9. large animal med- ruminant urinary tract disorders
1/68
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
69 Terms
what is the anatomy of bovine/small ruminant kidneys?
bovine: have lobulated kidneys, with the left palpable per rectum
small ruminants: have smooth kidneys that can be palpated via the skin

why is the bladder hard to feel/palpate in late gestation in cows?
bc under the large uterus
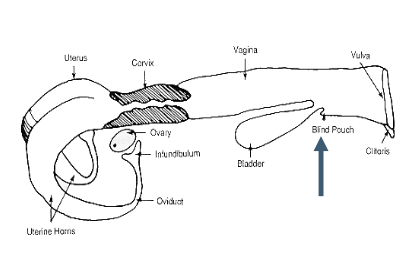
what do female ruminants have in their urethra that may make catheterization difficult?
sub-urethral diverticulum
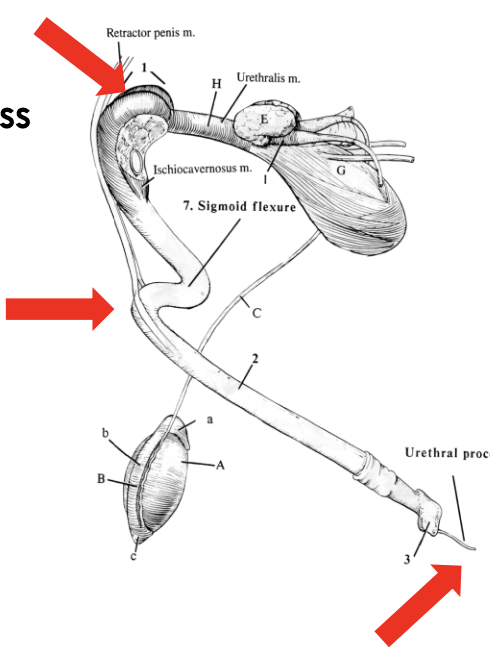
why is catheterization in male ruminants difficult?
due to sigmoid flexure (also traps calculi) and dorsal diverticulum
small ruminants also have a urethral process making it more difficult
how can urine be collected in male goats/cattle?
goats: wait for them to stand up (will usually urinate when standing up)
cattle: warm water cleaning of prepuce, and dry massage of preputial orifice
what history/clinical signs may be indicative of urinary disorders in ruminants?
discolored urine, colic, stranguria
any sad buck/wether is a possible urolithiasis case
how is the urinary system of ruminants examined on physical exam?
-palpate kidneys transabdominally or left kidney/bladder per rectum (check for pain, or loss of lobulation in bovine)
-palpate urethra rectally/perineally for pulsation (stones)
-palpate urethra in sheath and urethral process
-inspect prepuce for dryness, crystals, inflammation, etc.
presence of what in the urinalysis may be indicative or urinary disorders?
USG in azotemia
presence of blood
WBCs
protein
--> culture urine where indicated (ideally sterile collection via catheter)
how can CBC be useful for identifying urinary disorders?
can be useful if disease is associated with inflammation or hemorrhage (anemia)
what chem panel values are of concern in patients with urinary disorders?
BUN
creatinine
electrolytes
pH
lactate
