HA: Final Exam Review
1/83
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
84 Terms
Lengthening and tortuosity of aorta (meaning that aorta be looking like a snake instead of straight and stiff). This results in kinking or buckling of the carotid artery low in the neck on the (R)
what are some findings in regards to the CV/PV system of older adults?
stenosis from atherosclerotic plaque
in older adults, systolic bruits heard in the middle or upper portions of the carotid arteries indicate?
myocardial contraction is less responsive to stimulation from beta-adrenergic catecholamines. HR also tends to drop during rest & exercise, but stroke volume is still maintained. Increased left myocardial stiffness on the left ventricle is present & dependence on atrial contraction increases due to diastolic dysfunction from decreased early diastolic filling.
what is important to remember in regards to the cardiac output of older adults?
there is a loss of atrial contraction & an onset of atrial fibrillation due to decreased ventricular filling
why does risk of heart failure increase in older adults?
🫀 Their heart doesn’t respond to adrenaline like it used to → slower heart rate.
💪 But it still pumps a decent amount of blood each beat (stroke volume = still vibin’).
🧱 The left ventricle gets stiff → hard to fill up with blood.
💃 So the atria step in to give it a boost — because relaxation phase (diastole) is slacking.
In older adults, how is cardiac output affected?
🧱 Old hearts = stiff ventricles
💃 They depend on atrial contraction (“atrial kick”) to fill properly
⚡ AFib = no atrial kick = heart doesn’t fill up w/ blood well
💣 That leads to poor pumping = heart failure symptoms show up
🎓 Common in older adults → assess for AFib + HF signs like fatigue, dyspnea, crackles, edem
what would be a consequence as a result of decreased cardiac output in older adults?
😬 1. “Just part of getting old.” They think symptoms are “normal aging” (like joint pain, fatigue, memory slips). 2. Fear of losing independence. They don’t want to end up in a home, so they stay quiet. Or they might want to avoid expenses.🙅♀ 3. Stoicism / embarrassment. Pride or generational values—some don’t want to "bother the nurse" or admit they’re struggling so they tend to overlook their symptoms or simply forget about them due to cognitive deficits.
why do older adults underreport symptoms?
start the visit with open-ended questions such as “How can I help you today?”
when it comes to the older adult, they tend to give a more positive rating in regards to their health even when affected by disease or disability. So when they come in for a visit, It is best to?
Answer: C – Many older adults think pain is “just aging” and may not speak up.
Why might older adults not report pain after surgery?
A. They have a higher pain threshold
B. They are more likely to seek medications
C. They believe pain is normal at their age
D. They experience less pain
B. Ensure hearing aids and glasses are on.
"In HESI/ NCLEX world, PRIORITY = Access First. If the senses are off, the patient is cut off. We start there."
The nurse is assessing an older adult being discharged. What is the PRIORITY action?
A. Give simple instructions
B. Ensure hearing aids and glasses are on
C. Provide a brochure in large print
D. Face the patient and speak in low tones
complete a through medication history
ask the patient to bring in all their meds including OTC (remember polypharmacy & adverse effects are common amongst this population group)
ask specific questions in regards to OTC, herbal supplements, vitamin/nutritional supplements or mood altering drugs
understand how medications work
when an older adiult comes in for a visit, what is important in regards to medications?
✅ Answer: C
Why? You need a FULL medication list to safely assess for interactions, duplications, and polypharmacy. Assessment comes before teaching or evaluating labs.
An 82-year-old patient is being seen for a health assessment. Which of the following is the nurse’s PRIORITY action related to medication use?
A. Ask the patient to describe their morning routine
B. Review the patient’s recent lab results
C. Request that the patient bring all medications, including OTCs and supplements
D. Teach the patient about avoiding herbal remedies
✅ Answer: B
Why? In older adults, new-onset confusion or dizziness is often caused by medication side effects or interactions. Get the med history FIRST for a safe, targeted response.
