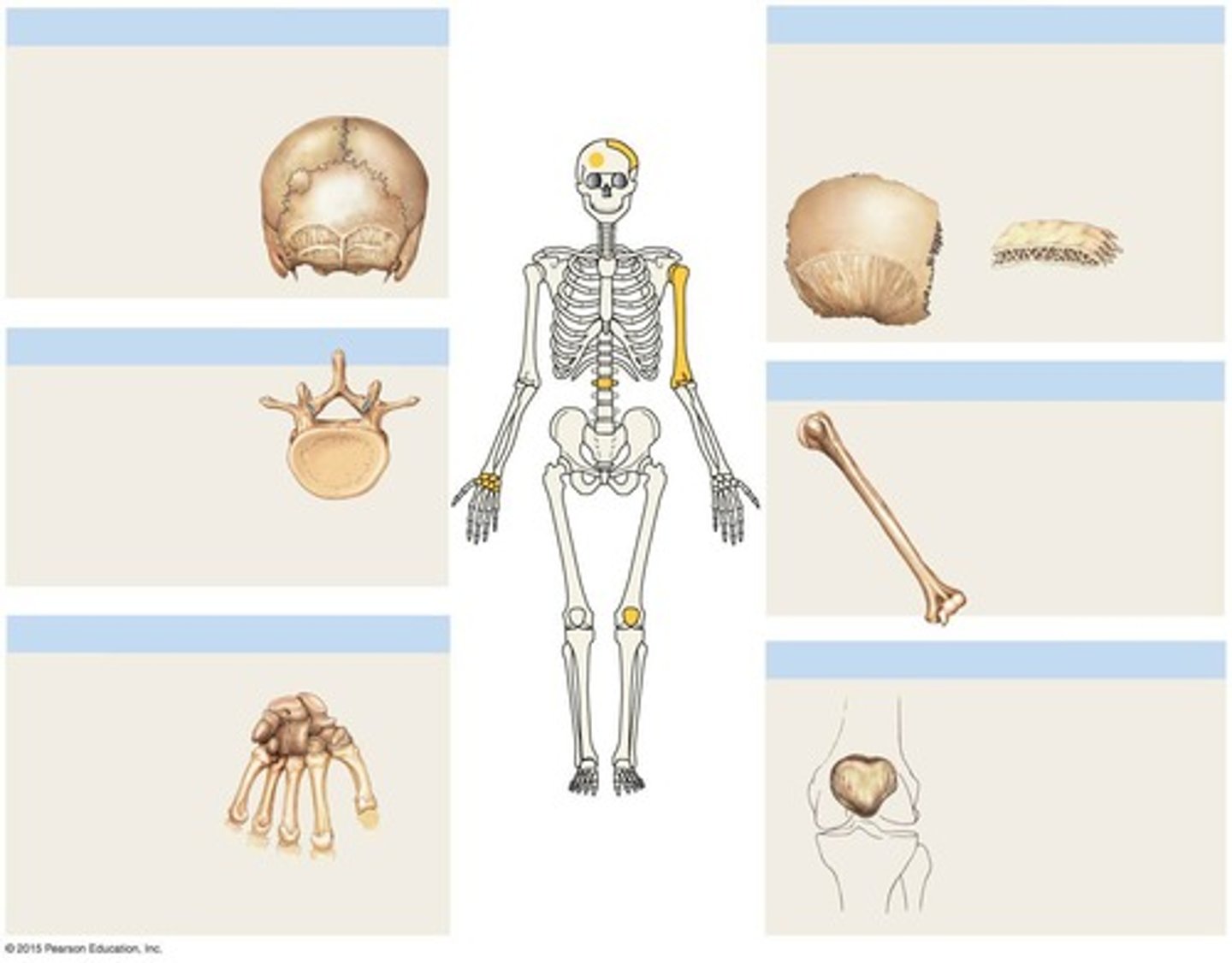
What are Flat bones? Examples ?
Thin, curved plates protecting soft organs.
-Ex. roof of the skull, the sternum (breastbone), the ribs, and scapulae (shoulder blades)
What are Long bones? Examples?
Longer than wide, crucial for movement. ; Rigid levers acted upon by muscles
-Located in the arm and forearm, thigh and leg, palms, soles, fingers, and toes
What are Short bones? Examples?
Equal length and width, allow gliding movements. -Glide across one another in multiple directions
-Ex. the carpal bones (wrists) and tarsal bones (ankles)
What are Irregular bones? Examples?
Complex shapes, do not fit other categories.
-Ex. vertebrae that form the spinal column, the bones of the pelvis, and several bones in the skull
What are Sutural bones? Examples?
Small, flat bones between skull flat bones. (joints)
What are Sesamoid bones? Examples?
Small, round bones developed inside tendons.
Patella
What are Dynamic tissues
Living tissues that interact with organ systems.
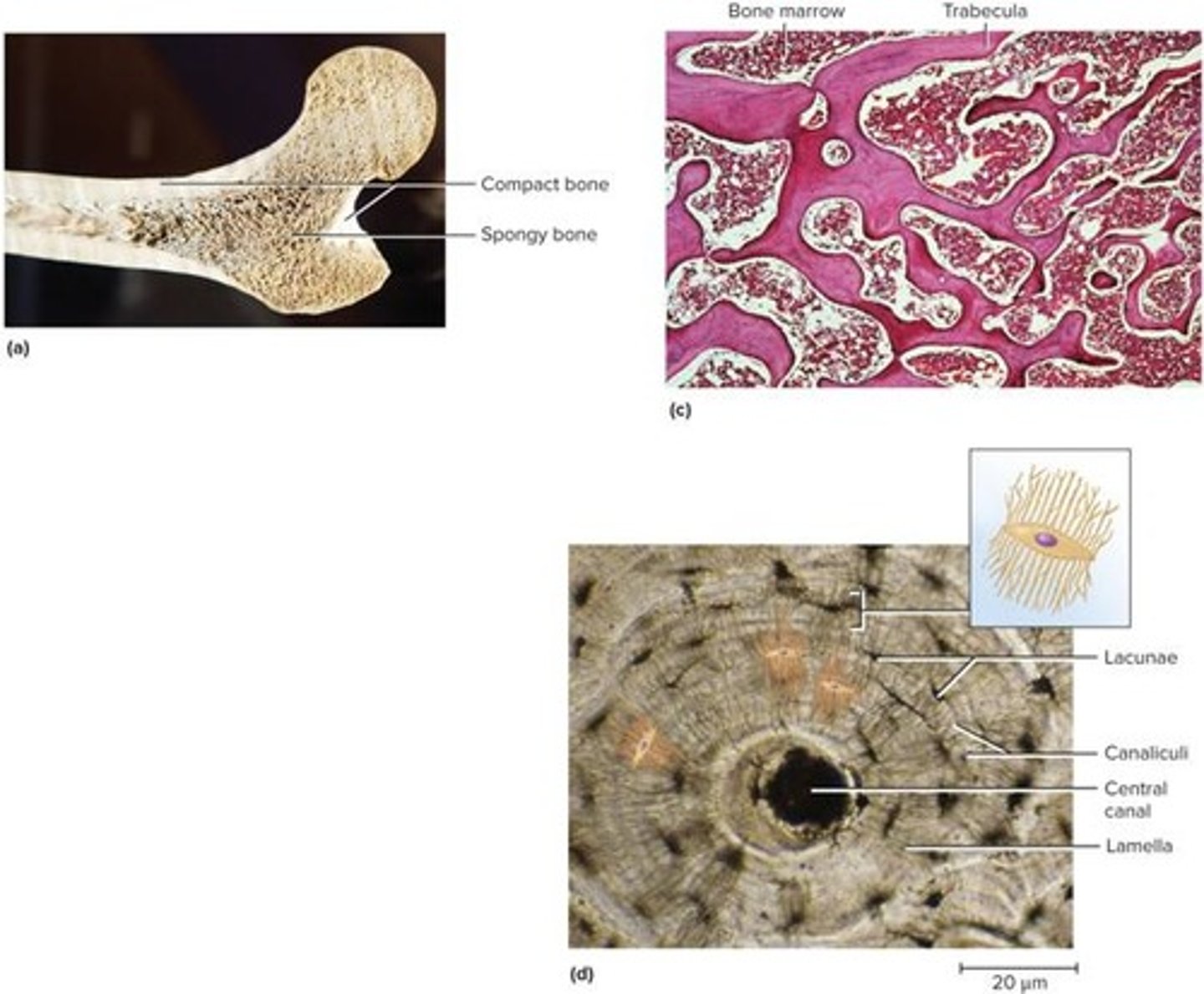
What is Compact bone
Dense outer shell providing strength.
