11.3 kidney regulation
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
36 Terms
kidney functions
to conserve nutrients and water, to balance salts, concentrate wastes for excretion
control osmolarity: mainly by adjusting water loss
control total fluid volume: mainly by adjusting Na+ loss
control pH, mainly by adjusting bicarbonate loss or gain
involved w blood pressure and blood volume control
makes renin (is an enzyme, a protease, also called angiotensinogenase)
RAAS
water reabsorption in the kidney can be regulated by
antidiuertic hormone (ADH)
ADH (what does it do + what stimulates it?)
released from pituitary when osmoreceptors in the hypothalamus detect an increase in osmolarity of body fluids
angiotensin (peptide hormone) also stimulates secretion of ADH
increases water reabsorption, stimulates thirst
thirst
too little water in the blood, detected by the hypothalamus
more ADH produced by the pituitary gland
more water reabsorbed by the kidneys, caused by ADH
blood becomes less concentrated
negative feedback: hypothalamus detects change in blood concentration. pituitary produces less ADH. blood returns to correct osmotic concentration
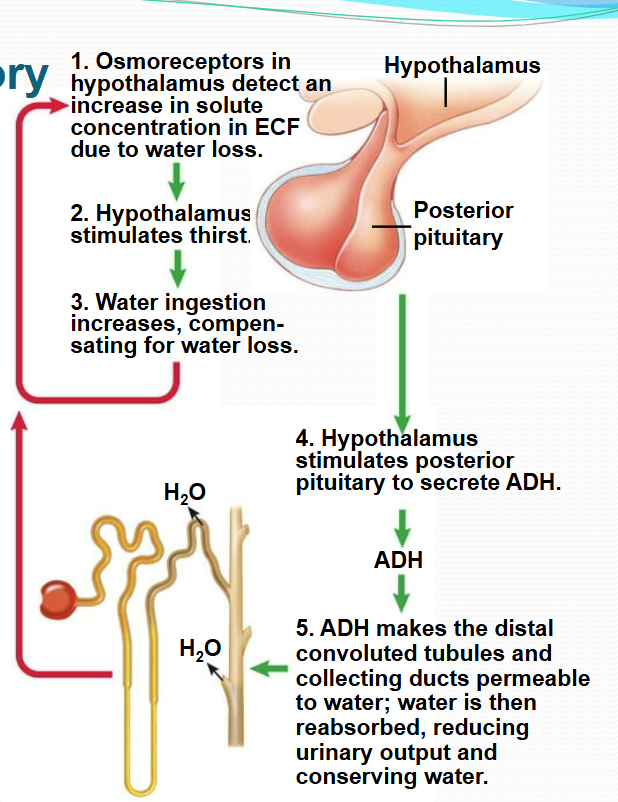
ADH regulatory system steps
sensors of blood pressure + parasympathetic and sympathetic activation
baroreceptors in aorta and carotids detect “stretch”, send signals to medulla oblongata (brainstem)
to decrease blood pressure: activation of the parasympathetic nervous system and inhibition of the sympathetic nervous system
parasympathetic activation leads to a decreased cardiac output via decrease in heart rate, resulting in a tendency to decrease blood pressure
sympathetic: increased contractility of the heart, heart rate, and arterial vasoconstriction, which tends to increase blood pressure
intra-renal baroreceptors = __ → __, an enzyme, leads to an __ in blood pressure
juxtaglomerular cells, renin, increase
__ → __ (__, is a protein hormone, inhibits the effects of __ and leads to blood pressure __)
atria, ANP, atrial natriuretic factor (ANF), renin, decrease
ANP promotes __ + define __
natriuresis: loss of sodium, is the process of excretion of sodium in the urine via action of the kidneys
total Na+ → total __ → __
fluid volume, blood pressure
