Motor Speech Disorders Exam 1
1/134
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
135 Terms
CNS and PNS
Dysarthria profiles are variable and based on speech and physiological characteristics that are the result of damage to
1)
2)
Spastic
This type of dysarthria is caused by bilateral upper motor neuron damage
Recurrent Laryngeal nerves, Pharyngeal Plexus, Superior Laryngeal nerves
In flaccid dysarthria, which 3 branches of the Vagus (V)nerve are damaged?
Vagus (V)
If this CN is damage, it leads to difficulty tensing the vocal folds and modulating pitch during speech?
respiration
when there is widespread spinal nerve damage in flaccid dysarthria, what area related to speech production is predominantly affected?
motor
upper motor neurons take _______ impulses created in the brain and transmit them to the lower motor neurons in the cranial and spinal nerves
Trigeminal (V, 5)
Damage to which CN leads to the inability to elevate the mandible for speech and mastication?
F
T or F:
Fast speech rate is a hallmark characteristic of Spastic Dysarthria
F
T or F:
Distorted vowels and consonants are most likely to result when there is a widespread of spinal nerve damage
Ataxic
In what type of Dysarthria are the following tasks useful to assess speech characteristics:
1. conversational speech
2. sentence repetition tasks
3. reading
4. non-speech AMR's of the jaw
Hypokinetic
Damage to the Basal ganglia and the subcortical structures will result in this type of dysarthria:
cerebellum
ataxic dysarthria is caused by damage to the _______
hyperkinetic
this is a group of Dysarthria's with perceptual effects of involuntary movements resulting in distorted and/or interrupted execution of speech. The impact on speech output will vary depending on the type, severity, and location of excessive movements
Stroke, Parkinson's Disease (PD), Chronic Traumatic Encephalopathy (CTE)
What etiologies are associated with Hypokinetic Dysarthria?
Chorea
Involuntary, quick dancelike movements of the feet, hands, extremities, head, and neck
hypokinetic
In Sally's case history, she reports that people have difficulty understanding her. They often ask her to repeat and speak up because they cannot hear her, but she feels like she is speaking at an adequate level. She fatigues and her speech intelligibility diminishes over time. Sally's symptoms are most in line with which type of dysarthria?
