CNS Lecture 4 - Bodily movement, muscles, reflexes, brain motor centers, corticospinal tract, speech
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
48 Terms
Sensory input use
Used by the brain to control bodily movement
Flow of motor commands
Motor commands generated in higher brain centers
Sensorimotor cortex
Signals from sensorimotor cortex descent the brainstem and to the spinal cord motor neurons which innervate muscle fibers
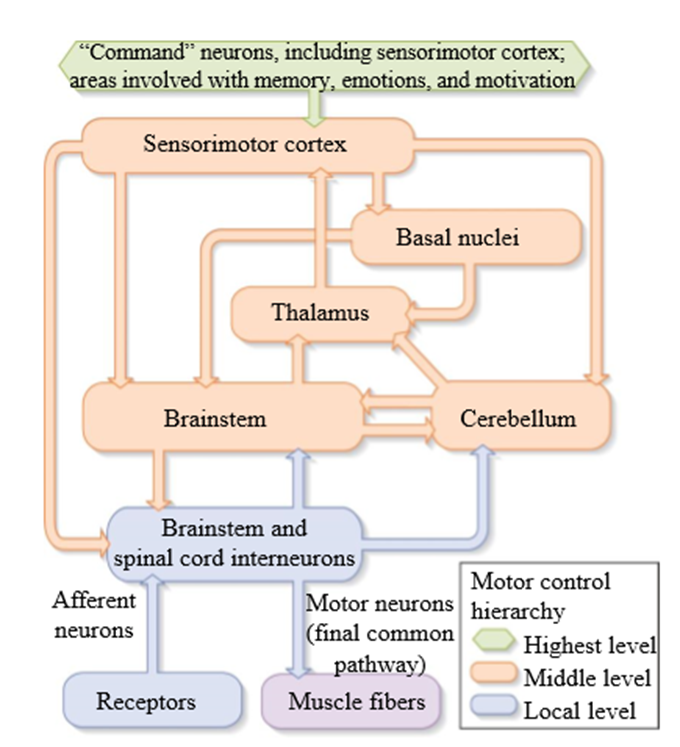
Flow of information from sensory receptors
Information from sensory receptors
Sensory pathways ascend to the brainstem, cerebellum, and the thalamus
Transmits sensory information to the sensorimotor cortex
In the sensorimotor cortex combined with input from other parts of the brain to form output commands to the brainstem, basal ganglia, and cerebellum
Basal ganglia and the cerebellum send their outputs to the thalamus and the brainstem
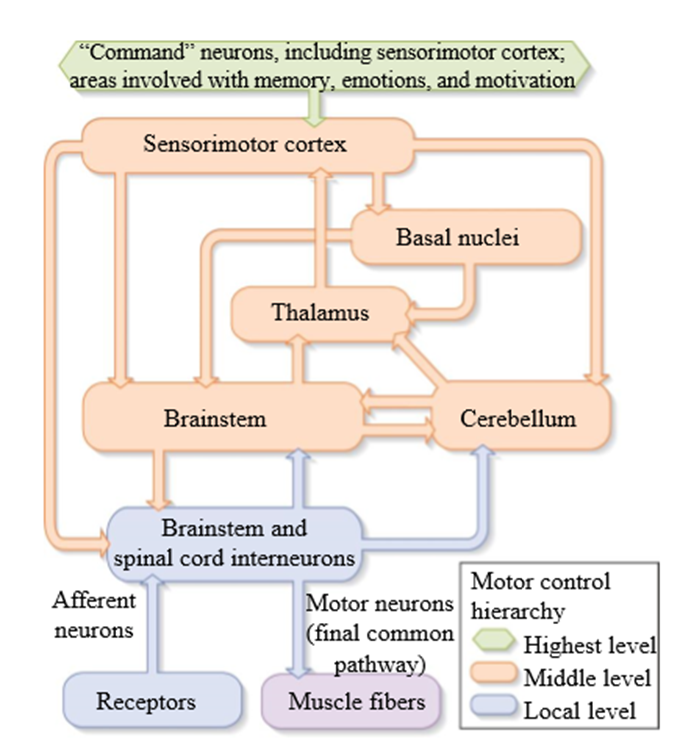
Supraspinal Centers
Involved in generating motor commands (supraspinal - above the spinal cord)
Sensorimotor cortex, brainstem, cerebellum, cerebral cortex, thalamus, basal ganglia (basal nucleus)
What parts of the brain issue motor commands via the brainstem and spinal cord
Sensorimotor cortex, cerebellum, and basal ganglia
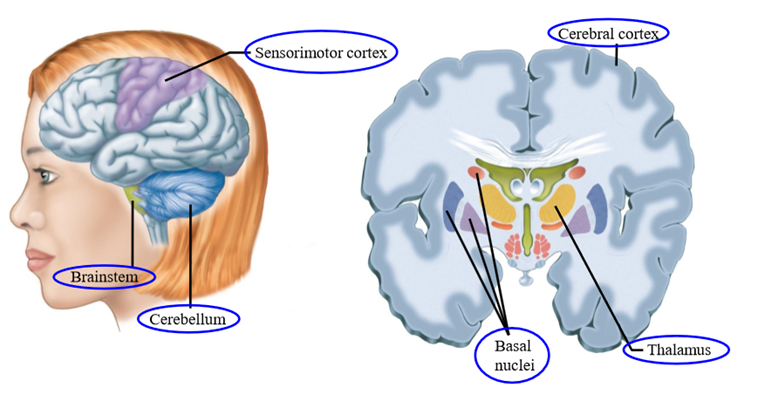
Feedback control
involves receptors which send sensory information back to the central nervous system to generate the desired movement.
