Periapical Inflammatory Disease
Normal Radiographic Appearance
Alveolar bone
Periodontal ligament (radiolucent line)
Lamina dura
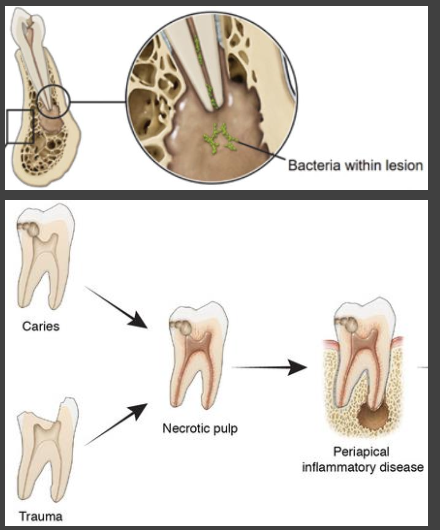
What is periapical inflammatory disease?
Local inflammatory response of bone around a tooth root
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
82 Terms
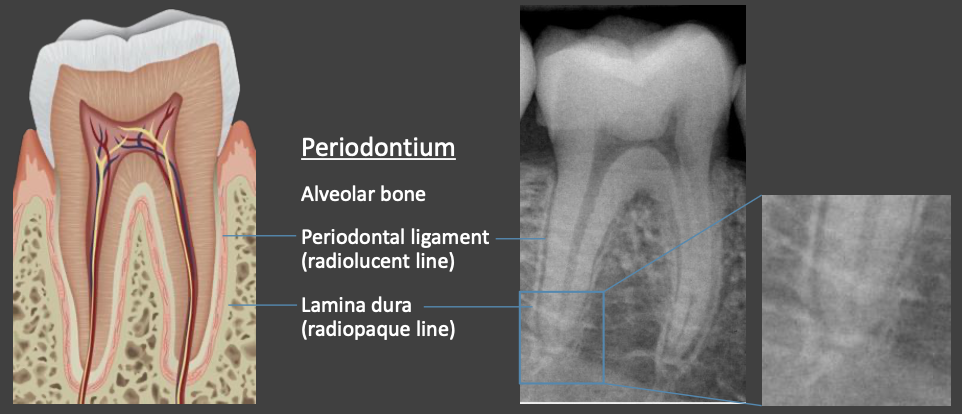
Normal Radiographic Appearance
Alveolar bone
Periodontal ligament (radiolucent line)
Lamina dura
What is periapical inflammatory disease?
Local inflammatory response of bone around a tooth root
What is the most common cause of periapical inflammatory disease?
Pulpal necrosis is most common cause
Secondary to bacterial, chemical, or physical trauma to pulp
Most commonly caries
What causes inflammation in PDL and bone?
Metabolites from necrotic pulp exit apex
What are the histopathological manifestation charactered by inflammatory infiltrate?
Abscess – collection of pus
Granuloma – formed when body attempts to isolate and eliminate inflammatory response
Cyst – entrapped epithelial cell rests of Malassez stimulated to proliferate a cyst lining
What structures cannot be differentiated by radiologic imaging?
Periapical abscess, granuloma, and cyst
Define apical periodontitis
Clinical diagnostic term used in endodontics
Inflammation of apical periodontium of pulpal origin
May or may not be apparent on imaging

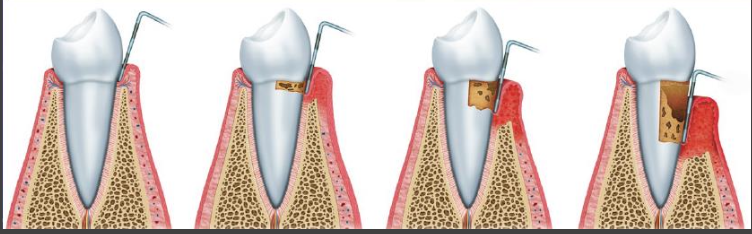
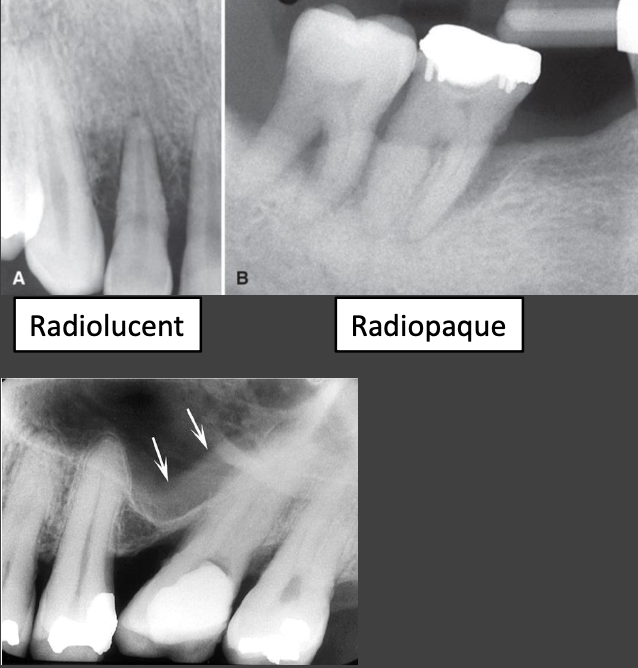
Define Rarefying Osteitis
Radiologic diagnosis for inflammatory process associated with bone resorption at tooth apex
Appears as localized area of increased radiolucency
Rarefying refers to loss of bone mineralization
Osteitis refers to inflammation of bone

Define Sclerosing (condensing) osteoitis
Radiologic diagnosis for inflammatory response associated with bone deposition around tooth apex
Appears as a relatively diffuse area of increased radiopacity
Sclerosing refers to increase in bone matrix density (hardening of bone)
Commonly occurs at periphery of an area of rarefying osteitis

What is the clinical presentation for periapical inflammatory disease?
It may not necessarily correlate with imaging findings and this is a trend with a lot of pathologies
What is the clinical presentation of acute periapical disease?
Severe pain and swelling
Pain to palpation and percussion
Tooth may become mobile
Drainage of pus through fistula or parulis may relieve pain
What is the clinical presentation of chronic periapical disease?
