Drugs Used in the Treatment of Pain and Affecting the Musculoskeletal System: Part 1
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
66 Terms
Pain
◦An unpleasant sensory and emotional experience associated with actual or potential tissue damage
◦Personal and individual experience
◦Whatever the client says it is
◦Exists when the client says it exists
Pain involves:
◦Physical factors
◦Psychologic factors
◦Cultural factors
if patient is unconsious
give pain meds if vitals and injury are appropriate
acute pain
•Sudden onset
•Usually subsides once treated
•Chronic pain
•Persistent or recurring
•Lasts 3 to 6 months
•Often difficult to treat
•Tolerance
•Physical dependence
Gate Theory of Pain Transmission
- The most common and well-described theory.
- Uses the analogy of a gate to describe how impulses from damaged tissues are sensed in the brain.
- Many current pain management strategies are aimed at altering this system
WHO ladder approach
based on patient pain level this is how they prescribe meds
step 1
-non opiod
-little pain TO MILD (fall, headache, bruise)
-NSAIDS, tylenol, motrin
-1-3 on pain scale
step 2
-mild to moderate pain
-weak opioid with a non opioid (OTC)
-acetaminophen with oxycodone
-vicoprophen
-4-7 on pain scale
STEP 3
strong opiod with non-opioid
-fentynal
-dilaudid
-hydromorphone
-morphine
-severe pain
-8-10 on scale
Opioid Analgesic Agonists: Mechanism of Action
◦Agonists = bind to an opioid receptor in the brain ---> cause an analgesic response (reduction in pain sensation)
opioid analgesic agonist indications
◦To alleviate severe pain
◦Cough center suppression (vikadin/hydrocodone)
◦Treatment of diarrhea
◦Balance anesthesia
for opioids you need to monitor for (what tests should you check)
-CNS DEPRESSION
-RESPIRATORY DEPRESSION
-must check for BP/HR/RR/O2 sat
-mental status checks AAO?
Opioid Analgesics Agonists Examples
◦codeine sulfate
◦fentanyl
◦hydromorphone (Dilaudid)
◦methadone hydrochloride (Dolophine)
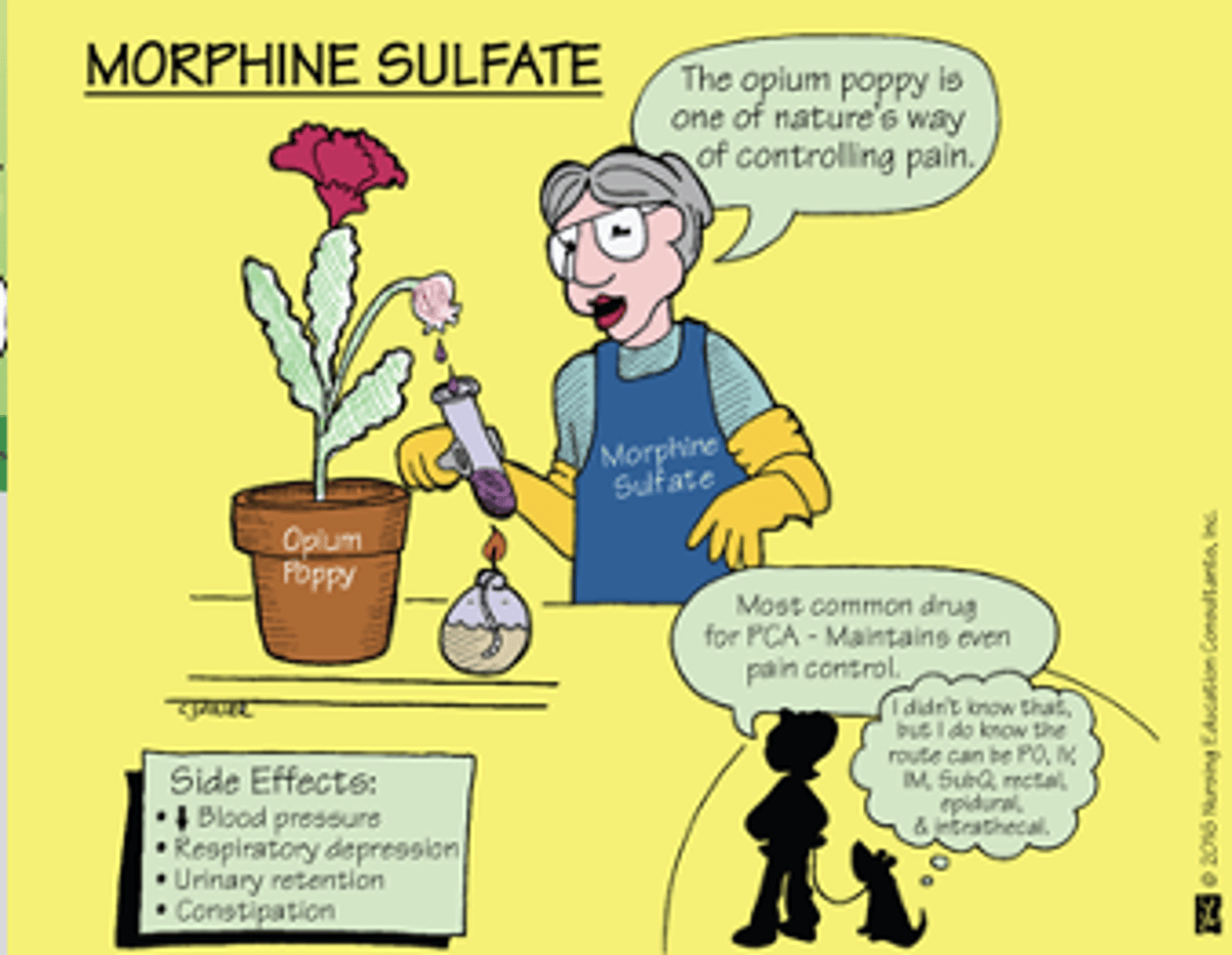
◦morphine sulfate
◦oxycodone hydrochloride
◦Percodan when combined with aspirin
◦Percocet when combined with acetaminophen
◦hydrocodone
◦Vicodin when combined with acetaminophen
contraindications for opioid analgesic agonists
•Known drug allergy
•Severe asthma
use opioid analgesic agonists with CAUTION in
•Respiratory insufficiency