The nurse is assessing a 79-year-old patient who reports dizziness and new confusion. What is the nurse’s FIRST action?
A. Assess for recent falls
B. Ask the patient to list all medications, including OTCs and herbals
C. Notify the provider
D. Check the patient’s vital signs
✅ Answer: D
Why? OTCs can interact with prescribed meds, especially in polypharmacy situations. This is a safety priority and prevents adverse effects.
Which instruction would be MOST important when educating an older adult about their medications?
A. "Always take your medication with food."
B. "Avoid grapefruit juice with your cholesterol medicine."
C. "Don’t take vitamins unless your doctor says so."
D. "Only take over-the-counter meds if your doctor approves them."
10 minute geriatric screener
assess 8 things
vision
hearing
leg mobility
urinary incontinence
nutrition weight loss
memory
depression
physical disability
Do you have difficulty driving, watching television or doing any of your daily activities because of your eyesight? If yes, then test each eye with the Snellen Chart with contact lenses if pt has any
what should you ask when assessing vision on the 10 minute geriatric screener?
yes to the questions & inability to read greater than 20/40 on Snellen chart
a positive (abrnomal) finding in regards to vision on the 10 min geriatric screener is?
inability to hear 1,000 or 2000 Hz in both ears or either of these frequencies in one ear
a positive screen for hearing on the 10 min geriatric screener is?
unable to complete task in 15 sec
when assessing mobility on the 10 min geriatric screener, you tell the patient “rise from the chair. walk briskly, turn, walk back to the chair, and sit down.” what is a positive screen (abnormal finding) for leg mobility?
answering yes to being unable to hold urine and getting wet as well as losing urine in at least 6 separate occasions.
a positive screen for urinary incontinence in the 10 min geriatric screener, would mean?
yes to losing 10 lbs over past 6 mths WITHOUT TRYING
weighing the pt & they’re <100 lbs
an abnormal positive screen for nutrition/weight loss on the10 min geriatric screener, is ?
unable to remember all 3 items after 1 min
on the 10 min geriatric screener, what is a positive screen for memory?
✅ Answer: B
Why? A positive 2-question screen = needs full assessment (GDS) next—not panic, not assumptions.
The nurse performs the depression screening from the 10-Minute Screener. The patient answers “yes” to both screening questions. What should the nurse do next?
A. Refer immediately for psychiatric hospitalization
B. Document results and perform a full Geriatric Depression Scale (GDS)
C. Ask the family if the patient has always been sad
D. Notify the patient’s insurance provider
Answer: C
Why? This Mini-Cog result is positive for cognitive decline = early dementia screening is now a priority.
During a geriatric screening, the patient draws a clock with all numbers on one side and cannot recall any of the three words given. What is the nurse’s best action?
A. Ask the patient to try again in 5 minutes
B. Document normal age-related changes
C. Notify the provider of potential cognitive impairment
D. Provide reassurance and reschedule the exam
Answer: B
Why? A TUG test taking >12 seconds = fall risk = priority safety concern 🚨
Cognition and incontinence matter, but fall risk = immediate injury threat.
The nurse is using the 10-Minute Geriatric Screener with a 78-year-old patient. Which finding should the nurse report to the provider FIRST?
A. The patient forgot one of the three words in the Mini-Cog
B. The patient takes more than 12 seconds to complete the TUG test
C. The patient reports recent bladder leaks
D. The patient reports weight loss of 7 pounds over 3 months
SAFETY (falls, meds, confusion)
Function loss
Unrecognized decline
Clues of hidden depression or dementia
In regards to the 10- minute Geriatric Screener, Whenever you see words like “FIRST,” “BEST,” “MOST important”, you should look for?
✅ Answer: C
Why? Classic stress incontinence—pressure ↑ = leakage
An older adult tells the nurse they “sometimes leak a little” when sneezing or laughing. Which type of incontinence is most likely?