atrial natriuretic peptide (ANP)
promotes natriuresis (loss of sodium)
atrial myocytes synthesize, store and release ANP in response to stretch (indicated by high blood volume)
a major effect of ANP is renal vasodilation → increase blood flow = increased glomerular filtration rate (GFR), more filtrate is processed, more urine (w Na+ and water) is released
more Na+ excreted (natriuresis). water follows salt. drop blood volume. lower blood pressure
autoregulation system for blood pressure
involves interactions btwn the glomerulus and nephron
filtration rate is kept constant during small variations in blood pressure
juxtaglomerular apparatus: located in region where distal convoluted tubule contacts the afferent arteriole which carries blood to the glomerulus
end result: signals from the JG cells act to constrict or dilate afferent arterioles which keep the blood flow and filtration constant during small variations in blood pressure under normal circumstances
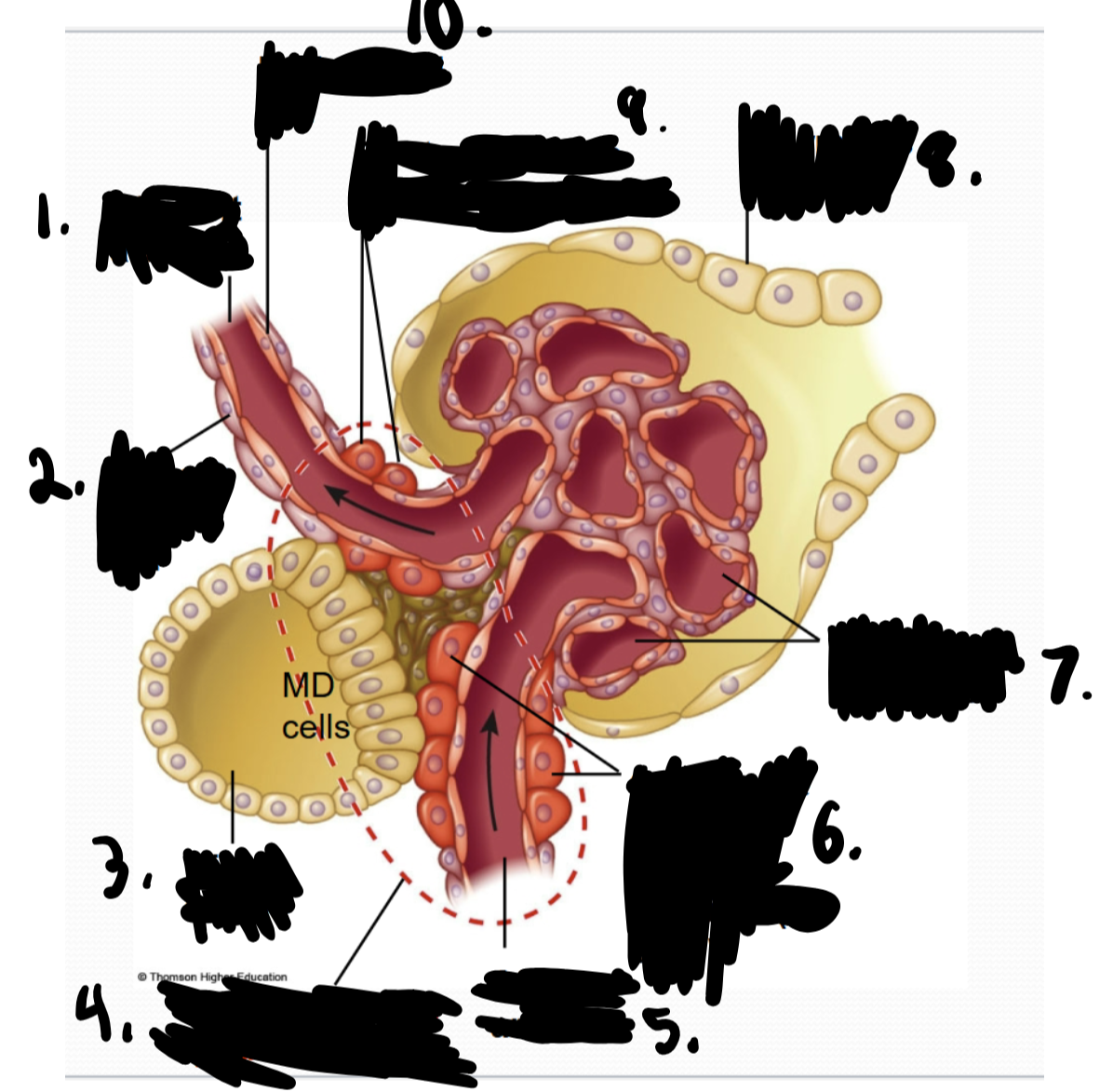
efferent arteriole, smooth muscle cell, distal tubule, juxtaglomerular apparatus (JGA), afferent arteriole, contractile cells of afferent arteriole (JG cells), glomerular capillaries, Bowman’s capsule, contractile cells of efferent arteriole, endothelial cell
blood pressure changes
changes in blood volume/pressure occur when the body loses or gains Na+
Na+ loss reduces the osmolarity of the body fluids → so less water is reabsorbed in the kidneys
less water → less blood volume → blood pressure drops
excessive intake of salty food has opposite effect
hyponatremia + causes
low levels of sodium in the blood, causes: severe vomiting or diarrhea taking certain meds, including antidepressants and pain medications, kidney disease
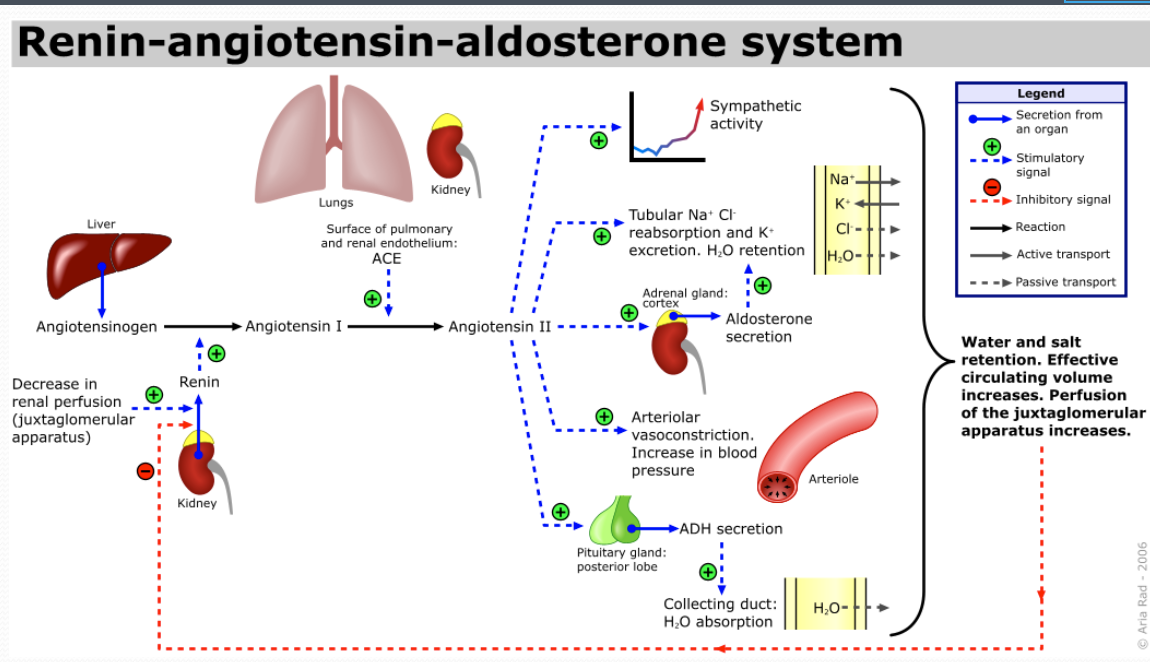
renin-angiotensin-aldosterone system (RAAS)
when blood volume and blood pressure drop, constituents of RAAS act to raise blood pressure
renin (enzyme, released from JGA) triggers angiotensin production by converting angiotensinogen to angiotensin I which is converted to angiotensin II)
angiotensin → angiotensin II stimulates arteriole constriction, ADH (increases water reabsorption), and aldosterone (hormone from adrenal gland)
