Commensal Bacteria and Pathogens Overview
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
54 Terms
Mutualism
Necessary for survival of both organisms (e.g. in cows bacteria break down cell walls of grass).
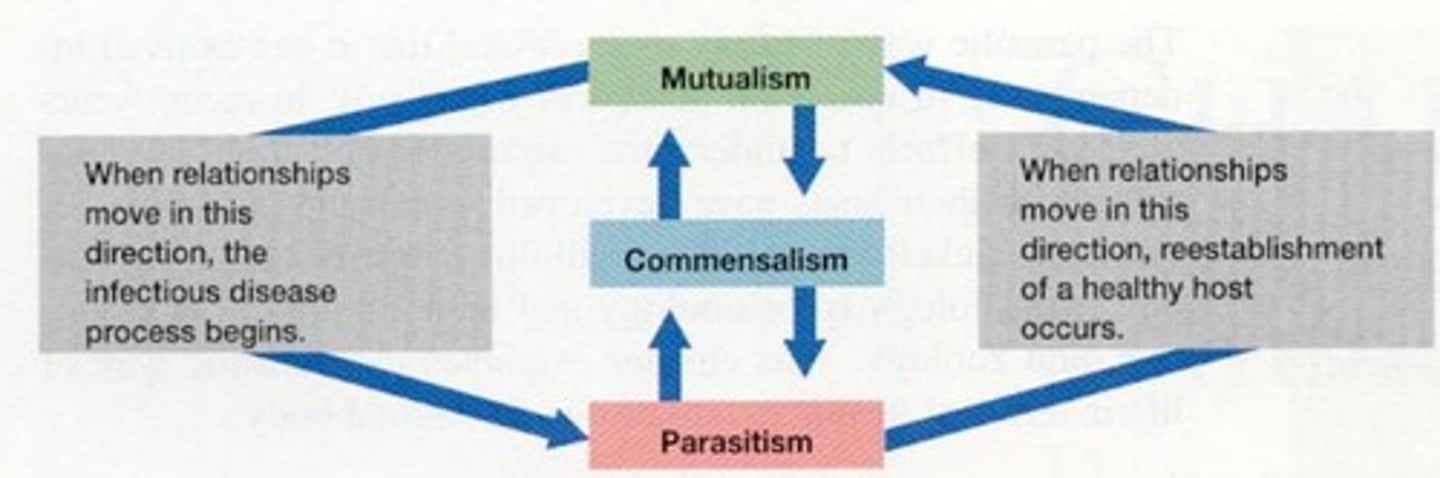
Commensalism
Not metabolically dependent and both organisms can survive without each other (e.g. in colon bacteria get food from us, but they also synthesise certain aromatic amino acids and vitamins for us).
Parasitism
Not metabolically dependent, but parasites don't harm the host yet.
Infection
When the organism gets part of the host.
Disease
When the organism causes symptoms.
Asymptomatic carrier
Human doesn't have symptoms, but carries an infection and can cause disease in another.
Dermal layer of skin
Very dry, so not a very good environment for bacteria.
