2. large animal med- hemolymphatics #2 disorders associated with blood loss/acquired hemostatic disorders
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
what is guttural pouch mycosis?
fungal infection in the guttural pouch, can spread to the roof of the medial compartment and cause erosion of the internal carotid artery--> epistaxis

what are the clinical presentations of guttural pouch mycosis?
sudden non-exertional associated epistaxis, mild to profound
usually unilateral
what other clinical signs are associated with guttural pouch mycosis?
dysphagia
pharyngeal paralysis
laryngeal hemiplasia
horner's syndrome
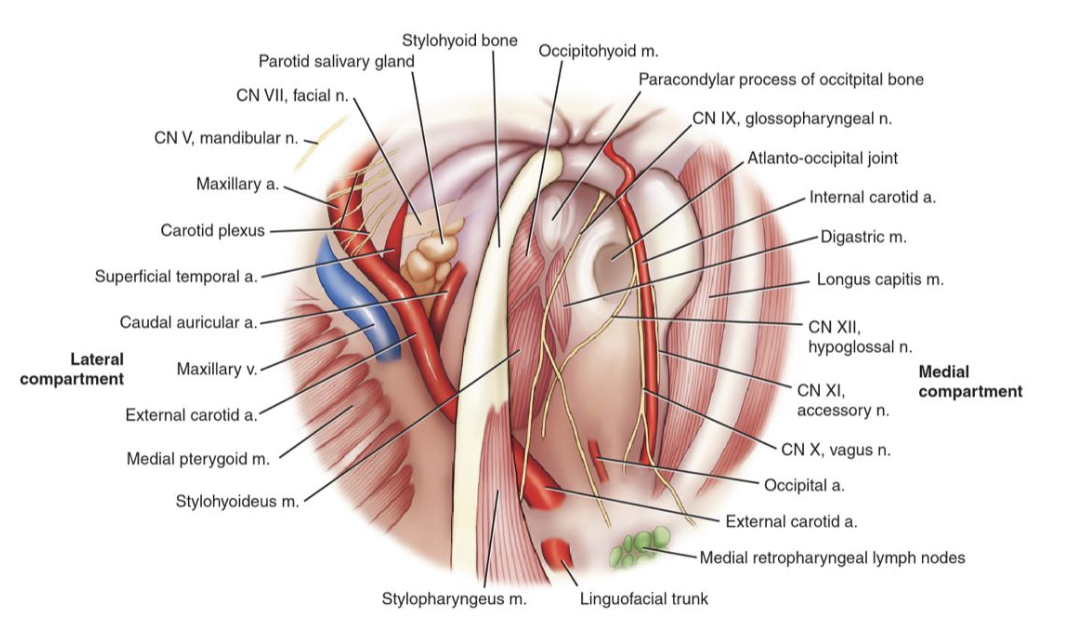
which horses are more likely to have guttural pouch mycosis?
stabled horses in warmer months
what are the clinical signs/presenting complaints for hemoperitoneum in horses?
colic + signs of anemia

what are the most common causes of hemoperitoneum?
trauma to the spleen
uterine artery rupture in mares
neoplasia
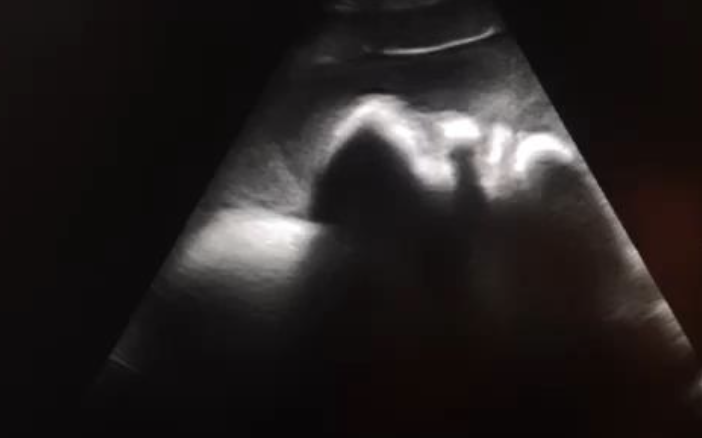
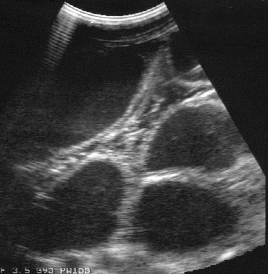
how is hemoperitoneum diagnosed?
ultrasound: swirling echogenic fluid
abdominocentesis: hemorrhagic (PCV >18%, TP >3.2)
what are the treatment goals for hemoperitoneum?
1. restoring perfusion and oxygen delivery to tissues by correcting fluid deficits
2. stopping further blood loss