A. Urge
B. Overflow
C. Stress
D. Functional
✅ Answer: B
Why? Always assess before referring or intervening. Bates emphasizes a clear history to determine type & cause.
The nurse is assessing an older adult with reports of urinary leakage. What should the nurse do FIRST?
A. Refer the patient to a urologist
B. Ask about the onset, frequency, and triggers
C. Recommend adult briefs
D. Test for a UTI
urge incontinence
cause: overactive bladder
“gotta go NOW”
overflow incontinence
cause: can’t empty fully
keyword: “dribbles + distended bladder”
functional incontinence
cause: cannot get to the toilet due to a mobility issue (does not have to be physical can also be cognitive)
mixed incontinence
cause: combo of stress + urge (overactive bladder + leak attack due to weak pelvic muscles as a result of laughing or sneezing)
✅ Answer: A
Why? They may not make it to the toilet in time—mobility issue = functional.
Which older adult is MOST at risk for functional incontinence?
A. A patient with Parkinson’s who uses a walker
B. A patient who drinks 4 cups of coffee daily
C. A patient with weak pelvic floor muscles
D. A patient with benign prostatic hyperplasia
<10 seconds because >20 that is abnormal (according to book)
what is the normal scoring for the timed up and go test for the elderly?
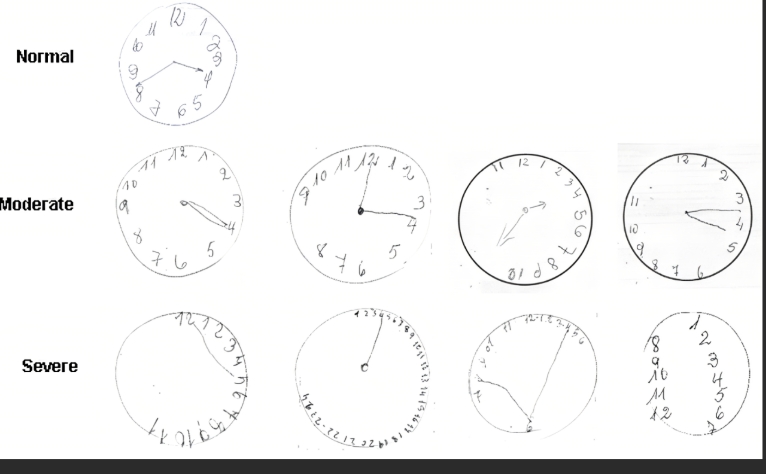
The Clock Drawing Task (Mini-Cog)
What Counts as a “Clock Error”?
Examples of clock errors that raise a red flag:
Numbers are missing, jumbled, or not spaced correctly
All numbers are on one side of the clock
Hands point to the wrong time
Hands are not clearly distinguishable (no difference in length)
They draw random shapes or scribbles
No numbers at all
These errors may suggest early dementia, Alzheimer’s, or other cognitive decline—especially when combined with poor word recall from the Mini-Cog test.
delirium + depression
onset: sudden but depression may have building for weeks
cognitive baseline: normal baseline when not depro
clock drawing on mini cog: tried, may draw a basic clock
Was this patient functioning fine until recently, but feeling sad? → Probably depression
delirium + dementia
onset: sudden + slow memo decline
cognitive baseline” already has chronic cognitive decline
clock errors, disorganized thinking, may not even attempt
Was this patient already confused for months? → Probably dementia
Answer: B – This patient had a mood baseline of depression, was functional, and now has sudden confusion = delirium superimposed on depression
A 78-year-old patient suddenly becomes withdrawn and disoriented during hospitalization. Her daughter reports she has seemed “down” for months but was living independently. Which condition is most likely?