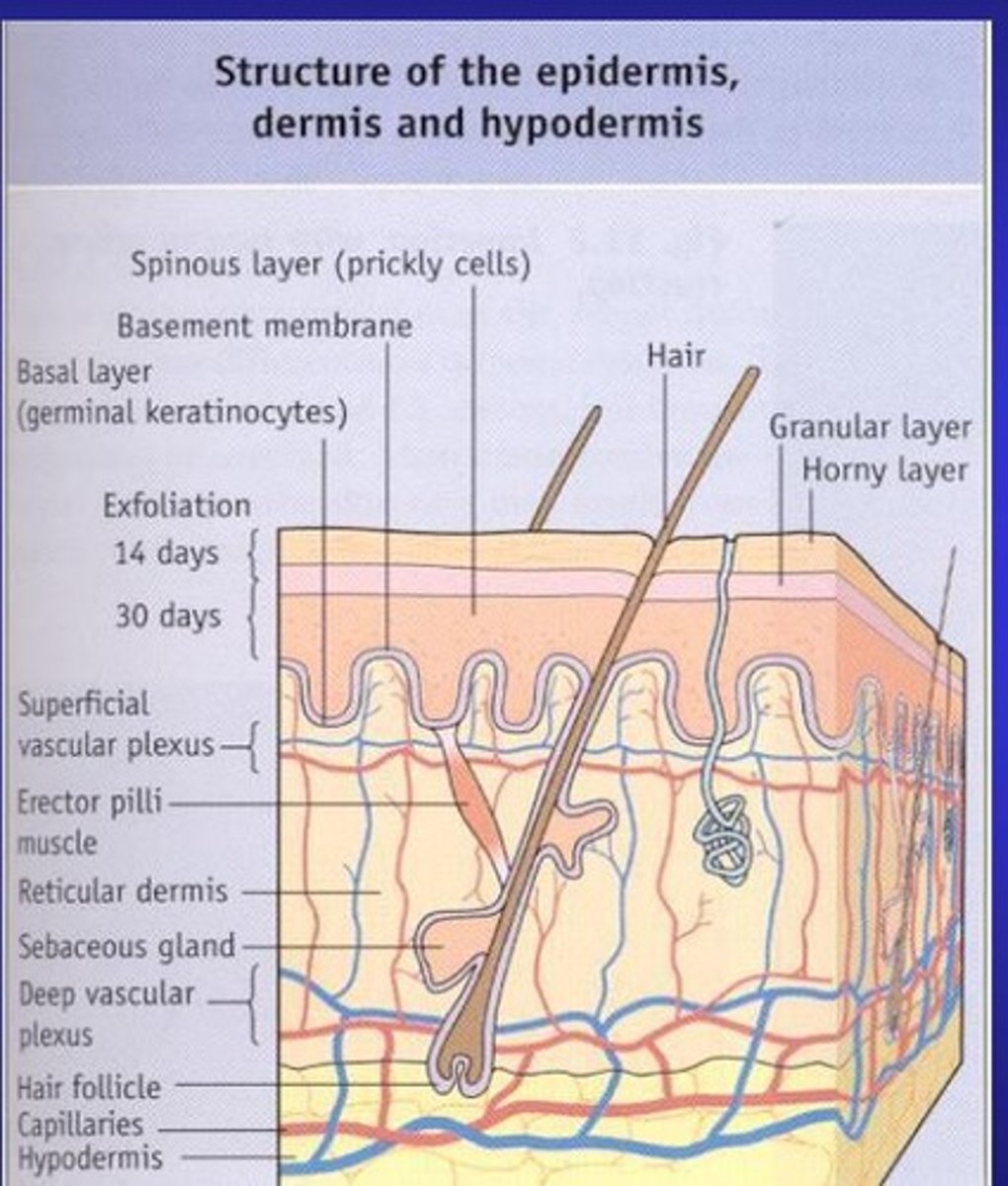
Fatty acids
Cause pH to be acidic, sebaceous glands produce a salty environment and keratinocytes secrete antimicrobial peptides that inhibit bacteria.
Staphylococcal mastitis
Can occur when some bacteria enter via hair follicles, sebaceous gland or teat canals.
Stratum corneum
Fungi can infect this non-living keratinous structure (hair, nails).
Common sites of infection
Wounds, abrasions, and burns are common sites of infection (e.g. for streptococci, water-borne Leptospira or blood-borne hepatitis B).
Rabies virus
Can be transmitted through bites.