Potentially asymptomatic
Intermittent episodes of pain (acute exacerbations of chronic inflammatory response)
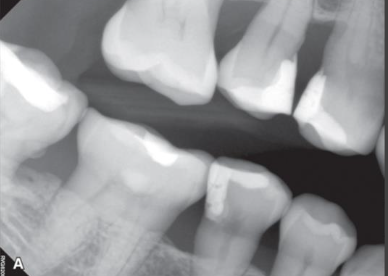
What is the main radiographic exam used to diagnose periapical lesions?
Intraoral periapical images
Panoramic – helps if lesion extent is beyond borders of PA
CBCT may be used if more severe condition beyond periapical inflammatory disease suspected
Useful for detecting periosteal new bone formation (osteomyelitis) and bone sequestra (osteonecrosis)
MDCT may be useful to evaluate soft tissue spread of infection
Spread into soft tissue spaces – abscess, cellulitis, Ludwig’s angina
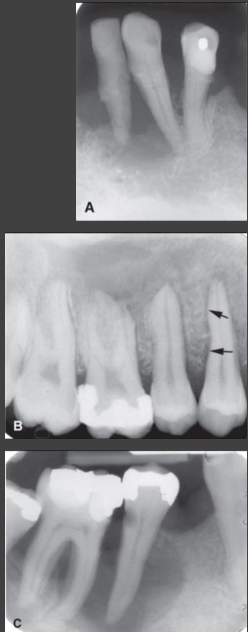
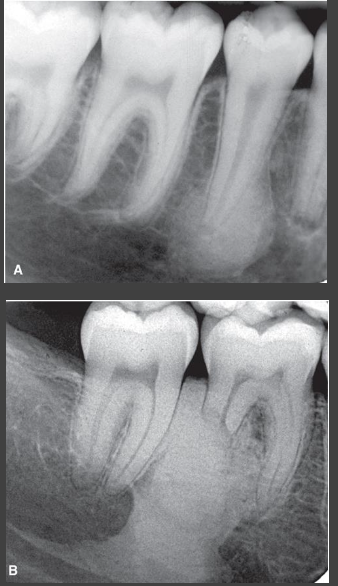
What are some radiographic features of a periapical lesion?
Vary depending on the disease stage
Early lesions
Little to no change
Diagnosis may rely on pulp vitality tests and clinical signs/symptoms
Lamina dura becomes less distinct or lost and PDL widens
Periapical radiolucency (PARL)
Longer-standing lesions
Radiolucent region at apex
More diffuse surrounding area of radiopacity

Where might you find a periapical inflammatory lesion?
Around apex or adjacent to apical 1/3 of root
Epicenter adjacent to apex of involved tooth
Migrates apically away from apex as lesion enlarges
Less commonly adjacent to root surface at the
exit of an accessory root canal
site of a perforation from root canal instrumentation
site of root fracture
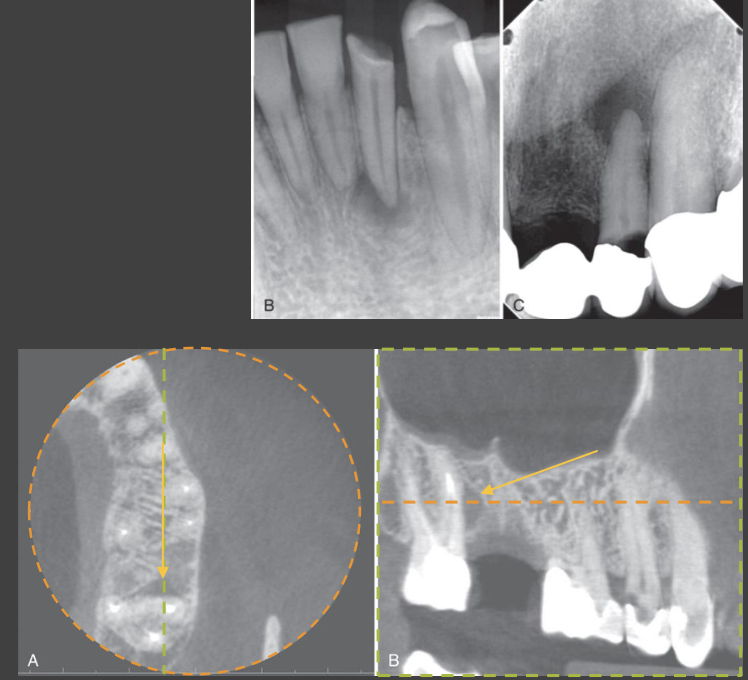
What should the periphery to a periapical inflammatory lesion look like?
Poorly to moderately well-defined
Smooth, hydraulic contour
Radiolucent area often has a radiopaque periphery with variably wide transition zone
Width depends on amount of sclerosis
Reflects chronicity of inflammation—bone deposition/density increases with time
Rarely well defined, corticated with a narrow zone of transition

What does the internal structure of a periapical inflammatory lesion look like?
Early changes may be masked by anatomic superimposition
Change not apparent until sufficient lamina dura and bone loss
Thickness of cortices particularly in mandibular posterior
Zygomatic process over maxillary molars
Earliest change: focal widening of apical PDL space
Loss of definition of the adjacent lamina dura
Most often totally radiolucent
No discrete internal mineralization
Occasionally entirely sclerotic (sclerosing osteitis), but usually some apical PDL space widening
What effects do periapical inflammatory lesions have on the surrounding structure?
Sclerosis (reactive bone formation)
Cortical erosion
Periosteal new bone formation
Odontogenic mucositis
Adjacent tooth resorption or hypercementosis
What is sclerosis?
Sclerotic bone reaction may include
Thicker than normal trabeculae
Increase in number of trabeculae per unit area
Reduction in size of marrow spaces and narrowing of minor vascular channels
Can reduce local blood supply
Can extend to adjacent teeth, non-tooth-bearing areas, or to bone borders

What is a periosteal reaction?
Early stages (small size) have little or no effects
Enlarges and extends to a bone border (cortex of mandible/maxilla, maxillary sinus)
Erodes or perforates the bone surface
Stimulates periosteal new bone formation (periosteal reaction)
Deposition of paired layers of new bone and connective tissue at surface
Halo pattern – adjacent to maxillary sinus (periostitis)
Onion skin pattern – at outer cortical bone surface
How does a periosteal reaction affect the periosteum?