Feedback control steps
Motor command is a desired limb position
Spinal cord transmtsts command to muscles by alpha motal neuronal axons
Causes muscle contraction
Receptors in muscles, joints and skin signal posiiton in limb, report back to spinal cord via afferent axons
In Spinal cord - actual position of limb is sibttracted from desired position
Difference drives motor neurons to contract muscle to shorten the difference
Moves the muscle from the current position to the desired position
With external load - deflects arm form desired position
Spinal cord will correct from external load by minimizing the difference
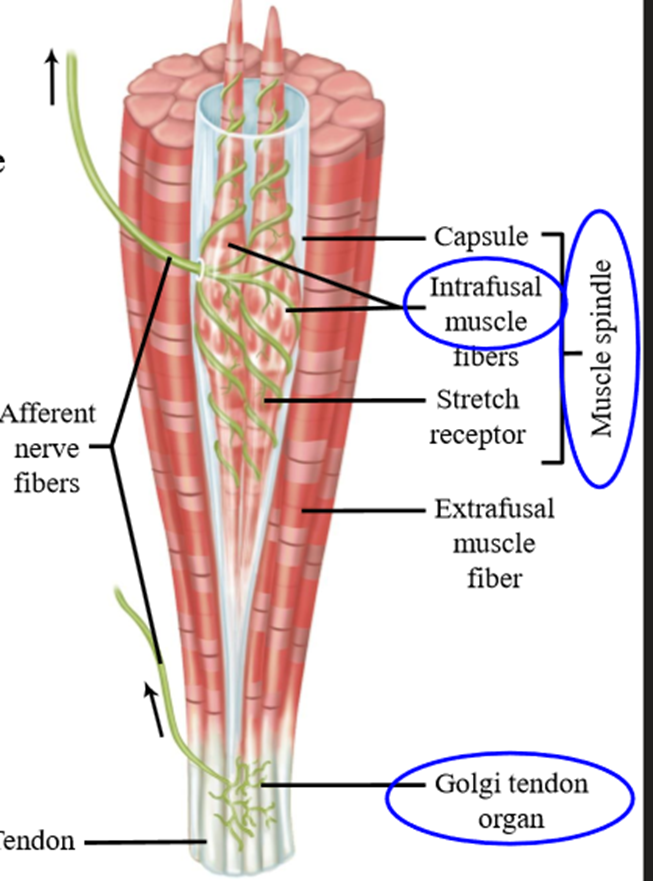
Two receptors that carry the most relevent movement sensory information
Muscle spindles: Receptors signaling change in muscle length
Golgi tendon organs: Receptors signaling change in muscle force
Muscle Spindles
Sensory receptor that signals change in muscle length. Composed of connective tissue capsule, intrafusal muscle fibers, and stretch receptors
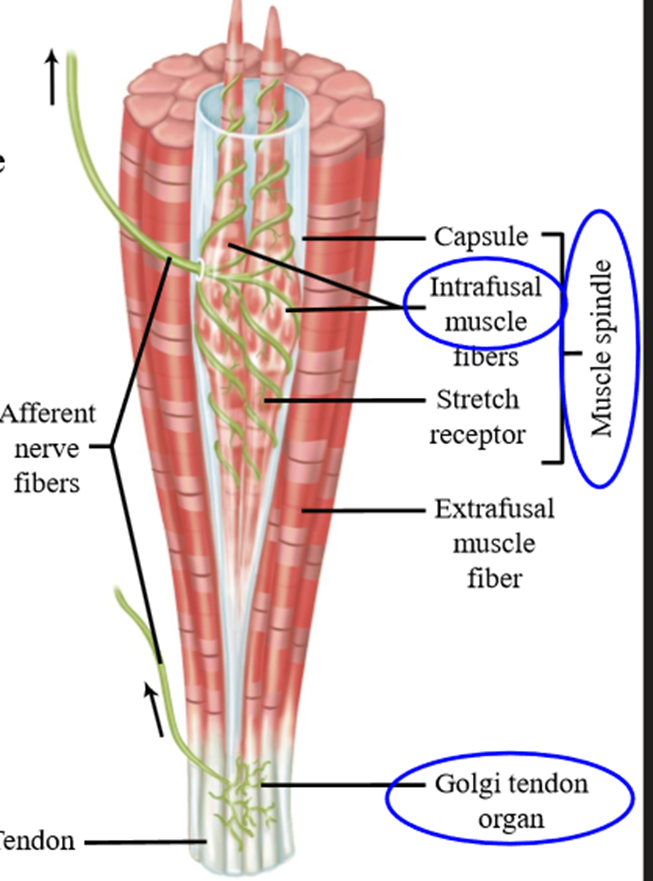
Muscle spindle function
Sensory endings (give rise to group 1 and group 2 afferents) respond to changes in muscle length
Muscle spindle sensory endings anatomy
Spiral around intrafusal muscle fibers (fibers inside muscle spindle)
