PSYC 336 - Clinical
1/105
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
106 Terms
Epidemiology
The prevalence and distribution of a disorder in a population.
Etiology
The cause(s) of a disorder.
Pathology
The underlying psychological/ neurobiological features of a disorder.
Transdiagnostic
factor that is part of serval diagnosis
The essentialist approach to mental disorders
Mental disorders are natural categories whose true nature can be discovered and described
Categories represent empirically verifiable similarities among and differences between people
The social constructionist approach of mental disorders
Concepts of mental disorders (of categories) are social constructions
Syndrome Heterogeneity
different causal mechanisms may relate to the same disorder, and multiple outcomes of interest can occur within one individual.
Comorbidity
the co-occurrence of two or more disorders in a single individual
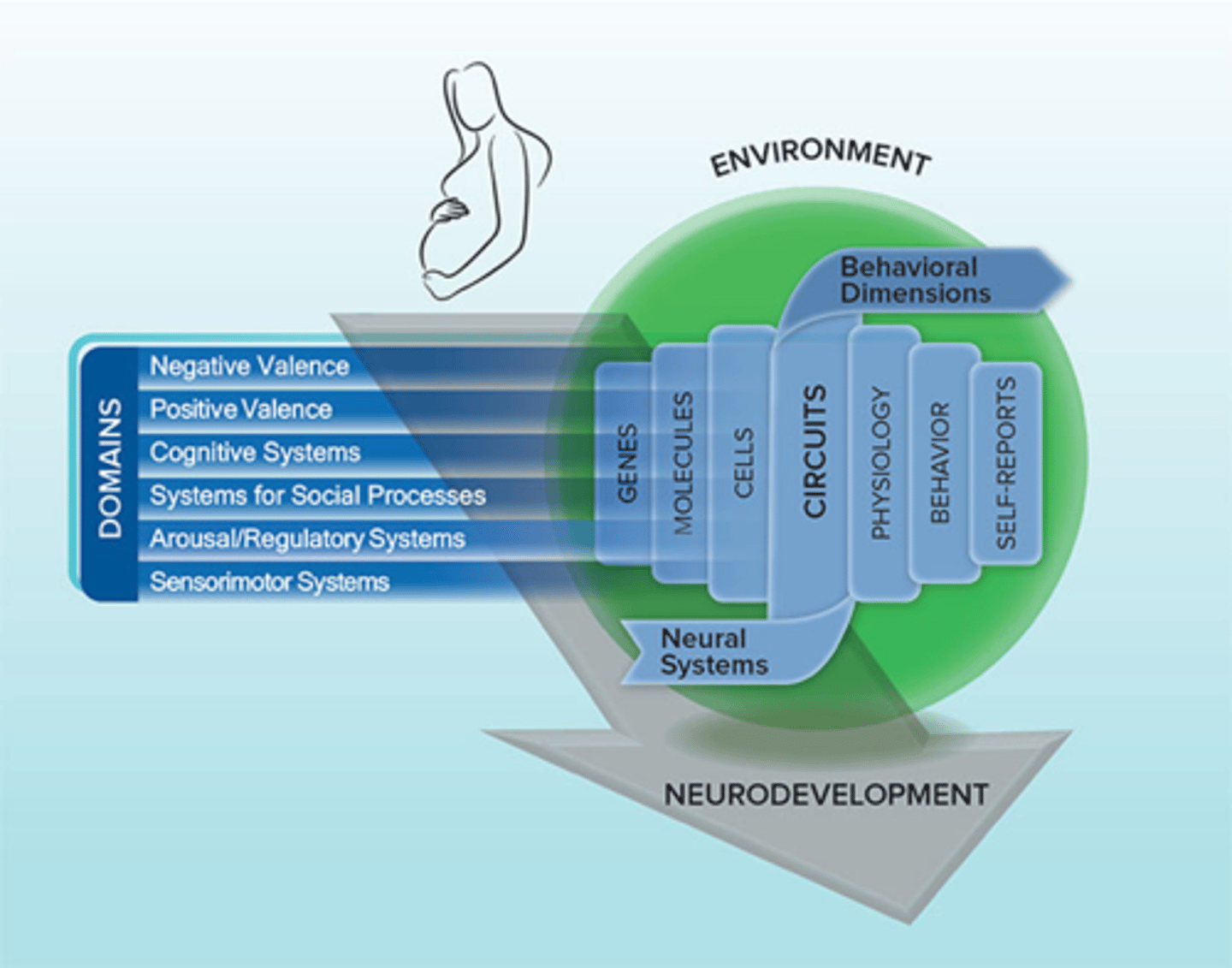
RDoC
Psychopathology research moving toward transdiagnostic domains of functioning that have a clear neurobiological/cognitive basis (bottom up)
Panic Attack
Abrupt surge of intense fear or discomfort that is diagnosed by the presence of 4 or more of the 13 symptoms
Full blown panic attack
four or more symptoms
acrophobia
two of the following symptoms
Public transportation
Open spaces
Enclosed spaces
Standing in line
Being in a crowd
Being outside of the home alone
Noncognitive panic
no symptoms of loss of control, dying or going crazy despite reporting intense fear and arousal
Nocturnal panic attack
waking from sleep in a state of panic with symptoms that are similar to panic attacks
These are common for people with panic disorder
Agoraphobia without panic disorder occurs
1/3 of the rate of panic disorder
commorbity statistics for panic disorder
93.7% of individuals with this disorder have at least one or more chronic physical or mental disorder
People with panic disorder meet the criteria for 4.5 more mental disorders
Including
behavioural features of panic disorder
1. avoidance of particular situations
2. interoceptive avoidance
3. safety behaviours
4. experiential avoidance
interoceptive avoidance
Strong sensitivity to and avoidance of internal bodily symptoms associated with anxiety and panic
Exercise, sex, caffeine, alcohol, saunas, wearing neckties, anger, scary movies
safety behaviors
Behaviors intended to avoid disaster, dysfunctional emotion regulation strategies
Check pulse
Be near hospital
Carrying antianxiety medication
Having a safe person
Experiential avoidance
Person is unwilling to remain in contact with private experiences