--> blood gas can often provide the most relevant values quickly and is more economic (than doing chem panel)
what ancillary tests should be performed if suspicious of uroabdomen?
compare peripheral to abdominal fluid creatinine in possible uroabdomen cases
(abdominal >2x higher than serum creatinine)
what are causes of pre-renal azotemia?
reduced renal perfusion causing decreased GFR (due to dehydration, hemorrhage, shock)
severe hypo-perfusion can eventually cause renal failure
increases in BUN/creat can be profound in ruminants
what causes renal azotemia?
intrinsic dysfunction results in impaired excretion of urea, creat, potassium, etc.
hypo-perfusion or toxic, inflammatory, or infectious damage
what causes post-renal azotemia?
urinary obstruction (common in ruminants)
can cause renal dysfunction if severe or chronic
pre-renal azotemia is unlikely to cause serious renal injury if?
if volume is quickly restored and underlying cause is neutralized
what does severe azotemia and poor response to therapy strongly indicate?
renal disease
what should be done if obstruction is suspected in small ruminants?
exteriorize penis
-sedate with medazolam/ketamine/torb or ace
-avoid xylazine (is a diuretic)
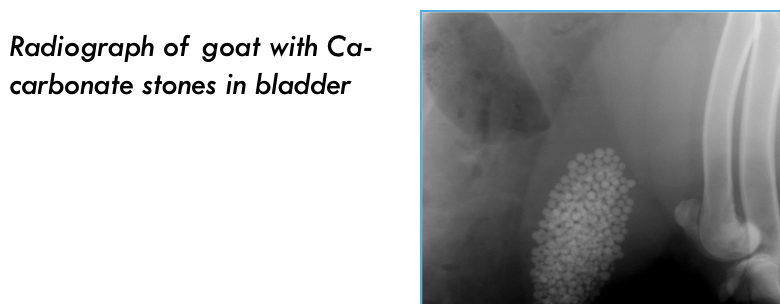
how can radiographs be used to diagnose small ruminants suspected to have urolithiasis?
will pick up calcium-carbonate stone (not struvite or mucus plugs since not mineral-dense)
how can ultrasound be used to diagnose small ruminants suspected to have urolithiasis?
transabdominal: identify uroperitoneum, evaluate right kidney, evaluate bladder of small ruminants (from right inguinal region)
transrectal: bladder/L kidney in bovine
stone localization along urethra
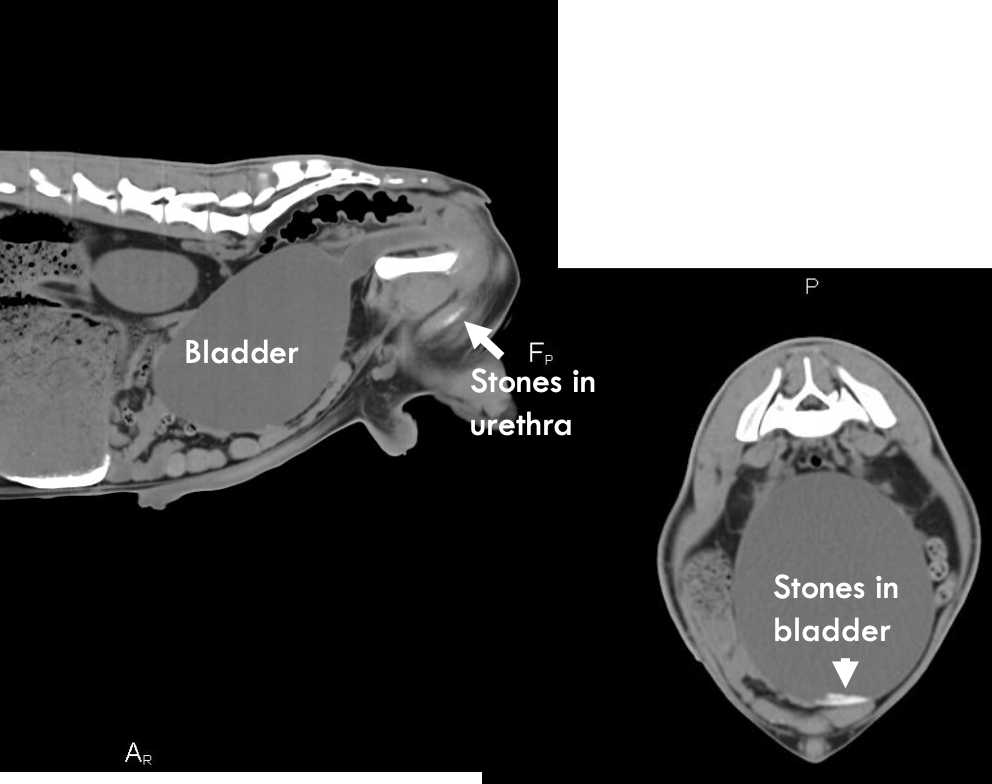
how can CT be used to identify urinary disorders in ruminants?
picks up stones, umbilical issues in calves/small ruminants (usually not cost effective)
CT scan of goat with Ca-carbonate stones in bladder