Dense soft tissue lining floors of air cavities and covering bone surfaces
Inner osteogenic layer with mesenchymal stem cells
Outer connective tissue layer with fibroblasts and collagen
Sharpey fibers – extensions of collagen that anchor periosteum to bone surface
What else do you see in a periosteal reaction?
Inflammatory response travels through Haversian and Volkmann canal systems to bone surface
Response elevates/distends adherent periosteum (limited by Sharpey fibers)
Simulates stem cell differentiation into osteoblasts
New bone is deposited
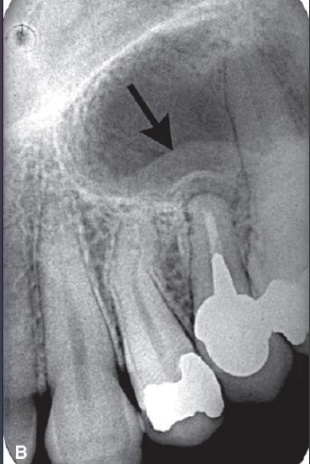
What is odontogenic mucositis?
thickening of mucosal lining (nasal cavity or maxillary sinus) stimulated by inflammatory mediators from periapical inflammatory disease
What are some effects on adjacent teeth?
Mirrors response of bone, may be asymmetric and nonuniform around root
Exteral resoption
Another effect on adjacent teeth, there is change in smooth, tapering root contour
Hypercementosis
Another effect on adjacent teeth, production of additional cementum; bulbous roots
What are some effects on adjacent deciduous teeth?
Displacement and/or disruption of erupting succedaneous (permanent) teeth
Differential diagnoses for periapical inflammatory disease
Types of periapical inflammatory lesions
Periapical/radicular cyst
Periapical granuloma
Normal Anatomy (mental foramen, incisive foramen)
Dense bone island (DBI; idiopathic osteosclerosis)*
Other pathology
Periapical cemento-osseous dysplasia (PCOD)*
Malignancy

What is Periapical Cemento-Osseous Dysplasia?
Imaging characteristics cannot reliably differentiate early radiolucent PCOD from periapical inflammatory disease
Diagnosis may rely on clinical exam
Tooth adjacent to PCOD will be vital
Tooth with periapical inflammatory disease will be nonvital
More mature PCOD lesions demonstrate central internaln radiopacities
External root resorption is more common in inflammation than PCOD
PCOD commonly associated with hypercementosis
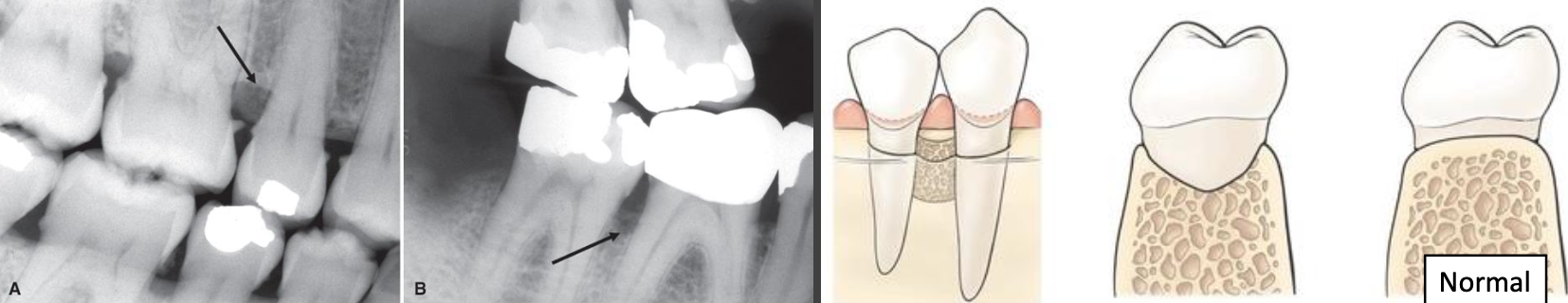
What is Dense Bone Island?
Can mimic sclerosing osteitis
Normal PDL space
Occasionally can cause root resorption
Associated tooth tests vital
Narrow transition zone
Periphery is smoother and uniform
Sclerosing osteitis has wide transition zone

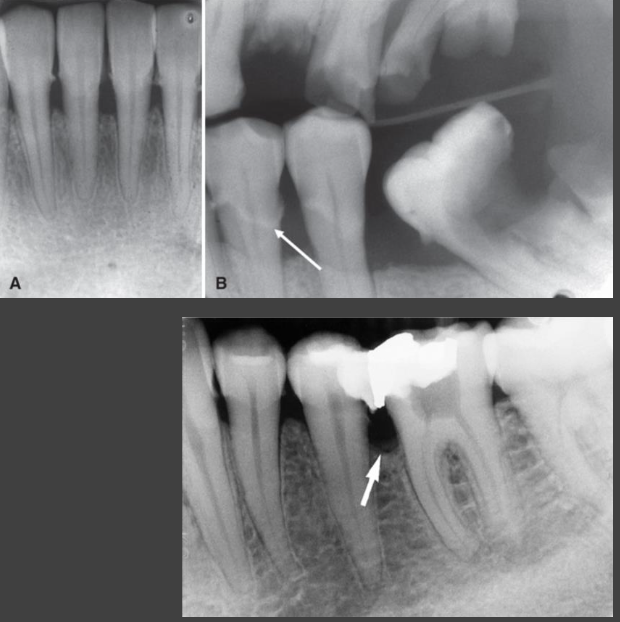
What is this
Sclerosing osteitis
What is this
Dense Bone Island
How do malignancies manifest in periapical inflammatory lesions?
Metastatic lesions and blood-borne malignancies (ex. leukemia)
May develop within the apical periodontal ligament space
Usually see other surrounding bone changes
Multiple, variably sized regions of cancellous bone destruction
How would you differentiate between a cyst and a granuloma?