what is the prognosis of hemoperitoneum?
survival rate is 51-74% --> strongly associated with underlying cause
what are the clinical signs of vena cava thrombosis in cattle?
bilateral epistaxis
respiratory distress
weight loss

what animals are at higher risk of developing vena cava thrombosis?
often seen in feedlot cattle on high grain diets
what is the pathophysiology of vena cava thrombosis?
1. rumen acidosis (from high grain diet) -->
2. formation of liver abscesses -->
3. thrombus of caudal vena cava -->
4. pulmonary abscesses -->
5. pulmonary hypertension -->
6. aneurysm formation -->
7. rupture and massive hemorrhage
how is vena cava thrombosis diagnosed?
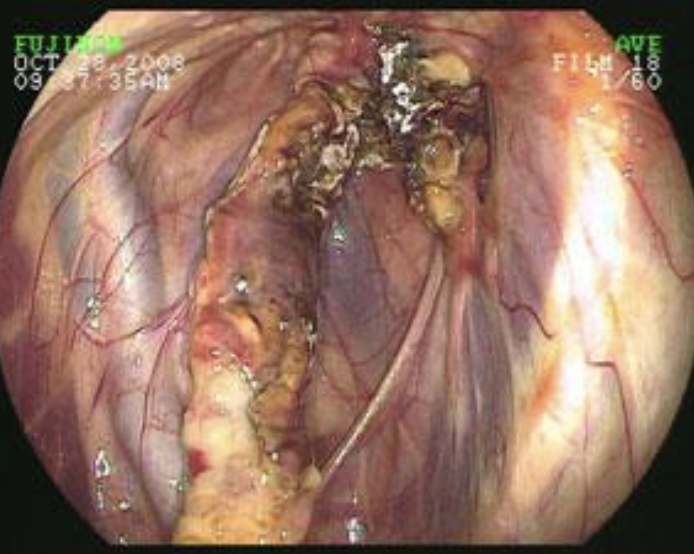
1. endoscopy (visualization of blood in trachea)
2. ultrasound: liver abscess, dilation of CVC
3. radiographs (only works in about 1/3 of cows due to size)

what is the treatment for vena cava thrombosis?
none- this dz is fatal

what causes jejunal hemorrhage syndrome?
etiology is unknown, likely associated with diet and management

which animals are affected by jejunal hemorrhage syndrome?
older dairy cows in the first 100 days of lactation

where is the location of lesions in jejunal hemorrhage syndrome?
intraluminal hemorrhage, usually in the jejunum, with subsequent bowel obstruction

what are the clinical signs of jejunal hemorrhage syndrome?
anorexia
tachycardia
normo-/hypothermia
+/- abdominal pain
+/- melena
pinging on right side (if bowel is distended)

how is jejunal hemorrhage syndrome diagnosed?
presence of distended loops of intestine on rectal exam and ultrasound
what is the prognosis of jejunal hemorrhage syndrome?
guarded
which intestinal parasites cause anemia in equids?
not many cause anemia
strongylus vulgaris (large strongyle, causes arteritis of mesenteric artery)
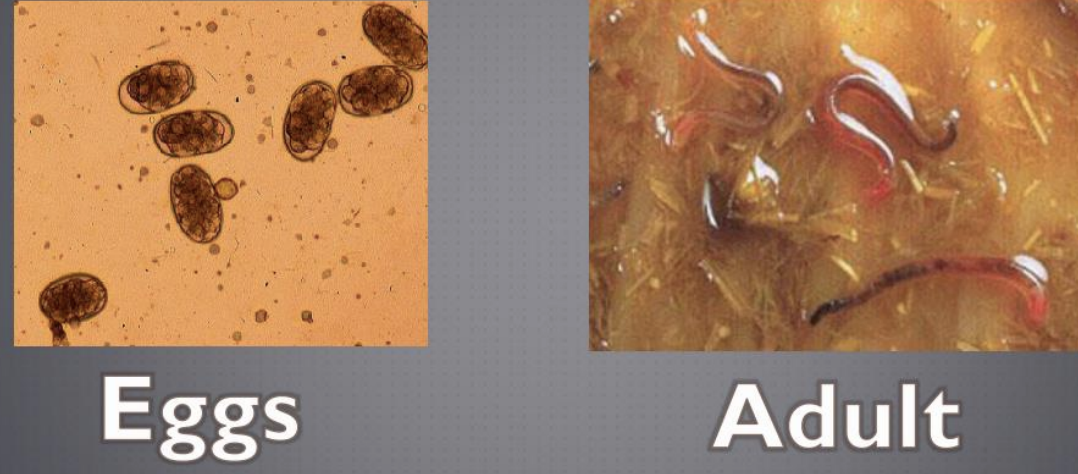
which intestinal parasites cause anemia in ruminants/camelids?
haemonchus contortus--> goats are generally more susceptible than sheep or cattle