Watching TV, Eating
Avoiding feelings
cognitive features of panic disorder
Greater anxiety responses to panic
They fear situations that elicit body sensations like cardiovascular, respiratory and audiovestibular exercises and inductions
Emotional features of panic disorder
neuroticism is a
Interaction With Environmental Factors inducing panic disorder
- early caregiving attachment
- parenting
- abuse
- stress
biological features of panic disorder
Heritability accounts for approximately 30%-40% of the variance
the gene polymorphism 5-HTTLPR - a promoter region of the serotonin transporter gene
Neurocircuitry for panic disorder
-reduced volume of the amygdala
-low baseline GABA levels
-blunted benzodiazepine sensitivity
- HPA axis is dysregulated
Etiological Models for panic disorder: Clark and others
Catastrophic misappraisals of bodily sensations are central to the development and the maintenance of panic disorder
Etiological Models for panic disorder: Interoceptive fear conditioning
Low-level somatic sensations of arousal or anxiety become conditioned stimuli due to their association with intense fear, pain, or distress
branches of CBT for panic disorder
PCT (panic control treatment)
Clark's cognitive therapy for panic disorder
Psychological treatments for panic disorder
- CBT (PCT + Clarkes)
- ACT (for resistant patients)
- MBSR
- CART (breathing only)
Biological Treatments for Panic Disorer
- SSRI
- Benzodiazepines (reduce number of attacks)
prevention of panic disorder
CBT prevention in people who have had 1-2 attacks
Group CBT for people who have experienced attacks but no panic disorder
Diagnostic criteria for panic disorder
Both 1 and 2
1. Recurrent unexpected panic attacks + at least 4 symptoms listed
2. 1 month of concern or changes of behavior to avoid
Prevalence of panic disorder
12 month: 2.4
Lifetime: 4.7
2x more common in women
age of onset: 20s
Cognitive-Behavioral Model of Panic Disorder
- People with this Disorder pay very close attention to their bodily sensations
- misinterpret bodily sensations as signs of imminent catastrophe
the fear of fear itself
classical conditioning of panic disorder
previously neutral situations (ex: driving) become associated with panic sensations
operant conditioning of panic disorder
avoidance is maintained by negative reinforcements (relief)
Social Anxiety Disorder - diagnostic delemas
a continuum of anxiety. Hard to know where to make that 'cut'
Diagnostic criteria for social anxiety disorder
A. Marked fear or anxiety about one or more social situations in which the individual is exposed to possible scrutiny by others.