which animals can cytoscopy be used to evaluate for urinary disorders?
female animals only- can evaluate bladder/ureters
scopes are not small enough to examine male ruminant urinary systems
what is tubular necrosis (nephrosis)?
category of renal disease in which necrosis of renal tubules is a prominent feature
-toxic, inflammatory, infectious, or hemodynamic origin
-causes acute or chronic renal insufficiency
what are the laboratory findings of tubular necrosis?
azotemia
isosthenuria (USG 1.008-1.014)
electrolyte derangements
what are some etiologies of tubular necrosis?
1. plants: oak, oxalate, vitamin-D analogues
2. metals: mercury, arsenic, copper (hemoglobin)
3. drugs: aminoglycosides, oxytet, NSAIDs
4. toxemia: bacterial toxins (+ dehydration and nephrotoxic signs)
5. other: monensin, ethylene glycol, pigmenturia (myoglobin)

what are clinical signs of tubular necrosis?
-anorexia, lethargy
-anuria, oliguria, polyuria
-azotemia with poor response to appropriate fluids, isosthenuria
-electrolyte derangements: high P, low K, Ca, Na, Cl
-weight loss
-edema with chronicity

what are potential causes of low sodium and chloride in ruminants?
renal insufficiency
GI disease
3rd spacing into cavities (uroabdomen)
iatrogenic
what is the treatment for tubular necrosis?
1. remove toxin or cease drugs (rumenotomy, activated charcoal)
2. correct hydration
3. diuretics in specific cases (furosemide, mannitol, dextrose)

what is the goal of correcting hydration in patients with tubular necrosis?
restore glomerular filtration rate and promote urine output
-via IV, small NG tube, or rumenostomy
what does prognosis of tubular necrosis depend on?
depends on response to treatment
what do cystitis and pyelonephritis in ruminants usually result from?
usually a result from ascending infection, most cases occur 3 months after calving

what etiologic agents are most commonly isolated in cases of cystitis/pyelonephritis?
1. corynebacterium renale (gram + rod and normal (commensal) flora of distal female repro tract and sheath of male)
2. trueperella pyogenes
3. e. coli

what are the clinical signs of acute cystitis?
-dysuria: tail swishing, arched stance after urinating, treading the feet
-pollakiuria
- +/- gross hematuria and polyuria

what are the clinical signs of acute pyelonephritis?
all clinical signs of cystitis plus:
-fever, anorexia
-sudden drop in milk production
-colic: renal or ureteral pain

what are the chronic clinical signs of cystitis/pyelonephritis?
vague and inconsistent:
-inappetance and weight loss
-poor growth rate
-decreased milk production
-urination behavior may be normal (look for crystals and scalding--> indicate dribbling)
-polyuria
-variable presence of fever
-gross urine abnormalities may be absent or intermittent
what urinalysis findings are seen with cystitis/pyelonephritis?
increased WBCs and RBCs
proteinuria (if chronic)
variable specific gravity
what chemistry findings may be seen with cystitis/pyelonephritis?
azotemia and electrolyte anomalies suggest severe bilateral disease
what CBC/hemogram findings may be seen with cystitis/pyelonephritis?
may be normal with uncomplicated cystitis
-neutrophilia
-hyperfibrinogenemia (>600mg/dL)
-high total protein (globulins) unless hypoalbuminemia
-mild non-regenerative anemia
how is cystitis/pyelonephritis diagnosed?
1. clinical and laboratory findings
--> catheterized urine culture valuable for diagnosis
2. ultrasound: bladder and kidneys
3. endoscopy (females): ureteral catheterization if possible
what should be determined when making a diagnosis of cystitis/pyelonephritis?
-if cystitis alone or with pyelonephritis
-causative agent
-rule out other dz such as traumatic reticuloperitonitis
how is cystitis differentiated from urolithiasis?
cystitis and urolithiasis both cause dysuria, but:
-larger volume of urine in cystitis than obstruction
-bladder is less likely distended in cystitis
what is the sex predisposition for cystitis vs. urolithiasis in ruminants?
females: cystitis
males: urolithiasis
how is cystitis with pyelonephritis differentiated from just cystitis alone?
cystitis with pyelonephritis:
-enlarged, painful or less lobulated kidney on rectal
-ultrasound anomalies of kidney possible
-systemic signs of illness and CBC/chem changes
-endoscopy of bladder to check ureters, collect urine
-culture of C. renale increases likelihood of kidney involvement
what is the treatment for cystitis/pyelonephritis?
procaine penicillin best choice for c. renale (monitor appetite, temp, and urine strip daily)
if no improvement in 96hrs, consider changing to abx w/ definite gram-negative spectrum
isolate cows with c. renale (contagious!) and decontaminate their areas
what is pizzle rot?
contagious, ulcerative infection of the mucus membrane and skin of the prepuce or vulvar region due to c. renale
very resistant and can live 6 months in wool/scabs

