lecture 19, the female reproductive system
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
17 Terms
the female gonads are
ovaries
located in the pelvic cavity on either the uterus
responsible for production of gamete
each ovary consists of 4 layers
superficial epithelium (mesothelium)
simple cuboidal
on surface, wallpaper
tunica albuginea
dense irregular connective tissue
helps the epithelium bind
ovarian cortex
outer layer of the ovary
contains ovarian follicles
all the follicles are developed here
ovarian medulla (internal)
the center area of the ovary
contains blood vessels, lymph vessels
need nerves too
living structure
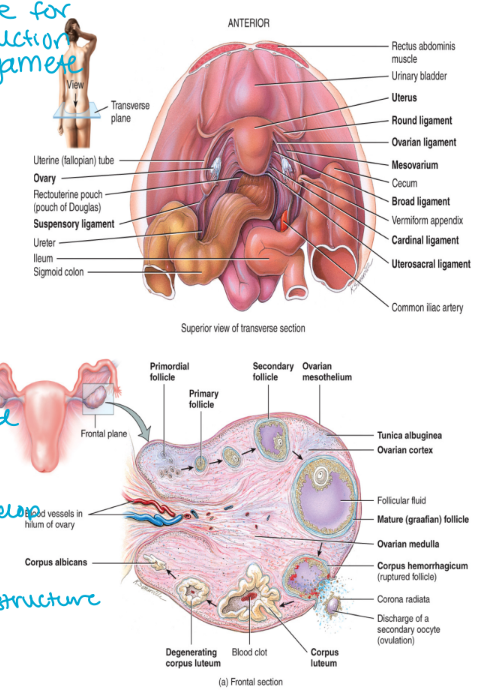
membranes that support the ovary include
mesovarium: suspends the ovary between the uterus (medial) and the pelvic wall (lateral)
suspensory ligament: anchors the ovary to the pelvic wall
the ovarian ligament: attaches the ovary to the uterus
1 and 2 are part of the broad ligament
tents over the uterus supporting the uterine tubes, uterus, and vagina
made from peritoneum
holding things so they don’t wall
oogenesis
refers to the production of gametes within the follicles ovary
oogonia (2n cells)
mitosis
primary oocytes (2n cells), present in the ovary at birth
meiosis I: is completed once per month at puberty
the others stay quiet
they are there since birth
1x secondary oocyte (n cell) + 1x polar body (n cell) which is discarded
structures is ovulated and meiosis II completes following fertilization
1 haploid gets to proceed
putting recycled material elsewhere
wont complete meiosis II if there is no fertilization
1x ovum (n cell) +1x polar body (n cell) which is discarded (still haploid)
one primary oocyte will give rise to one ovum and two polar bodies
polar bodies are the ‘waste’ of the process and are broken down

stages of oogonia/oocyte development (1-2)
first oogonia appear in females 11 weeks post-fertilization
the oogonia begin to undergo mitosis → 2n cells
the oogonia differentiate into primary oocytes → 2 n cells (increase the number)
building a human
diploid cells that will undergo mitosis
there are up to 2 million primary oocytes in the ovaries at bith
these are the total number of oocytes that will ever be present in a female
new oocytes will never form
the primary oocyte is surrounded by a follicle which support and protects the oocyte
you support it for reproductive process
the primary oocyte enter into meiosis I wait in prophase I until puberty begins
