Adaptive Immunity
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
20 Terms
What is the difference between innate and adaptive (acquired) immunity?
Innate Immunity:
Nature: Nonspecific; responds the same way to all pathogens.
Speed: Rapid response, dominant in the first 12 hours after exposure.
Components: Includes antimicrobial proteins and certain cells present in the bloodstream.
Memory: Lacks immunological memory; responds the same way upon repeated exposure.
Adaptive Immunity:
Nature: Specific; targets unique markers called antigens.
Speed: Slower response, taking 3–5 days to become dominant.
Components: Involves two arms: cell-mediated immunity (T cells) and antibody-mediated immunity (B cells and antibodies).
Memory: Has immunological memory, allowing quicker and more efficient responses upon subsequent exposures.
Both systems work together, with innate immunity providing immediate defense and adaptive immunity offering targeted and long-lasting protection.
What are the two "arms" of the adaptive immune response? What type(s) of lymphocyte cell is involved in each?
Cell-Mediated Immunity:
Lymphocyte Involved: T cells
Function: This arm is primarily responsible for targeting and destroying infected or cancerous cells. T cells recognize specific antigens presented by infected cells and help orchestrate the immune response.
Antibody-Mediated Immunity (Humoral Immunity):
Lymphocyte Involved: B cells
Function: B cells produce antibodies that circulate in the bloodstream and bind to specific antigens. This helps neutralize pathogens or mark them for destruction by other immune cells.
Each arm of the adaptive immune system plays a crucial role in identifying and responding to specific antigens, providing a targeted and efficient immune response. This specificity and the ability to remember past infections are key features of adaptive immunity.
Where in the body are lymphocytes first made? Where do different types of lymphocytes mature?
Lymphocytes are first made in the bone marrow through a process called leukopoiesis
B Lymphocytes (B cells): These cells mature in the bone marrow. You can remember this by associating "B" with "bone marrow."
T Lymphocytes (T cells): These cells migrate to the thymus gland, located in the mediastinum, to complete their maturation. The "T" in T cells stands for "thymus.”
How does the body ensure that is doesn't have lymphocytes flowing around that will recognize its own cells?
Central Tolerance: During maturation, lymphocytes that strongly recognize self-antigens are typically eliminated through a process called negative selection.
Peripheral Tolerance: Some self-reactive lymphocytes may escape central tolerance. In the peripheral tissues, additional mechanisms, such as regulatory T cells and anergy (a state of inactivity), help prevent these cells from causing autoimmunity
What is an antigen? Where are they typically found? Are antibodies the only things that can recognize antigens?
An antigen is a substance that can be recognized by B or T cells, triggering an immune response.Antigens are typically peptides but can also include carbohydrates, lipids, and metals like nickel.
Exogenous antigens are taken into cells by phagocytosis, while endogenous antigens can be foreign or self, such as those encoded by your DNA.
T cells also play a crucial role. T cells recognize antigens presented by major histocompatibility complex (MHC) molecules on cell surfaces. This recognition is essential for the immune response, as T cells cannot directly interact with free antigens.
What is the difference between an endogenous antigen and an exogenous antigen? Which type is presented by MHC Class I molecules and which by MHC Class II molecules?
Endogenous Antigens: These are antigens that originate from within a cell. They can be self-antigens or foreign antigens, such as those from viruses or intracellular bacteria that have infected the cell. Endogenous antigens are typically presented by Class I MHC molecules, which are found on nearly all nucleated cells. This presentation is crucial for the activation of cytotoxic T (TC) cells, which can then target and destroy infected or cancerous cells.
Exogenous Antigens: These antigens come from outside the cell. They include components from bacteria, viruses, or other pathogens that are ingested by antigen-presenting cells (APCs) like dendritic cells, macrophages, and B lymphocytes. Exogenous antigens are presented by Class II MHC molecules, which are found on the surfaces of APCs. This presentation is important for the activation of helper T (TH) cells, which then stimulate other immune responses.
Which type of cell presents antigen on an MHC Class I molecule and which on an MHC Class II molecule? Why is this important to a proper immune response?
MHC Class I Molecules: These are found on nearly all nucleated cells and present endogenous antigens. This means they display antigens that originate from within the cell, such as viral proteins or abnormal proteins from cancer cells.
MHC Class II Molecules: These are found on antigen-presenting cells (APCs) like dendritic cells, macrophages, and B lymphocytes. They present exogenous antigens, which are derived from pathogens or particles that the cell has ingested.