what are causes of pizzle rot?
normal flora proliferates in response to high urinary urea concentrations:
-high dietary protein
what are clinical signs of pizzle rot?
dysuria
pain
impaired breeding in males and females
what is the treatment for pizzle rot?
clipping hair, topical agents, and systemic penicillin or tetracycline
which animals are most prone to obstructive urolithiasis?
male ruminants, especially wethers and steers (castrated males)
can develop at any age
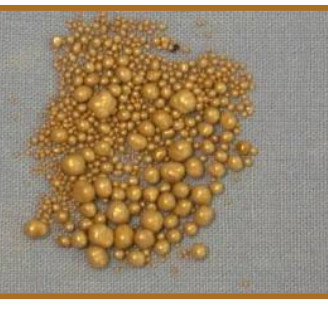
what are different types of stones causing obstructive urolithiasis?
-struvite (related to low Ca:P ratios)
-silicate (ruminants on native grass in western US)
-calcium carbonate (round, gold stones- OR)
-calcium oxalate
-mucoprotein plugs (clover pasture, hormonal implants)
what are potential consequences of obstructive urolithiasis?
urethral obstruction (partial/complete)
urethral rupture
bladder rupture
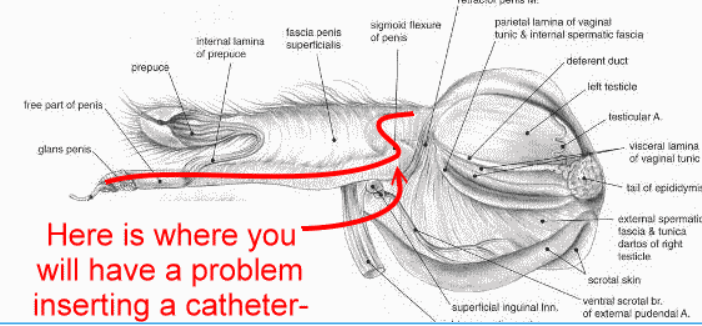
what are the common sites of entrapment in obstructive urolithiasis?
1. sigmoid flexure: steers, also sheep and goats
2. urethral process: common site in sheep and goats
sometimes the entire urethra is a string of stones
what are the clinical findings of acute obstructive urolithiasis?
-anxiety, colic
-stranguria; occasional secondary rectal prolapse
-mild urethral swelling at site of obstruction
-crystals and blood on preputial hairs
-anuria or dribbling
-tachycardia

what are the clinical findings of urinary tract rupture (24-48 hours)?
-urethral rupture in steers causes ventral and preputial edema
-in chronic cases, skin and SQ tissues begin to slough
-bladder rupture relieves stranguria
-progressive abdominal distension

