Heart rate and blood pressure
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
20 Terms
Cardiac Cycle (heart beat)
Systole (Ventricles contract - Expel Blood)
Diastole (Ventricles relax - Filling)
Heart Rate
Frequency of Cardiac Cycle measured in Beats Per Minute (BPM)
Measuring Heart Rate
Electrocardiogram (ECG)
“Gold Standard”
Auscultation
Listening to heart beat (e.g. Stethoscope)
3rd intercostal space, left of sternum
Palpation
Feeling heart beat
Brachial, Carotid, Radial, and Temporal arteries
Auscultation
Insert ear tips in ears so the tips point forward/down
Gently tap the diaphragm to test for sound
Position the stethoscope just below the left pectoralis major muscle firmly against the skin
3rd intercostal space, left of sternu,
Start counting

HR Palpation Technique
Use tips of index and middle fingers (thumb have a pulse)
Apply light pressure to find a string pulse
Don;t be afraid to move around
Start stopwatch sumultaneously with pulse beat
Count the number of beats you hear / feel
1st beat is zero
Heart Rate = # of beats counted in 20 seconds x 3
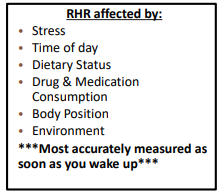
Resting Heart Rate
Heart Rate when you are at complete rest
Not Always, indicative of cardiorespiratory fitness
Measure for 30 sec x 2
Classification
Bradycardia (<60 bpm)
Normal (60-100 bpm)
Tachycardia (>100 bpm)
Exercising Heart Rate
Steady-state HR – after about 3 min, a difference in HR of no more than 5 bpm during a 1 min. period
Measured via radial pulse palpation, auscultation with a stethoscope, or the use of HR monitors.
Radial pulse is most typical for palpation; Duration = 10 seconds
Post-Exercise
Hr can drop rapidly following exercise, begin timing pulse counts as quickly as possible
Average of 2-3 measures fro greater accuracy
Recovery Heart Rate
May take up to 30 minutes for HR to return to RHR
What is the minimum amount of time needed for a cool down?
◦ Minimum of 3 minutes cool down (~110 BPM)
◦ BEST is 1 minute at 85% intensity, 1 minute at 65% , 1 minute at 45%
The rate of reduction is associated with CVD risk
Less than 12 BPM reduction (at 1 Minute) = Increased risk for CVD
More than 50 BPM reduction (at 1 Minute) = Reduced risk for CVD
Also guides progress and can help identify overheating or dehydration (viscosity)
Maximal Heart Rate
The highest heart rate value attainable during an all-out effort to the point of exhaustion.
Age related decline may range from 3 – 7%
Disease and sedentary behavior increase the speed of decline
Determing Maximal Heart Rate
Direct Measurement
Measuring heart reate during maximal effort (typically during maximal exercise test)
Indirect Measurement
Prediction Equations
Fox and Haskell (1971): HRmax = 220 - Age
Inbar (1994): 205.8-[0.685 x Age]
Tanake et al. (2001): Hrmax =208-[0.7 x Age]
Nes (2012): 211 - 0.64 x Age
Cardiac Output - CO or Q
is the total amount of blood pumped by the heart per minute
CO and blood Pressure are also related
An increase in CO will result in an increase in BP
Typical Values
Males: 5.6 L/min
Females: 4.9 L/min
CO =SV x HR
Stroke Volume
The volume of blood pumped out of the left ventricle of the heart in one heart beat.