at puberty one primary oocyte will undergo meiosis I per month
this produces one secondary oocyte (n) and one polar body (n) which will be discarded (now haploid)
follicle stimulating hormone (FSH) is needed for this development to occur (encourages development)

stages of oogenesis (2-3)
secondary oocyte (n)
begins meiosis II and stops in metaphase II
it is this form of the egg that is released during ovulation each month
there are enough secondary oocytes to provide for ~500 ovulations in a woman’s lifetime
if fertilization, then meiosis II is complete
sister chromosomes not pulled apart yet
go past prophase II
fertilization
this process takes ~24 hours
it begins with fusion of the sperm and the secondary oocyte
trigger
metaphase II and on needs to complete
once fusion occurs the secondary oocyte undergoes meiosis II forming the ovum
the nuclei of the sperm and the ovum fuse following the completion of meiosis II generating zygote
have a nucleus that is now diploid
mitotic divisions now

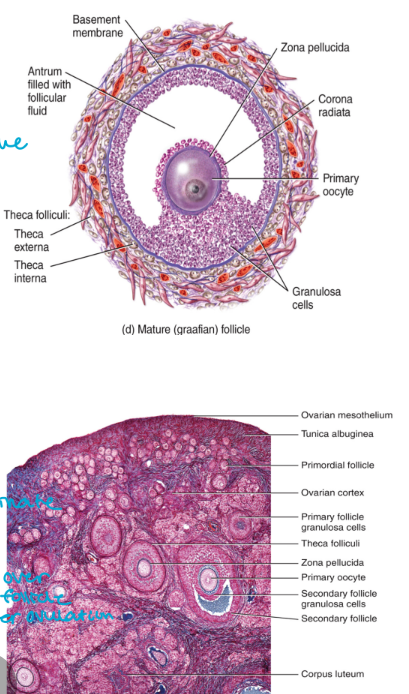
ovarian follicles (1-3)
located in the cortex of the ovary (big space)
primordial follicles
preset in the ovary at birth
the primary oocyte is surrounded by a single layer of flat follicular cells
primary follicles
stratified layer of cells (lots of cell present)
single layer called the granulosa proliferates under the influence f FSH forming the zona pellucida (immediately around oocyte)
the surrounding tissue forms theca cells
the primary follicle contains the primary oocyte is present in childhood
secondary follicles
located in the ovaries during puberty (~250,000 oocyte remain at puberty)
the primary oocyte undergoes meiosis I becoming the secondary oocyte at puberty
the granulosa and theca cells begin secreting estrogen
antrum → fluid filled structure, gets bigger and bigger
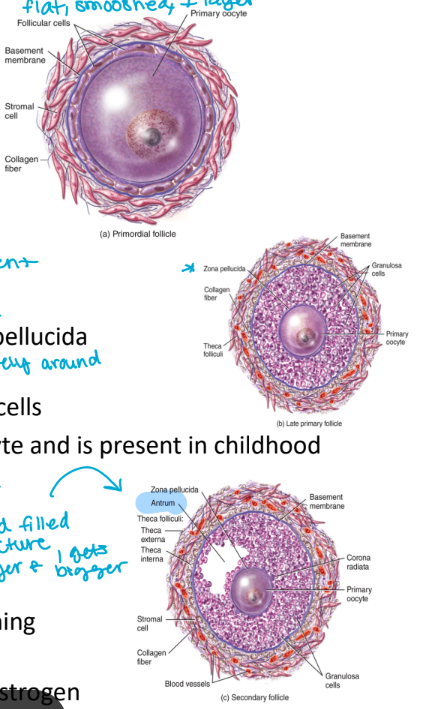
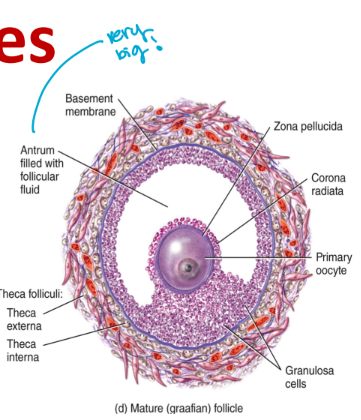
ovarian follicles (step 4)
Graafian follicles (mature secondary follicles)
small fluid-filled sacs merge forming a fluid filled cavity in the follicle called the antrum
this structure moves closer to the ovary surface
the corona radiata is the layer of granulosa cells that immediately surround the oocyte
it is this structure that will be ovulated
rising levels of estrogen produced by the follicle trigger an increase in luteinizing hormone (LH)
the increasing level of LH trigger the completion of meiosis I generating a secondary oocyte → arrests at the beginning of metaphase II (went through meiosis I)