Microflora
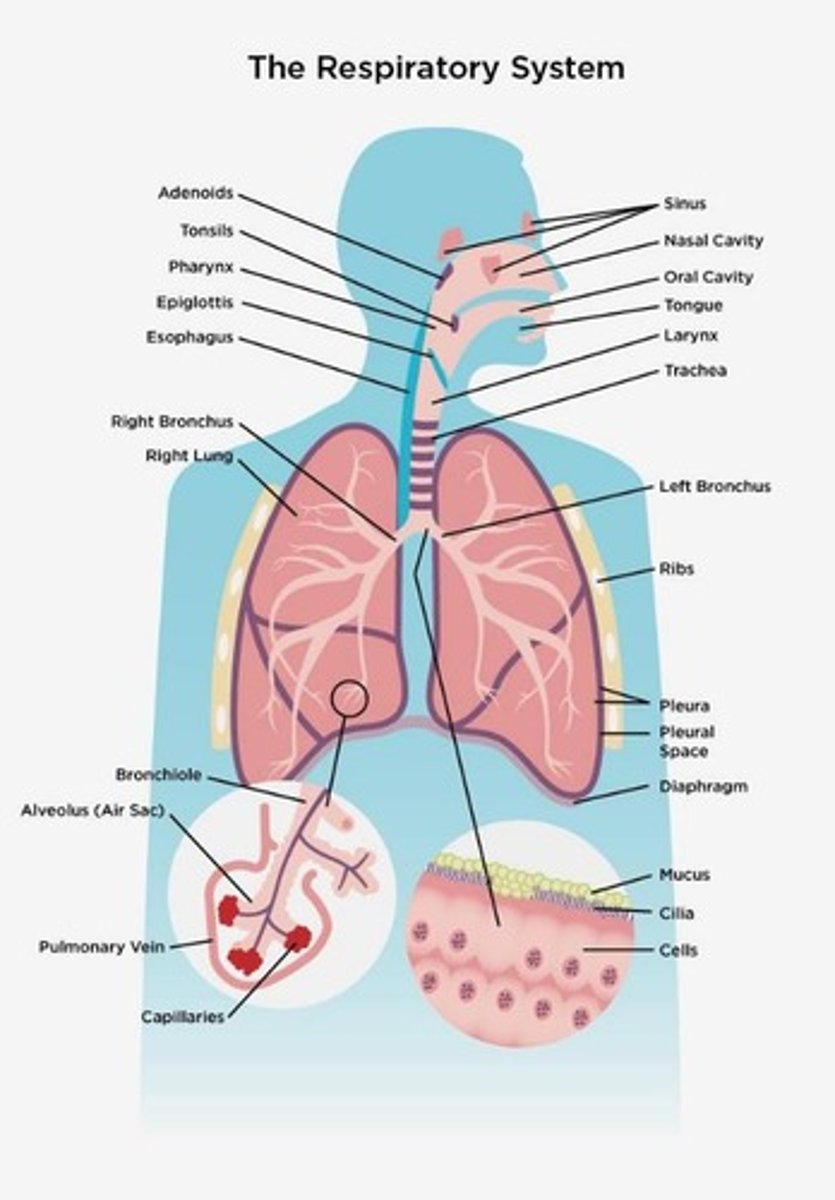
Inside the nose, similar to skin.
Ciliary actin
Carries mucus produced in the lungs to the back of the throat, causing washing out.
Lysozyme
Found in saliva, breaks the glycosidic bond between GAD and NAM.
Adhesins
Bacteria bind to receptors on molecules and form a mucociliary sheet (e.g. influenza, Measles, Rhinovirus).
B. pertussis
Inhibits ciliary activity.
Neisseria
Can cause meningitis in some individuals.
Poor dental hygiene
Can lead to overgrowth of microorganisms in the mouth, producing acid and causing plaques and decay.
Lower respiratory tract
Organisms can cause pneumonia, often settled out before reaching alveoli where phagocytes eat the pathogens.
Gastrointestinal gut
Protected by acid, mucus, bile, and enzymes.