A. Dementia with delirium
B. Depression with delirium
C. Delirium alone
D. Early-onset dementia
fibroadenoma
benign tumor, most common breast mass
usual age: 15-25 usually puberty & young adulthood, but up to age 55
number: usually single, may be multiple
shape: round, disk-like or lobular
consistency: may be soft, usually firm, free moving
delineation: well delineated
mobility: very mobile
tenderness: usually nontender
retraction signs: absent
cancer
most common breast mass
age: 30-90, most common over age of 50
shape: usually single, though may coexist with other nodules
shape: irregular or stellae
delineation: not clearly delineated from surrounding tissues
mobility: may be fixed to skin or underlying tissues, immobile
tenderness: usually nontender
retraction signs: may be present
cyst
age: 30-50, regress after menopause except w/ estrogen therapy
number: single or multiple
shape: round
consistency: soft to firm, usually elastic
delineation: well delineated
mobility: mobile
tenderness: often tender
retraction signs: absent
✅ Answer: C – Breast cyst
🧠 Tender + fluctuates with cycle = cyst, especially in premenopausal age group.
A 48-year-old woman presents with a soft, tender breast lump that seems to get worse before her period. The lump is mobile, and there are no skin changes. Which diagnosis is most likely?
A. Breast carcinoma
B. Fibroadenoma
C. Breast cyst
D. Mastitis
✅ Answer: B – Refer for imaging and biopsy
🧠 Red flag signs: fixed, hard, skin changes = cancer until proven otherwise.
The nurse is assessing a 56-year-old woman who reports finding a hard lump in her breast. The lump is fixed, irregular, and non-tender. Skin dimpling is also present. What is the nurse’s next best action?
A. Educate about benign breast conditions
B. Refer for imaging and biopsy
C. Reassure the patient and recheck in 6 months
D. Apply a warm compress to reduce swelling
✅ Answer: C – this screams breast cancer
🔥 Peau d’orange = lymphatic obstruction = 🚨🚨🚨
Which of the following findings would require the MOST urgent follow-up?
A. A round, mobile lump that is tender during menstruation
B. A small, rubbery lump that is unchanged for 2 years
C. A firm, immobile lump with nipple inversion and peau d’orange
D. A smooth lump in a 21-year-old patient
✅ Answer: A – Fibroadenoma
🧠 Young + mobile + firm + nontender = textbook fibroadenoma.
A 23-year-old woman presents with a round, rubbery, non-tender lump in her right breast. The lump is highly mobile and she denies nipple discharge. What is the most likely finding?
A. Fibroadenoma
B. Breast cancer
C. Breast cyst
D. Fibrocystic changes
seizures
paroxysmal disorder caused by sudden excessive electrical discharge in the cerebral cortex or its underlying structures
loss of consciousness may be present, feelings, thought processes, sensation
ask: have you ever had any seizures or spells? any fits or convulsions?
✅ Answer: B – Vasovagal syncope
💡 Classic trigger + short LOC + quick recovery + no post-ictal state = textbook VVS
A patient becomes pale, reports feeling dizzy, then faints while standing during a blood draw. He regains consciousness within 30 seconds, alert and oriented, with no confusion or incontinence. What condition does this most likely indicate?
A. Generalized tonic-clonic seizure
B. Vasovagal syncope
C. Absence seizure
D. Transient ischemic attack (TIA)
prodrome nausea (shows up before episode begins)
diaphoresis
pallor due to fear
hypotension
what to look for in vasovagal syncope?
cranial nerve VII
it is the facial nerve and carries nerve fibers that control facial movement and expression. The facial nerve also carries nerves that are involved in taste to the anterior 2/3 of the tongue and producing tears (lacrimal gland).
both sensory & motor
taste for sweet, salty, sour, bitter
CN V
sensory & motor (the feel and chew)
face, sinuses, teeth, corneal reflex, MOTOR: MASTICATION, clenching jaw
CN IX
GAG REFELX, posterior eardrum & earcanal
CN X
= Uvula movement.