Cannot radiographically distinguish cysts from granuloma (or abscess)
Rarefying osteitis – umbrella term; radiologic diagnosis describing localized inflammatory condition arising from a necrotic tooth
Biopsy needed to distinguish – epithelial lining of cyst
Features associated with cyst
Large growth (> 1 cm)
Expansion
Displacement of adjacent structures
Endodontically Treated Teeth periapical radiolucency
Persistent or recurrent inflammatory disease after endodontic treatment
Possible etiologies
Inadequate endodontic treatment
Unusual root canal morphology
Presence of untreated canal
Perforation of root surface
Root fracture
CBCT can help determine etiology of persistent or recurrent disease
Periapical scar – fibrous healing defect
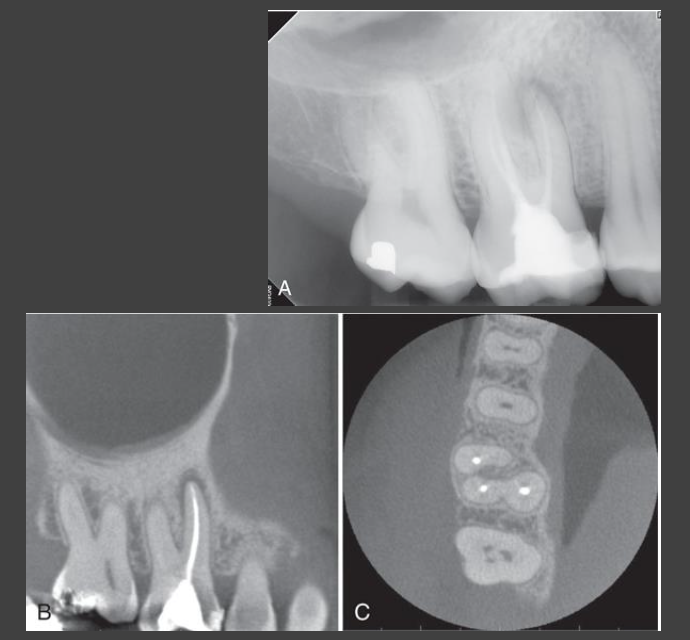
How would you be able to tell the lesion is from a endodontically treated tooth?
Periapical scar – fibrous healing defect
Pattern of healing bone
Compare imaging over time
Clinical signs/symptoms
Asymptomatic
What is the initial management for periapical radiolucency?
Don’t automatically assume
Perform vitality test
Identify etiology
Compare to prior radiographs and/or follow-up
What does the periodontium do and what are the components of it?
Supports the teeth in the jaws
Gingiva
Periodontal ligament (PDL)
Cementum
Alveolar processes of jaws
How does one get periodontal disease?
Inflammatory response to bacteria in periodontal tissues that may lead to loss of junctional epithelium and bone around teeth
Dental plaque biofilm plays primary role in initiation
Cyclic periods of active inflammation and tissue destruction and
quiescence
What is the incidence of periodontal disease?
42% of U.S. adults aged 30–79 years have periodontitis
Significant increase in prevalence with age
Defined as having clinical attachment loss (≥3 mm, multiple sites) and probing depths (>3 mm, multiple sites OR >4 mm, single site)
What is gingivitis?
Inflammation of gingiva (swelling, edema, erythema). It does not always progress to periodontitis but periodontitis is always preceded by gingivitis
What is periodontitis?
Pocket formation and/or gingival recession and clinical attachment loss
What are some clinical signs of periodontal disease?
Clinical signs: bleeding on probing, purulent exudate, tooth mobility
Usually painless
Can ultimately lead to tooth loss
How would you clinically and radiographically asses peridontits?
Conduct the clinical exam first
Image when the clinical exam suggests periodontitis
What would a provider do in a clinical exam?
Probing, bleeding, purulence, gingival recession, clinical attachment loss, mobility, etc.
Acts as foundation to justify acquisition of radiographs
What should imaging contribute to from the clinical exam?
Information on periodontal status not derived from clinical exam
What do images provide in terms of periodontits?
A record that can be used to evaluate disease longitudinally
Radiographs are helpful for periodontits in the evaluation of
Amount of bone present
Condition of alveolar crests
Bone loss in furcation areas
Width of PDL space
Local irritating factors that increase risk of periodontal disease
Calculus
Poorly contoured or overextended restorations
Root length and morphology and crown-to-root ratio
Open interproximal contacts, which may be sites for food impaction
Anatomic considerations
Root proximity
Position of the maxillary sinus in relation to a periodontal deformity
Position of the mental foramen in relation to the alveolar crest
What is periapical cementoosseous dysplasia?
Non-inflammatory benign fibroosseous lesion

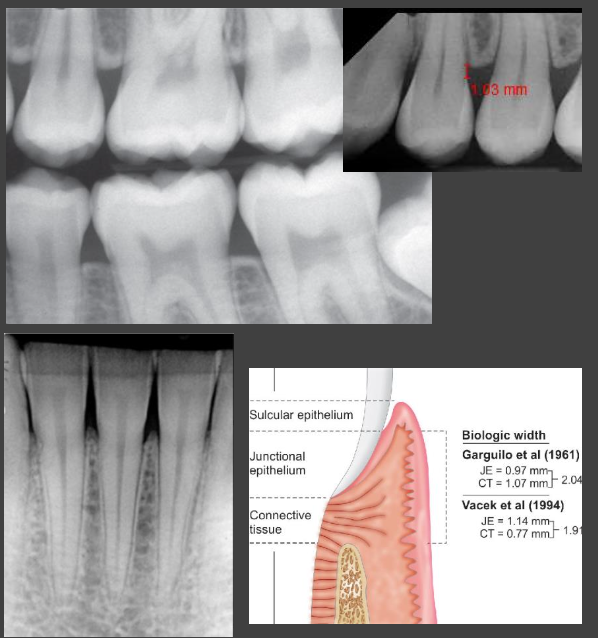
What radiographic modality would you use for periodontal disease?
Intraoral images (BWs and PAs), which have the highest spatial resolution of any modality. However, many radiologic signs of periodontal disease are subtle (early bone loss, changes to PDL space and lamina dura)
What do bitewings serve as for periodontal disease?
The primary imaging choice for periodontal diseases
Most accurately depict distance between CEJ and interradicular alveolar crest
Vertical BW - long axis of receptor in vertical orientation to capture bone levels
Vertical for pockets > 6mm ; Horizontal generally ok for pockets < 6mm
What do PAs serve as for periodontal disease?
Evaluation of percentage of root affected by bone loss (crown:root ratio)
Often distorts relationship between CEJ and crest due to greater variation in vertical angulation (anatomic limitations)
What are some limitations of using intraoral images?
