The ICU Book Chapter 9: Systemic Oxygenation
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
How is tissue oxygenated evaluated?
Unable to be measured in the clinical setting
Evaluated indirectly using global measures of systemic oxygen transport (i.e. O2 delivery and O2 uptake as well as a presumed marker of inadequate tissue oxygenation (i.e. plasma lactate)
Oxygen Saturation of Hemoglobin (SO2)
Oxygenation of the hemoglobin pool, fraction of the hemoglobin pool that is fully saturated with oxygen
Measured by oximetry as the ratio of oxygenated hemoglobin to total hemoglobin
What are the principal determinants of SO2
PO2 in blood
The affinity of hemoglobin for binding O2
What are two advantages of the S shape of the oxyhemoglobin dissociation curve?
PaO2 is normally on the upper, flat part of the curve, which means that a large drop in PaO2 (down to 60 mmHg) results in only minor changes in SO2
PvO2 (which is ~40 mmHg) is on the steep portion of the curve which facilitates O2 uptake in the pulmonary capillaries
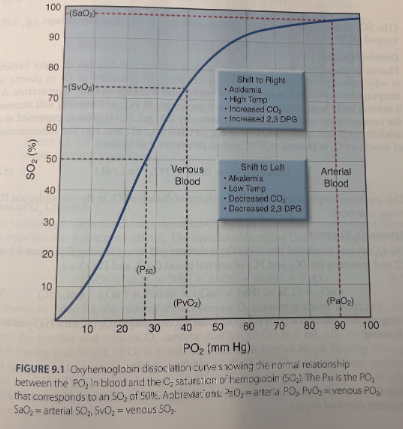
What does a shift of the oxyhemoglobin dissociation curve to the right facilitate?
O2 release in tissues
What is the effect of a shift of the oxyhemoglobin dissociation curve to the left?
Impedes O2 release
P50
The PO2 that corresponds to a SO2 of 50%
Normally about 27 mmHg
Will increase when the curve shifts to the right
Will decrease when the curve shifts to the left
Effects of shifts in the oxyhemoglobin dissociation curve in the pulmonary and systemic capillaries
Have opposing effects in the pulmonary and systemic capillaries
A shift to the left impedes O2 release systemically but facilitates O2 uptake in the lungs
What makes up the concentration of O2 in the blood?
O2 bound to hemoglobin + O2 dissolved in plasma
Hemoglobin-Bound Oxygen Equation
Concentration of hemoglobin-bound O2 (HbO2) is determined by the concentration of hemoglobin, the O2 binding capacity of hemoglobin (1.34 mL O2 per gram Hb), and the O2 saturation of hemoglobin (SO2)
HbO2 = 1.34 x [Hb] x SO2
What does the solubility of O2 in plasma depend on?
Temperature-dependent
Varies inversely with a change in body temperature
Dissolved O2 Equation
At normal body temperature (37*C), each increment in PO2 of 1 mm Hg will increase the concentration of dissolved O2 in plasma by 0.03 mL/L
Expressed as a solubility coefficient of 0.03 mL/L/min
Concentration of dissolved O2 in plasma at 37*C:
Dissolved O2 = 0.003 x PO2 (mL/dL)
CaO2 Equation
(CaO2) = (1.34 x [Hb] x SaO2) + (0.003 x PaO2)
Normal arterial O2 content is about 20 mL/dL (or 200 mL/L) and only 1.5% represents dissolved oxygen
How does a 50% reduction in [Hb] affect CaO2?
Results in an equivalent 50% reduction in CaO2
Anemia has a much greater influence on arterial oxygenation than hypoxemia
How does a 50% reduction in PaO2 affect CaO2?
Results in only a 20% decrease in CaO2
What is the normal mixed venous O2 content?
About 15 mL/dL and less than 1% represents dissolved O2
What is the difference between arterial and venous O2 content?
(CaO2 - CvO2) = 5 mL/dL or 50 mL/L
Means that 50 mL of O2 is extracted from each liter of blood flowing through the capillaries
What % of the total blood volume do arteries contain?
25%
What % of the total blood volume does the venous circulation contain?
75%
What % of the O2 in the blood is not available for aerobic metabolism?
About 70% because it is in the venous circulation
What are the three parameters that describe transport of O2 from the lungs to metabolizing tissues?
The rate of O2 delivery in the arterial blood (O2 delivery)
The rate of O2 uptake from the systemic microcirculation (O2 uptake)
The fractional excretion of O2 from capillary blood (O2 extraction ratio)
Oxygen Delivery (DO2) Equation
DO2 = CO x CaO2 x 10
The multiplier of 10 is used to convert the CaO2 from mL/dL to mL/L
DO2 = CO x (1/34 x [Hb] x SaO2) x 10
Oxygen Uptake (VO2)
The rate of O2 transport from the systemic capillaries into the tissues
Since oxygen isn’t stored in the tissues, VO2 is also a measure of the oxygen consumption in systemic tissues
Oxygen Uptake (VO2) Equation
VO2 = CO x (CaO2 - CvO2) x 10
A modified version of the Fick equation for cardiac output (CO = VO2/CaO2-CvO2)
Called the reverse Fick method
VO2 = CO x 1.34 x [Hb] x (SaO2 - SvO2) x 10
By what % must the VO2 that is calculated from the modified Fick equation change to be considered significant?