aldosterone increases Na+ reabsorption in the kidneys, raising the osmolarity of body fluids → water to be reabsorbed from the kidney tubule back to the body fluids
ANF __ the effects of renin
inhibits
juxtaglomerular apparatus (JGA)
the site of blood pressure regulation via the renin-angiotensin-aldosterone system (RAAS) in the kidney
located at the side of the glomerulus
is formed by the conjunction of cells of (1) the macula densa (distal tubule), (2) juxtaglomerular (JG) cells of the afferent arteriole, and (3) some others (extraglomerular mesangial cells)
macula densa
macula densa cells monitor the Na+ concentration in the filtrate and regulate via paracrine signals the release of renin by the adjacent juxtaglomerular cells
low Na+ macula densa cells signal JG cells to make renin
juxtaglomerular cells (JG)
specialized smooth muscle cells in the wall of the afferent arteriole which synthesize and secrete renin
juxtaglomerular cells secrete __ in response to a drop in __ by __ in the __, or when stimulated by __
renin, pressure, stretch receptors (baroreceptors), vascular walls, macula densa cells (osmoreceptors)
angiotensin I is converted to angiotensin II by
ACE (angiotensin converting enzyme)
notes on backside
increase in sympathetic activity results in increase in rate and force of contraction and constriction of blood vessels, which help to increase blood pressure
aldosterone also stimulates the secretion of K+ into the tubular lumen
another way of knowing the RAAS
low blood volume (intra-renal baroreceptors: JG cells) or low Na+ (macula densa cells) → the kidneys secrete renin
renin stimulates the production of angiotensin I. (renin is protease that cleaves plasma angiotensinogen into angiotensin I)
angiotensin I → angiotensin II → blood vessels to constrict → increased blood pressure
angiotensin II stimulates the secretion of aldosterone from the adrenal cortex
aldosterone → increase the reabsorption of sodium and water in kidney
this increases the volume of fluid in the body (which also increases blood pressure)
renin, angiotensin, and aldosterone are all produced when blood pressure is
too low
the actions of ANP are the opposite of what renin would trigger:
inhibits the reabsorption of Na+ directly (on the nephron)
inhibits the release of aldosterone, which has the same ultimate effect: no Na+ absorption