Class I molecules help the immune system identify and eliminate cells that are infected or cancerous, while Class II molecules help orchestrate a broader immune response to external threats. This dual system ensures that the body can effectively respond to a wide range of pathogens and abnormal cells.
What is another name for a helper T lymphocyte cell? What about a cytotoxic T lymphocyte cell?
A helper T lymphocyte cell is also known as a CD4 cell.These cells play a crucial role in the immune system by helping to activate other immune cells, such as B cells and cytotoxic T cells, through the release of cytokines.
a cytotoxic T lymphocyte cell is referred to as a CD8 cell. These cells are primarily responsible for directly attacking and destroying infected or cancerous cells by recognizing antigens presented on MHC Class I molecules.
Do helper T lymphocyte cells recognize antigens presented on MHC Class I or Class II molecules? What about cytotoxic T lymphocyte cells?
Helper T lymphocyte cells, also known as TH cells, recognize antigens presented on MHC Class II molecules.
Cytotoxic T lymphocyte cells, or TC cells, recognize antigens presented on MHC Class I molecules.
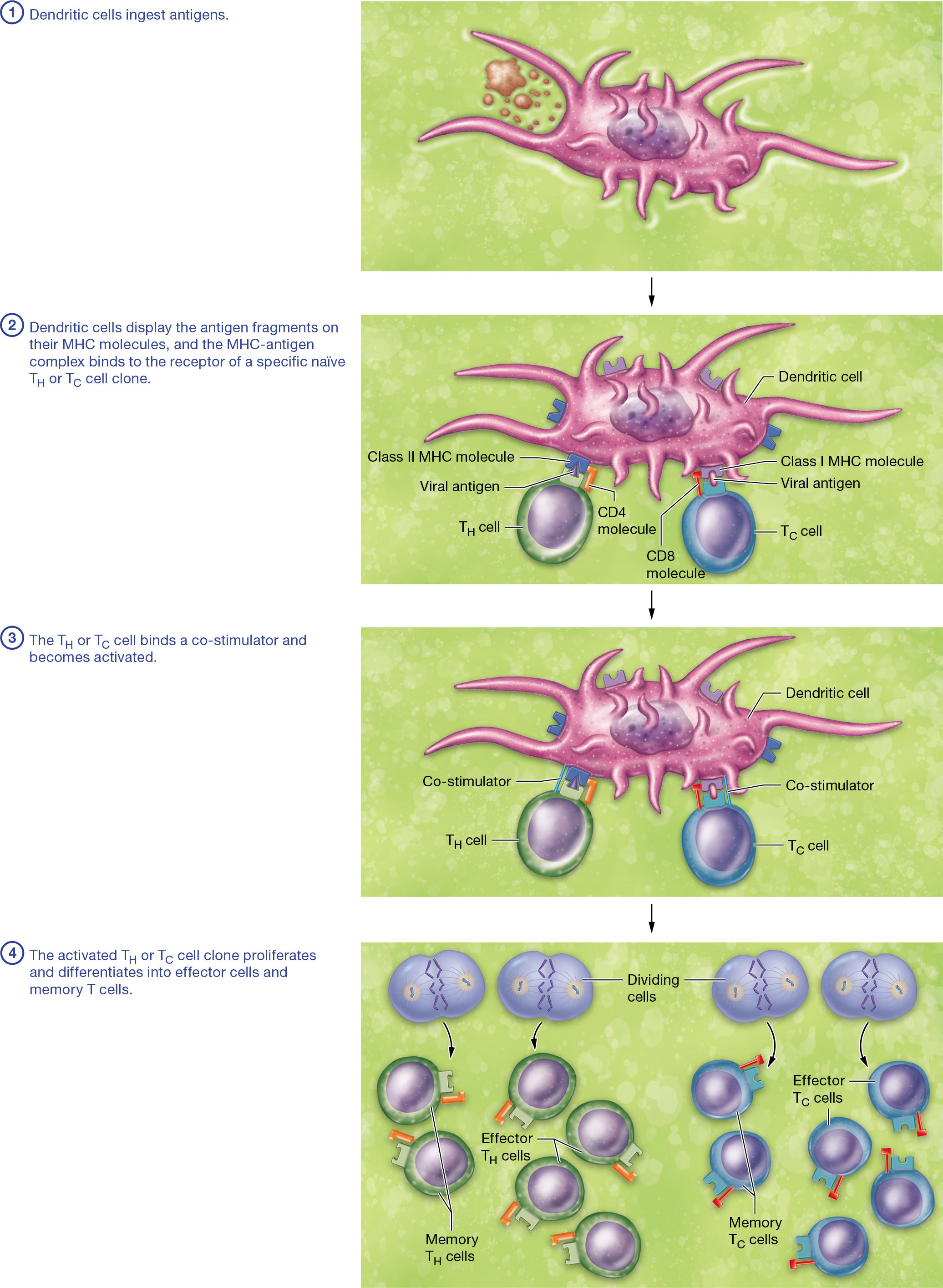
How are T lymphocytes activated? In the context of immunology, what is a "clone"?