By at least 18%
Calculated vs Measured VO2
The calculated VO2 is not the whole body VO2 because it does not include the VO2 of the lungs
VO2 of the Lungs
Normally the VO2 of the lungs accounts for less than 5% of the whole-body VO2, but it can make up 20% of the whole body VO2 when there is inflammation in lungs
Measured VO2
The measurement of the whole body VO2 involves simultaneous measurements of the O2 concentration in inhaled and exhaled gas
VO2 = minute ventilation (VE) x (FIO2 - FEO2)
Measured VO2 has a reported variability of +/-5% so less than calculated VO2 but requires specialized equipment and trained personnel
Oxygen Extraction Ratio (O2ER) Equation
O2ER = VO2/DO2
VO2 - ratio of O2 uptake
DO2 - O2 delivery
O2ER = (SaO2 - SvO2)/SaO2
If the SaO2 is close to 100%, the denominator can be eliminated
O2ER = SaO2 - SvO2
Oxygen Extraction Ratio
Expresses the fractional uptake of O2 into tissues
What is the normal O2ER?
VO2 is normally about 25% of the DO2 so the normal O2ER is 0.25
Only 25% of the O2 delivered to the capillaries is taken up into the tissues when conditions are normal
Maintaining a Constant VO2
The oxygen transport system operates to maintain a constant VO2 in the face of decreases in DO2 which is accomplished by compensatory increases in the O2 extraction ratio
If the increase in O2 extraction cannot fully compensate for a decrease in DO2 then the VO2 will begin to decrease which marks the onset of oxygen-limited (anaerobic) metabolism
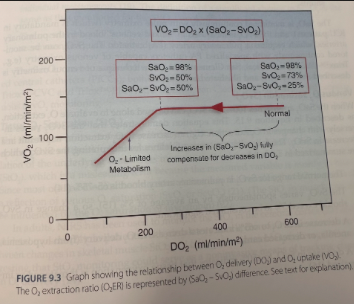
Using (SaO2-SvO2) Difference to Measure O2 Extraction
Can be used as a measure of O2 extraction as long as the SaO2 exceeds 90%
What is normal (SaO2-SvO2)?
20-30%
What does an increase in (SaO2-SvO2) above 30% indicate?
A decrease in O2 delivery (from hypoxemia, anemia, or decreased cardiac output)
What does an increase in (SaO2-SvO2) to 50% or greater indicate?
That tissue oxygenation is threatened or impaired
What does a decrease in (SaO2-SvO2) to <20% indicate?
A defect in O2 utilization in tissues, which is usually the result of sepsis
Has also been called “peripheral shunting” since it mimics the changes produced by peripheral arteriovenous shungs
How are SaO2 and SvO2 monitored?
SaO2 is monitored continuously with pulse oximetry
SvO2 is measured in “mixed venous” blood in the pulmonary arteries, which requires a pulmonary artery (PA) catheter
Venous O2 Saturation (SvO2) for Evaluating Oxygen Extraction
When SaO2 approaches 100%, the SvO2 can be used alone to evaluate O2 extraction
SvO2 varies inversely with changes in O2 extraction
An increase in O2 extraction will result in a decrease in SvO2
What is the normal range for SvO2 in pulmonary artery blood?
65-75%
What % change in SvO2 is considered significant?
SvO2 varies spontaneously by an average of 5% so a change in SvO2 should exceed 5% to be considered significant
What does a decrease in SvO2 to <65% indicate?
A decrease in O2 delivery (from hypoxemia, anemia, or decreased cardiac output)
What does a decrease in SvO2 to 50% or less indicate?
That tissue oxygenation is threatened or impaired
What does an SvO2 of 80% or higher indicate?