how are intestinal parasites prevented?
-pasture rotation
-strategic deworming
-fecal egg count reduction-efficacy assessment
-mineral supplementation
what is hemophilia A?
an inherited coagulation disorder resulting in factor 8 deficiency
seen in horses, cattle, sheep: x-linked inheritance and recessive, only reported in males
what is vasculitis?
inflammation and necrosis of vasculature, specifically blood vessel walls
which species commonly get vasculitis?
horses
not common in ruminants
what causes vasculitis in horses?
anaplasmosis
EIA
EVA
AHS (African Horse Sickness)
purpura hemorrhagica (complication following Strangles)
idiopathic

what causes vasculitis in ruminants?
malignant catarrhal fever (cattle)
bluetongue (sheep)

how is vasculitis definitively diagnosed?
histopathology of full thickness punch biopsies (at least 6mm in diameter) of skin in affected area
what is purpura hemorrhagica?
immune-mediated vasculitis of horses

what causes purpura hemorrhagica in horses?
sequela to infection with stretococcus spp., corynebacterium, or influenza virus
occurs 2-4 weeks after initial respiratory infection

what are clinical signs of purpura hemorrhagica?
-profound edema of all 4 limbs +/- serum exudation from skin
-petechiae and ecchymoses of MM
-fever
-lethargic and anorexic
-reluctant to move (bc legs hurt)

what is the pathophysiology of purpura hemorrhagica?
type 3 HS response to bacterial or viral antigens with immune complexes deposited in blood vessel walls

how is purpura hemorrhagica definitively diagnosed?
skin biopsy + SeM antibody titer >1:12,800 (if strangles is underlying etiology)

what is the treatment for purpura hemorrhagica?
-treat primary cause
-address inflammation and immune response (corticosteroids for 2-4 wks)
-supportive care
-local therapy for edema
what is the causative agent of equine anaplasmosis?
Anaplasma phagocytophilum (formerly Ehrlichia equi)
-an intracellular, gram-negative bacteria
-zoonotic
-transmitted by ticks
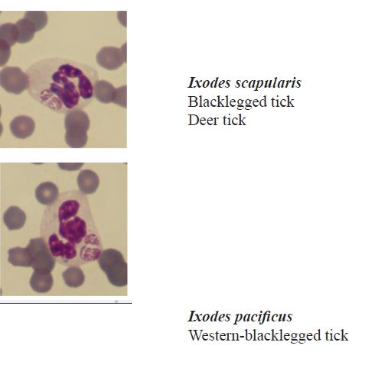
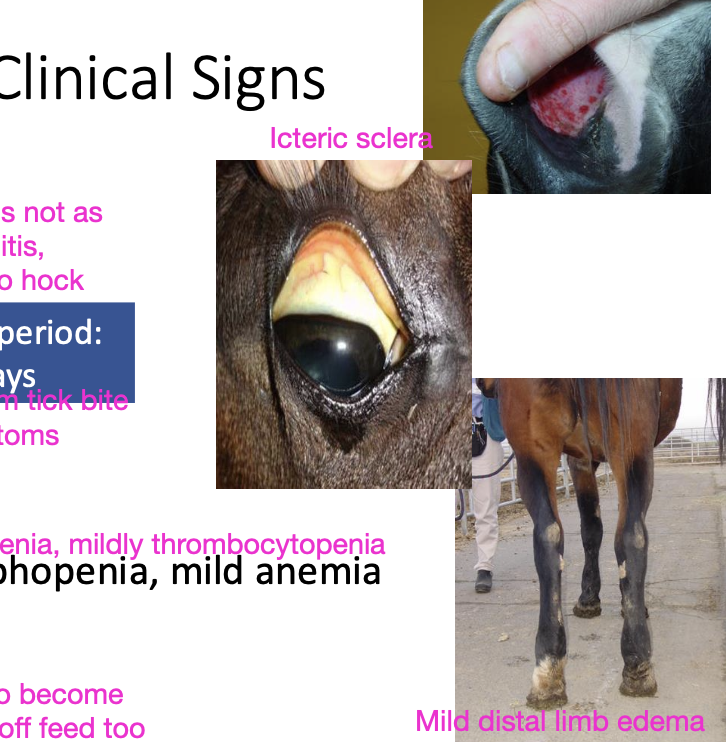
what are the clinical signs of equine anaplasmosis?
-fever
-mild distal limb edema
-inappetence
-icterus
-lethargy
-mucosal petechiae
-pancytopenia (neutropenia, lymphopenia, mild anemia)
-mild thrombocytopenia)
- +/- ataxia (rare)
how long is the incubation period of equine anaplasmosis?
8-12 days
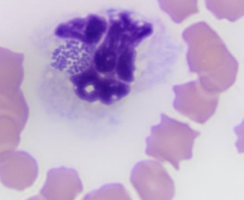
how is equine anaplasmosis diagnosed?
-blood smear: morulae present in neutrophils 3-5 days after onset of fever
-PCR: buffy coat from EDTA sample (most sensitive, faster)
-serology: 4-fold increase in IFA titer in paired samples
how is equine anaplasmosis treated?
spontaneous recovery is possible in 2-3 weeks if no complications
treatment of choice: tetracyclines to shorten clinical course + supportive care (oxytetracycline OR doxycycline, NSAIDS, IV fluids)