◦ Typical Value = 70 ml; 55 – 100 ml
Determinants
Gender (Men > Women)
Heart Size
Training Status C
ontractility of heart
Duration of Contraction
◦ (normal = 0.8 seconds)
Pulse Pressure
Tells us about vascular compliance
Measures stress exerted on small arteries affecting nutrient exchange
Correlation with Heart Function (see Stroke Volume and Cardiac Output)
PP = Systolic Blood Pressure - Diastolic Blood Pressure
Rate Pressure Product
Refers to the ability of the heart to provide blood (and oxygen) to itself
RPP = HR x Systolic Pressure
Highly correlated to O2 consumption by heart
Improvement > Improved VO2 max
Mean Arterial Pressure
A useful concept because it can be usued to calculate overall blood flow
Average blood pressure or average arterial pressure during a single cardiac cycle
Estimation = DBP + 1/3 (SBP-DBP)
Points of Interest
Normal (77-97 mmHg)
Varies by location
Standing Person: Head = 62; Ankle = 180
Influences occurrence of Edema, Fainting, Athreosclerosis, Kidney Failure, and Aneursym
Measuring Blood Pressure
Sphygmomanometer
Gauge graduated in millimeters of mercury (mm Hg) attached to an inflatable cuff
Cuff is wrapped around the upper arm 1” above antecubital fossa and inflated to a pressure that will shut off the brachial artery.
Stethoscope used to listen to the sounds of blood flow in the brachial artery (1 cm superior and medial of the antecubital fossa)
Blood Pressure Reading
Systolic
Pressure on arterial wall when blood is being pumped from the left Diastolic
Pressure on arterial wall when the heart is at rest
The unit for expressing BP is mm Hg referring to the Mercury (Hg) used to measure BP in a sphygmomanometer
Inflating Cuff
Cuff should be inflated ~20 – 30mmHg over estimated SBP (1st Korotkoff sound)
….200 is always a safe bet with clinical populations
Estimating SBP
Use previous measurement
◦ During exercise, keep in mind that SBP increases
Palpate radial artery while inflating cuff
◦ SBP when pulse disappears
◦ Obtain estimate of SBP by palpating radial artery while inflating cuff.
◦ DBP is estimated by subsequently decreasing pressure by 2-3 mm Hg · s −1 and noting when the pulse reappears
BP Assessment procedures
1. Patients should be seated quietly for at least 5 min in a chair with back support (rather than on an examination table) with their feet on the floor and their arms supported at heart level. Patients should refrain from smoking cigarettes or ingesting caffeine for at least 30 min preceding the measurement.
2. Measuring supine and standing values may be indicated under special circumstances.
3. Wrap cuff firmly around upper arm at heart level; align cuff with brachial artery.
4. The appropriate cuff size must be used to ensure accurate measurement. The bladder within the cuff should encircle at least 80% of the upper arm. Many adults require a large adult cuff.
5. Place stethoscope chest piece below the antecubital space over the brachial artery.
6. Quickly inflate cuff pressure to 20-30 mm Hg above the estimated SBP previously determined via palpation
7. Slowly release pressure at rate equal to 2–3 mm Hg · s −1 .
8. SBP is the point at which the first “thud” or the Korotkoff sound is heard (phase 1), and DBP is the point before the disappearance of Korotkoff sounds (phase 5).
9. At least two measurements should be made (minimum of 1 min apart) and the average should be taken.
10. BP should be measured in both arms during the first examination. Higher pressure should be used when there is consistent interarm differences.
11. Provide to patients, verbally and in writing, their specific BP numbers and BP goals.
Measuring Exercise BP
Client should not grasp handlebars or handrails.
Have tubing protruding from bladder superior instead of inferior.
Stabilize client’s arm between your arm and trunk.
Position manometer at eye level.
Inflate cuff well above anticipated value.
Potential Sources of Error
1. Technician (Inexperience, auditory acuity, reaction time)
2. Faulty Equipment (Inaccurate Sphygmomanometer, Improper Cuff size)
3. Procedural Errors (Rate of inflation/deflation, Sphygmomanometer/Stethoscope placement, Allowing patient to hold something/flex elbow)
4. External Distractions (i.e. Background noise)
5. Certain physiologic abnormalities (e.g. damaged brachial artery, subclavian steal syndrome, arteriovenous fistula)
6. Client not properly positioned or gripping an item