T Lymphocyte Activation
Antigen Presentation: Dendritic cells ingest antigens and display fragments on their MHC molecules. These MHC-antigen complexes bind to specific T cell receptors on naïve T helper (TH) or cytotoxic T (TC) cell clones.
Clonal Selection: The binding of the T cell receptor to the MHC-antigen complex triggers T cell activation. This process is called clonal selection because the antigen selects a specific T cell clone.
Co-stimulation: For full activation, T cells require binding to co-stimulators on the dendritic cell. This ensures that T cells are only activated when necessary.
Proliferation and Differentiation: Activated T cells proliferate and differentiate into effector cells, which perform immediate immune responses, and memory T cells, which provide long-term immunity.
Clonal Concept in Immunology
In immunology, a "clone" refers to a group of cells derived from a single progenitor cell, all having the same antigen specificity. This concept is crucial for understanding how the immune system targets specific pathogens.
What actions do activated helper T lymphocytes perform? What about activated cytotoxic T lymphocytes?
Activated Helper T Lymphocytes (TH Cells)
Activated TH cells primarily function by secreting cytokines, which are signaling molecules that enhance the immune response. Here are some key actions they perform:
Secretion of Cytokines: TH cells release various interleukins, such as Interleukin-2 and Interleukin-3, which have different roles in the immune response.
Interleukin-3: Stimulates macrophages, enhancing their phagocytic activity and triggering them to produce Interleukin-12, which further stimulates TH cells.
Interleukin-2: Activates and promotes the proliferation of cytotoxic T (TC) cells.
Various Interleukins: Stimulate B cell proliferation and antibody production.
Activated Cytotoxic T Lymphocytes (TC Cells)
Activated TC cells have a direct role in destroying infected or abnormal cells:
Destruction of Infected Cells: TC cells recognize and bind to infected cells presenting antigens on MHC class I molecules and induce apoptosis, effectively killing the infected cells.
How are B cells activated? Which cells produce antibodies?
B cells are activated through a multi-step process involving antigen binding and interaction with T-helper (TH) cells. Here's a simplified breakdown:
Antigen Binding: B cells have specific receptors that bind to antigens. This binding is the first step in B cell activation.
Antigen Presentation: The B cell processes the bound antigen and presents it on its surface using class II MHC molecules.
TH Cell Interaction: A TH cell recognizes the antigen-MHC complex on the B cell and binds to it. This interaction is crucial as the TH cell secretes cytokines that fully activate the B cell.
Differentiation: Once activated, B cells differentiate into plasma cells and memory B cells. Plasma cells are the ones that produce and secrete antibodies, which are crucial for neutralizing pathogens.
What is the difference between an effector cell and a memory cell? How do memory cells give the human body an advantage upon secondary exposure to a pathogen?
Effector cells are responsible for the immediate response to an antigen. They actively engage in eliminating pathogens by performing functions such as releasing cytokines or directly killing infected cells.
Memory cells, on the other hand, are long-lived and remain in the body after the initial infection has been cleared. They provide the immune system with a "memory" of the pathogen. Upon secondary exposure to the same pathogen, memory cells enable a faster and more efficient immune response. This is because they can quickly recognize the antigen and do not require a co-stimulator for activation, unlike naïve T cells.
What are some differences between a primary and a secondary immune response? Is a "primary" immune response the same thing as "innate" immunity?
The primary and secondary immune responses are both part of the adaptive immune system
Primary Immune Response: This occurs when your body is first exposed to an antigen. It has a longer lag phase (4-5 days) as B cells proliferate and differentiate. The primary antibody produced is IgM, and the response peaks in 7-14 days. This response is slower and less robust, which is why you often feel sick during this time.
Secondary Immune Response: This happens upon subsequent exposure to the same antigen. It has a shorter lag phase (1-3 days), and antibody levels peak faster (3-5 days) and are much higher. The main antibody is IgG, which binds more effectively to antigens. This response is quicker and more efficient, often preventing illness.
What is the difference between "active" and "passive" immunity? What types of stimuli can provide each?
Active and passive immunity are two types of antibody-mediated immunity
Active Immunity:
Mechanism: Your body's immune system actively responds to an antigen.