Hyperkinetic
Per MD report, the patients exhibiting failed connections that properly inhibit cortical motor discharges. Therefore, the patient presents with unrefined motor plans that present as excessive uncontrolled movements. This is most representative of which dysarthria?
Flaccid
The patient presents with weakness or paralysis of musculature used to produce speech and hyporeflexia (lack of appropriate reflexes). Lesion site is indicative of Final Common Pathway (FCP) involvement. This most likely represents what kind of dysarthria?
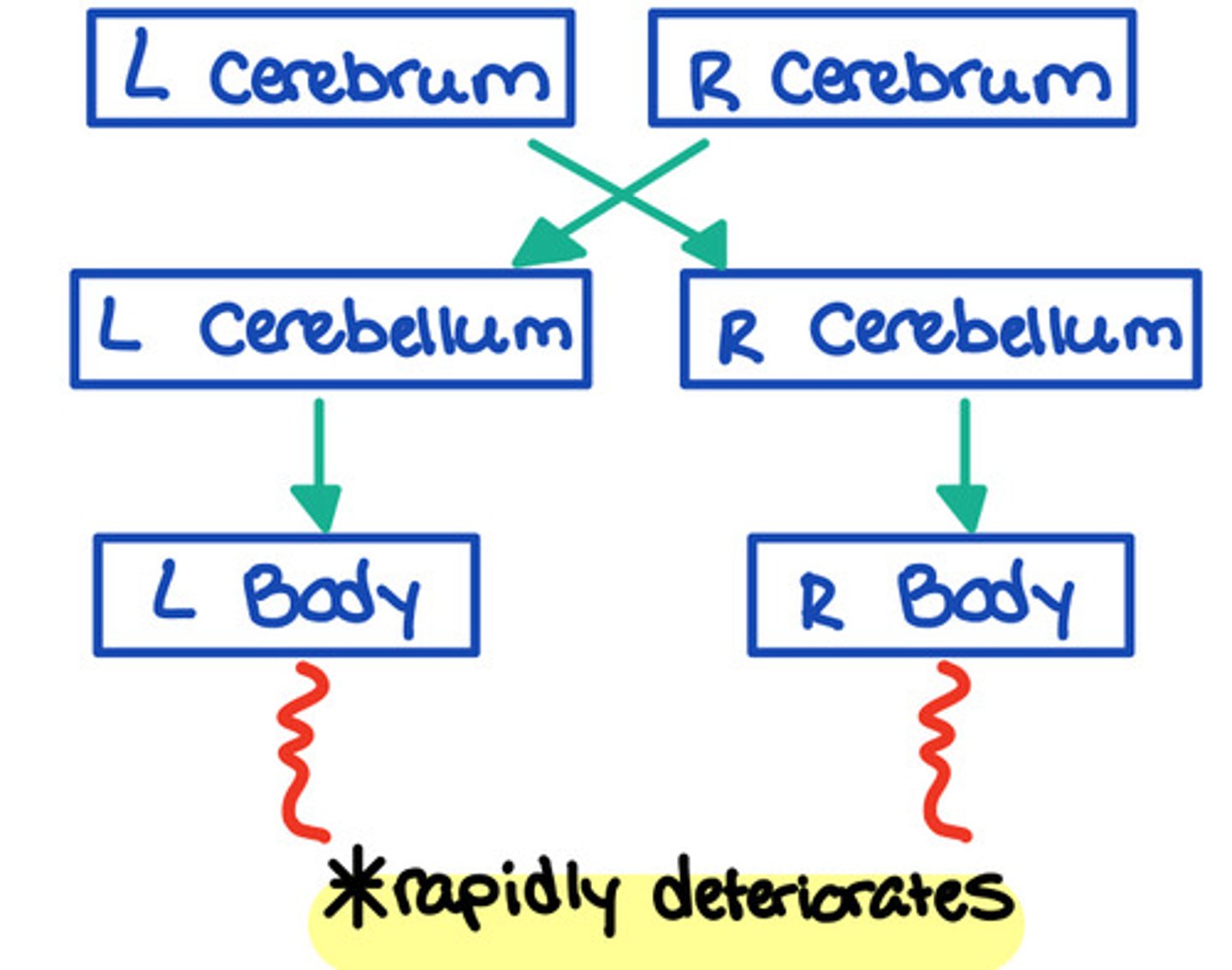
right side
Upon reviewing the electronic medical record, the CT scan indicates a cerebrovascular infarct (stroke) on the right cerebellar region. What side of the body would the clinician expect the patient to have difficulty moving?
This is representative of Ataxic Dysarthria:
Damage to the cerebellum or to the neural tracts that connect the cerebellum to the rest of the central nervous system (CNS)
1. Each cerebellar hemisphere is connected to the opposite thalamus and cerebral hemisphere
2. Each cerebellar hemisphere helps control movement on the ipsilateral side of the body.
Motor Speech Disorders (MSDs)
- speech disorders resulting neurological impairments affecting the planning, programming, control, or execution of speech
- Malfunction of the tactile (touch), kinesthetic (movement), and proprioceptive (awareness) sensations
Dysarthria
control vs. execution
- Group of neurological speech disorders produced by damage to the CNS or PNS that affect speech production
- Symptoms vary based on the type and location of brain lesions
- Reflect abnormalities in strength, speech, range, steadiness, tone, or accuracy
Apraxia
planning vs. programming
- Lack of movement or action for speech production
- Different types: Inability to move eyes, limbs, oral structures
Telltale signs:
1. groping
2. no pattern
3. no muscle coordination
CN V (5)
Trigeminal
Sensory and motor
Controls the muscles of mastication
CN VII (7)
Facial
Sensory and motor
Controls the muscles of mastication, including the lips
CN VIII (8)
Vestibulocochlear (auditory)
Sensory
Serves the sense of hearing
CN IX (9)
Glossopharyngeal
Sensory and motor
Contributes to the pharyngeal movement.