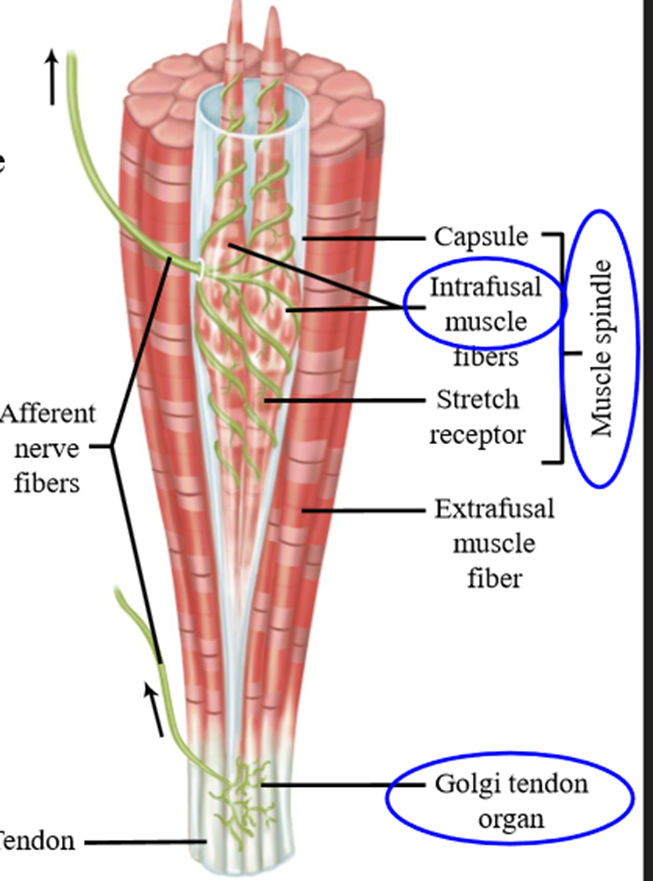
Golgi tendon organs
Tendons at the end of muscles, sensory endings respond to force produced by the muscle. Sensory endings give rise to group 1 B sensory afferents
Muscle spindle group 1A afferent function
Respond to muscle/tendon vibration, as well as responding to muscle length changes
Muscle spindle group 1A physiotherapy
tendon vibration (activates muscle spindle afferents) alleviates spasticity (overactive stretch reflex)
Muscle receptor recordings
The muscle spindle signals the length of a flexor muscle and the tendon organ signals the force in an extensor muscle.
Muscle spindle composition
Intrafusal muscle fibers, surrounded by connective tissue and stretch receptors
Only generate tiny amounts of force
Extrafusal muscle fibers
Main muscle fibers found outside muscle spindle - produce measurable force
2 types of motor neurons that innervate a muscle
Alpha + Gamma motor neurons
Alpha motor neurons
Activate main muscle extrafusal (outside muscle spindle) fibers to contract
Axons have conduction velocities as muscle spindle 1A and tendon organ 1B
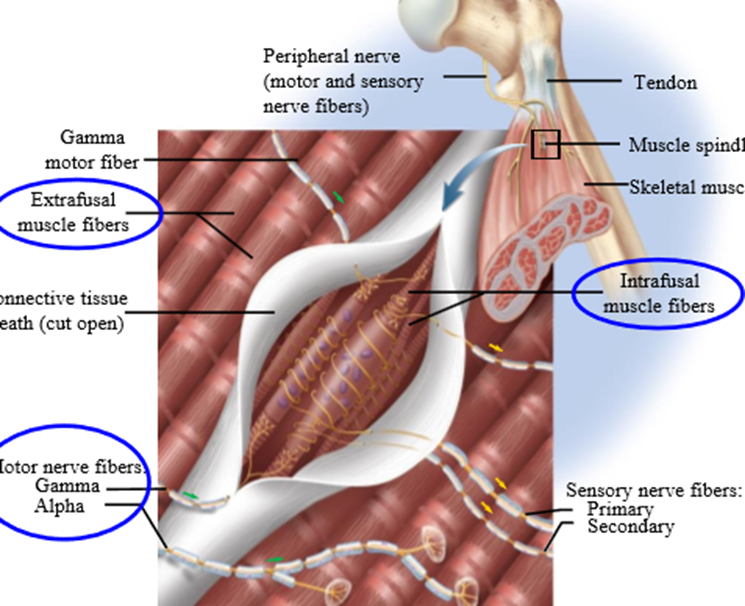
Gamma motor neurons
Activate intrafusal (inside muscle spindles) muscle fibers at each end of muscle spindle
