KNES 495 - Final
1/364
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
365 Terms
Digestive disorders statistics
Make up 1/3 of the doctor visits among patients older than 65
35% to 40% of geriatric patients will have at least
one GI symptom in any yearConstipation, fecal incontinence,
Diarrhea, irritable bowel syndrome (IBS),
Reflux disease and swallowing disorders
Digestive changes as you age
↓ taste buds
↓ pancreatic enzymes
↓ GI absorption
↓ GI motility
constipation
↓ Sphincter activity
Heart burn
↓ GI blood flow
↓ Gastric acid secretion
↓ Absorption of iron, calcium, & folic acid.
Common signs and symptoms of digestive disorders
Perforations
cause peritonitis and septicemia
Alteration in motility
Diarrhea (15% of 65+ Canadians)
Nausea / Vomiting
Constipation (25% of those 65+)
Bleeding and digestive disorders
Hematemesis (esophagus or stomach)
• Blood in vomit
Hematochezia
• Blood in feces (bright red)
Melena (stomach or top part of intestines)
• Blood in feces (dark, tarry)
Gastrointestinal Bleeding in the Elderly
Bleeding is common in patients over 65
75% of the bleeding is in the upper tract
50% is due to NSAID use
50% is due to ulcers or erosions (peptic or esophageal)
Females are at higher risk than males
Digestive disorders diagnostic tests
X-ray
GI series
Barium swallow and enema
Occult blood
Blood in feces
Endoscopic exam
Esophagogastroduodenoscopy (EGD
colonoscopy
Oral Health and Aging
30% of Canadians over the age of 65 are missing teeth (endentulous)
Osteoporosis of mandible and maxilla bones
Sunken jaw
tooth loss
Aging of teeth
Bad breath
Yellowish brown discoloration
Recession of pulp from crown
Narrowing of root canal
Pulp calcification
Teeth fracture easily
Odontoblasts secrete less dentin
Roots become brittle
Teeth shorten due to wear
Discolouration
Gum recession and infection (peridontitis)
Gum bleeding
Periodontal disease
1 in 5 Canadians have periodontal disease
7 out of 10 will experience gum disease in their lifetime
More severe in Men
Gum recession and inflammation causes the loosening and loss of teeth
Periodontal disease: Canadian statistics
5% of Canadians have no teeth
21% of population over the age of 65
1 in 5 Canadians over the age of 60 have full dentures
More than half have bridges
Dysphagia
Difficulty swallowing may be associated with
Difficulty with chewing (choking risk)
Nerve dysfuncton - Stroke or Parkinson’s disease or ALS
Failure of lower esophageal sphincter to relax
Reduced peristaltic contractions in esophagus
Reduced saliva production
Deglutination - Swallowing
Food to the back of the throat
Tongue rises pushes posterior
Soft palate and hyoid elevates / Epiglottis closes
Peristaltic contraction of the esophagus
8-20 seconds for food movement
Dysphagia symptoms, causes and treatments
Symptoms
Pain on swallowing
Coughing, gagging
Food “getting stuck”
Weight loss? Change in voice?
Causes
Poor muscle or nerve function
Abnormal growths
Chronic inflammation (eg. Smoking)
Narrowing of esophagus
Treatments
Surgery, stents, dilations
Lifestyle changes (Eat slowly, chew well, sit straight, exercise)
Dysphagia Stages
Stages 1 and 2 – difficulty eating dry foods
Stages 3 and 4 – semi-solid and liquids only
Stages 5 and 6 – unable to swallow fluid
Gastro-Esophageal-Reflux Disease (GERD) symptoms
Reflux of gastric acid into the esophagus
Seen in 35% of individuals 50-79 yrs old
Symptoms
Chest pain / burning
Burping
Bad breath
Tooth decay
Coughing
Excess saliva
Gastro-Esophageal-Reflux Disease (GERD) causes and treatment
Causes
Decreased emptying of stomach
- Slower digestion with aging
increased gastric pressure (over-eating)
Decreased low esophageal sphincter pressure
Increased gastric secretion
Treatment
H2 receptor blockers
- suppress gastric secretion
Esophagitis
Long-term reflux
bleeding, ulceration, and scarring
Treatment:
Avoid large meals
Avoid spicy foods
loose clothing
gum
Surgery if severe
Hiatal Hearnia
Wider diaphragmatic opening with aging
Part of stomach moves into chest
Symptoms
Heartburn (↑ with age)
Or asymptomatic
Treat
Avoid large food intake / spicy food
Surgery may be required
Aging and the stomach
Diabetics
Gastric emptying slows by up to 50%
Peptic (Gastric) Ulcer
Hole caused by inflammation and necrosis