the LH surge also triggers ovulation
the Graafian follicle bursts and release the secondary oocyte into the peritoneal cavity
the ovulated oocyte consists of the oocyte, the zona pellucida and the corona radiata
ovulation
the Graafian follicle remains in the vary without its contents
becomes corpus luteum (estrogen will be kept as endocrine tissue)
endocrine tissue
when it bursts, rest stays
the central space of the follicle fills with blood and clots
the corpus luteum forms from proliferation of the granulosa and theca cells
the corpus luteum functions to produce estrogen and progesterone
if it drops can cause the pregnancy to terminate
if fertilization does not occur the corpus luteum disintegrates and becomes the corpus albicans (left over of follicle after ovulation)
estrogen and progesterone secretion halts resulting in the beginning of a new cycle
source of hormones drop
can count the scar tissue to see how many time one has ovulated
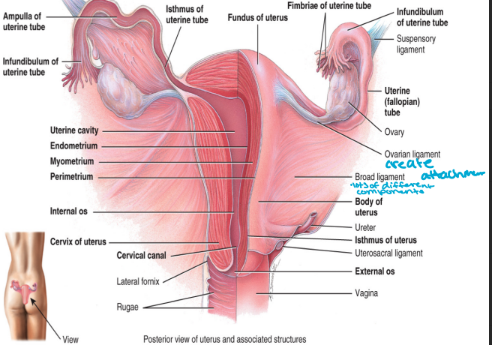
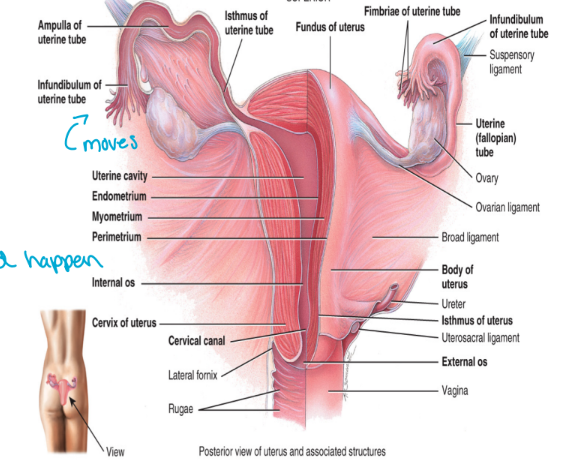
fallopian tubes
also called the uterine tubes
consist of the
infundibulum
contains fimbriae
suspend over the ovary
ampulla
this is the middle 2/3 of the fallopian tubes
where fertilization should happen
isthmus
the portion of the fallopian tube that connects to the uterus
fallopian tube does not contact ovary
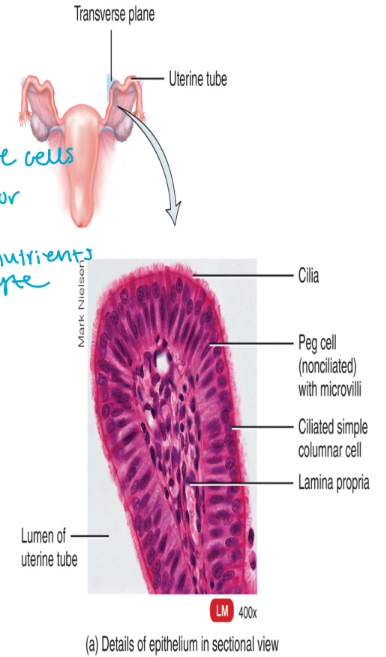
fallopian tube histology
the mucosa
consists of ciliated simple columnar epithelium
cilia assist in the movement of the oocyte along the length of the fallopian tube
there is also non-ciliated columnar epithelial (elongated cells) cells called peg cells → contain microvilli (important for secretions → gives nutrients to oocyte)
secretes a nutrient rich fluid
the mucularis externa
smooth muscle (involuntary)
assists in the movement of the oocyte along the length of the tube with rhythmic contractions
serous membrane
visceral peritoneum
adventitia (out of peritoneum)
low in the abdomen
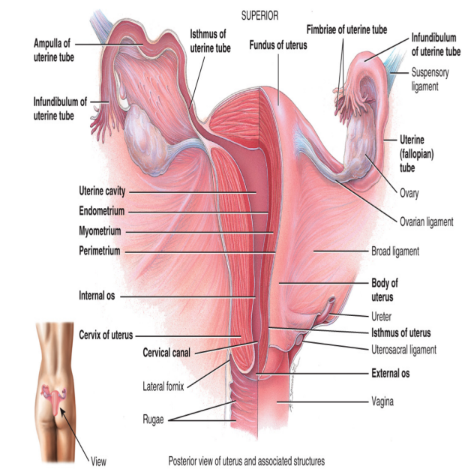
uterus
is attached to the abdominal wall by supportive membranes (if not suspended it will collapse)
broad ligament
portion of the parietal peritoneum (extension)
sheets that drapes over everything
suspends the uterus laterally
round ligament
composed of fibrous connective tissue (anterior surface)
attaches the uterus to the anterior wall of the body
the uterosacral ligament
portion of the peritoneum
attaches the uterus to the sacrum
posterior