When you ask your patient to say "Ahhh" during an oral exam: The soft palate & uvula should rise midline.
pupil constriction
occulomotor CN III is known for?
✅ Correct Answer: C – CN IX and X
Rationale: These control swallowing, gag reflex, and speech. New slurred speech and dysphagia could indicate a stroke or other neuro impairment.
The nurse is assessing an older adult client with new-onset slurred speech and difficulty swallowing. Which cranial nerves should the nurse assess first?
A. Cranial nerves II and III
B. Cranial nerves VII and VIII
C. Cranial nerves IX and X
D. Cranial nerves V and VI
✅ Correct Answer: C – CN III (Oculomotor)
Rationale: CN III controls most eye movement, the eyelid (levator palpebrae), and pupil constriction. This pattern is classic for CN III palsy.
A nurse performs a cranial nerve assessment on a patient who presents with a drooping left eyelid, a dilated left pupil, and the inability to move the left eye up or in. Which cranial nerve is most likely affected?
A. CN IV – Trochlear
B. CN VI – Abducens
C. CN III – Oculomotor
D. CN II – Optic
✅ Correct Answer: B – CN VII (Facial) – Both
Rationale: CN VII controls facial expression, taste, saliva/tear production (motor + sensory = both). Drooping/drooling = facial nerve issue.
A nurse is caring for a client with a suspected brainstem lesion. When testing cranial nerve function, the nurse notes impaired facial movement, drooling, and the inability to close the eyes tightly. Which cranial nerve is likely involved, and what is its function classification?
A. CN V – Sensory
B. CN VII – Both
C. CN VIII – Sensory
D. CN XII – Motor
✅ Correct Answer: C – CN VI (Abducens)
Rationale: CN VI controls the lateral rectus muscle (eye abduction). If the eye won’t move laterally, this nerve is likely damaged.
A nurse performs an eye assessment and notes that the patient cannot move their right eye laterally. Which cranial nerve is most likely affected?
A. CN III – Oculomotor
B. CN IV – Trochlear
C. CN VI – Abducens
D. CN VII – Facial
✅ Correct Answer: B – Notify the provider
Rationale: This could signal CN II (optic) or CN III (oculomotor) damage. Absence of both direct and consensual response = neuro red flag 🚩
During a cranial nerve assessment, the nurse shines a light into the patient’s right eye and observes no direct or consensual pupillary response. What is the priority action?
A. Reassess using a Snellen chart
B. Notify the provider of possible optic or oculomotor nerve dysfunction
C. Ask the patient if they wore sunglasses recently
D. Document findings as age-related
✅ Correct Answer: B – CN III (Oculomotor)
Rationale: CN III does eyelid elevation, pupil constriction, and eye movement. Injury = "down and out" position + blown pupil + ptosis = classic CN III palsy.
The nurse is assessing a client after a head injury. The client has ptosis, a dilated pupil, and the right eye is turned down and out. Which cranial nerve is affected?
A. CN II
B. CN III
C. CN IV
D. CN VI
✅ Correct Answer: B – CN IV (Trochlear)
Rationale: CN IV controls the superior oblique, which moves the eye down and in. Patients may have trouble reading or walking down stairs.
A nurse is testing extraocular movements and observes that the patient’s eye does not move downward and inward. Which cranial nerve is most likely involved?
A. CN III – Oculomotor
B. CN IV – Trochlear
C. CN VI – Abducens
D. CN II – Optic
dysarthria
defective articulation, a speech disorder that affects the motor control of speech causing slurred, slow, weak, or imprecise articulation of speech
aphasia
language disorder that affects comprehension and expression of language, leading to difficulties with word finding, grammar, & sentence structure
dysphonia
results from impaired volume, quality, or pitch of the voice (having abnormal voice also known as hoarseness)
anhedonia
loss in pleasure of activities associated w/ depression
✅ Correct Answer: D – Depression
Rationale: Depression in older adults often looks like dementia, but with slowed thinking, loss of interest, and low mood. Screening is critical.