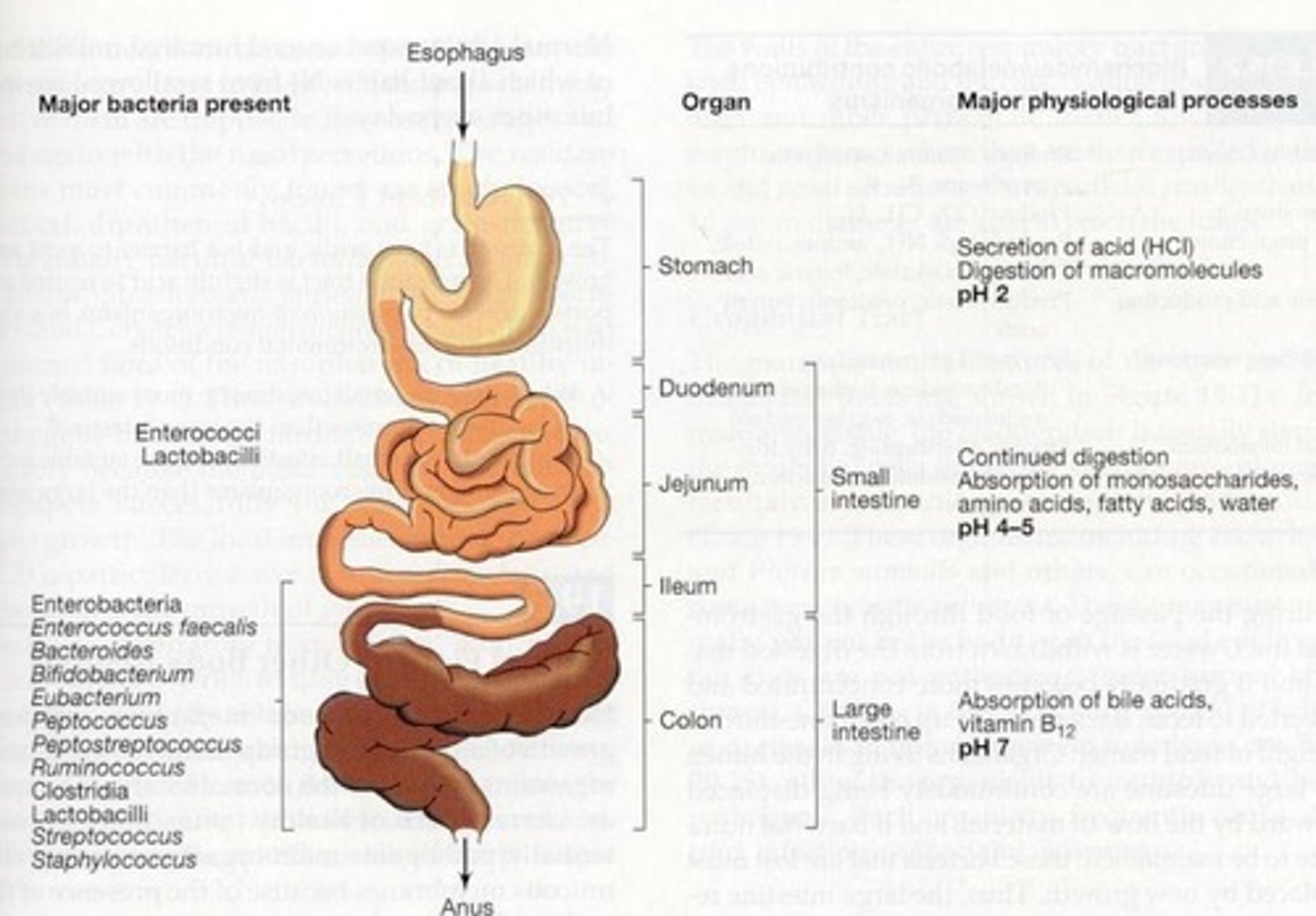
Microbial adhesins
Mucus contains molecules that bind to them and microbe-specific secretory IgA antibodies.
Attachment to intestinal surface
Involves bacteria like Vibrio cholera (diarrhoea, cholera, enteric fever), Rotavirus (diarrhoea), and Poliovirus.
Giardia lamblia
A parasite that adheres to the microvilli and has its own microvillar sucking disk.
Tapeworms
Adhere to the mucus in the gastrointestinal tract.
Acid resistance in stomach
Helicobacter pylori, Mycobacterium tuberculosis (causes intestinal tuberculosis), Enteroviruses (hepatitis A, poliovirus etc)
Lactobacilli
Can start growing in small intestines; most organisms are in large intestines.