2D superimposition prevents effective visualization of infrabony defects
Acquire multiple images of same site at different angulations
Typically underestimate amount of bone loss
Do not demonstrate soft tissue–to–hard tissue relationships (no information on pocket depth)
Bone level often measured relative to CEJ position
Not valid reference when there is supraeruption or passive eruption in cases of severe attrition
What is the role of a panoramic radiographic in periodontitis?
Overview of teeth and jaws in single image
Should NOT be primary imaging tool for evaluation of periodontal diseases
Multiple superimpositions and distortions especially in anterior areas
Lower spatial resolution
Inaccurate measurements of bone loss
NO evidence supports role for extraoral bitewing images in evaluation of periodontal bone loss


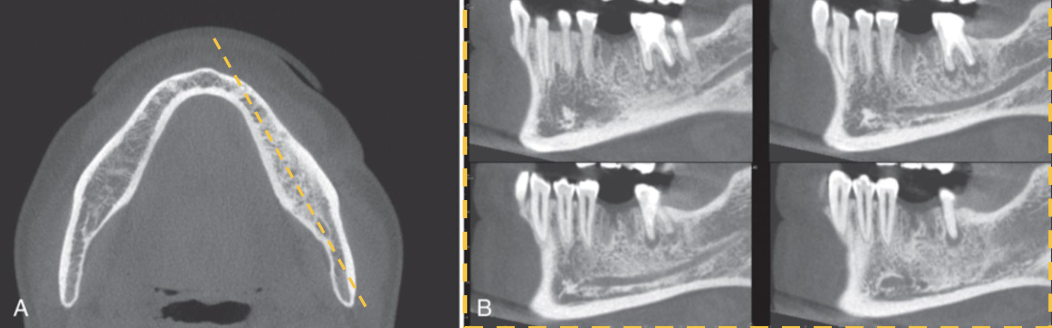
What is the role of a CBCT in periodontitis?
Advantage: elimination of anatomical superimpositions
Better visualization of complex vertical and crater defects, furcations, buccal/lingual cortical plate loss
Limited by artifacts from metallic restoration
Current evidence does NOT support use for imaging of periodontium
Insufficient advantage over intraoral imaging techniques
May be indicated in guiding surgical management in select cases
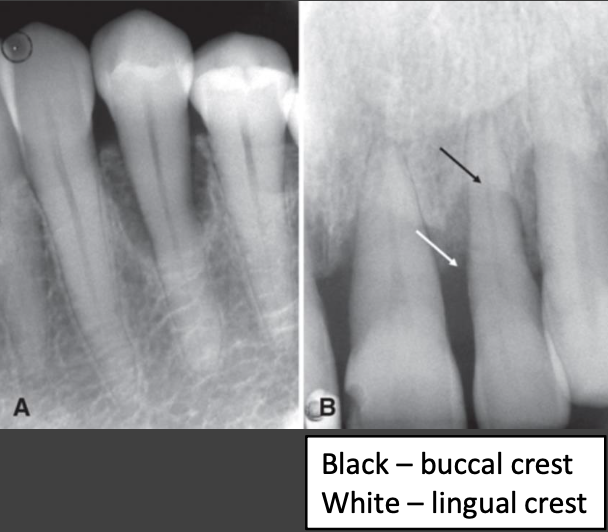
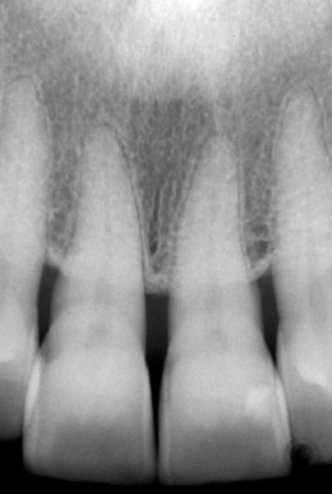
What is the appearance of a normal radiograph?
Thin layer of radiopaque cortical bone overlying crest
Lack of cortication can be seen both with and without periodontitis
Crest is 0.5–2.0 mm apical to CEJ
Parallel to imaginary line connecting CEJs of adjacent posterior teeth
Peak-like between anterior teeth
Sharp, well-defined angle between lamina dura and crest
Coronal PDL space typically thin and uniform
May appear slightly wider around premolar and erupting teeth
If lamina dura forms sharp angle with crest, likely normal
Increased radiolucency of crest due to thin buccal/lingual thickness
What are some features of imaging?
No radiographic changes associated with gingivitis (confined to gingiva)
Features of periodontitis same as other inflammatory conditions of bone
Changes in morphology of supporting bone
Loss of interproximal crestal bone and bone overlapping buccal/lingual root surfaces
Changes to trabecular density and pattern
Usually combo of bone reduction/loss and formation
Acute lesions predominantly display loss - increase in radiolucency due to decrease in number and/or spatial density of trabeculae
Chronic lesions have greater component of sclerosis - increase in radiopacity due to increase in thickness and/or spatial density of trabeculae
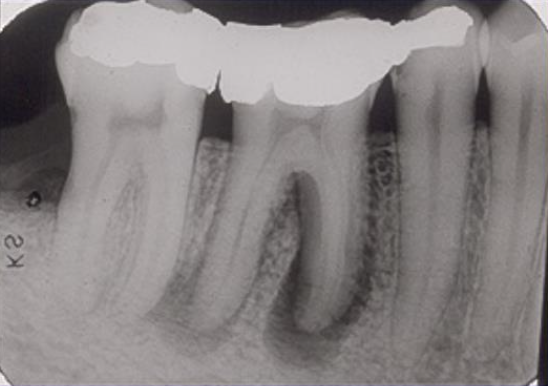
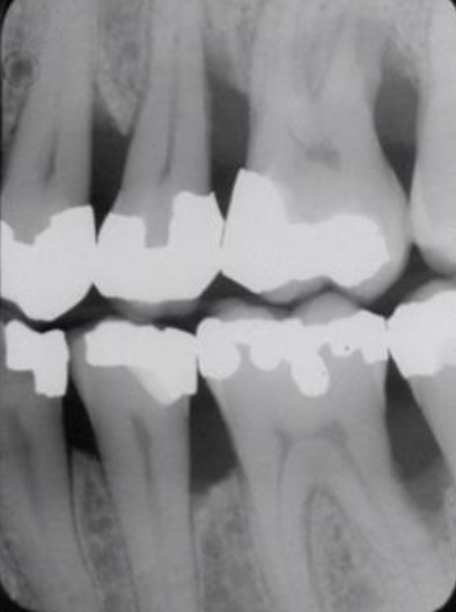
What are some early changes to look out for in a BW or PA?