•Elevated intracranial pressure (ICP)
•Morbid obesity or sleep apnea (diagrpagm is compressed)
•Paralytic ileus- no motility or blood flow in intestines (bowel can die)
•Pregnancy
interactions for opioid analgesis agonists
•Alcohol
•Antihistamines
•Barbiturates
•Benzodiazepines
•MAOIs
-these all in blue cause drowsiness
-ANYTHING THAT CAUSES FURTHER CNS DEPRESSION, can become a safety issues
opioids analgesics adverse effects
•Central Nervous System (CNS) depression*
•Nausea and vomiting (N/V)
•Urinary retention
•Diaphoresis and flushing
•Pupil constriction (miosis)
•Constipation*
•Itching
what is commonly ordered with an opioid?
anti-emmetic and anti-histamines
to stop N/V/D and itching
•Toxicity for opioid analgesics
•Severe respiratory depression
•Opioid antagonist reverses toxic effects
antidotes for opioid toxicity
•naloxone (Narcan)
•naltrexone (ReVia)
narcan can be given
-IV, PO, SL
-may need to give multiple doses, nasal spray
Opioid Withdrawal/Opioid Abstinence Syndrome
•Anxiety, irritability
•Chills, hot flashes, diaphoresis
•Joint pain
•Lacrimation, rhinorrhea
•N/V, abdominal cramps, diarrhea
•Confusion
Opioid Ceiling Effect (Tolerance)
•Drug reaches a maximum analgesic effect
•Analgesia does not improve, even with higher doses
will you get hooked?
not with short term use
-whene them off
with a patient who has tolerance what do you do
-first thing you do is increase the dose
what if the patient is at the maximum dose?
-add another drug
fentanyl
-schedule 2
-IV, topical, transmucousal
morphine
Partial Agonists MOA
◦Mixed action = bind to a pain receptor = cause a weaker neurologic response that a full agonist
◦Schedule IV: lower risk of misuse or addiction
partial aognists are not and should not
◦Not strong enough to manage long-term chronic pain
◦Should NOT be given concurrently with full opioid agonists
EXAMPLES of partial agonists
◦buprenorphine (Buprenex)
◦butorphanol (Stadol)
◦nalbuphine (Nubain)
◦pentazocine (Talwin)
if patients on partial agonists dont get relieve they get
full ones
Opioid Antagonist
-aka antidote
◦Antagonists = reverse the effects of these drugs on pain receptors by binding to a pain receptor = exerting no response
◦Drug of choice for the complete or partial reversal of opioid-induced respiratory depression
◦Indicated in cases of suspected acute opioid overdose
do you need an order for antidote?