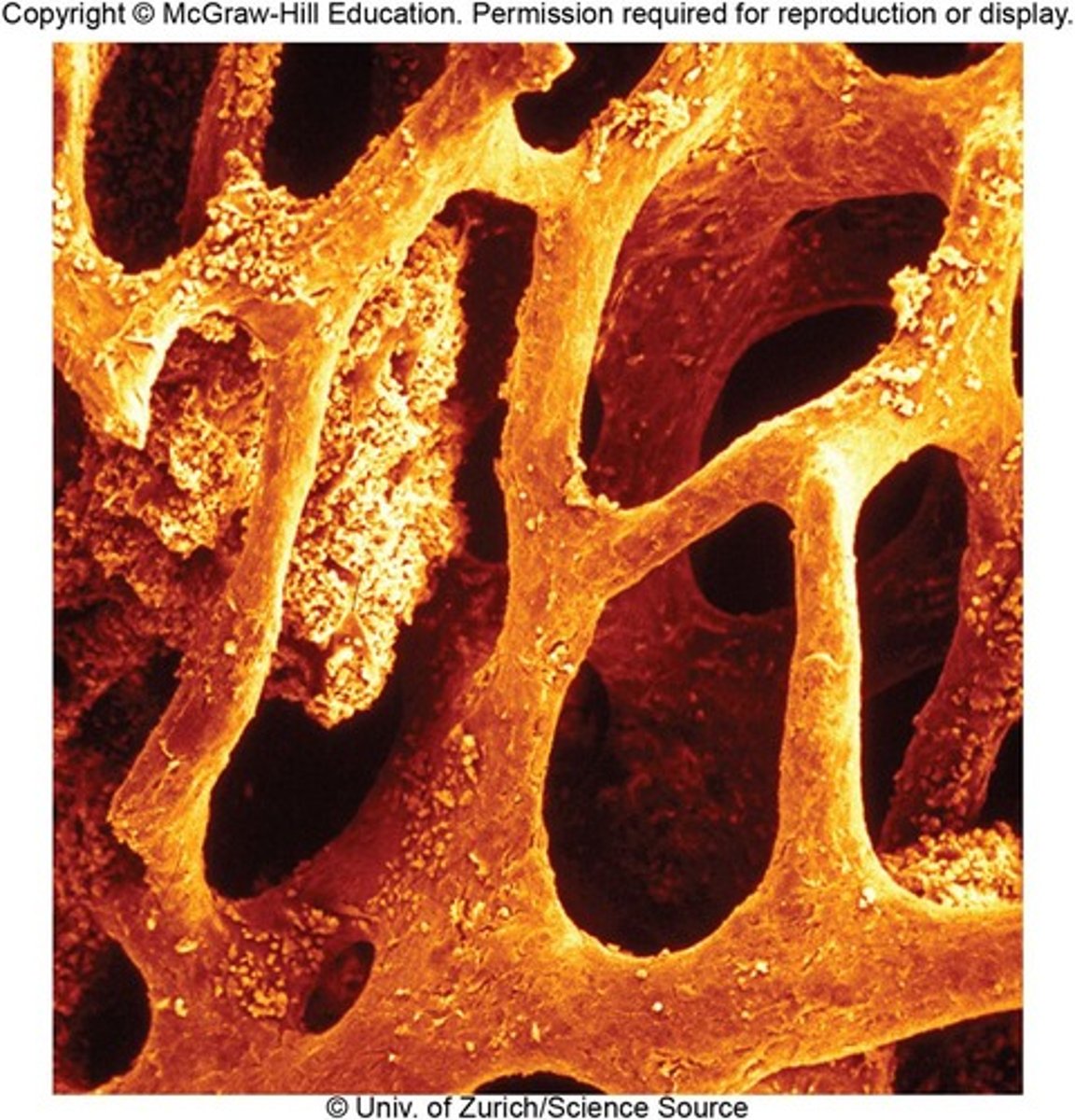
What is Spongy bone
Loosely organized bone tissue, lighter.