Areas of localized erosion of interproximal alveolar crest
Anterior: blunting of crests and mild loss of bone height
Posterior: loss of sharp angle between crest and lamina dura
Angle may appear “rounded off” with a more irregular border
Cortical surface of bone edge may become more diffuse
Radiographic evidence of bone loss follows disease onset
Takes ~ 6-8 months of disease progression until radiographic bone loss evident
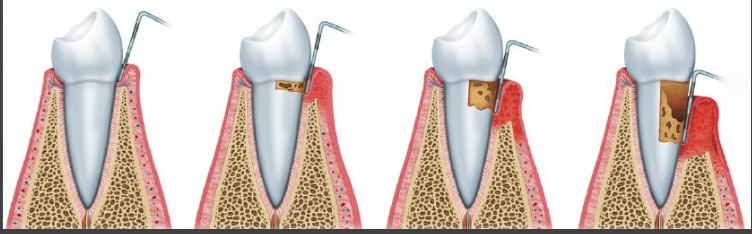
What are some defects in morphology of alveolar process and crest?
Horizontal bone loss
Vertical bone loss
Interdental craters
Furcation defects
Loss of buccal or lingual cortical plates
What are components to look for in the presence and severity of defects?
They vary regionally via
Distribution (generalized or localized)
Severity (mild, moderate, severe)
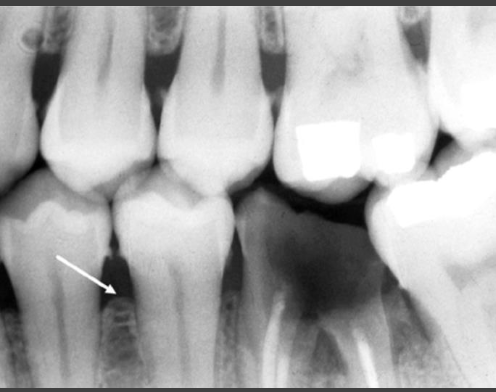
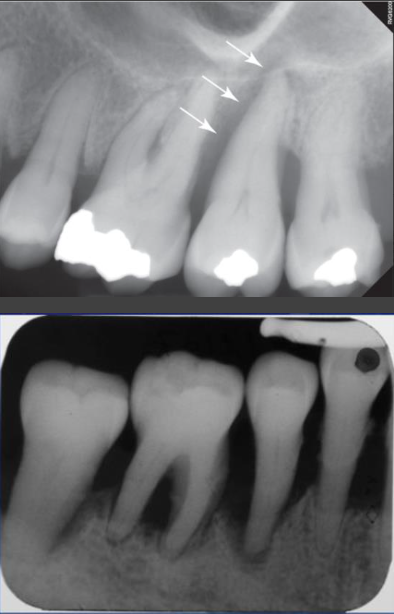
What is horizontal bone loss?
Loss in height of alveolar process
Crest of buccal/lingual cortical plates and intervening interdental bone resorbed
Crest parallels imaginary line joining CEJs of adjacent teeth
Severity based on bone level relative to root length (distance between CEJ and apex)
Within coronal 15%
Within coronal 15%–33% of root
Beyond (apical to) coronal 33% of root length
When CEJs of adjacent teeth are at different levels, crest may appear angled
When teeth supraerupt, bone may not follow → apical position of crest relative to CEJ
May occur during passive eruption of severely attrited teeth
Bone loss not caused by periodontitis
Bone loss at a single exam does not indicate current disease activity
Reestablishment of crestal cortication is good indicator of stabilization
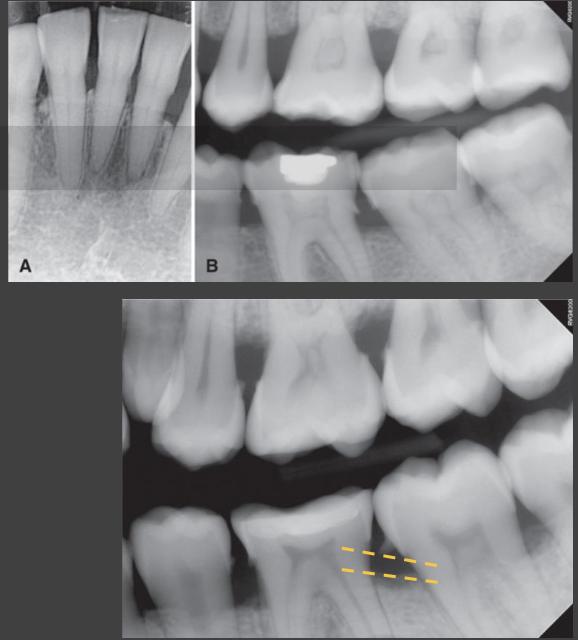
Horizontal Bone Loss
maxillary second premolar is supraerupted; etiology of low bone level (arrow) relative to CEJ is not necessarily periodontal disease

Horizontal Bone Loss
Passive eruption related to severe attrition; apparent increase in distance from CEJ to bone height (arrows) cannot be attributed to periodontal disease. However, resultant change in bone level relative to the CEJ still may be clinically significant.