-no hospital has standing policy for patients on opioids that they can receive narcan
naloxone (Narcan) now available without
◦a prescription and is being used by first responders for opioid/illegal drug overdoses
naltrexone (ReVia)
- oral form used for alcohol and opioid addiction
Failure of the drug to significantly reverse the effects of the presumed opioid overdose indicated
◦that the condition may not related to opioid overdose
how do you know a patient needs an antidote
-VITALS
-LOW RR/BP
-AFTER GIVING AN OPIOID
Non-Opioid Analgesic Agents
acetaminophen (Tylenol) IS MOST COMMON
acetaminophen MOA
◦Inhibits prostaglandin synthesis = blocking peripheral pain impulses; also decreases febrile body temperatures by acting on the hypothalamus
order for tylenol has to say
PRN for what
if it doesn't say PRN pain you cant give it for fever and vice versa
Indications: for tylenol
◦Mild to moderate pain and fever
◦Contraindications: tylenol
◦Known drug allergy
◦Severe liver disease
◦Glucose-6-phosphate dehydrogenase (G6PD) deficiency
◦Interactions: tylenol
◦Alcohol
◦Phenytoin, barbiturates
◦Warfarin
◦Isoniazid, rifampin
◦Beta blockers
◦Anticholinergics
tylenol adverse effects
◦Skin disorders
◦N/V
◦Blood dyscrasias
◦Nephrotoxicity
◦Hepatotoxicity
FDA limits dosage to
◦4,000 mg/day
Clients with liver disease or chronic alcohol consumption NOT
◦exceed 2,000 mg/day
-usually will give you a different med
TYLENOL toxicity and overdose can lead to ______
antidote for this is?
hepatic necrosis
◦Antidote: acetylcysteine (Acetadote) smells like rotten egg and patient has to drink it
tylenol KILLS
LIVER and due to effects can lead to other organ issues like kidney and HTN
we get which lab when patient comes in
tylenol toxicity blood levels to know if they need antidote
Non-Opioid Analgesics: tramadol hydrochloride Mechanism of action
◦Creates a weak bond to mu opioid receptors and inhibits the reuptake of norepinephrine and serotonin
Indicated for moderate to moderately severe pain
tramadol interacts with
◦Selective serotonin reuptake inhibitors (SSRIs)
◦MAOIs
◦Neuroleptics
Non-Opioid Analgesics: tramadol hydrochloride (Ultram) AE
◦Drowsiness
◦Dizziness
◦Headache (HA)
◦N/V
◦Constipation
◦Respiratory depression
◦Seizure activity
-IF ITCHING YOU SHOULD STOP MED
Non-Opioid Analgesics: Lidocaine
◦Topical (local) anesthetic/transdermal patch
◦Indications: Postherpetic neuralgia (PHN)
◦Works by stopping nerves from sending pain signals
lidocaine patch teaching
◦Applied once a day and left in place no longer that 12 hours/day
◦NEVER apply more than 3 patches at one time
-wipe off residual before putting new one on
lidocaine has minimal adverse effects like
◦Burning or discomfort at patch site
◦Redness or swelling of the skin under the patch
feverfew
ADD info
•Assist primary drugs in relieving pain
•Nonsteroidal anti-inflammatory drugs (NSAIDs)-inflammation
•Antidepressants- play with nerves to decrease pain signals to brain
•Anticonvulsants- play with nerves to decrease pain signals to brain
•Corticosteroids- decrease inflammation
•Adjuvant drugs for neuropathic pain
•amitriptyline (Elavil)
•gabapentin (Neurontin)
•pregabalin (Lyrica)
- drowsiness
if you give a drowsy analgesic and patient is asleep when you go to reassess effectiveness
-do not wake them, them sleeping shows they are not in as much pain
-just assess patient vitals, color, breaths
Treatment of Pain in Special Situations
◦Patient-controlled analgesia (PCA)- patient presses when they want but there is limit per hour
◦Placebos- used in research hospitals control group
◦Breakthrough pain- pain med doesnt work so drs prescribe something a little stronger
Analgesics: Nursing Considerations
◦Before beginning therapy, perform a thorough history regarding allergies and use of other medications, including alcohol, health history, and medical history
◦Obtain baseline vital signs (VS) and intake and output (I&O)
◦Assess for potential contraindications and drug interactions
-pain assessments
-PQRST
PAIN SCALES
0-10
OR
FACES
NURSING CONSIDERATIONS MONITOR
◦Monitor for Adverse Effects
◦Varied according to medication administered
◦Monitor for Therapeutic Effects
◦Decreased severity of pain
◦Decreased complaints of pain
◦Increased periods of comfort
◦Improved activities of daily living, appetite, and sense of well-being
◦Decreased fever (acetaminophen)
◦Pain management includes pharmacologic and non-pharmacologic approaches; be sure to include other interventions as indicated
◦Follow proper administration guidelines
◦Intramuscular (IM)
◦Intravenous (IV)
◦Ensure safety measures, such as keeping side rails up, to prevent injury
◦Withhold dose and contact healthcare provider (HCP) if there is a decline in the client's condition or if VS are abnormal, especially if respiratory
◦Instruct clients NOT to take other medications or over-the-counter (OTC) preparations without checking with their HCP
◦Instruct clients to notify HCP for signs of allergic reaction(s) or adverse effect(s)
◦Oral preparations should be taken with food to minimize gastric upset
Be sure to medicate clients before the
◦the pain becomes severe
◦Think about performing a procedure such as a dressing change to a surgical wound?