Stimuli:
Naturally Acquired: Through exposure to an antigen via infection.
Artificially Acquired: Through vaccination.
Outcome: Production of memory cells and antibodies, providing long-lasting protection, potentially for years or a lifetime.
Passive Immunity:
Mechanism: You receive preformed antibodies from an external source.
Stimuli:
Naturally Acquired: Through passage from mother to fetus and in breast milk.
Artificially Acquired: Through injection of antibodies, such as antitoxins.
Outcome: No memory cells are formed, and protection is temporary, lasting only a few months.
How do vaccines reduce the probability that an individual will have serious complications upon exposure to a harmful pathogen?
by priming your immune system to respond more effectively. When you receive a vaccine, it introduces an antigen that triggers a primary immune response, leading to the production of memory cells. These memory cells "remember" the pathogen, so if you're exposed to it again, your body can mount a faster and stronger secondary immune response.
This secondary response is characterized by a rapid increase in IgG antibodies, which are more effective at neutralizing the pathogen. As a result, symptoms are minimized, and the risk of severe complications is significantly reduced.
What is an antibody? What are the major classes of antibodies?
Antibodies, also known as immunoglobulins, are Y-shaped proteins produced by B cells that play a crucial role in the immune response by recognizing and binding to specific antigens. Each antibody consists of four peptide chains: two heavy and two light chains, with variable regions responsible for antigen binding.
Major Classes of Antibodies:
IgG: The most abundant antibody in serum, capable of crossing the placenta to provide immunity to the fetus. It functions in opsonization, neutralization, and complement fixation.
IgA: Found in secretions like saliva and breast milk, IgA is a dimer that plays a role in agglutination and neutralization.
IgM: The largest antibody, a pentamer, is the first to respond to an antigen. It is effective in agglutination and complement fixation.
IgE: Involved in allergic responses, IgE binds to mast cells and basophils, triggering inflammation.
IgD: Found on B cell surfaces, IgD is involved in B cell activation.
In what ways do antibodies protect against pathogenic infection? What is the difference between neutralization and opsonization?
Neutralization: Antibodies bind to specific components of toxins, viruses, or bacteria, preventing them from interacting with and harming host cells. This effectively neutralizes the pathogen's ability to cause damage.
Opsonization: Antibodies, particularly IgG, coat pathogens, making them more recognizable and easier for phagocytes to engulf and destroy. This enhances phagocytosis.
Agglutination and Precipitation: Antibodies can bind to multiple antigens, causing them to clump together. This makes it easier for phagocytes to ingest these complexes.
Complement Activation: Antibodies activate complement proteins, leading to the formation of a membrane attack complex that can lyse pathogens.
Stimulation of Inflammation: Antibodies like IgE trigger the release of inflammatory mediators, enhancing the immune response.
Difference between Neutralization and Opsonization:
Neutralization involves antibodies binding to pathogens or toxins to block their harmful effects.
Opsonization involves antibodies coating pathogens to enhance their uptake and destruction by phagocytes.
What is a Type I "hypersensitive" immunological response? Which class of antibodies facilitate this response?
A Type I hypersensitive immunological response is commonly referred to as an allergic reaction
This type of hypersensitivity occurs when your immune system overreacts to a harmless substance, known as an allergen, such as pollen, dust mites, or pet dander.During the first exposure to an allergen, your immune system produces a specific class of antibodies called Immunoglobulin E (IgE). These IgE antibodies bind to mast cells and basophils, sensitizing them. Upon subsequent exposure to the same allergen, these sensitized cells release inflammatory mediators, leading to the symptoms associated with allergies, such as itching, swelling, and mucus production.
IgE is the key antibody class that facilitates this response
How are immunodeficiency and autoimmunity different? How can the HIV lead to immunodeficiency?
Immunodeficiency occurs when one or more components of the immune system are not functioning properly, leading to an increased susceptibility to infections. This can be primary (genetic or developmental) or secondary (acquired through infections like HIV, trauma, cancer, or medications).
Autoimmunity, on the other hand, happens when the immune system mistakenly attacks the body's own cells, recognizing them as foreign. This is due to self-reactive T and B cells and the production of autoantibodies.
HIV leads to immunodeficiency by targeting and destroying CD4⁺ T helper cells, which are crucial for coordinating the immune response. HIV binds to CD4 molecules on these cells, enters them, and uses reverse transcriptase to integrate its RNA into the host DNA. This process eventually leads to the destruction of these cells, weakening the immune system and resulting in acquired immunodeficiency syndrome (AIDS).