Caused in part by pepsin, low mucous (with aging)
Helicobacter pylori
NSAIDs
stomach and duodenum
Peptic (Gastric) Ulcer symptoms and risk factors
Symptoms
Pain
Bleeding (hematemesis or melena)
Risk Factors
Smoking / alcohol
Use of NSAIDS
Low fibre / poor diet
Spicy food
Stress
Classes of Bleeding Ulcers and Treatment
Classes of Bleeding Ulcers
Active bleeding
Non-bleeding visible vessel
Clotted / Dot
Clean base
Treatment:
Reduction of contributory factors
Antacids
Surgery in severe cases
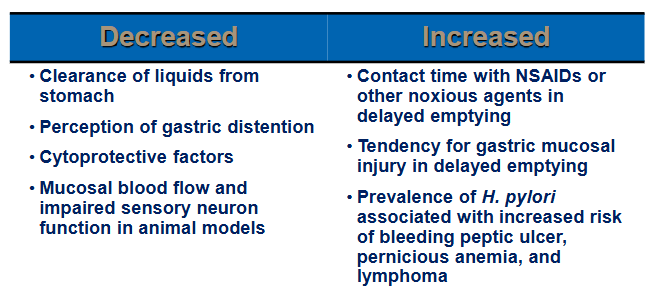
Functional Dyspepsia
Chronic disorder of the upper digestive tract
Poor sensation and peristalsis
Affects 30-45% of Canadians over 65
Functional Dyspepsia symptoms and causes
Symptoms
Nausea, vomiting
Belching
Bloating
Indigestion / heartburn
Causes
Slow emptying of stomach / Altered intestinal motility
Changing acid and enzyme levels
Gallstones / Ulcers / Cancer / GERD
Chronic inflammation
Functional Dyspepsia
Reduce individual food triggers
milk, alcohol, caffeine, fatty foods, mint, tomatoes, citrus fruits, and some spices
Medications
H2RA’s – block histamine
⬧ Eg. Zantac and PepcidPPI’s – block acid secretion
⬧ Nexium, Prevacid, LoSecMedications that increase gut motility
Lifestyle changes
Exercise regularly / No smoking, alcohol
Absorption in the Small Intestine with aging
Absorption decreases with aging
Reduced enzymes and carriers
Malabsorption syndrome
SI can’t absorb nutrients
- fats and minerals
- Diarrhea, foul feces
Causes
- Disease of intestinal wall
- Blocked exocrine ducts
Diet therapy
- Treat malnutrition
Diseases of the Small Intestine
Regional enteritis
Crohn’s disease
inflammatory bowel disease (IBD)
Often SI
Exacerbation / remission
Regional enteritis symptoms and treatment
Symptoms:
Anorexia
Flatulence
pain
Diarrhea and constipation
Supportive treatment:
Low-residue diet
Medications
surgery
Diseases of the Colon: Intestinal obstruction
Blockage in intestine or bowel
tumours, hernias, adhesions
volvulus, intussusception
paralytic obstruction
Intestinal obstruction: Symptoms and Treatment
Symptoms:
abdominal pain
distention
Nausea and vomiting
Treatment:
Nasogastric suctioning
Surgery
Ulcerative Colitis Symptoms
Chronic inflammation of colon
Symptoms:
Lower abdominal pain
Blood in stools
Anemia
Diarrhea
Ulcerative Colitis Treatment
Dietary limitations
Stress reduction
Mild sedatives
Anti-inflammatories
Surgery
Irritable bowel syndrome Symptoms
aka spastic colon
Inflammation of bowel with chronic lesions
Symptoms:
Abdominal pain
Altered motility
Diarrhea or constipation
Irritable bowel syndrome Causes and Treatment
Causes:
Spicy foods and seasonings
Caffeine
Alcohol
Stress
age
Treatment:
Avoidance causative factors
Hemorrhoids Causes
Varicose veins in rectum
Inflamed veins with prolonged stresses
Internal or external
Causes:
Pressure in anal area
Constipation
Age
Hemorrhoids aging effects and symptoms
Aging effects
less motility - constipation
blood flow to anal region (and lower body) slow
Blood is more likely to pool in the veins
Symptoms
Pain
Itching
Bleeding
Hemorrhoids prevention and treatment
Prevention:
Good bowel habits – fluids, fibre
Exercise
Avoid laxatives
Treatment:
Medications / creams
Warm sitz baths
Manual reduction
Cryosurgery
hemorrhoidectomy
Colorectal Cancer and Aging
90% of all cases occur in individuals aged > 50 years
Colorectal Cancer: warning signs, prevention and treatment
Warning Signs
Nocturnal Bowel movements
Weight loss
Diarrhea / constipation
Rectal bleeding
Preventative
Colonscopy
Fibre / diet / Exercise
Treatment
Surgery / chemotherapy if needed
Diverticular Diseases
Common with aging
5% of population younger than 40
50% of those aged 60 years and older
65% of those over 85 years of age
Diverticula
pouch-like projections
Two conditions
Diverticulosis
Diverticulitis
Diverticular Diseases: risk factors and potential causes
Risk factors
Lack of fibre in diet
- weak areas form pouches
Lack of exercise / obesity
Smoking / Alcohol
Potential causes:
Constipation
Pressure from moving dry, hard bowel movements
Genetics
Diverticulosis
Diverticula usually measure 0.5-1cm
Can exceed 2 cm
Some as large as 10 cm
Most people have no pain or symptoms – some will have
Diarrhea
Constipation
Flatulence
Heartburn