what are clinical signs of uremia?
weakness
anorexia
shock
how is obstructive urolithiasis diagnosed?
urinary tract examination, palpation
what serum chemistry changes are seen with obstructive urolithiasis?
-azotemia
-low Na, Cl
-high K
-depends on time course of obstruciton
how is ultrasound/radiographs used to diagnose obstructive urolithiasis?
ultrasound:
-identify stones and distended bladder
-subcutaneous fluid or uroperitoneum if ruptured
-check for hydronephrosis
rads: include entire urethra
what findings from abdominocentesis/fluid analysis is seen with obstructive urolithiasis?
creatinine in fluid is 2x that of serum creatinine
why may CT be indicated in some cases to diagnose obstructive urolithiasis?
to find missed stone, and check the bladder for stones
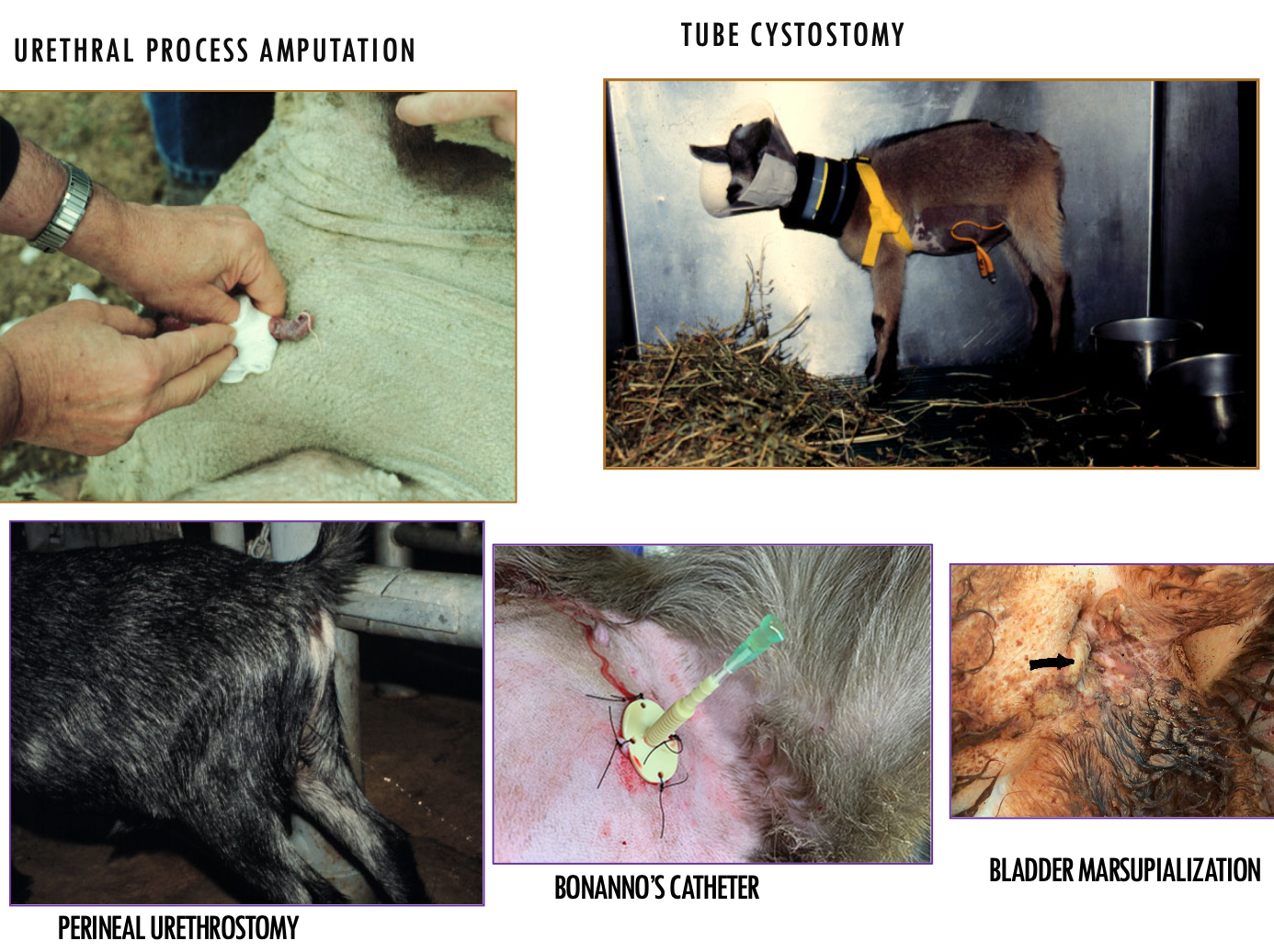
what is the treatment for obstructive urolithiasis?
-pain management/sedation
-metabolic/hemodynamic stabilization
-prevention of rupture (cystocentesis)
-relief of obstruction
-pain management
what meds can be used for pain management with obstructive urolithiasis?
-epidural or opioid (torb) analgesia
-sedation and relaxation: ace, midazolam, ketamine
-phenoazopyridine (urinary analgesic)
-NSAIDs (with caution until rehydrated)
what medical therapy is used for managing/treating obstructive urolithiasis?
-stabilization critical if anesthesia is planned
-need outlet for urine
-supportive care (isotonic NaCl bolus, then maintain)
-address hyperkalemia (dextrose, insulin, bicarb)
what are methods for creating an outlet for urine in medical management of obstructive urolithiasis?
-epidural/sedation may help relax urethra
-check if urethral process should be removed
-consider using curved catheter in urethra
-bonanno's catheter thru abdomen
-drain bladder or uroabdomen
how is obstructive urolithiasis due to calcium carbonite calculi prevented?
-reduce calcium be removing alfalfa hay
-urinary acidification (ammonium chloride)
-reduce dietary cation-anion balance with chloride
-avoid browsing
how is obstructive urolithiasis due to phosphatic or struvite calculi prevented?
-improve Ca:P ratio to 2:1
-avoid pelleted feeds and increase forage
-add NaCl at 3-5%
-add ammonium chloride at 0.5-1% of ration
-improve water intake (regular cleaning, shade, multiple water sites)
how is obstructive urolithiasis due to silica calculi prevented?
-add NaCl at 15% to creep feed for range calves
-add ammonium chloride at 1% of ration
-improve water intake
-consider grass hay supplementation for wethers/steers to reduce range grass intake
what are causes of red urine in ruminants?
hemoglobinuria or hematuria (myoglobinuria rare in ruminants)
--> hemoglobinuria: toxic, clostridium, immune mediated, water in neonates
--> hematuria: infection, stones, neoplasia
what are general causes of urinary straining/discomfort in ruminants?
infection
stones
neoplasia
what are the most common causes of renal dysfunction in ruminants?
hemodynamic or toxic causes