Bilateral innervation - single muscle not bilateral symmetry.
CN X (10)
Vagus
Sensory and motor
Contributes to movements of the pharynx and larynx and serves a sensory function for the pharynx, larynx, trachea, bronchi, and lungs.
Bilateral.
CN XI (11)
Spinal Accessory
Motor
Controls the movements of the muscles of the neck, thus indirectly influencing the position of the larynx. Controls turning of head & shrugging shoulders.
CN XII (12)
Hypoglossal
Motor
Controls the tongue movements. Bilateral except cells serving genioglossus muscle; which receives only contralateral fibers
bringing lips together
Bilateral facial weakness results in difficulty
spinal nerves (because it feeds into the diaphragm and Intercostals)
What type of nerves effect respiration when they are extensively damage
cerebral palsy
Spastic dysarthria occurs in children due to
unilateral
on one side
bilateral
on both sides
ipsilateral
on the same side
contralateral
on the opposite side
paresis
partial or incomplete loss of movement (weakness)
paralysis
total loss of movement
lesion
abnormal change in body tissue usually as a result of disease or trauma
speech systems
systems supporting the production of speech which includes articulator, phonatory, and respiratory systems
hypotonic
lack of appropriate muscle tone
hypertonic
excess/tightness of muscle tone
hyporeflexia
lack of appropriate reflexes
hyperreflexia
excess/overactive reflexes
fasciculations
visible isolated twitches in resting muscle
fibrillations
invisible, spontaneous contractions of individual muscle fibers
slurred speech
a hallmark characteristic characteristic of ataxic dysarthria is
F
T or F:
cognitive deficits in ataxic dysarthria are a result of damage to the cerebral hemisphere: _____: damage to the cerebellum itself
Parkinson's Disease
The most common movement disorder associated with hypokinetic dysarthria:
(key: shuffle, tremor, articulation, prosody, expressionless, slow movements, low intensity)
quiet or weak voice
a hallmark characteristic of hypokinetic dysarthria is report of:
static/resting tremor
- present in limbs, jaw, lips, and tongue
- pill-rolling movement: movement between thumb and forefinger, can be unilateral
cogwheel rigidity
- resistance of the limbs to passive stretch in all directions and full of ROM, has a jerky character
- different from spasticity where resistance to movement is greatest at beginning of the stretch and biased in one condition
posture
- involuntary flexion of the head, trunk and arms
- difficulty w/turning in bed, moving from sitting to standing position, adjusting to tilting or falling
bradykinesia
- difficulty w/movement, planning, initiation, and execution
- delay/false starts. slow and difficult to stop, reduced amplitude and speed of repetitive movements
akinesia
- "freezing"
- inability to move
hypomimia
reduced movement in the face resulting in masked or expressionless and unblinking facial expression
dyskinesias
general term used to refer to abnormal, involuntary movements regardless of etiology
dystonia
involuntary, slow, irregular, painful twisting of extremities and body that are manifested as abnormal and involuntary twisting of the body
spasm
involuntary, sudden muscle contraction
tics
involuntary, quick, repetitive, stereotyped movement
tremor
involuntary, rhythmic, quick movement occurring 3-5 times per second
athetosis
involuntary slow writhing movement