Inflammation of the diverticula
Infection and bleeding
Due to material caught in diverticula
10-25 % of diverticulosis patients become inflamed
Diverticulosis symptoms and treatment
Symptoms
Tenderness / cramps
Abdominal pain
Infection / Fever
Nausea, vomiting
Blood in the stool
Treatment
Low fibre diet in flare-ups
Hospital – IV feeding (to rest the bowel)
Anti-spasmodics
Pain meds
Surgery if perforated (Antibiotics)
Colostomy
Controlling Diverticular Disease
Diverticulosis
High fibre diet
Adds bulk and softens stools
Fruits, vegetables, whole grains and beans
⬧ Limit seeds (eg. popcorn)High volumes of water
Diverticulitis
Low fibre (residue) diet initially
- Gradually increase fibre (Doctor’s supervision)
Low fat diet
Exercise and Diverticular Disease
Important for colon health
Exercise increase gut movement
30 minutes most days of the week
Divide into 5 to 10 minute sessions
Moderate intensity
Brisk walking, swimming, dancing, yard work, housework
Constipation Causes
Transit time too slow in colon
Causes:
Diet is too low in fibre and fluid
Insufficient physical activity,
Irritable bowel syndrome,
Diabetes, stroke, hypothyroidism
Parkinson’s disease (low motility)
Gut biome imbalance
medication side effect
opiates, anti-depressants, calcium channel blockers, iron
Constipation Treatment
25% over age 65
Treatment
Adequate fluid and fibre
Increase exercise
Prunes / fruit
Laxatives
Stool softeners
Risk of hemorrhoids and chronic bowel inflammation
Diarrhea Causes
Loose stools at least 3 times a day
15% of people over 65
85% of aged digestive mortality involve diarrhea
Causes
Malabsorption
Medication side effects
Cancer
Infections
Diabetes
Celiac Disease / IBS
Diarrhea Treatment
Need transit through large intestine to slow down
Treatment
Bulk formers – fibre or psyllium
Eg. Metamucil (soak up water)
Meds to slow down motility
Immodium, Anti-spasmodics
Diet / Exercise
BRAT plan
⬧ Bananas, rice, yogurt, oats
Fecal Incontinence
In ~10% of people over 70
Causes
Weak pelvic floor
Weak sphincters
Neural changes
Risk Factors
Age, female
Stroke, diabetes
Urinary incontinence, bowel changes
Diseases that affect integrative function
Comprehensive Diseases
Affect more than one body system
Heart Failure
Diabetes
Liver Failure
Kidney Failure
Pancreas failure
Functions of the Liver
Makes bile from cholesterol
Makes plasma proteins (albumin)
to pull water out of tissues
Makes Clotting factors
Stores Nutrients (Fe, Mg, Cu, Zn)
Helps remove and recycle old RBCs
Stores/Metabolizes Vitamins
Makes glycogen
Angiotensinogen
Biotransformation
Effects of Aging on the Liver stats
Liver starts to show changes after the age of 35
Intensifies after age 60
Female > Male
30-50% decrease in liver size
30% decrease in blood flow to liver
Normal flow is ~1.5 L/min
10-20% decrease in perfusion
Effects of Aging on the Liver
Decreased number of hepatoctyes
Decreased Bile formation
Bile becomes lithogenic
More cholesterol within the bile
More likely to form gall stones
Increased fat in liver
Increased collagen
Increased lipofuscin (“age” pigments)
Decreased liver enzyme activity
Decreased Biotransformation
Drug clearance slowed (by up to 50%)
Made worse by alcohol, smoking, diet
More susceptible to drug-induced injury
Hepatitis and Cirrhosis more severe with age
Common signs and Symptoms of liver failure
Liver disease
Jaundice
Gallbladder disease
Pain
Diagnostic Tests for liver failure
Liver function tests
bilirubin, albumin, and enzymes
Ultrasound, x-rays, CAT scan
Biopsy
Liver Diseases: hepatitis causes
Inflammation of liver
Causes:
Chemical actions of drugs
Toxic substances
Chronic alcoholism
Group of viruses
Liver Diseases: hepatitis symptoms
Jaundice and liver enlargement
Myalgia and abdominal pain
Clay or light-colored stools
Dark-colored urine
Malaise
Anorexia
Fever
Hepatitis treatment and prevention
Treatment:
Rest
Good nutrition
Anti-virals
transplant
Prevention:
Good hygiene
vaccination
Special care when handling needles and body fluids
Cirrhosis
Chronic, irreversible, degenerative
Alcohol, toxins. disease
Loss of normal liver cells
No organization
Scar tissue
Cirrhosis Symptoms and Treatment
Symptoms
Nausea
Weight loss / Weakness
Inflammation then degeneration
⬧ Hobnailed (nodular)Ascites
⬧ High abdominal venous pr.