25-40 m/s velocity
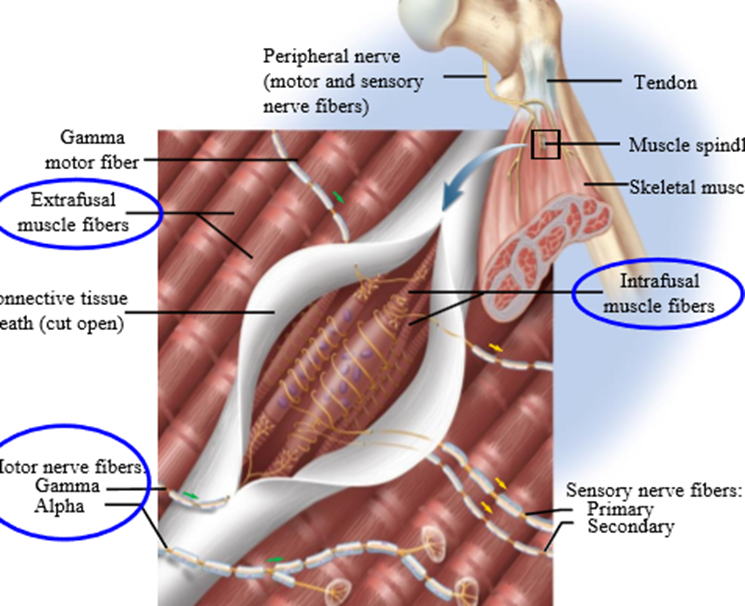
Muscle sensory ending location
Middle part of the spindle, which is non-contractile
Activation of gamma motor neurons
Intrafusal muscle fibers activate, stretching non-contractile middle part (sensory ending location)
Causes rapid firing during muscle stretch
Gamma motor neurons increase sensitivity of muscle spindles to length changes
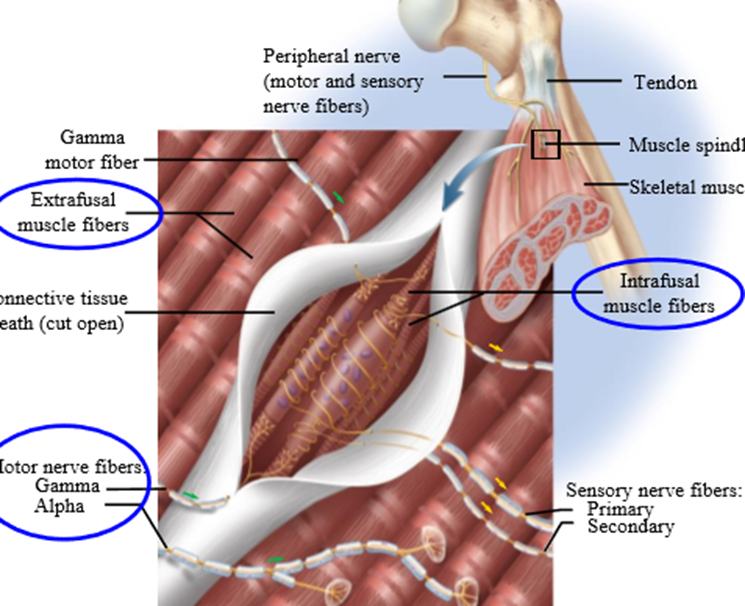
Golgi tendon organ afferents function
Signal muscle force
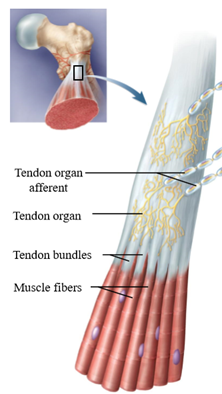
Alpha gamma co-activation theory
gamma motor neurons are coactivated with alpha motoneurons to keep the muscle spindle afferents firing during muscle shortening
If intrafusal muscle fibers are activated at the same time as alpha motor neurons, keeps muscle taught as muscle shorten
Elastic, non-contractile region remains the same length
Compensates for extrafusal shortening, allowing afferents to maintain/increase firing
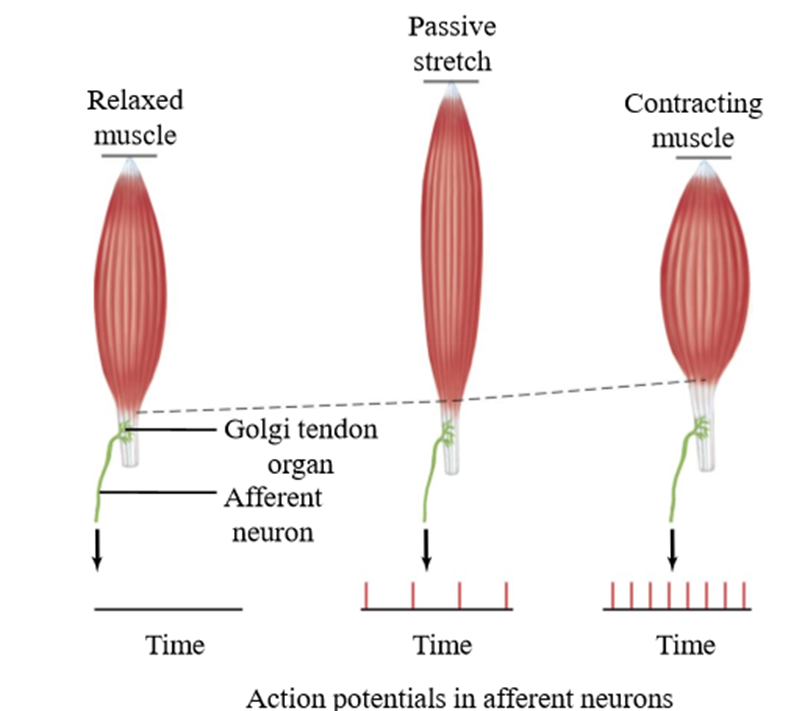
Activation of golgi tendon organs
Passive stretching causes Golgi tendon organs to respond with small increases in their rate of firing
Contraction of extrafusal muscle fibers causes golgi tendon organs to fire more rapidly