-Found in center of ends and center of shafts of long bones and in middle of nearly all others
-Covered by more durable compact bone
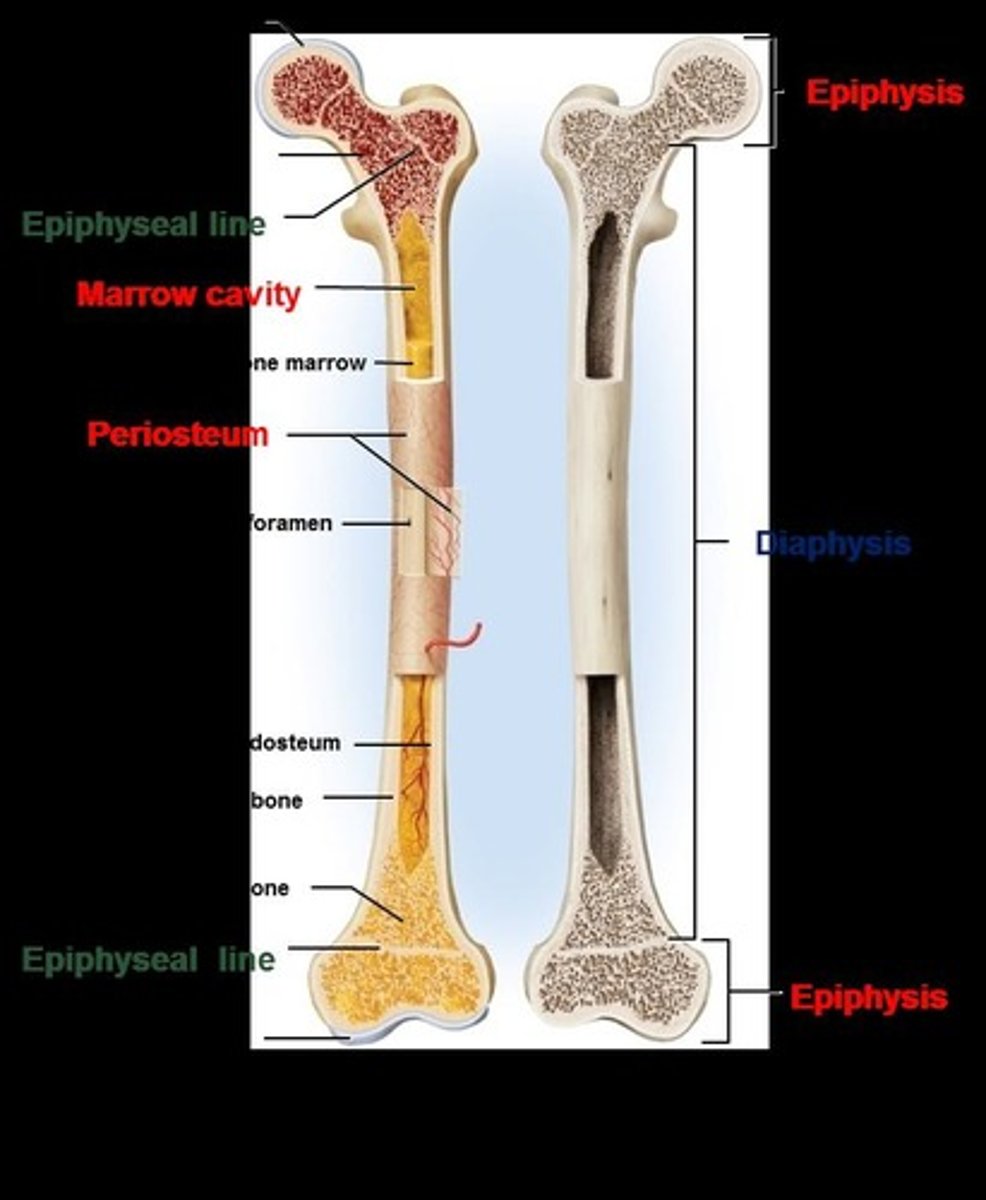
What are long bone features?
-Diaphysis — shaft that provides leverage
•Medullary cavity (marrow cavity)—space in the diaphysis of a long bone that contains bone marrow
-Epiphyses — enlarged ends of a long bone
•Strengthen joint and anchor ligaments and tendons
Extra info about General features of Bones?
Spongy bone= a lot of red marrow
skeleton = 3/4 compact 1/4spongy bone
compact= does not break easily
What is the Articular cartilage
layer of hyaline cartilage that covers the joint surface; allows joint to move more freely, friction-free
EX.N=
articulation= touch
damage to cartilage= arthritis
No articular cartilage in head bc don't want brain moving
hyaline cartilage = take abuse
What is the Nutrient foramina
Minute holes allowing blood vessel penetration.
EX. N.=
foramina=holes, deliver nutrients break down nutrient to put in bloodstream
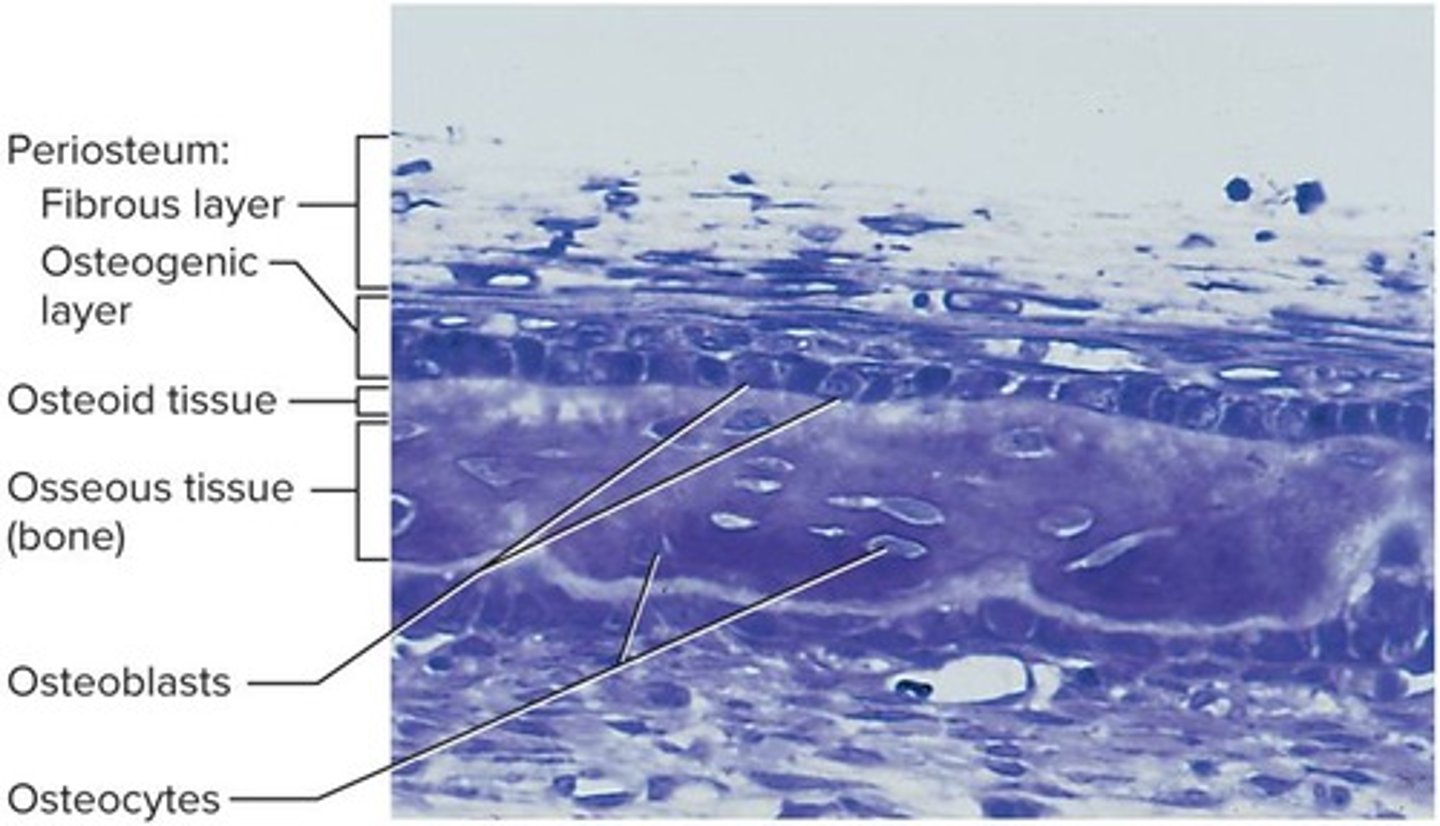
What is the Periosteum
external sheath covering most of bone
-Outer fibrous layer of collagen
•Some fibers continuous with tendons
•Perforating (Sharpey) fibers — outer fibers penetrate into bone matrix
-Inner osteogenic layer of bone-forming cells
•Important to bone growth and healing of fractures
Extra notes: damage = slowed growth
What is the Endosteum?