⬧ Organs swell
⬧ bleeding
Treat
transplant
Gallstones
consist of cholesterol, bilirubin, and calcium
Can block ducts
If small – gravel
Five Fs for risk of gall bladder diseases
Female
Fair complexion
Fat
Fertile
Forty or older
Cholecystitis
Inflammation of gallbladder
Eg. blockage
Symptoms:
RUQ pain
Nausea and vomiting after eating
Treatment:
Surgical excision
Liver Failure
Irreversible damage
Usually Chronic and gradual
Some acute failure
- Can be < 48 hours
Difficult to detect until end-stage
Causes of Chronic Liver failure
Hepatitis (B and C are most common)
Long-term alcohol and drug consumption
Aging
Cirrhosis
Hemochromatosis
Excess iron absorption
Malnutrition
Liver cancer
Causes of Acute Liver Failure
Tylenol overdose
Hepatitis
Ingestion of poisonous wild mushrooms
Reactions to some prescription and herbal meds
Progression of liver failure
Fatty liver
Liver fibrosis
Cirrhosis
Fatty Liver
Aka Hepatic steatosis
Build up of fats in the liver
Alcohol
Obesity, diabetes, hyperlipidemia
May be asymptomatic
Most common symptom is fatigue
May be reversible with diet control and exercise
NAFLD (non-alcoholic fatty liver disease vs AFLD - alcoholic
Liver Fibrosis
High inflammation
Oxidative stress
Mitochondrial dysfunction
apoptosis
Formation of fibroids
Progression from fatty liver disease or from hepatitis B or C
Cirrhosis
Extensive fibrotic scarring and inflammation
Death of cells
Loss of function
Irreversible degeneration
Needs Transplant
NAFLD – fatty liver
NASH –non-alcoholic steatic hepatitis
NAFLD vs. AFLD fatty liver
NAFLD (non-alcoholic fatty liver disease)
better recovery
AFLD - alcoholic
much harder to pull fats out
Early Symptoms of liver failure
nausea
vomiting
loss of appetite
diarrhea
fatigue
Later Symptoms of liver failure
Jaundice
Bleeding easily
Ascites (swollen abdomen)
hepatic encephalopathy
Myalgia
Digestive system with liver failure
Decreased bile
Decreased fat digestion
diarrhea
Decreased essential fatty acids
Decreased fat soluble vitamin
Eg. Vitamin K – clotting
Large intestine problems due to higher fat content
Poor storage of vitamins, nutrients, and minerals
Malnutrition
Affects enzyme activity and metabolism
Cardiovascular system with liver failure
↓ Angiotensinogen
Inability to control blood pressure
Sepsis / inflammation may occur
↓blood pressure
↓ blood proteins
Affects water balance
High portal pressure in liver
Edema
Atherosclerosis
Less fat processing
↓ blood proteins
Poor transport of hormones and vitamins
edema
↓ formation of clot factors
↓ vitamin K
Bleeding issues
Immune system with liver failure
↑ toxins
weakens immune response
Sepsis
Lymph system with liver failure
lymph vessels cannot drain the fluid caused by sepsis.