atrial natriuretic peptide (ANP) and the arterioles
causes dilation of the afferent arteriole that leads to the kidney nephron while constricting the efferent arteriole
if it dilates the afferent arteriole, it increases the rate of blood flow into the glomerulus
if it constricts the efferent arteriole, it decreases the rate of blood flow out of the glomerulus via the efferent arteriole
this increases the GFR (glomerular filtration rate), which increase the production of urine bc if the fluid is flowing in faster, you produce more urine and effectively decrease the reabsorption of Na+ and water
low blood pressure response summary (in that you want to bring the blood pressure up)
the juxtaglomerular apparatus and baroreceptors will respond directly to low blood pressure
renin is released → more aldosterone
reabsorption of Na+ increases and water will follow passively → an increase in fluid volume and an increase in cardiac output, resulting in an increase in blood pressure
at the same time, the increase in sympathetic activity that occurs due to low blood pressure will tend to constrict the blood vessels
angiotensin will also tend to constrict the blood vessels
blood vessel constriction will raise the total peripheral resistance (TPR)
raising the TPR and increasing the cardiac output will increase the blood pressure from low lvls back to normal lvls
high blood pressure response summary in which you want to bring blood pressure down
decrease your renin → less aldosterone: results in the decreased reabsorption of salt (so more salt in the kidney tubules, more water in the kidney tubules, more urine produced, less body fluid volume, lower blood pressure)
less renin, less angiotensin, and less sympathetic output: will cause blood vessels to dilate which will result in a decrease in total peripheral resistance (TPR)
increase ANP, increases the glomerular filtration rate (GFR) which also decreases the reabsorption of salt and water
results in a decrease in the plasma fluid volume, which amounts to a decrease in cardiac output. this will lower the blood pressure back to normal in situations when the blood pressure is too high
considering what angiotensin II does, when would a doctor give ACE an inhibitor?