Golgi tendon organs respond to force produced by a muscle, especially producing during active contraction
Muscle spindle activation by stretch reflex
Rapid increase in length of quad muscle activates muscle spindle afferents. Afferent APs travel to spinal cord, actiivgating quadricep motor neurons.
Muscles shorten again - reflex acts to counteract stretch - resist change and maintain desired state. Stretch reflex automatically performs substation
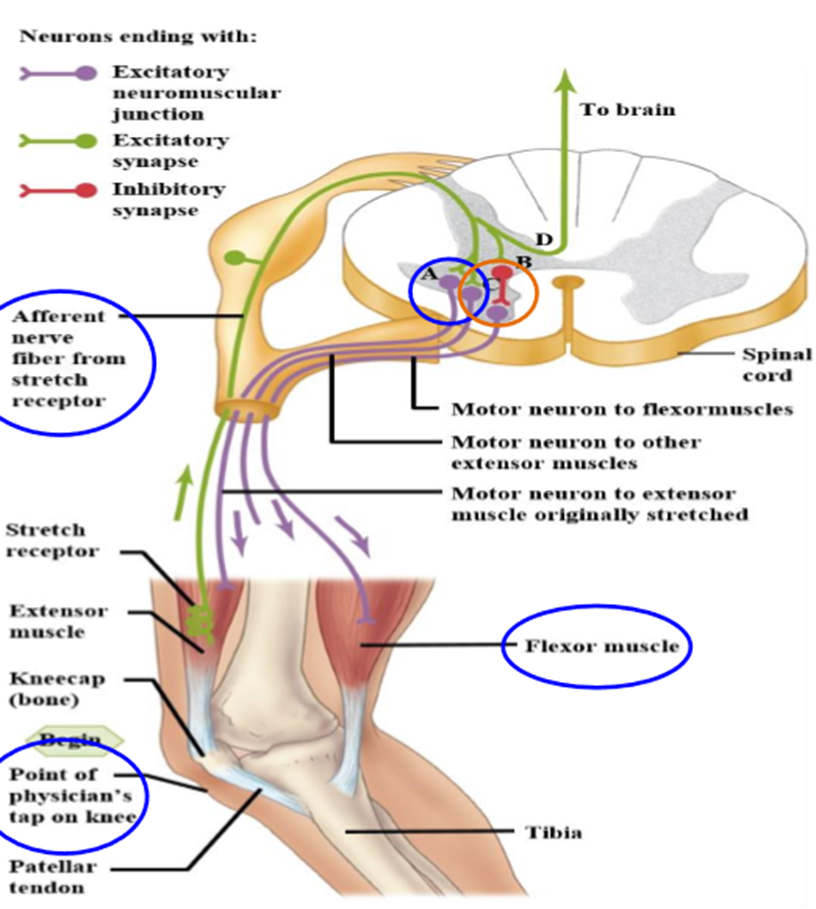
Afferent excitation of inhibitory neurons
Inhibits motoneurons that innervate antagonistic muscle
Golgi tendon activation by stretch relfex
Signals from Golgi tendon travel to spinal cord and have reverse reflex action than muscle spindle afferents
Activates an interneuron that inhibits extensor motor neuron
Activates interneuron which activates antagonist flexor motor neuron
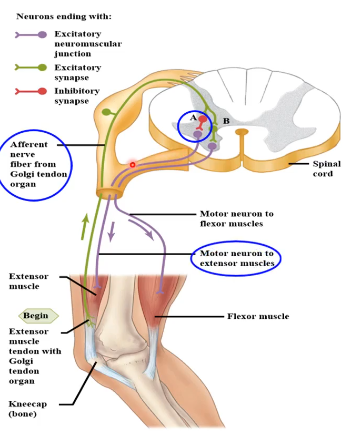
Competition by golgi tendon/muscle feedback in stretch reflex
Muscle spindle feedback resists increase in length by activating extensor motor neurons
Golgi tendon organ feedback resists increase in force by inhibiting extensor neurons
Results in muscle resisting stretch in a spring like manner
CNS allows control of “springiness”
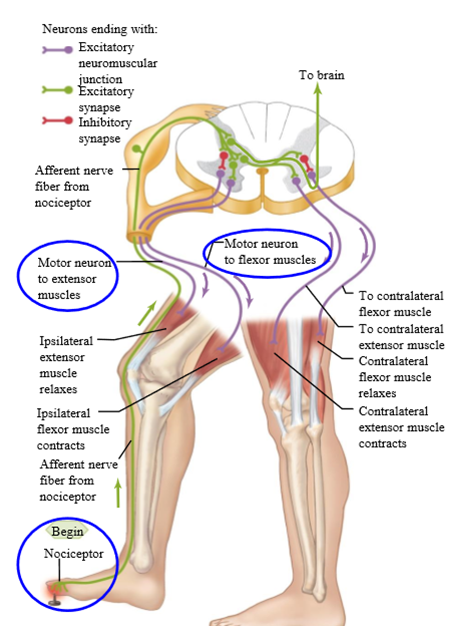