Nervous system with liver failure
Less ammonia converted to urea
↑ ammonia
Hepatic encephalopathy
Cerebellar shrinkage
Less cerebral function
Endocrine system with liver failure
↓ somatomedins
↓ cell growth and repair
↓ angiotensinogen/angiotensin
↓ thrombopoietin
So ↓ megakaryocytes
- ↓ platelets
Renal system with liver failure
fails to filter excess amino acids
Can’t process them into urea
Build-up of toxins (not biotransformed)
Leads to Kidney failure
Respiratory system with liver failure
Metabolic acidosis may occur
Result of retained amines
high levels of NH4+
lead to brain swelling and decreased blood flow to the brain
Body may Hyperventilate to compensate
May result in respiratory Alkalosis
Treatments for liver failure
Anti-virals (for Hep C)
In advanced stages
liver transplant
preventing progression
Alcohol stats
Globally
Alcohol-related deaths account for 5.1% of all deaths
In the US
Alcohol-related deaths account for more than 10% of all deaths
Large increase in the last 10 years
Primary cause of Liver failure and Fatty
Liver disease
Alcohol Processing
Absorbed in the stomach and small intestine
Bio-transformed by the liver
Acetaldehyde is the more toxic version
Acetate can then be excreted by the kidney
Higher Dehydrogenase Activity
Higher NADH
Triggers formation of fatty acids
- Steatosis
- Results in Alcoholic Fatty Liver disease
Liver toxicity
Impaired function
spirals
Alcoholic Liver Disease (ALD)
Alcohol-induced hepatitis
Excess biotransformation / inflammation
Alcohol intake to induce ALD
Males > 4 drinks/day or 14 drinks /week
Females > 3 drinks / day or 7 drinks / week
now dropped to like ½
Moderate
Males > 2 drinks / day
Females > 1 drink / day
1 standard drink – 14 g alcohol
1 beer or 1 glass of wine or 1 shot
Alcohol effects on the liver
Fatty liver
Fat deposits in hepatocytes
Alcoholic hepatitis
jaundice
Cirrhosis
Liver cancer
Alcohol Effect on Thiamin
B1 vitamin
Needed to activate steps in the metabolic pathways
E.g. Activates Pyruvate Dehydrogenase
⬧ Needed for aerobic respiraton
Alcohol processing will divert Thiamin away from the metabolic pathways and into the acetaldehyde pathways
Thiamin deficiency
Effects of Chronic Alcohol Abuse
Increased risk for:
Liver disease
Cardiovascular disease
Cancer
Pancreatitis
Type II Diabetes
Neurological disorders
Korsakoff’s syndrome (memory disorder – thiamin deficiency)
Death
Alcohol medical problems with the digestive system
oral cavity cancer
esophageal cancer
esophageal varices
Changes in Liver - portal pressures
⬧ Causes GI bleeding
Pancreatitis
All made worse when combined with smoking!!!!!
Alcohol medical problems with the cardiovascular system
Atrial fibrillation
Hypertension
Strokes
Cardiomyopathy
Heart failure
Alcohol medical problems with the kidney
Must secrete acetate
Can lead to kidney failure
Kidney inflammation
⬧ Blocked ducts
ADH inhibited
High excretion of water - Dehydration
Can lead to acid-base imbalance
Alcohol medical problems with the nervous system
acute intoxication with loss of consciousness
Withdrawal
Seizures
subdural haemorrhage
peripheral neuropathy
Wernicke-Korsakoff syndrome
Low thiamin
cerebellar degeneration
Balance problems
Fetal Alcohol syndrome
No alcohol intake is safe during pregnancy
Reduced brain size
Low body weight
Poor coordination
Small head size
Hyperactive behavior
Attention deficit
Poor memory
Alcohol – Endocrine Effects
Suppresses the CNS
decreased hormone release from Pituitary and Hypothalamus
Results in
Decreased thyroid hormone (decreased metabolism)
Decreased cortisol
Decreased growth hormone and cell repair
Poor water balance (ADH effects)
Possible reproductive effects long-term (FSH/ LH)
⬧ Testosterone / estrogen effects
⬧ Secondary sex characteristics
Alcohol - Blood Effects
Alcohol causes a thinning of the blood
Vasodilates the arterioles
Face becomes flushed
Can affect thermoregulation (lose heat faster)
Alcohol – Metabolic effects
Decreased ATP production
Thiamin deficiency
Due to alcohol biotransformation
Results in poor glucose metabolism
Lack of TPP
Slows pyruvate dehydrogenase – less ATP
can cause permanent metabolic dysfunction
Alcohol – Respiratory Effects
Breathing is suppressed at the medulla
Decreased blood oxygen
- Affects cell function
Reduced breathing – CO2 levels rise
Respiratory acidosis
If vomit is aspirated – risk of aspiration pneumonia or respiratory infections
Alcohol – Skin Effects
With ADH inhibited – body (and skin) becomes dehydrated
More wrinkles
Also causes skin inflammation and rashes
Acetaldehyde effect