when blood pressure is high
renal acid base regulation - proximal tubule: __ in the proximal tubule transport Na+ from the filtrate into proximal tubule cells and transport __ from the proximal tubule cells into the filtrate. this secreted __ combines w __, producing carbonic acid (H2CO3). the enzyme, __, is located in the __ of the proximal tubule cell. it converts __ to __ and __ which enter the cytoplasm of the proximal tubule cell, where __ is also present. here, __ catalyzes the reaction btwn __ and __ to form __, which dissociates to form __ and __. this bicarbonate can then diffuse through the __ and enter the blood. hence, there is little H+ in the filtrate at this location
renal acid base regulation - proximal tubule: Na+/H+ pumps in the proximal tubule transport Na+ from the filtrate into proximal tubule cells and transport H+ from the proximal tubule cells into the filtrate. this secreted H+ combines w bicarbonate (HCO3-), producing carbonic acid (H2CO3). the enzyme, carbonic anhydrase (CA), is located in the apical cell membrane of the proximal tubule cell. it converts H2CO3 to H2O and CO2 which enter the cytoplasm of the proximal tubule cell, where CA is also present. here, CA catalyzes the reaction btwn H2O and CO2 to form carbonic acid, H2CO3, which dissociates to form HCO3- and H+. this bicarbonate can then diffuse through the basolateral membrane and enter the blood. hence, there is little H+ in the filtrate at this location
renal acid base regulation - distal tubule: in the distal tubule, __ is secreted into the filtrate using __ (located on __). __, located at the __ of the tubule cells help maintain a concentration gradient which facilitates the diffusion of __ into the distal tubule cell
renal acid base regulation - distal tubule: in the distal tubule, H+ is secreted into the filtrate using H+ ATPase pumps (located on apical side). Na+/K+ ATPase pumps, located at the basolateral membrane of the tubule cells help maintain a concentration gradient which facilitates the diffusion of Na+ into the distal tubule cell
what if your pH is too high? (your blood is basic: alkalosis)
if a person has alkalosis, there will be less H+ present in the filtrate to react w the HCO3- in the filtrate
the net effect is that less HCO3- will be reabsorbed into the blood and more will excreted in the urine
bc HCO3- serves as a buffering agent in the blood, if there is less of it, more H+ will remain, which will bring down the pH back to normal, compensating for the alkalosis
what if your pH is too low? (blood is acidic)
the proximal tubule cells can make extra bicarbonate (more than is reabsorbed from the filtrate) from the metabolism of glutamine
in this process, HCO3- is formed and released into the blood while ammonia (NH3) and ammonium ion (NH4+) are produced and enter the filtrate
extra bicarbonate serves as a buffer in the blood
the ammonia (NH3) and the phosphates (HPO4 2-, which have been secreted into the filtrate) react w excess H+, allowing the H+ to be eliminated in the urine in a buffered state as NH4+ and H2PO4-
erythropoietin (EPO)
hormone produced primarily by the kidneys, plays a key role in the production of red blood cells (RBCs), which carry oxygen from the lungs to the rest of the body
why can’t you drink seawater?
drinking seawater to maintain hydration is counterproductive; more water must be excreted to eliminate the salt (via urine) than the amount of water that is gained from drinking the seawater itself
this occurs bc the renal system actively regulates human blood’s sodium chloride within a very narrow range 9 g/L (0.9% by weight)
drinking seawater temporarily increases blood’s concentration of sodium chloride
this in turn signals the kidney to excrete sodium, but seawater’s sodium concentration is above the kidney’s maximum concentrating ability
eventually the blood’s sodium concentration will rise to toxic lvls, removing water from all cells and interfering w nerve conduction, ultimately producing fatal seizure and heart arrhythmia