Thin layer of reticular connective tissue lining marrow cavity
-Has cells that dissolve osseous tissue and others that deposit it
Epiphyseal plate
Area of hyaline cartilage that separates epiphyses and diaphyses of children's bones
-Enables growth in length
-Epiphyseal line — in adults, a bony scar that marks where the growth plate used to be
Extra Notes : You can grow bc of chondrocyte
bone growth via hyaline cartilage
Ca + phosphate harden= done growing.
Features of long bone
Epiphyses and diaphysis
Compact and Spongy
Marrow cavity
Articular Cartilage
Periosteum
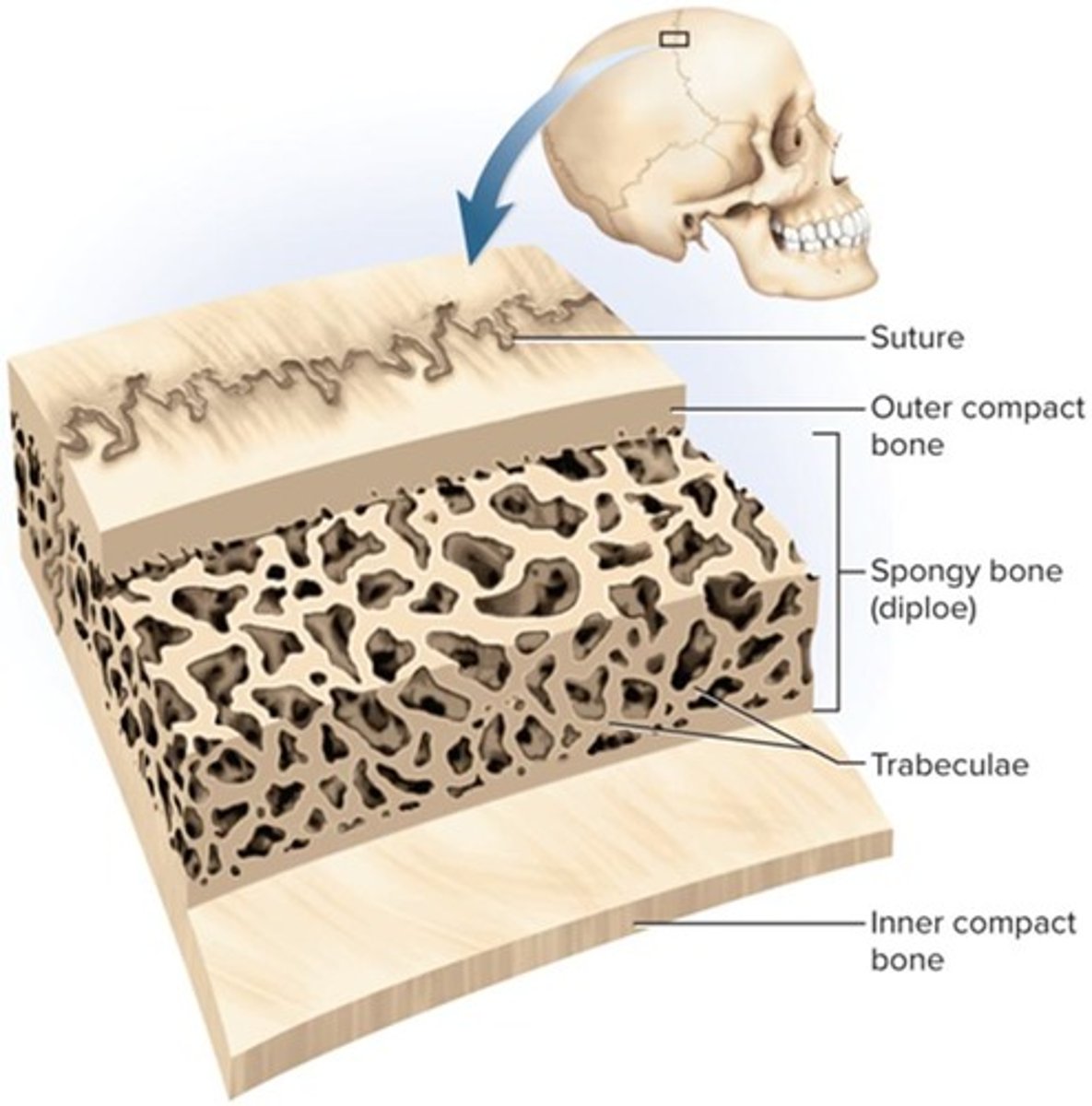
General features of Flat bone?
-Sandwich-like construction
Two layers of compact bone enclosing a middle layer of spongy bone
Both surfaces covered with periosteum
Diploe — spongy middle layer
•Absorbs shock
Marrow spaces lined with endosteum
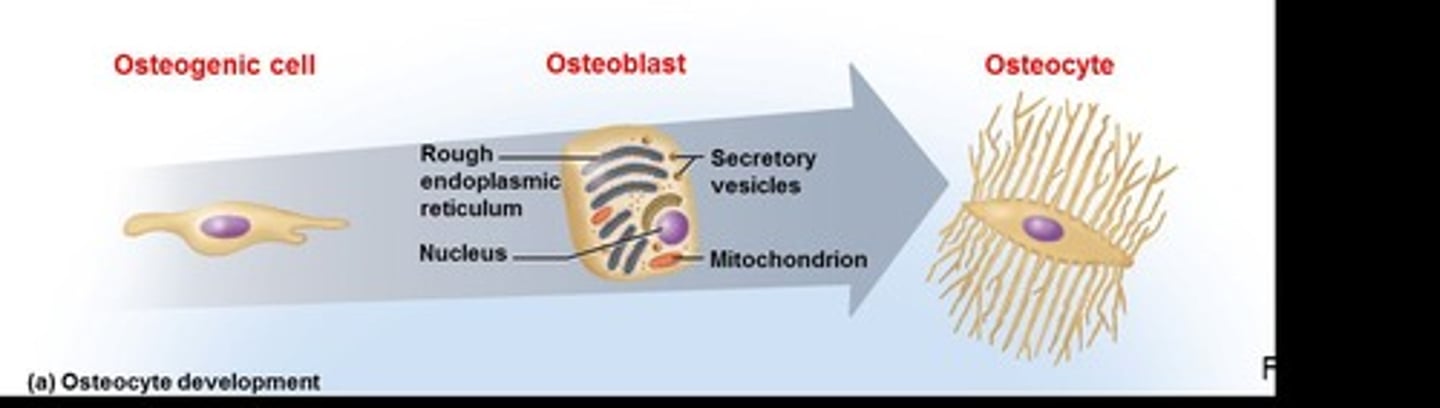
What are the four principal types of bone cells?