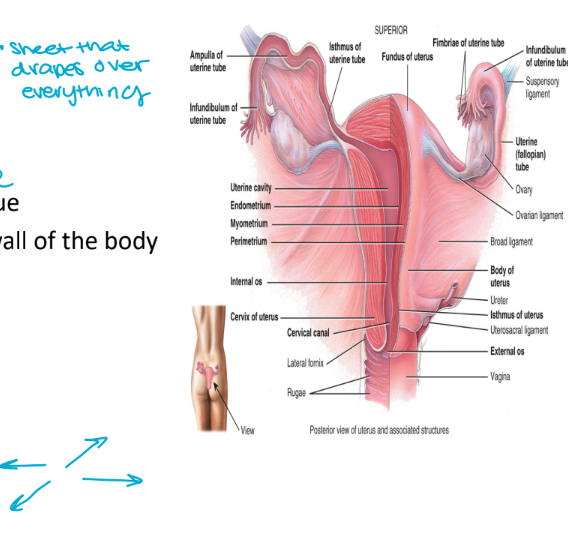
the uterus is a hollow organ consisting of the
fundus which is higher than the fallopian tube level
body which is the major portion of the uterus
cervix which is the inferior, narrow portion of the uterus that opens into the vagina (plug comes out)
the uterine cavity is the space in the body that houses the uterus
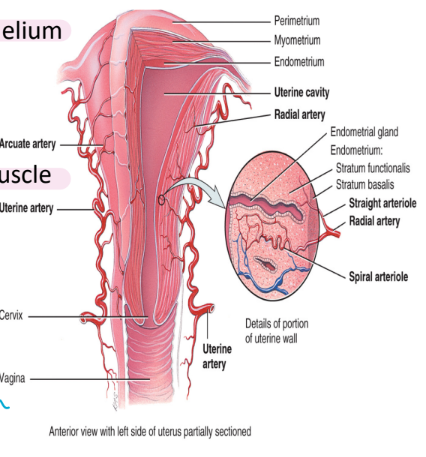
histology of the uterus
consists of 3 layers
the outer peritoneum
the visceral peritoneum → simple squamous epithelium
a serous membrane
the myometrium
composed of the muscularis externa → smooth muscle
three layers total
the endometrium
mucous membrane → open to outside
consists if simple columnar epithelium
endometrial glands (secretions to support growing a human)
thick lamina propria connective tissue
two layers
stratum functionalist: located nearest to the uterine cavity
shed during menstruation (thicker and thicker, trying to create fresh bearing)
stratum basalis: permanent layer that gives rise to a new stratum functionalism after mensuration → mitosis
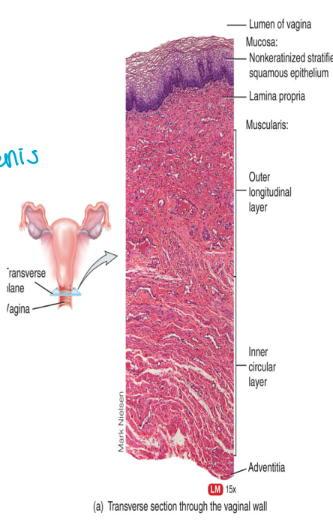
the vagina
functions as the
birth canal
site of sperm deposition and transport
exit for menstrual flow
naturally mean to happen
contains
mucosa
stratified squamous epithelium and connective tissue (for abrasion of baby or penis)
rugae to stimulate the penis and allow for expansion of the vaginal cavity
a muscularis layer
two layers of smooth muscle
facilitates stretching during childbirth and intercourse
elastic
adventitia
areolar connective tissue (covering)
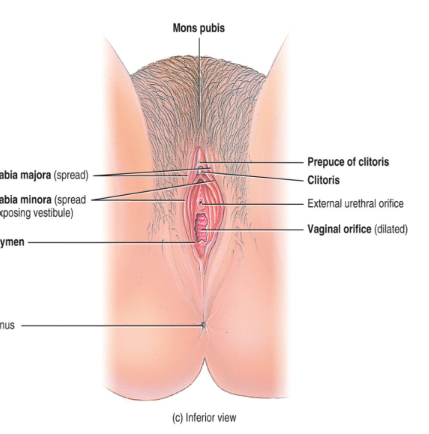
external genitalia
the labia majora has the same origin as the scrotum in the male (just doesn’t drop out)
the labia minora has the same origin as the male penis
the clitoris has the same origin as the erectile tissue of the male penis (fills with blood, vascularity)
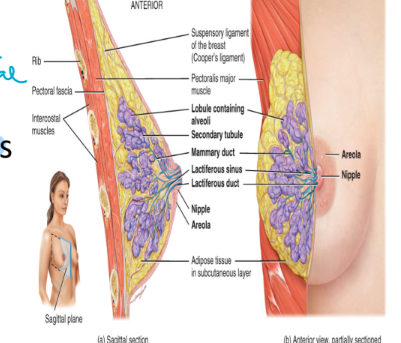
the mammary glands
each breast contains one mammary gland
mammary glands are modified sudoriferous glands that secrete milk
contain small compartments called lobules
lobules contain milk secreting glands called alveoli (connect to central canal)
milk produced in the alveoli move through the lactiferous ducts which open into the nipples
sucking is high to low pressure
the breast lie over top of the pectorals major and the serratus anterior muscles
each breast is attached to the epimysium of the muscle below by sensory ligaments called Cooper’s ligaments
not strong, loose, saggy