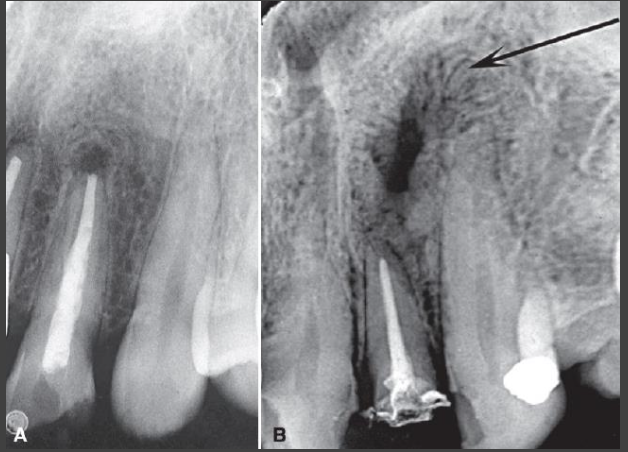
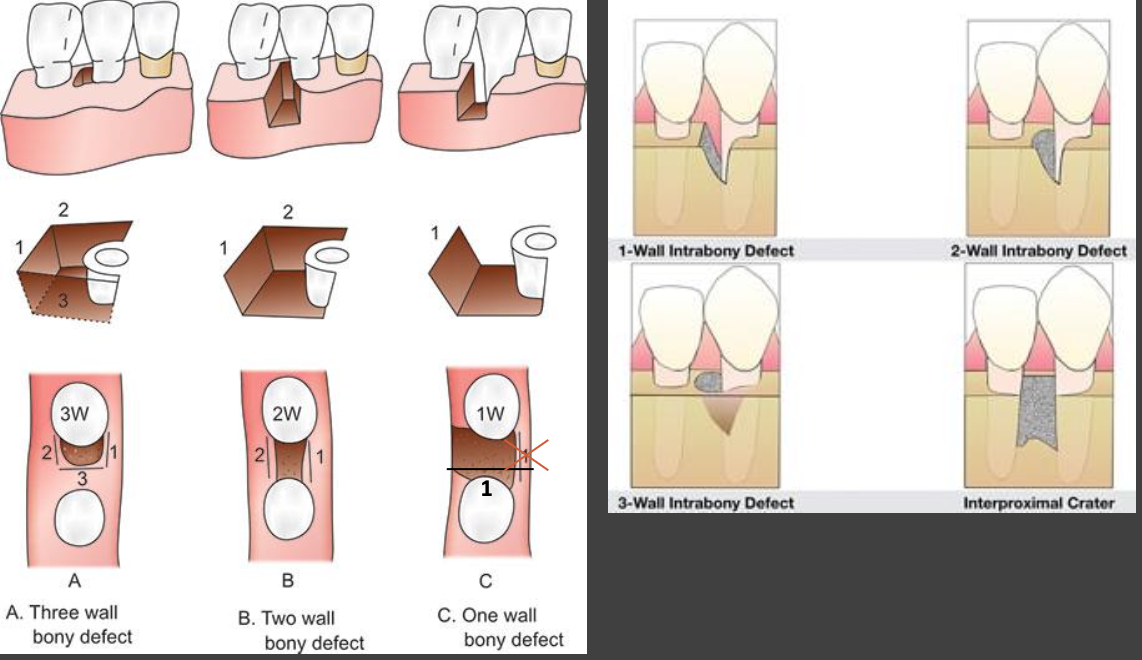
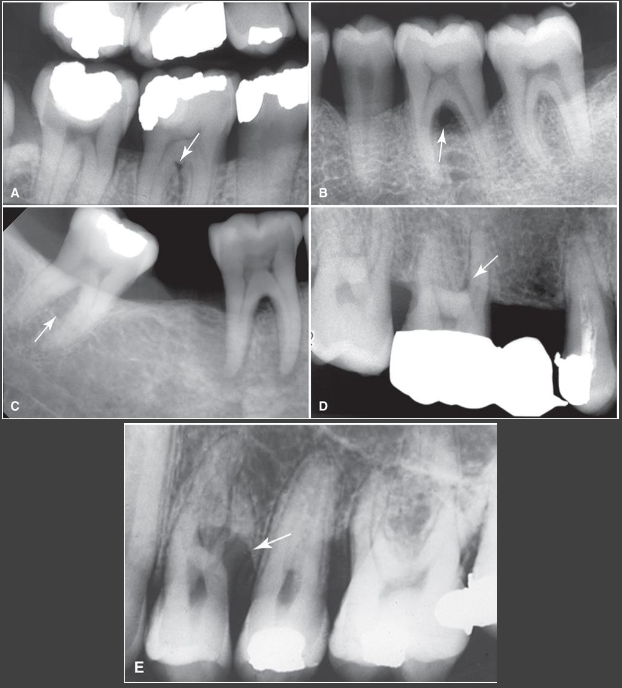
What is Vertical (Angular) Bone Loss?
V- or triangular-shaped defect extending apically from crest along affected root surface
Crest typically angulated obliquely to line connecting CEJ of affected tooth to adjacent tooth
Early stage – abnormal widening of PDL space at crest
Defect walls
3-walled: both buccal and lingual cortical plates intact
2-walled: one of plates resorbed
1-walled: when both plates lost
Assessment of number of walls
Difficult on intraoral images due to superimposition
Visualization of pocket depth may be aided by inserting gutta-percha point before imaging
Clinical and surgical inspections are best
CBCT can help but should not be routinely used
Early stage vertical bone loss
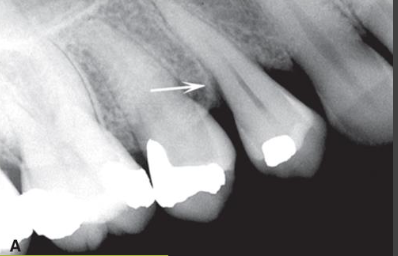
1 wall vertical bone loss
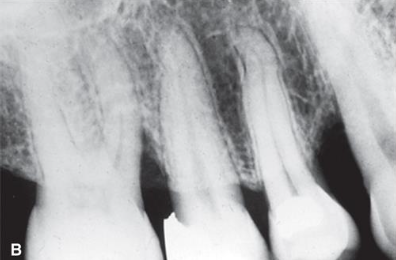
Diagram of vertical bone loss

Vertical Bone loss in stage IV periodontitis
Bone loss confined to region of 1st molars
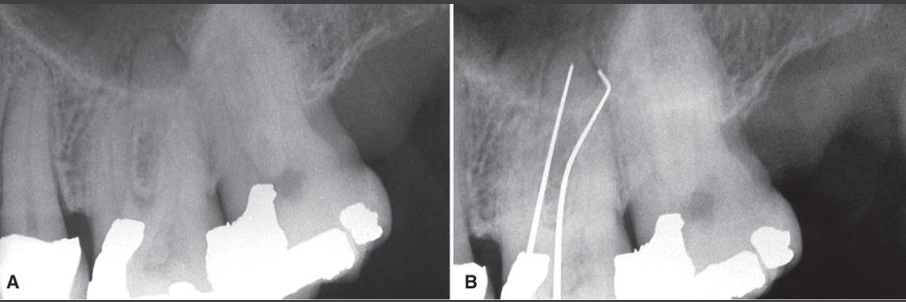
Gutta-percha used to visualize depth of infrabony defects. (A) image fails to show osseous defect (B) image reveals osseous defect extending to region of apex using gutta-percha
Vertical Bone Loss Examples
Appearance also suggests interdental crater defects
What are interdental craters?