Flexor withdrawal reflex
Afferent signals from nociceptors cause reflex activation of the flexor motor neurons and reflex inhibition of extensor motor neurons, resulting in removing leg from pain
Occurs through spinal cord
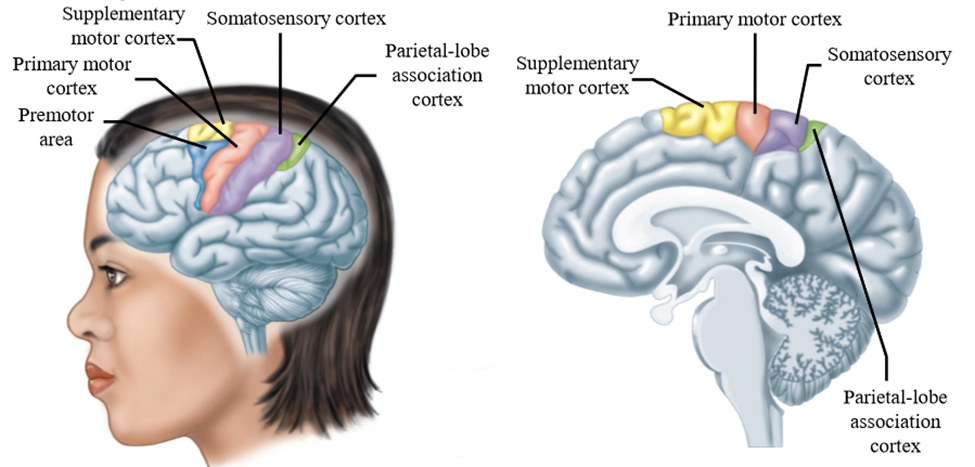
Major motor areas of the cerebral cortex
Pre-motor cortex, supplemntary cortex, primary motor (sensorimotor) cortex, somatosensory cortex, parietal lobe association cortex
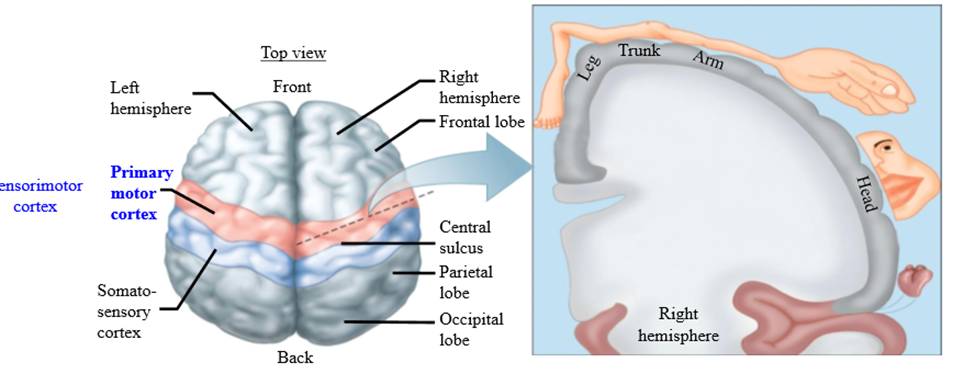
Somatotopic maps
Stimulating specific parts of the brain causes body part movement
Somatotopic representation of the primary motor cortex and the parts it controls
Primary motor cortex = sensorimotor cortex
Primary sensory cortex = somatosensory cortex
Hand and feet representation are large compared to other body parts
TMS
Transcranial magnetic stimulation - neurons in primary motor cortex can be activated
Move magnetic coil over different somatotropic representation areas causes movement of body parts (mostly hands and feet)
Research tool used in spinal cord operations to check for conduction block (thoracic surgery - make sure legs are still working)
Corticospinal Tract (pyramidal tract)
Conveys signals from the sensorimotor cortex through the brainstem to the spinal cord.