ballism
Bilateral, involuntary, irregular, possibly wild or violent flinging of extremities
Hemiballismus
unilateral, involuntary, irregular, possibly wild or violent flinging of extremities
myoclonus
- involuntary single or repetitive brief, lighting
-like jerks of a body part
- can be rhythmic or non-rhythmic
- cannot be inhibited willfully
Spastic Dysarthria (Hallmark Characteristics)
- Strained/strangled/harsh vocal quality
- Reduced pitch and loudness variability
- Slow speech rate
- Slow and regular speech alternating motion rates (AMRs)
articulation, phonation, respiration (of the speaker)
speaker oriented approaches target
indirectly affect speech function (medication affects the whole body)
the aim of pharmacological treatment serves to
patient is unable to produce no more than 1 word per breath group
clinicians should work towards increasing support for speech breathing if
addressing articulation in conjunction with respiration and intensity
accuracy and precision of articulation is solely accomplished by
t
T or F
the focus of speaker Orientec approaches is to restore to precious state or compensate for impairment
improve comprehensibility of messages and efficiency of transmission
focus of communication oriented approaches is to
surgical and pharmacological
effective management approaches for hyperkinetic dysarthria are primarily
myasthenia graves
behavioral treatment approaches are contraindicated for
presence of specific dysarthria types and underlying causes
management for mixed dysarthria is determined by
F
T or F
if you have implemented treatment do not change until you have reached the time period indicated in your plan of car
flaccid dysarthria (clinical characteristics)
- Flaccid weakness or paralysis of musculature to produce speech
- Paralysis is indicative of Final Common Pathway Damage: Hyporeflexia
- Diminished reflexes
- Low muscle tone (hypotonia) and weakness in the muscle
- Atrophy
- Hypoactive gag reflex
- Nasal backflow while swallowing
flaccid dysarthria (etiologies)
- Muscle disease: muscular dystrophy & polymyositis
- Vascular disorders
- The result from damage of varying degrees to 1 cranial nerve or multiple cranial nerves (Bulbar Palsy)
flaccid dysarthria (site of lesion)
Peripheral nervous system OR lower motor neuron (LMN) involvement
CN V (Trigeminal-flaccid)
jaw weakness, reduced sensation from face, jaw, lips, tongue, articulatory imprecision.
specific site of lesion?
type of dysarthria?
CN VII (Facial-flaccid)
unilateral facial weakness; mild articulatory distortions
specific site of lesion?
type of dysarthria?
CN IX (Glossopharyngeal -flaccid)
- Rarely damaged in isolation
- May present with reduced gag reflex
- May affect pharyngeal elevation: 1. During swallowing and 2. During resonant or phonatory functions
CN X (Vagus-flaccid)
weakness of velopharyngeal and laryngeal muscles; hypernasality, nasal emmision, breathiness
All 3 branches are damaged
1. Pharyngeal plexus: innervates muscles of pharynx and velum
2. Superior Laryngeal Nerves: monotone voice, tenses the VF and modulates pitch
3. Recurrent laryngeal nerves: breathy/hoarse voice bc paresis/paralysis of VF
CN XI (Accessory-flaccid)
- Unclear what the damage may cause
- Works with the vagus nerve to innervate the velum, pharynx, and larynx
tongue weakness; imprecise articulation specific site of lesion?type of dysarthria?