2 walled, trough-like defect or depression in crest between teeth
Buccal and lingual cortical walls extend further coronally than resorbed bone between them
Band-like or irregular region of bone with less density at crest
More dense normal bone adjacent to base of crater
More common in posterior segments (broader buccal-lingual dimension)
What is buccal/lingual cortical plate loss?
Loss of cortical plate overlying tooth root
Difficult to detect if lack of bone loss at interproximal region
May occur alone or with another type of bone loss
Increase in radiolucency of tooth root near alveolar crest
Shape is usually semicircular with depth directed apically
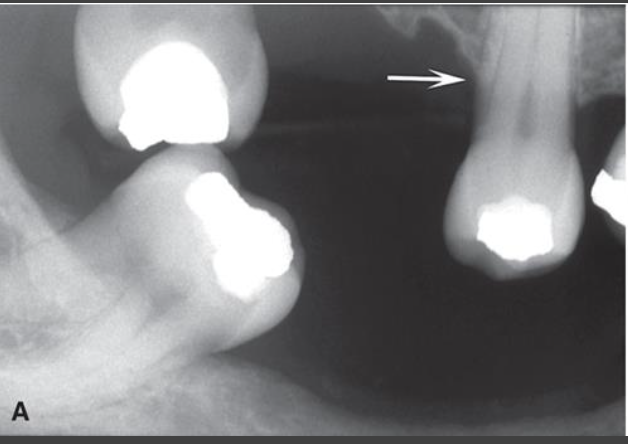
What is furcation involvement?
Apical extent of bone loss to and beyond furcation level of multirooted teeth
Widening of PDL space at apex of bony crest of furcation
More radiolucent appearing furcation area
Can be masked by external oblique ridge or root morphology
Harder to see around maxillary molars (palatal root)
Most commonly involved maxillary 1st molar furcation is mesial
J shape radiolucency with hook of “J” extending into trifurcation
Radiolucent triangle with apex pointing toward furcation
Definitive diagnosis with clinical exam, sometimes surgical exploration
CBCT – detailed characterization when needed for treatment planning
What is trabecular bone density?
Periodontal diseases may stimulate adjacent
Loss of bone density (rarefaction) - more common in early or acute lesions
Reactive bone formation (sclerosis) - may extend a distance from the periodontal lesion
Usually see both
Rarely no apparent change in surrounding bone
Inflammatory products from lesion may diffuse through maxillary sinus floor to cause regional mucositis
What is the classification of periodontal disease based on?
Tissue types affected – gingiva only or with involvement of alveolar process
Staging – disease severity and complexity of management
Grading – historical rate of progression and future risk of progression
Association with other conditions – systemic or genetic conditions, combined endodontic-periodontic lesions
What is periodontitis subcategorized into?
Necrotizing periodontal diseases (NPDs), periodontitis, and periodontitis as direct manifestation of systemic diseases
Radiographic appearance of all three of these subcategories is similar
How might you see periodontic lesions in endodontics?
Inflammatory lesions of periodontal or pulpal origin may develop independently and merge
One may induce the other
Periodontal lesion may extend to apex causing secondary pulpitis
Periapical inflammatory disease may extend coronally to crest causing retrograde periodontitis
Angular defect to apex communicating with periapical rarefying osteitis
Usually relatively uniform width
Widens slightly at crest creating funnel shape
May affect one or multiple surfaces of tooth or be circumferential
Treatment is complicated – both endodontic and periodontal therapy
What are some other conditions affecting periodontium?
Periodontal abscess
Rapidly progressing destructive lesion
Usually originates in deep soft tissue periodontal pocket
Occurs when coronal portion of pocket becomes obstructed
Pain, swelling, sometimes draining fistula
May not be visible changes on imaging if acute
Radiolucent region develops if persists
Round area often superimposed over root
Loss of lamina dura on involved surface
Bridge of bone may be visible over coronal aspect separating it from crest
After treatment some of lost bone may regenerate

What are local irritating factors?
Create environment where disease may develop
Aggravate existing disease
Calculus deposits
Prevent effective cleansing
Most commonly at mandibular incisors
Defective restorations
Poor contours and overhanging margins can accumulate plaque
Enamel pearls and cervical enamel projections
Aberrant enamel formations
Commonly in furcation regions of multirooted teeth
Alter periodontal attachment
Create sites prone to biofilm accumulation
How would you evaluate periodontal theray?
Signs of successful treatment are occasionally visible
Not universally seen
No apparent changes in many cases
Good indicators of disease stabilization
Reestablishment of interproximal crestal cortex
Reestablishment of sharp angle between cortex and lamina dura
Other possible indicators of successful treatment
Sclerosis of previously radiolucent margins of defect
Remineralization of previously radiolucent bone
X-ray beam angulation and exposure settings may affect crest visibility
Too high exposure – black image; thin bone may not be apparent, giving impression bone is resorbed
Too low exposed – light image; giving impression of bone growth
Treatment success and healing best assessed clinically
What are some differential diagnosis of bone loss around teeth?
Malignant neoplasms (squamous cell carcinoma)
More extensive bone destruction of localized region beyond periodontium (invasive pattern)
Irregular widening of PDL space along entire length and destruction of the lamina dura
Invasive border- poorly defined, ragged or irregular periphery
Langerhans cell histiocytosis
Often manifests as one or more regions of bone destruction around roots of teeth
Appearance of “teeth floating in space”
Epicenter of bone destruction at mid-root level rather than crest – “scooped-out” with crest less resorbed or intact
Raise suspicion of other disease if
Presence of few adjacent loose teeth when rest of mouth shows no sign of periodontal disease
Bone destruction does not have pattern/morphology of periodontal disease (apical progression)
Bone destruction has ill-defined borders and lacks a peripheral sclerotic bone response