- Axons from neurons in the sensorimotor cortex form the CST
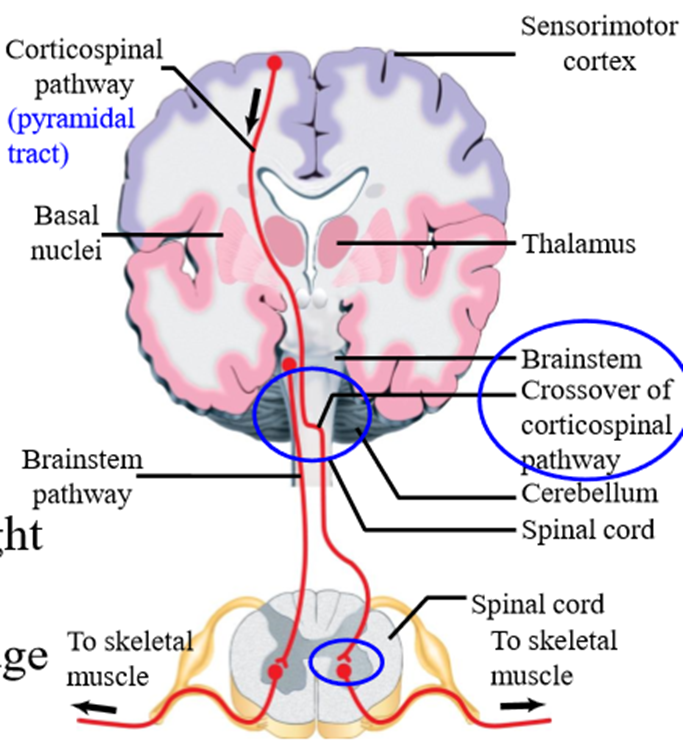
CST crossing
Crosses to the the contralateral side of the nervous system at the brainstem level
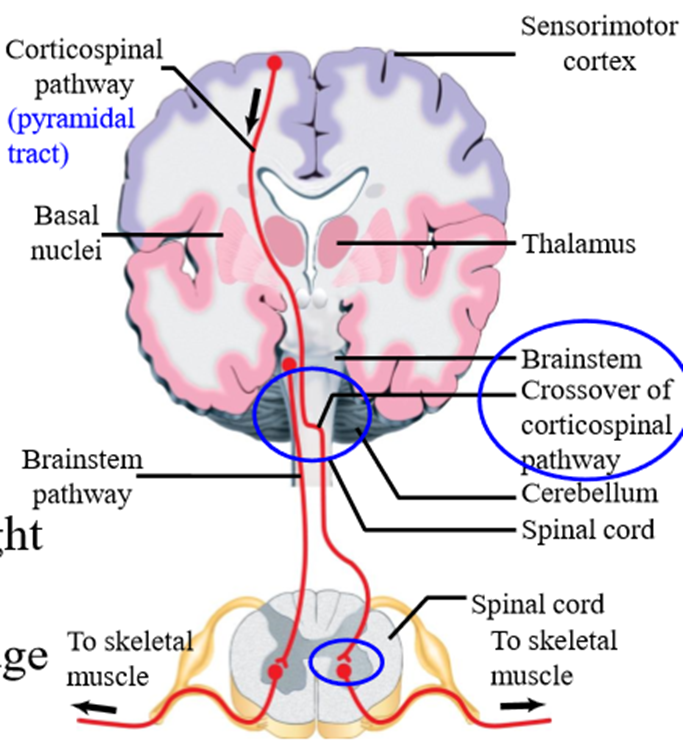
What do CST neurons connect with
Makes monosynaptic connections with spinal alpha motoneurons, whose axons activate muscles
- Only one neuronal synapse away from muscles
CST Lesions
Stroke, Cerebrovascular accident (CVA), brain attack
- Cannot move limb on the contralateral side of the body (hemiplasia)
- Motor control problems occur on the side of the body opposite to the site of the brain damage
Symptoms of CST Lesions
- Weakness (paresis) or complete paralysis of extremities
- Exaggerated stretch reflex in antigravity muscles
<Hypertonus - excessive level of skeletal muscle tension/activity
< Spasticity is a state of increased muscular tone with exaggeration of tendon reflexes
- Muscle spasm
- Speech deficits - seen when lesion on left side of brain
- Attention deficits
<Aphasia - inability to understand meaning of sensory inputs/defect in language.