how is equine anaplasmosis prevented?
tick controlled
no vaccines available
what are the 3 major mechanisms of thrombocytopenia?
1. abnormal sequestration (usually in the spleen)
2. shortened platelet survival (consumption or destruction)
3. decreased or ineffective platelet production
what are the clinical consequences of thrombocytopenia?
-hemorrhage usually from small vessels (no 'plug')
-petechial hemorrhage and bruising
-profuse bleeding is rare
what are causes of primary immune mediated thrombocytopenia?
idiopathic (diagnosed by exclusion)
what are causes of secondary immune mediated thrombocytopenia?
1. drug-related (esp. penicillin, ceftiofur, TMS)
2. lymphoma or other neoplasms
3. infectious (EIA, BVD, anaplasmosis)
4. alloimmune thrombocytopenia in foals and mule foals
5. may accompany immune-mediated hemolytic anemia
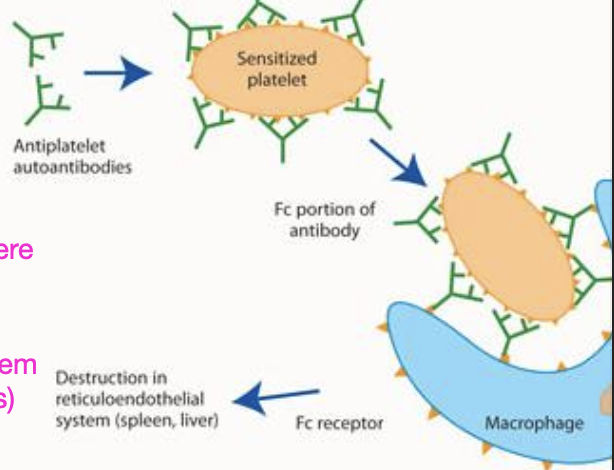
what is the pathogenesis of immune-mediated thrombocytopenia (IMTP)?
antibodies bind to surface of platelets, which are then removed by the mononuclear phagocyte system causing thrombocytopenia
what does the severity of clinical signs with IMTP depend on?
severity of clinical signs depends on degree of thrombocytopenia:
-platelets <40k --> excessive hemorrhage in response to trauma
-platelets <10k --> spontaneous bleeding
what are other clinical signs of IMTP?
-petechiae/bruising
-prolonged mucosal bleeding time
-hematomas less commonly
-PT and APTT are normal
how can IMTP be diagnosed?
1. CBC: platelets <40,000, mild anemia and hypoproteinemia
2. coagulation testing
-prolonged bleeding time
-abnormal clot retraction
-PT, PTT and fibrinogen within normal ranges
3. bone marrow biopsy (megakaryocytic and erythroid hyperplasia- regenerative response)