B. The individual fears that they will act in a way or show anxiety symptoms that will be negatively evaluated
C. The social situations almost always provoke fear or anxiety
D. The social situations are avoided or endured with intense fear or anxiety
E. The fear or anxiety is out of proportion to the actual threat posed by the social situation and to the sociocultural context
F. The fear, anxiety, or avoidance is persistent (6+months)
G. The fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
lifetime prevalence of social anxiety, and one year prevalence
L: 8-13 %
Y: 6.7%
social anxiety disorder onset and sex ratio
- childhood and early adolescence
- 2x in women
people with psychological vulnerability's to developing social anxiety disorder display
Behavioral inhibition: An early childhood temperament factor that involves fear of novelty. Related to shyness and social reticence in preschool and elementary school years
STRONGEST RISK FACTOR
OCD defenition
the presence of obsessions or compulsions that produce significant distress and cause noticeable interference with various aspects of functioning
obsessions
intrusive thoughts, ideas, images, impulses, or doubts that a person experiences as senseless and that evoke anxiety
RESISTED, meaning they are accompanied by the sense that they need to be dealt with or neutralized or even avoided
categories of obsessions
Contamination
Guilt and responsibility of harm
Uncertainty
Taboo thoughts about sex
Violence and blasphemy
Need for order and symmetry
Compulsions
Urges to preform overt, or mental rituals in response to obsessions to reduce anxiety and distress
Categories of compulsions
Decontamination
Checking
Ordering and arranging
Mental rituals
the insight factor of OCD
the degree to which the person views their obsessional fears and compulsive behavior as reasonable
can be:
- good
- poor
- absent
tic OCD
OCD when patient has a history of Tourette's syndrome
Interpersonal Aspects of OCD
Negative impact on the sufferer's relationships
High relationship conflict
Worse if friends or partners or family engage in
Symptom accommodation
Body Dismorphic Disorder
Intrusive, distressing thoughts concerning one's appearance
Repeated checking
OCPD
Personality traits like perfectionism, inflexibility, need for control
Negatively impacts interpersonal relationships, occupational functioning, and other domains of a persons life
Ego-syntonic
Commodity with OCD and OCPD
23-32% OCD display OCPD symptoms
OCPD may be associated with poor OCD treatment
Prevalence and Epidemiology of OCD
Lifetime prevalence: 0.7-2.9%
Slightly more in females
Typical onset is 25
Men: 21
Females: 22-24
Learning Model of OCD
Mowrers 1960 two stage theory
- Fear acquisition
- Maintenance
Operant conditioning creating avoidance habits, maintaining the fear and OCD
Cognitive Deficit Models of OCD - Reality monitoring
The ability to discriminate between memories to actual versus imagined events
Cognitive Deficit Models of OCD - Inhibitory Deficits
Cognitive inhibition - the ability to dismiss extraneous mental stimuli
People with OCD have difficulty forgetting negative material
Limitations of cognitive deficit models
Don't account for heterogeneity of OCD
Some wash hands, some have metal compulsions
Cognitive Behavioural Models of OCD
The most promising
Emotional disturbance is brought not by situations and stimuli themselves, but how one make sense of the situations and stimuli
Limitations of the Cognitive Behavioural Models of OCD
implies that successful treatment for OCD must accomplish two things
1. Correction of maladaptive beliefs and appraisals that lead to obsessional fear
2. The termination of avoidance and compulsive rituals
seretonin hypothesis of OCD
Hypersensitivity of the postsynaptic serotonergic receptors
Neurobiological structural models of OCD
- Abnormalities in the orbitofrontal subcortical circuits
- Overactivity in the processing information in the initiation of behavioral process areas of the brain
- Increased glucose utilization in the orbitofrontal cortex
Psychological treatment of OCD
CBT is derived from the cognitive behavioral model
Considered the most effective approach to the psychological treatment of OCD
Two types of CBT
ERP
CT
exposure and response prevention
Entails confrontation with stimuli that provoke obsessional fear, but that objectively pose a low risk of harm
Habituation
Overtime the anxiety associated with physiological responding subsides
delivery of ERP
A few hours of assessment and treatment planning
Assessment of obsessions, compulsive rituals, avoidance strategies and anticipated consequences of confronting feared situations
15 hours of treatment sessions, about 90 minutes each
key requirements for ERP success
Physiological arousal and subjective fear must be evoked
Fear responses must gradually diminish during exposure
Initial fear response at the beginning of each exposure session
should decline across sessions
efficiency of ERP
Improvement rates 50-70%
Cognitive Therapy + Delivery
Targets faulty beliefs that lead to obsessive fear
Rationale for treatment
Socialized to the cognitive behavioral framework for understanding OCD
Biological Treatment for OCD
SSRI
20-40% reduction in obsessions and compulsions
Neurosurgical treatment (not favourable)
Panic Disorder and transdiognostic