Osteogenic cells- bone stem cell
Osteoblasts- building
Osteocytes- Mature bone cell=solidify= calcium + phosphate--> remodels based on needs
Osteoclasts- bone dissolving cells
What are osteogenic cells and function?
stem cells found in endosteum and inner layer of periosteum
-Arise from embryonic mesenchyme
Multiply continuously and give rise to most other bone cell types
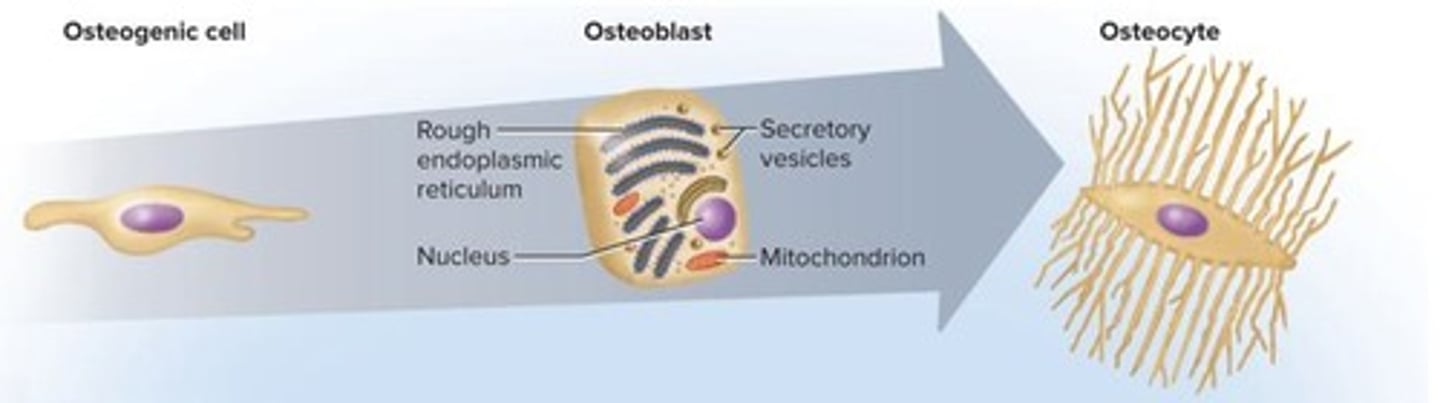
What are Osteoblasts
Bone building cells
-Form single layer of cells under endosteum and periosteum
-Nonmitotic (no mitosis)
-Synthesize soft organic matter of matrix which then hardens by mineral deposition
-Stress stimulates osteogenic cells to multiply rapidly and increase the number of osteoblasts which reinforce bone
-Secrete hormone osteocalcin
•Stimulates insulin secretion of pancreas
•Increases insulin sensitivity in adipocytes which limits the growth of adipose tissue
EX.N=
stressing body through HIIT--> Ca+ Phosphate deposited --> prevent osteoporosis
What are Osteocytes
former osteoblasts that have become trapped in the matrix they deposited
-Lacunae — tiny cavities where osteocytes reside
-Canaliculi — little channels that connect lacunae
-Cytoplasmic processes of osteocytes reach into canaliculi and contact processes of neighboring cells
•Gap junctions allow for passage of nutrients, wastes, signals
-Some osteocytes reabsorb bone matrix while others deposit it
-Contribute to homeostatic mechanism of bone density and calcium and phosphate ions
-Act as strain sensors — when stressed, produce biochemical signals that regulate bone remodeling (shape and density changes that are adaptive) EX: bump on head bc of phone (evolution)
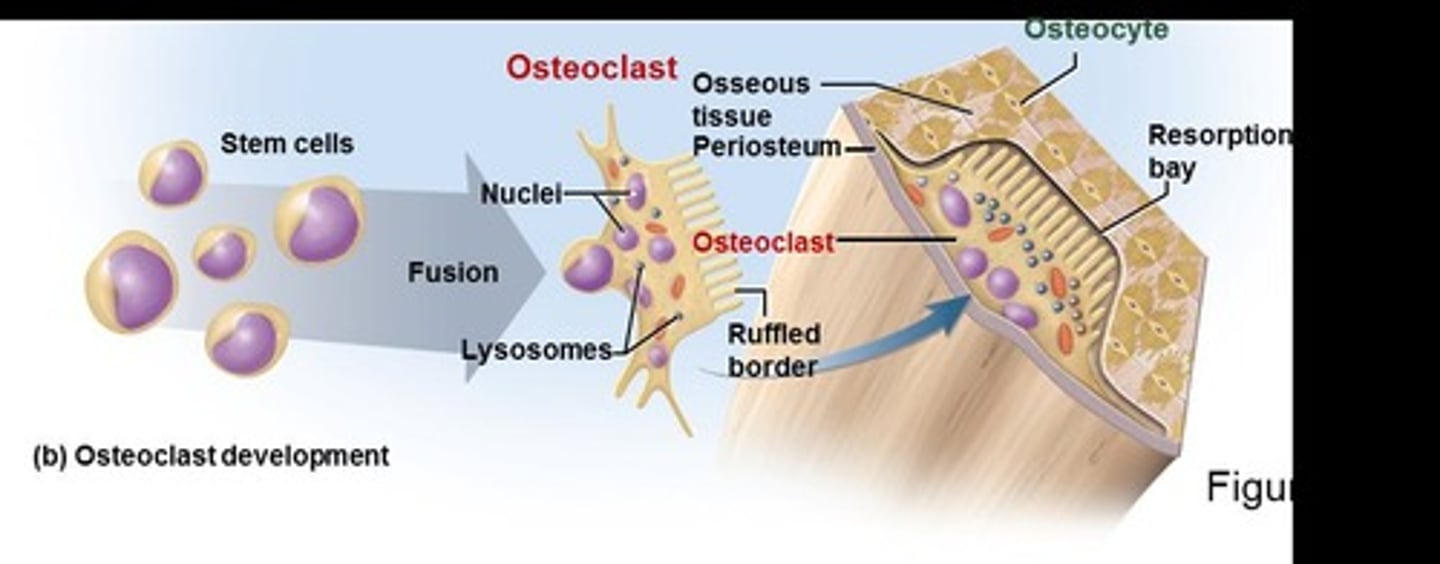
What are Osteoclasts?
bone-dissolving cells found on bone surface
-Osteoclasts develop from same bone marrow stem cells that give rise to blood cells (different origin from other bone cells)
-Very large cells formed from fusion of several stem cells
•Have multiple nuclei in each cell (3-4 nuclei, up to 50)
-Ruffled border (large surface area) faces bone - Several deep infoldings of the plasma membrane which increases surface area and resorption efficiency
-Cells often reside in resorption bays (pits in bone surface)
-Dissolving bone is part of bone remodeling
What is the Matrix of osseous tissue and function?
dry weight, about one-third organic and two-thirds inorganic matter
•Organic matter — synthesized by osteoblasts
-Collagen, carbohydrate - protein complexes, such as glycosaminoglycans, proteoglycans, and glycoproteins
•Inorganic matter
-85% hydroxyapatite (crystallized calcium phosphate salt)
-10% calcium carbonate
-Other minerals (fluoride, sodium, potassium, magnesium)
What makes bone a composite material?
a combination of a ceramic and a polymer
-Hydroxyapatite and other minerals are the ceramic and collagen (protein) is the polymer
-Ceramic portion allows the bone to support body weight without sagging
-Polymer (protein) gives some flexibility
What is rickets?
disease caused by mineral deficiency and resulting in soft, deformed bones (malleable bones)
Osteogenesis imperfecta
Brittle bone disease due to collagen defect.
What are Osteons?
Haversian systems in compact bone structure.