what gives a definitive diagnosis of IMTP?
demonstration of antibodies on platelet surface via flow cytometry
how is IMTP treated?
1. stop any suspected triggering medications
2. treat underlying disease if present
3. immunosuppression (to decrease antibodies forming)
4. blood products (PRP or whole blood)
prognosis depends on cause and response to therapy
what is disseminated intravascular coagulation (DIC)?
an acquired hypercoagulable syndrome, always secondary to underlying disease (GI dz, septic process, renal dz, trauma, neoplasia, hemolytic anemia)
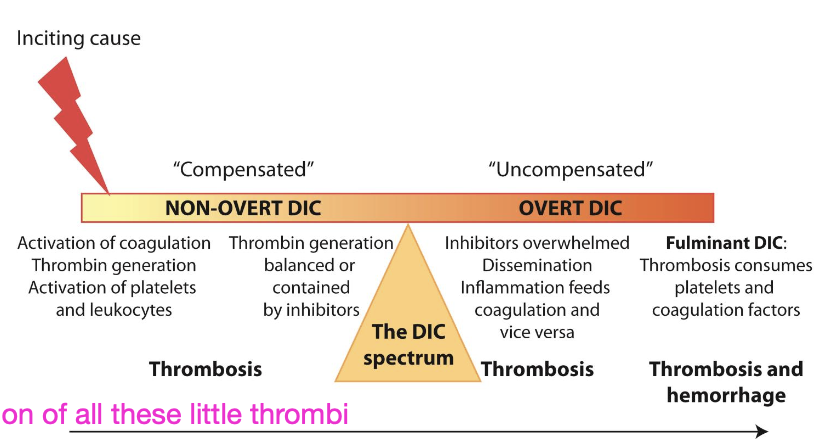
what is the key feature of DIC?
fibrin deposition in microvasculature
what are the clinical signs of DIC?
variable
-generalized thrombosis and/or hemorrhage
-thrombophlebitis
-petechiae
-epistaxis
-melena
-multiple organ dysfunction (kidney, liver, GI, laminitis)
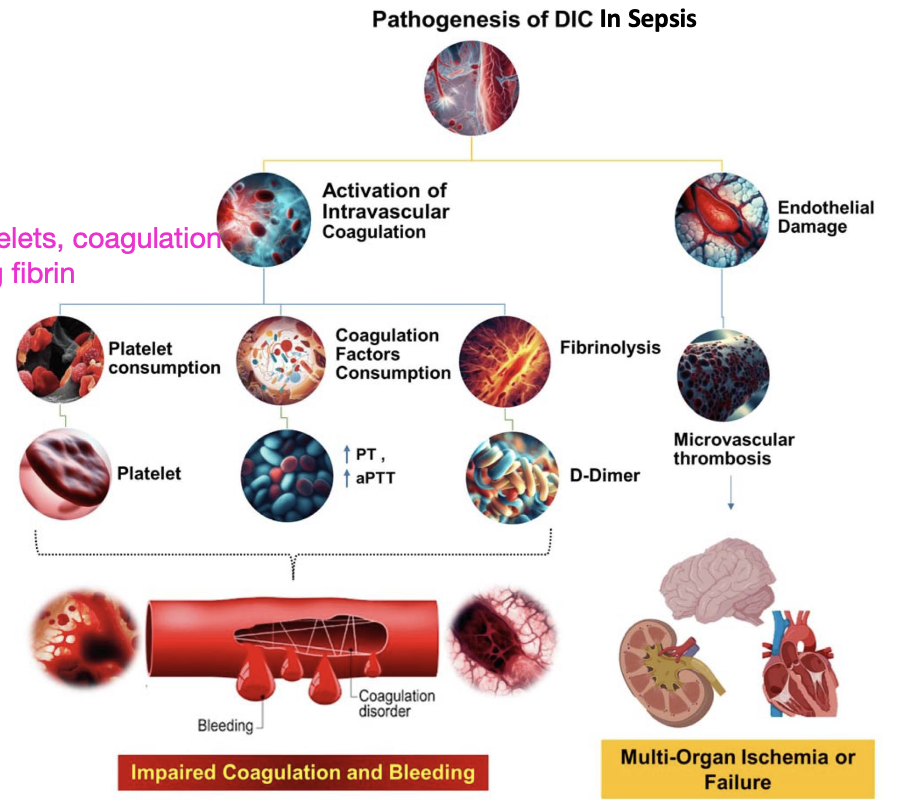
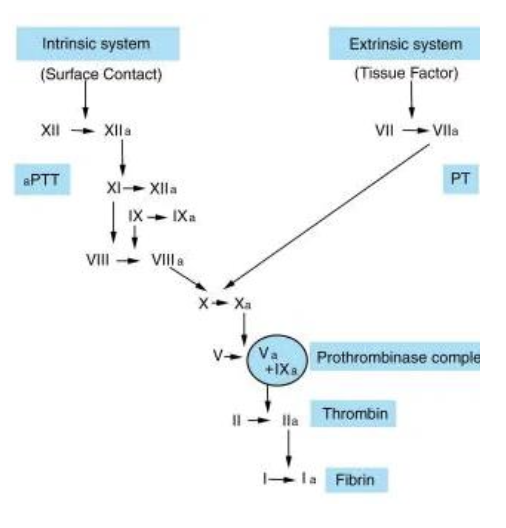
how is DIC diagnosed?
3 or more of the following lab changes AND consistent clinical signs:
-thrombocytopenia
-prolonged PT
-prolonged PTT
-reduced fibrinogen
-elevated D-dimers (FDP)
TEG used to identify hypercoagulable state