Appendicitis
Microbes found in colon move to appendix causing disease.
Lactobacilli in urogenital tract
Colonise the vagina, metabolise the glycogen produced by estrogens forming lactic acid giving acidic pH 5.
Health of vagina
Strongly related to lactobacilli, which prevents overgrowth of organisms in vagina.
Urinary tract protection
Long and constant washing out by urine protects it.
Gonocci and chlamydia
Attach to the urethra cell, which is then engulfed by bacterium = parasite-directed endocytosis.
E. coli in urinary tract
Commonly invade urinary tract causing UTIs, urethritis, and cystitis.
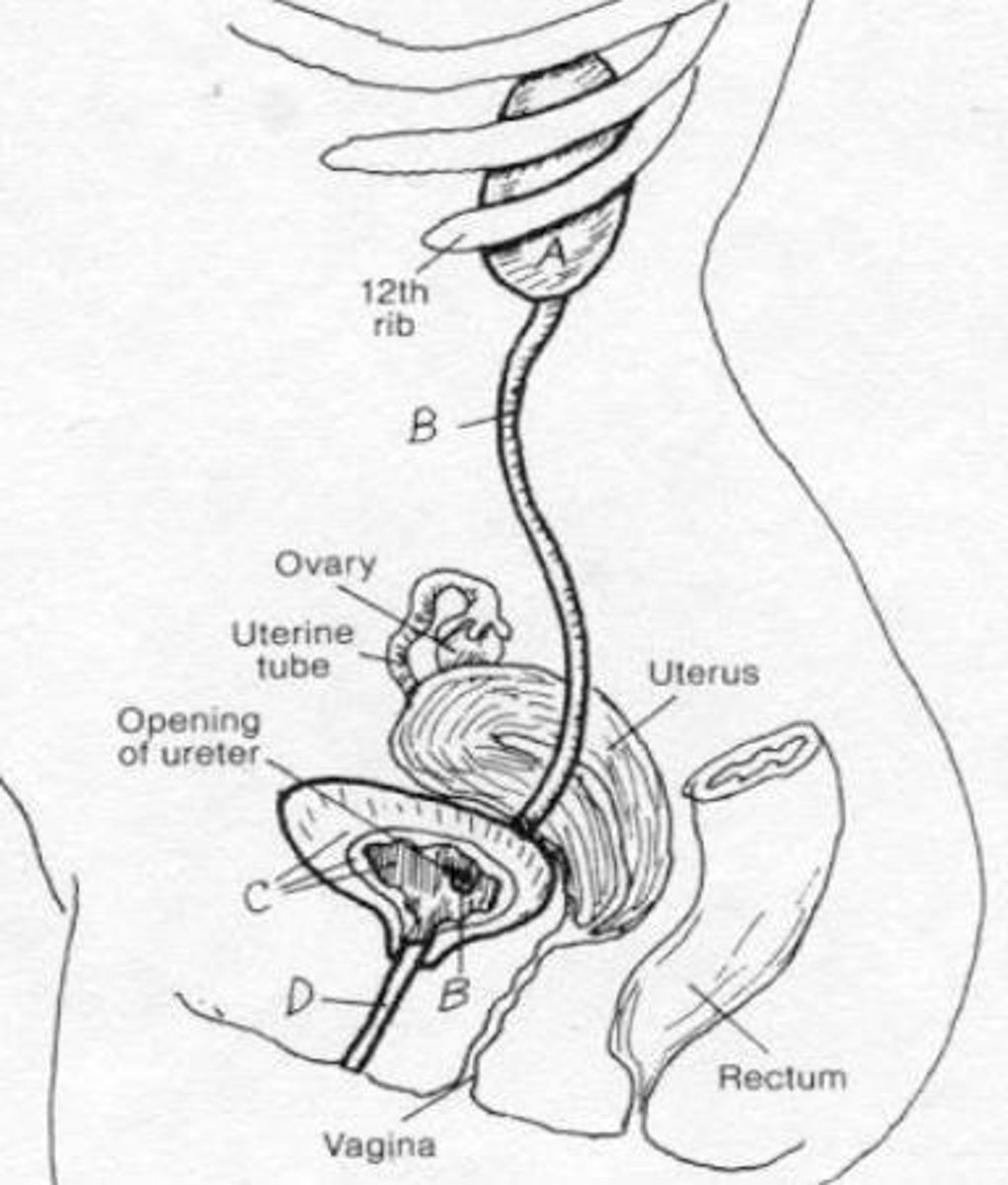
Urinary tract infections in women
More common due to shorter tract length 5cm vs 20cm in males.