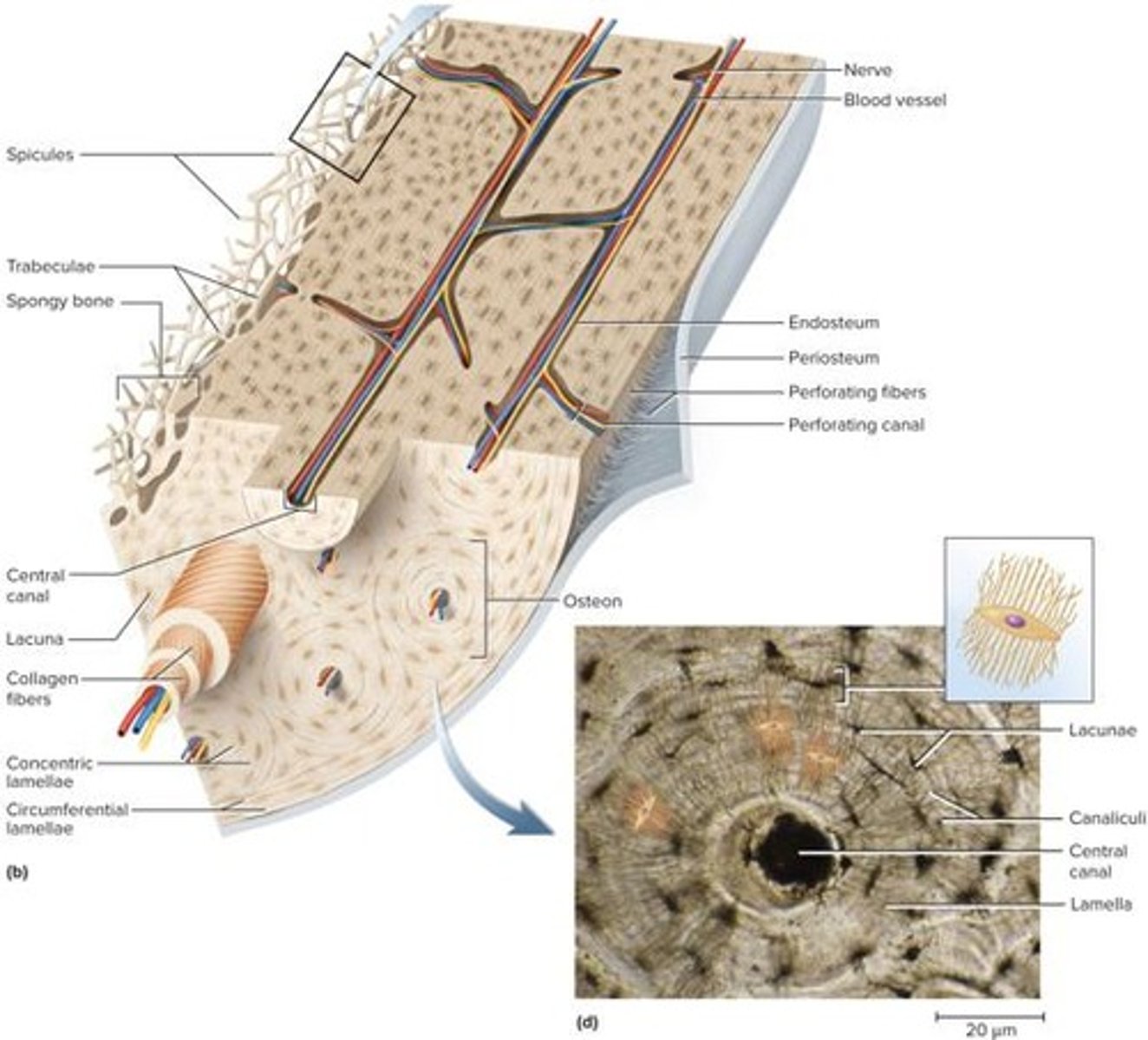
what are Perforating canals
Transverse passages connecting central canals.
what are circumferential lamellae?
fill outer region of dense bone
What are interstitial lamellae?
fill irregular regions between osteons
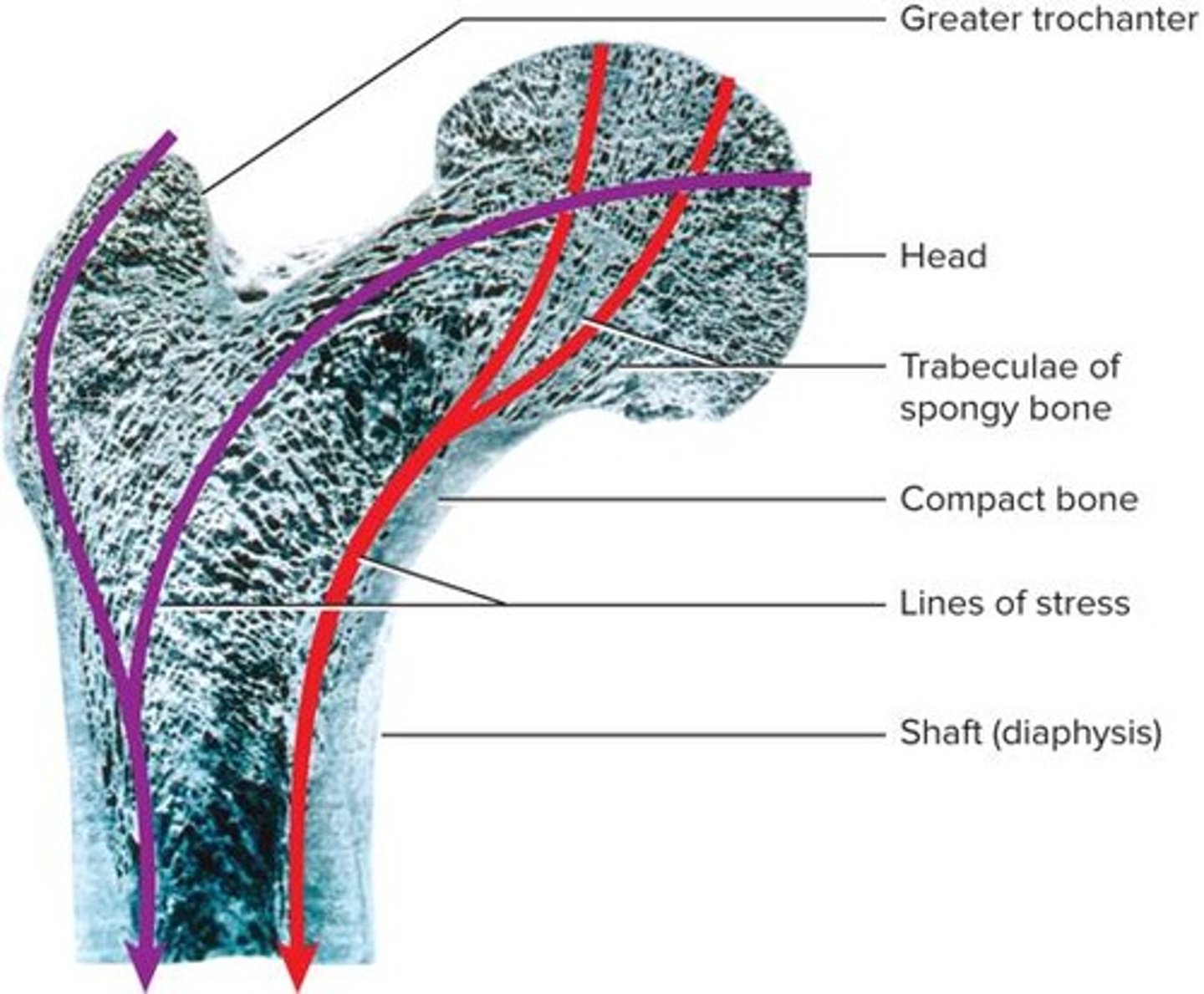
What does spongy bone consist of?