how is DIC treated?
-manage the underlying disease process
-intravenous fluid therapy (crystalloids, colloids)
-NSAIDs
-heparin (inhibition of microvascular thrombosis)
-blood component therapy as needed (whole blood, plasma)


what is moldy sweet clover poisoning?
improperly cured hay or silage of melilotus spp.
natural coumarins are converted to dicoumarol by plant molds during curing
what is the toxic agent of moldy sweet clover poisoning? what is its affect?
dicoumarol, is a vitamin K antagonist
interferes with hepatic production of factors 2, 7, 9, and 10 (7 shortest half life, will see PT -extrinsic prolonged first)
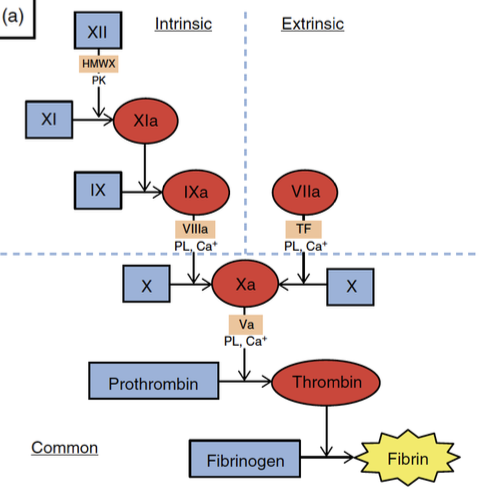
which coagulation-cascade pathway is affected first with moldy sweet clover poisoning?
affects the extrinsic pathway first (prolonged PT) because factor 7 has the shortest half life
-PT elevation can precede onset of clinical signs
-eventually all coag. times will be abnormal
what CBC changes are seen with moldy sweet clover poisoning?
anemia with normal platelet count
what are the clinical signs of moldy sweet clover poisoning?
onset in 2-7 days due to short half life of factor 7
-prolonged or excessive hemorrhages from injection sites
-epistaxis
-melena
-SC hematomas at points of trauma

how is moldy sweet clover poisoning diagnosed?
coagulation tests: initially only PT is increased, but later on PT and aPTT will be abnormal
toxicology: dicoumarol levels in feed and blood
how is moldy sweet clover poisoning treated?
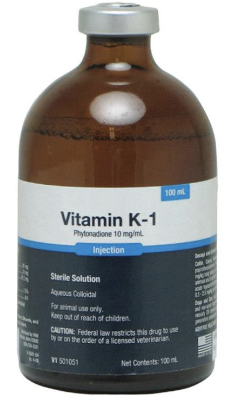
-stop feeding contaminated hay/silage
-vitamin K1 (NOT K3 - is toxic to horses, less effective)
-whole blood or plasma transfusions as required
what is the pathogenesis of warfarin toxicosis?
an anticoagulant rodenticide, pathogenesis is the same for dicoumarol (vitamin K antagonism affecting factors 2, 7, 9, 10)
what is the treatment for warfarin toxicosis?
same as for dicoumarol:
-vitamin K1 supplementation
-transfusion as needed