An older adult is forgetful, has low energy, poor appetite, and complains of feeling “slowed down.” The nurse suspects:
A. Early-stage Alzheimer’s
B. Delirium from infection
C. Normal aging
D. Depression
✅ Correct Answer: B – Assess for suicidal ideation with a plan
Rationale: This is a red flag statement. The nurse must immediately assess suicide risk level (intent, plan, means, timing). This is a priority safety issue.
An older adult with known depression tells the nurse, “I sometimes think I’d be better off not waking up.” What is the nurse’s best response?
A. “It’s common to feel that way when you’re down.”
B. “Do you have a plan for hurting yourself?”
C. “Have you been taking your medications regularly?”
D. “Let’s talk about something positive.”
mini mental state examination
a brief questionnaire widely used to screen adult pts for cognitive dysfunction or dementia
questions involve testing orientation, registration, attention, calculation, recall, language & ability to follow simple instructions
only used in pts fluent in English, have min of 8th grade education
a score of 0-17 would have severe cognitive impairment
a score of 30 is normal
True
true or false, when it comes to the mini mental state examination, the maximum score is 30 pts and as cognition declines so does the score.
rovsign’s sign
Palpation of left lower abdomen causes pain in the right lower abdomen.
positive in appendicitis
obturator’s sign
is a clinical sign of acute appendicitis, it is defined as discomfort felt by the subject/patient on the slow flexion & internal rotation of the hip joint, while the right knee is flexed. It indicates an inflamed pelvic appendix that is in contact with the obturator internus muscle

psoas signs
is elicited by having the patient lie on his or her left side while the right thigh is flexed backward. Pain may indicate an inflamed appendix overlying the psoas muscle.

PAD
cause: Atherosclerosis = narrowed arteries ↓ blood flow to extremities
s/s: Cool, pale legs, hair loss, intermittent claudication, ulcers on toes, pain ↑ w/ elevation
KEY: ↓ pulses, dry wounds, cap refill slow, ABI < 0.9
action: dangle legs
dependent rubor when elevated white, when lowered turns red,

PVD
cause: Vein valves weak = blood pools = stasis
s/s: Warm, red skin, edema, varicose veins, ulcers near ankles, pain ↓ w/ elevation
KEY: Pulses present, skin brown & thick, wet ulcers
action: elevate legs!
palpitations
may result from an irregular heartbeat, from rapid acceleration or slowing of the heart, or from increased forcefulness of cardiac contraction
dyspnea
an uncomfy awareness of breathing that is inappropriate to a given level of exertion
aortic murmurs, soft diastolic murmur of aortic regurgitation may be missed if not listened to this position (aortic insufficiency)
Sitting Leaning Forward, exhale completely and stop breathing in expiration accentuates?
pt being supine w/ HOB elevated 30 degrees
cardiac examination involves?
to locate PMI since these positions bring ventricular apex and left ventricular outflow tract closer to the chest wall
why should pt be placed in left lateral decubitus position?
pleura/pleurae
2 serous membranes that cover the outer surface of the lung
visceral pleura
parietal pleura
visceral pleura
lies Next to lungs
No sensory Nerves;
parietal pleura
lines the inner rib cage & upper surface of the diaphragm
Rich nerve innervation;
Lines inner rib cage
inflammation produces pleuritic pain with deep inspiration, for example, in pleurisy, pneumonia, and pulmonary embolism
pleural effusion
accumulation of fluid between the pleurae
pt with pleuritis will avoid taking deep breaths due to pain. worsening sharp pain often occurs during breathing, coughing, or sneezing. These actions cause pleura to move, which aggravates the inflammation. As a result, the patient may take shallow breaths in an attempt to reduce discomfort.
Is the patient with pleuritis, taking deep breaths? WHY?
percussion
realtively high in pitch