Impaired O2 utilization in metabolizing tissues
Usually the result of sepsis
Central Venous O2 Saturation (ScvO2)
O2 saturation in the superior vena cava
Central Venous O2 Saturation (ScvO2) for Evaluating Oxygen Extraction
Central venous O2 saturation (ScvO2) - O2 saturation in the superior vena cava
The ScVO2 is lower than the SvO2 in healthy subjects but it is higher than the SvO2 in critically ill patients. The ScvO2 is heavily influenced by the cerebral venous O2 saturation and the elevated ScvO2 in circulatory shock is attributed to peripheral vasoconstriction with relative preservation of cerebral blood flow
Despite the discrepancy between ScVO2 and SvO2, changes in ScvO2 generally mirror those in the SvO2 and trends in the ScvO2 are considered more reliable than individual measurements. The definition of a significant change in ScvO2 is the same as SVO2 (i.e. >5%)
The normal range of ScvO2 is not well defined, but a ScvO2 of 70% is one of the recommended goals of hemodynamic management in circulatory shock
ScvO2 can be monitored with central venous catheters or peripherally inserted central catheters
Tissue O2 Saturation (StO2) for Monitoring Oxygen Extraction
Near-infrared spectroscopy (NIRS) is a form of oximetry that uses an optical probe on the skin to measure the O2 saturation of hemoglobin in the microcirculation of the underlying tissue
Measurement is known as the tissue O2 saturation (StO2)
Primarily a reflection of venous O2 saturation
In patients with circulatory shock, there is a close correlation between changes in skeletal muscle StO2 and changes in systemic O2 delivery (DO2) suggesting that StO2 monitoring could serve as a noninvasive means of tracking changes in O2 delivery
One of the major limitations is the inability to define normal and abnormal levels
What is considered the most reliable marker of inadequate tissue oxygenation?
An increase in plasma lactate concentration >2 mmol/L
Lactate and Survival
Clinical studies have shown that the mortality rate in critically ill patients is directly related to the initial plasma lactate level and to the time required for the lactate level to return to normal after treatment is initiated
Contrary evidence
Tissue PO2 levels are actually increased in patients with septic shock
Cells normally operate at very low PO2 levels
An oxygen-poor environment in cells is advantageous because it limits the risk of oxidative cell injury
Lactate Clearance
Time required to normalize the plasma lactate
What are the two general pathways for glucose metabolism?
Glycolysis
Oxidative phosphorylation
Glycolysis
Located in the cytoplasm
Operates in the presence or absence of oxygen
Pivotal point with formation of pyruvate
When O2 is available, pyruvate moves into mitochondria via the enzyme pyruvate dehydrogenase
When O2 is not available, pyruvate is reduced to lactate using the enzyme lactate dehydrogenase (LDH)
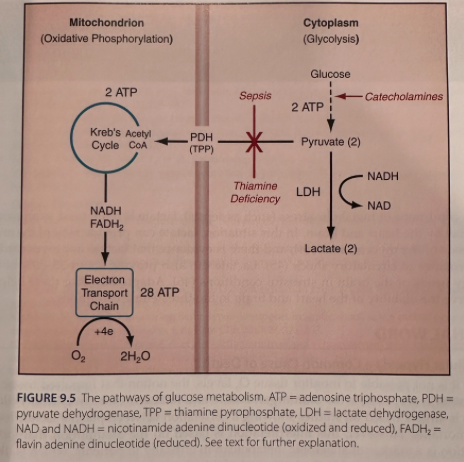
Oxidative Phosphorylation
Located in mitochondria
Produces ATP
Proceeds only in the presence of oxygen
What are the sources of hyperlactatemia in sepsis and septic shock?
Two sources of this phenomenon identified
Principal source is inhibition of pyruvate dehydrogenase (PDH) enzyme that allows pyruvate to enter mitochondria and fuel oxidative phosphorylation
Caused by bacterial products (e.g. endotoxin) and proinflammatory cytokines
Not a result of cell hypoxia
Catecholamine-driven increase in the rate of glycolysis
Hyperlactatemia with Physiologic Stress
Stressful conditions are associated with an increase in glucose uptake into cells which is attributed to the accumulation of a glucose transporter protein at the cell surface
This effect, combined with the stimulatory effect of catecholamines, results in a considerable increase in the rate of aerobic glycolysis and therefore an increase in aerobic lactate production
Lactate with Thiamine Deficiency
The PDH enzyme requires thiamine pyrophosphate (TPP) as a cofactor and deficiency of this cofactor will divert pyruvate to the production of lactate and enhance aerobic lactate production
Hyperlactatemia in Critically Ill Patients
Lactate production in critically ill patients may be predominantly aerobic in origin
Any increase in lactate concentration typically represents something other than O2 limitation; hypoxia-driven lactate accumulation is the exception rather than the rule
Lactate as Oxidative Fuel
Lactate is an alternative fuel source during periods of metabolic stress, rather than a waste product of anaerobic metabolism
The energy yield from the oxidative metabolism of lactate is equivalent to that of glucose
Lactate can serve as a source of energy when glucose availability is threatened by heightened metabolic demands
In conditions of metabolic stress (such as sepsis), lactate is often used as an oxidative fuel by the heart and brain
Lactate can provide 60% of the energy needs of the myocardium and there is evidence that lactate improves cardiac performance in circulatory shock
Lactate can also provide about 25-30% of the energy needs of the brain in stressful conditions