spinal nerves (flaccid)
- When damage is widespread, it can affect respiration for speech production
Results in:
1 decreased in speech loudness
2 shortened utterances
3 impaired prosody
4 strained vocal quality
Flaccid dysarthria (speech characteristics)
Respiration
- Speech on residual air
- Slow respiratory rate
Resonance
- Hypernasality
- Nasal emission
Phonation
- Harsh or hoarse
- Breathiness
- Audible inspirations (stridor)
Articulation
- Imprecise consonants and vowels
- Prolonged segments
- Decreased force
Prosody
- Reduced utterance length (short phrases)
- Reduced rate
- Mono pitch
- Monoloudness
flaccid dysarthria (confirmatory characteristics)
- Breathiness, hoarseness, diplophonia, short phrases, reduced maximum vowel duration, vocal flutter
- Audible inspiration, inhalatory stridor, weak cough, weak glottal coup
spastic dysarthria (clinical characteristics)
- Spasticity is hypertonia (excessive muscle tone) and resistance to passive movement: Tense
- Difficulty with neuromuscular execution
spastic dysarthria (etiologies)
- Anything that may produce damage to the Bilateral Upper Motor Neuron (UMN) pathways
- Vascular disorders
- Degenerative diseases: Peripheral lateral sclerosis (PLS) and amyotrophic lateral sclerosis (ALS)
- Trauma or cerebral palsy in children
spastic dysarthria (speech characteristics)
Respiration
- Shallow inhalations/exhalations
Resonance
- Hypernasality
- Phonation
- Low pitch, pitch breaks
- Harshness
- Strained, strangled voice
Articulation
- Labored
- Reduced range of motion
- Decreased oral section control
- Imprecise consonants
- Distorted vowels
Prosody
- Reduced utterance length (short phrases)
- Reduced stress
- Mono pitch
- Monoloudness
- Slow rate
spastic dysarthria (confirmatory signs)
- Strained, strained-harsh, strained-strangled voice quality
- Grunt at end of expiration
ataxic dysarthria (clinical characteristics)
- Presence of abnormal uncoordinated movements
- Non-Aphasic Cognitive-Communication Deficits
- Specific localization to the cerebellum OR cerebellar control circuit
When listening to a patient with dysarthria
1. Underlying weakness
2. Resistance to movement
3. Restriction of movement
4. Poor timing, control, and coordination
ataxic dysarthria (etiologies)
- Any process that damages the cerebellum or cerebellar control circuit
- Degenerative
- Vascular
- Traumatic
- Demyelinating
ataxic dysarthria (site of lesion)
- Damage to the cerebellum or to the neural tracts that connect the cerebellum to the rest of the CNS
- Each cerebral hemisphere is connected to the opposite thalamus and the cerebral hemisphere
- Each cerebellar hemisphere helps control movement on the ipsilateral of the body
ataxic dysarthria (speech characteristics)
- Most evident in articulation and prosody
Phonatory- respiratory-prosodic
- Monoloudness
- Excessive loudness variations
Phonatory- prosodic insufficiency
- Harshness
- Mono pitch
Articulation
- Imprecise consonants
- Irregular articulatory breakdowns
- Distorted vowels
Prosodic excess
- Excess and equal stress
- Prolonged phonemes
- Prolonged intervals
- Slow rate
ataxic dysarthria (tasks to assess)
- Conversational speech, sentence repetition tasks, reading and non-speech AMR’s of the jaw, lips, and tongue
- Oral mech exam
Patient description of Symptoms
1 *Slurred speech
2 *“Drunken” speech
3 Rapid deterioration of speech
4 *Reducing their rate of speech improves intelligibility
Hypokinetic Dysarthria (clinical characteristics)
- Rigidity, reduced force, reduced range of movement, and slow/sometimes fast repetitive movements on speech
Problem with motor control
1 Preparation
2 Maintenance
3 Switching motor programs
Hypokinetic Dysarthria (etiologies)
- Any process that interferes with basal ganglia control circuit
- Degenerative: Parkinson’s Disease (PD)
hypokinetic dysarthria (site of lesion)
- Damage to the Basal Ganglia Control Circuits and their structures
Striatum
Circuit
1 Regulates muscle tone, controls postural adjustments
2 Regulates movements
3 Scales the force, amplitude, and duration of movements
4 Assists with learning, preparing, and initiation of movements
hypokinetic dysarthria (speech characteristics)
- Most evident in voice, articulation, and prosody
Phonatory- respiratory-prosodic
- *Monoloudness
Phonatory-prosodic
- *Mono pitch
Phonatory
- Harsh voice quality
- Breathy voice
- Low pitch
Articulation
- Imprecise consonants
- *Repeated phonemes
Articulatory-prosodic
- *Shorts rushes of speech
- *Variable rate
Prosodic
- *Reduced stress
- *Inappropriate silences
- *Increased rate in segments
- *Increase of rate overall