Koch's postulates
1) Organism must be found in all hosts with disease 2) Organism must be isolated in pure culture 3) Organism should produce the same disease when inoculated into a healthy host 4) Organism should be re-isolated in pure culture.
Problems with Koch's postulates
Being isolated, the fact it would infect (asymptomatic carrier), ethics.
Molecular Version of Koch's postulates
1) Genes (or their products) have pathogenic potential 2) Gene should be found in all pathogenic strains but not in avirulent strains 3) Disruption of the gene should reduce virulence 4) Avirulent strains can be transformed into virulent strains by cloning the gene 5) The gene must be expressed during the infectious process 6) The gene product should elicit an immune response.
Transmissibility of pathogen
Transmission-entry of disease.
Respiratory/salivary spread
Influenza, Tubercle bacilli, Streptococci, herpes simplex virus.
Faecal-oral spread
Cholera, Hepatitis A.
Venereal spread
Chlamydia, Gonococci, Herpes Simplex virus, HIV.
Vector transmission
Malaria (biting arthropod).
Vertebrae reservoir
Rabies.
Vector-vertebrae reservoir
Plague, yellow fever.
Skin transmission
Staphylococci, human papillomavirus.
Milk transmission
HIV, cytomegalovirus.
Blood transmission
Hepatitis B & C, HIV.
Factors affecting transmissibility
Dependent on number of microorganisms shed, microorganisms' stability in the environment, number of microorganisms required to infect a fresh host.
Virulence factors
1) Adhesion and colonization of host 2) Colonization of mucosal surfaces 3) Invasion of pathogen 4) Growth and multiplication 5) Evasion of immune response 6) Anti-phagocytic strategies 7) Exit strategy to transmit to the next host.
E. coli biofilms
A good way of adhering and growing; E. coli produces film, is gram negative (found in colon usually).
Microorganisms need iron
As a co-factor, however, iron is bound to Hg and hence not openly available.
Siderophores
Bacteria produce siderophores (catechols/hydroxamates) to chelate free iron.
In July 2015, a report was released indicating the Gram-negative bacterium Pseudomonas aeruginosa was found on hospital sinks 10 years after the initial outbreak in a neonatal intensive care unit. P. aeruginosa causes ear and eye infections, but can cause pneumonia or septicaemia in vulnerable individuals like new-borns. Explain how the current discovery of the presence of this reported bacterium could lead to recurrence of nosocomial disease.
P. aeruginosa can form biofilms, which can live in the pipes and water systems. Bacteria can also stay dormant in harsh conditions and germinate when conditions improve, causing diseases 10 years after a break. Newborne babies have poor immune system, hence they cannot fight off the bacteria causing more severe symptoms. Long term presence can also make bacteria resistant to antibiotics and disinfectants, making it harder to kill.
A microbiologist has identified a new Gram-negative pathogen causing liver disease in rats. They suspect that the bacterium's fimbriae are a virulence factor. Describe how molecular Koch's postulates could be used to test this hypothesis.
1) identify the gene for fimbriae
2) inactivate the gene, to see if virulence is reduced
3) restore the gene to see if bacteria starts causing liver disease again
4) inject rats with the wild-type gene, if it's casuing the disease, but mutant doesn't then it's essential for virulence
5) check for an antibody produced from fimbriae, as it's gene product should cause an immune response