Panic occurs in many situations ex: SAD
highly transdiognostic
Motivational Enhancement theory
a therapy designed to quickly produce internally motivated change, helps to develop internal motivation to change
Environmental Moderators of social anxiety
Parental anxiety: Can be a diathesis and/or stress
Insecure attachment: high parental rejection, low parental warmth
Stressful social experiences: Rejection, Victimization
in vivo exposure
Gradual exposure to feared situations in order to extinguish fear
Examples for panic disorder in vivo exposure:
Driving
Public Transporation
Bridges
Waiting in lines
Nomothetic
on average what happens in certain treatments and how they work
Idiographic
what is going to work for that particular person
dysfunctional beliefs of OCD
inflated responsibility, overestimation of threat, exaggeration of the importance of thoughts, need to control thoughts, perfectionism, uncertainty
Experiment to prove sub-threshold Psychopathology
2000 female twin pairs with symptoms of depression
Tested:
Risk of depression recurrence over 5 years
Risk of depression in co-twin over 5 years
Conclusion:
DSM diagnostic criteria are not reflective of natural discontinuity in depressive symptoms as experienced in the general population
Line separating no diagnosis from diagnosis is arbitrary - a convection not a fact
Traumatic stressors stats
quite common with a lifetime prevalence of trauma being 60.7% for men and 51.2% for women
strong predictors of unhealthy trauma recovery
- Severity of event
- Lack of social support
- Ongoing post-event stress
PTSD DSM-5 Criteria
A. exposure
- direct, eyewitness, learning, repeated
B. Intrusion
C. Avoidance
D. Negative cognition and mood
E. Hyperarousal
F. 1 month or more
G. distress impairment
H. Not another disorder
Acute Stress Disorder (ASD)
occurs within a month after exposure to traumatic stress
PTSD diagnostic specifier add ons
Presence of depersonalization
Presence of Derealization
Genetic factors of PTSD
1/3 of the variance in PTSD may be attributed to genetic factors
most studied candidate gene is 5-HTTLPR polymorphism
FK506-binding protein 5 is a marker of the HPA axis
Neaurobiological changes with PTSD
Decreased mPFC activation and increased amygdala activation
hippocampus changes
Classical conditioning model of PTSD
The experience of danger or perceived danger is the unconditioned stimuli (US) which then leads to the development of learned danger signals (the conditioned stimuli CS)
criticism of Classical conditioning model of PTSD
If a traumatic or stressful life event is conceptualized as a central etiologic event, then exposure should almost inevitably lead to disorder - which it does not
Impaired fear extinction hypothesis
People with PTSD have impairments in learning new inhibitory associations to trauma-related reminders
Dual representation of memory in PTSD
Provides an account of intrusive memories that makes explicit links to underlying neural processes
Contextual representations (C-reps)
Sensory representations (S-reps)
Contextual representations (C-reps)
Flexible representations that are consciously accessible, context-dependent, and connected to the inferior temporal cortex, hippocampus and Para-hippocampus brains structures
PTSD memory
Sensory representations (S-reps)
Inflexible, involuntary, sensation bound, disintegrated from the autobiographical memory base and are connected to the superior partial areas, amygdala, insula areas of the brain
Memories of the trauma are over represented in S-reps
Cognitive models of PTSD
-maladpative appraisals or interpretations of traumatic event, response and environment are pivotal in perpetuating sense of threat
Emotional models of PTSD
Emphasize the processing of the emotional experience of trauma exposure
A psychodynamic processing model in which PTSD symptoms are the result of an inability to intergrade the traumatic event into existing cognitive schemas
prolonged grief disorder
Prevent the individual from fully processing and accepting the loss of a loved one
Stress disorder
exposure based interventions for trauma
Help reduce trauma related distress by facilitating new learning about the meaning of the trauma and altering maladaptive beliefs about oneself, others, and the world
Prolonged exposure
In vivo exercise
Imagined exposure
ex:
EMDR
NET
Cognitive treatments for trauma
Changes in the person's understanding of the trauma and its meaning in their life
Update the trauma memory
Discussion of key themes:
Challenges to safety
Trust
Power
Self esteem
pre trauma
characteristics of the individual and environment that preceded trauma exposure
-Lower socio-economic status
-Lower intelligence
-Childhood trauma
-Prior adult or child trauma
-Prior worse adjustment
peri-trauma
Characteristics of the trauma and the environmental and individual response to the trauma
Things about the trauma that makes them likely to develop
- Trauma severity
- Perceived life threat
- Peri-traumatic emotions
post-trauma
Individual and environmental factors that occur after the trauma
Things that happened after event that makes them more likely to develop
- Ongoing life stress
- Lack of social support
- Negative cognitions
resilience factors to trauma development
Spirituality
Connections to family
Close bonds with others as a result of shared history, experiences, and culture