-Lattice of bone covered with endosteum
•Slivers of bone called spicules
•Thin plates of bone called trabeculae
-Spaces filled with red bone marrow
•Few osteons and no central canals
-All osteocytes are close to bone marrow
•Provides strength with minimal weight
Trabeculae
develop along bone's lines of stress
Gives strength in endosteum
what is Bone marrow?
soft tissue occupying marrow cavities of long bones and small spaces (trabeculae) of spongy bone
Red marrow (myeloid tissue)
-Contains hemopoietic tissue—produces blood cells
-In nearly every bone in a child
-In adults, found in skull, vertebrae, ribs, sternum, part of pelvic girdle, and proximal heads of humerus and femur
Yellow marrow found in adults
-Most red marrow turns into fatty yellow marrow
-Fatty marrow that does not produce blood
Can transform back to red marrow in the event of chronic anemia
Ex N-
children reb bone marrow --> more blood--> more o2 ---> more energy
anemic conditions can turn yellow back to red.
What is ossification or osteogenesis
Formation of bone
What are the two methods that bone develops in human fetus and infants?
-Intramembranous ossification
•Produces flat bones of skull and clavicle in fetus
•Thickens long bones throughout life
-Endochondral ossification
What are the 4 steps of intermembranous ossification
1)Deposition of osteoid tissue into embryonic mesenchyme
2)Calcification of osteoid tissue and entrapment of osteocytes
3)Honeycomb of spongy bone with developing periosteum
4)Filling of space to form compact bone at surfaces, leaving spongy bone in middle
Dogs Can Have Fun
What is Endochondral ossification?
During infancy and childhood, the epiphyses fill with spongy bone
•Cartilage is limited to the articular cartilage covering each joint surface and to the epiphyseal plate
-A thin wall of cartilage separating the primary and secondary marrow cavities
-Epiphyseal plate persists through childhood and adolescence
-Serves as a growth zone for bone elongation
By late teens to early 20s, all remaining cartilage in the epiphyseal plate is generally consumed
-Gap between epiphyses and diaphysis closes (metaphysis - epiphyseal line)
-Primary and secondary marrow cavities unite into a single cavity
-Bone can no longer grow in length
EX. N
line = done growing
gap= growth opportunities
chondrocytes= bone growth
What does ossification continue to do throughout life?
growth and remodeling of bones
length and width
What are the zones of the Metaphysis (5)
The region between diaphysis and epiphysis in growing bones.
1)Zone of reserve cartilage Typical histology of resting hyaline cartilage
(RESTING)
2)Zone of cell proliferation Chondrocytes multiplying and lining up in rows of small flattened lacunae
MORE OF ITS MULTIPLY CHONDROCYTES
3)Zone of cell hypertrophy Cessation of mitosis; enlargement of chondrocytes and thinning of lacuna walls
(GROW IN SIZE)
4)Zone of calcification Temporary calcification of cartilage matrix between columns of lacunae
(SOLIDIFYING)
5)Zone of bone deposition Breakdown of lacuna walls, leaving open channels; death of chondrocytes; bone deposition by osteoblasts, forming trabeculae of spongy bone
( MATURE BONE)
What is appositional growth ?
occurs at bone surface
-Continual growth in diameter and thickness
-Intramembranous ossification
-Osteoblasts of inner periosteum deposit osteoid tissue
•Become trapped as tissue calcifies
-Lay down matrix in layers parallel to surface
•Forms circumferential lamellae
•Osteoclasts of endosteum enlarge marrow cavity
With bone enlongation what happens to the Epiphyseal plate?
cartilage transitions to bone
-Functions as growth zone where bone elongates
-Has typical hyaline cartilage in the middle with transition zones on each side where cartilage is replaced by bone
What is Interstitial Growth
Growth from within the epiphyseal plate.
-Bone elongation is a result of cartilage growth within the epiphyseal plate
Epiphyses close when cartilage is gone — epiphyseal line of spongy bone marks site of former epiphyseal plate
•Lengthwise growth is finished
•Occurs at different ages in different bones
Ex.N
Toddler=megamind to protect the brain
what happens with Bone Remodeling
Absorption and deposition throughout life.
-Repairs microfractures, releases minerals into blood, reshapes bones in response to use and disuse
•Remodeling is a collaborative and precise action of osteoblasts and osteoclasts
•Bony processes grow larger in response to mechanical stress
what is Wolff's Law
Bone architecture determined by mechanical stresses.
osteoclasts breaks to allow shifting (braces)
what is Dwarfism, and the 2 types?
Abnormal short stature due to growth issues.
Achondroplastic Dwarfism
Pituitary Dwarfism
what is Achondroplastic Dwarfism
Long bones stop growing; normal torso.
•Normal torso, short limbs
-Failure of cartilage growth in metaphysis
-Spontaneous mutation produces mutant dominant allele
Pituitary Dwarfism
Lack of growth hormone; normal proportions with short
stature
what is the physiology of osseous tissue?
A mature bone remains a metabolically active organ
-Involved in its own maintenance of growth and remodeling
-Exerts a profound influence over the rest of the body by exchanging minerals with tissue fluid
What happens if there is a disturbance of calcium homeostasis in the skeleton?
• disrupts function of other organ systems
-Especially nervous and muscular
What is Mineral deposition (mineralization)?
process in which calcium, phosphate, and other ions are taken from blood and deposited in bone
-Osteoblasts produce collagen fibers that spiral the length of the osteon
-Fibers become encrusted with minerals that harden the matrix
•Hydroxyapatite crystals form at solubility product — critical level of calcium times phosphate concentration
•First few crystals act as seed crystals that attract more calcium and phosphate from solution
What is Abnormal calcification (ectopic ossification)?
formation of a calculus (calcified mass) in another soft organ such as a lung, brain, eye, muscle, tendon, or
artery (arteriosclerosis)
caused by injury usually
EX.N
elastic cartilage hardens- cauliflower ear
ateriosclerosis= less blood flow , stretched more than usual, calcium+phospahte to fill tear= plaque, can lead to death.
lung solidifying= cant get o2--> no energy= death.
What is Mineral resorption
process of dissolving bone and releasing minerals into blood
-Performed by osteoclasts at ruffled border
-Hydrogen pumps in membranes secrete hydrogen into space between osteoclast and bone surface
-Chloride ions follow by electrical attraction
-Hydrochloric acid (pH 4) dissolves bone minerals
-Acid protease enzyme digests collagen
ex.N braces = -Tooth moves because osteoclasts dissolve bone ahead of tooth; osteoblasts deposit bone behind the tooth
Why is calcium homeostasis important?
•Calcium and phosphate are used for much more than bone structure
•Phosphate is a component of DNA, RNA, ATP, phospholipids, and pH buffers
•Calcium needed in neuron communication, muscle contraction, blood clotting, and exocytosis
•Minerals are deposited in the skeleton and withdrawn when they are needed for other purposes
•Total of about 1,100 g of calcium in adult body with 99% of it in bones
-Most exists as part of hydroxyapatite, but a little is in a form that is easily exchanged with the blood
-About 18% of skeletal calcium is exchanged with blood each year
•Normal calcium concentration in blood plasma is 9.2 to 10.4 mg/dL
-45% as Ca^(2+) that can diffuse across capillary walls and affect other tissues
-Rest in reserve, bound to plasma proteins
What is Hypocalcemia?