<Apraxia - problem using day-to-day objects
<Hemineglect - Occurs when patients are not aware of items on one side of their body
CST lesions other name:
Upper motoneuron lesions
Why are CST lesions called upper motoneuron lesions
Final output pathway of the brain, synapsing onto spinal alpha motoneurons (lower motoneurons)
Which side of the brain controls speech
Left side
2 main speech areas:
Broca's area + Wernicke's area
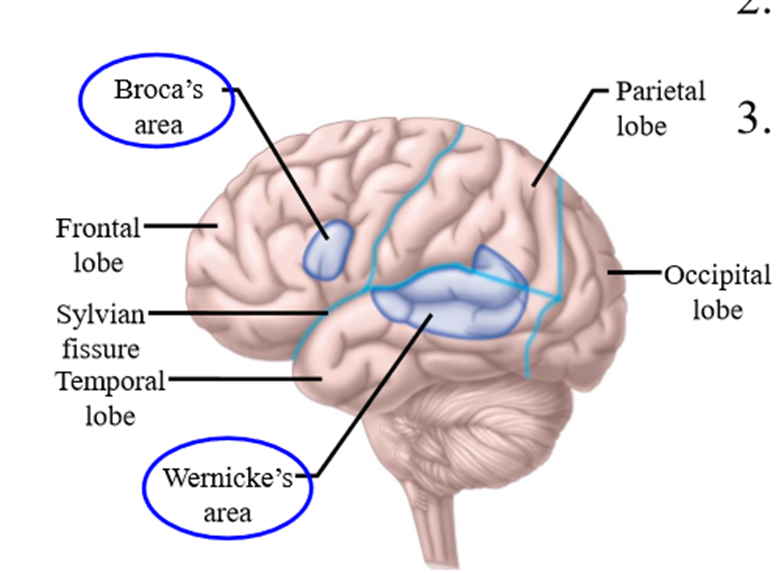
Broca's area function
Motor aspects of speech (production)
- Control larynx, tongue and lips
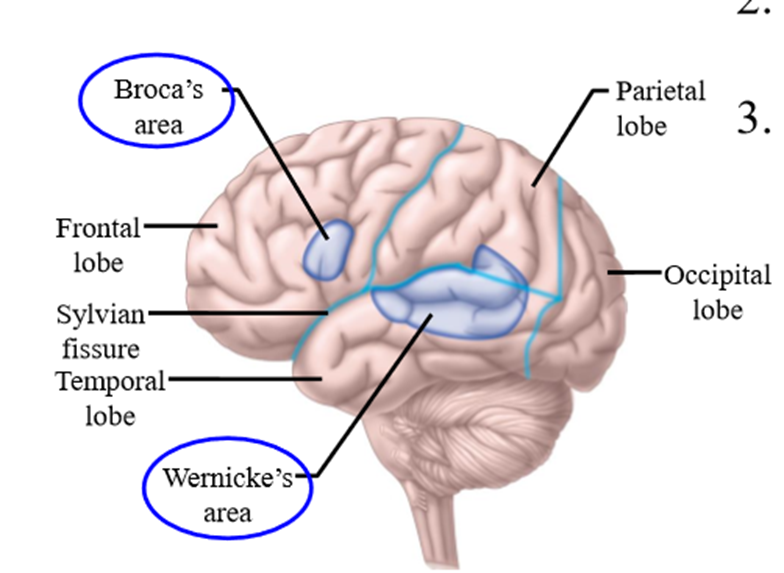
Broca's area lesion
Slurring speech
Wernicke's area function
Comprehension of language + Association of visual, auditory, and tactile input with words
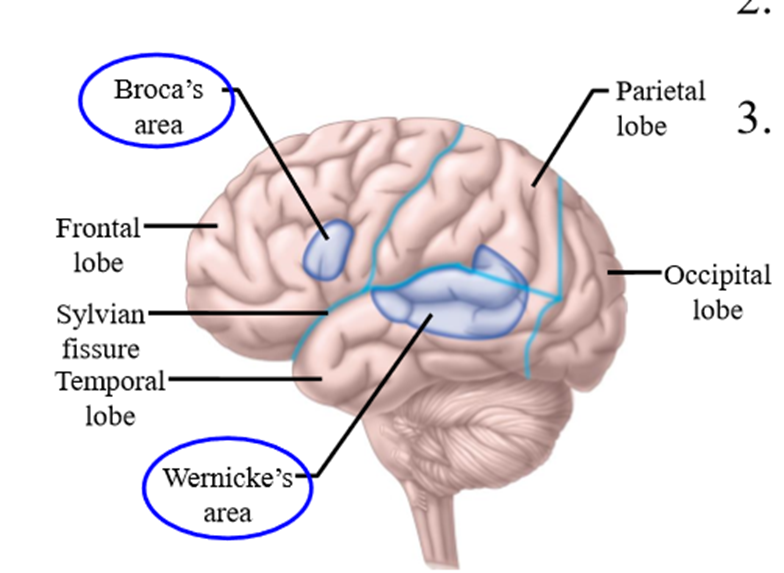
Werenicke's area lesion
Sensory aphasia - difficulty of understanding meaning of words
Dyslexia - Results in difficulty in reading aloud fluently
Example of sensory aphasia
o A person is handed a pen and says it is a spoon. When asked to use it, they write their name
o A problem in producing the correct linguistic response, yet the appropriate motor response is made
o Indicates that the sensory to motor transformation is separate from the sensory to linguistic transformation
PET Scan of language based activities
o Distinct areas of the brain are specialized for hearing, seeing, speaking and generating words