Deficient calcium levels causing nervous system excitability.
-Changes membrane potentials and causes overly excitable nervous system and tetany (muscle spasms)
•Laryngospasm can cause suffocation
-Caused by vitamin D deficiency, diarrhea, thyroid tumors, underactive parathyroid glands
-Pregnancy and lactation increase risk of hypocalcemia
-Accidental removal of parathyroid glands during thyroid surgery ( losing parathyroid gland = cant regulate calcium level--> death)
Ex. N
can't absorb calcium without vitamin D
What is Hypercalcemia?
Excessive calcium levels leading to reduced nerve excitability.
-Makes ion channels less responsive and thus nerve and muscle are less excitable
•Can cause emotional disturbance, muscle weakness, sluggish reflexes, cardiac arrest
-Hypercalcemia rarely occurs
What things does calcium homeostasis depend on?
Dietary intake
uniary and fecal losses
exchanges between osseous tissue
What three hormones regulate calcium homeostasis?
-Calcitriol, calcitonin, and parathyroid hormone
What is Calcitriol
Hormone that raises blood calcium levels.
•most active form of vitamin D
•Produced by actions of skin, liver, and kidneys
-Epidermal keratinocytes use UV radiation to convert
7-dehydrocholesterol to previtamin D_3; warm sun on skin converts this to vitamin D_3
-Liver adds hydroxyl group converting that to calcidiol
-Kidney adds hydroxyl group converting that to calcitriol
it increases calcium absorption by small intestine
-It also increases calcium resorption from the skeleton
•Stimulates osteoblasts to release RANKL, a chemical that stimulates production of more osteoclasts
-It weakly promotes kidney reabsorption of calcium ions, so less lost in urine
-Calcitriol is also necessary for bone deposition—helping provide adequate calcium and phosphate
-Inadequate calcitriol results in abnormal softness of bones in children (rickets) and in adults (osteomalacia)
What does calcitriol synthesis and action look like
Skin --> blood-->liver add OH di ---> Kidney add another OH ---> tri---> absorb calcium.
What is Calcitonin?
Hormone lowering blood calcium by inhibiting osteoclasts.
— secreted by C cells (clear cells) of thyroid gland when blood calcium levels rise too high
•Lowers blood calcium concentration in two ways:
-Inhibits osteoclasts thereby reducing bone resorption
-Stimulates osteoblasts to deposit calcium into bone
•Important in children, weak effect in adults
-Osteoclasts more active in children due to faster remodeling
May inhibit bone loss in pregnant and lactating women
What is Parathyroid Hormone (PTH)
•secreted by parathyroid glands on posterior surface of thyroid
•PTH released when calcium levels low in blood
PTH raises calcium blood level by four mechanisms
-Stimulates osteoblasts to secrete RANKL, thereby increasing osteoclast population and bone resorption
-Promotes calcium reabsorption by kidneys, so less lost in urine
-Promotes the final step of calcitriol synthesis in the kidneys, enhancing calcium-raising effect of calcitriol
-Inhibits collagen synthesis by osteoblasts, inhibiting bone deposition
Negative Feedback Loop
Mechanism correcting calcium level imbalances. for both hypecalcemia and hypocalcemia
Why is phosphate homeostasis important ?
•Average adult has 500 to 800 g phosphorus with 85% to 90% of it in the bones
•Normal plasma concentration is 3.5 to 4.0 mg/dL
•Occurs in two main forms
-HPO_4^(2-) and 〖H_2 PO〗_4^- (monohydrogen and dihydrogen phosphate ions)
•Phosphate levels are not regulated as tightly as calcium levels
•Calcitriol raises phosphate levels by promoting its absorption by small intestine
•PTH lowers blood phosphate levels by promoting its urinary excretion
What other factors affect Bone Growth?
Hormones and vitamins influencing bone development.
•Bone growth especially rapid in puberty and adolescence
-Surges of growth hormone, estrogen, and testosterone occur and promote ossification
-These hormones stimulate multiplication of osteogenic cells, matrix deposition by osteoblasts, and chondrocyte
multiplication and hypertrophy in metaphyses
EX.N
estrogen =more growth
Extra Notes abt bone growth
Bone growth especially rapid in puberty and adolescence (Continued)
-Girls grow faster than boys and reach full height earlier
•Estrogen has stronger effect than testosterone on bone
growth
-Males grow for a longer time and also taller
•Anabolic steroids cause growth to stop
-Epiphyseal plate "closes" prematurely
-Results in abnormally short adult stature
what is orthopedics?
branch of medicine dealing with prevention and correction of injuries and disorders of bones, joints, and muscles
•Includes the design of artificial joints and limbs and the treatment of athletic injuries
what is a Fracture?
Breaks in bone due to stress or trauma.
what is a pathological fracture?
break in a bone weakened by disease (such as bone cancer or osteoporosis)
-Usually caused by a stress that would not break a healthy bone
What are the classifications of fractures based on structural characteristics 3
-Direction of fracture line
-Break in the skin
-Multiple pieces
•Example: comminuted—three or more pieces
What are the 9 major factures types
•Transverse fractures
•Displaced fractures
•Compression fractures
•Spiral fractures
•Epiphyseal fractures
•Comminuted fractures
•Greenstick fractures
•Colles fractures
•Pott's fractures
"The Doctor Can Spot Every Crack, Gap, Chip, Problem."
what ate the general categories of fractures?
Closed or simple
•Completely internal (no break in skin)
•Only seen on x-rays
Open or compound
Project through the skin
•More dangerous due to:
•Infection
•Uncontrolled bleeding
What is a transverse fractures ?
•Break shaft across long axis
What is a Spiral fractures
•Produced by twisting stresses
Spread along length of bone
What is a Displaced fracture
•Produce new and abnormal bone arrangements
•Nondisplaced fractures retain normal alignment
what is a Compression fracture
Occurs in vertebrae under extreme stress.
Often associated with osteoporosis
What is a Greenstick fracture
One side broken, one side bent; common in children.
•Long bones have yet to fully ossify
What is a Comminuted fractures
Shatter affected area producing fragments
What is a Epiphyseal fracture
•Occur where bone matrix is calcifying
•A clean transverse fracture of this type heals well
•If not monitored, breaks between epiphyseal plate and cartilage can stop growth at site
Fix quickly*
What is a Pott's fracture
Bimalleolar fracture at the ankle.
•Occurs at ankle and affects both medial malleolus and lateral malleolus
What is a Colles fracture
Break in the distal radius.
What is the healing process of fractures
1)The Hematoma formation
hematoma is converted to granulation tissue by invasion of cells and blood capillaries.
2)Soft callus formation
Deposition of collagen and fibrocartilage converts granulation tissue to a soft callus.
3)Hard callus formation-
Osteoblasts deposit a temporary bony collar around the fracture to unite the broken pieces while ossification occurs.
4)Bone remodeling-
Small bone fragments are removed by osteoclasts, while osteoblasts deposit spongy bone and then convert it to compact bone.
bone wont break in same spot